Abstract
Background and Overview
The authors set out to identify factors associated with implementation by U.S. dentists of four practices first recommended in the Centers for Disease Control and Prevention’s Guidelines for Infection Control in Dental Health-Care Settings—2003.
Methods
In 2008, the authors surveyed a stratified random sample of 6,825 U.S. dentists. The response rate was 49 percent. The authors gathered data regarding dentists’ demographic and practice characteristics, attitudes toward infection control, sources of instruction regarding the guidelines and knowledge about the need to use sterile water for surgical procedures. Then they assessed the impact of those factors on the implementation of four recommendations: having an infection control coordinator, maintaining dental unit water quality, documenting percutaneous injuries and using safer medical devices, such as safer syringes and scalpels. The authors conducted bivariate analyses and proportional odds modeling.
Results
Responding dentists in 34 percent of practices had implemented none or one of the four recommendations, 40 percent had implemented two of the recommendations and 26 percent had implemented three or four of the recommendations. The likelihood of implementation was higher among dentists who acknowledged the importance of infection control, had practiced dentistry for less than 30 years, had received more continuing dental education credits in infection control, correctly identified more surgical procedures that require the use of sterile water, worked in larger practices and had at least three sources of instruction regarding the guidelines. Dentists with practices in the South Atlantic, Middle Atlantic or East South Central U.S. Census divisions were less likely to have complied.
Conclusions
Implementation of the four recommendations varied among U.S. dentists. Strategies targeted at raising awareness of the importance of infection control, increasing continuing education requirements and developing multiple modes of instruction may increase implementation of current and future Centers for Disease Control and Prevention guidelines.
Keywords: Dentistry, infection control, guidelines
A strategic goal of the Division of Oral Health of the Centers for Disease Control and Prevention (CDC), Atlanta, is to promote prevention of disease transmission in dental health care settings by providing evidence-based information and recommendations regarding dental infection control and by maintaining high levels of adoption of the current CDC infection control guidelines in dental practice.1 CDC published infection control recommendations for dentistry first in 19862 and again in 1993.3 These guidelines were developed partly in response to published reports regarding nine clusters of hepatitis B virus (HBV) transmission to patients from infected dental health care providers (DHCPs) during the 1970s and 1980s,4 a high prevalence of markers of past HBV infection among dentists and oral surgeons5 and transmission of HIV from an infected dentist to five patients.6 These guidelines focused on preventing transmission of blood-borne pathogens to DHCPs and patients through the use of standard precautions such as barrier precautions and the safe handling of sharp instruments.
Serologic evidence of past HBV infection among U.S. dentists decreased from prevaccine levels of 14 percent in 1972 to 9 percent in 1992.5 In 2007, there was a report of transmission of HBV from an infected patient to another in a dental surgeon’s office.7 In 2009, five cases of acute hepatitis B were diagnosed among three patients and two volunteers at a two-day portable dental clinic in West Virginia.8 During retrospective investigation, CDC investigators and West Virginia public health officials identified multiple infection control breaches that had taken place, but sparse documentation did not allow for linkage of specific breaches with transmission. There have been no documented cases of patient-to-patient transmission of HIV or hepatitis C virus in a dental setting. The declines in HBV infection and rare occurrences of blood-borne pathogen transmissions in dental settings probably reflect both increased levels of immunity due to use of the HBV vaccine and increased use of universal precautions.5,9
CDC, in collaboration with infection control experts from other federal agencies, academia, and private and professional organizations, published Guidelines for Infection Control in Dental Health-Care Settings—2003.4,10 The document updated and consolidated previous dental infection control recommendations and those from other relevant CDC guidelines, such as those regarding hand hygiene, and added new evidence-based recommendations. Among others, these included designating a person in the practice to coordinate the infection control program, maintaining dental unit water quality, complying with federal mandates to use safer medical devices (specifically, syringes and scalpels) and following recommended protocols after an exposure to blood.11–15 CDC mailed more than 200,000 copies of the 2003 guidelines to actively practicing DHCPs, dental education program directors, state boards of dental examiners and dental laboratories. Staff of the CDC’s Division of Oral Health published an overview of the background of the guidelines and all of the recommendations.10
Little information is available on private-practice dentists’ attitudes toward, knowledge of and implementation of the 2003 guidelines. The purpose of our study was to identify factors associated with implementation by U.S. dentists of four recommendations in the 2003 CDC infection control guidelines that would serve as indicators of guideline adherence. In addition, we explored strategies to improve guideline implementation.
METHODS
CDC contracted an independent research organization (RTI International, Research Triangle Park, N.C.) to develop the questionnaire, collect and analyze the data and submit final reports. RTI subcontracted data collection to the American Dental Association’s (ADA’s) Survey Center. The sample was selected from a pool of 115,437 dentists practicing in the United States who owned or co-owned a private dental practice. In January 2008, the ADA mailed the survey to a stratified random sample of 6,825 dentists. We considered owners of dental practices the most appropriate people to complete the survey because of their responsibility for oversight of a practice’s infection control program. Only one dentist per practice was chosen for the survey. ADA staff members completed two follow-up mailings and a telephone follow-up call at one, three and five weeks after the mailing of the initial survey package. ADA staff members oversampled periodontists and oral surgeons to allow for separate analyses of infection control recommendations related to these surgical specialties (data not presented here). To assess whether the responding sample was comparable with the original sample, we compared several demographic and practice characteristics of the full sample against those of the respondents. CDC’s Human Subjects Review Board approved the study protocol.
RTI developed survey questions that were based on research questions provided by CDC, information included in the guidelines and the results of a literature search regarding facilitators of and barriers to guideline implementation. CDC staff members reviewed the questions and provided comments. (The questionnaire is available as Appendix A in the supplemental data to the online version of this article at http://jada.ada.org.) Survey items asked for information about the responding dentist’s
-
▀
demographic, professional and practice characteristics;
-
▀
number of continuing dental education (CDE) credits in infection control earned since January 2004;
-
▀
attitudes about the importance of using up-to-date infection control practices;
-
▀
number of sources of instruction regarding the guidelines;
-
▀
knowledge about the need for use of sterile water during all surgical procedures;
-
▀
implementation of four new infection control recommendations.
We conducted a small pilot test among a sample of 30 dentists not participating in the survey to ensure that the questions and instructions in the survey were complete, correct and understandable to the survey’s target population. Dentists received $25 for completing the pilot test and providing comments.
We constructed an index of attitudes toward infection control to help determine the importance of infection control as perceived by self and others. The attitudes index was a composite measure of each dentist’s responses to four Likert-type questions aimed at assessing the importance to the primary practice’s reputation among patients and other dentists of following the latest infection control practices, staff members’ beliefs that the latest infection control practices have been implemented and the responding dentist’s perception of the importance of implementing the latest infection control practices. The response options were extremely important (4), very important (3), important (2) and somewhat important (1). (The individual questions used to create the attitudes index are in Appendix A [items 27, 28, 29, and 30] in the supplemental data to the online version of this article at http://jada.ada.org.) Cronbach α, on the basis of the four Likert-type questions, was 0.864. Based on Nunnally’s rule of thumb, a Cronbach α that exceeds 0.70 shows a sufficient level of reliability.16
We included a question to assess dentists’ knowledge of the four surgical procedures during which sterile water or saline should be used for irrigation: gingivectomy, extraction of an impacted third molar, soft-tissue biopsy and bone recontouring. We calculated the percentage of correct responses for this question to represent dentists’ knowledge of these procedures. To construct the outcome variable, we asked dentists about their implementation of four new infection control practices in the preceding 12 months:
-
▀
designating an infection control coordinator to monitor all infection control activities;
-
▀
using a separate water system for each dental unit that had been monitored at least once in the preceding 12 months to determine dental water quality;
-
▀
routinely documenting percutaneous injuries;
-
▀
using safer medical devices, such as safer syringes and safer scalpels, as mandated by the Occupational Safety and Health Administration (OSHA).14
Regarding the second of these recommendations, although monitoring of water quality is recommended, CDC has not made a specific recommendation regarding the frequency of monitoring. However, CDC does recommend consulting with the manufacturer of the dental unit or water delivery system to determine the best method of maintaining acceptable water quality (that is, < 500 colony-forming units per milliliter) and the recommended frequency of monitoring. We arbitrarily chose 12 months as the longest period, assuming that if dentists had not monitored water quality in the past 12 months, they likely did not do so at all.
Regarding the fourth of these recommendations, safer medical devices, as defined by OSHA,17 include “sharps with engineered sharps injury protections,” defined as a nonneedle sharp or a needle device—used for withdrawing body fluids, accessing a vein or artery or administering medications or other fluids—with a built-in safety feature or mechanism that effectively reduces the risk of an exposure incident. We also asked dentists about the use of needle-recapping devices in their practices. OSHA does not consider these to be safer medical devices; however, OSHA does consider their use to be a safer work practice in that they allow for one-handed needle recapping. The survey included a fifth infection control recommendation regarding the presence of chronic skin rashes or respiratory symptoms suggestive of latex allergy. We did not include the responses to it in our analyses because so few dentists reported any symptoms. We created a summary score ranging from 0 to 4 to represent the number of recommendations implemented. We used this score as an indicator of dentists’ guideline implementation behavior, with the summary score of 4 showing the highest level of implementation.
We have weighted estimates in this report to represent the entire population, as of January 2008, of 115,437 practicing U.S. dentists who owned or co-owned their practices. (For information on the weighting procedure, see Appendix B in the supplemental data to the online version of this article at http://jada.ada.org).
We conducted bivariate analyses to assess whether each of the 14 potential factors was associated with each of the four recommendations and the score for total number of recommendations implemented (from 0 to 4). Because of the number of bivariate tests conducted, we considered significant only the results of statistical tests (t test, χ2) with a P value less than .0001. We used a conservative P value to protect against the risk of finding apparent associations that were due to chance alone. Factors significantly associated with the total number of recommendations in bivariate analyses were included in the multivariate model. Because of the small number of responses in the 0 and 4 categories in this analysis, we grouped the scores for number of implemented recommendations into three levels: 0 to 1, 2, or 3 to 4. Because this measure had three ordered categories, we used a proportional odds model with a cumulative logit link. This method supported assessment of the effect of each factor in the model at three levels of guideline implementation, independent of other factors in the model. To account for large sampling fractions in some strata, defined by specialty, we assumed the sampling was without replacement. We reported the odds ratio to assess the strength of the association and corresponding confidence intervals, and we used the F test and associated P values for all factors in the final model to assess the statistical significance of associations. We assessed potential interactions. We used software to conduct data management (SAS, Version 9.2, SAS Institute, Cary, N.C.) and analyses (SUDAAN, Version 10.0.1, RTI International). We weighted all analyses to account for oversampling of periodontists and oral surgeons and for unit nonresponse. We adjusted standard errors for the clustered sampling design.
RESULTS
Characteristics of the surveyed population
Of the 6,825 dentists in the original sample, we considered 577 ineligible because they no longer practiced, were deceased or never claimed their mail. Of 6,248 eligible dentists in the final sample, 3,042 completed and sent surveys, resulting in an adjusted response rate of 48.7 percent. The full sample and respondent dentists were comparable in all characteristics except race or ethnicity and ADA membership status. In comparison with the full sample, 5.3 percent more of the respondents were white, 4.0 percent fewer were of unknown race or ethnicity and 6.9 percent fewer were ADA members (P < .0001). Responding dentists were predominantly middle-aged, male and white; the majority practiced dentistry in metropolitan areas; and more than two-thirds practiced in four of the nine U.S. Census divisions (Middle Atlantic, East North Central, South Atlantic and Pacific) (Table 1). General practitioners (80.2 percent) outnumbered all other types of dentists. The majority of dentists worked in small practices with one to four other staff members, worked 31 to 40 hours per week on average and had been in their current practice 20 years or more. Finally, more than one-half of participating dentists reported having earned at least six CDE credits in infection control since January 2004, whereas 15 percent earned none.
TABLE 1.
Characteristics of dentists and practices (n = 3,042) completing the 2008 survey regarding guidelines for infection control in dental care settings.*
| VARIABLE | NO. OF RESPONDENTS† | ESTIMATED‡ NO. OF DENTISTS |
ESTIMATED‡ PERCENTAGE OF DENTISTS |
|---|---|---|---|
| Age (Years) | |||
| Younger than 45 | 491 | 17,795 | 16.8 |
| 45–54 | 1,038 | 36,444 | 34.5 |
| 55–64 | 1,091 | 37,302 | 35.3 |
| 65 or older | 422 | 14,114 | 13.4 |
| Sex | |||
| Female | 406 | 14,761 | 14.0 |
| Male | 2,635 | 90,856 | 86.0 |
| Race or Ethnicity | |||
| White | 2,500 | 86,114 | 88.1 |
| Other | 316 | 11,627 | 11.9 |
| Practice Location | |||
| Metropolitan area | 2,582 | 88,971 | 84.2 |
| Nonmetropolitan area | 460 | 16,684 | 15.8 |
| U.S. Census Division | |||
| New England | 183 | 6,073 | 5.8 |
| Middle Atlantic | 488 | 16,772 | 15.9 |
| East North Central | 505 | 17,738 | 16.8 |
| West North Central | 236 | 8,798 | 8.3 |
| South Atlantic | 496 | 16,598 | 15.7 |
| East South Central | 102 | 3,628 | 3.4 |
| West South Central | 256 | 8,793 | 8.3 |
| Mountain | 210 | 7,598 | 7.2 |
| Pacific | 566 | 19,655 | 18.6 |
| Practice Specialty | |||
| General practice | 2,225 | 84,730 | 80.2 |
| Oral and maxillofacial surgery | 296 | 4,388 | 4.2 |
| Periodontics | 289 | 3,139 | 3.0 |
| All other specialties | 232 | 13,326 | 12.6 |
| Practice Size (Total No. of Employees) | |||
| 1–3 | 827 | 29,066 | 27.5 |
| 4–5 | 987 | 34,670 | 32.8 |
| 6–8 | 761 | 26,621 | 25.2 |
| 9 or more | 467 | 15,297 | 14.5 |
| Average No. of Hours Worked per Week | |||
| Fewer than 31 | 735 | 25,620 | 24.2 |
| 31–35 | 1,006 | 35,361 | 33.5 |
| 36–40 | 1,025 | 36,139 | 34.2 |
| 41 or more | 276 | 8,535 | 8.1 |
| No. of Years in Current Practice | |||
| Fewer than 10 | 446 | 15,819 | 15.7 |
| 10–19 | 777 | 26,649 | 26.4 |
| 20–29 | 966 | 33,663 | 33.3 |
| 30+ | 796 | 24,835 | 24.6 |
| No. of Infection Control CDE§ Credits Earned Since 2004 | |||
| 0 | 422 | 13,924 | 14.9 |
| 1–5 | 835 | 28,729 | 30.8 |
| 6–10 | 834 | 29,320 | 31.4 |
| 11 or more | 613 | 21,398 | 22.9 |
Guidelines from the Centers for Disease Control and Prevention, as documented by Kohn and colleagues.4
Respondents with missing data or for whom these items did not apply were excluded from these analyses.
Estimates have been weighted to the total population of 115,437 U.S. practicing dentists who owned or co-owned their practices.
CDE: Continuing dental education.
Attitudes index score
Dentists reported that their reputation among patients for following the latest infection control recommendations was most important when compared with the perceptions of other staff members, other dentists or themselves regarding that subject. The attitudes index scores ranged from 1 to 4 with a mean (standard error [SE]) of 3.45 (0.68), indicating that, on average, dentists viewed the importance to their practice of following the latest infection control guidelines as being between very important and extremely important.
Sources of instruction regarding the guideline recommendations
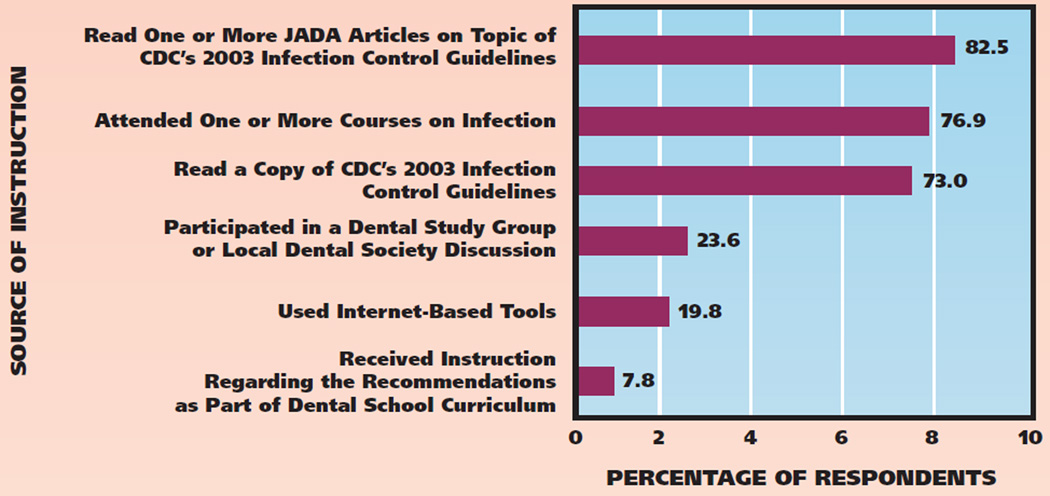
Dentists overwhelmingly received instruction on implementing the recommendations from at least one related article in The Journal of the American Dental Association (82.5 percent), from workshops and courses about the guidelines (76.9 percent) and from a copy of the 2003 CDC guidelines4 (73.0 percent) (Figure, page 1132).
Figure.
Respondents’ sources of instruction regarding the Centers for Disease Control and Prevention’s (CDC’s) 2003 guidelines for infection control in dental health care settings.4 Nonresponses to the questionnaire items pertaining to this topic were not included in the analysis. JADA: The Journal of the American Dental Association.
Knowledge of surgical procedures
Fifty-eight percent of dentists reported having used sterile water or saline with procedures performed in the past 12 months (data not shown). Overall, only 32.5 percent correctly identified the four surgical procedures for which sterile water or saline is recommended and 23.9 percent identified none correctly (Table 2, page 1133).
TABLE 2.
Number of respondents and estimated number and percentage of U.S. dentists who correctly identified surgical procedures for which use of sterile water is recommended.*
| NO. OF CORRECTLY IDENTIFIED SURGICAL PROCEDURES |
NO. OF RESPONDENTS† |
ESTIMATED NO. OF DENTISTS‡ |
ESTIMATED PERCENTAGE OF DENTISTS‡ |
|---|---|---|---|
| 0 | 641 | 22,390 | 23.9 |
| 1 | 271 | 9,415 | 10.1 |
| 2 | 485 | 16,921 | 18.1 |
| 3 | 434 | 14,429 | 15.4 |
| 4 | 938 | 30,424 | 32.5 |
According to the guidelines documented by Kohn and colleagues,4 those procedures are gingivectomy, extraction of an impacted third molar, soft-tissue biopsy and bone recontouring.
Respondents with missing data or for whom these items did not apply were excluded from these analyses.
Estimates have been weighted to the total population of 115,437 dentists practicing in the United States who owned or co-owned their own private practices.
Implementation behavior
The number of recommendations implemented varied greatly across practices (Table 3, page 1133). Almost 34 percent of practices had implemented zero or one, 39.5 percent two, and 26.6 percent three or four. The two most frequently cited recommendations implemented were designating an infection control coordinator and always documenting percutaneous injuries.
TABLE 3.
Number of respondents and estimated number and percentage of U.S. dentists who implemented four new infection control recommendations in the preceding 12 months.
| RECOMMENDATION | NO. OF RESPONDENTS* |
ESTIMATED NO. OF DENTISTS† |
ESTIMATED PERCENTAGE OF DENTISTS† |
|---|---|---|---|
| Has a Designated Practice Infection Control Coordinator | |||
| No | 592 | 20,858 | 20.4 |
| Yes | 2,351 | 81,294 | 79.6 |
| Has Separate Dental Waterline System and Periodically Monitors Water Quality | |||
| No | 1,655 | 59,050 | 66.6 |
| Yes | 838 | 29,605 | 33.4 |
| Always Documents Percutaneous Injuries | |||
| No | 387 | 14,004 | 16.6 |
| Yes | 2,083 | 70,485 | 83.4 |
| Tried or Used Safer Syringe or Safer Scalpel | |||
| No | 2,101 | 73,157 | 78.9 |
| Yes | 579 | 19,500 | 21.1 |
| Number of Recommendations Implemented (0–4) | |||
| 0 | 223 | 8,249 | 7.8 |
| 1 | 768 | 27,529 | 26.1 |
| 2 | 1,233 | 41,790 | 39.5 |
| 3 | 655 | 22,574 | 21.4 |
| 4 | 163 | 5,513 | 5.2 |
Respondents with missing data or for whom these items did not apply were excluded from these analyses.
Estimates have been weighted to the total population of 115,437 dentists practicing in the United States who owned or co-owned their own private practices.
The four recommendations
Designating an infection control coordinator
Almost 80 percent of dentists reported having a designated infection control coordinator in the practice (Table 3). Most often the coordinator was the responding dentist (44.3 percent), a chairside assistant (35.8 percent) or a dental hygienist (10.2 percent). Another dentist in the practice, a sterilization assistant, an office manager, a nurse or a receptionist composed the remaining 9.7 percent of infection control coordinators (data not shown).
Dental unit water quality and separate dental unit waterline systems
Approximately 62 percent of practices reported using separate dental unit waterline systems and 40.2 percent reported monitoring dental unit water quality at least annually. Among practices that monitored water quality, 34.4 percent did so weekly, 27.8 percent daily, 18.4 percent monthly, 14.3 percent quarterly and 5.1 percent at least annually (data not shown). About one-third (33.4 percent) of practices reported both using separate water systems and monitoring water quality at least annually (Table 3), whereas 32.8 percent neither had separate water systems nor monitored water quality (data not shown).
Referring and documenting percutaneous injuries
Six percent of dentists reported having experienced one or more percutaneous injuries in the previous 12 months and 14.4 percent reported such injuries among staff members. Overall, 50.9 percent of dentists and staff members with percutaneous injuries reportedly were referred for medical follow-up and the injuries of 73.4 percent of those were documented; fewer than one-half (48.4 percent) both were referred medically and underwent documentation of their injuries (data not shown). An estimated 83.4 percent of dentists reported always documenting percutaneous injuries experienced by themselves and staff members (Table 3).
Trying or using safer syringes and safer scalpels
Approximately 21 percent of dentists reported having used a safer syringe or scalpel in the preceding 12 months (Table 3); 16.9 percent used a safer syringe and 11.7 percent used a safer scalpel, suggesting that at least 7.6 percent had used both. About 41 percent reported having used a needle recapping device in their practice (data not shown).
Factors associated with implementing infection control recommendations
In the bivariate analysis, the attitude index and the number of correctly identified surgical procedures requiring sterile water were associated with implementation of each of the four new recommendations and with the summary score for implementation behavior (Table 4, page 1134). The number of infection control CDE credits earned since January 2004 and the number of sources of instruction on the guidelines were associated with four of the five measures. Ten factors associated with the summary score of the total number of recommendations implemented (0–4) in bivariate analyses were included in the initial proportional odds model (Table 4); of these, seven were associated independently with the outcome after accounting for the other factors (Table 5).
TABLE 4.
Factors associated with four infection control recommendations and a summary score of the total number of recommendations implemented (0–4).*
| FACTORS POTENTIALLY ASSOCIATED WITH IMPLEMENTATION AND KNOWLEDGE OF GUIDELINES† |
RESPONSE TO RECOMMENDATION | TOTAL NO. OF RECOMMENDATIONS IMPLEMENTED (0–4) |
|||
|---|---|---|---|---|---|
| Practice Has Infection Control Coordinator |
Practice Uses Separate Water System and Monitors Water Quality |
Practice Always Documents Percutaneous Injuries |
Practice Has Tried or Used New Safety Devices to Prevent Percutaneous Injuries in Past Year |
||
| Age Group | ✔‡ | ✔ | ✔ | ||
| Sex | ✔ | ||||
| Race or Ethnicity | ✔ | ✔ | |||
| Metropolitan Versus Nonmetropolitan Area | ✔ | ||||
| Geographic U.S. Census Division | ✔ | ✔ | ✔ | ||
| State-Required Infection Control CDE§ Credits | ✔ | ||||
| Years in Current Practice | ✔ | ✔ | ✔ | ||
| Practice Size | ✔ | ✔ | |||
| No. of Hours Worked per Week | ✔ | ✔ | |||
| Dental Specialty | ✔ | ✔ | |||
| No. of Infection Control CDE Credits Earned Since January 2004 | ✔ | ✔ | ✔ | ✔ | |
| Score on Attitude Index of Infection Control | ✔ | ✔ | ✔ | ✔ | ✔ |
| No. of Sources of Instruction Regarding the Guidelines | ✔ | ✔ | ✔ | ✔ | |
| Knowledge Regarding Sterile Water Use (No. of Correctly Identified Surgical Procedures) | ✔ | ✔ | ✔ | ✔ | ✔ |
Respondents with missing data or for whom these items did not apply were excluded from these analyses.
Guidelines from the Centers for Disease Control and Prevention, as documented by Kohn and colleagues.4
✔ indicates significance at P < .0001.
CDE: Continuing dental education.
TABLE 5.
Final proportional odds model of the association of dental and practice characteristics and knowledge of sterile water use with the total number of infection control recommendations implemented.
| FACTORS | DEGREES OF FREEDOM |
ODDS RATIO† | CONFIDENCE INTERVAL |
F TEST |
|---|---|---|---|---|
| Score on Attitude index of Infection Control | ||||
| Important/Somewhat important | 2 | Reference | 49.5 | |
| Very important | 1.06 | (0.83–1.37) | ||
| Extremely important | 2.05 | (1.62–2.61) | ||
| Years in Current Practice | ||||
| Fewer than 10 | 1.57 | (1.31–1.90) | ||
| 10–19 | 3 | 1.70 | (1.45–1.99) | 15.5 |
| 20–29 | 1.33 | (1.14–1.56) | ||
| 30 or more | Reference | |||
| Continuing Dental Education Credits | ||||
| 0 | Reference | |||
| 1–5 | 3 | 1.41 | (1.17–1.68) | 14.2 |
| 6–10 | 1.56 | (1.30–1.88) | ||
| More than 10 | 1.87 | (1.55–2.27) | ||
| No. of Correctly Identified Surgical Procedures Requiring the Use of Sterile Water | ||||
| 0–1 | 2 | Reference | 14.1 | |
| 2–3 | 1.08 | (0.94–1.24) | ||
| 4 | 1.46 | (1.26–1.69) | ||
| Practice Size (No. of Employees) | ||||
| 1–3 | Reference | |||
| 4–5 | 3 | 1.22 | (1.04–1.42) | 8.6 |
| 6–8 | 1.15 | (0.97–1.34) | ||
| 9 or more | 1.61 | (1.34–1.94) | ||
| Sources of Instruction Regarding the Guidelines | ||||
| 0 | Reference | |||
| 1 | 4 | 1.86 | (1.39–2.48) | 6.6 |
| 2 | 1.90 | (1.42–2.52) | ||
| 3 | 2.23 | (1.64–3.03) | ||
| 4–6 | 1.91 | (1.37–2.65) | ||
| Census Division | ||||
| New England | 1.13 | (0.86–1.50) | ||
| Middle Atlantic | 0.65 | (0.53–0.80) | ||
| East North Central | 0.96 | (0.79–1.17) | ||
| West North Central | 0.81 | (0.64–1.03) | 5.7 | |
| South Atlantic | 8 | 0.73 | (0.60–0.89) | |
| East South Central | 0.51 | (0.38–0.68) | ||
| West South Central | 0.78 | (0.60–1.00) | ||
| Mountain | 0.91 | (0.73–1.14) | ||
| Pacific | Reference | |||
Having an infection control coordinator, using separate water systems and monitoring dental unit water quality, always documenting percutaneous injuries and using a safer scalpel or syringe. The recommendation implementation scores were grouped as 0 or 1, 2 and 3 or 4.
Odds ratios and F test values in bold are statistically significant.
In the final proportional odds model, implementation of three or four recommendations was associated with a higher attitudes index score, followed by years in current practice, a higher number of CDE credits, identification of the correct number of surgical procedures requiring the use of sterile water, practice size, number of sources of instruction regarding the guidelines4 and geographic U.S. Census division (Table 5). We found no significant interactions. Implementation was more likely among dentists who perceived that following the latest infection control recommendations was extremely important, had spent less than 30 years in their current practice, had earned one or more related CDE credits, correctly identified all four procedures requiring the use of sterile water, and worked in a practice with four or five or nine or more DHCPs and other staff members. Implementation was less likely among dentists who practiced in the South Atlantic, Middle Atlantic or East South Central U.S. Census divisions (Table 5).
DISCUSSION
Implementation of infection control recommendations
The purpose of this study was to identify factors associated with dentists’ implementation of four practices first recommended in CDC’s 2003 infection control guidelines for dental health care settings.4 Our findings suggest that implementation of these recommendations was neither complete nor uniform across all practices. A higher percentage of dentists reported implementation of the recommendation for documenting all percutaneous injuries, followed by having a designated infection control coordinator, having a separate dental unit waterline system and monitoring water quality at least annually, and trying or using safer syringes or scalpels. Although 39.5 percent and 21.4 percent of practices had implemented two or three of the recommendations, respectively, only 5.2 percent had implemented all four, 26.1 percent had implemented only one and almost 8 percent had implemented none.
We found that dentists who perceived that following the latest infection control recommendations was extremely important were most likely to implement the recommendations. This finding is consistent with those of other researchers who determined that personal attitudes are associated most strongly with guideline implementation.18 The second strongest factor, years in the current practice, was associated inversely with the number of recommendations implemented; that is, the number of recommendations implemented was higher among dentists who had been in their current practice less than 30 years. Investigators in several systematic reviews found that younger health care professionals with less experience were more inclined to implement clinical practice guidelines than were older professionals with more experience.19–21 In a Canadian survey of approximately 4,000 dentists, the use of barrier protection such as gloves, masks and eye protection was highest among younger dentists.22,23 One explanation could be that younger dentists have received more extensive and varying types of instruction on dental infection control than have older practitioners.
The number of CDE credits earned since the guidelines were released was the third strongest factor. In the Canadian study, a participant’s report of having accrued more than six hours of CDEs in infection control in the preceding two years was the most important predictor of “excellent compliance” with recommended infection control procedures.22,23 The authors suggested that dentists who were more conscientious about the use of recommended infection control procedures also may have been more conscientious about attending CDE programs. At the time of our survey, the National Board of Dental Examiners estimated that less than one-third of states required CDE in infection control to maintain licensure (M. Fratamico, advocacy manager, Academy of General Dentistry, Chicago, written communication, Sept. 5, 2008). If more states mandated CDE in infection control, compliance with recommended infection control procedures might be increased further.
Implementation increased with the number of correctly identified surgical procedures for which sterile water or saline is recommended. “Oral surgical procedures involve the incision, excision, or reflection of tissue that exposes the normally sterile areas of the oral cavity … ; therefore, an increased potential exists for localized or systemic infection.”4 We are concerned that dentists, on average, correctly identified only one-half of the procedures for which CDC recommends the use of sterile irrigating solutions. Further exploration of these data is needed to determine whether factors such as dental specialty or age are associated with sterile water use and methods of sterile water delivery.
Respondents in practices with nine or more DHCPs and other staff members were more likely to have implemented the four recommendations than were those in solo or smaller practices. Sadowsky and colleagues24 found that practitioners in large dental practices and settings other than private practices, such as teaching institutions and hospitals, tended to adopt innovations more readily than did dentists in smaller practices. This association appears reasonable given that cumulative instruction on the guidelines likely increases with the number of DHCPs in the practice or setting. Approximately 60 percent of U.S. dental practices are owned and operated by a single dentist who likely hires and trains his or her own staff members.25 Targeting interventions to dentists in solo practices could increase guideline awareness, knowledge and instruction to implement infection control recommendations more fully among these dental practices.
Study results have shown that using multiple modes of instruction regarding implementation of guidelines, particularly those that involve active participation, has been more effective than using single modes.19,21 The number of dental meetings attended per year,26 enrollment in educational courses27 and attendance at CDE programs about infection control—specifically, more than six hours in the preceding two years22,23—all had a positive effect on dentists’ guideline implementation. Our findings that guideline implementation was associated with the number of modes of infection control instruction a practitioner uses (workshops, journal articles, Internet-based learning) are consistent with the results of these previous reports. Combinations of targeted interventions such as Internet-based education, interactive educational meetings and reminders (manual or automated) could be developed to promote implementation of recommended infection control practices.18 However, further research regarding the relative effectiveness of different strategies and combinations is needed.
It is not entirely clear why dentists in certain census divisions were less likely to have complied with the recommendations than were those in other divisions. In the Canadian survey, dentists in practices located in cities with a population greater than 500,000 had higher rates of compliance with a combination of infection control recommendations than did dentists in practices in more rural areas.23 Thus, the lesser compliance in the South Atlantic, Middle Atlantic or East South Central U.S. Census divisions may reflect the more rural nature of those regions. Additional analysis is needed to understand the associations between guideline implementation and geographic location more fully.
Limitations
The results of our study may be subject to the limitations common to surveys. Approximately one-half of the dentists surveyed failed to return a completed questionnaire, which may have led to nonresponse bias. Nonetheless, except for race or ethnicity and ADA membership status, the responding sample was comparable with the original sample. Our study findings also may be subject to response bias in that some dentists may have provided answers that they perceived to be socially or professionally desirable. In addition, recall bias may have occurred because dentists were surveyed retrospectively on events occurring during the preceding 12 months or, in the case of earned CDE credits, the preceding four years. Furthermore, despite our having weighted our data to accommodate nonresponse and oversampling of periodontists and oral surgeons, our findings are not representative of the entire population of U.S. dentists, because the sample was limited to dentists who owned or co-owned a private practice. Hence, dentists in community health center dental clinics, military practices and practices operating within health care organizations were not included. Finally, in using a conservative P value of less than .0001, we may have failed to identify some factors that also were associated with implementation of the recommendations.
CONCLUSIONS AND CLINICAL IMPLICATIONS
Our findings suggest that strategies aimed at raising the awareness of the importance of infection control to dentists could advance implementation of the CDC recommendations. Including more broad-based infection control education in DHCPs’ school and allied health curricula could improve consistency and implementation of CDC guidelines across dental practices. Working with state licensing boards to require CDE credits for infection control for relicensure could provide additional sources of instruction and continued dissemination of the guidelines. In addition, combining and developing multiple modes of instruction regarding the guidelines, including new technologies such as Web casts, podcasts and social networking, also may serve to encourage guideline implementation. Conducting focus groups among DHCPs could identify motivational factors and dentists’ receptiveness to innovative instructional modes and technologies for guideline instruction. Developers of future dental infection control guidelines should include all types of DHCPs as part of the workgroup developing the guidelines so that the recommendations are clearly understandable and can be implemented by all members of the dental team. Finally, when new guidelines are developed, the use of an evaluation plan can ensure that the guidelines’ effects can be measured in terms of outcomes and the costs of implementation.28
Supplementary Material
Acknowledgments
The authors thank Jon Ruesch, who when this study was conducted was the director, Survey Center, American Dental Association, Chicago, for his effort in the collection of the data for this research project.
ABBREVIATION KEY
- ADA
American Dental Association.
- CDC
Centers for Disease Control and Prevention.
- CDE
Continuing dental education.
- DHCP
Dental health care provider.
- HBV
Hepatitis B virus.
- JADA
The Journal of the American Dental Association.
- OSHA
Occupational Safety and Health Administration.
Footnotes
Disclosure. None of the authors reported any disclosures.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, Atlanta.
Contributor Information
Jennifer L. Cleveland, Email: JLCleveland@cdc.gov, Division of Oral Health, National Center for Chronic, Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, MS F-10, 4770 Buford, Highway, Atlanta, Ga. 30341.
Arthur J. Bonito, RTI International, Research Triangle Park, N.C., when this article was written.
Tammy J. Corley, Division of Oral Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta.
Misty Foster, RTI International, Research Triangle Park, N.C.
Laurie Barker, Division of Oral Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta.
G. Gordon Brown, RTI International, Research Triangle Park, N.C.
Nancy Lenfestey, RTI International, Research Triangle Park, N.C..
Linda Lux, RTI International, Research Triangle Park, N.C..
References
- 1.U.S. Department of Health and Human Services. Oral Health Program: Strategic Plan 2011–2014. Atlanta: Centers for Disease Control and Prevention, National Center for Chronic Disease and Health Promotion, Oral Health Program; 2011. [Accessed May 29, 2012]. Centers for Disease Control and Prevention, Division of Oral Health; National Center for Chronic Disease Prevention and Health Promotion. www.cdc.gov/OralHealth/stratplan/index.htm. [Google Scholar]
- 2.Centers for Disease Control (CDC) Recommended infection-control practices for dentistry. MMWR Morb Mortal Wkly Rep. 1986;35(15):237–242. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Recommended infection control practices for dentistry, 1993. MMWR Recomm Rep. 1993;41(RR-8):1–12. [PubMed] [Google Scholar]
- 4.Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM Centers for Disease Control and Prevention (CDC) Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52(RR-17):1–61. [PubMed] [Google Scholar]
- 5.Cleveland JL, Siew C, Lockwood SA, Gruninger SE, Gooch BF, Shapiro CN. Hepatitis B vaccination and infection among U.S. dentists, 1983–1992 (published correction appears in JADA 1996;127[10]: 1469–1470) JADA. 1996;127(9):1385–1390. doi: 10.14219/jada.archive.1996.0457. [DOI] [PubMed] [Google Scholar]
- 6.Ciesielski C, Marianos D, Ou CY, et al. Transmission of human immunodeficiency virus in a dental practice. Ann Intern Med. 1992;116(10):798–805. doi: 10.7326/0003-4819-116-10-798. [DOI] [PubMed] [Google Scholar]
- 7.Redd JT, Baumbach J, Kohn W, Nainan O, Khristova M, Williams I. Patient-to-patient transmission of hepatitis B virus associated with oral surgery (published online ahead of print March 21, 2007) (published correction appears in J Infect Dis 2007;195[12]: 1874) J Infect Dis. 2007;195(9):1311–1314. doi: 10.1086/513435. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Viral hepatitis outbreaks: healthcare-aassociated hepatitis B and C outbreaks reported to the Centers for Disease Control and Prevention (CDC) in 2008–2011. [Accessed Aug. 29, 2012]; www.cdc.gov/hepatitis/Outbreaks/HealthcareHepOutbreakTable.htm.
- 9.Cleveland JL, Cardo DM. Occupational exposures to human immunodeficiency virus, hepatitis B virus, and hepatitis C virus: risk, prevention, and management. Dent Clin North Am. 2003;47(4):681–696. doi: 10.1016/s0011-8532(03)00041-7. [DOI] [PubMed] [Google Scholar]
- 10.Kohn WG, Harte JA, Malvitz DM, Collins AS, Cleveland JL, Eklund KJ. Guidelines for infection control in dental health-care settings: 2003. JADA. 2004;135(1):33–47. doi: 10.14219/jada.archive.2004.0019. [DOI] [PubMed] [Google Scholar]
- 11.Shearer BG. Biofilm and the dental office (published correction appears in JADA 1996;127[4]:436) JADA. 1996;127(2):181–189. doi: 10.14219/jada.archive.1996.0166. [DOI] [PubMed] [Google Scholar]
- 12.Williams HN, Kelley J, Folineo D, Williams GC, Hawley CL, Sibiski J. Assessing microbial contamination in clean water dental units and compliance with disinfection protocol. JADA. 1994;125(9):1205–1211. doi: 10.14219/jada.archive.1994.0164. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Labor, Occupational Safety and Health Administration. OSHA instruction: enforcement procedures for the occupational exposure to bloodborne pathogens. Washington: U.S. Department of Labor, Occupational Safety and Health Administration; 2001. [Accessed May 29, 2012]. Directive No. CPL 02-02-069. www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=directives&p_id=2570. [Google Scholar]
- 14.U.S. Department of Labor, Occupational Safety and Health Administration. Occupational Exposure to Bloodborne Pathogens. Needlestick and Other Sharps Injuries; [Accessed Sept. 13, 2012]. 29 CFR Part 1910 (Docket No. H370A), RIN 1218-AB85. Final Rule. www.osha.gov/pls/oshaweb/owadisp.show_document?p_id=16265&p_table=FEDERAL_REGISTER. [Google Scholar]
- 15.Centers for Disease Control and Prevention. Updated U.S. Public Health Service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep. 2001;50(RR-11):1–52. [PubMed] [Google Scholar]
- 16.Nunnally JC. Psychometric Theory. 2nd ed. New York City: McGraw-Hill; 1978. [Google Scholar]
- 17.U.S. Department of Labor, Occupational Safety and Health Administration. Frequently Asked Questions. [Accessed May 29, 2012]; www.osha.gov/needlesticks/needlefaq.html.
- 18.Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8(6):iii–iv. 1–72. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 19.Francke AL, Smit MC, de Veer AJ, Mistiaen P. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak. 2008;8:38–49. doi: 10.1186/1472-6947-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simpson SH, Marrie TJ, Majumdar SR. Do guidelines guide pneumonia practice? A systematic review of interventions and barriers to best practice in the management of community acquired pneumonia. Respir Care Clin N Am. 2005;11(1):1–13. doi: 10.1016/j.rcc.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Davis DA, Taylor-Vaisey A. Translating guidelines into practice: a systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. 1997;157(4):408–416. [PMC free article] [PubMed] [Google Scholar]
- 22.McCarthy GM, MacDonald JK. A comparison of infection control practices of different groups of oral specialists and general dental practitioners. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(1):47–54. doi: 10.1016/s1079-2104(98)90397-3. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy GM, Koval JJ, MacDonald JK. Compliance with recommended infection control procedures among Canadian dentists: results of a national survey. Am J Infect Control. 1999;27(5):377–384. doi: 10.1016/s0196-6553(99)70001-5. [DOI] [PubMed] [Google Scholar]
- 24.Sadowsky D, Kunzel C, Frankel M. Predictors of dentists’ level of knowledge regarding the recommended prophylactic regimen for patients with rheumatic heart disease. Soc Sci Med. 1985;21(8):899–907. doi: 10.1016/0277-9536(85)90146-7. [DOI] [PubMed] [Google Scholar]
- 25.American Dental Association, Survey Center. ADA Survey of Dental Practice 2008. Chicago: American Dental Association; 2009. [Google Scholar]
- 26.Dorsey M, Overman P, Hayden WJ, Mayberry W, Requa-Clark B, Krust K. Relationships among and demographic predictors of dentists’ self-reported adherence to national guidelines. Soc Sci Med. 1991;32(11):1263–1268. doi: 10.1016/0277-9536(91)90041-a. [DOI] [PubMed] [Google Scholar]
- 27.Gordon BL, Burke FJ, Bagg J, Marlborough HS, McHugh ES. Systematic review of adherence to infection control guidelines in dentistry. J Dent. 2001;29(8):509–516. doi: 10.1016/s0300-5712(01)00043-4. [DOI] [PubMed] [Google Scholar]
- 28.Larson E. Status of practice guidelines in the United States: CDC guidelines as an example. Prev Med. 2003;36(5):519–524. doi: 10.1016/s0091-7435(03)00014-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.