Abstract
Objective
The purpose of this study was to examine whether parenting moderated the association between maternal depressive symptoms and initial levels and growth of preadolescent internalizing and externalizing symptoms.
Method
This study used a community sample of pre-adolescent children (N=214; 8–12 years old at Time 1), measuring maternal depressive symptoms and parenting at Time 1, and preadolescent internalizing and externalizing symptoms at each year for 3 years.
Results
After modeling latent growth curves of internalizing and externalizing symptoms, growth factors were conditioned on maternal depressive symptoms, positive (acceptance and consistent discipline) and negative (rejection and physical punishment) parenting, and the interactions of depression and parenting. Maternal rejection moderated the relation of maternal depression with internalizing symptoms, such that high rejection exacerbated the effects of maternal depressive symptoms on initial levels of preadolescent internalizing problems. There were no significant interactions predicting externalizing problems.
Conclusion
The findings highlight how specific parenting behaviors may alter the way in which maternal depressive symptoms confer risk for behavior problems.
Keywords: maternal depression, parenting, preadolescence, internalizing symptoms, externalizing symptoms
Several factors, including father involvement, child self-regulation, and supportive environments, appear to minimize the negative effect that maternal depression has on offspring (Mezulis, Hyde, & Clark, 2004; Silk, Shaw, Forbes, Lane, & Kovacs, 2006). Notably, these moderating factors are external to the mother. In contrast, little is known about factors exhibited by depressed mothers that may also minimize or exacerbate risk to children. A critical, yet frequently overlooked, moderating factor of maternal depression is the parenting behaviors of the mother herself. Although it is known that compromised parenting is an important factor by which maternal depressive symptoms confer risk for child and adolescent psychopathology (Foster, Garber, & Durlak, 2008; Pugh & Farrell, 2012; van der Molen, Hipwell, Vermeiren, & Loeber, 2011), there is evidence to suggest that parenting may not be uniformly compromised in the presence of depression (Lovejoy, Graczyk, O’Hare, & Neuman, 2000). In fact, the deleterious effects of maternal depressive symptoms on children’s adjustment problems may be mitigated if a mother is able to engage in positive parenting. Conversely, negative aspects of parenting may exacerbate children’s risk for developing mental health problems of their own. As depression is a heterogeneous disorder (American Psychiatric Association, & DSM-5 Task Force, 2013; Lamers et al., 2012; Østergaard, Jensen, & Bech, 2011) it is reasonable to expect that mothers with depressive symptoms may engage in a wide range of parenting behaviors, spanning both positive behaviors, such as acceptance and consistent discipline, and negative behaviors, such as rejection and physical punishment. This study examined whether positive and negative aspects of maternal parenting mitigated or exacerbated the effects of maternal depressive symptoms on initial levels and trajectories of child adjustment problems.
To date, only a few cross-sectional studies have examined whether parenting interacts with maternal depression to predict adjustment in children. In one such study of a sample of 15-year-olds (Brennan, Le Brocque, & Hammen, 2003), adolescent-perceived maternal warmth, low psychological control, and low emotional over-involvement each interacted with maternal depression to predict resilient outcomes. The current study highlights the possibility that parenting is not uniformly compromised in the face of depressive symptoms, and further, identifies specific parenting behaviors that may mitigate the risk associated with maternal depression. When considering parenting dimensions that may exacerbate risk, another cross-sectional study of 9–15 year old children found that for girls, but not for boys, maternal insensitivity, in the context of depression, predicted significantly greater internalizing problems (Garai et al., 2009).
The present study sought to build upon this sparse literature. First, this study employed a longitudinal design that examines initial levels and trajectories of preadolescent adjustment in relation to maternal depressive symptoms and parenting. The presence of longitudinal effects suggests an important pathway by which these interactions relate to the unfolding of mental health concerns over time. Second, this study builds upon the previous literature by simultaneously testing multiple dimensions of positive and negative parenting behaviors. Examining a total of four parenting behaviors (two positive and two negative dimensions) may provide a more nuanced understanding of how parenting, in the context of maternal depression, predicts the development of internalizing or externalizing problems.
Testing these relations during preadolescence is important for several reasons. Given the developmental task of individuating during preadolescence, mothers must renegotiate aspects of parenting that provide both continued support, oversight, and also autonomy granting (Jaffee & Poulton, 2006). Children’s perception of their mother’s ability to engage in this push and pull of warmth and control, or to struggle with these changing dynamics, are shown to be associated with differences in the emergence of adjustment problems (Buschgens et al., 2010; Mesman & Koot, 2000). Furthermore, the preadolescent period marks the time when higher internalizing or externalizing symptoms relative to peers may indicate a greater likelihood for developing serious psychopathology during the adolescent period (Merikangas, Nakamura, & Kessler, 2009). Therefore, modeling initial levels and trajectories of adjustment problems is critical to identify children at greatest risk.
In addition to developmental considerations, confounding variables need to be considered when examining the links between maternal depression, parenting, and child adjustment. Specifically, maternal depression is more often noted in women in low income families, which is also a known risk factor for child adjustment problems (Hasin, Goodwin, Stinson, & Grant, 2005; Perry & Fantuzzo, 2010). In addition, child age and sex are differentially associated with adjustment problems (Merikangas et al., 2009). As such, family income, child age and sex were included as covariates. Finally, as clinical diagnoses as well as a continuum of maternal depressive symptoms have been shown to be related to poorer child outcomes (Goodman et al., 2011), we chose to examine how parenting in the presence of the continuum of maternal depressive symptoms would be relevant to changes in pre-adolescents’ adjustment.
Method
Participants
Third through fifth grade children and their mothers were recruited through children’s public school classrooms. Schools were selected to represent the range of sociodemographic characteristics of the urban area surrounding our Pacific Northwest university to ensure that the sample included an adequate representation of families of color, single- and two-parent households, and a full range of family income. Approximately 1280 families from 59 classrooms in 13 schools were approached to participate; 697 families returned the information forms, with 313 families indicating potential interest in participating. One child in the target grades per family was asked to participate, and if there was more than one child in the target grades in the family, one child was randomly selected to participate. Children with developmental disabilities and families not fluent in English were excluded from the study to ensure that questionnaires were fully understood. At Time 1, 214 families participated, at Time 2, 196 families participated, and at Time 3, 201 families participated. Participants with missing data on any variable at Times 2 or 3 were compared to those with complete data on child age, child sex, family income, maternal depressive symptoms, all parenting dimensions and T1 internalizing and externalizing problems. The t-tests indicated that participants with any missing data (n=27) only differed from those with no missing data (n=187) on income (missing, M=4.71, SD=2.54; no missing, M=6.89, SD=3.18, t (208) = 3.22, p<0.01). The relation of income to missingness was a moderate effect (r = 0.35), however, it did not reach previously cited thresholds for introducing substantial bias (e.g., r >0.40; Collins et al, 2001).
Children’s mean age at Time 1 was 9.5 years (SD = 1.0, range 8–12). The sample included 14% African American children, 2% Asian American children, 3% Latino or Hispanic children, 3% Native American, 72 % European American or White children, and 6% children identified with multiple ethnic backgrounds. Fifty-six percent of children were female. Ninety-four percent of the female primary caregivers were biological, 4% were adoptive, and 2% were grandmothers. Seventy percent of children lived in households with two caregivers. Annual family income was distributed roughly evenly across sextiles of income: 11% less than $20,000; 11.4% $21,000 to $40,000; 17.1% $41,000 to $60,000; 16.7% $61,000 to $80,000; 19% $81,000 to $100,000, and 15.7% over $100,000. Mothers’ average level of educational attainment was some college or technical/professional school.
Procedures
Data were collected in highly scripted 2.5 hour home visits. After confidentiality was explained, mothers signed informed consent forms and children signed assent forms. Mothers and children were interviewed by separate, trained interviewers in separate rooms when possible to maintain privacy. Families received $40 ($50 if 2 parents participated) for participating at time 1, with compensation increasing by $10 each year the family participated. Each assessment was separated by 1 year. All procedures were approved by the University of Washington Institutional Review Board.
Measures
Maternal depressive symptoms and children’s perception of parenting were measured at Time 1. Mother and child report of child adjustment were measured at all three time points. Means, standard deviations, and ranges of scales are reported in Table 1.
Table 1.
Correlations, means, and standard deviations of key study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child Age | - | .06 | .00 | −.14 | −.05 | −.05 | .17* | −.19* | −.06 | −.11 | −.01 | −.03 | .00 | .15 |
| 2. Child Sex | - | -- | −.08 | .14* | −.08 | .12 | −.12 | .08 | .02 | .01 | .03 | .29** | .31** | .31** |
| 3. Family Income | - | -- | -- | −.32** | .06 | −.23** | .13 | −.26** | −.26** | −.28** | −.27** | −.24** | −.29** | −.23** |
| 4. Maternal Depressive Symptoms | - | -- | -- | -- | −.11 | .17* | −.14* | .12 | .28** | .26** | .26** | .22** | .18* | .18* |
| 5. Acceptance | - | -- | -- | -- | -- | −.44** | .19** | −.16** | −.26** | −.25** | −.25** | −.25** | −.27** | −.19** |
| 6. Rejection | - | -- | -- | -- | -- | -- | −.61** | .45** | .45** | .33** | .26** | .39** | .40** | .18* |
| 7. Consistent Discipline | - | -- | -- | -- | -- | -- | -- | −.35** | −.35** | −.17* | −.14 | −.30** | −.30** | −.20** |
| 8. Physical Punishment | - | -- | -- | -- | -- | -- | -- | -- | .50** | .30** | .30** | .53** | .44** | .36** |
| 9. Time 1 Internalizing | - | -- | -- | -- | -- | -- | -- | -- | -- | .64** | .58** | .57** | .43** | .27** |
| 10. Time 2 Internalizing | - | -- | -- | -- | -- | -- | -- | -- | -- | -- | .76** | .40** | .52** | .34** |
| 11. Time 3 Internalizing | - | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | .40** | .48** | .53** |
| 12. Time 1 Externalizing | - | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | .66** | .58** |
| 13. Time 2 Externalizing | - | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | .68** |
| 14. Time 3 Externalizing | - | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
|
| ||||||||||||||
| Means | - | -- | -- | 17.38 | 31.65 | 10.04 | 7.31 | 1.07 | 18.55 | 17.21 | 16.48 | 4.53 | 4.07 | 3.74 |
| SD | - | 9.87 | 7.05 | 5.96 | 5.61 | 2.11 | 5.30 | 5.63 | 5.04 | 3.36 | 3.07 | 3.16 | ||
| Range | - | -- | -- | 1.00–53.00 | 0.00–40.00 | 0.00–32.00 | 0.00–30.00 | 0.00–12.00 | 9.00–41.00 | 0.00–40.00 | 9.50–37.00 | 0.05–23.50 | 0.00–21.00 | 0.00–18.50 |
Sex = Girls = 1, Boys = 2.
p ≤ .05;
p ≤ .01
Maternal Depression
Mothers reported on their depressive symptoms over the previous month using the 20-item Center for Epidemiological Studies—Depression Scale (CES-D; Radloff, 1977). This measure has been reliably used in community and clinical settings with an alpha of .91 calculated in the present study. Mothers indicated how true each item was for them, with each item ranging on a four-point scale, 0 (never), 1 (rarely), 2 (sometimes), and 3 (often). A sizable portion of the sample, 46.3%, scored equal to or greater than 16 which is the cut-off used to identify mild levels of depression and 10% scored equal to or greater than 32, which is used as the clinically significant cut-off score (Berkman et al., 1986). Given our interest in examining maternal depressive symptoms, the continuous score was used in analyses.
Parenting
At Time 1, children reported on their mother’s parenting. Children’s report of parenting was selected to reflect the child’s individual experience of parenting rather than shared family experiences reflected in parent report of parenting (Feinberg, Neiderhiser, Howe, & Hetherington, 2001). Children reported on maternal acceptance (10 items), rejection (8 items), and inconsistent discipline (8 items) using a version of the Child Report of Parenting Behavior Inventory (CRPBI), a scale that has been used in a community sample of children (Teleki, Powell, & Dodder, 1982). Inconsistent discipline was reversed scored in order to become the consistent discipline measure. The CRPBI has been measured in numerous preadolescent samples that have reported alphas > .80 for the subscales. Children responded using a 5-point scale to indicate whether each item was 0 (never), 1 (rarely), 2 (sometimes), 3 (often) or 4 (always) like the parent. Scale alphas for acceptance, rejection, and inconsistent discipline were .89, .78, and .82, respectively. In addition, children reported on the physical punishment subscale of the Alabama Parenting Questionnaire (APQ; Shelton, Frick, & Wootton, 1996, α = .70). The response format was similar to the CRPBI, and children indicated whether parents spanked, slapped or hit them with an object. Scores ranged from 0–12, with 61% of the sample scoring 0, and approximately 9% of the sample scoring 3 or greater, suggesting that a small minority of the sample reported moderate to high levels of physical punishment.
Children’s Internalizing and Externalizing Problems
Mother and child report of adjustment problems were obtained and combined to create a cross-reporter measure in order capture various perspectives of symptoms and reduce shared reporter variance (King, Lengua, & Monahan, 2013). All mother and child reports were scored using a mean weighted sum, derived by multiplying the mean of the items by the number of items. Prior to combining cross-reporter measures, several analytic steps were taken to determine whether this approach was acceptable. First, we assessed the feasibility of creating a combined externalizing problems score. Mothers reported on children’s externalizing problems using 21 items from the Child Behavior Checklist (Achenbach, 1991) that were identified by expert ratings and empirical criteria as indicating conduct problems and oppositional behaviors (Lengua et al 2001). Mothers rated their children’s behavior on a scale of 0 (not true), 1 (sometimes true), or 2 (often true) such that higher scores indicated greater externalizing problems (T1 M= 4.11, SD= 3.53; T2 M= 3.77; SD=3.78; T3 M = 3.49; SD= 3.30). Children’s report of externalizing problems was assessed using the delinquent and aggressive behavior subscales (28 items) of the Youth Self Report (Achenbach, 1991) in which children rated items as 0 (not true), 1 (sometimes true), or 2 (often true). Higher scores indicated greater externalizing problems (T1 M = 4.88; SD= 4.38; T2 M = 4.41, SD = 4.07; T3 M = 4.00; SD = 4.18). Mother and child report of externalizing problems were correlated .40, .40, and .42 (all p<.001) at times 1, 2, and 3, respectively. Mother and child report of externalizing problems were then averaged (composite α = .87).
Next, we examined the feasibility of creating an aggregate internalizing problems score. Self-report of child depression was assessed with the 27-item Child Depression Inventory (CDI, Kovacs, 1981) in which children endorsed statements on a scale of 0–2 with higher scores indicating more severity (T1 M = 5.63, SD = 5.03; T2 M = 4.78, SD = 5.07; T3 M = 4.28, SD = 5.08). Children were also administered 19 of the 28 items on the Revised Children’s Manifest Anxiety Scale (RCMAS, Reynolds & Richmond, 1978). Nine items were excluded that were identified as poor indicators of anxiety or as overlapping with temperament or depression following procedures used in prior research (Lengua, West & Sandler, 1998). Children rated the items either as 1 (No) or 2 (Yes) with higher scores indicating higher anxiety (T1 M = 24.39, SD = 4.35; T2 M = 22.87, SD = 4.07; T3 M = 21.96, SD = 3.35). Next, the scales were combined by summing the items from the two scales to create a child report internalizing problems score (T1 M = 29.89, SD = 8.65; T2 M = 27.65, SD = 8.40, T3 M = 26.20, SD = 7.43). Mother’s reported on children’s internalizing symptoms using 24 items from the CBCL identified in a previous study as indicating depressive and anxious/obsessive symptoms (Lengua et al., 2001), rating their children’s behavior as 0 (not true), 1 (sometimes true), or 2 (often true) with higher scores indicating more internalizing problems (T1 M = 7.11, SD = 4.94; T2 M = 6.75, SD = 4.96; T3 M = 6.45, SD = 4.79). Mother and child report of internalizing symptoms were correlated .20 (p<.01) at all 3 time points. Next, mother and child internalizing symptoms scores were averaged such that both reporters contributed equally to the internalizing symptom composite (composite α = .88).
Additional steps were taken to ensure that it was appropriate and feasible to combine across reporters (Lengua, 2008). Specifically, a confirmatory factor analysis (CFA) was conducted to verify the adequacy of a cross-reporter composite of internalizing and externalizing problems. The CFA, based on the covariance matrix and using maximum likelihood estimation, demonstrated an adequate fit to the data at all time points, with all estimated factor loadings being significant. This suggests that combining across reporters was feasible. Ultimately, observed scores were used instead of factor scores as to not bias the internalizing symptoms score to be weighted more by child report which included two measures and to simplify analyses.
Analytic Plan
Families were included if they had available data from at least one time point. All analyses were conducted in Mplus 6.0 (Muthen & Muthen, 2006) and used Full Information Likelihood Estimation (FIMLE). Use of FIMLE was considered appropriate given that the missing data analyses reported above suggest little bias was introduced by missing data. Correlations between the parenting variables were also examined to assess for potential multicollinearity. The highest correlation between any of the two parenting variables was < .7. In addition, Variance Inflation Factor statistics ranged from 1.09 to 2.01 and tolerance statistics ranged from .50 to .92, indicating that multicollinearity was not likely a problem.
Next, unconditional latent growth curve (LGC) models were specified for internalizing and externalizing problems. After these models were specified, the intercept and slope of internalizing and externalizing problems, were conditioned or regressed on covariates (child age, sex, family income, and co-occurring behavior problem), maternal depressive symptoms, the four parenting variables (acceptance, consistent discipline, rejection, physical punishment) and all four parenting by maternal depression interactions to test whether parenting moderated the effects of maternal depressive symptoms on child outcome. To test for moderation, we used the multiplicative of the mean-centered parenting and maternal depressive symptoms variables (Curran, Bauer, & Willoughby, 2004). Because LGC considers change over time, three way interactions were examined with maternal depressive symptoms as the focal predictor (Preacher, Curran, & Bauer, 2006).
Results
Table 1 presents the descriptive statistics and correlations among the covariates, maternal depression, and parenting. Our a priori decision to include the covariates (family income, child age, child sex, and co-occurring time 1 behavior problems) was supported by significant correlations with study variables. In addition, maternal depressive symptoms were related to greater rejection and inconsistent discipline, as well as greater internalizing and externalizing problems. Modest to moderate associations between maternal depressive symptoms and parenting suggested that there was variability in parenting at different levels of depressive symptoms. Thus, it was plausible that parenting might moderate the relation of maternal depressive symptoms to initial levels and slopes of internalizing and externalizing problems.
Growth in Symptoms
Latent growth curve models were used to examine the initial levels and trajectories of internalizing and externalizing symptoms over time. Models were specified in which factor loadings were set to define the intercept as levels of symptoms at Time 1 and the slope as linear change across 3 years. Model fit was evaluated using the Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Root Mean Square Error of Approximation (RMSEA), and the Standardized Root Mean Square Residual (SRMR). For CFI and TLI, we used the conventional cutoffs of ≥.90 for acceptable fit and ≥.95 for good fit (Hu & Bentler, 1999; McDonald & Ho, 2002). RMSEA values <.08 represent acceptable fit, while values <.05 indicate good fit (Chen, Curran, Bollen, Kirby, & Paxton, 2008). SRMR values <.10 support acceptable fit, while values <.08 support good fit (Bryne, 1998). Consistent with the assumptions of LGC, growth factors were first examined without predictors to examine variability in levels and changes of children’s internalizing and externalizing symptoms. The internalizing symptoms model fit the data well, χ2 (1) = .61, p = .44, RMSEA = <.001, CFI = 1.00, TLI = 1.004, SRMR = .01, as did the externalizing problems unconditional model, χ2 (1) = .03, p = .87, RMSEA = <.001, CFI = 1.00, TLI = 1.012, SRMR = .002. The mean values for the slopes were negative for internalizing symptoms, b = −1.02, p < .001, and externalizing problems, b = −.41, p < .001, indicating that on average, symptoms decreased across the three years. However, approximately 27% of children had increasing internalizing symptoms and 34% had increasing externalizing symptoms from time 1 to 3. Variance for the slope of internalizing symptoms was significant (b = 4.63, p <.001), while the variance for the externalizing problems slope was not (b = .53, p = .29). Despite the non-significant variance around the externalizing slope, we proceeded with analyses because in conditional models, the covariates might clarify variance of the factors and additional degrees of freedom provide additional power to detect variations in effects.
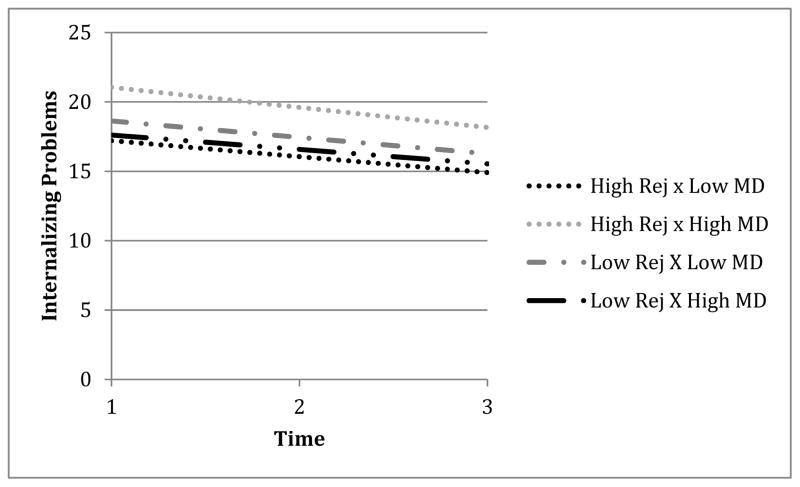
Next, we tested the main and moderated effects of maternal depression and the four parenting variables on the initial levels and slopes of internalizing and externalizing problems (Table 2). The model for internalizing symptoms fit the data well, χ2 (14) = 14.74, p =.40, RMSEA = .02, CFI = .99, TLI = .99, SRMR =.013, and the externalizing problems model demonstrated an acceptable fit, χ2 (14) = 25.16, p =.03, RMSEA = .07, CFI = .96, TLI = .89, SRMR = .02. Maternal depressive symptoms were associated with higher initial levels of internalizing problems. Greater physical punishment was associated with higher initial internalizing and externalizing problems. There was a significant interaction between rejection and maternal depressive symptoms predicting the intercept of child internalizing problems. There were no significant interactions predicting the slopes of internalizing or externalizing problems. The significant interaction was probed following guidelines set forth by Preacher, Curran & Bauer (2006), which tested for significance at +/− 1 SD of rejection (i.e. +/− 5.96) and maternal depressive symptoms (i.e. +/−9.87). As shown in Figure 1 preadolescents who had mothers with high depressive symptoms and high rejection had the highest initial internalizing problems (M = 21.06) relative to those with mothers high in depressive symptoms and low rejection (M = 17.62), who did not differ from the other groups in their levels of internalizing symptoms.
Table 2.
Unstandardized (b), standard errors (SE), and the standardized coefficient (β) of maternal depression, parenting, and interactions of maternal depression and parenting regressed on the intercept and slope of pre-adolescent internalizing and externalizing problems.
| Internalizing Intercept | Internalizing Slope | Externalizing Intercept | Externalizing Slope | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| b | SE | β | b | SE | β | b | SE | β | b | SE | β | |
| Child Sex | .24 | .56 | .03 | .27 | .30 | .10 | .24 | .36 | .05 | .23 | .20 | .17 |
| Child Age | −.40 | .28 | −.09 | .24 | .15 | .18 | −.20 | .18 | −.08 | .02 | .10 | .03 |
| Family Income | −.12 | .10 | −.08 | −.03 | .05 | −.07 | −.08 | .06 | −.10 | −.01 | .03 | −.05 |
| Time 1 Externalizing | .52 | .11 | .36 | −.09 | .06 | −.21 | -- | -- | -- | -- | -- | -- |
| Time 1 Internalizing | -- | -- | -- | -- | -- | -- | .20 | .04 | .40 | −.06 | .02 | −.45 |
| Maternal Depression | .09 | .03 | .19 | −.01 | .02 | −.06 | .01 | .02 | .04 | −.003 | .01 | −.04 |
|
| ||||||||||||
| Acceptance | −.05 | .05 | −.07 | −.01 | .02 | −.05 | −.04 | .03 | −.12 | −.003 | .02 | −.03 |
| Rejection | .10 | .08 | .12 | .001 | .04 | .003 | .04 | .05 | .09 | −.05 | .03 | −.39 |
| Consistent Discipline | −.07 | .06 | −.10 | .05 | .03 | .23 | −.02 | .11 | −.05 | −.02 | .02 | −.21 |
| Physical Punishment | −.44 | .18 | .20 | −.14 | .09 | −.21 | .28 | .01 | .22 | −.06 | .06 | −.19 |
|
| ||||||||||||
| Interaction of Maternal Depression x Acceptance | .002 | .004 | .03 | −.003 | .002 | −.18 | −.002 | .003 | −.06 | .000 | .001 | .01 |
| Rejection | .02 | .007 | .23 | .000 | .004 | −.02 | −.005 | .004 | −.11 | .001 | .002 | .06 |
| Consistent Discipline | .01 | .01 | .13 | −.01 | .004 | −.25 | −.001 | .004 | −.03 | −.003 | .002 | −.22 |
| Physical Punishment | −.03 | .02 | −.11 | −.01 | .01 | −.11 | −.02 | .01 | −.12 | .004 | .006 | .10 |
p ≤ .05 is bolded
Figure 1.
Interaction of Rejection x Maternal Depressive Symptoms predicting initial levels of preadolescent internalizing problems.
Finally, the possibility that the pattern of relations differed across gender was explored by using cross-group or “stacked” models that compared a model in which parameter estimates were free to be estimated separately across gender with a model in which parameter estimates were constrained to be equal across gender. The difference score in the nested chi-squares was non-significant (Internalizing symptoms model = χ2 difference (2) = 2.31, p =n.s.; Externalizing symptoms model = χ2 difference (2) = 2.99, p =n.s), indicating that there were not significant differences in parameter estimates across girls and boys.
Discussion
The study tested whether children’s perceptions of positive and negative parenting moderated the relation between maternal depressive symptoms and initial levels and trajectories of internalizing and externalizing problems in preadolescents. Although there was a direct effect of maternal depression on initial levels of child internalizing symptoms, we also found evidence that this association was conditioned by maternal rejection, which exacerbated the association between maternal depressive symptoms and preadolescents’ initial levels of internalizing problems. In addition, the use of physical punishment was associated with higher initial levels of both internalizing and externalizing problems, even when controlling for the other parenting variables.
Prior to discussing the significant findings, it is important to comment on the pattern of symptoms observed in this sample over the three years. For most children, symptoms of internalizing and externalizing problems declined over time (Kiff et al., 2011; Lengua, 2008), even though a sizable minority of children demonstrated increasing symptoms. Although it is typically assumed that symptoms increase with age, a pattern of declining symptoms in this developmental period has been previously noted (Gullone, King, & Ollendick, 2001).
The current study adds to the small literature on whether parenting moderates the association of maternal depression on child adjustment. We found that preadolescent’s whose mothers’ depressive symptoms were coupled with higher levels of maternal rejection reported the highest initial levels of internalizing problems, suggesting that maternal rejection exacerbated the effects of maternal depressive symptoms. It may be that experiencing rejection from a mother high in depressive symptoms may overwhelm a preadolescents ability to regulate their emotions, which contributes to higher internalizing symptoms (Keenan, Hipwell, Hinze, & Babinski, 2009). In addition, it could be that depressed mothers who do not engage in rejecting behaviors toward their children have other additional resources, such as social or partner support, or are engaged in mental health treatment, all of which support their overall parenting. Additionally, these resources may contribute to lower behavior problems in relatively advantaged children compared to children who experience their mother with depression to be rejecting. In contrast to our hypotheses, we did not find evidence that preadolescent’s perceptions of positive aspects of parenting, such as consistent discipline and acceptance, were protective in the presence of maternal depressive symptoms. There could be several reasons why we did not find evidence that positive parenting attenuated the effects of maternal depressive symptoms on child outcome. First, it may be that children who perceive their mothers as accepting and consistent are at lower risk for emotional and behavioral problems, regardless of whether their mother was depressed. It is also possible that the preadolescent children who perceived their mothers as more accepting and consistent were doing better in ways that were not measured in our study.
It is also noteworthy that significant results were limited to associations with intercept and not slope. There were no significant main effects or interactions predicting trajectories of internalizing and externalizing problems. It is possible that the exacerbating effects of parenting in the presence of maternal depression are time-specific, having contemporaneous rather than long-term effects. This could be tested in future work by the inclusion of maternal depression and parenting effects at each time point. However, such a model would have overtaxed the sample size available.
In addition to a significant interaction, there were several important main effects to consider. It is interesting to note that different patterns of results were found when comparing findings from the zero-order correlations, to the regression effects in which all parenting dimensions were tested simultaneously, and to the interaction effects. For instance, when considering only the correlational patterns, maternal depressive symptoms were related to both internalizing and externalizing problems, which is consistent with the literature (Goodman, et al., 2011). However, the relation between maternal depressive symptoms and externalizing problems was minimized when tested simultaneously with the covariates, parenting variables and interaction effects in the model. In contrast, maternal depressive symptoms continued to significantly predict internalizing problems. This suggests that the development of internalizing versus externalizing problems maintains different pathways (Cicchetti & Rogosch, 1996) and also highlights that univariate versus multivariate approaches to understanding the relation among maternal depression, parenting, and child outcomes may differ. In contrast, physical punishment was an important predictor of both internalizing and externalizing problems suggesting that it has rather pervasive effects on children’s adjustment (Bender et al., 2007; Stormshak, Bierman, McMahon, & Lengua, 2000), despite being relatively rare at this developmental stage.
The study had several strengths, which include adding to the small literature on the effects of maternal depression symptoms during preadolescence (Lovejoy et al., 2000). First, by controlling for initial levels of co-occurring behavior problems while testing multiple parenting behaviors simultaneously, we were able to examine the unique predictors of initial levels and trajectories of internalizing and externalizing problems. Second, from a theoretical perspective, the present study focus is rare in that it examined the possibility that mothers with depressive symptoms may engage in some aspects of positive parenting. The maternal depression literature is dominated by studies that set forth to examine the deleterious effects of maternal depression on parenting imparted by a mother’s depression symptoms. While we did not find evidence to support the notion that positive parenting in the context of maternal depression was associated with fewer child symptoms, the framework of this study is a worthy direction for future investigation.
Despite these strengths, the study had several limitations. Other important variables were either not measured or not included due to power constraints. Within and outside the home, fathers’ influence and potential psychopathology (Brennan, Hammen, Katz, & Le Brocque, 2002), neighborhood risk (Bush, Lengua, & Colder, 2010), and peer relations (Kupersmidt & Coie, 1990) are critical predictors of child outcome during the pre-adolescent period. Another limitation to this study was our use of questionnaire measures and the shared reporter variance resulting from children reporting on parenting and their own symptoms. Although we attempted to mitigate this concern by using aggregated mother and child report of symptoms, the results are nonetheless biased by shared-reporter variance. The study was also limited due to our inability to model maternal depressive symptoms and parenting at each time point, which would have permitted examining the time-varying effects of the predictors. A larger sample would also have increased the power to be able to detect potentially significant interactions, which are notably challenging to detect in the social sciences (McClelland & Judd, 1993). Furthermore, it is possible that the sample may not be adequately representative of the community, potentially undermining the generalizability of the findings, however, this is unlikely to have introduced much bias as the sample was stratified on income to obtain adequate variability on risk and parenting variables. A final limitation is that causal inferences are limited by the non-experimental design of the study.
Summary
This study provides modest evidence that internalizing and externalizing problems in preadolescents differ as a function of maternal depressive symptoms and parenting. Clinical implications of this work include the potential benefit of addressing parenting in the context of maternal depressive symptoms, as the interaction of a child’s experience of maternal depressive symptoms and rejecting parenting may exacerbate emotional problems.
Acknowledgments
Support for this research was provided by NIMH Grant #R29MH57703 to the third author.
References
- Achenbach TM. Manual for the child behavior checklist and revised child behavior profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- American Psychiatric Association, American Psychiatric Association, & DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5. Arlington, Va: American Psychiatric Association; 2013. [Google Scholar]
- Bender HL, Allen JP, McElhaney KB, Antonishak J, Moore CM, Kelly HO, Davis SM. Use of harsh physical discipline and developmental outcomes in adolescence. Development and Psychopathology. 2007;19(1):227–242. doi: 10.1017/S0954579407070125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman LF, Berkman CS, Kasl S, Freeman DH, Jr, Leo L, Ostfeld AM, Brody JA. Depressive symptoms in relation to physical health and functioning in the elderly. American Journal of Epidemiology. 1986;124(3):372–388. doi: 10.1093/oxfordjournals.aje.a114408. [DOI] [PubMed] [Google Scholar]
- Brennan PA, Hammen C, Katz AR, Le Brocque RM. Maternal depression, paternal psychopathology, and adolescent diagnostic outcomes. Journal of Consulting and Clinical Psychology. 2002;70(5):1075–1085. doi: 10.1037/0022-006X.70.5.1075. [DOI] [PubMed] [Google Scholar]
- Bryan 1998.Byrne BM. Structural Equation Modeling with LISREL, PRELIS and SIMPLIS: Basic Concepts, Applications and Programming. Mahwah, New Jersey: Lawrence Erlbaum Associates; 1998. [Google Scholar]
- Buschgens CJM, van Aken MAG, Swinkels SHN, Ormel J, Verhulst FC, Buitelaar JK. Externalizing behaviors in preadolescents: familial risk to externalizing behaviors and perceived parenting styles. European Child & Adolescent Psychiatry. 2010;19(7):567–575. doi: 10.1007/s00787-009-0086-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush NR, Lengua LJ, Colder CR. Temperament as a moderator of the relation between neighborhood and children’s adjustment. Journal of Applied Developmental Psychology. 2010;31(5):351–361. doi: 10.1016/j.appdev.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An Empirical Evaluation of the Use of Fixed Cutoff Points in RMSEA Test Statistic in Structural Equation Models. Sociological Methods & Research. 2008;36(4):462–494. doi: 10.1177/0049124108314720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Equifinality and multifinality in developmental psychopathology. Development and Psychopathology. 1996;8(04):597–600. doi: 10.1017/S0954579400007318. [DOI] [Google Scholar]
- Curran PJ, Bauer DJ, Willoughby MT. Testing Main Effects and Interactions in Latent Curve Analysis. Psychological Methods. 2004;9(2):220–237. doi: 10.1037/1082-989X.9.2.220. [DOI] [PubMed] [Google Scholar]
- Feinberg M, Neiderhiser J, Howe G, Hetherington EM. Adolescent, parent, and observer perceptions of parenting: Genetic and environmental influences on shared and distinct perceptions. Child Development. 2001;72(4):1266–1284. doi: 10.1111/1467-8624.00346. [DOI] [PubMed] [Google Scholar]
- Foster CJE, Garber J, Durlak JA. Current and past maternal depression, maternal interaction behaviors, and children’s externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2008;36(4):527–537. doi: 10.1007/s10802-007-9197-1. [DOI] [PubMed] [Google Scholar]
- Garai EP, Forehand RL, Colletti CJM, Reeslund K, Potts J, Compas B. The relation of maternal sensitivity to children’s internalizing and externalizing problems within the context of maternal depressive symptoms. Behavior Modification. 2009;33(5):559–582. doi: 10.1177/0145445509342581. http://dx.doi.org.pitt.idm.oclc.org/10.1177/0145445509342581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14(1):1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Gullone E, King NJ, Ollendick TH. Self-Reported Anxiety in Children and Adolescents: A Three-Year Follow-Up Study. The Journal of Genetic Psychology. 2001;162(1):5–19. doi: 10.1080/00221320109597878. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of Major Depressive Disorder: Results From the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Jaffee SR, Poulton R. Reciprocal Effects of Mothers’ Depression and Children’s Problem Behaviors from Middle Childhood to Early Adolescence. In: Huston AC, Ripke MN, editors. Developmental contexts in middle childhood: Bridges to adolescence and adulthood. New York, NY US: Cambridge University Press; 2006. pp. 107–129. [Google Scholar]
- Keenan K, Hipwell A, Hinze A, Babinski D. Equanimity to Excess: Inhibiting the Expression of Negative Emotion is Associated with Depression Symptoms in Girls. Journal of Abnormal Child Psychology. 2009;37(5):739–747. doi: 10.1007/s10802-009-9301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiff L, Lengua LJ, Bush NR. Temperament variation in sensitivity to parenting: predicting changes in depression and anxiety. Journal of Abnormal Child Psychology. 2011;39(8):1199–212. doi: 10.1007/s10802-011-9539-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King KM, Lengua LJ, Monahan KC. Individual differences in the development of self-regulation during pre-adolescence: Connections to context and adjustment. Journal of Abnormal Child Psychology. 2013;41(1):57–69. doi: 10.1007/s10802-012-9665-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school aged children. Acta Paedopsychiatry. 1981;46:305–315. [PubMed] [Google Scholar]
- Kupersmidt JB, Coie JD. Preadolescent peer status, aggression, and school adjustment as predictors of externalizing problems in adolescence. Child Development. 1990;61(5):1350–1362. doi: 10.2307/1130747. [DOI] [PubMed] [Google Scholar]
- Lamers F, Rhebergen D, Merikangas KR, de Jonge P, Beekman ATF, Penninx BWJH. Stability and transitions of depressive subtypes over a 2-year follow-up. Psychological Medicine. 2012;42(10):2083–2093. doi: 10.1017/S0033291712000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengua LJ. Anxiousness, Frustration, and Effortful Control as Moderators of the Relation between Parenting and Adjustment in Middle-childhood. Social Development. 2008;17(3):554–577. doi: 10.1111/j.1467-9507.2007.00438.x. [DOI] [Google Scholar]
- Lengua LJ, Sadowski CA, Friedrich WN, Fisher J. Rationally and empirically derived dimensions of children’s symptomatology: Expert ratings and confirmatory factor analyses of the CBCL. Journal of Consulting and Clinical Psychology. 2001;69:683–698. [PubMed] [Google Scholar]
- Lengua LJ, West SG, Sandler IN. Temperament as a predictor of symptomatology in children: assessing contamination of measures. Child Development. 1998;69(1):164–181. [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20(5):561–592. doi: 10.1016/S0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114(2):376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues in Clinical Neuroscience. 2009;11(1):7–20. doi: 10.31887/DCNS.2009.11.1/krmerikangas. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesman J, Koot HM. Common and specific correlates of preadolescent internalizing and externalizing psychopathology. Journal of Abnormal Psychology. 2000;109(3):428–437. doi: 10.1037/0021-843X.109.3.428. [DOI] [PubMed] [Google Scholar]
- Mezulis AH, Hyde JS, Clark R. Father Involvement Moderates the Effect of Maternal Depression During a Child’s Infancy on Child Behavior Problems in Kindergarten. Journal of Family Psychology. 2004;18(4):575–588. doi: 10.1037/0893-3200.18.4.575. [DOI] [PubMed] [Google Scholar]
- Muthen B, Muthen L. Mplus user’s guide (Version) 6. Los Angeles, CA: Muthen & Muthen; 2006. [Google Scholar]
- Østergaard SD, Jensen SOW, Bech P. The heterogeneity of the depressive syndrome: When numbers get serious. Acta Psychiatrica Scandinavica. 2011;124(6):495–496. doi: 10.1111/j.1600-0447.2011.01744.x. [DOI] [PubMed] [Google Scholar]
- Perry MA, Fantuzzo JW. A multivariate investigation of maternal risks and their relationship to low-income, preschool children’s competencies. Applied Developmental Science. 2010;14(1):1–17. doi: 10.1080/10888690903510281. [DOI] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Pugh KL, Farrell AD. The impact of maternal depressive symptoms on adolescents’ aggression: Role of parenting and family mediators. Journal of Child and Family Studies. 2012;21(4):589–602. doi: 10.1007/s10826-011-9511-y. [DOI] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children’s manifest anxiety. Journal of Abnormal Child Psychology. 1978;6:271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child Psychology. 1996;25(3):317–329. doi: 10.1207/s15374424jccp2503_8. [DOI] [Google Scholar]
- Silk JS, Shaw DS, Forbes EE, Lane TL, Kovacs M. Maternal Depression and Child Internalizing: The Moderating Role of Child Emotion Regulation. Journal of Clinical Child & Adolescent Psychology. 2006;35(1):116–126. doi: 10.1207/s15374424jccp3501_10. [DOI] [PubMed] [Google Scholar]
- Stormshak EA, Bierman KL, McMahon RJ, Lengua LJ Conduct Problems Prevention Research Group. Parenting practices and child disruptive behavior problems in early elementary school. Journal of Clinical Child Psychology. 2000;29(1):17–29. doi: 10.1207/S15374424jccp2901_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teleki JK, Powell JA, Dodder RA. Factor analysis of reports of parental behavior by children living in divorced and married families. Journal of Psychology: Interdisciplinary and Applied. 1982;112(2):295–302. doi: 10.1080/00223980.1982.9915387. [DOI] [PubMed] [Google Scholar]
- Van der Molen E, Hipwell AE, Vermeiren R, Loeber R. Maternal characteristics predicting young girls’ disruptive behavior. Journal of Clinical Child and Adolescent Psychology. 2011;40(2):179–190. doi: 10.1080/15374416.2011.546042. [DOI] [PMC free article] [PubMed] [Google Scholar]