Abstract
Purpose
Over one third of breast cancer survivors experience upper extremity disability. Black women present with factors associated with greater upper extremity disability, including: increased body mass index (BMI), more advanced disease stage at diagnosis, and varying treatment type compared with Whites. No prior research has evaluated the relationship between race and upper extremity disability using validated tools and controlling for these factors.
Methods
Data were drawn from a survey study among 610 women with stage I–III hormone receptor positive breast cancer. The QuickDASH (Disabilities of the Arm, Shoulder and Hand) is an 11-item self-administered questionnaire that has been validated for breast cancer survivors to assess global upper extremity function over the past 7 days. Linear regression and mediation analysis estimated the relationships between race, BMI and QuickDASH score, adjusting for demographics and treatment types.
Results
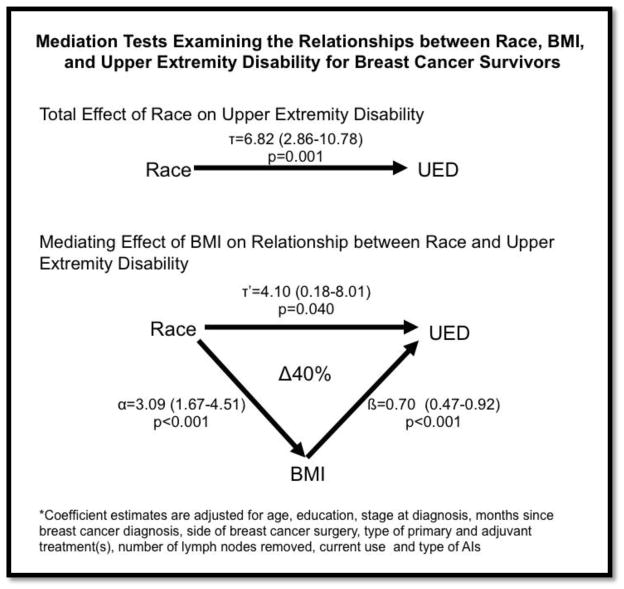
Black women (n=98) had 7.3 points higher average QuickDASH scores than White (n=512) women (p<0.001). After adjusting for BMI, age, education, cancer treatment, months since diagnosis, and aromatase inhibitor status, Black women had an average 4-point (95% confidence interval: 0.18–8.01) higher QuickDASH score (p=0.04) than White women. Mediation analysis suggested that BMI attenuated the association between race and disability by 40%.
Conclusions
Even several years post-treatment, Black breast cancer survivors had greater upper extremity disability, which was partially mediated by higher BMIs. Close monitoring of high BMI Black women may be an important step in reducing disparities in cancer survivorship. More research is needed on the relationship between race, BMI, and upper extremity disability.
Keywords: breast cancer, upper extremity function, disability, Black/African-American, Philadelphia, Pa
Background
Over 35% of breast cancer survivors experience upper extremity disability (UED),[1] and report that UED after cancer is associated with even greater psychosocial burden than the cancer diagnosis itself.[2] Breast cancer survivors with any functional limitations are at significantly higher risk of all-cause mortality compared to those who have no limitation.[3] Upper extremity function is of particular concern for breast cancer survivors, who face increased UED due to breast cancer surgery, radiation, or chemotherapy to the upper body region.[4] UED may be worsened by co-morbid physical conditions like obesity or changes in weight,[5] may persist for at least 2 years post-surgery, and may be affected by primary and adjuvant cancer treatment types as well as patient characteristics. For example, UED is worse among patients who receive axillary lymph node dissection (≥ 5 nodes removed) compared with sentinel lymph node biopsy (<5 nodes removed).[6] Use of aromatase inhibitors (i.e., anastrozole, letrozole, exemestane), which are now part of standard adjuvant hormone therapy for ER+ breast cancers, may increase the likelihood of pain in the upper extremity.[7, 8] Non-steroidal aromatase inhibitors (e.g., Anastrazole and Letrozole) are more likely to be associated with musculoskeletal symptoms than steroidal aromatase inhibitors (e.g., exemestane).[9, 10] Although these treatment types may contribute to UED, several studies have demonstrated that functional disability/limitations are more influenced by patient demographic characteristics, time since surgery, and various social factors than by clinical factors such as type of treatment or disease stage.[11, 12]
Among breast cancer survivors, racial disparities have been documented in physical functioning, physical well-being, pain and disability outcomes with Non-Hispanic Black women faring worse than Non-Hispanic White women.[13–15] These disparities outline a broader context within which race may contribute to differential UED rates for Black and White women. Race/ethnicity may be a key patient demographic characteristic in UED, given that race is associated with factors associated with poor functioning, including high BMI,[16, 17] weight gain after breast cancer,[18] later stage at diagnosis,[19–22] and underuse of sentinel lymph node biopsy, adjuvant chemotherapy, radiation, and hormone therapy.[23–25] For instance, Non-Hispanic Black women have higher rates of obesity than Non-Hispanic White women, which might lead Black women to worse functioning by predisposing them to debilitating conditions like breast-cancer related lymphedema (BCRL).[26, 27] Yet, Black women have lower rates of axillary lymph node dissection that may decrease BCRL incidence and hence lead to better physical functioning.[23, 28] Due to lower rates of ER+ breast cancers, [29] Non-Hispanic Black women are less likely than Non-Hispanic White women to use aromatase inhibitors (AIs); less AI usage could contribute to lower UED risk for Non-Hispanic Black women. It is not yet known to what extent factors such as stage of diagnosis, treatment types, BMI, and AI usage directly or indirectly contribute to differences in upper body functional limitation by race and should be further explored in an effort to improve survivorship care.
Few studies have explicitly explored associations between race and UED among breast cancer survivors, though some have controlled for race.[11, 30–32] Some have shown no differences in upper extremity function by race[30] or full mediation by BMI,[32] while others did not report findings specific to upper body functioning by race,[11] or did not exclusively focus on breast cancer.[31] Often, prior studies did not use validated scales to measure UED, nor account for co-morbid conditions, such as obesity, that might affect functioning. These limitations in prior studies leave gaps in the research literature on how to identify which breast cancer survivors are at greatest risk for UED. This warrants further exploration of the associations between UED, race, and co-morbid conditions for breast cancer survivors using measures of functional limitation that have been validated in breast cancer survivors. The purpose of this observational study was to evaluate the extent to which race and obesity contributes to differences in UED among Black or White breast cancer survivors, using a validated scale, and controlling for social and physical patient characteristics associated with breast cancer treatment.
Methods
Participants were drawn from the baseline assessment of an ongoing longitudinal study examining genetic determinants of symptom distress and disease outcomes among postmenopausal women with hormone receptor positive breast cancer who were prescribed aromatase inhibitors (AIs). The purpose of that study was to evaluate whether genetic polymorphisms in estrogen synthesis and metabolism predict toxicities of AI therapy and breast cancer outcomes. Further details of that study have been previously published.[33] Patients were recruited from breast cancer clinics in an academic tertiary care teaching hospital and a community hospital between November 2011 and June 2014. Eligibility criteria for the ongoing longitudinal study were (1) female sex; (2) age 18 or older; (3) history of stage I, II, or III breast cancer; (4) current use of a third-generation AI for at least 6 months or discontinuation of AIs before the full duration of prescribed therapy; (5) postmenopausal; (6) completed primary cancer treatments (surgery, chemotherapy, radiotherapy); and (7) able to understand written English and participate in an informed consent process. All measures and procedures were approved by the Institutional Review Board of the University of Pennsylvania.
Of the original 720 in the ongoing longitudinal study for whom there were complete baseline data: 18 were excluded for not self-identifying as Black or White; 1 was excluded for being >500 months since breast cancer diagnosis; 4 were excluded due to no self-reported treatment for breast cancer; and 87 were excluded for missing data on number of lymph nodes removed. For the present analysis, the resulting sample size was 610 respondents.
Primary Outcome
The QuickDASH is a shortened version of the Disabilities of the Arm, Shoulder and Hand[34] questionnaire, and is a self-administered questionnaire that has been validated among Black and White breast cancer survivors to assess global arm function over the past 7 days.[35] Validation has shown that the QuickDASH has high reliability and validity in a racially diverse population of various ages and educational statuses, with Cronbach’s alpha of 0.93, all items loading on one factor with an eigenvalue of 6.7 which explained 61% of the variance, and high test-retest reliability at 2 weeks (ICC=0.78).
The QuickDASH can be scored in two components: the disability/symptom section (11 items, scored 1–5) and the optional high performance sport/music or work modules (4 items, scored 1–5). The optional questions were omitted since respondents were unlikely to currently be in jobs that require high physical performance (e.g., professional athlete) due to their average age and cancer treatment history. The assigned values for all completed responses were summed and averaged, yielding a summary score out of five. This summary score was transformed to a score out of 100 by subtracting one and multiplying by 25, to make the score easier to compare to other measures scaled on a 0–100 scale. Higher scores indicate greater disability, with a highest possible score of 100 points.
Covariates
Demographic variables, including race (Black or White), age (continuous), education (high school graduate or less or more than high school), as well as clinical variables, including BMI (continuous), time since breast cancer diagnosis (continuous, in years), side of surgery (unilateral or bilateral), treatments received (yes or no for lumpectomy, mastectomy, chemotherapy, radiation, reconstruction), and current AI usage and type of AI used in the past month, including non-steroidal AIs (Arimidex (Anastrazole) and Femara (Letrozole)) and steroidal AIs (Aromasin (Exemestane)) were assessed by self-report survey. Number of lymph nodes (continuous variable) removed across all breast cancer surgeries was abstracted from patient medical records.
Statistical Analysis
Descriptive statistics were calculated for each key variable. Comparisons among Black and White participants were tested using t-tests for continuous variables and chi-square tests for categorical variables. QuickDASH score by each variable was examined; continuous variables were recoded into categorical variables based on clinically significant groupings in order compare QuickDASH scores using t-tests (for two-category variables) or oneway ANOVA tests (for multi-category variables). For time since cancer diagnosis, 24 months was used as a cut-off because previous studies suggest that functional limitation may persist at least 2 years post-surgery.[6] Bivariable and multivariable linear regressions were used to assess the independent and collective associations of each key variable with the QuickDASH score outcome.
Mediation analysis was performed based on established criteria for assessing mediation,[36–38] and as applied to this study was designed to demonstrate that: (1) race, the exposure, is associated with QuickDASH score, the outcome; (2) race is associated with BMI, the mediator; (3) BMI is associated with QuickDASH score; and (4) BMI completely or partially attenuates the association between race and BMI.[39] Testing of these criteria has performed by (1) regressing QuickDASH Score on race, adjusting for all factors except BMI; (2) regressing BMI on race, adjusting for all other factors; (3) regressing QuickDASH score on BMI and race, adjusting for all other factors; and (4) comparing the parameter estimates for race in the QuickDASH outcome model that includes BMI to the one that did not include BMI. To show the degree of attenuation by BMI, representing the percent of the association between race and QuickDASH score that is explained by BMI, the percent change in the race parameter estimate was calculated based on its value in the models with BMI and without BMI.
Results
A total of 610 women were eligible in the final sample. As summarized in Table 1, the average QuickDASH score for the final sample was 19.5 (SD=17.5) out of a possible 100 points indicating the highest level of disability. QuickDASH scores reported ranged from 0 to 86.4 out of 100 total points. In this sample, the QuickDASH scale had a Cronbach’s alpha of 0.91, with all items loading on one factor with an eigenvalue of 6.1 which explained 55% of the variance. Participants had an average BMI of 28, average age of 63 years, were most likely to have a high school degree equivalent or less, were most likely to have been Stage I at cancer diagnosis, were approximately 2.5 years (40.6 months) out from diagnosis, and were most likely to have had unilateral surgery. The majority had lumpectomy and radiation, with an average of 7.5 lymph nodes removed during surgery. Approximately 87% had reported AI usage in the past month, with the majority (72%) using Arimidex (Anastrazole).
Table 1.
Participant Characteristics
| All (N=610) | Black (n=98) | White (n=512) | p | |
|---|---|---|---|---|
| QuickDASH Score (95% CI) | 19.5 (18.1, 20.9) | 25.7 (21.5, 30.0) | 18.4 (16.9, 19.8) | <0.001 |
| BMI (95% CI) | 28.0 (27.5, 28.6) | 31.2 (29.9, 32.4) | 27.5 (26.9, 30.0) | <0.001 |
| Age (95% CI) | 63 (62, 64) | 65 (63, 67) | 63 (62, 64) | 0.03 |
| Education (%) | <0.001 | |||
| High School Graduate or Less | 129 (21.2) | 42 (42.9) | 87 (17.0) | |
| More than High School | 481 (78.9) | 56 (57.1) | 425 (83.0) | |
| Cancer Stage at Diagnosis (%) | 0.77 | |||
| I | 345 (57.5) | 54 (57.5) | 291 (57.5) | |
| II | 177 (29.5) | 26 (27.7) | 151 (29.8) | |
| III | 78 (13.0) | 14 (14.9) | 64 (12.7) | |
| Months Since Diagnosis (95% CI) | 40.6 (37.6, 43.6) | 35.4 (29.1, 41.7) | 41.6 (38.2, 44.9) | 0.14 |
| Side of Surgery (%) | 0.40 | |||
| Unilateral | 549 (90.6) | 91 (92.9) | 458 (90.2) | |
| Bilateral | 57 (9.4) | 7 (7.1) | 50 (9.8) | |
| Lumpectomy (%) | 406 (66.6) | 61 (62.2) | 345 (67.4) | 0.32 |
| Mastectomy (%) | 251 (41.2) | 28 (28.6) | 223 (43.6) | <0.001 |
| Chemotherapy (%) | 294 (48.2) | 42 (42.9) | 252 (49.2) | 0.25 |
| Radiation (%) | 436 (71.5) | 73 (74.5) | 363 (70.9) | 0.47 |
| Reconstruction (%) | 189 (30.9) | 28 (28.5) | 161 (31.5) | 0.57 |
| Lymph Nodes Removed | 7.5 (6.8, 8.1) | 7.6 (6.0, 9.1) | 7.4 (6.7, 8.1) | 0.86 |
| AI Used in Past Month (%) | ||||
| Not currently using | 80 (13.1) | 12 (12.2) | 68 (13.2) | 0.43 |
| Arimidex (Anastrazole) | 437 (71.6) | 72 (73.5) | 365 (71.3) | |
| Femara (Letrezole) | 70 (11.5) | 12 (13.3) | 57 (11.1) | |
| Aromasin (Exemestane) | 23 (3.8) | 1 (1.0) | 22 (4.3) |
Of the total sample population, 98 respondents were Black (16%) and 512 were White (84%). Black women had significantly higher BMI (31.2 vs 27.5, p<0.001), were older (65 vs 63, p=0.03), were less likely to have had post-secondary education (57.1% vs 83% more than high school education, p<0.001), and experienced greater upper extremity disability (UED) as measured by higher QuickDASH score (25.7 vs 18.4, p<0.001). White women were significantly more likely to have had a mastectomy (43.6% vs 28.6%, p<0.001) than Black women. There were no statistically significant differences in cancer stage at diagnosis, months since diagnosis, side of surgery, lumpectomy, chemotherapy, radiation, reconstruction, number of lymph nodes removed, or AI usage between Black and White cancer survivors in this sample.
Table 2 shows the value of QuickDASH scores by key variables. QuickDASH score was significantly higher with each increasing BMI category (p<0.001), and higher among those with a high school education or less (p=0.005). QuickDASH score did not differ by age category, cancer stage at diagnosis, months since diagnosis, side of surgery, type of surgery or adjuvant treatment, breast reconstruction, lymph node dissection, or type of AI used in the past month.
Table 2.
Summary Statistics of QuickDASH Scores by Key Variables
| QuickDASH Score (Mean) | Standard Deviation | Min Max Values | p* | |
|---|---|---|---|---|
| Race | <0.001 | |||
| White | 18.4 | 16.49 | 0 77.3 | |
| Black | 25.7 | 21.15 | 0 86.4 | |
| BMI* | <0.001 | |||
| <25 | 19.2 | 16.2 | 0 68.2 | |
| 25–30 | 18.4 | 17.5 | 0 86.4 | |
| >30 | 20.8 | 18.1 | 0 77.3 | |
| Age* | 0.30 | |||
| <55 | 19.2 | 16.2 | 0 65.9 | |
| 55–65 | 18.4 | 17.5 | 0 77.3 | |
| >65 | 20.8 | 18.1 | 0 86.4 | |
| Education | 0.005 | |||
| High School Graduate or Less | 23.4 | 20.6 | 0 86.4 | |
| More than High School | 18.5 | 16.4 | 0 77.3 | |
| Cancer Stage at Diagnosis* | 0.28 | |||
| I | 19.7 | 16.0 | 0 86.4 | |
| II | 18.0 | 16.0 | 0 75 | |
| III | 21.7 | 17.1 | 0 70.5 | |
| Months since Diagnosis | 0.14 | |||
| 24 Months or Less | 20.8 | 18.1 | 0 77.3 | |
| More than 24 months | 18.7 | 17.1 | 0 86.4 | |
| Side of Surgery | 0.65 | |||
| Unilateral | 19.6 | 17.8 | 0 86.4 | |
| Bilateral | 18.5 | 14.6 | 0 68.8 | |
| Lumpectomy | 0.73 | |||
| No | 19.8 | 17.5 | 0 86.4 | |
| Yes | 19.4 | 18.6 | 0 77.3 | |
| Mastectomy | 0.40 | |||
| No | 20.0 | 18.4 | 0 86.4 | |
| Yes | 18.8 | 16.2 | 0 75.0 | |
| Chemotherapy | 0.59 | |||
| No | 19.9 | 18.5 | 0 86.4 | |
| Yes | 19.1 | 16.4 | 0 75 | |
| Radiation | 0.71 | |||
| No | 19.9 | 17.9 | 0 77.3 | |
| Yes | 19.4 | 17.4 | 0 86.4 | |
| Reconstruction | 0.89 | |||
| No | 19.6 | 17.8 | 0 77.3 | |
| Yes | 19.4 | 16.8 | 0 86.4 | |
| Lymph Nodes Removed | 0.85 | |||
| Sentinel (< 5 removed) | 19.4 | 18.2 | 0 86.4 | |
| Axillary (>=5 removed) | 19.7 | 16.7 | 0 75.0 | |
| AI Used in Past Month | 0.19 | |||
| Not currently using | 22.4 | 19.6 | 0 77.3 | |
| Arimidex (Anastrazole) | 18.6 | 16.8 | 0 86.4 | |
| Aromasin (Exemestane) | 21.3 | 17.0 | 0 56.8 | |
| Femara (Letrezole) | 21.8 | 19.2 | 0 77.3 |
Oneway ANOVAs calculated for significance testing of categorical variables with more than 2 categories
Bivariable analysis in Table 3 suggested that Black women had average QuickDASH scores that were 7.3 points higher than White women (p<0.001), indicating significantly greater UED among Black women. Black race was associated with a 4.10 significantly higher QuickDASH score (p=0.04) when adjusting for BMI, age, education, cancer stage at diagnosis, months since diagnosis, side of surgery, type of surgery or adjuvant treatment, breast reconstruction, number of lymph nodes removed, and use of AIs in the past month. In analysis adjusted for demographic and clinical factors, each 1-unit increase in BMI was associated with a 0.70-point increase in QuickDASH score (p<0.001). The final model accounted for approximately 12% of the variance in QuickDASH scores.
Table 3.
Bivariable and Multivariable Linear Regression Results for QuickDASH Scores
| Unadjusted Parameter Estimate | 95% CI | p | Adjusted Parameter Estimate | 95% CI | p | |
|---|---|---|---|---|---|---|
| Black | 7.33 | 3.59, 11.09 | <0.001 | 4.10 | 0.18, 8.01 | 0.04 |
| BMI | 0.74 | 0.52, 0.95 | <0.001 | 0.70 | 0.48, 0.92 | <0.001 |
| Age | 0.12 | −0.01, 0.26 | 0.08 | 0.12 | −0.04, 0.28 | 0.13 |
| More than HS Education | −4.92 | −8.31, −1.53 | 0.005 | −2.72 | −6.62, 0.80 | 0.13 |
| Cancer Stage at Diagnosis | 0.30 | −1.66, 2.27 | 0.76 | −0.58 | −3.18, 2.02 | 0.66 |
| Months Since Diagnosis | −0.014 | −0.05, 0.22 | 0.46 | −0.03 | −0.07, 0.007 | 0.10 |
| Bilateral Surgery | −1.10 | −5.89, 3.69 | 0.65 | −1.82 | −6.55, 2.922 | 0.45 |
| Lumpectomy | −0.53 | −3.48, 2.43 | 0.73 | −0.14 | −3.89, 3.61 | 0.94 |
| Mastectomy | −1.21 | −4.04, 1.63 | 0.40 | −1.35 | −6.43, 3.73 | 0.60 |
| Chemotherapy | −0.77 | −3.56, 2.02 | 0.59 | 0.26 | −3.21, 3.74 | 0.88 |
| Radiation | −0.58 | −3.67, 2.51 | 0.71 | −1.69 | −5.60, 2.22 | 0.40 |
| Reconstruction | −0.22 | −3.24, 2.80 | 0.89 | 1.83 | −2.41, 6.09 | 0.40 |
| Lymph Nodes Removed | 0.15 | −0.03, 0.33 | 0.10 | 0.17 | −0.05, 0.39 | 0.13 |
| AI in Past Month | ||||||
| None (ref) | -- | -- | -- | -- | -- | -- |
| Arimidex (Anastrazole) | −3.80 | −7.97, 0.38 | 0.08 | −3.97 | −8.06, 0.13 | 0.06 |
| Aromasin (Exemestane) | −1.00 | −9.13, 7.11 | 0.81 | 2.11 | −5.86, 10.08 | 0.60 |
| Femara (Letrezole) | −0.51 | −6.13, 5.11 | 0.86 | −1.50 | −7.05, 4.05 | 0.60 |
For final model: R2=0.12; Adjusted R2=0.09
Figure 1 shows the mediation analysis designed to test the mediating role of BMI in the association between race and UED, as measured by QuickDASH score. Race was significantly associated with UED (τ =6.82, p=0.001) adjusting for all other factors, except BMI (total effect; coefficient estimate denoted by τ). Race was significantly associated with BMI (α =3.09, p<0.001) adjusting for all other factors. In the presence of BMI, race was still significantly associated with BMI (direct effect: τ′ =4.10, p=0.04), but the strength of the association between race and UED was smaller. When BMI is included in the model along with all other covariates, the strength of the association between race and UED was attenuated by 40%.
Figure 1.
Test of BMI as Mediator between Race and Upper Extremity Disability
Conclusions
This study has examined racial differences in upper extremity disability (UED) for Black or White breast cancer survivors, as measured by the QuickDASH, and accounting for physical and social characteristics associated with breast cancer treatment. This study found that after accounting for physical characteristics and treatment-related factors Black breast cancer survivors experience greater UED than White breast cancer survivors, even several years post-treatment. The differences in race may be partially explained by higher BMIs among Black breast cancer survivors. These findings have implications for which patients should be targeted for additional monitoring of upper body changes after breast cancer surgery.
This study contributes to a small but growing body of literature that examined race differences in function after breast cancer surgery. The present study was designed to assess differences by race using a validated patient-reported outcome for assessing UED in breast cancer survivors. The UED measure used in the present study assessed the entire upper body region, including the arm, shoulder and hand giving a more comprehensive measure of disability than explored in the past. Thus, it overcomes limitations in other studies which did not find significant UED differences by race, including: sample sizes that may have been too small to detect differences by race,[11, 30] were focused on overall impairments,[11, 32] were not specific to breast cancer,[31] or did not use a validated scale focused on the upper extremity specifically.[11, 31, 32] Though contrasting the findings in previous studies, this current study offers strong evidence of racial differences in UED exist after breast cancer.
Our results further suggest that obesity plays an important role in explaining differences in UED by race. Higher BMIs may predispose Black women to experience greater adverse effects of treatment or surgical complications. Black women have higher BMI than White women both before[40–42] and after breast cancer surgery,[43, 44] leaving Black women at increased risk of experiencing UED even before a breast cancer diagnosis[45] and which may be exacerbated due to weight gain after breast cancer surgery. High BMI is associated with greater presence of adverse treatment effects such as breast-cancer related lymphedema, the presence of which could translate into higher scores on validated measures assessing disability.[27, 46–48] High BMIs also contributes to higher levels of surgical complications,[49–52] including increased operating and recovery times, slower and poorer healing, and higher levels of infection in breast cancer surgery.[52–59] Lower levels of physical activity among Black breast cancer survivors compared with White cancer survivors [60, 61] may lead to both higher BMI and differences in how much the upper body is used. A plausible but less explored possibility is that BMI may have an effect on upper body tissue healing after breast cancer surgery, which may be modified by lower breast tissue density for Black women compared to Whites that has been observed in several studies. [62–64] The relationship between BMI and tissue healing is still uncertain, and may be a potential area of study to better understand differences in functioning after breast cancer.
Still, BMI only partially mediated the relationship between race and UED differences, suggesting a residual effect of race over and above BMI’s contribution to UED differences by race. Race is a social construct,[65, 66] which means that any residual effects of race over and above its contribution to BMI may represent unmeasured social factors that are embodied due to racial grouping. Social factors that have been associated with race and BMI may be the underlying root causes of race differences in UED after breast cancer treatment, and may be the underlying root cases of higher QuickDASH scores for Black women. For disparities in Black breast cancer survivors, these may be social factors that directly relate to embodied psychosocial stressors that are associated with experiences of discrimination and differential access to clinical care.[67, 68] For example, in a study of breast cancer survivors seen at a military hospital, there were no differences in QuickDASH scores by race.[30] That study’s authors suggest that the lack of difference in UED by race was likely due to being in a military system where health access was equal across races and presumably not a barrier to care.[30] Additional social factors, like socioeconomic position and quality of healthcare access, may be helpful additions to explaining the residual effects of race on UED differences, over above the contributions of BMI.
Study results must be considered in the context of the study’s limitations. All patients were post-menopausal breast cancer survivors seen at an academic school of medicine and who were prescribed AIs, thus results may not be generalizable to the general population of breast cancer survivors. Second, the QuickDASH is a patient-reported outcome that is subject to recall and social-desirability bias. Future research combining subjective and objective functional assessments may help determine the clinical importance of the findings discovered in the current study. No information was available on UED prior to breast cancer surgery, and racial differences in UED may have been present prior to surgery; however, the present study would confirm that racial differences in UED persist after surgery, regardless of pre-surgery UED levels. Differential rates of post-surgical adverse treatment effects may also have contributed to differences in QuickDASH scores. The present study did not directly assess adverse treatment effects, but did assess BMI and lymph node removal, which are two major risk factors for surgical complications and adverse treatment effects. Surgical treatment type was self-reported because clinical chart data were limited to treatments from one institution. Self-report of breast cancer treatment has been validated as over 90% accurate within the first 6 months, but may wane over time;[69] however, self-reported treatment allowed the analysis to account for all treatments a patient had across all institutions.
Despite these study limitations, we identified racial disparities in upper extremity disability between Black and White women with breast cancer. Obesity as a partial mediator affirms the need for breast cancer survivors to maintain a healthy weight as a way to reduce disparities in cancer survivorship outcomes; however, addressing obesity is only part of the challenge. Future studies are needed to fully explore race differences in UED after breast cancer surgery, in the context of BMI, adverse effects of surgery, and social factors. Intervention research developed to promote optimal functioning and reduce differences by race may need to include targeted interventions/therapies for Black women with a specific emphasis on those who have high BMIs. Successfully addressing the issue of obesity for Black breast cancer survivors may be an important step in reducing disparities in physical functioning, psychosocial burden faced after cancer treatment, mortality, and improving quality of life.
Acknowledgments
Research Support: This study was supported by National Institutes of Health / National Cancer Institute 1R01CA158243. Dr. Dean is supported in part by the National Institutes of Health and National Cancer Institute grant number 1K01CA184288.
Acronyms Used in Text
- AI
Aromatase inhibitor
- BMI
Body mass index
- QuickDASH
Disabilities of the Arm, Shoulder and Hand
- UED
Upper extremity disability
Footnotes
The abstract and some of the results have been presented in a poster presentation at the American Society of Clinical Oncology 2015 conference. The full manuscript has never been published, in whole, to any audience or entity.
Conflict of Interest Statement/Financial Disclosures: None. The authors declare that they have no conflict of interest.
References
- 1.Levy EW, Pfalzer LA, Danoff J, Springer BA, McGarvey C, Shieh C-y, Morehead-Gee A, Gerber LH, Stout NL. Predictors of functional shoulder recovery at 1 and 12 months after breast cancer surgery. Breast cancer research and treatment. 2012;134(1):315–324. doi: 10.1007/s10549-012-2061-1. [DOI] [PubMed] [Google Scholar]
- 2.Banks E, Byles JE, Gibson RE, Rodgers B, Latz IK, Robinson IA, Williamson AB, Jorm LR. Is psychological distress in people living with cancer related to the fact of diagnosis, current treatment or level of disability? Findings from a large Australian study. Medical Journal of Australia. 2010;193(5):S62. doi: 10.5694/j.1326-5377.2010.tb03931.x. [DOI] [PubMed] [Google Scholar]
- 3.Braithwaite D, Satariano WA, Sternfeld B, Hiatt RA, Ganz PA, Kerlikowske K, Moore DH, Slattery ML, Tammemagi M, Castillo A. Long-term prognostic role of functional limitations among women with breast cancer. Journal of the National Cancer Institute. 2010;102(19):1468–1477. doi: 10.1093/jnci/djq344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rietman J, Dijkstra P, Hoekstra H, Eisma W, Szabo B, Groothoff J, Geertzen J. Late morbidity after treatment of breast cancer in relation to daily activities and quality of life: a systematic review. European Journal of Surgical Oncology (EJSO) 2003;29(3):229–238. doi: 10.1053/ejso.2002.1403. [DOI] [PubMed] [Google Scholar]
- 5.Voskuil D, van Nes J, Junggeburt J, van de Velde C, Van Leeuwen F, de Haes J. Maintenance of physical activity and body weight in relation to subsequent quality of life in postmenopausal breast cancer patients. Annals of oncology. 2010:mdq151. doi: 10.1093/annonc/mdq151. [DOI] [PubMed] [Google Scholar]
- 6.Rietman J, Geertzen J, Hoekstra H, Baas P, Dolsma W, De Vries J, Groothoff J, Eisma W, Dijkstra P. Long term treatment related upper limb morbidity and quality of life after sentinel lymph node biopsy for stage I or II breast cancer. European Journal of Surgical Oncology (EJSO) 2006;32(2):148–152. doi: 10.1016/j.ejso.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 7.Mao JJ, Stricker C, Bruner D, Xie S, Bowman MA, Farrar JT, Greene BT, DeMichele A. Patterns and risk factors associated with aromatase inhibitor-related arthralgia among breast cancer survivors. Cancer. 2009;115(16):3631–3639. doi: 10.1002/cncr.24419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mao JJ, Chung A, Benton A, Hill S, Ungar L, Leonard CE, Hennessy S, Holmes JH. Online discussion of drug side effects and discontinuation among breast cancer survivors. Pharmacoepidemiology and drug safety. 2013;22 (3):256–262. doi: 10.1002/pds.3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henry NL, Azzouz F, Desta Z, Li L, Nguyen AT, Lemler S, Hayden J, Tarpinian K, Yakim E, Flockhart DA. Predictors of aromatase inhibitor discontinuation as a result of treatment-emergent symptoms in early-stage breast cancer. Journal of Clinical Oncology. 2012;30(9):936–942. doi: 10.1200/JCO.2011.38.0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coleman R, Bolten W, Lansdown M, Dale S, Jackisch C, Merkel D, Maass N, Hadji P. Aromatase inhibitor-induced arthralgia: clinical experience and treatment recommendations. Cancer treatment reviews. 2008;34(3):275–282. doi: 10.1016/j.ctrv.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Yoon J, Malin JL, Tao ML, Tisnado DM, Adams JL, Timmer MJ, Ganz PA, Kahn KL. Symptoms after breast cancer treatment: are they influenced by patient characteristics? Breast cancer research and treatment. 2008;108(2):153–165. doi: 10.1007/s10549-007-9599-3. [DOI] [PubMed] [Google Scholar]
- 12.Campbell KL, Pusic AL, Zucker DS, McNeely ML, Binkley JM, Cheville AL, Harwood KJ. A prospective model of care for breast cancer rehabilitation: function. Cancer. 2012;118(S8):2300–2311. doi: 10.1002/cncr.27464. [DOI] [PubMed] [Google Scholar]
- 13.Blinder VS, Griggs JJ. Seminars in oncology: 2013. Elsevier; 2013. Health disparities and the cancer survivor; pp. 796–803. [DOI] [PubMed] [Google Scholar]
- 14.Paskett ED, Alfano CM, Davidson MA, Andersen BL, Naughton MJ, Sherman A, McDonald PG, Hays J. Breast cancer survivors’ health-related quality of life. Cancer. 2008;113(11):3222–3230. doi: 10.1002/cncr.23891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Green CR, Hart-Johnson T, Loeffler DR. Cancer-related chronic pain. Cancer. 2011;117(9):1994–2003. doi: 10.1002/cncr.25761. [DOI] [PubMed] [Google Scholar]
- 16.Schmitz K, Neuhouser ML, Agurs-Collins T, Zanetti KA, Cadmus-Bertram L, Dean LT, Drake BF. Impact of obesity on cancer survivorship and the potential relevance of race and ethnicity. Journal of the National Cancer Institute. 2013;105(18):1344–1354. doi: 10.1093/jnci/djt223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schmitz KH, Agurs-Collins T, Neuhouser ML, Pollack L, Gehlert S. Impact of Energy Balance on Cancer Disparities. Springer; 2014. Impact of Obesity, Race, and Ethnicity on Cancer Survivorship; pp. 63–90. [Google Scholar]
- 18.Rock CL, Flatt SW, Newman V, Caan BJ, Haan MN, Stefanick ML, Faerber S, Pierce JP. Factors associated with weight gain in women after diagnosis of breast cancer. Women’s Healthy Eating and Living Study Group. Journal of the American Dietetic Association. 1999;99(10):1212–1221. doi: 10.1016/s0002-8223(99)00298-9. [DOI] [PubMed] [Google Scholar]
- 19.Haas JS, Earle CC, Orav JE, Brawarsky P, Keohane M, Neville BA, Williams DR. Racial segregation and disparities in breast cancer care and mortality. Cancer. 2008;113(8):2166–2172. doi: 10.1002/cncr.23828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dai D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health & place. 2010;16(5):1038–1052. doi: 10.1016/j.healthplace.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 21.Russell EF, Kramer MR, Cooper H, Gabram-Mendola S, Senior-Crosby D, Jacob Arriola KR. Metropolitan area racial residential segregation, neighborhood racial composition, and breast cancer mortality. PubMed Cancer Causes Control. 2012;23(9):1519–1527. doi: 10.1007/s10552-012-0029-4. [DOI] [PubMed] [Google Scholar]
- 22.Warner TE, Lin Gomez S. Impact of neighborhood racial composition and metropolitan residential segregation on disparities in breast cancer stage at diagnosis and survival between black and white women in California. J Community Health. 2010;35(4):398–408. doi: 10.1007/s10900-010-9265-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wheeler SB, Reeder-Hayes KE, Carey LA. Disparities in Breast Cancer Treatment and Outcomes: Biological, Social, and Health System Determinants and Opportunities for Research. The oncologist. 2013 doi: 10.1634/theoncologist.2013-0243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, Cooper D, Gansler T, Lerro C, Fedewa S. Cancer treatment and survivorship statistics, 2012. CA: a cancer journal for clinicians. 2012;62(4):220–241. doi: 10.3322/caac.21149. [DOI] [PubMed] [Google Scholar]
- 25.Bickell NA, Wang JJ, Oluwole S, Schrag D, Godfrey H, Hiotis K, Mendez J, Guth AA. Missed opportunities: racial disparities in adjuvant breast cancer treatment. Journal of Clinical Oncology. 2006;24(9):1357–1362. doi: 10.1200/JCO.2005.04.5799. [DOI] [PubMed] [Google Scholar]
- 26.Togawa K, Ma H, Sullivan-Halley J, Neuhouser ML, Imayama I, Baumgartner KB, Smith AW, Alfano CM, McTiernan A, Ballard-Barbash R. Risk factors for self-reported arm lymphedema among female breast cancer survivors: a prospective cohort study. Breast Cancer Research. 2014;16(4):414. doi: 10.1186/s13058-014-0414-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mak SS, Yeo W, Lee YM, et al. Risk factors for the initiation and aggravation of lymphoedema after axillary lymph node dissection for breast cancer. Hong Kong Med J. 2009;15(3):8–12. [PubMed] [Google Scholar]
- 28.Reeder-Hayes K, Bainbridge J, Meyer A, Amos K, Weiner B, Godley P, Carpenter W. Race and age disparities in receipt of sentinel lymph node biopsy for early-stage breast cancer. Breast Cancer Research and Treatment. 2011;128(3):863–871. doi: 10.1007/s10549-011-1398-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Cancer Society. Breast Cancer Facts & Figures 2013–2014. Atlanta: American Cancer Society, Inc; 2013. [Google Scholar]
- 30.Morehead-Gee AJ, Pfalzer L, Levy E, McGarvey C, Springer B, Soballe P, Gerber L, Stout NL. Racial disparities in physical and functional domains in women with breast cancer. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2012;20(8):1839–1847. doi: 10.1007/s00520-011-1285-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ness KK, Wall MM, Oakes JM, Robison LL, Gurney JG. Physical performance limitations and participation restrictions among cancer survivors: a population-based study. Annals of epidemiology. 2006;16(3):197–205. doi: 10.1016/j.annepidem.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 32.Gallicchio L, Calhoun C, Helzlsouer KJ. Association between race and physical functioning limitations among breast cancer survivors. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2014;22(4):1081–1088. doi: 10.1007/s00520-013-2066-2. [DOI] [PubMed] [Google Scholar]
- 33.Mao JJ, Su HI, Feng R, Donelson ML, Aplenc R, Rebbeck TR, Stanczyk F, DeMichele A. Association of functional polymorphisms in CYP19A1 with aromatase inhibitor associated arthralgia in breast cancer survivors. Breast Cancer Res. 2011;13(1):R8. doi: 10.1186/bcr2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand)[corrected] The Upper Extremity Collaborative Group (UECG) American journal of industrial medicine. 1996;(29):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 35.LeBlanc M, Stineman M, DeMichele A, Stricker C, Mao JJ. Validation of QuickDASH Outcome Measure in Breast Cancer Survivors for Upper Extremity Disability. Archives of Physical Medicine and Rehabilitation. 2014;95 (3):493–498. doi: 10.1016/j.apmr.2013.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 37.Judd CM, Kenny DA. Process analysis estimating mediation in treatment evaluations. Evaluation review. 1981;5(5):602–619. [Google Scholar]
- 38.James LR, Brett JM. Mediators, moderators, and tests for mediation. Journal of Applied Psychology. 1984;69(2):307. [Google Scholar]
- 39.Mediation. [ http://davidakenny.net/cm/mediate.htm]
- 40.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA: the journal of the American Medical Association. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 41.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA: the journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 42.Kumanyika S. Obesity in black women. Epidemiologic reviews. 1987;9:31–50. doi: 10.1093/oxfordjournals.epirev.a036307. [DOI] [PubMed] [Google Scholar]
- 43.Dignam JJ, Wieand K, Johnson KA, Raich P, Anderson SJ, Somkin C, Wickerham DL. Effects of obesity and race on prognosis in lymph node-negative, estrogen receptor-negative breast cancer. Breast cancer research and treatment. 2006;97(3):245–254. doi: 10.1007/s10549-005-9118-3. [DOI] [PubMed] [Google Scholar]
- 44.Irwin ML, McTiernan A, Bernstein L, Gilliland FD, Baumgartner R, Baumgartner K, Ballard-Barbash R. Physical activity levels among breast cancer survivors. Medicine and science in sports and exercise. 2004;36(9):1484. [PMC free article] [PubMed] [Google Scholar]
- 45.Ferraro KF, Su Y-p, Gretebeck RJ, Black DR, Badylak SF. Body mass index and disability in adulthood: a 20-year panel study. American Journal of Public Health. 2002;92(5):834–840. doi: 10.2105/ajph.92.5.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kwan ML, Darbinian J, Schmitz KH, Citron R, Partee P, Kutner SE, Kushi LH. Risk factors for lymphedema in a prospective breast cancer survivorship study: the Pathways Study. Archives of Surgery. 2010;145(11):1055. doi: 10.1001/archsurg.2010.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meeske KA, Sullivan-Halley J, Smith AW, McTiernan A, Baumgartner KB, Harlan LC, Bernstein L. Risk factors for arm lymphedema following breast cancer diagnosis in Black women and White women. Breast cancer research and treatment. 2009;113(2):383–391. doi: 10.1007/s10549-008-9940-5. [DOI] [PubMed] [Google Scholar]
- 48.Young A, Weltzien E, Kwan M, Castillo A, Caan B, Kroenke CH. Pre-to post-diagnosis weight change and associations with physical functional limitations in breast cancer survivors. Journal of Cancer Survivorship. 2014;8 (4):539–547. doi: 10.1007/s11764-014-0356-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abdel-Moneim R. The hazards of surgery in the obese. International surgery. 1984;70(2):101–103. [PubMed] [Google Scholar]
- 50.Choban PS, Flancbaum L. The impact of obesity on surgical outcomes: a review. Journal of the American College of Surgeons. 1997;185(6):593–603. doi: 10.1016/s1072-7515(97)00109-9. [DOI] [PubMed] [Google Scholar]
- 51.Bamgbade OA, Rutter TW, Nafiu OO, Dorje P. Postoperative complications in obese and nonobese patients. World journal of surgery. 2007;31(3):556–560. doi: 10.1007/s00268-006-0305-0. [DOI] [PubMed] [Google Scholar]
- 52.Demark-Wahnefried W, Campbell KL, Hayes SC. Weight management and its role in breast cancer rehabilitation. Cancer. 2012;118(S8):2277–2287. doi: 10.1002/cncr.27466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davenport DL, Xenos ES, Hosokawa P, Radford J, Henderson WG, Endean ED. The influence of body mass index obesity status on vascular surgery 30-day morbidity and mortality. Journal of vascular surgery. 2009;49(1):140–147.e141. doi: 10.1016/j.jvs.2008.08.052. [DOI] [PubMed] [Google Scholar]
- 54.Schuster JM, Rechtine G, Norvell DC, Dettori JR. The influence of perioperative risk factors and therapeutic interventions on infection rates after spine surgery: a systematic review. Spine. 2010;35(9S):S125–S137. doi: 10.1097/BRS.0b013e3181d8342c. [DOI] [PubMed] [Google Scholar]
- 55.Anaya DA, Dellinger EP. The obese surgical patient: a susceptible host for infection. Surgical infections. 2006;7(5):473–480. doi: 10.1089/sur.2006.7.473. [DOI] [PubMed] [Google Scholar]
- 56.Poirier P, Alpert MA, Fleisher LA, Thompson PD, Sugerman HJ, Burke LE, Marceau P, Franklin BA. Cardiovascular evaluation and management of severely obese patients undergoing surgery a science advisory from the American Heart Association. Circulation. 2009;120(1):86–95. doi: 10.1161/CIRCULATIONAHA.109.192575. [DOI] [PubMed] [Google Scholar]
- 57.Chen CL, Shore AD, Johns R, Clark JM, Manahan M, Makary MA. The impact of obesity on breast surgery complications. Plastic and reconstructive surgery. 2011;128(5):395e–402e. doi: 10.1097/PRS.0b013e3182284c05. [DOI] [PubMed] [Google Scholar]
- 58.McCarthy CM, Mehrara BJ, Riedel E, Davidge K, Hinson A, Disa JJ, Cordeiro PG, Pusic AL. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plastic and reconstructive surgery. 2008;121(6):1886–1892. doi: 10.1097/PRS.0b013e31817151c4. [DOI] [PubMed] [Google Scholar]
- 59.Selber JC, Kurichi JE, Vega SJ, Sonnad SS, Serletti JM. Risk factors and complications in free TRAM flap breast reconstruction. Annals of plastic surgery. 2006;56(5):492–497. doi: 10.1097/01.sap.0000210180.72721.4a. [DOI] [PubMed] [Google Scholar]
- 60.Hong S, Bardwell WA, Natarajan L, Flatt SW, Rock CL, Newman VA, Madlensky L, Mills PJ, Dimsdale JE, Thomson CA. Correlates of physical activity level in breast cancer survivors participating in the Women’s Healthy Eating and Living (WHEL) Study. Breast cancer research and treatment. 2007;101(2):225–232. doi: 10.1007/s10549-006-9284-y. [DOI] [PubMed] [Google Scholar]
- 61.Paxton RJ, Phillips KL, Jones LA, Chang S, Taylor WC, Courneya KS, Pierce JP. Associations among physical activity, body mass index, and health-related quality of life by race/ethnicity in a diverse sample of breast cancer survivors. Cancer. 2012;118(16):4024–4031. doi: 10.1002/cncr.27389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McCormack VA, Perry N, Vinnicombe SJ, dos Santos Silva I. Ethnic variations in mammographic density: a British multiethnic longitudinal study. American journal of epidemiology. 2008;168(4):412–421. doi: 10.1093/aje/kwn169. [DOI] [PubMed] [Google Scholar]
- 63.Ursin G, Ma H, Wu AH, Bernstein L, Salane M, Parisky YR, Astrahan M, Siozon CC, Pike MC. Mammographic density and breast cancer in three ethnic groups. Cancer Epidemiology Biomarkers & Prevention. 2003;12(4):332–338. [PubMed] [Google Scholar]
- 64.del Carmen MG, Halpern EF, Kopans DB, Moy B, Moore RH, Goss PE, Hughes KS. Mammographic breast density and race. American Journal of Roentgenology. 2007;188(4):1147–1150. doi: 10.2214/AJR.06.0619. [DOI] [PubMed] [Google Scholar]
- 65.Krieger N. Refiguring “Race” Epidemiology: Epidemiology, Racialized Biology, and Biological Expressions of Race Relations. International Journal of Health Services. 2000;30(1):211–216. doi: 10.2190/672J-1PPF-K6QT-9N7U. [DOI] [PubMed] [Google Scholar]
- 66.Krieger N. A glossary for social epidemiology. Journal of epidemiology and community health. 2001;55(10):693–700. doi: 10.1136/jech.55.10.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Campesino M, Saenz DS, Choi M, Krouse RS. Oncology nursing forum: 2012. Onc Nurs Society; 2012. Perceived discrimination and ethnic identity among breast cancer survivors; pp. E91–E100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Quach T, Nuru-Jeter A, Morris P, Allen L, Shema SJ, Winters JK, Le GM, Gomez SL. Experiences and perceptions of medical discrimination among a multiethnic sample of breast cancer patients in the Greater San Francisco Bay Area, California. American journal of public health. 2012;102(5):1027–1034. doi: 10.2105/AJPH.2011.300554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Oberst K, Bradley CJ, Schenk M. Breast and prostate cancer patient’s reliability of treatment reporting. Journal of registry management. 2008;36 (1):12–15. [PubMed] [Google Scholar]