Abstract
Shiftwork, regarded as a significant occupational stressor, has become increasingly prevalent across a wide range of occupations. The adverse health outcomes associated with shiftwork are well documented. Shiftwork is an integral part of law enforcement, a high-stress occupation with elevated risks of chronic disease and mortality. Sickness absence is an important source of productivity loss and may also serve as an indirect measure of workers’ morbidity. Prior studies of shiftwork and sickness absenteeism have yielded varying results and the association has not been examined specifically among police officers. The objective of this study was to compare the incidence rate of sick leave (any, ≥3 consecutive days) among day-, afternoon-, and night-shift workers in a cohort of police officers and also examine the role of lifestyle factors as potential moderators of the association. Participants (N = 464) from the Buffalo Cardio-Metabolic Occupational Police Stress (BCOPS) study examined between 2004 and 2009 were used. Daily work history records that included the shift schedule, number of hours worked, and occurrence of sick leave were available for up to 15 yrs starting in 1994 to the date of the BCOPS study examination for each officer. Poisson regression analysis for ungrouped data was used to estimate incidence rates (IRs) of sick leave by shift, and comparison of IRs across shifts were made by computing incidence rate ratios (IRRs) and their 95% confidence intervals (CIs). Sick leave occurred at a higher rate on the night shift (4.37 per 10 000 person-hours) compared with either day (1.55 per 10000 person-hours) or afternoon (1.96 per 10000 person-hours) shifts. The association between shiftwork and sickness absence depended on body mass index (BMI). For overweight individuals (BMI ≥ 25 kg/m2), the covariate-adjusted incidence rate of sick leave (≥1 day) was twice as large for night-shift officers compared with those working on the day (IRR = 2.29, 95% CI: 1.69–3.10) or afternoon (IRR= 1.74, 95% CI: 1.29–2.34) shift. The IR of three or more consecutive days of sick leave was 1.7 times larger for those working on night shift (IRR = 1.65, 95% CI: 1.17–2.31) and 1.5 times larger for those working on afternoon shift (IRR= 1.50, 95% CI: 1.08–2.08) compared with day shiftworkers. For subjects with normal BMI (<25 kg/m2), the incidence rates of sick leave did not differ significantly across shifts. In conclusion, shiftwork is independently associated with sickness absence, with officers who work the night shift having elevated incidence of sick leave. In addition, overweight officers who work the night shift may be at additional risk for sickness absence.
Keywords: BMI, police officers, shiftwork, sick leave, ungrouped poisson regression
INTRODUCTION
Shiftwork has become a major component of work life across a wide range of occupations and it is estimated that between 15% and 30% of the working population in industrialized countries is involved in shiftwork (Andrzejczak et al., 2011). Shiftwork, particularly night or rotating shift, is regarded as a significant occupational stressor and has been linked to adverse health outcomes including metabolic disorders and cardiovascular disease (CVD) (Andrzejczak et al., 2011; De Bacquer et al., 2009; Knutssen & Boggild, 2000; Koller, 1983; Violanti et al., 2009; Wang et al., 2011; Zimmerman, 2012). In addition, shiftworkers have higher morbidity than day workers (Bockerman & Laukkanen, 2010; Bourbonnais et al., 1992; Eyal et al., 1994; Foss et al., 2011; Higashi et al., 1988; Kaerlev et al., 2004; Morikawa et al., 2001; Niedhammer et al., 2008; Ohayon et al., 2002; Tüchsen et al., 2008b), although the significance and magnitude of the increased risk varies widely across studies (Alexopoulos et al., 2008; d’Errico & Costa, 2012; Kleiven et al., 1998; Merkus et al., 2012; Tüchsen et al., 2008a). Sick leave absenteeism is an important source of productivity loss (Henderson et al., 2005; van den Heuvel et al., 2010) and constitutes the largest part (60–70%) of total absence from work (Luz & Green, 1997). For example, the cost of health-related employee absenteeism in the United States is approximately $225 billion per year (Stewart et al., 2003). More importantly, sickness absence may be an important and convenient index of workers’ morbidity or general well-being (Alexopoulos et al., 2008; Kivimäki et al., 2003; Labriola, 2008; Luz & Green, 1997; Vahtera et al., 2004) but it is not a simple function of ill-health (Duijts et al., 2007; Eriksen et al., 2003).
It is commonly hypothesized that shiftwork is linked to sick leave absence via disruption of the sleep-wake cycle and other important biological rhythms (e.g., hormones such as melatonin and cortisol, alertness, performance, body temperature, and metabolism), which consequently leads to increased chronic health problems (e.g., CVD, diabetes, metabolic syndrome, cancer, stomach problems) or injury (Andrzejczak et al., 2011; Arendt, 2010; Kaerlev et al., 2004). However, whether or not shiftwork causes more sickness absence is unclear and the underlying causal pathway is uncertain. A recent meta-analysis (Merkus et al., 2012) suggests that the association between shiftwork and sick leave may be schedule and population specific and more high-quality studies that utilize detailed shiftwork exposure are necessary. Also, adverse health effects of shiftwork tend to manifest gradually over time, which necessitates the need for long-term work history measure that accurately assess both duration of shiftwork and sickness absenteeism rather than relying on self-reported data, which are generally based on shorter time frames.
Policing is a high-stress occupation that is prone to a high level of traumatic and nontraumatic stressors (Liberman et al., 2002; Zimmerman, 2012), such as killing someone while on duty, being physically attacked, seeing abused children or a fellow officer being killed, as well as organizational and administrative pressures and demands. Work absenteeism may have implications for the individual officer’s coworkers through increased workload, overtime work, long work hours, and performing tasks for which they may not be adequately trained (Bamberger & Biron, 2007; Johns, 1997), and may also entail safety implications to private citizens and the community at large. Police officers represent an understudied occupational group (Korlin et al., 2009; Zimmerman, 2012) and there have been no prior studies, to our knowledge, that quantified the influence of long-term shiftwork on sickness absence among officers. In addition, obesity, which is a national public health crisis, is more prevalent among officers compared with the general population. Although studies (Harvey et al., 2010; Neovius et al., 2009) show a positive linear association between body mass index (BMI) and the number of work days missed due to sickness, evidence is scarce on the role of BMI and other health behaviors as potential moderators of the association between shiftwork and sickness absenteeism.
This investigation, therefore, examines the association between shiftwork and sick leave, among police officers, using objective and long-term daily work history data and tests the hypothesis that officers working predominantly on night or afternoon shift had higher risk of sickness absenteeism compared with day-shift workers. In addition, we tested the role of lifestyle factors (e.g., BMI), sex, and physical and mental health conditions as potential moderators of the association of interest.
METHODS
Study Population
Participants were from the cross-sectional Buffalo Cardio-Metabolic Occupational Police Stress (BCOPS) study and included 464 police officers from the Buffalo, New York, Police Department who were examined between June 4, 2004, and October 2, 2009. Details of the BCOPS study, including recruitment, data collection, and variables assessed, are described elsewhere (Charles et al., 2011; Hartley et al., 2011). The study was approved by the Internal Review Board of the State University of New York at Buffalo, and the National Institute for Occupational Safety and Health (NIOSH) Institutional Review Board (IRB). These approvals indicate that the protocol conforms to international ethical standards (Portaluppi et al., 2010).
Measures and Study Design
Data originated from two sources: (1) demographic, physical, biological, and psychosocial characteristics from the BCOPS study examination; and (2) a daily longitudinal work history data set obtained from the Buffalo, New York, Police payroll department that spanned 15 yrs (1994 to date of examination). The work history data were used to derive the exposure (shiftwork) and two binary outcome variables representing occurrence of any sick leave or any sick leave lasting three or more consecutive days. Other measures assessed during the BCOPS study examination were considered as covariates and potential effect modifiers for modeling. Hours of physical activity were assessed using the Seven-Day Physical Activity Recall questionnaire developed in the Stanford Five-City Project (Sallis et al., 1985).
Derivation of Shiftwork and Sick Leave Variables
The work history database contained a day-by-day account of activities, including the start and end time of work, the type of activity (e.g., regular work), the type of leave (e.g., sick leave), and the number of hours worked on each activity for 430 of 464 officers. The distribution of work start times was examined and 48% of the records started at 07:00 or 08:00 h, 30% at 16:00 h, and 21% at 20:00 or 21:00 h; consistent with standard shift start times. These start times were used to classify the shift for a given day into one of the following three categories: day shift (start times between 04:00 and 11:00 h), afternoon shift (between 12:00 and 19:00 h), and night shift (between 20:00 and 03:00 h). Officers were scheduled on 10-h permanent (nonrotating) shifts. Although officers were scheduled on permanent shifts since 1994, they occasionally worked on shifts other than their permanent shift to cover for other officers who may be on sick or injury leave or vacation in their districts or other districts. To account for this, we derived a variable that represents the shift a participant spent the majority of his/her work hours (the dominant shift). The total hours worked by each participant during the time period spanning from 1994 to date of examination or date of first sick leave (whichever came first) was partitioned into hours worked on the day, afternoon, and night shifts. A dominant shift for each subject was defined as the shift that had the largest percentage of the total hours worked. For example, officer who worked 20% on day, 70% on the afternoon, and 10% on night shift is classified as an afternoon shiftworker (the dominant shift).
The occurrence of sickness was identified when the payroll record indicates that an officer is paid for regular work but is off duty due to sickness. No additional information was available concerning the type of sickness or its severity. Certification from a physician is needed when the sickness absence lasts three or more consecutive days. We chose to examine only first occurrence of any sick leave and first occurrence of sick leave lasting 3 or more days based on the premise that first occurrence is often of greater interest for etiologic studies than subsequent occurrences in the same person, because the first occurrence affects the rate of subsequent occurrences (Rothman et al., 2008).
Statistical Analysis
Of the 430 participants with work history data, 6 prevalent cases of sick leave were excluded and the remaining 424 (initially free of sick leave) were examined over the observation period for occurrence of both sick leave measures. The association of potential confounders with the exposure of interest (shiftwork) and the outcome variable (sick leave) was examined using chi-square tests and analysis of variance (ANOVA).
For computation of incidence rates, the following variables were ascertained for each subject: (a) first occurrence of sick leave (any, ≥3 consecutive days); (b) the first date each event occurred; and (c) the shift during which each event was first reported. Poisson regression analyses for ungrouped data (Loomis et al., 2005) were used to estimate the incidence rates (IRs) of sick leave for each shift. The analysis is a retrospective cohort in design where past payroll records were used to follow the shift, work hours, age, and occurrence of sick leave for each participant from 1994 to date of first sick leave or to date of examination, whichever came first. This method utilized the actual shift (rather than the dominant shift) worked by the participants and computes the incidence rates as follows: (1) the procedure tracks and accumulates person-time (time-at-risk in work hours) contributed by each study participant to each shift. A participant was eligible to contribute person-time to all three shifts until date of occurrence of the first sick leave; (2) total person-time at risk for each shift is then derived by summing up the contribution of person-time by all participants in each of the respective shifts; (3) using the shift at which the event was first reported, the total number of participants with sick leave (number of incident cases) for each shift is counted; and (4) the incidence rate for a specific shift is then computed as the number of participants with first sick leave divided by total person-time at risk for the shift and the result expressed per 10000 working hours. The incidence rate ratios (IRRs), and their 95% confidence intervals (CIs), were then computed as measures of association. The unadjusted and age- and multivariate-adjusted IRRs were estimated. The multivariate model adjusted for the following covariates: age, sex, rank, smoking, sleep quality, workload, anxiety, depression, metabolic syndrome, and child care duty after work. A covariate was selected into the multivariate model based on prior evidence from the literature and whether it was associated with either the exposure or outcome. Potential effect modifiers of the association of interest were tested by including their interaction terms in the multivariable model. Interaction terms involving sex, life style factors (BMI, alcohol consumption, smoking, sleep quality, physical activity), a measure of a chronic health condition (metabolic syndrome), a measure of mental health (Center for Epidemiologic Studies Depression Scale [CES-D] score), and workload were tested. For all tests, statistical significance was assessed at the 5% level, except for interaction terms (10%). The type I error rate for interaction tests was raised to 10% to account for reduced power of testing interaction terms. To verify the results from the primary method of data analyses (the Poisson regression analyses), an alternative (secondary) analytic approach was employed. This involved application of a survival analysis technique (Kaplan-Meier curves) to examine how time to first sick leave (in work hours) varies by dominant shift. For each participant, time to first sick leave was calculated as the total number of hours worked at the regularly scheduled time from the first date of work history record to the date of the first event or to the examination date, whichever came first. All analyses were conducted using the SAS system, version 9.2 (SAS Institute, Cary, NC).
RESULTS
Demographic and Lifestyle Characteristics
The demographic and lifestyle characteristics of the participants are presented by dominant shift (Table 1) and sick leave status (Table 2). The study population consists of 75% males and the majority was white (78%), married (75%), and had a rank of patrol officer (65%). The mean age was 42.6 yrs (range: 27–70). Participants on the day shift were significantly older with longer years of service, and had a higher percentage of former smokers (31.4%) and a higher percentage of women (35%) compared with the afternoon and night shift groups (Table 1). Night-shift workers reported significantly greater prevalence of high workload (74.1%) and higher mean depression score and were composed of fewer officers with a rank of captain or detective (11.7%). Compared with participants who did not take sick leave, those who did were younger with shorter years of service, reported poor sleep quality more frequently (55.8% versus 38.3%), and were more likely to be women (27% versus 9.5%), and the majority had a rank of patrol officer (69.6% versus 28.6%) (Table 2).
TABLE 1.
Demographic and life style characteristics of study participants by dominant shift, BCOPS study, 2004–2009.
| Day shift (n=191) |
Afternoon shift (n=122) |
Night shift (n=111) |
|||||
|---|---|---|---|---|---|---|---|
| Characteristics | n | % | n | % | n | % | p Valuea |
| Sex | |||||||
| Women | 67 | 35.1 | 17 | 13.9 | 23 | 20.7 | >0.001 |
| Men | 124 | 64.9 | 105 | 86.1 | 88 | 79.3 | |
| Race | |||||||
| White | 140 | 74.5 | 98 | 81.0 | 88 | 80.7 | 0.472 |
| Black | 45 | 23.9 | 20 | 16.5 | 20 | 18.4 | |
| Hispanic | 3 | 1.6 | 3 | 2.5 | 1 | 0.90 | |
| Education | |||||||
| ≤High school/GED | 24 | 12.6 | 10 | 8.3 | 15 | 13.6 | 0.183 |
| College <4 yrs | 109 | 57.1 | 61 | 50.4 | 64 | 58.2 | |
| College 4+ yrs | 58 | 30.4 | 50 | 41.3 | 31 | 28.2 | |
| Marital status | |||||||
| Single | 25 | 13.1 | 15 | 12.5 | 10 | 9.0 | 0.348 |
| Married | 144 | 75.4 | 91 | 75.8 | 80 | 72.1 | |
| Divorced | 22 | 11.5 | 14 | 11.7 | 21 | 18.9 | |
| Smoking status | |||||||
| Current | 31 | 16.5 | 16 | 13.2 | 21 | 18.9 | 0.025 |
| Former | 59 | 31.4 | 21 | 17.4 | 25 | 22.5 | |
| Never | 98 | 52.1 | 84 | 69.4 | 65 | 58.6 | |
| Rank | |||||||
| Patrol officer | 119 | 62.3 | 72 | 59.5 | 86 | 77.5 | 0.006 |
| Sergeant/Lieutenant | 21 | 11.0 | 22 | 18.2 | 12 | 10.8 | |
| Captain/Detective | 51 | 26.7 | 27 | 22.3 | 13 | 11.7 | |
| Work load | |||||||
| Low/medium | 67 | 36.2 | 52 | 44.1 | 28 | 25.9 | 0.017 |
| High | 118 | 63.8 | 66 | 55.9 | 80 | 74.1 | |
| Child care after work | 63 | 34.2 | 27 | 22.7 | 30 | 27.3 | 0.086 |
| Sleep quality (poor) | 93 | 52.8 | 60 | 52.2 | 60 | 57.1 | 0.719 |
| Metabolic syndrome | 55 | 29.3 | 33 | 27.1 | 32 | 29.1 | 0.906 |
| Age (years) | 191 | 44.6 ±8.8 | 122 | 42.0 ±7.2 | 111 | 40.0 ± 6.2 | >0.001 |
| Body mass index (kg/m2) | 190 | 29.1 ±5.1 | 122 | 29.8 ±4.8 | 111 | 29.3 ±4.1 | 0.452 |
| Hours of physical activity/week | 189 | 14.6 ± 12.1 | 121 | 16.6 ± 15.6 | 109 | 15.0 ± 12.3 | 0.427 |
| Average hours of sleep/day | 185 | 6.3 ± 1.2 | 120 | 6.1 ±1.1 | 110 | 6.1 ± 1.2 | 0.177 |
| No. of alcohol drinks/week | 191 | 6.5± 11.1 | 121 | 4.9 ±6.7 | 111 | 5.3 ± 10.3 | 0.301 |
| Years of service | 191 | 17.3 ±9.3 | 121 | 16.7 ±6.9 | 111 | 12.8 ±5.9 | >0.001 |
| CES-D score | 189 | 7.0 ±5.5 | 122 | 7.8 ± 7.3 | 110 | 9.1 ±8.5 | 0.046 |
| PTSD score | 161 | 25.7 ±7.4 | 111 | 26.3 ±8.6 | 97 | 27.5 ± 11.3 | 0.278 |
| Anxiety score | 182 | 6.5 ± 7.2 | 119 | 5.9 ±6.7 | 109 | 6.8 ± 7.4 | 0.579 |
| No. of children | 153 | 2.5 ± 1.2 | 101 | 2.5 ± 1.3 | 89 | 2.8 ± 1.5 | 0.193 |
p Values are from χ2 tests of independence or Fisher’s exact test for categorical variables and from ANOVA testing differences in means across dominant shift for continuous variables. Results for the continuous variables are means ± SD.
TABLE 2.
Demographic and life style characteristics of study participants by sick leave (any occurrence) status, BCOPS study, 2004–2009.
| No sick leave (n=42) |
Any sick leave (n=382) |
||||
|---|---|---|---|---|---|
| Characteristics | n | % | n | % | p Valuea |
| Sex | |||||
| Women | 4 | 9.5 | 103 | 27.0 | 0.013 |
| Men | 38 | 90.5 | 279 | 73.0 | |
| Race | |||||
| White | 34 | 81.0 | 292 | 77.7 | 0.169 |
| Black | 6 | 14.3 | 79 | 21.0 | |
| Hispanic | 2 | 4.7 | 5 | 1.3 | |
| Education | |||||
| ≤High school/GED | 3 | 7.1 | 46 | 12.1 | 0.626 |
| College <4 yrs | 24 | 57.1 | 210 | 55.3 | |
| College 4+ yrs | 15 | 35.7 | 124 | 32.6 | |
| Marital status | |||||
| Single | 5 | 11.9 | 45 | 11.8 | 0.949 |
| Married | 32 | 76.2 | 283 | 75.5 | |
| Divorced | 5 | 11.9 | 52 | 13.7 | |
| Smoking status | |||||
| Current | 5 | 11.9 | 63 | 16.7 | 0.113 |
| Former | 16 | 38.1 | 89 | 23.5 | |
| Never | 21 | 50.0 | 226 | 59.8 | |
| Rank | |||||
| Patrol officer | 12 | 28.6 | 265 | 69.6 | <0.001 |
| Sergeant/Lieutenant | 4 | 9.5 | 51 | 13.4 | |
| Captain/Detective | 26 | 61.9 | 65 | 17.0 | |
| Work load | |||||
| Low/medium | 10 | 25.6 | 137 | 36.8 | 0.165 |
| High | 29 | 74.4 | 235 | 63.2 | |
| Child care after work | 9 | 23.7 | 111 | 29.6 | 0.444 |
| Sleep quality (poor) | 12 | 38.3 | 201 | 55.8 | 0.009 |
| Metabolic syndrome | 18 | 42.9 | 102 | 27.0 | 0.030 |
| Age (years) | 42 | 50.5 ±10.1 | 382 | 41.8 ±7.2 | <.001 |
| Body mass index (kg/m2) | 42 | 30.6 ±6.0 | 381 | 29.3 ±4.7 | 0.079 |
| Hours of physical activity/week | 42 | 15.5 ±11.3 | 378 | 15.3 ± 13.4 | 0.906 |
| Average hours of sleep/day | 41 | 6.3 ±1.2 | 379 | 6.2 ± 1.2 | 0.709 |
| No. of alcohol drinks/week | 41 | 6.4 ± 10.3 | 376 | 5.7 ±9.7 | 0.652 |
| Years of service | 42 | 23.9 ±9.6 | 381 | 15.1 ±7.4 | <.001 |
| CES-D score | 42 | 6.4 ±4.8 | 379 | 8.0 ±7.1 | 0.175 |
| PTSD score | 26 | 25.5 ±7.1 | 343 | 26.4 ±9.1 | 0.640 |
| Anxiety score | 39 | 4.3 ±6.2 | 371 | 6.6 ± 7.2 | 0.049 |
| No. of children | 31 | 2.5 ± 1.1 | 312 | 2.6 ± 1.3 | 0.776 |
p Values are from χ2 tests of independence or Fisher’s exact test for categorical variables and from t test testing differences in means between no sick leave and any sick leave for continuous variables. Results for the continuous variables are means ± SD.
Shiftwork and Incidence of Any Sick Leave
The incidence rates (IRs) and the incidence rate ratios (IRRs) of first sick leave by shiftwork are shown in Table 3. During the observation period, 90% (n = 381) of the 424 participants had at least one sick leave occurrence, whereas 42 did not report sick leave. Of the 381 who reported sick leave, 128 were day-, 104 were afternoon-, and 149 were night-shift workers. Overall, the incidence rate of sick leave was the highest (4.4 per 10 000 person-hours) on the night shift, followed by afternoon (2.0 per 10000 person-hours) and day (1.6 per 10 000 person-hours) shifts. Age-adjusted incidence rates were 2-fold higher for officers on the night shift compared with those on the day shift (IRR=2.08, 95% CI: 1.63–2.67) or afternoon shift (IRR = 1.96, 95% CI: 1.53–2.53). Adjustment for additional covariates (age, sex, rank, smoking, sleep quality, workload, anxiety, depression, metabolic syndrome, and child care duty after work) attenuated the rate ratios slightly, yet the rates were still significantly higher for officers on the night shift compared with those on the day (IRR=2.04, 95% CI: 1.56–2.68) or afternoon (IRR = 1.69, 95% CI: 1.29–2.22) shift.
TABLE 3.
Incidence rate (IR) and incidence rate ratio (IRR) of sick leave (≥1 day) by shift and body mass index (BMI), BCOPS study, 2004–2009.
| BMI | Shift | Number at riska |
Person-hoursb | Number sickc |
Incidence rated per 10 000 person- hours (95% CIe) |
Shifts compared | Unadjusted IRR (95% CI) |
Age-adjusted IRR (95% CI) |
Multivariatef-adjusted IRR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| All subjects | Day | 341 | 816923 | 128 | 1.55 (1.30–1.85) | Night versus day | 2.82 (2.22–3.57) | 2.08 (1.63−2.67) | 2.04 (1.56−2.68) |
| Afternoon | 293 | 524 295 | 104 | 1.96 (1.27−3.03) | Afternoon versus day | 1.26 (0.97−1.64) | 1.06 (0.82−1.38) | 1.21 (0.91−1.61) | |
| Night | 290 | 339 408 | 149 | 4.37 (2.90−6.59) | Night versus Afternoon | 2.23 (1.73−2.87) | 1.96 (1.53−2.53) | 1.69 (1.29−2.22) | |
| Normal (BMI <25 kg/m2) | Day | 67 | 148 073 | 33 | 2.23 (1.62−3.17) | Night versus day | 2.23 (1.30−3.81) | 1.41 (0.81−2.48) | 1.29 (0.70−2.40) |
| Afternoon | 56 | 47808 | 14 | 2.93 (1.10−7.50) | Afternoon versus day | 1.27 (0.68−2.37) | 0.76 (0.39−1.46) | 0.76 (0.35−1.66) | |
| Night | 48 | 43 054 | 22 | 5.11 (2.11−12.1) | Night versus Afternoon | 1.75 (0.90−3.43) | 1.86 (0.95−3.64) | 1.70 (0.77−3.75) | |
| Overweight (BMI ≥25 kg/m2) | Day | 274 | 668 850 | 95 | 1.42 (1.15−1.72) | Night versus day | 3.04 (2.33−4.00) | 2.32 (1.76−3.06) | 2.29 (1.69−3.10) |
| Afternoon | 237 | 476487 | 90 | 1.89 (1.14−3.05) | Afternoon versus day | 1.33 (0.99−1.78) | 1.16 (0.87−1.56) | 1.31 (0.95−1.81) | |
| Night | 242 | 296353 | 127 | 4.29 (2.67−6.82) | Night versus Afternoon | 2.29 (1.75−3.00) | 2.00 (1.52−2.63) | 1.74 (1.29−2.34) |
The number of participants who contributed person-time (i.e., work hours) to that specific shift. Note that a participant can contribute person-hours to one or two or all three shifts but first sick leave occurs in only one of the three shifts.
The total number of hours of work at regularly scheduled time for each shift. This is the total time (in hours) at risk for first sick leave. Person-time (defined as the total number of work hours) at each of the three shifts was computed using work history data until the date of first sick leave for those with sick leave and until the date of BCOPS study examination for those with no sick leave.
The number of participants with sick leave.
Incidence rate is computed as the number of participants with first sick leave divided by total person-hours for the shift and the result expressed per 10 000 working hours.
The 95% confidence interval (CI) was computed using the Poisson regression model for ungrouped data.
Adjusted for age, sex, rank, smoking, sleep quality, workload, anxiety, depression, metabolic syndrome, and child care duty after work. Interaction p value (BMI × shift) = 0.054.
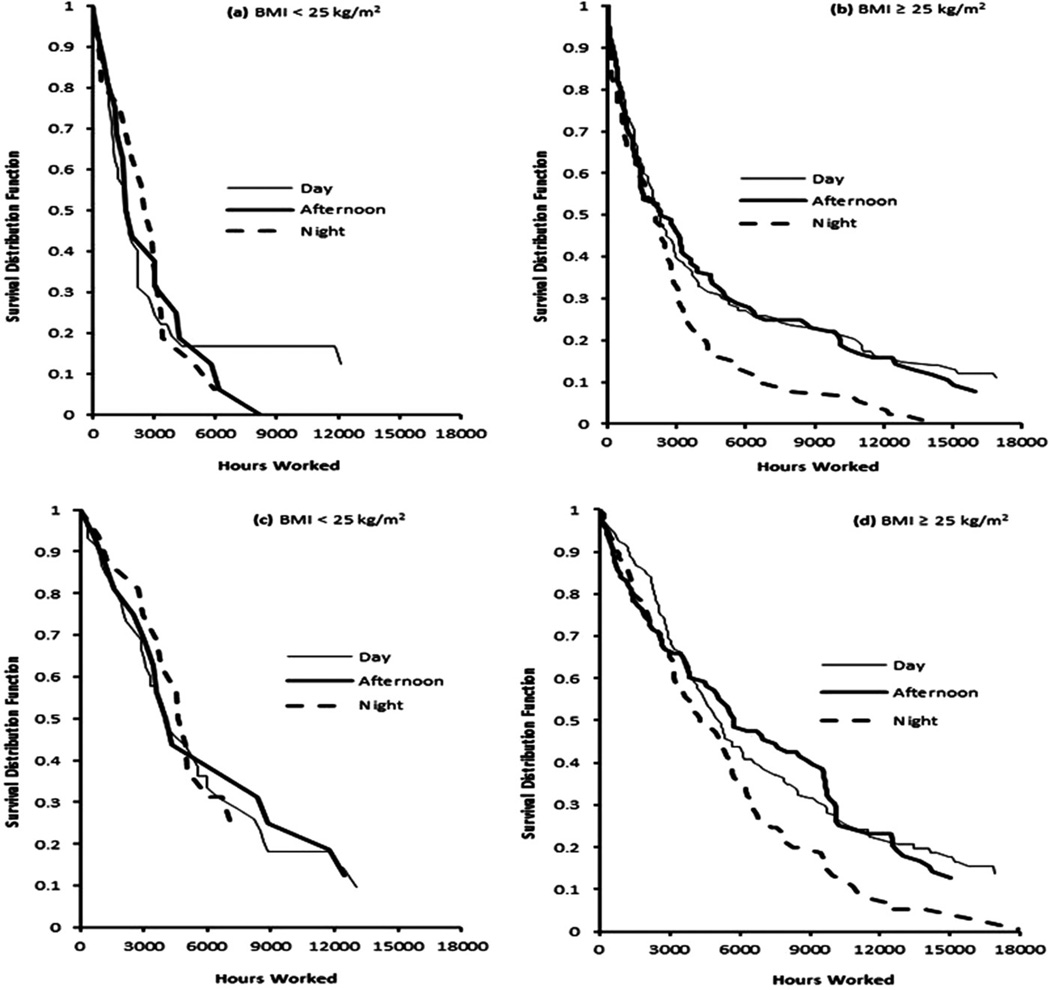
The magnitude of this association depended on the levels of BMI (interaction p value = 0.054; Table 3). For individuals with normal BMI (<25 kg/m2), differences in IRs across shifts were not significant. However, for overweight subjects, the covariate-adjusted incidence rate of sick leave for night-shift workers was twice as large as for day-shift workers (IRR=2.29, 95% CI: 1.69– 3.10) and 74% larger than the rate for afternoon-shift workers (IRR = 1.74, 95% CI: 1.29–2.34). Incidence rates for day and afternoon shifts, however, did not differ significantly (IRR = 1.31, 95% CI: 0.95–1.81). The Kaplan-Meier survival curves shown in Figure 1(a) and (b) compare the probability of working (surviving) past a time T without taking sick leave. The survival curves of sick leave for individuals with normal BMI did not differ across shifts (log-rank test for homogenity of the survival curves, p = 0.940). However, for overweight subjects, the likelihood of working without taking sick leave is the lowest for night-shift officers (log-rank test for homogenity of the survival curves, p = 0.014) and the difference in the survival probabilities between the night shift and the other two shifts appears to be more pronounced after 3000 work hours.
FIGURE 1.
Kaplan-Meier survival curves of any sick leave (a and b) and sick leave of ≥3 consecutive days (c and d) by BMI categories. The survival curves were significantly different across shifts for overweight subjects regardless of duration of sick leave (p= 0.004 for any sick leave, p= 0.006 for ≥3 consecutive days) but not for normal-weight subjects.
Shiftwork and Incidence of Sick Leave (≥3 Consecutive Days)
A sick leave of three or more consecutive days was treated as a proxy measure of physician-certified sick leave because officers are generally required to present documentation of sickness if absent for three or more consecutive days and the work history database does not contain information regarding sick leave certification. During the assessment period, 84% (n=355) of the 424 officers had at least one sick leave absence that lasted three or more consecutive days, whereas the remaining 16% (n=69) had no sick leave (n=42) or had a sick leave that lasted less than three consecutive days (n = 27). The officers with three or more consecutive days of sick leave (n=355) were compared with the referent group (n=69) with respect to demographic, physical, and psychosocial measures (data not shown). The result showed that those with three or more consecutive days of sick leave were younger (41.9 versus 46.5 yrs), had fewer years of experience (15.4 versus 18.9 yrs), were more likely to report child care after work (31.3% versus 17.2%). and consisted of a higher proportion of patrol officers (68.9% versus 47.8%) and reported higher anxiety scores (6.7 versus 4.7).
Table 4 shows the incidence rates (IRs) and the incidence rate ratios (IRRs) of first sick leave lasting three or more consecutive days by shift. Of the 355 with three or more consecutive days of sick leave, 120 occurred on day shift, 120 on afternoon shift, and the remaining 115 on night shift. The pattern of the incidence rate for ≥3 consecutive days of sick leave across shifts is similar to that of any occurrence of sick leave, but the rates were smaller in magnitude given the relatively lower prevalence of ≥3 consecutive days of sick leave. The incidence rates were highest for those working on night shift (1.73 per 10 000 person-hours), followed by afternoon (1.38 per 10 000 person-hours) and the day shift (1.07 per 10 000 person-hours). After accounting for a number of potential confounders, the incidence rate of ≥3 consecutive days of sick leave was 46% larger for night-shift officers (IRR = 1.46, 95% CI: 1.08–1.97) and 41% larger for afternoon-shift workers (IRR= 1.41, 95% CI: 1.06–1.88) compared with those on the day shift. However, the magnitude of the association between shiftwork and sick leave was dependent on BMI (interaction p value = 0.043). For officers with normal BMI, there was no significant association between shift worked and incidence of sick leave lasting ≥3 consecutive days. Among overweight officers, those who worked on the night (IRR=1.65, 95% CI: 1.17–2.31) and afternoon (IRR= 1.50,95% CI: 1.08–2.08) shifts had incidence rates that were 65% and 50% larger, respectively, compared with incidence rates of those on the day shift. The rates of certified sick leave absence for night-and afternoon-shift officers did not differ significantly (IRR=1.10, 95% CI: 0.81–1.48).
TABLE 4.
Incidence rate (IR) and incidence rate ratio (IRR) of sick leave (≥3 consecutive days) by shift and body mass index (BMI), BCOPS study, 2004−2009.
| BMI | Shift | Number at riska |
Person-hoursb | Number sickc |
Incidence rated per 10 000 person- hours (95% CIe) |
Shifts compared | Unadjusted IRR (95% CI) |
Age-adjusted IRR (95% CI) |
Multivariatef-adjusted IRR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| All subjects | Day | 360 | 1073 569 | 120 | 1.07 (0.89−1.28) | Night versus day | 1.62 (1.25−2.10) | 1.42 (1.08−1.86) | 1.46 (1.08−1.97) |
| Afternoon | 339 | 866330 | 120 | 1.38 (0.90−2.14) | Afternoon versus day | 1.29 (1.00−1.67) | 1.18 (0.91−1.54) | 1.41 (1.06−1.88) | |
| Night | 325 | 657704 | 115 | 1.73 (1.11−2.69) | Night versus Afternoon | 1.25 (0.97−1.62) | 1.19 (0.93−1.55) | 1.03 (0.79−1.36) | |
| Normal (BMI <25kg/m2) | Day | 69 | 231761 | 31 | 1.34 (0.94−1.90) | Night versus day | 1.17 (0.63−2.17) | 1.01 (0.53−1.92) | 1.00 (0.47−2.13) |
| Afternoon | 65 | 105411 | 18 | 1.80 (0.71−4.53) | Afternoon versus day | 1.35 (0.76−2.38) | 1.14 (0.62−2.10) | 1.34 (0.66−2.73) | |
| Night | 57 | 95 559 | 15 | 1.57 (0.60−4.13) | Night versus Afternoon | 0.87 (0.44−1.71) | 0.88 (0.45−1.74) | 0.75 (0.35−1.59) | |
| Overweight (BMI≥25kg/m2) | Day | 274 | 841808 | 89 | 1.00 (0.80−1.23) | Night versus day | 1.76 (1.32−2.36) | 1.56 (1.15−2.11) | 1.65 (1.17−2.31) |
| Afternoon | 291 | 760 920 | 102 | 1.33 (0.81−2.19) | Afternoon versus day | 1.33 (0.99−1.78) | 1.23 (0.92−1.66) | 1.50 (1.08−2.08) | |
| Night | 268 | 562 146 | 100 | 1.76 (1.06−2.91) | Night versus Afternoon | 1.32 (1.01−1.75) | 1.26 (0.95−1.67) | 1.10 (0.81−1.48) |
The number of participants who contributed person-time (i.e., work hours) to that specific shift. Note that a participant can contribute person-hours to one or two or all three shifts but first sick leave of three or more consecutive days occurs in only one of the three shifts.
The total number of hours of work at regularly scheduled time for each shift. This is the total time (in hours) at risk for first sick leave of three or more consecutive days. Person-time (defined as the total number of work hours) at each of the three shifts was computed using work history data until the date of first event for those with sick leave of three or more consecutive days and until the date of BCOPS study examination for those with no sick leave or sick leave lasting less than three consecutive days.
The number of participants with sick leave of at least three consecutive days.
Incidence rate is computed as the number of participants with first sick leave divided by total person-hours for the shift and the result expressed per 10 000 working hours.
The 95% confidence interval (CI) was computed using the Poisson regression model for ungrouped data.
Adjusted for age, sex, rank, smoking, sleep quality, workload, anxiety, depression, metabolic syndrome, and child care duty after work. Interaction p value (BMI × shift) = 0.043.
Figure 1(c) and (d) shows the Kaplan-Meier survival curves for three or more consecutive days of sick leave for each shift. For officers with normal BMI, the survival curves for sick leave did not differ across shifts (log-rank test for homogenity of the survival curves, p = 0.829). However, for overweight officers, the likelihood of working without taking sick leave lasting three or more consecutive days is the lowest for night-shift officers (log-rank test for homogenity of the survival curves, p = 0.006) and the difference in the survival probabilities between the night shift and the other two shifts appears to be more pronounced after 6000 work hours.
DISCUSSION
The current study utilized long-term (15 yrs) daily objective work history data to estimate the incidence rate of sick leave absenteeism among officers working on day, afternoon, and night shifts. After adjusting for a number of factors, the results show that those working on night shift were at higher risk for sickness absenteeism. In addition, the association was dependent on BMI. Among officers with normal BMI, no significant association was observed between shiftwork and sickness absence. However, among overweight officers, those on night shift were twice as likely to have a sickness absence (any) compared with those on the day shift and 74% more likely compared with afternoon shift. The incidence rates of three or more consecutive days of sickness absence (proxy measure of certified sick leave) were at least 50% larger for those on night and afternoon shifts compared with those working on the day shift.
Evidence suggests that shiftwork including irregular work hours, i.e., evening, night, and rotating shifts, disrupts the normal circadian rhythms, especially the sleep-wake cycle. The rate of sleep disorders among shiftworkers is reported to be higher compared with the general population (Ohayon et al., 2002). Although shiftwork is hypothesized to be linked with sickness absence via disruption of biological rhythms, prior studies that examined the association between shiftwork and sickness absence report inconsistent results. The findings from our study are consistent with prior studies that reported higher sickness absence among shiftworkers (Bourbonnais et al., 1992; Tüchsen et al., 2008b). Women caring for the elderly who worked on evening shift were reported to have a 29% higher risk of sickness absence compared with daytime workers (Tüchsen et al., 2008b). A similar study on nurses indicated a 96% increased risk for those on night shift and a 67% increased risk for those on evening shift relative to day workers (Bourbonnais et al., 1992). Male shiftworkers were also reported to have higher likelihood or prevalence of sickness absence compared with those on day shift (Bockerman & Laukkanen, 2010; Eyal et al., 1994; Foss et al., 2011; Higashi et al., 1988; Kaerlev et al., 2004; Morikawa et al., 2001; Niedhammer et al., 2008; Ohayon et al., 2002). Other studies were either inconclusive (Kleiven et al., 1998; Tüchsen et al., 2008a) or in disagreement (Alexopoulos et al., 2008; d’Errico & Costa, 2012) with current results.
The strength as well as significance of the association between shiftwork and sickness absenteeism could depend on a number of parameters, including the occupation being studied, specific shift schedules compared, sex, potential risk factors accounted for, moderators considered, type of illness, and the study design. Some of the variability in results across studies could be attributable to these differences. In addition, there is a wide variation in assessment of the outcome measure (sickness absence), the exposure (shiftwork), length of the observation or recall period, and the reported measure of association to allow direct comparisons across studies. For example, duration of sick leave was broadly defined as ≥1 day (Ohayon et al., 2002), ≥2 days (Bockerman & Laukkanen, 2010), ≥3 days (Duijts et al., 2007; Kleiven et al., 1998), 1–5 days (Nakata et al., 2004), 1–7 days (Morikawa et al., 2001), ≥6–8 days (Bourbonnais et al., 1992; d’Errico & Costa, 2012, Niedhammer et al., 2008), and ≥2 weeks (Lund et al., 2006; Tüchsen et al., 2008a, 2008b). With respect to shiftwork, some studies classified participants using finer categories such as day-, evening-, night-, and rotating-shift workers, whereas others utilize the general shift- (i.e., outside the regular work hours) versus day workers classification system.
The findings from the current study also indicate that the association between shiftwork and sickness absence was stronger among overweight officers. The higher risk of sickness absence among overweight shiftworkers may suggest that their work performance and health may be more adversely affected by interference with the body’s normal circadian rhythm compared with those with normal weight. Although BMI is a convenient measure of obesity, it is not the ideal measure of body fat because larger muscle mass also contributes to the body mass index. Therefore, we performed stratified analysis of the association of interest using an alternative measure, abdominal obesity (present/absent). Abdominal obesity was defined using waist circumference (≥102cm for men and ≥88cm for women). Among those with abdominal obesity, the multivariate-adjusted incidence of sick leave (≥3 consecutive days) was 2.3 times higher for those working on night shift relative to day-shift workers (IRR = 2.28, 95% CI: 1.30–3.99), but the comparison was not significant among those without abdominal obesity (IRR=1.22, 95% CI: 0.85–1.76). This is consistent with results reported by Harvey et al. (2010) and Neovius et al. (2009). In a study of workers from the London public transportation system, Harvey et al. (2010) found that obese employees take significantly more short- and long-term sickness absence than workers of a healthy weight; obese individuals typically took an extra 4 days of sick leave every year. In the United States, obese workers had 1–3 extra days of absence per person/year compared with their normal-weight counterparts (Neovius et al., 2009). Harvey et al. (2010) speculated that the higher rate of sickness absence among overweight subjects is due to greater susceptibility to nonchronic medical problems and taking longer to recover from them, and they may cope with symptoms of ill health in different ways relative to those of healthy weight, causing them to have a lower threshold for taking time off.
In our sample, we also compared the prevalence of chronic medical conditions as defined by Grundy et al. (2005) between normal-weight (n = 77) and overweight (n = 346) officers. Results showed that overweight officers had significantly higher prevalence of elevated blood pressure (45% versus 27%), glucose intolerance (29% versus 12%), low high-density lipoprotein (HDL) cholesterol (47% versus 18%), and high triglycerides (37% versus 9%) compared with their normal-weight counterparts. Given the statistical adjustment for metabolic syndrome, the increased risk of sickness absence among overweight night-shift officers was independent of these chronic medical conditions and consequently may affect coworkers who often have to carry the extra workload, which may lead to fatigue and lower quality of job performance.
The current study has several limitations and strengths. Shortcomings include the retrospective cohort study design, which limits casual inference, recruitment limited to police officers only, sickness absences that were not physician certified, and the type of sickness was not available. The unadjusted and age-adjusted analyses are methodologically valid because shift schedule, work hours, sickness absence, and age were followed concurrently. However, the other covariates (rank, smoking, sleep quality, workload, anxiety, depression, metabolic syndrome, and child care duty after work) including BMI (which was used as effect modifier) were measured at the end of the follow-up at the time of the clinic visit and their use is based on the general assumption that values for these variables remained the same during the observation period (1994 to date of examination). The survival curves of sick leave could be affected by potential misclassification of subjects by dominant shift. However, further examination of the data shows that the misclassification may be minimal. Within each dominant shift, the distribution of percent of total hours worked on that specific shift was examined: 147 of the 191 subjects with dominant day shift spent over 70% of their work hours on the day shift; 90 of the 122 subjects with dominant afternoon shift spent over 70% of their work hours on the afternoon shift; and 77 of the 111 subjects with dominant night shift spent over 70% of their time on night shift. The data suggest that dominant shift as a categorical variable captures the shift during which a participant spent the majority of his/her work hours. Sex differences may exist in physiological status and social status (e.g., social role conflict), which may not be accounted for by including gender as a covariate in the multivariate analysis. Future investigations of shiftwork and sickness absence may consider stratified analyses by sex so that the results could be inferred to the corresponding population. In the current study, the majority of the women (63%) dominantly worked on day shift, leaving small number of women on afternoon and night shifts and consequently we were not able to stratify by sex. For subjects with normal BMI, results of the analyses from the Poisson regression as well as survival analysis technique may be subject to instability (less precision) due to a small number of cases of sickness absence. Hence, comparison of survival curves across shift categories is more precise (high powered) within overweight subjects relative to comparisons within normal-weight subjects. The study has a number of strengths especially the use of objective, day-to-day work history records that spanned multiple years from which shiftwork and incidence of sick leave were ascertained. Previous studies defined shiftwork and sickness absence using data only from the past year (Bockerman & Laukkanen, 2010; Eyal et al., 1994; Higashi et al., 1988; Niedhammer et al., 2008; Ohayon et al., 2002; Tüchsen et al., 2008b) and often either shiftwork or sickness absence or both were self-reported (d’Errico & Costa, 2012; Eriksen et al., 2003; Nakata et al., 2004; Tüchsen et al., 2008a, 2008b), whereas our study utilizes more objective data derived from a much longer period of time. Although examination of medical certification may improve the reliability of sickness absence and help verify the type of sickness, medical certification data assume that the subject has sought medical care and ignore those who did not seek such care. The current study captures all reported sickness absences. The concept of any sickness absence that refers to first sick leave lasting 1 or more days in this study captures not only sickness absence with physical symptoms but also absences due to stress or fatigue (the so called “mental health” day off from work), which usually lasts for only 1 day. The Poisson regression for ungrouped data tracked person-time at risk and occurrence of sick leave for all three shift schedules during the observation period and the results were therefore not subject to misclassification by shift.
In summary, this study showed that officers on night and afternoon shifts are at greater risk of sickness absence and this was particularly evident among overweight officers. The findings are consistent with prior evidence that both obesity and shiftwork are risk factors for adverse health outcomes and their combined effect may lead to greater risk of sickness absence. This study adds to the body of knowledge regarding the association of long-term shiftwork with sickness absenteeism among high-stress occupations and may have future implications that ultimately lead to interventions that could improve shiftworkers’ health and also alleviate the economic burden associated with sick leave absenteeism (Merkus et al., 2012). For example, obese workers cost 27.4% higher in health care costs (Goetzel et al., 2012). A recent study (Zimmerman, 2012) indicates that workplace programs to promote the health and fitness of police officers can be an effective means for reducing cardiovascular risk but are commonly lacking despite the fact that currently employed police personnel have a high prevalence of traditional risk factors for CVD and obesity may be more common in police officers compared with other groups. Workplace obesity prevention programs can reduce obesity, lower health care costs, lower absenteeism, and increase employee productivity (http://www.cdc.gov/leanworks/). Future studies with larger sample size and a prospective design that take into account potential confounders, mediators, and effect modifiers are worthwhile and could provide better insight into the likely casual pathways between shiftwork and sickness absenteeism.
Acknowledgments
This work was supported by the National Institute for Occupational Safety and Health (NIOSH), contract no. 200-2003-01580. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
Footnotes
DECLARATION OF INTEREST
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Alexopoulos EC, Konstantinou EC, Bakoyannis G, et al. Risk factors for sickness absence due to low back pain and prognostic factors for return to work in a cohort of shipyard workers. Eur Spine J. 2008;17:1185–1192. doi: 10.1007/s00586-008-0711-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrzejczak D, Kapała-Kempa M, Zawilska B. Health consequences of shift work. Przegl Lek. 2011;68:383–387. [PubMed] [Google Scholar]
- Arendt J. Shift work: coping with the biological clock. Occup Med (Lond) 2010;60:10–20. doi: 10.1093/occmed/kqp162. [DOI] [PubMed] [Google Scholar]
- Bamberger P, Biron M. Social comparison and absenteeism explaining the impact of referent norms on employee excessive absenteeism. Organ Behav Hum Decis Process. 2007;103:179–196. [Google Scholar]
- Bockerman P, Laukkanen E. What makes you work while you are sick? Evidence from a survey of workers. Eur J Public Health. 2010;20:43–46. doi: 10.1093/eurpub/ckp076. [DOI] [PubMed] [Google Scholar]
- Bourbonnais R, Vinet A, Ve´zina M, Gingras S. Certified sick leave as a non-specific morbidity indicator: a case-referent study among nurses. Br J Ind Med. 1992;49:673–678. doi: 10.1136/oem.49.10.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles LE, Violanti JM, Gu JK, et al. Sleep duration and biomarkers of metabolic function among police officers. J Occup Environ Med. 2011;53:831–837. doi: 10.1097/JOM.0b013e31821f5ece. [DOI] [PubMed] [Google Scholar]
- De Bacquer D, Van Risseghem M, Clays E, et al. Rotating shift work and the metabolic syndrome: a prospective study. Int J Epidemiol. 2009;38:848–854. doi: 10.1093/ije/dyn360. [DOI] [PubMed] [Google Scholar]
- d’Errico A, Costa G. Socio-demographic and work-related risk factors for medium- and long-term sickness absence among Italian workers. Eur J Public Health. 2012;22:683–688. doi: 10.1093/eurpub/ckr140. [DOI] [PubMed] [Google Scholar]
- Duijts SF, Kant I, Swaen GM, et al. A meta-analysis of observational studies identifies predictors of sickness absence. J Clin Epidemiol. 2007;60:1105–1115. doi: 10.1016/j.jclinepi.2007.04.008. [DOI] [PubMed] [Google Scholar]
- Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of sickness absence: a three month prospective study of nurses’ aides. Occup Environ Med. 2003;60:271–278. doi: 10.1136/oem.60.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyal A, Carel RS, Goldsmith JR. Factors affecting long-term sick leave in an industrial population. Int Arch Occup Environ Health. 1994;66:279–282. doi: 10.1007/BF00454367. [DOI] [PubMed] [Google Scholar]
- Foss L, Gravseth HM, Kristensen P, et al. The impact of workplace risk factors on long-term musculoskeletal sickness absence: a registry-based 5-year follow-up from the Oslo health study. J Occup Environ Med. 2011;53:1478–1482. doi: 10.1097/JOM.0b013e3182398dec. [DOI] [PubMed] [Google Scholar]
- Goetzel RZ, Pei X, Tabrizi MJ, et al. Ten modifiable health risk factors are linked to more than one-fifth of employer-employee health care spending. Health Aff (Millwood) 2012;31:2474–2484. doi: 10.1377/hlthaff.2011.0819. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome. An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- Hartley TA, Burchfiel CM, Fekedulegn D, et al. Associations between police officer stress and the metabolic syndrome in the BCOPS study cohort. Int J Emerg Ment Health. 2011;13:243–256. [PMC free article] [PubMed] [Google Scholar]
- Harvey SB, Glozier N, Carlton O, et al. Obesity and sickness absence: results from the CHAP study. Occup Med (Lond) 2010;60:362–368. doi: 10.1093/occmed/kqq031. [DOI] [PubMed] [Google Scholar]
- Henderson M, Glozier N, Holland EK. Long term sickness absence. BMJ. 2005;330:802–803. doi: 10.1136/bmj.330.7495.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higashi T, Sakurai H, Satoh T, Toyama T. Absenteeism of shift and day workers with special reference to peptic ulcer. Asia Pac J Public Health. 1988;2:112–119. doi: 10.1177/101053958800200206. [DOI] [PubMed] [Google Scholar]
- Johns G. Contemporary research on absence from work: correlates, causes, and consequences. Int Rev Ind Organ Psychol. 1997;12:115–174. [Google Scholar]
- Kaerlev L, Jacobsen LB, Olsen J, Bonde JP. Long-term sick leave and its risk factors during pregnancy among Danish hospital employees. Scand J Public Health. 2004;32:111–117. doi: 10.1080/14034940310017517. [DOI] [PubMed] [Google Scholar]
- Kivimäki M, Head J, Ferrie JE, et al. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ. 2003;327:346–349. doi: 10.1136/bmj.327.7411.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiven M, Bøggild H, Jeppesen HJ. Shift work and sick leave. Scand J Work Environ Health. 1998;24:128–133. [PubMed] [Google Scholar]
- Knutssen A, Boggild H. Shiftwork and cardiovascular disease: review of disease mechanisms. Rev Environ Health. 2000;15:359–372. doi: 10.1515/reveh.2000.15.4.359. [DOI] [PubMed] [Google Scholar]
- Koller M. Health risks related to shift work. An example of time-contingent effects of long-term stress. Int Arch Occup Environ Health. 1983;53:59–75. doi: 10.1007/BF00406178. [DOI] [PubMed] [Google Scholar]
- Körlin J, Alexanderson K, Svedberg P. Sickness absence among women and men in the police: a systematic literature review. Scand J Public Health. 2009;37:310–319. doi: 10.1177/1403494808098508. [DOI] [PubMed] [Google Scholar]
- Labriola M. Conceptual framework of sickness absence and return to work, focusing on both the individual and the contextual level. Work. 2008;30:377–387. [PubMed] [Google Scholar]
- Liberman A, Best S, Metzler T, et al. Routine occupational stress and psychological distress in police. Policing Int J Police Strategies Manage. 2002;25:421–439. [Google Scholar]
- Loomis D, Richardson DB, Elliott L. Poisson regression analysis of ungrouped data. Occup Environ Med. 2005;62:325–39. doi: 10.1136/oem.2004.017459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund T, Labriola M, Christensen KB, et al. Physical work environment risk factors for long term sickness absence: prospective findings among a cohort of 5357 employees in Denmark. BMJ. 2006;332:449–452. doi: 10.1136/bmj.38731.622975.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luz J, Green MS. Sickness absenteeism from work—a critical review of the literature. Public Health Rev. 1997;25:89–122. [PubMed] [Google Scholar]
- Merkus SL, van Drongelen A, Holte KA, et al. The association between shift work and sick leave: a systematic review. Occup Environ Med. 2012;69:701–712. doi: 10.1136/oemed-2011-100488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morikawa Y, Miura K, Ishizaki M, et al. Sickness absence and shift work among Japanese factory workers. J Hum Ergol (Tokyo) 2001;30:393–398. [PubMed] [Google Scholar]
- Nakata A, Haratani T, Takahashi M, et al. Association of sickness absence with poor sleep and depressive symptoms in shift workers. Chronobiol Int. 2004;21:899–912. doi: 10.1081/cbi-200038104. [DOI] [PubMed] [Google Scholar]
- Neovius K, Johansson K, Kark M, Neovius M. Obesity status and sick leave: a systematic review. Obes Rev. 2009;10:17–27. doi: 10.1111/j.1467-789X.2008.00521.x. [DOI] [PubMed] [Google Scholar]
- Niedhammer I, Chastang JF, David S. Importance of psychosocial work factors on general health outcomes in the national French SUMER survey. Occup Med. 2008;58:15–24. doi: 10.1093/occmed/kqm115. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Lemoine P, Arnaud-Briant V, Dreyfus M. Prevalence and consequences of sleep disorders in a shift worker population. J Psychosom Res. 2002;53:577–583. doi: 10.1016/s0022-3999(02)00438-5. [DOI] [PubMed] [Google Scholar]
- Portaluppi F, Smolensky MH, Touitou Y. Ethics and methods for biological rhythm research on animals and human beings. Chronobiol Int. 2010;27:1911–1929. doi: 10.3109/07420528.2010.516381. [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd ed. Philadelphia: Lippincott, Williams & Wilkins; 2008. p. 758. [Google Scholar]
- Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: results from the American productivity audit. J Occup Environ Med. 2003;45:1234–1246. doi: 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]
- Tüchsen F, Christensen KB, Lund T. Shift work and sickness absence. Occup Med. 2008a;58:302–304. doi: 10.1093/occmed/kqn019. [DOI] [PubMed] [Google Scholar]
- Tüchsen F, Christensen KB, Nabe-Nielsen K, Lund T. Does evening work predict sickness absence among female carers of the elderly? Scand. J Work Environ Health. 2008b;34:483–486. doi: 10.5271/sjweh.1287. [DOI] [PubMed] [Google Scholar]
- Vahtera J, Pentti J, Kivimaki M. Sickness absence as a predictor of mortality among male and female employees. J Epidemiol Community Health. 2004;58:321–326. doi: 10.1136/jech.2003.011817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Heuvel SG, Geuskens GA, Hooftman WE, et al. Productivity loss at work; health-related and work-related factors. J Occup Rehab. 2010;20:331–339. doi: 10.1007/s10926-009-9219-7. [DOI] [PubMed] [Google Scholar]
- Violanti JM, Burchfiel CM, Hartley TA, et al. Atypical work hours and metabolic syndrome among police fficers. Arch Environ Occup Health. 2009;64:194–201. doi: 10.1080/19338240903241259. [DOI] [PubMed] [Google Scholar]
- Wang S, Armstrong E, Cairns J, et al. Shift work and chronic disease: the epidemiological evidence. Occup Med. 2011;61:78–89. doi: 10.1093/occmed/kqr001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman H. Cardiovascular disease and risk factors in law enforcement personnel: a comprehensive review. Cardiol Rev. 2012;20:159–166. doi: 10.1097/CRD.0b013e318248d631. [DOI] [PubMed] [Google Scholar]