Abstract
Objective
To determine if a workplace stress-reduction intervention decreases reactivity to stress among personnel exposed to a highly stressful occupational environment.
Methods
Personnel from a surgical intensive care unit (SICU) were randomized to a stress reduction intervention or a wait-list control group. The 8-week group mindfulness-based intervention (MBI) included mindfulness, gentle yoga and music. Psychological and biological markers of stress were measured one week before and one week after the intervention.
Results
Levels of salivary α-amylase, an index of sympathetic activation, were significantly decreased between the 1st and 2nd assessments in the intervention group with no changes in the control group. There was a positive correlation between salivary α-amylase levels and burnout scores.
Conclusions
These data suggest that this type of intervention could not only decrease reactivity to stress, but also decrease the risk of burnout.
INTRODUCTION
Personnel of workplaces inherently stressful, such as hospital intensive care units, are exposed to the effects of stress in their everyday environment. Stress affects the regulation of various allostatic systems with activation of the sympathetic-adrenal-medullary (SAM) pathway and the hypothalamic-pituitary-adrenal (HPA) axis. The release of the various neurotransmitters and hormones involved in these systems can change the function of the peripheral and central nervous systems leading to various symptoms with irritability, nervousness, feeling overwhelmed, having difficulty concentrating, or remembering, and changes in appetite, sleep, heart rate, and blood pressure being the most common. When stress is part of the work environment, it is often difficult to control and can lead to repeated insults that affect the individual’s health and impact his/her ability to function. Indeed, employees experiencing stress are on sick leave more often than other workers1. A stressful work environment is common for health care professionals and several studies have shown the deleterious effects of stress among this population2,3,4. Associations have been found between workplace stressors and changes in the physical and mental health of nurses5. Chronic stress at work can also lead to burnout that is characterized by a feeling of emotional exhaustion associated with emotional numbness and/or negative attitude towards self and others6.
Among health care professionals, the personnel of hospital emergency departments and intensive care units (ICU) who provide care to seriously ill or injured patients are exposed to a particularly high-stress work environment. Burnout is especially high among critical care health workers7. Burnout scores are higher for nurses working in intensive care/emergency services and operating rooms than for nurses working in outpatient clinics8. In a recent study of more than 3,000 ICU staff, 37% felt highly stressed and 29% had severe burnout9. In a 2008 study, about one-third of emergency medicine physicians reported burnout as a significant problem in their profession10 and in a more recent survey, almost 70% of emergency medicine physicians reported some burnout compared to 45% for all aggregated specialties11. Stress and burnout can lead to functional impairment in both the social and occupational environment. Emotional exhaustion among acute care personnel has been found to be related to poor patient care12 depersonalization associated with increased number of medical errors among surgeons4 and nurse burnout associated with increased levels of patient infection13. Most individuals working in high-stress conditions recognize the high level of stress associated with their work but do not necessarily identify the effects of stress on their physiology, health and behavior.
While work-related stress often cannot be eliminated, effective coping strategies may help decrease its deleterious effects. In particular, decreasing reactivity to stress may moderate its impact on behavior. Mind-body interventions are particularly well suited to decrease stress reactivity, given their ability to activate the relaxation response and turn down the stress response14. While most mind-body techniques target reduction of the physiological stress response, developing non-reactivity to internal experiences is one of the key components of mindfulness. Mindfulness allows the recognition of one’s own internal bodily reactions by increasing interoceptive awareness and, at the same time, promotes experiencing without judgment and the development of non-reactivity to internal experience. The effects of mindfulness on mental and physical health may be mediated through increased resilience to stress15. The effects of mindfulness on reactivity to stressors in a laboratory environment have been documented15. The SICU work environment represents a real-life stressor recurring on a constant basis and is difficult to amend given the nature of the work. To decrease the effects of stress among SICU personnel, this study implemented a low-dose 8-week workplace adapted mindfulness-based intervention (MBI)16,17 and analyzed the effects of the intervention on biological and psychological markers of stress.
Salivary α-amylase was used as a biological marker of stress while psychological components of stress and burnout were measured using well-established self-report questionnaires. Chronic stress and stress reactivity have been found associated with increased levels of salivary α-amylase18. Increases in salivary amylase correlate not only with experimental stressors, but also with the number and severity of critical life events, suggesting that everyday stress contributes to the regulation of salivary α-amylase levels19. This enzyme has been proposed as a marker of stress-induced activation of the autonomic nervous system19. The secretion of salivary α-amylase is controlled by sympathetic activation through β-adrenergic receptors. Epinephrine and norepinephrine increase in response to stress as part of the activation of the SAM pathway. Saliva flow rate is under the control of the parasympathetic system but does not seem to be a confounder of salivary α-amylase concentrations20,21. Sympathetic activation occurs very rapidly while cortisol elevation, which reflects activation of the HPA endocrine system, takes place more slowly. Indeed, salivary α-amylase levels peak earlier and return to normal faster than salivary levels of cortisol after an acute stressor. Salivary α-amylase thus represents a potential marker to measure effects of stress reduction interventions19. Levels of α-amylase do not display gender differences either at baseline or after acute stress response22, and, in contrast to cortisol, their circadian variations are pronounced only during the first hours following awaking. The objective of this study was to determine if providing a workplace-adapted MBI to SICU personnel decreases biological indexes of stress reactivity and psychological self-reported measures of stress.
METHODS
Participants
Participants were personnel, 18 or older, from the surgical intensive care unit (SICU) of a large academic medical center. The study was approved by the university ethical review board, and all participants provided signed informed consent. Eligibility criteria included any personnel working in the SICU and having contact with the patients or their families. Individuals practicing mindfulness, yoga, or exercising more than 30 minutes a day were excluded, as were individuals with third trimester pregnancy or a history of recent surgery if it limited ability to perform the gentle yoga movements.
Study design
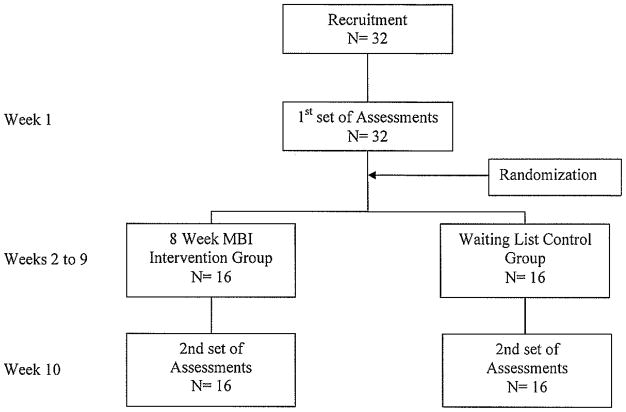
The study adhered to the CONSORT guidelines for randomized trials23. Eligible participants were randomized 1:1 using Graphpad software to intervention group or waiting list control group, with stratification by gender and type of work. Assessments were performed for all participants, intervention or controls, one week before the date of the first scheduled intervention (baseline time point) and one week after the last day of the MBI-group intervention (2-month time point) in. The collection of biological samples and self-report questionnaires were completed during a 2-hr time-frame during the early afternoon, on the same day and at the same time for all participants to control for work-related environmental changes. See Fig 1 for flow diagram of the study. The intervention was provided free of charge. Questionnaires and samples were coded. Sample size was limited by the convenience sample available within the workplace constraints.
Figure 1.
Experimental Design and Study Flow diagram.
Intervention
The 8-week group MBI combines a didactic introduction/discussion and a combination of mindfulness and yoga practices with music at each session16. The intervention was delivered by M. Klatt, a trained mindfulness and certified yoga instructor, who developed the MBI to be pragmatically performed in a work setting. The protocol combines elements of mindfulness meditation, yoga movements, and relaxation through music. All sessions last 1 hour except for week 5 session that lasts 2 hours and includes mindful eating. After introduction of the weekly theme/prompt, the participants are led through a body scan, gentle stretching, yoga, progressive relaxation, and/or an eating meditation (for the two hour session), and then into formal meditation. Each week a different topic is highlighted. The music is standardized to be the same background music in each session, and in the background of each meditation practice contained on CDs, which were provided to participants to facilitate daily practice. The intervention is 8 weeks in length, paralleling the mindfulness-based-stress-reduction (MBSR) traditional program, with shortening of the group session duration for the setting. Participants are asked to perform 20-minute daily individual practices if possible. The group stress-reduction sessions were delivered at the workplace during work hours. Work coverage was assured for the participants during the time of the group sessions and assessments.
Control condition
Participants randomly assigned to the control wait-list group received the mindfulness sessions after the 1st group had finished their 8 week intervention and after completion of the 2nd set of assessments.
Measures
Biological marker
Salivary α-amylase was measured in saliva collected with a Salivette kit (Sartstedt Inc. Newton, NC). Subjects were instructed to gently chew on the cotton swab to stimulate saliva secretion and saliva collection tubes were kept at 4°C until centrifugation at 4°C at 2000 g for 10 min. Clear saliva supernatants were kept frozen at −70 °C until assayed. Alpha-amylase was measured using a quantitative enzymatic kinetic method with the chromogenic substrate, 2-chloro-p-nitrophenol linked to maltotriose (Salivary α-amylase kit, Salimetrics, State College, PA). The enzymatic action of α-amylase on this substrate was measured in microtiter plates by absorbance at 405 nm with a spectrophotometer. Increases of absorbance of samples were transformed into amylase concentration using the linear regression calculated from the standard curve ran on each microplate. Results were expressed as units per ml of sAA. Intra-assay coefficient of variation was 3.1% and inter-assay coefficient of variation 13.3%.
Psychological Measures
Psychological stress was assessed using the Perceived Stress Scale (PSS) and the Depression Anxiety Stress Scale (DASS-21). The PSS inquires about the stress experienced during the past month on a 5-point Likert scale24. It measures the degree to which situations in the individual’s life are perceived as stressful, and its reliability has been demonstrated25. The DASS26 includes several stress-related questions, allowing the assessment of negative emotional reactivity to stressors and general tension27. It has been tested in large groups of subjects and found to have good discriminant validity28. Cronbach’s α, was 0.90 for the DASS stress scale. Burnout was assessed with the Maslach Burnout Inventory and the Professional Quality of Life (ProQOF). The Maslach’s inventory analyzes three different areas characteristic of burnout: emotional exhaustion, depersonalization and low personal accomplishment29. Cronbach’s α was 0.90 for emotional exhaustion, 0.79 for depersonalization and 0.71 for personal accomplishment29. The ProQOF has 30 items referring to the last 30 days. Subscales measure compassion satisfaction, secondary traumatization, and risk of burnout30,31. Mindfulness was assessed with the Five Facet Mindfulness Questionnaire (FFMQ), which measures observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience32,33. The scale presents good internal consistency with Cronbach’s α of 0.75 for non-reactivity, 0.83 for observing, 0.87 for acting with awareness, 0.91 for describing, and 0.87 for non-judging32. Participants were also asked to rate the level of their work stress on a Likert scale from 1 to 10.
Statistical analysis
“Intention to treat “analyses which included all subjects randomized were performed. Characteristics of the sample were analyzed using mean ± standard deviation. Two-tailed t-tests and chi-square analyses were used to compare groups at baseline. For each measurement the changes between baseline and 2-month values were assessed in each study arm using the paired t-test. For secondary analyses, the associations between psychological measures of stress and mindfulness facets were estimated using a Pearson correlation. Analyses were performed with Graphpad Instat, version 3.10, and a level of p < 0.05 was considered statistically significant.
RESULTS
More than 200 individuals working in the SICU were eligible to participate and were informed about the study through flyers and information provided at staff meetings. Thirty two individuals were interested in participating and all were eligible to participate due to minimal exclusion criteria to reflect real workplace conditions. Participants (n = 32) were randomized 1:1 to intervention (MBI) or wait-list (Control) groups. There was no drop-out and all participants completed the 2 sets of assessments. Nurses represented 69% of participants in each group. There was a limited number of males in our sample, and the stratification by gender assured equal distribution between the two groups (87.5% females for both groups) controlling for possible gender differences in the response to the intervention. The average age of the participants was 44.2 and the number of years of experience was 14.5 years with 11.8 years working in the SICU. There were no significant differences between the two groups for age (p = 0.9496, t= 0.0638), years of experience (p = 0.9485, t = 0.06512), or years working in the SICU (p = 0.8702, t = 0.1648). To control for potential changes in the levels of stress in the work environment, the study was designed with a waiting list control group and the assessments were done at the same time for all the participants.
Participants scored the stress level of their work at 7.15 ± 1.89 on a scale of 1 to 10 (with 10 being most stressful) at baseline with no significant difference between the two groups (p=0.8833, t= 0.1480). The levels of work stress did not change between the 1st and 2nd sets of assessments (p=0.2316, t=1.224 and p=0.6905, t=0.4021 for MBI and control groups respectively).
On the PSS, only 12% of participants had a score < 10 (low stress), while 37% had a score > 16 (high stress). There was no significant difference between the two groups at baseline (p = 0.0910, t = 1.746). PSS scores did not significantly change between pre-and post-intervention (114% and 115%, respectively for MBI and waiting list group, at 2-months compared to baseline (p = 0.1835, t = 1.394 for intervention group and p = 0.2732, t = 1.137 for control group). On the DASS stress subscale, 37% had score > 14, the cut-off value for stress, with no significant difference between the two groups (p = 0.1552, t = 1.458). However, in contrast to the PSS, DASS stress scores decreased 25% in the MBI group (p = 0.040, t = 2.245) compared to a non-significant 13% decline in the control group (p = 0.6675, t = 0.4339) between baseline and 2-month assessments (Fig 2). The number of participants with DASS stress scores > 14 decreased 66% in the MBI group with no change in the control group.
Figure 2. Decrease in DASS-stress scores between baseline and 2-month assessments.
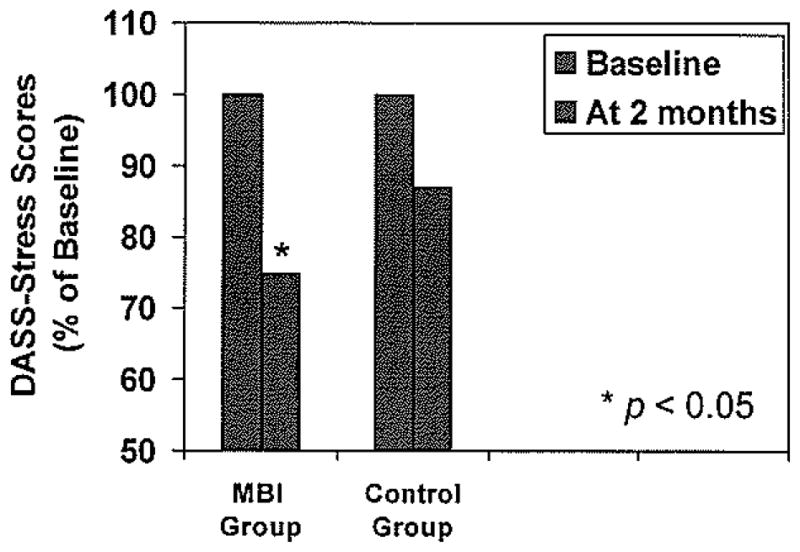
DASS stress scores were measured at the same time in the intervention (MBI) and the waiting list (Control) group, one week before (Baseline) and one week after (2 month) the 8-week intervention.
On the Maslach’s burnout inventory, the average emotional exhaustion subscale score was 23.12±10.1 with 28% of participants having scores > 26 and no difference between intervention and control groups (p = 0.3185, t = 1.0124). The scores were 7.78±5.53 for depersonalization and 36.5±7.449 for personal accomplishment with no significant difference between the groups (p = 0.685, t = 0.4909 and p = 0.3508, t = 0.9477 respectively). The scores did not significantly changes between pre- and post-intervention. However, the number of participants with scores > 26 on emotional exhaustion decreased 34% in the MBI intervention group with no change in the waiting list control group. There was also a positive correlation of DASS stress scores with the Maslach’s inventory emotional exhaustion scores (Pearson correlation coefficient r = 0.6359, p < 0.0001) and with the ProQOL burnout scores (r = 0.6753, p < 0.0001). In addition, there was a strong negative correlation between DASS stress scores and FFMQ non-reactivity scores (r = −0.49, p < 0.0001). A weaker, though still significant, negative correlation was also found with the FFMQ observing scores (r = −0.2842, p = 0.0053). The other facets of mindfulness as measured on the FFMQ (describing, acting with awareness, non-judging of inner experience) did not correlate with DASS stress scores. There were significant negative correlations between scores of the FFMQ non-reactivity and emotional exhaustion on the Maslach’s inventory and burnout on the ProQOL scale (r = −0.3105, p = 0.0125 and r = −0.4998, p < 0.0001 respectively) (Fig 3).
Figure 3. Correlations between FFMQ non-reactivity and DASS stress, Maslach emotional exhaustion and ProQOL burnout scores.
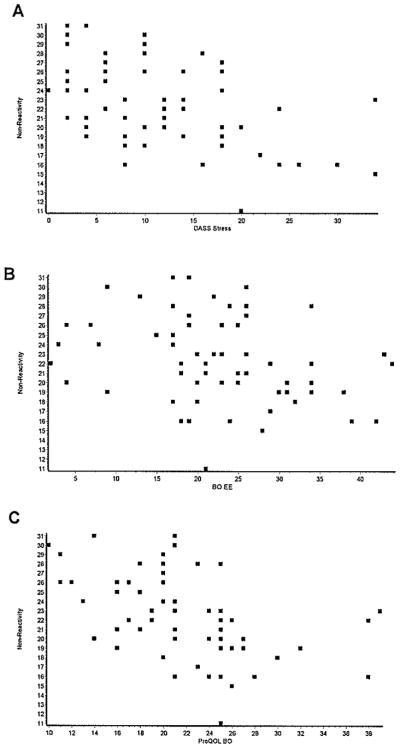
Pearson correlations were calculated between scores on the FFMQ non-reactivity subscale and the (A) DASS stress, (B) Maslach Inventory emotional exhaustion and (C) ProQOL burnout subscale scores.
Salivary α-amylase levels are low upon awakening, increase rapidly during the first hour after waking, and then plateau for the rest of the day34. To avoid the changes that occur immediately after waking, measurements were done between 1 and 3 pm. Measurements were done in the work setting during a work day to reflect the effects of the stress associated with the work environment on the levels of the enzyme. The average value for all participants was 93.6 ±15.9 units/ml (mean ± SEM) with no difference between the two groups (p = 0.6812, t = 0.4152). Levels of salivary α-amylase were reduced by 40% between baseline and 2-month time-points in the MBI group (p = 0.026, t = 2.562) compared to 4% in the control group (Fig 4). There were positive correlations between salivary α-amylase levels and both DASS stress and Maslach emotional exhaustion scores, though neither reached significance (p = 0.0586 and p = 0.0660, respectively). Salivary α-amylase was, however, significantly correlated with ProQOL burnout scores (r = 0.3490, p = 0.0058).
Figure 4. Decrease in salivary α-amylase levels between baseline and 2-month assessments.
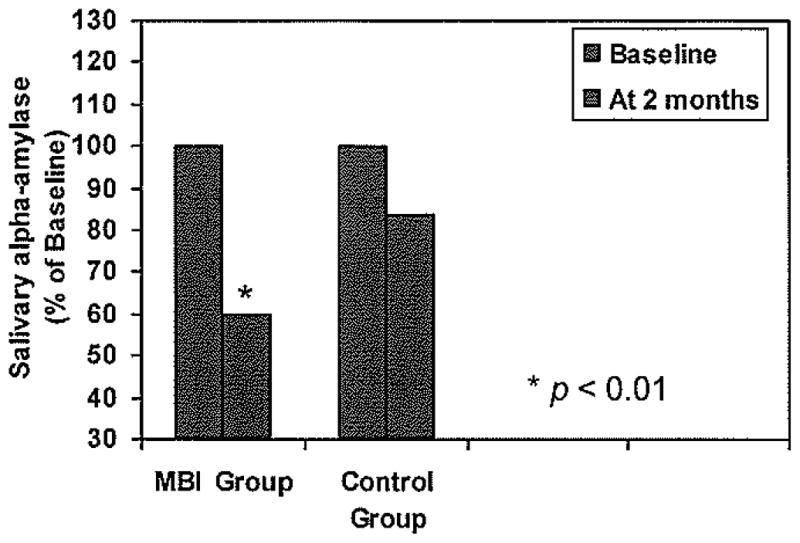
Salivary α-amylase was measured using the enzyme substrate maltotriose linked to chromogenic 2-chloro-p-nitrophenol. Levels were measured at the same time in the intervention (MBI) and the waiting list (Control) group one week before (Baseline) and one week after (2 month) the 8-week intervention.
DISCUSSION
Participants displayed levels of stress (37%) identical to those reported in a large study of 3,000 ICU personnel (37%)8. In the present study, the scores of the PSS did not change in either group. However, the scores of the DASS stress were reduced in the intervention group with no change in the control group. The two scales refer to two different time periods (past month for the PSS and past week for the DASS), which could account for the non-concordance of the scale scores. A weekly measure of PSS during an MBSR intervention for individuals with chronic stress found that PSS scores decreased only during the last week of the 8-week program35. The fact that all the assessments were performed one week after the last group session makes it less likely that the change in the DASS was due to the immediate effect of the intervention or that PSS scores were measured too early to detect an effect. The difference in the types of stress symptoms measured by the two scales may explain the discrepancy. The DASS stress scale measures emotional and physical reactions to stress. The items include: over-reacting, getting agitated, being irritable, being touchy, and unable to relax. The stress subscale of the DASS has been shown to be a reliable instrument for stress measurement and not just a measure of psychological distress28. The PSS, on the other hand, is intended to measure the degree to which situations are appraised as stressful. Several items of the PSS measure factors of stress that are related to the environment (“things outside your control,” ”difficulties piling so high that you could not overcome them,” ” could not cope with all the things you had to do”). These items may reflect inherently stressful aspects of the SICU workplace that are not likely to change between two assessments. On the PSS, only 4 out of the 10 items assess over-reactivity while others measure overload, inability to act, and loss of control. Separate analysis of the 4 items of the PSS corresponding to over-reactivity showed a decrease in scores (although non-significant, p = 0.09) and no change in the other items. These results support the idea that the discrepancy between the PSS and DASS stress scale reflects the type of items measured rather than the time period to which the scale refers to. The participants’ scores on the PSS may accurately reflect their evaluation of their work stress, which did not decrease between the two assessments. A study among overweight/obese women found that anxiety levels decreased in the intervention group but PSS scores and levels of chronic stress did not change after a mindfulness intervention36. Similarly, among students, an MBSR intervention did not change PSS scores at 2 months follow-up37.
The DASS stress data, however, suggest that the intervention reduced participants’ reactivity to stress. This conclusion is also supported by the finding that the levels of salivary α-amylase were reduced by 40% in the intervention group. Salivary amylase is a good marker of SAM pathway activation, and a sensitive marker of autonomic reactions to stress, especially sympathetic nervous system function. It is more sensitive than heart rate variability, for instance38, and it negatively correlates with changes in salivary oxytocin, which suppresses sympathetic activation39. Salivary α-amylase is usually measured in response to acute stress. Given that the assessments were done at the workplace during the work day and that participants rated the stress level of their work at above 7 on a 1 to 10 scale suggest that salivary α-amylase levels reflected activation of the sympathetic system in response to work stress.
Elicitation of the relaxation response reduces sympathetic nervous system activity40, a mechanism for decreasing reactivity to stress41. Long-term practitioners of the relaxation response, through use of various mind-body techniques, have been shown to report lower levels of stress than novices, as well as a reduction in biological markers of stress, such as norepinephrine levels during a relaxation response elicitation42. Non-reactivity is one of the skills, or facets of mindfulness, learned in MBI, and the one that changed the most rapidly during traditional MBSR35. The significant negative correlation between DASS stress and FFMQ non-reactivity scores suggests that the changes in stress symptoms and markers may be directly linked to this specific characteristic of the intervention. Other studies involving MBSR interventions have yielded results that support this finding. For example, increase in skin conductance, another measure of stress reactivity, has been found to decrease during MBSR sessions43 or after stress stimuli following MBSR44. Also, non-reactivity was shown to be inversely correlated with insula activation during stress45. Given that the insula controls emotions and autonomic functions, non-reactivity behavior may reduce the automatic emotional response and the sympathetic response to stress via inhibition of the insula activation induced by negative stimuli. While stress increases the volume of the amygdala, which is implicated in threat detection and physiological responses to stress, an 8-week MBSR intervention has been associated with reduced gray matter density of this structure46. Mindfulness has also been shown to induce a down-regulation of the left amygdala activation during emotional processing in novice practitioners47. It is reasonable to hypothesize that, although the SICU environment remained the same and the participants’ cognitive appraisal of its stressful character did not change, mindfulness training decreased the negative affect and sympathetic reactivity associated with the participants’ perception of stress in their environment. In a recent study, Arch et al (2014)48 hypothesized that a self-compassion training based on meditation decreased the sympathetic response, as reflected by lower salivary alpha amylase levels, to an acute social stressor leading to “lower defensiveness, active acceptance and greater easefulness rather than effort to exert control”.
Levels of burnout (28%) among participants in this study were very similar to those reported (29%) in the large ICU survey of Merlani et al9, suggesting that they are representative of this population. In our sample, emotional exhaustion was 23.1±10.1 and depersonalization 7.8±5.5. These findings closely match those found in a survey of 253 members of the Section of Internal Medicine of the Society of Critical Care Medicine, in which the average emotional exhaustion subscale score was 22.2±9.5 and depersonalization score was 7.1 ± 5.149. In our sample, the mean personal accomplishment score was 36.5 ± 7.5 compared to 30.9 ± 6.4 in the referred study. There was no significant difference between mean scores on any of the Maslach’s Inventory subscales between pre- and post-intervention, although the percentage of individuals with high scores for emotional exhaustion decreased in the intervention group and not in the waiting-list group. There were negative correlations between FFMQ non-reactivity scores and both Maslach’s Inventory emotional exhaustion and ProQOL burnout scores, suggesting that increasing non-reactivity may help to prevent burnout.
Effective coping occurs when strategies are used to manage stressful situations successfully. Programs to elicit the relaxation response using mind-body strategies have been developed for patients to cope with chronic stress41. A few types of interventions have been studied for work-related stress: An 8-month stress reduction intervention in an industrial plant decreased stress reactivity and salivary α-amylase50. A randomized study of a biweekly 9-month small group discussion incorporating elements of mindfulness for physicians found no change in stress but a decrease in emotional exhaustion and depersonalization in the intervention group at 9 and 12 months51. Although the activation of the sympathetic system in response to an acute situation requiring quick decision and action can be beneficial in the SICU environment, symptoms of stress reactivity, such as over-reacting, getting agitated, using a lot of nervous energy, being irritable, may impair functioning, with potential implications both for SICU personnel and the patients for whom they care. Chronic activation of the sympathetic system carries deleterious consequences on heath. Interventions intended to decrease reactivity to stress and specifically designed for high-stress workplace environments could prevent the deleterious effects of stress on the personnel’s health and behavior.
A limitation of this study is the small sample size. However, the fact that the characteristics of the sample matched previous studies for burnout suggests that the sample is representative of this population. There may have also been a bias in the participant sampling by self-selection of individuals open to the idea of a group intervention with mindfulness and yoga components. The generalization of this type of intervention may also be hindered by the specific constraints of this environment and the required support of the institution for it to be feasible.
CONCLUSION
A workplace-adapted MBI can decrease reactivity to stress among SICU personnel as shown by changes in biological indexes. The awareness of the negative effects of stress and burnout among health care professional provides an opportunity for developing evidence-based interventions that can help mitigate these effects and benefit, not only the health providers themselves, but also patients and institutions.
Acknowledgments
Funding: Funded in part by the OSU Harding Behavioral Health Stress, Trauma and Resilience program.
Footnotes
Conflict of Interest: None declared
References
- 1.McCraty R, Atkinson M, Tomasino D. Impact of a workplace stress reduction program on blood pressure and emotional health in hypertensive employees. J Altern Complem Med. 2003;9:355–369. doi: 10.1089/107555303765551589. [DOI] [PubMed] [Google Scholar]
- 2.Lambert VA, Lambert CE. Literature review of role stress/strain on nurses: an international perspective. Nurs Health Sci. 2001;3:161–172. doi: 10.1046/j.1442-2018.2001.00086.x. [DOI] [PubMed] [Google Scholar]
- 3.Lambert VA, Lambert CE, Itano J, Inouye J, Kim S, Kuniviktikul W, Sitthimongkol Y, Pongthavomkamol K, Gasemgitvattana S, Ito M. Cross-cultural comparison of workplace stressors, ways of coping and demographic characteristics as predictors of physical and mental health among hospital nurses in Japan, Thailand, South Korea and the USA (Hawaii) Int J Nurs Stud. 2004;41:671–84. doi: 10.1016/j.ijnurstu.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, Collicott P, Novotny P, Sloan J, Freischlag J. Burnout and Medical Errors Among American Surgeons. Ann Surg. 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 5.Chang EM, Daly J, Hancock KM, Bidewell JW, Johnson A, Lambert VA, Lambert CE. The relationships among workplace stressors, coping methods, demographic characteristics and health in Australian nurses. J Prof Nurs. 2006;22:30–38. doi: 10.1016/j.profnurs.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annual Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 7.Embriaco N, Papazain L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. 2007;13:482–488. doi: 10.1097/MCC.0b013e3282efd28a. [DOI] [PubMed] [Google Scholar]
- 8.Ilahn MN, Durukan E, Taner E, Maral I, Bumin MA. Burnout and its correlates among nursing staff: questionnaire survey. J Adv Nurs. 2007;61:100–106. doi: 10.1111/j.1365-2648.2007.04476.x. [DOI] [PubMed] [Google Scholar]
- 9.Merlani P, Verdon M, Businger A, Domenighetti G, Pargger H, Ricou B STRESI+ Group. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Resp Crit Care. 2011;184:1140–6. doi: 10.1164/rccm.201101-0068OC. [DOI] [PubMed] [Google Scholar]
- 10.Cydulka RK, Korte R. Career satisfaction in emergency medicine: the ABEM longitudinal study of emergency physicians. Ann Emerg Med. 2008;51:714–722. doi: 10.1016/j.annemergmed.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, West CP, Sloan J, Oreskovich MR. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–85. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 12.Rathert C, Williams ES, Lawrence ER, Halbesleben JR. Emotional exhaustion and workarounds in acute care: Cross sectional tests of a theoretical framework. Int J Nurs Stud. 2012;49:969–977. doi: 10.1016/j.ijnurstu.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40:486–90. doi: 10.1016/j.ajic.2012.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benson H, Beary JF, Carol MP. The relaxation response. Psychiatry. 1974;37:37–46. doi: 10.1080/00332747.1974.11023785. [DOI] [PubMed] [Google Scholar]
- 15.Creswell JD, Pacialio LE, Lindsay EK, Brown KW. Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology. 2014;44:1–12. doi: 10.1016/j.psyneuen.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Klatt MD, Buckworth J, Malarkey WB. Effects of Low-Dose Mindfulness-Based Stress Reduction (MBSR-Id) on Working Adults. Health Educ Behav. 2009;36:601–14. doi: 10.1177/1090198108317627. [DOI] [PubMed] [Google Scholar]
- 17.Malarkey WB, Jarjoura D, Klatt M. Workplace based mindfulness practice and inflammation: a randomized trial. Brain Behav Immun. 2013;27:145–54. doi: 10.1016/j.bbi.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Stegeren A, Rohleder N, Everaerd W, Wolf OT. Salivary alpha amylase as marker for adrenergic activity during stress: effect of beta-blockade. Psychoneuroendocrinology. 2006;31:137–41. doi: 10.1016/j.psyneuen.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 19.Nater UM, Rohleder N. Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: current state of research. Psychoneuroendocrinology. 2009;34:486–96. doi: 10.1016/j.psyneuen.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 20.Rohleder N, Wolf JM, Maldonado EF, Kirschbaum C. The psychosocial stress-induced increase in salivary alpha-amylase is independent of saliva flow rate. Psychophysiology. 2006;43:645–52. doi: 10.1111/j.1469-8986.2006.00457.x. [DOI] [PubMed] [Google Scholar]
- 21.Engert V, Vogel S, Efanov SI, Duchesne A, Corbo V, Ali N, Pruessner JC. Investigation into the cross-correlation of salivary cortisol and alpha-amylase responses to psychological stress. Psychoneuroendocrinology. 2011;36:1294–302. doi: 10.1016/j.psyneuen.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 22.Takai N, Yamaguchi M, Aragaki T, Eto K, Uchihashi K, Nishikawa Y. Gender-specific differences in salivary biomarker responses to acute psychological stress. Ann NY Acad Sci. 2007;1098:510–515. doi: 10.1196/annals.1384.014. [DOI] [PubMed] [Google Scholar]
- 23.Boutron I, Moher D, Altamn DG, Schulz KF, Ravaud P. Methods and processes of the CONSORT group: example of an extension for trials assessing nonpharmacologic treatments. Ann Intern Med. 2008;148:60–66. doi: 10.7326/0003-4819-148-4-200802190-00008-w1. [DOI] [PubMed] [Google Scholar]
- 24.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 25.Mitchell AM, Crane PA, Kim Y. Perceived stress in survivors of suicide: psychometric properties of the Perceived Stress Scale. Res Nurs Health. 2008;31:576–85. doi: 10.1002/nur.20284. [DOI] [PubMed] [Google Scholar]
- 26.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–43. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 27.Sukantarat KT, Williamson RC, Brett SJ. Psychological assessment of ICU survivors: a comparison between the Hospital Anxiety and Depression scale and the Depression, Anxiety and Stress scale. Anaesthesia. 2007;62:239–43. doi: 10.1111/j.1365-2044.2006.04948.x. [DOI] [PubMed] [Google Scholar]
- 28.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–39. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 29.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory. 3. Palo Alto: Consulting Psychologist Press; 1996. [Google Scholar]
- 30.Stamm BH. Measuring compassion satisfaction as well as fatigue: Developmental history of the Compassion Satisfaction and Fatigue Test. In: Figley CR, editor. Treating Compassion Fatigue. New York: Brunner-Routledge; 2002. pp. 107–119. [Google Scholar]
- 31.Stamm BH. The ProQOL Manual: The professional quality of life scale: compassion satisfaction, burnout and compassion fatigue/secondary trauma scales. Baltimore: Sidran Press; 2005. [Google Scholar]
- 32.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 33.Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Walsh E, Duggan D, Williams JM. Construct validity of the five facet mindfulness questionnaire in meditating and non-meditating samples. Assessment. 2008;15:329–42. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- 34.Nater UM, Rohleder N, Schlotz W, Ehlert U, Kirschbaum C. Determinants of the diurnal course of salivary alpha-amylase. Psychoneuroendocrinology. 2007;32:392–401. doi: 10.1016/j.psyneuen.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 35.Baer RA, Carmody J, Hunsinger M. Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction intervention. J Clin Psychol. 2012;68:755–765. doi: 10.1002/jclp.21865. [DOI] [PubMed] [Google Scholar]
- 36.Daubenmier J, Lin J, Blackburn E, Hecht FM, Kristeller J, Maninger N, Kuwata M, Bacchetti P, Havel PJ, Epel E. Changes in stress, eating, and metabolic factors are related to changes in telomerase activity in a randomized mindfulness intervention pilot study. Psychoneuroendocrinology. 2012;37:917–28. doi: 10.1016/j.psyneuen.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shapiro SL, Brown KW, Thoresen C, Plante TG. The moderation of mindfulness-based stress reduction effects by trait mindfulness: results from a randomized controlled trial. J Clin Psychol. 2011;67:267–77. doi: 10.1002/jclp.20761. [DOI] [PubMed] [Google Scholar]
- 38.Inagaki T, Miyaoka T, Okazaki S, Yasuda H, Kawamukai T, Utani E, Wake R, Hayashida M, Horiguchi J, Tsuji S. High salivary alpha-amylase levels in patients with schizophrenia: A pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:688–91. doi: 10.1016/j.pnpbp.2010.03.024. [DOI] [PubMed] [Google Scholar]
- 39.Holt-Lunstad J, Birmingham WA, Light KC. Influence of a “warm touch” support enhancement intervention among married couples on ambulatory blood pressure, oxytocin, alpha amylase, and cortisol. Psychosomatic Med. 2008;70:976–985. doi: 10.1097/PSY.0b013e318187aef7. [DOI] [PubMed] [Google Scholar]
- 40.Hoffman JW, Benson H, Arns PA, Stainbrook GI, Landsberg GL, Young JB, Gill A. Reduced sympathetic nervous system responsivity associated with the relaxation response. Science. 1982;215:190–192. doi: 10.1126/science.7031901. [DOI] [PubMed] [Google Scholar]
- 41.Park ER, Traeger L, Vranceanu AM, Scult M, Lerner JA, Benson H, Denninger J, Friecchione GL. The development of a patient-centered program based on the relaxation response: the relaxation response resilience program (3RP) Psychosomatics. 2013;54:165–174. doi: 10.1016/j.psym.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 42.Chang BH, Dusek JA, Benson H. Psychobiological changes from relaxation response elicitation: long-term practitioners vs. novices. Psychosomatics. 2011;52:550–559. doi: 10.1016/j.psym.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 43.Lush E, Salmon P, Floyd A, Studts JL, Weissbecker I, Sephton SE. Mindfulness meditation for symptom reduction in fibromyalgia: psychophysiological correlates. J Clin Psychol Med Settings. 2009;16:200–7. doi: 10.1007/s10880-009-9153-z. [DOI] [PubMed] [Google Scholar]
- 44.Ortner CNM, Kilner SJ, Zelazo PD. Mindfulness meditation and reduced emotional interference on a cognitive task. Motivation and Emotion. 2007;31:271–83. [Google Scholar]
- 45.Paul NA, Stanton SJ, Greeson JM, Smoski MJ, Wang L. Psychological and neural mechanisms of trait mindfulness in reducing depression vulnerability. Soc Cogn Affect Neurosci. 2013;8:56–64. doi: 10.1093/scan/nss070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hölzel BK, Carmody J, Evans KC, Hoge EA, Dusek JA, Morgan L, Pitman RK, Lazar SW. Stress reduction correlates with structural changes in the amygdala. Soc Cogn Affect Neur. 2010;5:11–17. doi: 10.1093/scan/nsp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taylor VA, Grant J, Daneault V, Scavone G, Breton E, Roffe-Vidal S, Courtemanche J, Lavarenne AS, Beauregard M. Impact of mindfulness on the neural responses to emotional pictures in experienced and beginner meditators. Neuroimage. 2011;57:1524–33. doi: 10.1016/j.neuroimage.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 48.Arch JJ, Brown KW, Dean DJ, Landy LN, Brown KD, Laudenslager ML. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective response to social evaluative threat in women. Psychonearoendocrinology. 2014;42:49–58. doi: 10.1016/j.psyneuen.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guntupalli KK, Fromm RE., Jr Burnout in the internist–intensivist. Intensive Care Med. 1996;22:625–630. doi: 10.1007/BF01709737. [DOI] [PubMed] [Google Scholar]
- 50.Limm H, Gündel H, Heinmüller M, Marten-Mittag B, Nater UM, Siegrist J, Angerer P. Stress management interventions in the workplace improve stress reactivity: a randomized controlled trial. Occup Environ Med. 2011;68:126–33. doi: 10.1136/oem.2009.054148. [DOI] [PubMed] [Google Scholar]
- 51.West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, Romanski SA, Henriksen Hellyer JM, Sloan JA, Shanafelt TD. Intervention to Promote Physician Well-being, Job Satisfaction, and Professionalism; A Randomized Clinical Trial. JAMA Intern Med. 2014;174:527–33. doi: 10.1001/jamainternmed.2013.14387. [DOI] [PubMed] [Google Scholar]