Abstract
Background
Patellofemoral pain syndrome (PFPS) is one of the most common disorders of the knee. Conservative approaches, as well as surgery, can decrease pain and the syndrome’s progress effectively.
Objective
The aim of this study was to determine the effectiveness of neoprene palumbo orthosis (NPO) and Genu direxa stable orthosis (GDSO) on pain and the activities of daily living (ADL).
Methods
Thirty patients (males, ages 18 to 40) participated in this randomized blinded clinical trial. All of them were diagnosed with patella femoral pain syndrome. The participants were divided randomly into two groups of 15, with one group using neoprene palumbo (intervention group) and the other group using Genu direxa stable orthoses (control group). Using the Visual Analogue Scale (VAS) and the Knee injury and Osteoarthritis Outcome Score (KOOS), pain intensity and activities of daily living (ADL) and joint stiffness were analyzed before treatment and after three weeks of treatment. Data were analyzed using paired samples t-test and independent samples t-test.
Results
Both orthoses reduced the patients’ pain. Both group showed meaningful improvement in pain reduction and ADL increase after using orthosis in each group. In comparing the variables, no significant differences were found between pain severity and ADL (p = 0.592, p = 0.887). In both groups, the mean of pain severity was different before, during, and after using orthosis (p < 0.05).
Conclusion
The results of this study indicated that Neoprene palumbo and genudirexa stable orthoses improved the signs of patello femoral pain syndrome, including pain intensity and ADL.
Keywords: neoprene palumbo orthosis, Genu direxa stable orthosis, patellofemoral pain syndrome
1. Introduction
Patellofemoral pain syndrome (PFPS) is one of the most common disorders of the knee (1), and it is a frequent phenomenon among athletes (1). According to reports, 25% of the recruits who visited the orthopedic clinic at a military hospital in the U.S. had PFPS. Besides slight changes in the patella’s femoral articular surface, the patients with PFPS had anterior knee pain with different grades in development of PFPS. Since hyaline cartilage is not innervated and is not supplied by any blood vessels directly, it generally cannot be repaired completely. The progression of cartilage lesions causes erosion to the subchondral bone, where there are many nerves, and the result is knee pain. Common reasons for hyaline erosion are trauma, bearing weight on a bent knee, especially in squatting and twisting positions, patellar subluxation and dislocation, abnormal size of patella, and hitting the knee on the dashboard in a car accident. Anterior knee pain in patients with PFPS typically occurs with activity and often worsens when they are descending steps or hills. It also can be triggered by prolonged sitting with the knee flexed. People tend to notice the pain particularly when going up or down stairs, squatting, kneeling, or running. It may also be aggravated by long periods of sitting with the knees bent (2). Sleeping with the knee bent is painful at night and decreases with knee’s extension. (3). The misalignment of the patella may occur for various reasons. One of the main causes in adolescents is an imbalance in strength between the medial and lateral muscles. One of the more popular theories in that this syndrome results from an imbalance in strength of the muscles that surround the patella (4). Although the medial and lateral parts of the quadriceps muscle and the Iliotibial band have important roles in the dynamic stability of the patella, the vastus medialis muscle has the most important role in balance and stability. Weakness, atrophy, and dysplasia shift the pressure zone from the center to the lateral facet of the patella and pain results from cartilage defects (5). Surgery for PTPS is considered to be the resort, and medical associations propose conservative approaches, such as medication, exercise, physical therapy, and orthotic devices, which can decrease and sometimes stop the progress of PTPS. Orthoses maintain the patella in the intercondylar groove during movement and decrease the severity of loads on the subchondral bone. Managing PTPS is a challenge because of the lack of consensus regarding its cause and treatment, so the treatment approach should be individualized by identifying its mechanisms and causes. Research has shown that orthoses can improve ADL in patients with PTPS (6). Grossland et al. stated the orthotic treatment increased ADL in 145 patents with patella dislocation, as 64% of the patients who wore knee sleeves for four weeks had reduced pain (7). In another study of 62 patients with patella dislocation and chondromalacia, Palumbo orthosis decreased the syndrome’s symptoms in 93% patients, and they could do activities they could not do before (8). Powers et al. investigated the influence of Donjoy orthosis and found that it reduced the intensity of the pain in the patellofemoral joint (9). In another study, the effect of orthosis on the strength of the quadriceps muscle was evaluated, and 88% of the patients with orthosis for four weeks had increased knee function and reduced pain (10). Although research has shown the benefits of orthoses in treating PTPS, there is a lack of evidence for the use of Neoprene palumbo and Genu direxa stable orthosis. The palumbo orthosis is made of neoprene with a patellar cut-out that prevents lateral shift of the patella (11). The Genu direxa stable orthosis is similar to the Palumbo orthosis, but it has two straps and a C-shaped lateral buttress to keep the patella from deviating too far laterally (11). These orthoses are recommended for reducing pain and increasing the function of patients with PTPS. The objective of this research was to determine the effects of neoprene palumbo and genu direxa stable orthoses on pain and ADL of patients with patello femoral pain syndrome.
2. Material and Methods
2.1. Research design, setting, and sampling
This research was a randomized blinded clinical trial. We allocated 30 male patients (18–40 years old) with patello femoral pain syndrome randomly into two groups (with 15 patients in each group). All subjects were evaluated and chosen in Shafa yahyaan and Valiasr Hospitals (Arak, Iran). People with BMIs of 20 kg/m2 or less are underweight, while people with BMIs of 40 or greater are extremely obese. The 30 participants in this study had normal BMIs in the range of 20–25 kg/m2. All participants (30 patients) were chosen and allocated into to two groups with 15 patients in each group. The patients in one group used the Neoprene palumbo orthosis for three weeks, and the patients in the other group used the Genu direxa stable orthosis for three weeks. At the start of this trial, a sample size of 30 patients was selected to provide 80% power to detect a reduction in the incidence of a defined set of acute complications from 30% to 15% at p = 0.05. Patients were divided randomly into two groups of 15 patients. Fifteen of the patients used the Neoprene palumbo orthosis for three weeks, and 15 patients used the Genu direxa stable orthosis for three weeks.
2.2. Selection criteria
All subjects were evaluated and chosen in Shafa yahyaan and Valiasr Hospitals (Arak, Iran) according to following inclusion criteria: 1) the duration of complaints was 2–6 months, 2) existing pain in patella or anterior of knee, 3) obtaining the written informed consent, 4) Body Mass Index (BMI) between 20 kg/m2 and 25 kg/m2, 5) age between 18 and 40 years, and 6) having a minimal value of 4 on the Visual Analogue Scale (VAS). Also, the exclusion criteria were: 1) having no limitation in the movement of the lower limb, and 2) Not taking pain killers.
2.3. Data collection method
The participants gave written informed consent after we had obtained baseline measures, including VAS and BMI. The visual analog scale (VAS) is a tool that is used extensively to measure pain. Patients were asked to indicate their perceived pain intensity (most commonly) along a 100-mm horizontal line. Number 0 means no pain and number 100 means maximum pain in the knee. BMI was calculated by dividing the patient’s weight in kilograms by the patient’s height in meters squared (BMI = X kg/m2). Before wearing the orthosis, the patients completed a Knee injury and Osteoarthritis Outcome Score (KOOS) questionnaire modified for osteoarthritis patients and knee injuries to evaluate the patients’ ADL (12). Because of differences in ADL during a day, we conducted the measurements between 8:00 and 9:00 A.M.
2.4. Using the effect of the orthosis on ADL and the level of pain
Patients were asked to consider different amount of pain before getting the orthosis (VAS1), and they were asked to repeat their VAS rating after wearing the orthosis and descending 10 steps from a short form (VAS2) and after wearing the orthosis for three weeks (VAS3). The patients were instructed how to put the orthosis on and how to take it off, and they were told to only take it off when they went to bed. They also were asked not to take any kind of pain killers and not to go to physical therapy. There were some multi-option questions in the questionnaire about joint rigidity, pain intensity, ADL, sports activity, and life quality. Each question had a score between 0–40 and each variable could have a score of between 0–100. The following equation shows how the total score was calculated for each variable: “Total score = (score × 100)/( 100 – 4) × number of questions”. A score of 0 means no pain, and a score of 10 means extreme pain. For instance, a patient who indicated a score of 55 for pain before the orthotic treatment and a score of 45 after orthotic treatment indicated that the orthotic intervention reduced the patient’s pain.
2.5. Statistical methods
Statistical analysis was done using SPSS software (version 13.0). The normal distribution was analyzed with the Kolmogorov-Smirnov test. We also compared pain reduction in three stages (VAS1, VAS2, and VAS3) with the repeated measure and paired t-test. The correlation between BMI and the intensity of pain were determined using the Pearson correlation coefficient.
2.6. Research ethics
The study was approved by the Research Ethics Board at the Iran University of Medical Sciences (CF07/4208). Approval was also obtained from the Iran University of Medical Sciences Research Ethics Committee at each participating site. Research Ethics Board approvals were kept current for the duration of the study. The trial was registered at the Iranian Registry of Clinical Trials and Current Controlled Trials IRCT138810112946N1. Also this study was conducted according to the Declaration of Helsinki, the Australian NHMRC National Statement on Ethical Conduct in Human Research 2007 (13) the Notes for Guidance on Good Clinical Practice as adopted by the Australian Therapeutic Goods Administration 2000 CPMP/ICH/135/95 (14) and the ICH GCP Guidelines.
3. Results
3.1. VAS and Koos questionnaires
We studied 30 males aged 18–40 with patellofemoral pain syndrome and normal weight-based BMI. The patients indicated the intensity of their pain using the VAS and assessed their quality of life in their daily living activities using a modified Koos questionnaire. Significantly, patients indicated that they had reduced pain after wearing the orthosis for three weeks as the mean (95% confidence interval) for VAS reduced from 49.05 (10.93) to 31.26 (4.38) and from 53.51 (3.70) to 31.47 (3.42) by using Neoprene Palumbo and Genu direxa orthoses, respectively.
3.2. Effect of using the orthosis on ADL level
There was a significant difference in ADL levels before and after using the orthosis in the two groups, since the mean was reduced from 35.48 (4.79) to 3.03 (25.58) and from 41.58 (3.96) to 25.09 (1.71) for patients with Neoprene palumbo and Genu direxa stable orthoses, respectively. These results showed an increase in the level of ADL for all patients. There was a significant difference between the mean for joint tightness in all patients after wearing the orthosis for three weeks (p < 0.05), since it was 47.11 (9.09) and 51.38 (7.36) before wearing the orthosis, and it was reduced to 33.52 (5.36) and 31.63 (7.61) for the palumbo and Genu direxa stable orthoses, respectively.
3.3. Effect of using the orthosis on the pain level
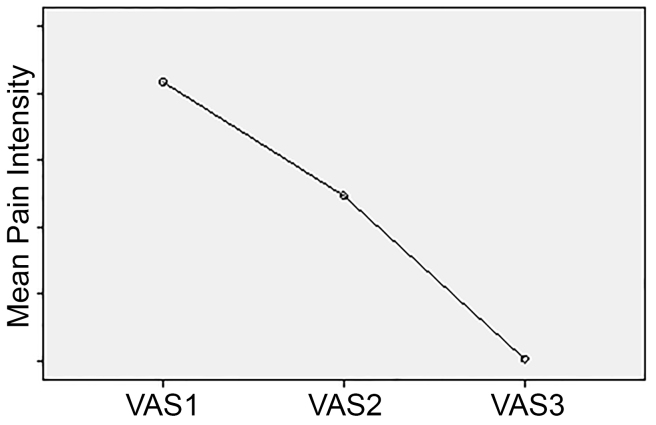
In comparing the baseline VAS, there were significant differences before, during, and after orthotic treatment in all patients (p < 0.05) (Table 1 and Figure 1). No statistical correlation between BMI and mean VAS before and after treatment was found in this study (p = 0.048).
Table 1.
Mean pain intensity before, during, and after orthotic treatment
| Pain intensity before, during, and after orthotic treatment | Mean Pain Severity | S.D. | p-value |
|---|---|---|---|
| VAS1 | 6.1667 | 1.34121 | <0.001 |
| VAS2 | 4.4667 | 1.43198 | <0.001 |
| VAS3 | 2.0333 | 0.76489 | <0.001 |
Figure 1.
Mean pain intensity before, during, and after three weeks of orthotic treatment
4. Discussion
4.1. VAS and Koos questionnaires
One of the most common sites of injury in physically-active adolescents and young adults is the knee; the patellofemoral pain syndrome is the most frequent complaint (11). Managing patellofemoral pain syndrome is a challenge, in part because of lack of consensus regarding its cause and treatment. This syndrome prevents patients from continuing their normal activities, because the pain has mental and psychological effects on the patient’s life. For instance, a runner or mountain climber cannot continue her or his activities (12).
4.2. Effect of using the orthosis on ADL level
In this syndrome, using an orthotic is one of the conservative, non-surgical methods that specialists recommend in the acute stage. In this research, we compared the effects of Neoprene Palumbo orthosis and Genu Direxa Stable orthosis on the intensity of pain and the ADL of patients with patellofemoral pain syndrome. The findings indicated that both orthoses reduced pain in the knee cap significantly. The pain may have been reduced by preventing lateral shifts in the patella and preventing deviation in the intertrochanteric groove (13, 14). Orthosis also may compensate for vastus medialis and iliotibial band inefficiency and may reduce pain by maintaining the patella’s dynamic stability. According to the statistical analysis, these orthoses increased the level of activity of daily living, including ascending stairs and sitting.
4.3. Effect of using orthosis on the pain level
In this study, we did not find any meaningful or statistical difference between patients who used Palumbo or Genu direxa stable orthoses with respect to their increased ADL or decreased pain. This research and other studies have presented the effects of orthotic treatment on PTPS, and it was concluded that orthosis can reduce pain by reducing the load applied to the subchondral bone (13). The orthosis also allowed increased levels of activity, including doing exercises, sitting, and ascending and descending stairs. The orthosis may affect the rigidity of the joint by increasing the level of activities and joint movements, thereby significantly increasing the range of motion and rigidity of the tibiofibular and patellofemoral joints (14). As a result, patients feel less rigidity and tightness in the knee joint after using orthoses because of the improvement in the components of the joint, such as cartilage.
5. Conclusions
This study indicated that Neoprene palumbo and Genu direxa stable orthoses improved the signs of patello femoral pain syndrome including the intensity of the pain and the activities of daily life. More studies are required to determine the most effective orthosis and its influence on the causes of patellofemoral pain syndrome.
Acknowledgments
The authors gratefully acknowledge the financial support for this work that was provided by the Iran University of Medical Sciences (IUMS).
Footnotes
iThenticate screening: August 15, 2015, English editing: August 26, 2015, Quality control: October 02, 2015
Trial registration: The trial was registered at the Iranian Registry of Clinical Trials (http://www.irct.ir) and Current Controlled Trials IRCT138810112946N1.
Fund: Funding for the research was provided by the Iran University of Medical and Health Services (No.: 89325-34).
Conflict of Interest: There is no conflict of interest to be declared.
Authors’ contributions: Both authors contributed to this project and article equally. Both authors read and approved the final manuscript.
References
- 1.Hinman R, Crossley K, McConnell J, Bennell K. Does the application of tape influence quadriceps sensorimotor function in knee osteoarthritis? Rheumatology. 2004;43(3):331–6. doi: 10.1093/rheumatology/keh033. [DOI] [PubMed] [Google Scholar]
- 2.Schache AG, Dorn TW, Williams GP, Brown NA, Pandy MG. Lower-limb muscular strategies for increasing running speed. J Orthop Sports Phys Ther. 2014;44(10):813–24. doi: 10.2519/jospt.2014.5433. [DOI] [PubMed] [Google Scholar]
- 3.Turek SL. Orthopedics principles and their application. 4th ed. Philadelphia: Lippincott J.B; 1989. [Google Scholar]
- 4.Donell ST, Glasgow MM. Isolated patellofemoral osteoarthritis. Knee. 2007;14(3):169–76. doi: 10.3109/17453671003628756. [DOI] [PubMed] [Google Scholar]
- 5.Ghasemi M, Bell F, Hullin M. Biomechanics of the lower limb in patients with anterlor knee pain. Gait Posture. 1995;3(3):186–7. doi: 10.1016/0966-6362(95)99127-7. [DOI] [Google Scholar]
- 6.Magee DJ. Orthopedic physical assessment. Elsevier Health Sciences; 2014. [Google Scholar]
- 7.Herrington L, Malloy S, Richards J. The effect of patella taping on vastus medialis oblique and vastus laterialis EMG activity and knee kinematic variables during stair descent. J Electromyogr Kinesiol. 2005;15(6):604–7. doi: 10.1016/j.jelekin.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Earl JE, Piazza SJ, Hertel J. The Protonics knee brace unloads the quadriceps muscles in healthy subjects. J Athl Train. 2004;39(1):44. [PMC free article] [PubMed] [Google Scholar]
- 9.Nester C, Van Der Linden M, Bowker P. Effect of foot orthoses on the kinematics and kinetics of normal walking gait. Gait Posture. 2003;17(2):180–7. doi: 10.1016/S0966-6362(02)00065-6. [DOI] [PubMed] [Google Scholar]
- 10.Powers CM, Chen P-Y, Reischl SF, Perry J. Comparison of foot pronation and lower extremity rotation in persons with and without patellofemoral pain. Foot Ankle Int. 2002;23(7):634–40. doi: 10.1177/107110070202300709. [DOI] [PubMed] [Google Scholar]
- 11.Bunch WH, Keagy RD. Principles of orthotic treatment. 1st ed. Baltimore: Lippincott, Wiliams & Wilkins; 1976. [Google Scholar]
- 12.Negahban H, Mostafaee N, Sohani SM, Mazaheri M, Goharpey S, Salavati M, et al. Reliability and validity of the Tegner and Marx activity rating scales in Iranian patients with anterior cruciate ligament injury. Disabil Rehabil Assist Technol. 2011;33(22–23):2305–10. doi: 10.3109/09638288.2011.570409. [DOI] [PubMed] [Google Scholar]
- 13.Health N, Council MR. National statement on ethical conduct in human research. Intern Med J. 2007 doi: 10.1111/j.1445-5994.2011.02528.x.. [DOI] [PubMed] [Google Scholar]
- 14.OF CWPOE. MEDICINAL PRODUCTS. EEC note for guidance: good clinical practice for trials on medicinal products in the European Community. CPMP Working Party on Efficacy of Medicinal Products. Pharmacol Toxicol. 1999;67:361–72. doi: 10.1111/j.1600-0773.1990.tb00847.x. [DOI] [PubMed] [Google Scholar]