In December 2013, the first local transmission of chikungunya virus in the Western Hemisphere was reported, beginning with autochthonous cases in Saint Martin. Since then, local transmission has been reported in 31 countries or territories throughout the Americas, including locations in the United States and its territories (Florida, Puerto Rico, and the U.S. Virgin Islands) (see figure). As of August 8, 2014, a total of 576,535 suspected and laboratory-confirmed chikungunya cases had been reported in the Americas, a case count that had nearly doubled over the previous month (see interactive graphic, available with the full text of this article at NEJM.org).1 The rapid spread of the virus is probably attributable to a lack of population immunity and the broad distribution in the Americas of vectors capable of transmitting the virus.
Figure. Countries and Territories with Autochthonous Transmission or Imported Cases of Chikungunya Virus Infection, as of August 1, 2014.
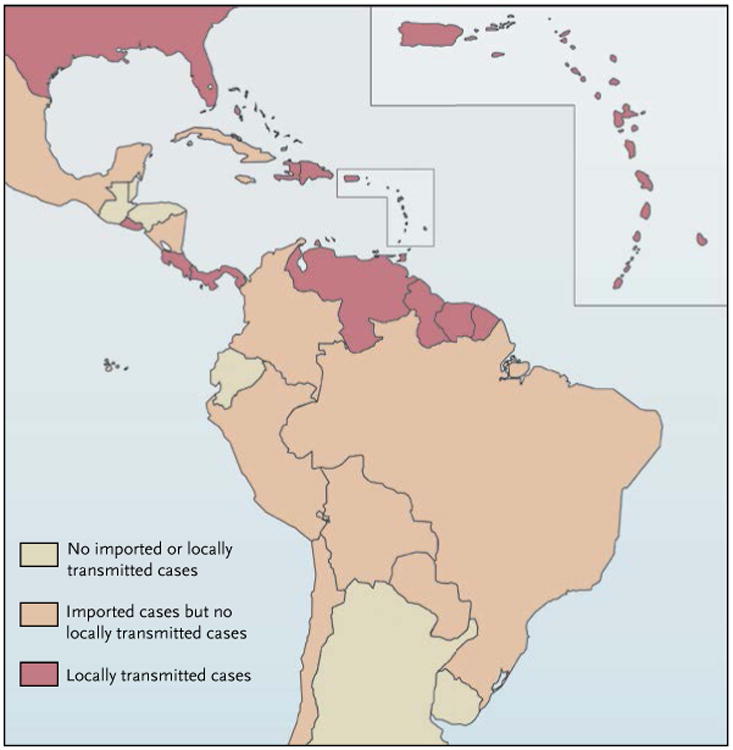
Data are from the Pan American Health Organization.
Chikungunya virus is a mosquito-borne alphavirus transmitted primarily by Aedes aegypti and Ae. albopictus mosquitoes. These vectors are aggressive daytimebiting mosquitoes that can also transmit dengue virus. Both are found throughout much of the Americas, including areas in the southern, eastern, and central United States. Humans are the primary amplifying host for chikungunya virus, meaning that they have high enough levels of viremia during the first week of illness to infect mosquitoes that bite them. The majority (72 to 97%) of infected people develop symptomatic disease.2 Although very rare, other modes of transmission have been documented, including bloodborne, in utero, and intrapartum transmission.
The most common clinical symptoms of chikungunya virus infection are acute fever and polyarthralgia. Joint pains are usually bilateral and symmetric, and they can be severe and debilitating.2 Other symptoms may include headache, myalgia, arthritis, conjunctivitis, vomiting, and maculopapular rash. Persons at risk for severe or atypical disease include neonates exposed intra partum, adults older than 65 years of age, and persons with underlying medical conditions (e.g., hypertension, diabetes, or cardiovascular disease).3
The acute symptoms of chikungunya typically resolve within 7 to 10 days. Some patients have a relapse of rheumatologic symptoms (e.g., polyarthralgia, polyarthritis, or tenosynovitis) in the months after the acute illness. Joint pains may persist for months to years in some patients (published studies have reported variable proportions, from 5 to 60%).2,3 Death due to chikungunya virus infection is rare (<1% of infected persons) and occurs mostly in older adults.
The differential diagnosis of chikungunya virus infection varies according to the place of resience, travel history, and exposures. Dengue and chikungunya viral infections have similar clinical features, can circulate in the same area, and occasionally coinfect the same person. Chikungunya virus infection more frequently causes high fever, severe arthralgia, arthritis, rash, and lymphopenia, whereas dengue virus infection more frequently causes neutropenia, thrombocytopenia, hemorrhage, shock, and death.2 Other diagnoses to consider include leptospirosis, malaria, rickettsia, group A streptococcus, rubella, measles, parvovirus, enteroviruses, adenovirus, other alphavirus infections (e.g., Mayaro, Ross River, Barmah Forest, o'nyong-nyong, and Sindbis viruses), postinfection arthritis, and rheumatologic conditions.
A diagnosis of chikungunya virus infection should be considered in patients with an acute onset of fever and polyarthralgia, especially if they have recently been in areas with known chikungunya outbreaks. A reverse-transcriptase–polymerase-chain-reaction test of serum for chikungunya viral RNA is usually positive in the first 5 days after illness onset, though it sometimes remains positive for up to 8 days after onset. Serum specimens collected 5 days or more after symptoms begin should also be evaluated for virus-specific IgM antibodies.2 Testing for chikungunya virus is available through several state health laboratories, one commercial laboratory, and the Centers for Disease Control and Prevention (CDC). Clinicians should report suspected chikungunya cases to their state or local health department to facilitate diagnostic testing and mitigate the risk of local transmission.
We currently have no specific treatment, vaccine, or preventive drug for chikungunya. Treatment is palliative and includes rest, fluids, analgesics, and antipyretics.3 Given the similar geography and symptoms associated with chikungunya and dengue, patients should also be evaluated for dengue virus infection; proper clinical management of dengue reduces the risk of complications and death. Persistent joint pain from chikungunya may be reduced by nonsteroidal anti-inflammatory drugs, glucocorticoids, or physiotherapy.3
Chikungunya virus infection is best prevented by avoiding mosquito bites — by staying indoors and using air conditioning or having intact screens on windows and doors to prevent mosquitoes from coming indoors, and by using insect repellents and wearing long sleeves and pants when outdoors. Infected persons should be protected from mosquitoes during the first week of illness to prevent further viral spread. At a community level, mosquito-habitat control and appropriate applications of larvicide and adulticide may reduce viral spread.3 However, experience with dengue in the Americas has taught us that substantial vector-control resources would be needed to curb the current outbreak.
Before the cases on Saint Martin, the only chikungunya cases identified in the Americas were in travelers. CDC data show that from 2006 through 2013, an average of 28 cases per year (range, 5 to 65) of chikungunya virus disease were identified in travelers visiting or returning to the United States from affected areas, mostly in Asia. None of these cases resulted in local transmission or outbreaks. As of August 5, a total of 484 laboratory-confirmed chikungunya cases had been reported in 2014 from U.S. states; although most occurred in travelers returning from affected areas, 4 locally transmitted cases have been identified in Florida. An additional 392 laboratory-confirmed and 1705 suspected cases have been reported from Puerto Rico and the U.S. Virgin Islands.
Given their similarities, dengue might provide the best predictive model for the expected course of chikungunya in the United States. In 2013, 2.4 million cases of dengue were reported in the Americas, including 773 travel-related and 49 locally transmitted cases in the continental United States. Several factors will probably help mitigate the spread of chikungunya in the continental United States, including the ability to avoid mosquito bites by using air conditioning in homes and businesses. During a dengue outbreak on the Texas–Mexico border in 1999, Ae. aegypti moquitoes were three times as abundant on the American side as on the Mexican side, but the number of persons infected with dengue virus was twice as high on the Mexican side.4 Analysis revealed that the absence of air conditioning in one's home was the factor most closely associated with testing positive for dengue.
There is no population immunity to chikungunya virus in the Americas. The number of cases will therefore continue to increase in places where local transmission has occurred, and the virus will spread to new areas in the region. In the French territories initially affected by the outbreak, 12 to 15% of the population has already presented for medical care with symptoms compatible with chikungunya virus infection.1 On the basis of previous surveys, we can expect at least 30% of populations in areas with local circulation to become infected unless control measures or seasonal conditions intervene.3,5 In temperate areas, colder temperatures and autumn conditions will reduce the abundance of vectors and probably stop virus transmission, as occurred with a chikungunya outbreak in Italy in 2007.5 In tropical areas, the intensity of transmission will probably wane as drier conditions take hold. However, because the relevant mosquitoes often breed in water-holding containers (e.g., flowerpots, gutters, buckets, or birdbaths) in and around homes, drier conditions are unlikely to stop transmission completely. In fact, there was a chikungunya outbreak in Kenya at a time of drought, since people were keeping more water-storage containers in and around their homes.
The future course of the chikungunya virus outbreak is uncertain. It is not known what role Ae. albopictus may play in transmitting this virus in more temperate areas or whether an enzootic cycle will be established to maintain the virus in the region. It's also unclear how the coexistence of chikungunya and dengue will affect the epidemiology of these diseases in the region or whether the long-term morbidity will be as pronounced as that seen after outbreaks around the Indian Ocean. Only time will tell how this emerging virus will behave in relatively new and uncharted territory.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Washington, DC: Pan American Health Organization; Chikungunya. http://www.paho.org/hq/index.php?option=com_topics&view=article&id=343&Itemid=40931. [Google Scholar]
- 2.Staples JE, Breiman RF, Powers AM. Chikungunya fever: an epidemiological review of a re-emerging infectious disease. Clin Infect Dis. 2009;49:942–8. doi: 10.1086/605496. [DOI] [PubMed] [Google Scholar]
- 3.Preparedness and response for chikungunya virus introduction in the Americas. Washington, DC: Pan American Health Organization; 2011. http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&gid=16984&Itemid=&lang=en) [Google Scholar]
- 4.Reiter P, Lathrop S, Bunning M, et al. Texas lifestyle limits transmission of dengue virus. Emerg Infect Dis. 2003;9:86–9. doi: 10.3201/eid0901.020220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moro ML, Gagliotti C, Silvi G, et al. Chikungunya virus in North-Eastern Italy: a seroprevalence survey. Am J Trop Med Hyg. 2010;82:508–11. doi: 10.4269/ajtmh.2010.09-0322. [DOI] [PMC free article] [PubMed] [Google Scholar]


