BACKGROUND
The optimal geographic configuration of health care systems is key to maximizing accessibility while promoting the efficient use of resources. This article reports the use of a novel approach to inform the optimal configuration of a national trauma system.
METHODS
This is a prospective cohort study of all trauma patients, 15 years and older, attended to by the Scottish Ambulance Service, between July 1, 2013, and June 30, 2014. Patients underwent notional triage to one of three levels of care (major trauma center [MTC], trauma unit, or local emergency hospital). We used geographic information systems software to calculate access times, by road and air, from all incident locations to all candidate hospitals. We then modeled the performance of all mathematically possible network configurations and used multiobjective optimization to determine geospatially optimized configurations.
RESULTS
A total of 80,391 casualties were included. A network with only high- or moderate-volume MTCs (admitting at least 650 or 400 severely injured patients per year, respectively) would be optimally configured with a single MTC. A network accepting lower-volume MTCs (at least 240 severely injured patients per year) would be optimally configured with two MTCs. Both configurations would necessitate an increase in the number of helicopter retrievals.
CONCLUSION
This study has shown that a novel combination of notional triage, network analysis, and mathematical optimization can be used to inform the planning of a national clinical network. Scotland’s trauma system could be optimized with one or two MTCs.
LEVEL OF EVIDENCE
Care management study, level IV.
KEY WORDS: Trauma systems, geographic information systems, multiobjective optimization
The configuration of health care services is of key importance when expeditious access to complex care is required, such as after major trauma. A trauma system is a regional network of designated trauma centers, with stratified capability, supported by emergency medical services, which aims to match patients’ needs with hospitals’ resources. Treatment within a trauma system has been shown to be associated with improved mortality and functional outcomes.1–3 Level I trauma centers (or, in Europe, major trauma centers [MTCs]) are specialist facilities designed to provide optimal care for the most severely injured patients. The time required to reach definitive care is recognized as a key determinant of outcome.4
Trauma system configuration is a topical and often contentious issue. This applies not only to developing networks, as in England and Scotland, but also to existing systems, as in North America. Historically, the configuration of a trauma system was often not considered as a whole but instead hinged on the designation and verification of individual hospitals as trauma centers. Furthermore, although the decision to seek trauma center status was based in part on need, other drivers included individual and institutional commitment as well as social, political, and economic considerations. The latter, in particular, have prompted concerns regarding the rapid expansion in the provision of trauma centers, potentially in excess of community need, resulting in a dilution of expertise.5 Political considerations are often founded on the paradigm that immediate access to care must be best when there is evidence that traveling further to a center capable of providing definitive care may be associated with better outcomes.6,7
Recognition of the benefits of an inclusive trauma system8 has precipitated a more holistic approach. Geospatial optimization—the siting of centers according to the geographic distribution of the injured population—has the potential to benefit both patients and institutions, by facilitating prompt access and promoting the efficient use of resources. A systematic approach to trauma system design can furthermore help to reassure stakeholders that the best configuration has been chosen.9 However, previous efforts to produce data-driven solutions to trauma system design have shortcomings, prompting the development of a novel approach, by our group, termed Geospatial Optimization of Systems of Trauma Care (GEOS).9
Scotland is in the process of establishing a national trauma system, which is due to go live in 2016. The currently proposed configuration of the network, following a series of stakeholder meetings, is for a system with four MTCs.10 However, several authorities—including the Royal College of Surgeons of Edinburgh—have expressed concerns that four MTCs may be too many.11 The aim of this study was to use the GEOS approach to identify geospatially optimized trauma network configurations for Scotland, to inform policy.
PATIENTS AND METHODS
Study Design
The methodology has been described in detail in a previously published article.9 In summary, this study involved the prospective collection of data on all trauma patients attended to by the Scottish Ambulance Service (SAS) and Emergency Medical Retrieval Service (EMRS) in Scotland, for a complete year. Patients were notionally triaged to appropriate levels of care, on the basis of clinical need. A modeling of all mathematically possible trauma system configurations was then undertaken, using a combination of network analysis and multiobjective optimization, identifying optimal network configurations. The study was considered by the North of Scotland Research Ethics Service and deemed a service evaluation and therefore did not require ethical approval. It was approved by the SAS Caldicott guardian (body responsible for electronic patient data access).
Prospective Triage
Scotland has a population of 5.3 million, concentrated in four major conurbations (Fig. 1). Prehospital care is provided by the SAS and the EMRS. Between July 2013 and June 2014, every patient 15 years and older, for whom a final diagnostic code relating to physical injury was recorded by the ambulance crew, was notionally triaged, using the Field Triage Decision Scheme.12 We did not include children because the organization of a pediatric trauma system differs. To enable the notional triage, bespoke data collection screens were added to the ambulances’ electronic patient record system. Patients who met the criteria of Step 1 of the triage algorithm (physiologic derangement) or Step 2 (critical injuries) were triaged to the highest level of care (MTC, equivalent to a North American Level I trauma center). Patients who met the criteria of Step 3 (mechanistic criteria) or Step 4 (special considerations) were triaged to trauma unit (TU) care. (A TU is broadly equivalent to a North American Level II/III trauma center.) All other patients were triaged to local emergency hospital (LEH) care (equivalent to a Level IV/V trauma center or nondesignated hospital). This algorithm is summarized in Figure 2. The electronic patient record also included clinical, demographic, and location data.
Figure 1.
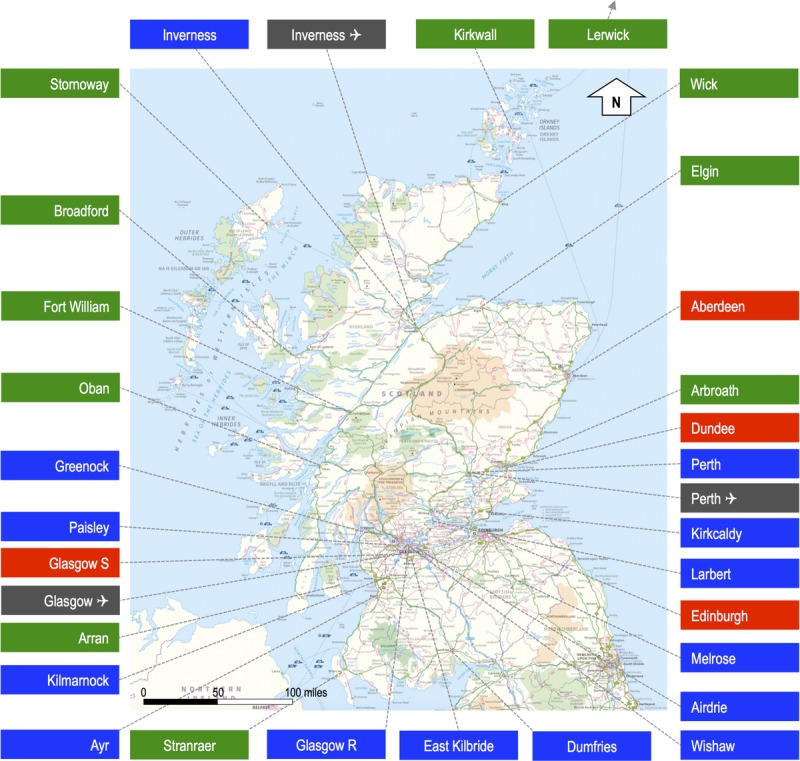
Study area and locations of candidate hospitals (excluding Shetland Isles). Locations in red indicate hospitals that could become MTCs, TUs, or LEHs. Locations in blue indicate hospitals that could become TUs or LEH. Hospitals in green could only become LEHs. The map also shows the locations of the three airfields with aeromedical retrieval assets. (Contains public sector information licensed under the Open Government Licence v3.0.).
Figure 2.
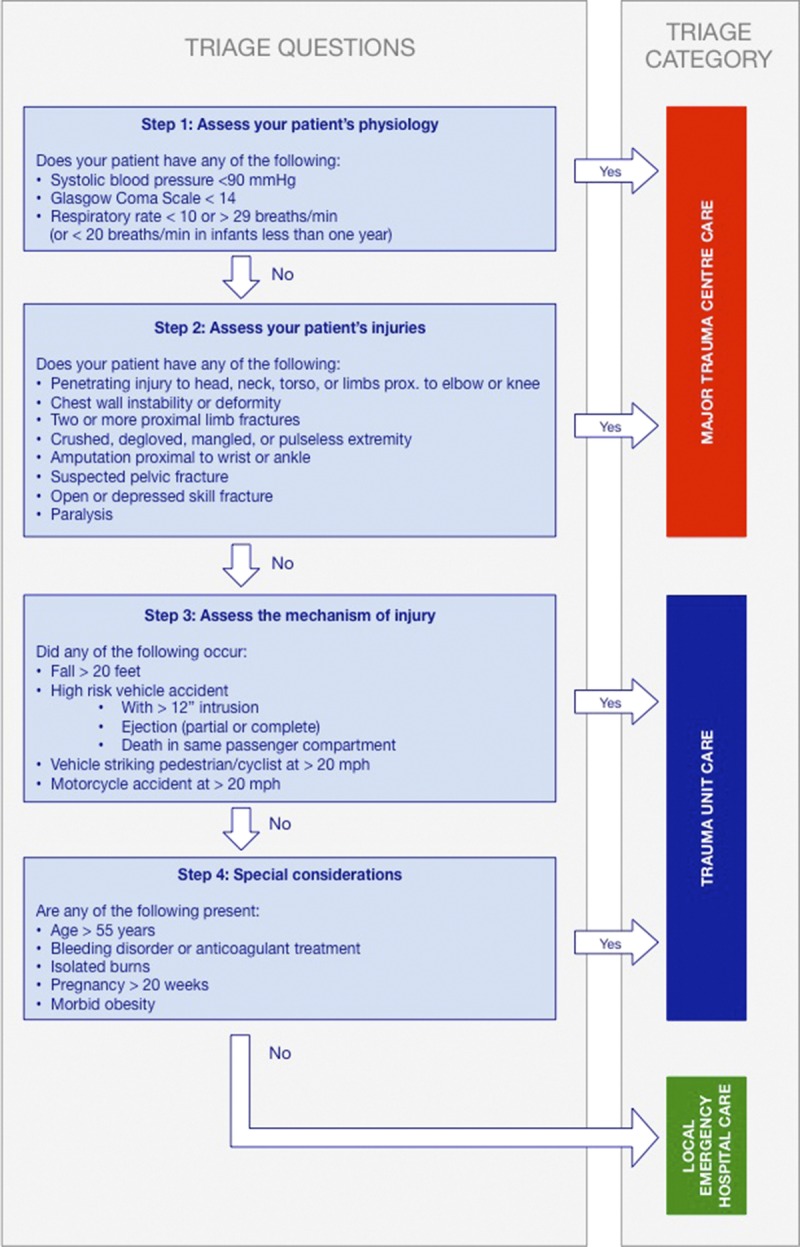
Triage algorithm.
Configuration Modelling
We used incident location data to calculate drive times and flight times from every incident location to every hospital in Scotland, which could potentially become an MTC or TU. In total, there were 18 candidate hospitals that could become TUs (Fig. 1), of which 4 (in the major cities of Glasgow, Edinburgh, Aberdeen, and Dundee) could also become MTCs, yielding more than 2 million mathematically possible configurations. Calculated drive times were adjusted to account for traffic conditions, considering time of the day, day of the week, road type, and population density. Ambulances conveying patients triaged to MTC care were assumed to travel at “blue-light speeds”. Flight times considered stand-to times, flight time from base to incident location, average loading times, and flight time to destination and assumed night-flying capability.
We then analyzed which hospital each patient would have gone to, given any particular configuration of trauma system, using a set of decision rules (Fig. 3).9 We used an access time threshold of 45 minutes, as used by many trauma systems. We also performed a sensitivity analysis, modeling a threshold of 60 minutes. Patients who could not have reached the desired level of care within this time frame were modeled as having been diverted to a lower-level center and flagged as “exceptions.” We assumed a maximum possible number of seven flights per helicopter per day based on average mission duration. For each analyzed configuration, we calculated the predicted total and median system travel times and the number of patient exceptions.
Figure 3.
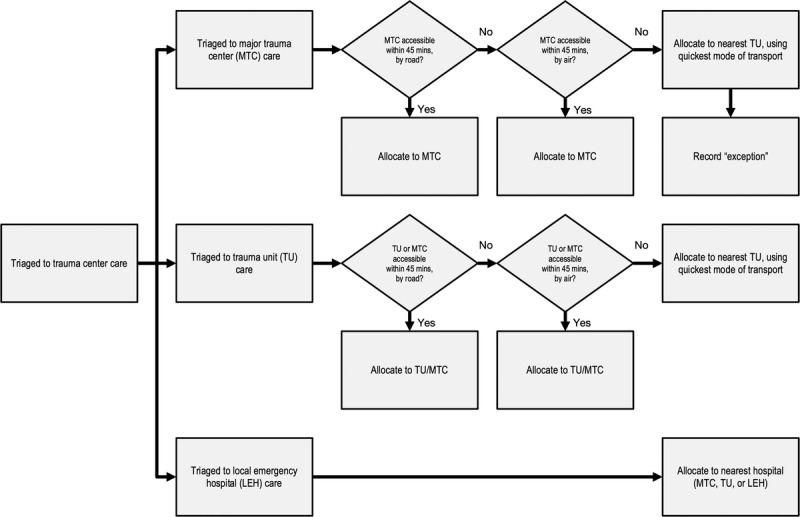
Tasking algorithm.
Statistical Analysis
We used a multiobjective optimization algorithm, which searches for optimal solutions to problems with two or more conflicting objectives, to determine geospatially optimized trauma system configurations. Specifically, we used the Non-dominated Sorting Genetic Algorithm (NSGA-2),13 with the objectives of minimizing total system travel time and minimizing the number of exceptions, reflecting the “time to definitive care” paradigm.4 The output is composed of a set of mathematically equal solutions, which cannot be mathematically or numerically ranked, as they are all deemed “optimal” (or “Pareto optimized”). The number of solutions can, however, be reduced by applying certain constraints. We selected the predicted annual volume of severely injured patients in the MTCs and the number of helicopters required as constraints. The choice of the former was based on the recognized relationship between trauma center case volume and mortality.4,14,15 We modeled minimum thresholds of at least 650 (“high volume”), 400 (“moderate volume”), and 240 (“low volume”) severely injured patients per year, as defined by Injury Severity Score (ISS). The number of severely injured patients per hospital was calculated from the number of patients triaged to each category, using coefficients based on Scottish Trauma Audit Group registry data, and the published sensitivity of the Field Triage Decision Scheme.16 The annual volume of severely injured patients in MTCs was calculated from the number of patients who were primarily admitted as well as the number of severely injured patients transferred secondarily from TUs, assuming a 90% transfer rate, to allow for patients deemed not to require specialist care or receiving palliative care.
We sequentially analyzed different constraints, reflecting priorities in system design. In essence, we attempted to maximize MTC case volume, using the smallest number of helicopters. If no feasible or acceptable solutions were obtained for a given case volume threshold, we increased the number of helicopters, to a maximum of double the current configuration. The performance characteristics of each trauma system configuration, which we examined, included the estimated number of primarily admitted patients (directly from the scene) with severe injury (per center), the number of interfacility transfers of patients with severe injury, the total number of severely injured patients (including interfacility transfers) per center, the median access time for all patients, the median access time for patients triaged to MTC care and taken to an MTC, and the number of helicopter flights required. Data were collated using Microsoft Excel (Microsoft, Redmond, WA). The modeling and multiobjective optimization were performed using MatLab (MathWorks, Natick, MA).
RESULTS
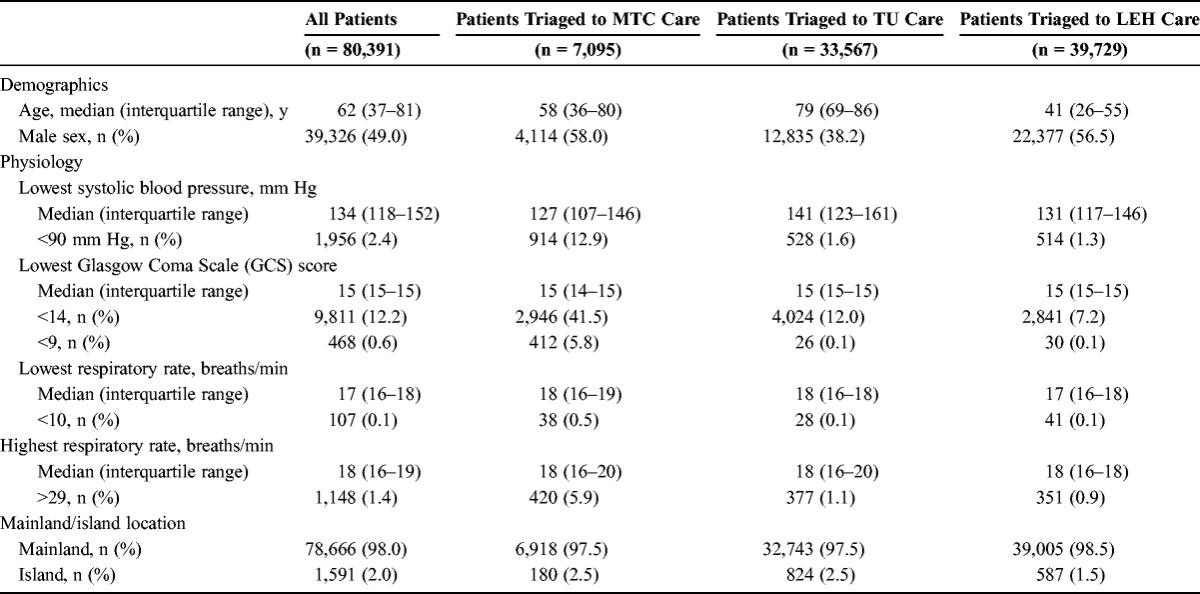
In total, 80,391 casualties were attended to by the SAS and EMRS over the year, underwent notional triage, and were included in our analysis. The median age was 62 years (interquartile range, 37–81 years). A total of 1,599 (1.9%) of incidents occurred on islands. Of the patients, 80,202 (99.8%) were retrieved by road ambulance and 192 (0.2%) by helicopter. A total of 7,095 (8.8%) were notionally triaged to MTC care, 33,567 (41.8%) to TU care, and 39,728 (49.4%) to local emergency hospital care. The groups, as expected, differed in terms of demographic and physiologic characteristics (Table 1). The spatial distribution of the incidents has been described previously.17
TABLE 1.
Characteristics of Study Population
Networks With High- or Moderate-Volume MTCs
There were 21 optimized configurations for a network with high- or moderate-volume MTCs. (Modelling and optimization with both volume thresholds produced the same set of results.) Nine of these configurations would require five helicopters, and the remainder, six. There were no feasible high- or moderate-volume configurations based on the current fleet size of three helicopters or four helicopters. The nine optimized configurations with the smallest number of helicopters all had one MTC, in Glasgow, and between 10 and 17 TUs (Table 2, Configurations A to I). Eight hospitals featured as TUs in all nine configurations. Configurations with a smaller number of TUs would be predicted to result in an increase in median travel time, a decrease in the proportion of patients reaching their destination within 45 minutes, an increase in the number of helicopter flights required, and a small decrease in the number of exceptions (as a result of more patients being taken to MTCs by helicopter). The reconfiguration of services in Scotland is currently focused on MTCs, and it is therefore likely that all hospitals that could become TUs would be designated as such. This configuration (Configuration A in Tables 2 and 3) would result in an estimated 864 severely injured patients per year being taken to the MTC in Glasgow. Of these, an estimated 328 would be primary admissions, and 536 would be secondary transfers. The latter figure includes both patients who could not primarily reach an MTC within the desired time, for geographic reasons, despite being triaged to MTC care, and those who were incorrectly triaged and mistakenly taken to a TU, as a result of the limited sensitivity of the triage protocol. The median access time for patients triaged to MTC care, who would be taken to an MTC, was estimated to be 21.9 minutes (Table 3).
TABLE 2.
Optimized Network Configurations
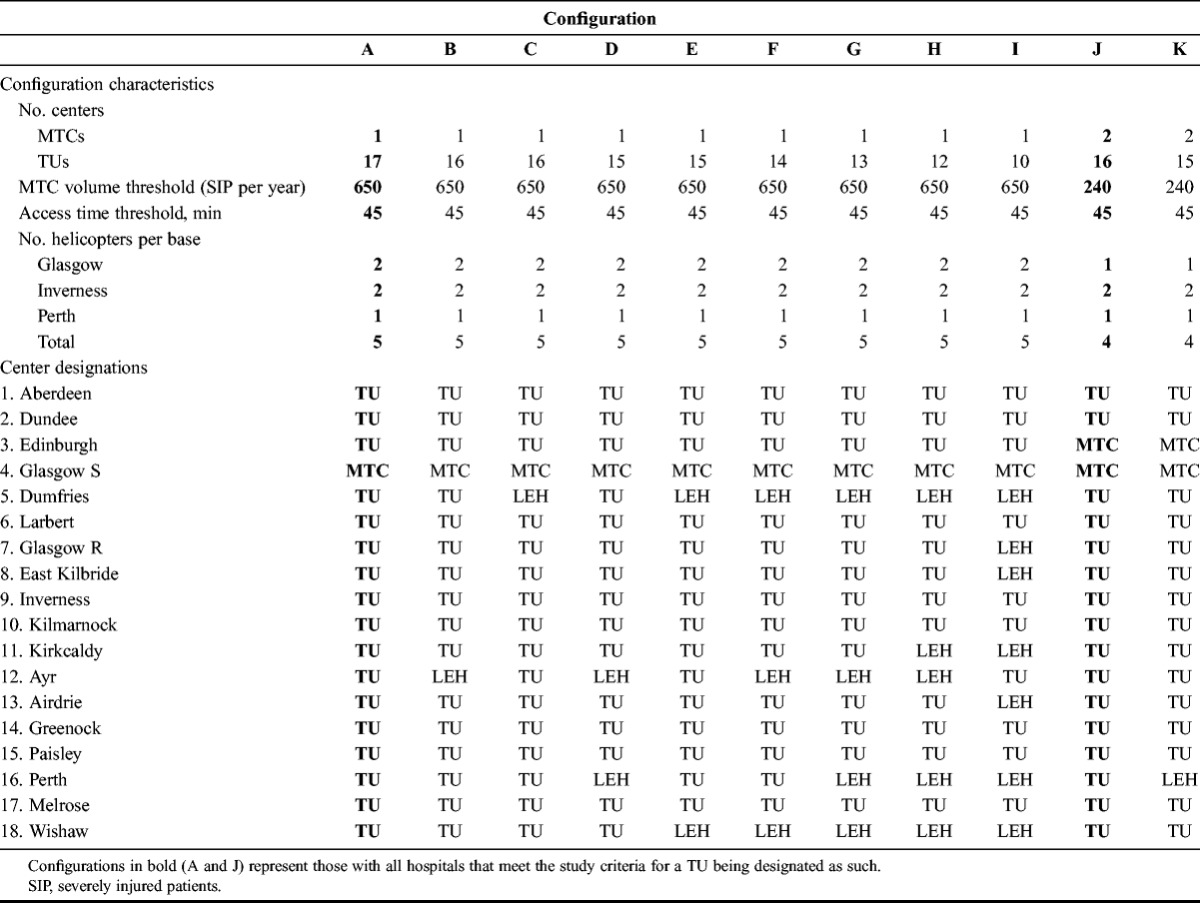
TABLE 3.
Predicted Performance of Optimized Network Configurations
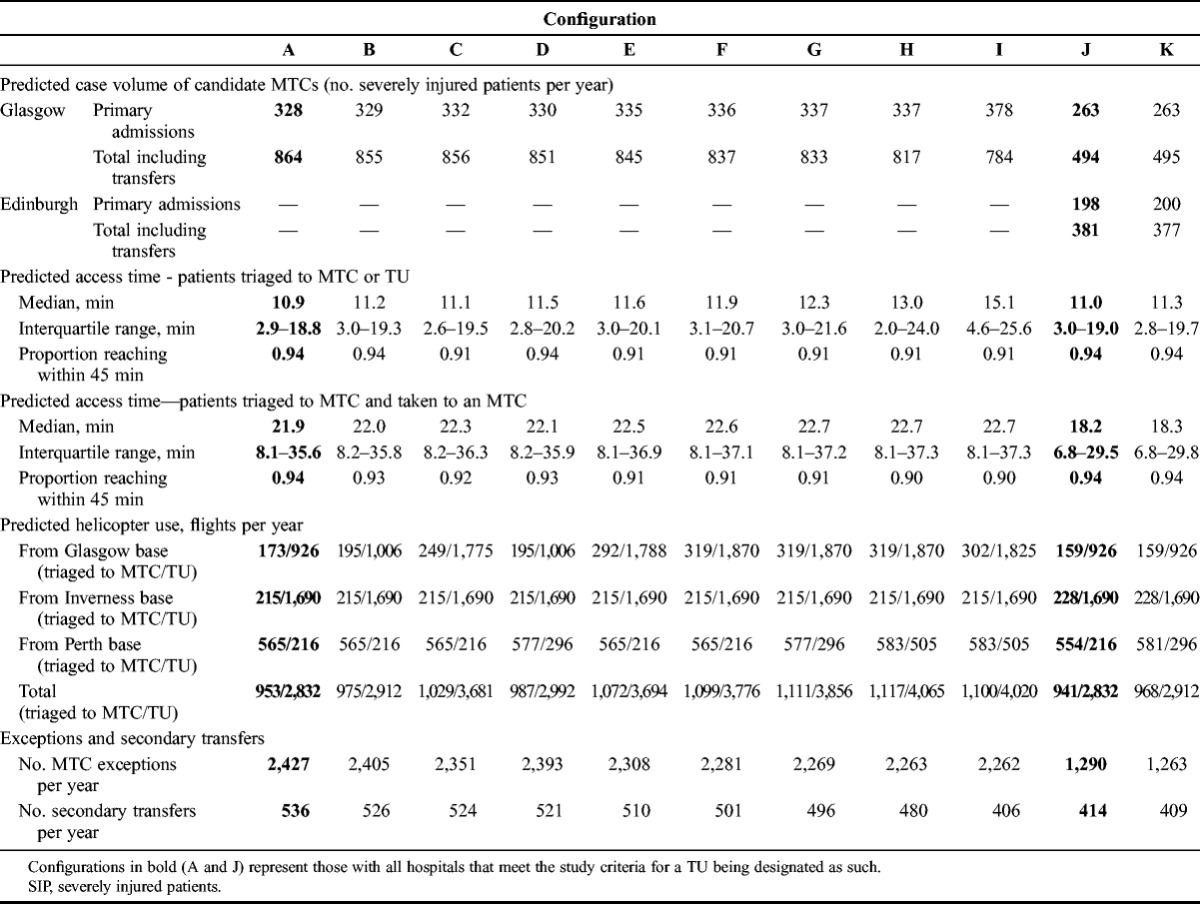
Networks With Low-Volume MTCs
If MTCs with lower annual case volumes were accepted, there would be 11 optimized configurations. Two of these could be realized with four helicopters, whereas the remainder would require at least five aircraft. The two configurations requiring only four helicopters are also shown in Table 2 (Configurations J and K). Both had two MTCs, in Glasgow and Edinburgh, and either 15 or 16 TUs. If all 16 hospitals that could become TUs were designated as such (Configuration J in Tables 2 and 3), the Glasgow MTC would be estimated to have moderate volume (494 severely injured patients per year, including secondary transfers), and the Edinburgh MTC would have low volume (381 severely injured patients per year, including secondary transfers). A total of 414 severely injured patients per year would require a secondary transfer. As before, this number includes both undertriaged patients and those who were correctly triaged but could not reach an MTC within 45 minutes. The estimated median access time for patients triaged to MTC care, who would be taken to an MTC, would be 18.2 minutes, which is slightly shorter than for a single-center configuration. The number of exceptions and secondary transfers would also be lower. If the number of helicopters was increased to five, an additional nine configurations would become feasible, all with two MTCs, in Glasgow and Edinburgh, and 10 to 16 TUs.
Helicopter Retrieval
The implementation of a trauma system with one or two MTCs and with the tasking criteria described is estimated to require an increase in primary helicopter retrievals. The configurations described would necessitate between 2,832 and 4,065 missions to be flown per year, depending on the choice of configuration, equating to approximately nine retrievals per day. However, only 941 to 1,117 of these flights would be for patients triaged to MTC care, the remainder being for patients triaged to TU care, injured in remote locations (Table 3).
Access Time Threshold Sensitivity Analysis
A sensitivity analysis with a 60-minute (as opposed to 45 minutes) access time threshold revealed a small number of additional configurations. Networks with high- or moderate-volume MTCs alone could be optimized with a single MTC in Glasgow, as before, or a single MTC in Edinburgh. However, such a configuration would be associated with markedly longer access times. Networks with low-volume MTCs had two MTCs, in Glasgow and Edinburgh (as before) or in Glasgow and Dundee. However, the latter combination would have been discounted if two fewer patients had been admitted to Dundee. Furthermore, this configuration would also be associated with markedly longer access times. In summary, lengthening the access time threshold to 60 minutes does not alter the conclusions.
DISCUSSION
This study has shown that a novel notional triage and mathematical optimization methodology can be used to inform the planning of a major national care system. This is the first time such a methodology has been used in this field. That the analysis is based on a complete and large national cohort of prospectively collected data adds to the robustness of the findings.
Our analysis indicates that a trauma system configuration with one MTC, in Glasgow, or two MTCs, in Glasgow and Edinburgh, would be optimal, based on observed data. These findings are at variance with the widely held belief that the geographic distribution and associated long access times would preclude a configuration with a single center.10 While such a configuration would result in a high proportion of patients who could not reach definitive care primarily and a high number of secondary transfers, these results should be viewed in the context of an inclusive trauma system, which would facilitate best possible care, even for those injured in remote areas.
The findings are also at variance with the intuitive assumption that, if two MTCs were required, these would be best placed as far apart as possible, in Glasgow and Aberdeen. These results are explained by the spatial distribution of the incidents and the clustering of case volume in the Glasgow/Edinburgh area in particular, as reported in our previous article,17 which exerts a “gravitational pull.”
Implications for Policymakers
Trauma system design is influenced by a number of forces, which vary with setting. Overdesignating high-level facilities risks diluting experience. In the United States, the principal reasons include the economic benefits and the prestige of trauma center status. In the United Kingdom and in Scotland in particular, there are no economic benefits to a hospital being designated as an MTC, but as the National Health Service is more susceptible to political influences, local opinion can strongly influence decision making. Robust data, as generated by the GEOS study, can help to make the process more objective and transparent.
Following the decision to regionalize trauma care in Scotland, the Scottish Government’s National Planning Forum had originally recommended a trauma system with four MTCs, in Glasgow, Edinburgh, Dundee, and Aberdeen.10 This study shows that such a configuration might not be optimal. For the two solutions identified as optimal in our analysis, for a given minimum MTC case volume, the decision as to which solution is best therefore relates, partly, to what is deemed an adequate center volume. The relationship between case volume and outcome is well recognized, but the improvements in mortality, which are seen with higher case volumes, are probably not the consequence of higher volume per se, but rather the ability to justify a different service delivery framework. A dedicated trauma service to coordinate and deliver care for the severely injured is key to improving outcomes but is only justifiable when there is a sufficient case volume. In addition, mortality is not the only measure of a high-quality service. The precise position of the inflection point on the volume/outcome curve is therefore not known, and it is probable that both configurations described would result in MTCs large enough to sustain a specialist service. Furthermore, choosing between the two optimal configurations identified by the modeling should also consider other factors, such as hospitals’ capacity, and issues that are less quantifiable, such as organizational commitment and resilience. Capacity is difficult to model because it is influenced by the number of admissions and the length of stay. Data on the latter were not available in our prehospital data set. In terms of the number of emergency department attendances alone, however, it seems probable that a configuration with two MTCs, in Glasgow and Edinburgh, would be better able to deal with the predicted increase in volume than a single-MTC configuration.
Both the single- and two-MTC system configurations (but, in fact, also the four-MTC configuration proposed by the Scottish Government) would require an increase in aeromedical retrievals, although a proportion of the primary helicopter retrievals predicted by this study were for patients triaged to TU care, with a low probability of major trauma who were injured in remote locations. Some of these patients might not always require helicopter transport or could be taken to a local emergency hospital, if a degree of provider judgment was applied. The anticipated need for increased aeromedical retrieval reflects Scotland’s geography and a probable underprovision of lift capacity, given the population characteristics. The cost of operating additional helicopters may seem substantial but should be viewed in the context of setting up and running additional MTCs, which is also considerable. The combined set-up cost for four MTCs is estimated to be in the region of £12 to £17 million ($19–$27 million). A detailed health economic analysis is in planning.
Strengths and Weaknesses
The strengths of the study lie in its prospective, systemwide, population-based design; its use of actual incident location data; and its application of multiobjective optimization to network analysis, which enables multiple, conflicting objectives to be considered. The use of prehospital triage decisions implicitly considers both undertriage and overtriage and thus provides a realistic model of patient flow.
Several previous studies18–20 have attempted to quantify access to trauma center care using “isochrone analysis” of census data, relying on the assumption that the distribution of the injured population mirrors that of the population in general, which does not always hold true.21 These issues are overcome by network analysis, a well-established technique for solving siting problems in operations research, which was used by Branas et al.22,23 in their seminal Trauma Resource Allocation Model for Ambulances and Hospitals (TRAMAH) study. However, the TRAMAH study was limited by the use of retrospectively calculated severity scores, obtained from trauma registries, to stratify injury severity. In reality, patient flow is determined by prehospital triage decisions, as used by the GEOS modeling. The positive predictive value of triage for determining severe injury is limited, and the resulting overtriage has implications for transport services and hospitals’ capacity.
Nevertheless, mathematical modeling also has limitations. No provision was made for provider judgment in triage, and the model is dependent on the sensitivity of Steps 1 and 2 of the Field Triage Decision Scheme for detecting severe injury. We used a conservative estimate of 45.5%, derived from a large multicenter study from the United States.16 It is possible that the performance of the Field Triage Decision Scheme in Scotland differs because of variations in case mix and application. Calculated drive times are estimates and did not consider the effects of weather, both of which may impact on the accuracy of the data. We considered making allowances for no-fly weather conditions, but the available data on which to base such modeling are limited, particularly as the entire flight path—rather than just the incident location—would have to be considered. Similarly, we did not make allowances for weather-related decreases in driving speeds. However, the model was built on a large data set, collected over a full year, to account for any seasonal variation in the geographic distribution of the incidents. It is possible that the injuries observed over this time may not be representative of what would happen every year, but the profile of the data is similar to that seen in previous years,24–26 which provides reassurance that the results are generalizable.
Future Research and Other Applications
This study adds to the literature on trauma system design, and while the data in this study pertains to the configuration of a trauma system for Scotland, the methodology could easily be adopted and adapted to other settings. In particular, the technique could also be used to compare mathematically optimized configurations with existing ones, to provide a form of quality assurance of the configuration of existing trauma systems. This latter application could help to address the issue of trauma center proliferation, which is an increasingly recognized problem in North America. Furthermore, trauma is not the only time-critical condition that requires complex care delivered by a hierarchical clinical network. The effect of hospital volume on outcome following percutaneous coronary intervention for myocardial ischemia, thrombolytic therapy for stroke, and the repair of ruptured abdominal aortic aneurysms is well recognized,27–29 and these treatments might also benefit from geospatially optimized systems of care.
CONCLUSION
This study has shown that a novel combination of notional triage, network analysis, and mathematical optimization methodology can be used to inform the planning of a major national care system. Scotland’s nascent trauma network would be optimally configured with one or two MTCs, and the latter configuration, in particular, seems feasible with regard to the capacity of the proposed centers and the additional need for aeromedical retrieval resources. Whatever configuration is eventually implemented, it should be carefully and continuously evaluated.
The methodology described here is not only applicable to trauma care or to Scotland. Whether explicitly considered or not, there is a geographic dimension to the design of any clinical network. The need to balance conflicting objectives—such as accessibility, center case volumes, and need for aeromedical transport—is a particular feature of networks caring for patients with highly acute conditions.
AUTHORSHIP
J.O.J. conceived, designed, and managed the study; assembled, analyzed, and interpreted the data; and wrote the draft and final versions of the manuscript. J.J.M. contributed to the design of the study, the interpretation of the data, and the writing of the draft and final versions of the manuscript. H.W. contributed to the design of the study, wrote the software, analyzed the data, and contributed to its interpretation and the writing of the draft and final versions of the manuscript. S.H. contributed to the design of the study and the writing of the draft and final version of the manuscript. R.L. contributed to the design of the study, the implementation of the notional triage, the extraction and assembly of the data, the interpretation of the results, and the writing of the draft and final versions of the manuscript. J.D.H. contributed to the writing of the draft and final version of the manuscript. M.K.C. contributed to the design of the study, the analysis and interpretation of the data, and the writing of the draft and final versions of the manuscript. J.O.J. was the chief investigator. All authors reviewed and approved the final manuscript.
DISCLOSURE
J.O.J. is a member of the Major Trauma Oversight Group (MTOG), the Scottish national trauma system implementation group. J.O.J. does not receive financial support from MTOG.
The Health Services Research Unit receives funding from the Chief Scientist Office of the Scottish Government Health and Social Care Directorates. J.O.J. receives academic salary support from NHS Research Scotland.
The GEOS study was funded by the North of Scotland Planning Group. The opinions expressed in this article are those of the authors alone.
Footnotes
The funders had no role in the design of the study, data collection, data analysis, data interpretation, writing of the report, or decision to submit the manuscript for publication.
The opinions expressed in this article are those of the authors alone.
REFERENCES
- 1. Gabbe BJ, Simpson PM, Sutherland AM, Wolfe R, Fitzgerald MC, Judson R, Cameron PA. Improved functional outcomes for major trauma patients in a regionalized, inclusive trauma system. Ann Surg. 2012; 255(6): 1009– 1015. [DOI] [PubMed] [Google Scholar]
- 2. MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006; 354(4): 366– 378. [DOI] [PubMed] [Google Scholar]
- 3. Mackenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Egleston BL, Salkever DS, Frey KP, Scharfstein DO. The impact of trauma-center care on functional outcomes following major lower-limb trauma. J Bone Joint Surg Am. 2008; 90(1): 101– 109. [DOI] [PubMed] [Google Scholar]
- 4.American College of Surgeons Committee on Trauma. Resources for Optimal Care of the. Chicago, IL; American College of Surgeons; 2006. [Google Scholar]
- 5. Markovchick VJ, Moore EE. Optimal trauma outcome: trauma system design and the trauma team. Emerg Med Clin North Am. 2007; 25(3): 643– 654. [DOI] [PubMed] [Google Scholar]
- 6. Garwe T, Cowan LD, Neas BR, Sacra JC, Albrecht RM. Directness of transport of major trauma patients to a level I trauma center: a propensity-adjusted survival analysis of the impact on short-term mortality. J Trauma. 2011; 70: 1118– 1127. [DOI] [PubMed] [Google Scholar]
- 7. Haas B, Gomez D, Zagorski B, Stukel TA, Rubenfeld GD, Nathens AB. Survival of the fittest: the hidden cost of undertriage of major trauma. J Am Coll Surg. 2010; 211: 804– 811. [DOI] [PubMed] [Google Scholar]
- 8. Utter GH, Maier RV, Rivara FP, Mock CN, Jurkovich GJ, Nathens AB. Inclusive trauma systems: do they improve triage or outcomes of the severely injured? J Trauma. 2006; 60: 529– 535. [DOI] [PubMed] [Google Scholar]
- 9. Jansen JO, Morrison JJ, Wang H, Lawrenson R, Egan G, He S, Campbell MK. Optimizing trauma system design: the GEOS (Geospatial Evaluation of Systems of Trauma Care) approach. J Trauma Acute Care Surg. 2014; 76(4): 1035– 1040. [DOI] [PubMed] [Google Scholar]
- 10.National Planning Forum Major Trauma Subgroup. A Quality Framework for Major Trauma Services. Edinburgh, Scotland: 2013. [Google Scholar]
- 11.Royal College of Surgeons of Edinburgh. Trauma Care in Scotland. Edinburgh, Scotland: Royal College of Surgeons of Edinburgh; 2012. [DOI] [PubMed] [Google Scholar]
- 12. Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, Wald MM, Jurkovich GJ, Newgard CD, Lerner EB, Centers for Disease Control and Prevention. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012; 61: 1– 20. [PubMed] [Google Scholar]
- 13. Deb K, Pratap A, Agarwal S, Meyarivan T. A fast and elitist multiobjective genetic algorithm: NSGA-II. IEEE T Evolut Comput. 2002; 6(2): 182– 197. [Google Scholar]
- 14. Nathens AB, Jurkovich GJ, Maier RV, Grossman DC, MacKenzie EJ, Moore M, Rivara FP. Relationship between trauma center volume and outcomes. JAMA. 2001; 285(9): 1164– 1171. [DOI] [PubMed] [Google Scholar]
- 15.National Audit Office. Major trauma care in England. London, England: HMSO; 2010. [Google Scholar]
- 16. Newgard CD, Zive D, Holmes JF, Bulger EM, Staudenmayer K, Liao M, Rea T, Hsia RY, Wang NE, Fleischman R, et al. A multisite assessment of the American College of Surgeons Committee on Trauma field triage decision scheme for identifying seriously injured children and adults. J Am Coll Surg. 2011; 213(6): 709– 721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jansen JO, Morrison JJ, Wang H, He S, Lawrenson R, Campbell MK, Green DR. Feasibility and utility of population-level geospatial injury profiling: prospective, national cohort study. J Trauma Acute Care Surg. 2015; 78(5): 962– 969. [DOI] [PubMed] [Google Scholar]
- 18. Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, Blatt AJ, ReVelle CS. Access to trauma centers in the United States. JAMA. 2005; 293(21): 2626– 2633. [DOI] [PubMed] [Google Scholar]
- 19. Hameed SM, Schuurman N, Razek T, Boone D, Van Heest R, Taulu T, Lakha N, Evans DC, Brown DR, et al. Access to trauma systems in Canada. J Trauma. 2010; 69(6): 1350– 1361. [DOI] [PubMed] [Google Scholar]
- 20. Kivell P, Mason K. Trauma systems and major injury centres for the 21st century: an option. Health Place. 1999; 5(1): 99– 110. [DOI] [PubMed] [Google Scholar]
- 21. Haas B, Doumouras AG, Gomez D, de Mestral C, Boyes DM, Morrison L, Nathens AB. Close to home: an analysis of the relationship between location of residence and location of injury. J Trauma Acute Care Surg. 2015; 78(4): 860– 865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Branas CC, MacKenzie EJ, ReVelle CS. A trauma resource allocation model for ambulances and hospitals. Health Serv Res. 2000; 35(2): 489– 507. [PMC free article] [PubMed] [Google Scholar]
- 23. Branas CC, Revelle CS. An iterative switching heuristic to locate hospitals and helicopters. Socio Econ Plan Sci. 2001; 35(1): 11– 30. [Google Scholar]
- 24. Morrison JJ, McConnell NJ, Orman JA, Egan G, Jansen JO. Rural and urban distribution of trauma incidents in Scotland. Br J Surg. 2013; 100(3): 351– 359. [DOI] [PubMed] [Google Scholar]
- 25.Scottish Trauma Audit Group. Audit of Trauma Management in Scotland 2012 (Reporting on 2011). Edinburgh, Scotland: ISD; 2012. [Google Scholar]
- 26.Scottish Trauma Audit Group. Audit of Trauma Management in Scotland 2013 (Reporting on 2012). Edinburgh, Scotland: ISD; 2013. [Google Scholar]
- 27. Dawkins KD, Gershlick T, de Belder M, Chauhan A, Venn G, Schofield P, Smith D, Watkins J, Gray HH, Joint Working Group on Percutaneous Coronary Intervention of the British Cardiovascular Intervention Society and the British Cardiac Society. Percutaneous coronary intervention: recommendations for good practice and training. Heart. 2005; 91(Suppl 6): vi1– vi27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011; 58(24): e44– e122. [DOI] [PubMed] [Google Scholar]
- 29. Saposnik G, Baibergenova A, O’Donnell M, Hill MD, Kapral MK, Hachinski V, Stroke Outcome Research Canada (SORCan) Working Group. Hospital volume and stroke outcome: does it matter? Neurology. 2007; 69(11): 1142– 1151. [DOI] [PubMed] [Google Scholar]


