Abstract
Background
The cyclooxygenase 2 (COX-2) pathway has been implicated in the molecular pathogenesis of many malignancies, including lung cancer. Apricoxib, a selective COX-2 inhibitor, has been described to inhibit epithelial-mesenchymal transition (EMT) in human malignancies. The mechanism by which apricoxib may alter the tumor microenvironment by affecting EMT through other important signaling pathways is poorly defined. IL-27 has been shown to have anti-tumor activity and our recent study showed that IL-27 inhibited EMT through a STAT1 dominant pathway.
Objective
The purpose of this study is to investigate the role of apricoxib combined with IL-27 in inhibiting lung carcinogenesis by modulation of EMT through STAT signaling.
Methods and Results
Western blot analysis revealed that IL-27 stimulation of human non-small cell lung cancer (NSCLC) cell lines results in STAT1 and STAT3 activation, decreased Snail protein and mesenchymal markers (N-cadherin and vimentin) and a concomitant increase in expression of epithelial markers (E-cadherin, β-and γ-catenins), and inhibition of cell migration. The combination of apricoxib and IL-27 resulted in augmentation of STAT1 activation. However, IL-27 mediated STAT3 activation was decreased by the addition of apricoxib. STAT1 siRNA was used to determine the involvement of STAT1 pathway in the enhanced inhibition of EMT and cell migration by the combined IL-27 and apricoxib treatment. Pretreatment of cells with STAT1 siRNA inhibited the effect of combined IL-27 and apricoxib in the activation of STAT1 and STAT3. In addition, the augmented expression of epithelial markers, decreased expression mesenchymal markers, and inhibited cell migration by the combination treatment were also inhibited by STAT1 siRNA, suggesting that the STAT1 pathway is important in the enhanced effect from the combination treatment.
Conclusion
Combined apricoxib and IL-27 has an enhanced effect in inhibition of epithelial-mesenchymal transition and cell migration in human lung cancer cells through a STAT1 dominant pathway.
Keywords: IL-27, Apricoxib, STAT1, STAT3, Epithelial-Mesenchymal Transition, COX-2, A549, Non-small cell lung cancer
Introduction
The tumor progression model is a complex interplay of irreversible genetic modifications coupled with reversible events in the tumor microenvironment. Reversible events such as epithelial-mesenchymal transition (EMT) represent a process whereby cells of epithelial origin remodel in response to extracellular signals or through intracellular effector molecules leading to a loss of apical-basolateral polarity, loss of intracellular junctions and decreased cell-cell adhesions [1]. The resulting protein modifications confer a motile phenotype to the epithelial cells, with partial or complete resemblance to the phenotype of mesenchymal cells [2]. EMT and its dysregulation have become widely studied as an integral step in fibrosis, carcinogenesis, and metastasis [1,3]. Therapeutic strategies aimed at targeting various pathways involved in EMT to prevent or reverse invasion and metastasis could be beneficial for both early and late stages of cancer.
Interleukin (IL)-27, a recently discovered member of the IL-12 cytokine family, has been shown to inhibit proliferation, angiogenesis, and metastasis in several cancer cell lines and in vivo models [4-10]. IL-27 is a heterodimeric molecule that is expressed by antigen presenting cells, and its receptor associates with cytoplasmic protein kinases, such as JAKs (Janus Kinases) to activate the transcriptional factors, STAT (Signal Transducer and Activator of Transcription), specifically STAT1 and STAT3 [11-13]. STAT1 and STAT3 are known to regulate transcription of target genes playing opposing roles in carcinogenesis, where STAT1 is a tumor suppressor and STAT3 is a tumor promoter [14]. Our recent study demonstrated that IL-27 activates both the STAT1 and STAT3 pathways in human non-small cell lung cancer (NSCLC) cells, and that the balance of STAT1 and STAT3 activation is important in inhibiting EMT [15]. We have also shown that IL-27 functions through a STAT1 dominant pathway, whose basal expression may also be responsible for repressing the oncogenic effects of STAT3 [15].
It has been shown that COX-2 overexpression induces carcinogenesis [16-18], making COX-2 an attractive anticancer therapeutic target. Numerous studies have been conducted to evaluate the role of COX-2 inhibitors in the chemoprevention of many cancers, including NSCLC [19,20]. Apricoxib is a novel COX-2 selective inhibitor with antitumor activity [21-23]. In preclinical studies, apricoxib was shown to inhibit tumor growth in solid tumors, including NSCLC and colon cancer and appeared to be more effective than other COX-2 inhibitors [22,23]. Kirane et al. showed that apricoxib treatment resulted in a shift towards a more epithelial phenotype in tumor cells and induced reversal of EMT in a xenograft model [24,25]. However, the mechanism, by which apricoxib exhibits antitumor activity associated with the reversal of EMT, remains unknown. Interestingly, Ho et al. showed that IL-27 exerted anti-tumor activity in lung cancer cells by suppressing COX-2 expression [26].
In this study, we hypothesized that apricoxib may target the tumor microenvironment by modulation of EMT through the STAT pathways and a combination treatment of apricoxib and IL-27 may enhance antitumor activity. To test this hypothesis, we examined the combined effect of apricoxib on IL-27 mediated STAT activation and EMT inhibition. We provide evidence that apricoxib potentiates IL-27 mediated-STAT1 activation and inhibits IL-27 mediated-STAT3 activation. In addition, treatment with apricoxib induces mesenchymalepithelial transition (MET) in lung cancer cells and potentiates the MET in combination with IL-27 through a STAT1 dependent mechanism. Our results provide new insights into the mechanisms by which a novel COX-2 inhibitor, apricoxib, may exhibit antitumor activity through STAT1-mediated induction of MET.
Materials and Methods
Cell lines and culture
Human NSCLC cells (A549) were obtained from the American Type Culture Collection (Rockville, MD). The cells were authenticated utilizing Promega's DNA IQ System and Powerplex 1.2 system and tested for Mycoplasma using the MycoAlert Mycoplasma Detection Kit (Lonza Walkersville). The cells were maintained in RPMI-1640 with L-glutamine (Hyclone, Logan, UT) supplemented with 5% fetal bovine serum (FBS; Gemini Bio-products, West Sacramento, CA) in a humidified atmosphere of 5% CO2 at 37°C.
Reagents
Recombinant human IL-27 (R&D Systems, Inc., Minneapolis, MN) was added at a concentration of 50 ng/mL in serum free medium. Opti-MEM I Reduced Serum Medium and Lipofectamine 2000 reagents (Invitrogen, Carlsbad, CA) were utilized for transfection. Apricoxib (also known as TG01; Tragara Pharmaceuticals, San Diego, CA) is a selective COX-2 inhibitor. It was diluted in ethanol and added to the cells at concentrations between 0.016-10 μM in a serum free medium.
Transfection of STAT1 small interfering RNA into A549
Cells were seeded in 6-well plates and grown to 40-50% confluence at the time of transfection. For each sample, 2.5 μL of siRNA was diluted in 200 μL of Opti-MEM I. STAT1 siRNA II (Cell Signaling) was used to inhibit STAT1, and a non-targeting siRNA was used as a control siRNA. Similarly, 2.5 μL of Lipofectamine 2000 was diluted in 200 μL of Opti-MEM I. After 5 minutes of incubation at room temperature, the diluted oligomer was combined with the diluted Lipofectamine 2000 and incubated for 30 minutes at room temperature. The oligomer-Lipofectamine 2000 complexes were then added to each well containing the cells and medium and mixed gently. The cells were then incubated at 37°C in a CO2 incubator for 6 hours after which the wells were washed and replaced with serum free medium. The cells were then treated with IL-27 and/or apricoxib per experimental design.
Western blot
Cell lysates were prepared with RadioImmunoPrecipitation Assay (RIPA) buffer (PBS, 1% NP-40, 0.5% Na-deoxycholate, 0.1% SDS) containing protease inhibitors on ice after washing with PBS and were centrifuged at 13,000 rpm for 15 minutes at 4°C. Protein concentrations of cell lysates were measured by BCA assay and up to 20 μg of total protein was used for each SDS-PAGE. Western blot was performed after transferring SDS-PAGE gels to Amersham Hybond-ECL membranes (GE Healthcare, Piscataway, NJ). Membranes were further processed to detect the following: phosphorylated-STAT1 (Tyr 701), phosphorylated-STAT3 (Tyr 705), Snail (Cell Signaling), N-cadherin, Vimentin, E-cadherin, γ-catenin, β-catenin (BD Biosciences, San Jose, CA), and GAPDH (Advanced ImmunoChemical, Long Beach, CA).
In vitro cell motility assay
A549 cells were plated in 24-well flat-bottom plates and allowed to adhere overnight prior to serum starvation. The cells were treated with various conditions when 50-60% confluence was reached and then grown for several days to 90-95% confluence. The cell monolayer was wounded by creating a scratch in each well with a 200 μL pipette tip. The same fields, where the scratch was made, were observed using a phase-contrast microscope (50x magnifications) for up to four days. Images were processed using Image J [27]. The leading edge was manually outlined using the pencil tool. Next, images were threshold such that only the outlines remained, creating a binary image. The area occupied by cells was calculated using the “analyze particles” function. Percent area invaded was calculated according to published procedures [28]: % area invaded = [100-(% area day 2 or day 4/% area day 0)*100].
Results
Apricoxib augments STAT1 activation and inhibits STAT3 activation mediated by IL-27
It has been previously shown that apricoxib exerts antitumor activity against NSCLC [25]. In addition, our laboratory has recently demonstrated that IL-27 activates both STAT1 and STAT3 transcriptional factors and shows antitumor activity in lung cancer cells [15]. We hypothesized that apricoxib may enhance the effect of IL-27-mediated STAT activation.
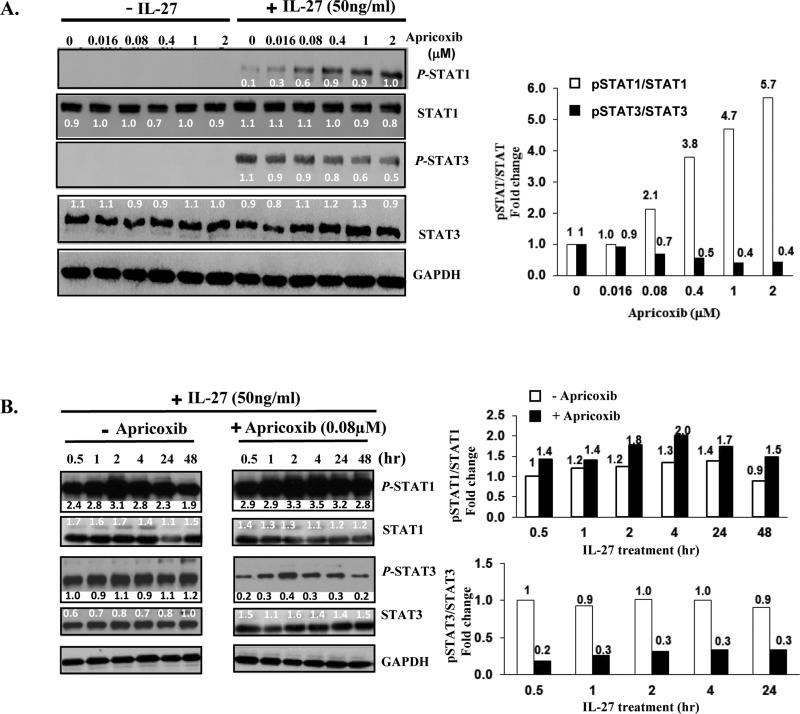
NSCLC A549 cells were treated with apricoxib (0.016-2 μM) for 4 hours prior to IL-27 exposure for 15 minutes. The activated (tyrosine phosphorylated) forms of STAT1 and STAT3 were assessed by Western blot. As shown in Figure 1A, apricoxib pretreatment prior to IL-27 exposure resulted in a dose-dependent increase in STAT1 activation and a concomitant decrease in STAT3 activation without significant changes in total STAT1 and STAT3 levels. Densitometric analysis showed that apricoxib treatment followed by IL-27 enhanced STAT1 activation in a dose-dependent manner and increased the activation by a factor of 5.7 at 2 μM apricoxib while the same treatment resulted in reduced STAT3 activation and decrease in the activation by a factor of 0.4 at 2 μM apricoxib (Figure 1A). In contrast, no treatment or apricoxib treatment alone showed no activation of the STAT pathways.
Figure 1.
Effect of apricoxib on IL-27 mediated STAT activation. (A) A549 cells were treated with apricoxib (0.016-2 μM) for 4 hours prior to IL-27 exposure IL-27 (50 ng/mL) for 15 minutes, and the tyrosine phosphorylated forms of STAT1 and STAT3 (P-STAT1; P-STAT3) were detected by Western Blot. The values above the figures represent the relative density of the bands after normalization to GAPDH by densitometry using NIH software, Image J. pSTAT/STAT levels were expressed as fold change with respect to 0 μM apricoxib treated cells. (B) The effect of pretreatment with apricoxib on IL-27 induced STAT activation. A549 cells were pretreated with apricoxib (0.08 μM) up to 48 hours prior to IL-27 (50 ng/mL) exposure for 15 minutes, and expression of STAT1 and STAT3 activation was demonstrated by Western Blot. At this apricoxib dose, pre-treatment for 4 hours was sufficient to augment STAT1 and inhibit STAT3 activation by IL-27. The values above the figures represent relative density of the bands after normalization to GAPDH by densitometry using NIH software, Image J. pSTAT/STAT levels were expressed as fold change with respect to 0 μM apricoxib with IL-27 (0.5 hr) treated cells.
Next, we determined if the duration of apricoxib pre-treatment had an impact on STAT activation. Cells were pretreated with apricoxib at a single dose (0.08 μM) for 0 to 48 hours prior to IL-27 exposure for 15 minutes. The single dose of 0.08 μM was chosen in consideration of the moderate activity of apricoxib on the IL-27-mediated STAT activation as shown in Figure 1A. As expected, apricoxib-pretreated cells showed further enhanced activation of STAT1 mediated by IL-27 from 30 minutes up to 48 hours compared to untreated cells (Figure 1B). More importantly, IL-27-mediated STAT3 activation was dramatically diminished by pretreatment of apricoxib. These results indicate that apricoxib intensifies the IL-27 effect on the activation of STAT1 and STAT3.
Densitometric analysis revealed that the enhanced effect of apricoxib pretreatment on IL-27-mediated STAT1 activation was maximal at 4 hours by a factor of 2.0. In addition, the IL-27-mediated STAT3 activation was decreased by a factor of 0.3 at 4 hours apricoxib pretreatment (Figure 1B). As the effects of apricoxib were most prominent at the pretreatment of 4-hour, at which point the maximal effect of both enhanced STAT1 activation and diminished STAT3 activation was shown, the 4-hour pretreatment was then utilized for further evaluation.
IL-27 enhances the apricoxib effect on the reversal of EMT
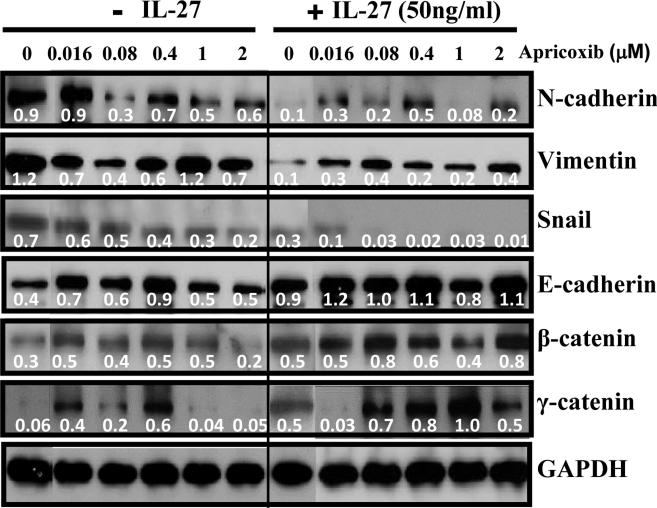
Recent studies showed that apricoxib reverses EMT in human colon and pancreatic cancer cells [24,25]. In addition, we have recently found that IL-27 induces mesenchymal-epithelial transition in lung cancer cells [15]. Thus, we determined whether apricoxib modulates IL-27 mediated MET. A549 human lung cancer cells were pretreated with apricoxib followed by IL-27. In accordance with our previous observation, IL-27–treated cells showed more epithelial phenotype with decreased expression of the mesenchymal markers (N-cadherin, vimentin and snail) and increased expression of epithelial markers (E-cadherin, β- and γ-catenin) (Figure 2). When cells were treated with apricoxib (0.016-2 μM) alone, overall expression of N-cadherin, vimentin and snail, mesenchymal cell markers, was decreased compared to untreated cells. N-cadherin and vimentin expression levels were unchanged at 0.016 μM and 1 μM, respectively. It was notable that the apricoxib effect on the decreased expression of mesenchymal markers was augmented by the addition of IL-27 at 0.016-2 μM. It should be noted that cells completely lost expression of N-cadherin at 1 μΜ of apricoxib with combination of IL-27 in comparison to cells treated with apricoxib alone (densitometry value 0.5 vs 0.08). Furthermore, Snail expression was nearly undetectable by combination treatment of apricoxib with IL-27 and was further decreased compared to IL-27 treatment alone, suggesting that the decreased snail expression resulted from the enhanced actions of apricoxib and IL-27. In agreement with other studies [24,25], apricoxib treatment in our study also resulted in increased expression of E-cadherin in lung cancer cells at 0.016-2 μM.
Figure 2.
Effect of IL-27 and apricoxib combination of EMT marker expression. A549 cells were treated with apricoxib for 4 hours prior to IL-27 exposure for 24 hours. Expression levels of markers responsible for the mesenchymal (N-cadherin, vimentin, and snail) and epithelial (E-cadherin, γ-catenin, and β-catenin) phenotypes were evaluated by Western Blot after exposure to IL-27 (50 ng/mL) or apricoxib (0.016-2 μM) for 24 hours alone or in combination. The combination treatment resulted in down-regulation of N-cadherin (at 1 μM apricoxib) and Snail and up-regulation of the epithelial markers when compared to the IL-27 alone treatment group. The values above the figures represent relative density of the bands after normalization to GAPDH.
The increase in E-cadherin expression was enhanced by combination with IL-27.
Additionally apricoxib treatment resulted in increased expression of additional epithelial markers, β-catenin (0.016-1 μM) and γ-catenin (0.016-0.4 μM). The apricoxib effect of increase in expression of epithelial markers (β-catenin and γ-catenin) was further enhanced by the addition of IL-27. This enhanced effect was not observed in γ-catenin expression at the low concentration (0.016 μM). Although we found that the decreased expression of Snail by IL-27 was further diminished by apricoxib, the effect of apricoxib on the reversal EMT effect of IL-27 was not evident in other EMT markers such as N-cadherin and vimentin. Taken together, these results suggest that IL-27 augments the effect of apricoxib on the reversal of EMT in A549 lung cancer cells.
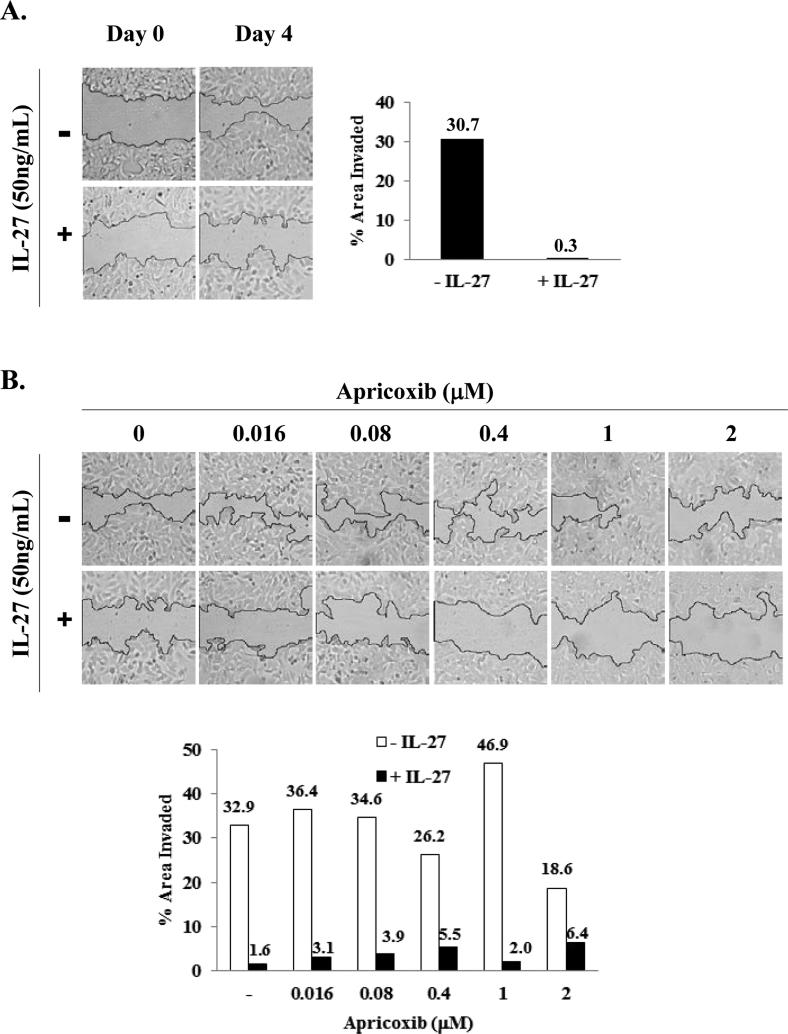
Apricoxib in combination with IL-27 augments the inhibition of cell motility
We have recently found that IL-27 inhibits in vitro cell migration [15]. We next examined the effect of apricoxib alone or in combination with IL-27 on cell motility. Scratch assay was conducted on A549 cells to assess cell migration that is a defining feature of the mesenchymal phenotype. As shown in Figures 3A, only a few cells migrated on day 4 after treatment with IL-27 (0.3% area invaded) while untreated cells showed considerable migration (31% area invaded). Untreated cells demonstrated cell migration within 16 hours after wounding (data not shown). When cells were treated with apricoxib at 0.016 ~ 2 μM, there was moderate inhibition only at 0.4 or 2 μM (32% area invaded at 0 μM apricoxib vs 26% and 18% area invaded at 0.4 and 2 μM, respectively) (Figure 3B, upper panel and Figure 3B, bottom figure). However, following apricoxib pretreatment, IL-27 treatment remarkably enhanced the inhibition of cell migration compared to apricoxib alone at 0.016 ~2 μM (Figure 3B, lower panel). The enhanced inhibitory effect on the migration was most prominent at 1 μM apricoxib treatment (46% area invaded at 1 μM apricoxib vs 2.0% area invaded at 1 μM apricoxib+IL-27) (Figure 3B, bottom figure). Our results indicate that combined treatment of apricoxib with IL-27 enhanced inhibition on cell migration.
Figure 3.
Effect of apricoxib on IL-27 mediated inhibition of cell motility in vitro. (A) Scratches were made in 90~95 % confluence after A549 cells were treated with IL-27 (50 ng/ml) at 60~70% confluence. The cells were then observed up to 4 days under the microscope for cell motility (100x magnification). The edges of the wound at day 0 are outlined with solid black lines. (B) The effect of apricoxib (0.016-2 μM) alone or with pre-treatment for 4 hours followed by IL-27 exposure (50 ng/mL) on A549 cell motility after 4 days of culture. Scratches were generated in the same way as in (A). Images were analyzed and % area invaded was measured as described in Materials and Methods.
STAT1 is required for the enhanced effect of apricoxib with IL-27 on reversal of EMT
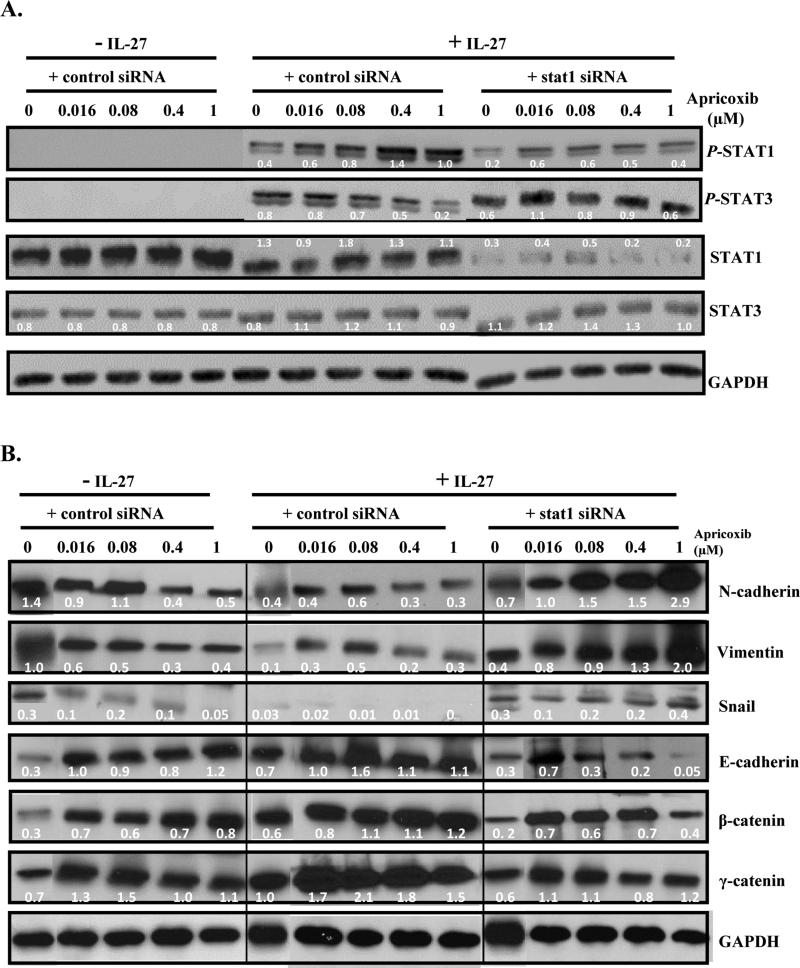
Our recent study showed that the EMT inhibitory effect of IL-27 is dependent on STAT1 activation [15]. To determine if STAT1 activation is required for the enhanced effect of apricoxib and IL-27 on inhibition of reversal EMT, cells were transfected with STAT1 siRNA. After transfection with STAT1siRNA, cells showed effective knockdown (~90%) of STAT1 and remarkably reduced STAT1 activation (Figure 4A). IL-27 treatment induced robust activation of STAT1 and STAT3 in control siRNA-treated cells (Figure 4A). Pretreatment with apricoxib (0.016-1 μM) augmented IL-27-mediated STAT1 activation and suppressed STAT3 activation in a dose dependent manner (IL-27+control siRNA; Figure 4A). As expected, the augmented IL-27-mediated STAT1 activation by apricoxib was reversed by STAT1 siRNA treatment (IL-27+ stat1 siRNA; Figure 4A). STAT1 inhibition in IL-27 treated cells resulted in enhanced STAT3 activation, highlighting the potential of STAT1 in the regulation of STAT3 activation in lung carcinogenesis. The dramatic suppression of IL-27–mediated STAT3 activation by apricoxib (IL27+controlsiRNA+apricoxib) was completely reversed by inhibition of STAT1 activation (IL27+stat1siRNA+apricoxib; Figure 4A). These results suggest that apricoxib inhibits IL-27-mediated STAT3 activation by enhancing STAT1 activation.
Figure 4.
Role of STAT1 in the enhancing effect of apricoxib and IL-27 on the inhibition of EMT. A549 cells were treated with a STAT1 siRNA (40 nM) or a non-targeting control siRNA (40 nM) for 6 hours prior to treatment with IL-27 (50 ng/mL) for 15 minutes and/or apricoxib (0.016-1 μM) for 4 hours. Activated and total STAT1 and STAT3 expression levels (A) and EMT marker expression (B) were demonstrated by Western blot. The values above the figures represent relative density of the bands after normalization to GAPDH.
To evaluate the role of STAT1 in apricoxib and IL-27 combined treatment mediated EMT inhibition, A549 cells were transfected with STAT1 siRNA or control siRNA for 6 hours prior to treatment with apricoxib and IL-27 (Figure 4B). IL-27 treatment induced MET in A549 cells displaying dramatically decreased expression of mesenchymal markers (N-cadherin, vimentin and Snail) and increased expression of epithelial markers (E-cadherin, β-catenin and γ-catenin) compared to untreated cells (–IL-27+control siRNA vs. +IL27+control siRNA; Figure 4B) and the STAT1 inhibition reversed the effect of IL-27 (Figure 4B, IL27+stat1siRNA; Figure 4B). Apricoxib pretreatment followed by IL-27 treatment (+IL-27+control siRNA+apricoxib; Figure 4B) led to a further reduction of mesenchymal markers expression and increase in epithelial marks expression when compared with apricoxib alone (-IL-27+control siRNA+apricoxib; Figure 4B). Snail expression was nearly undetectable with combined apricoxib (0.08-1 μM) and IL-27 treatment (+IL-27+control siRNA+apricoxib; Figure 4B). In addition, the combined apricoxib and IL-27 treatment mediated inhibition of EMT was reversed by STAT1 inhibition (+IL-27+STAT1 siRNA+apricoxib; Figure 4B). Inhibition of STAT1 showed significant dose-dependent increase in mesenchymal markers and decrease in epithelial markers. Together, these results suggest that STAT1 is required for the enhanced effect of apricoxib and IL-27 on induction of MET.
Combined apricoxib and IL-27 mediated inhibition of cell motility is dependent on STAT1
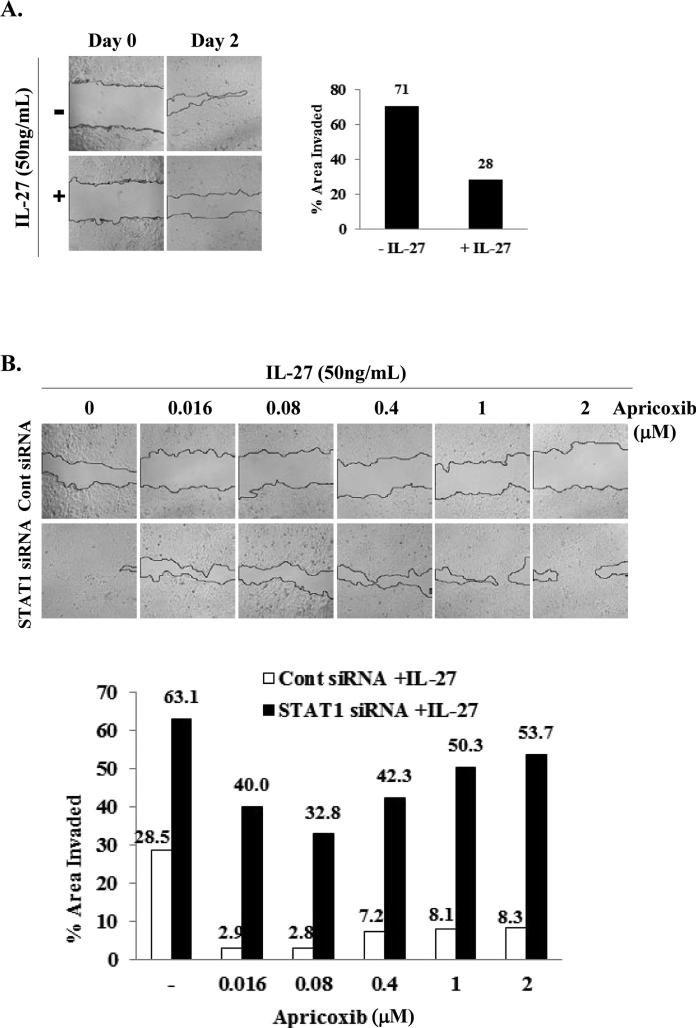
To further evaluate the functional significance of STAT1 inhibition in addition to reversal of MET, the impact of STAT1 on cell migration, a defining feature of the mesenchymal phenotype, was examined. IL-27 treatment for 2 days caused inhibition of cell motility (71% area invaded without IL-27 vs 28% area invaded with IL-27) (Figure 5A). Control siRNA treatment did not affect A549 cell motility in IL-27 treated cells (28% vs 29% of area invaded) (Figure 5B, upper panel and bottom figure). Similar to Figure 3B (lower panel, apricoxib+IL-27), the enhanced inhibitory effect on the cell migration by combined treatment of apricoxib and IL-27 was observed at 0.016 ~2 μM apricoxib (29% area invaded at 0 μM vs less than 10% area invaded at 0.016 ~2 μM apricoxib) (Figure 5B, upper panel and bottom figure). However, STAT1 inhibition reversed the enhanced inhibitory effect on cell migration resulting in increased cell motility in the combined apricoxib and IL-27 treated cells (Figure 5B, lower panel and bottom figure). These results suggest that STAT1 is required for the enhanced action of combined apricoxib and IL-27 mediated inhibition of cell migration.
Figure 5.
Effect of STAT1 inhibition on cell motility with IL-27 and apricoxib combination. (A) After treatment of A549 cells with IL-27 (50 ng/mL) at 60-70% confluence, a scratch was made in a monolayer of cells and the closure of the wound gap was observed under the microscope (50x magnification) up to 2 days. (B) The cells were treated with STAT1 or a non-targeting control siRNA (40 nM) for 6 hours and then pretreated with apricoxib (0.016-2 μM) for 4 hours followed by exposure to IL-27. Results show the cell migration at 2 days after IL-27 treatment. Images were analyzed and % area invaded was measured as described in Materials and Methods.
Discussion
STAT proteins are transcriptional factors with important roles in regulating cytokine dependent inflammation and immunity that become activated when phosphorylated by Janus Activated Kinases (JAKs) [13]. The JAK/STAT pathway is central in determining whether immune responses in the tumor microenvironment promote or inhibit tumor initiation and malignant progression. STAT1 activation has been associated with antitumor properties including suppression of tumor proliferation, induction of apoptosis, and inhibition of angiogenesis [29-33]. In contrast, aberrant activation of STAT3 has been implicated in promoting cell cycle progression, suppressing apoptosis, and conferring a malignant phenotype [13,29,30,34,35]. Thus, transcription factors STAT1 and STAT3 have opposing roles in carcinogenesis. In our recent study, IL-27 mediated inhibition of epithelial-mesenchymal transition was shown to be dependent on a STAT1 dominant pathway highlighting the importance of STAT1 in repressing lung carcinogenesis and described a new anti-tumor mechanism of IL-27 [15].
Cyclooxygenase-2 (COX-2), a key enzyme in the biosynthesis of prostaglandins, has been found to be overexpressed in lung cancer tissues and is associated with poor prognosis [36-39]. In a murine lung cancer model, Ho et al. demonstrated that IL-27 directly inhibits lung tumorigenicity through suppression of COX-2 and prostaglandin E2 (PGE2) [26]. However, A549 cells maintained in our laboratory showed minimal expression of COX-2 and endogenous PGE2, which were not appreciably inhibited by apricoxib treatment alone (data not shown). The A549 cell line was genotyped to confirm identity of the cell line.
On this basis, we hypothesized that combination treatment of IL-27 and selective COX-2 inhibition (apricoxib) may potentiate the anti-tumor properties of each agent. We previously demonstrated that IL-27 stimulation of human non-small cell lung cancer (NSCLC) cell lines resulted in STAT1 and STAT3 activation, development of an epithelial phenotype, and inhibition of cell migration [15]. The present study showed that combination treatment of apricoxib and IL-27 on lung cancer cells potentiated activation of STAT1 and suppressed IL-27-mediated STAT3 activation resulting in an enhanced effect in inhibiting epithelial-mesenchymal transition and cell migration in human lung cancer cells.
STAT3 has been shown to be constitutively activated in many human cancers and has been implicated in oncogenic transformation and progression [40-43]. Thus, suppression of STAT3 activation by combination treatment of apricoxib with IL-27 may improve anti-tumor efficacy and clinical outcome. Our study provides an insight into modulation of the JAK/STAT pathway by selective COX-2 inhibitors that can polarize a divergent pathway such as the IL-27-STAT1/STAT3 axis. IL-27 is a member of the IL-12 cytokine family [12]. This concept is supported by another report where COX-2 inhibition decreased IL-12 induced STAT3 activation in T cells, resulting in amelioration of an autoimmune disease [44].
The interplay of markers responsible for epithelial and mesenchymal phenotypes drives the plasticity of epithelial cells to undergo morphologic changes to represent those of mesenchymal cells [1,45]. Ho et al. demonstrated that A549 cells with detectable baseline expression of COX-2 showed inhibition of EMT after being treated with a COX-2 specific inhibitor [46]. In the present study, combination treatment of apricoxib and IL-27 on lung cancer cells inhibited EMT as demonstrated by increased expression of epithelial markers and decreased expression of mesenchymal markers, and inhibition of cell migration, an important property of mesenchymal differentiation and metastasis.
In other cancer models such as pancreatic and colon cancers, apricoxib or apricoxib combination therapy exhibited antitumor activities including reversal of EMT associated with inhibition of COX-2 activity [24,25]. Previous phase II clinical study combining a COX-2 inhibitor with other drugs showed promising results with prolonged survival [21]. However, the in vivo apricoxib combination therapy showed minimal effect in tumors with low expression of COX-2 [24]. In this study, we showed that the combination treatment of apricoxib with IL-27 enhanced the EMT reversal effect of apricoxib in A549 cells with minimal baseline expression of COX-2 through a STAT1 dependent mechanism. Our results suggest that apricoxib can enhance IL-27 antitumor activity in a limited COX-2 expressing cancer cell line thorough a COX-2 independent mechanism. Several studies reported COX-2 independent mechanisms of antitumor effect of COX-2 inhibitors [47-52]. In addition, A549 cells in other laboratory contained very low cox-2 protein level and activity [53]. Consistent with our findings, other selective COX-2 inhibitors showed antitumor activity by a COX-2 activity independent mechanism in lung cancer cells including A549 cells that express minimal COX-2 [52].
In summary, the present study demonstrated that IL-27 stimulation of human non-small cell lung cancer (NSCLC) cell lines results in: 1) STAT1 and STAT3 activation, 2) development of an epithelial phenotype, including a decrease in Snail protein and mesenchymal markers (N-cadherin and vimentin) and a concomitant increase in epithelial markers (E-cadherin and γ-catenin) and 3) inhibition of cell migration. Additionally, we demonstrated that: 1) the selective COX-2 inhibitor, apricoxib, in combination with IL-27 potentiates activation of STAT1 and suppresses STAT3 activation, and 2) IL-27 intensifies the apricoxib effect on EMT reversal through a STAT1 mechanism. These findings suggest that the STAT1 dependent enhanced action of combined apricoxib and IL-27 on antitumor activity may be a potential target for lung cancer prevention and therapy.
Acknowledgements
This work was supported by the National Institutes of Health/National Heart, Lung and Blood Institute [5T32HL072752]; National Cancer Institute [L30 CA142223-01, 1K23 CA131577-01A1]; Thoracic Surgery Foundation for Research and Education (TSFRE) Grant; Jonsson Cancer Center Foundation; STOP Cancer Research Award; and Ronald Binder Memorial Fund for Lung Cancer Research; NIH/National Center for Advancing Translational Science UCLA Clinical and Translational Science Institute #UL1TR000124]. We would also like to acknowledge the support of Tragara Pharmaceuticals (San Diego, CA) for providing apricoxib necessary for execution of experiments in this study.
Footnotes
Citation: Lee MH, Kachroo P, Pagano PC, Yanagawa J, Wang G, et al. (2014) Combination Treatment with Apricoxib and IL-27 Enhances Inhibition of Epithelial-Mesenchymal Transition in Human Lung Cancer Cells through a STAT1 Dominant Pathway. J Cancer Sci Ther 6: 468-477. doi:10.4172/1948-5956.1000310
References
- 1.Thiery JP, Sleeman JP. Complex networks orchestrate epithelialmesenchymal transitions. Nat Rev Mol Cell Biol. 2006;7:131–142. doi: 10.1038/nrm1835. [DOI] [PubMed] [Google Scholar]
- 2.Christiansen JJ, Rajasekaran AK. Reassessing epithelial to mesenchymal transition as a prerequisite for carcinoma invasion and metastasis. Cancer Res. 2006;66:8319–8326. doi: 10.1158/0008-5472.CAN-06-0410. [DOI] [PubMed] [Google Scholar]
- 3.Shook D, Keller R. Mechanisms, mechanics and function of epithelialmesenchymal transitions in early development. Mech Dev. 2003;120:1351–1383. doi: 10.1016/j.mod.2003.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Cocco C, Giuliani N, Di Carlo E, Ognio E, Storti P, et al. Interleukin-27 acts as multifunctional antitumor agent in multiple myeloma. Clin Cancer Res. 2010;16:4188–4197. doi: 10.1158/1078-0432.CCR-10-0173. [DOI] [PubMed] [Google Scholar]
- 5.Oniki S, Nagai H, Horikawa T, Furukawa J, Belladonna ML, et al. Interleukin-23 and interleukin-27 exert quite different antitumor and vaccine effects on poorly immunogenic melanoma. Cancer Res. 2006;66:6395–6404. doi: 10.1158/0008-5472.CAN-05-4087. [DOI] [PubMed] [Google Scholar]
- 6.Chiyo M, Shimozato O, Yu L, Kawamura K, Iizasa T, et al. Expression of IL-27 in murine carcinoma cells produces antitumor effects and induces protective immunity in inoculated host animals. Int J Cancer. 2005;115:437–442. doi: 10.1002/ijc.20848. [DOI] [PubMed] [Google Scholar]
- 7.Hisada M, Kamiya S, Fujita K, Belladonna ML, Aoki T, et al. Potent antitumor activity of interleukin-27. Cancer Res. 2004;64:1152–1156. doi: 10.1158/0008-5472.can-03-2084. [DOI] [PubMed] [Google Scholar]
- 8.Shimizu M, Shimamura M, Owaki T, Asakawa M, Fujita K, et al. Antiangiogenic and antitumor activities of IL-27. J Immunol. 2006;176:7317–7324. doi: 10.4049/jimmunol.176.12.7317. [DOI] [PubMed] [Google Scholar]
- 9.Yoshimoto T, Morishima N, Mizoguchi I, Shimizu M, Nagai H, et al. Antiproliferative activity of IL-27 on melanoma. J Immunol. 2008;180:6527–6535. doi: 10.4049/jimmunol.180.10.6527. [DOI] [PubMed] [Google Scholar]
- 10.Salcedo R, Stauffer JK, Lincoln E, Back TC, Hixon JA, et al. IL-27 mediates complete regression of orthotopic primary and metastatic murine neuroblastoma tumors: role for CD8+ T cells. J Immunol. 2004;173:7170–7182. doi: 10.4049/jimmunol.173.12.7170. [DOI] [PubMed] [Google Scholar]
- 11.Hunter CA. New IL-12-family members: IL-23 and IL-27, cytokines with divergent functions. Nat Rev Immunol. 2005;5:521–531. doi: 10.1038/nri1648. [DOI] [PubMed] [Google Scholar]
- 12.Villarino AV, Huang E, Hunter CA. Understanding the pro- and anti-inflammatory properties of IL-27. J Immunol. 2004;173:715–720. doi: 10.4049/jimmunol.173.2.715. [DOI] [PubMed] [Google Scholar]
- 13.Leonard WJ, O'Shea JJ. Jaks and STATs: biological implications. Annu Rev Immunol. 1998;16:293–322. doi: 10.1146/annurev.immunol.16.1.293. [DOI] [PubMed] [Google Scholar]
- 14.Darnell JE., Jr STATs and gene regulation. Science. 1997;277:1630–1635. doi: 10.1126/science.277.5332.1630. [DOI] [PubMed] [Google Scholar]
- 15.Kachroo P, Lee MH, Zhang L, Baratelli F, Lee G, et al. IL-27 inhibits epithelial-mesenchymal transition and angiogenic factor production in a STAT1-dominant pathway in human non-small cell lung cancer. J Exp Clin Cancer Res. 2013;32:97. doi: 10.1186/1756-9966-32-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsujii M, DuBois RN. Alterations in cellular adhesion and apoptosis in epithelial cells overexpressing prostaglandin endoperoxide synthase 2. Cell. 1995;83:493–501. doi: 10.1016/0092-8674(95)90127-2. [DOI] [PubMed] [Google Scholar]
- 17.Tsujii M, Kawano S, Tsuji S, Sawaoka H, Hori M, et al. Cyclooxygenase regulates angiogenesis induced by colon cancer cells. Cell. 1998;93:705–716. doi: 10.1016/s0092-8674(00)81433-6. [DOI] [PubMed] [Google Scholar]
- 18.Tsujii M, Kawano S, DuBois RN. Cyclooxygenase-2 expression in human colon cancer cells increases metastatic potential. Proc Natl Acad Sci U S A. 1997;94:3336–3340. doi: 10.1073/pnas.94.7.3336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.St John MA, Wang G, Luo J, Dohadwala M, Hu D, et al. Apricoxib upregulates 15-PGDH and PGT in tobacco-related epithelial malignancies. Br J Cancer. 2012;107:707–712. doi: 10.1038/bjc.2012.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rao PN, Grover RK. Apricoxib, a COX-2 inhibitor for the potential treatment of pain and cancer. IDrugs. 2009;12:711–722. [PubMed] [Google Scholar]
- 21.Lipton A, Campbell-Baird C, Witters L, Harvey H, Ali S. Phase II trial of gemcitabine, irinotecan, and celecoxib in patients with advanced pancreatic cancer. J Clin Gastroenterol. 2010;44:286–288. doi: 10.1097/MCG.0b013e3181cda097. [DOI] [PubMed] [Google Scholar]
- 22.Senzaki M, Ishida S, Yada A, Hanai M, Fujiwara K, et al. CS-706, a novel cyclooxygenase-2 selective inhibitor, prolonged the survival of tumor-bearing mice when treated alone or in combination with anti-tumor chemotherapeutic agents. Int J Cancer. 2008;122:1384–1390. doi: 10.1002/ijc.23250. [DOI] [PubMed] [Google Scholar]
- 23.Ushiyama S, Yamada T, Murakami Y, Kumakura S, Inoue S, et al. Preclinical pharmacology profile of CS-706, a novel cyclooxygenase-2 selective inhibitor, with potent antinociceptive and anti-inflammatory effects. Eur J Pharmacol. 2008;578:76–86. doi: 10.1016/j.ejphar.2007.08.034. [DOI] [PubMed] [Google Scholar]
- 24.Kirane A, Toombs JE, Ostapoff K, Carbon JG, Zaknoen S, et al. Apricoxib, a novel inhibitor of COX-2, markedly improves standard therapy response in molecularly defined models of pancreatic cancer. Clin Cancer Res. 2012;18:5031–5042. doi: 10.1158/1078-0432.CCR-12-0453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kirane A, Toombs JE, Larsen JE, Ostapoff KT, Meshaw KR, et al. Epithelial-mesenchymal transition increases tumor sensitivity to COX-2 inhibition by apricoxib. Carcinogenesis. 2012;33:1639–1646. doi: 10.1093/carcin/bgs195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ho MY, Leu SJ, Sun GH, Tao MH, Tang SJ, et al. IL-27 directly restrains lung tumorigenicity by suppressing cyclooxygenase-2-mediated activities. J Immunol. 2009;183:6217–6226. doi: 10.4049/jimmunol.0901272. [DOI] [PubMed] [Google Scholar]
- 27.Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9:671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sherry DM, Parks EE, Bullen EC, Updike DL, Howard EW. A simple method for using silicone elastomer masks for quantitative analysis of cell migration without cellular damage or substrate disruption. Cell Adh Migr. 2013;7:469–475. doi: 10.4161/cam.27294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang S, Bucana CD, Van Arsdall M, Fidler IJ. Stat1 negatively regulates angiogenesis, tumorigenicity and metastasis of tumor cells. Oncogene. 2002;21:2504–2512. doi: 10.1038/sj.onc.1205341. [DOI] [PubMed] [Google Scholar]
- 30.Stephanou A, Latchman DS. STAT-1: a novel regulator of apoptosis. Int J Exp Pathol. 2003;84:239–244. doi: 10.1111/j.0959-9673.2003.00363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hosui A, Klover P, Tatsumi T, Uemura A, Nagano H, et al. Suppression of signal transducers and activators of transcription 1 in hepatocellular carcinoma is associated with tumor progression. Int J Cancer. 2012;131:2774–2784. doi: 10.1002/ijc.27580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bromberg JF, Horvath CM, Wen Z, Schreiber RD, Darnell JE., Jr Transcriptionally active Stat1 is required for the antiproliferative effects of both interferon alpha and interferon gamma. Proc Natl Acad Sci U S A. 1996;93:7673–7678. doi: 10.1073/pnas.93.15.7673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Battle TE, Lynch RA, Frank DA. Signal transducer and activator of transcription 1 activation in endothelial cells is a negative regulator of angiogenesis. Cancer Res. 2006;66:3649–3657. doi: 10.1158/0008-5472.CAN-05-3612. [DOI] [PubMed] [Google Scholar]
- 34.Townsend PA, Scarabelli TM, Davidson SM, Knight RA, Latchman DS, et al. STAT-1 interacts with p53 to enhance DNA damage-induced apoptosis. J Biol Chem. 2004;279:5811–5820. doi: 10.1074/jbc.M302637200. [DOI] [PubMed] [Google Scholar]
- 35.Bromberg J, Darnell JE., Jr The role of STATs in transcriptional control and their impact on cellular function. Oncogene. 2000;19:2468–2473. doi: 10.1038/sj.onc.1203476. [DOI] [PubMed] [Google Scholar]
- 36.Fidler IJ. The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nat Rev Cancer. 2003;3:453–458. doi: 10.1038/nrc1098. [DOI] [PubMed] [Google Scholar]
- 37.Liotta LA, Stetler-Stevenson WG. Tumor invasion and metastasis: an imbalance of positive and negative regulation. Cancer Res. 1991;51:5054s–5059s. [PubMed] [Google Scholar]
- 38.Sun S, Schiller JH, Spinola M, Minna JD. New molecularly targeted therapies for lung cancer. J Clin Invest. 2007;117:2740–2750. doi: 10.1172/JCI31809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brown JR, DuBois RN. Cyclooxygenase as a target in lung cancer. Clin Cancer Res. 2004;10:4266s–4269s. doi: 10.1158/1078-0432.CCR-040014. [DOI] [PubMed] [Google Scholar]
- 40.Deng JY, Sun D, Liu XY, Pan Y, Liang H. STAT-3 correlates with lymph node metastasis and cell survival in gastric cancer. World J Gastroenterol. 2010;16:5380–5387. doi: 10.3748/wjg.v16.i42.5380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Niu G, Wright KL, Huang M, Song L, Haura E, et al. Constitutive Stat3 activity up-regulates VEGF expression and tumor angiogenesis. Oncogene. 2002;21:2000–2008. doi: 10.1038/sj.onc.1205260. [DOI] [PubMed] [Google Scholar]
- 42.Horiguchi A, Oya M, Shimada T, Uchida A, Marumo K, et al. Activation of signal transducer and activator of transcription 3 in renal cell carcinoma: a study of incidence and its association with pathological features and clinical outcome. J Urol. 2002;168:762–765. [PubMed] [Google Scholar]
- 43.Chang KC, Wu MH, Jones D, Chen FF, Tseng YL. Activation of STAT3 in thymic epithelial tumours correlates with tumour type and clinical behaviour. J Pathol. 2006;210:224–233. doi: 10.1002/path.2041. [DOI] [PubMed] [Google Scholar]
- 44.Muthian G, Raikwar HP, Johnson C, Rajasingh J, Kalgutkar A, et al. COX-2 inhibitors modulate IL-12 signaling through JAK-STAT pathway leading to Th1 response in experimental allergic encephalomyelitis. J Clin Immunol. 2006;26:73–85. doi: 10.1007/s10875-006-8787-y. [DOI] [PubMed] [Google Scholar]
- 45.Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002;2:442–454. doi: 10.1038/nrc822. [DOI] [PubMed] [Google Scholar]
- 46.Ho MY, Liang SM, Hung SW, Liang CM. MIG-7 controls COX-2/PGE2-mediated lung cancer metastasis. Cancer Res. 2013;73:439–449. doi: 10.1158/0008-5472.CAN-12-2220. [DOI] [PubMed] [Google Scholar]
- 47.Grosch S, Tegeder I, Niederberger E, Brautigam L, Geisslinger G. COX-2 independent induction of cell cycle arrest and apoptosis in colon cancer cells by the selective COX-2 inhibitor celecoxib. FASEB J. 2001;15:2742–2744. doi: 10.1096/fj.01-0299fje. [DOI] [PubMed] [Google Scholar]
- 48.Hwang DH, Fung V, Dannenberg AJ. National Cancer Institute workshop on chemopreventive properties of nonsteroidal anti-inflammatory drugs: role of COX-dependent and -independent mechanisms. Neoplasia. 2002;4:91–97. doi: 10.1038/sj.neo.7900226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Grösch S, Maier TJ, Schiffmann S, Geisslinger G. Cyclooxygenase-2 (COX-2)-independent anticarcinogenic effects of selective COX-2 inhibitors. J Natl Cancer Inst. 2006;98:736–747. doi: 10.1093/jnci/djj206. [DOI] [PubMed] [Google Scholar]
- 50.Zhang X, Morham SG, Langenbach R, Young DA. Malignant transformation and antineoplastic actions of nonsteroidal antiinflammatory drugs (NSAIDs) on cyclooxygenase-null embryo fibroblasts. J Exp Med. 1999;190:451–459. doi: 10.1084/jem.190.4.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Denkert C, Fürstenberg A, Daniel PT, Koch I, Köbel M, et al. Induction of G0/G1 cell cycle arrest in ovarian carcinoma cells by the anti-inflammatory drug NS-398, but not by COX-2-specific RNA interference. Oncogene. 2003;22:8653–8661. doi: 10.1038/sj.onc.1206920. [DOI] [PubMed] [Google Scholar]
- 52.Ramer R, Walther U, Borchert P, Laufer S, Linnebacher M, et al. Induction but not inhibition of COX-2 confers human lung cancer cell apoptosis by celecoxib. J Lipid Res. 2013;54:3116–3129. doi: 10.1194/jlr.M042283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mitchell JA, Belvisi MG, Akarasereenont P, Robbins RA, Kwon OJ, et al. Induction of cyclo-oxygenase-2 by cytokines in human pulmonary epithelial cells: regulation by dexamethasone. Br J Pharmacol. 1994;113:1008–1014. doi: 10.1111/j.1476-5381.1994.tb17093.x. [DOI] [PMC free article] [PubMed] [Google Scholar]