Abstract
Eastern equine encephalitis virus (EEEV) is a medically important pathogen that can cause severe encephalitis in humans, with mortality rates ranging from 30-80%. Unfortunately there are no antivirals or licensed vaccines available for human use, and laboratory diagnosis is essential to differentiate EEEV infection from other pathogens with similar clinical manifestations. The Arboviral Diseases Branch (ADB) reference laboratory at the CDC Division of Vector-Borne Diseases (DVBD) produces reference antigens used in serological assays such as the EEEV immunoglobulin M antibody-capture enzyme-linked immunosorbent assay (MACELISA). However, EEEV is classified as a HHS select agent and requires biosafety level (BSL) 3 containment, limiting EEEV antigen production in non-select agent and BSL-2 laboratories. A recombinant Sindbis virus (SINV)/EEEV has been constructed for use under BSL-2 conditions and is not regulated as a select agent. Cell culture production of inactivated EEEV antigen from SINV/EEEV for use in the EEEV MAC-ELISA is reported here. Cell culture conditions and inactivation procedures were analyzed for SINV/EEEV using a recently developed antigen production algorithm, with the MAC-ELISA as the performance indicator.
Keywords: Sindbis/Eastern Equine Encephalitis chimeric virus, Antigen, Immunoglobulin M antibody-capture enzyme-linked immunosorbent assay (MAC-ELISA), Beta-propiolactone, Gamma-irradiation
1. Introduction
Eastern equine encephalitis virus (EEEV) is a medically important mosquito-borne human and equine pathogen in North and South America (Griffin, 2001; Wang et al., 2007; Weaver, 2001; Weaver et al., 1999). Primarily transmitted in an enzootic cycle between the mosquito vector Culiseta melanura and passerine birds in freshwater, hardwood swamp habitats (Brault et al., 1999; Villari et al., 1995; Wang et al., 2007; Weaver, 2001), transmission of EEEV can occur via bridge vectors to dead-end hosts, such as humans, horses, and other animals (Arrigo et al., 2008; Morris, 1988). There are licensed vaccines for equines; however, no antivirals or licensed vaccines are available for human use (Franklin et al., 2002; Wang et al, 2007). Personal protection from mosquito bites is the only effective prevention strategy during times of active transmission, and treatment options are very limited.
EEEV is a member of the family Togaviridae, genus Alphavirus, and has been classified into EEEV (formerly North American) and Madariaga virus (formerly South American) (Powers et al., 2012). Madariaga virus is not associated with severe human disease (Aguilar et al., 2007; Arrigo et al., 2008; Tsai et al., 2002; Wang et al., 2007; Weaver, 2001; Weaver et al., 1999); however, EEEV can cause severe encephalitis in humans. The mortality rate of clinical EEEV disease is 30-80% and up to 30% of patients who survive have long-term neurological sequelae (Johnson et al, 2011; Villari et al., 1995; Wang et al., 2007). Clinical signs and symptoms usually begin with high fever, headache, dizziness, and vomiting. Progression to severe encephalitis with coma and paralysis can occur by day 2 of the disease (Wang et al., 2007). Although large EEEV outbreaks have been reported, human infections are generally sporadic, with an average of six cases reported annually in the United States, primarily along the east coast (www.cdc.gov/easternequineencephalitis/Epi.html#map). Due to the sporadic nature of the disease and because clinical symptoms of EEEV infection may be similar to infections by other pathogens, laboratory-based diagnosis is necessary to identify individuals infected with EEEV and to implement prevention and control strategies (Arrigo et al., 2008).
EEEV infection is diagnosed in acute cases by virus isolation, detection of viral RNA in serum or cerebrospinal fluid, or serologically by detection of EEEV-specific immunoglobulin M (IgM) antibodies in an enzyme-linked immunosorbent assay (ELISA), with confirmation by the plaque reduction neutralization test (PRNT) (Beaty et al., 1995; Johnson et al., 2011; Lambert et al, 2003). The CDC Division of Vector-Borne Diseases (DVBD) Arboviral Diseases Branch (ADB) reference laboratory produces reagents for arbovirus diagnostics for which there are no commercial assays available, such as the EEEV IgM antibody-capture (MAC)-ELISA. Non-infectious antigens used in the MAC-ELISA are normally derived from live virus that has been inactivated, with the serological reactivity preserved. An algorithm for production of inactivated antigens from arboviruses grown in cell culture was recently developed and evaluated (Goodman et al., 2014). One method could not be used for all of the arboviruses, but rather needed to be optimized for each virus. The method used to inactivate the virus often had a significant effect on antigen reactivity, resulting in either antigen degradation or increased reactivity.
EEEV strain NJ-60 is the prototype virus used previously to produce EEEV antigen. EEEV strains require biosafety level (BSL) 3 containment and are classified as HHS select agents (www.selectagents.gov/Select%20Agents%20and%20Toxins%20List.html). Consequently, only select agent-registered laboratories with BSL-3 capacity are permitted to possess and work with EEEV strains. However, a recombinant Sindbis virus (SINV) /EEEV has been constructed in which genes expressing the EEEV immunogenic structural proteins have been inserted into the SINV backbone (Wang et al., 2007). SINV/EEEV can be used under BSL-2 conditions and is not regulated as a select agent. Previously, SINV/EEEV was shown to be a comparable alternative challenge virus for use in the PRNT by public health laboratories with BSL-2 facilities (Johnson et al., 2011). The use of SINV/EEEV to produce inactivated EEEV antigen needed to be assessed and is reported here. Of particular concern was the effect the inactivation procedure would have on antigen reactivity of the chimeric virus. Cell culture conditions and inactivation procedures were analyzed for SINV/EEEV using the previously developed antigen production algorithm, with the MAC-ELISA as the performance indicator (Goodman et al., 2014).
2. Materials and Methods
2.1. Viruses
Sindbis/Eastern Equine Encephalitits (N. American) chimeric virus strain 796 (SINV/EEEV) was obtained from the University of Texas Medical Branch, Galveston, Texas (Wang et al., 2007).
2.2. Tissue culture
Cell lines used in the growth curves were obtained at CDC DVBD. African green monkey kidney (Vero) cells, and baby hamster kidney (BHK-21) clones 13 and 15 cells, were maintained at 37°C in Dulbecco’s Modified Eagle Medium (DMEM, Life Technologies, Grand Island, NY) with 8% fetal bovine serum (FBS, Atlas Biologicals, Fort Collins, CO), 1mM sodium pyruvate (Life Technologies), 27mM sodium bicarbonate (Life Technologies), 0.1mM gentamicin (Lonza, Walkersville, MD), and 1uM amphotericin B (Sigma-Aldrich, St. Louis, MO).
2.3. Growth curves
Growth curves were performed in T150 cm2 cell culture flasks (Corning Inc. Life Sciences, Tewksbury, MA), as previously described (Goodman et al., 2014). Briefly, cells were infected at a multiplicity of infection (MOI) of 0.001 PFU/cell. Following adsorption of virus in 10 ml of media at 37°C for 1 hr, cells were maintained in 60 ml of media with 2% FBS (Atlas Biologicals). At 24 hr intervals, 1.0 ml of supernatant was removed and stored at −70°C until tested. Growth curves were carried out for 4 days until cytopathic effect (CPE) reached ~90-100%.
2.4. Virus titration
Virus titers were determined by 1% agarose double-overlay plaque titration assay in Vero cells, as previously described (Beaty et al., 1995). Plaques were visualized with second overlays applied with 0.005% neutral red (Sigma-Aldrich) following incubation for 2 days. Virus titers were recorded as log10 PFU/ml.
2.5. IgM antibody-capture enzyme-linked immunosorbent assay (MAC-ELISA)
The CDC MAC-ELISA was used, as previously described (Martin et al., 2000). Positive-to-negative (P/N) ratios were determined, where P was defined as the mean optical density (OD) of the positive control serum reacted on viral antigen and N was defined as the mean OD of the negative control serum reacted on viral antigen. Interpretation of test results were as follows: P/N < 2 = negative, P/N 2-3 = equivocal, P/N > 3 = positive. Additionally, for a test to be valid, the mean OD of the sample serum reacted on viral antigen had to be at least twice the mean OD of the sample serum reacted on normal cell culture or suckling mouse brain antigen.
2.6. Viral antigen activity
Viral antigen activity was evaluated by the CDC MAC-ELISA, as previously described (Martin et al., 2000; Goodman et al., 2014). EEEV IgM positive and normal control reference sera were obtained from the DVBD diagnostic laboratory. Briefly, untreated live virus or inactivated antigen was serially diluted two-fold and reacted against both constant EEEV IgM positive and normal control sera in the MAC-ELISA. Virus-specific antigen activity (VSAA) was defined as the optical density (OD) of viral antigen reacted against a constant positive control serum; acceptable VSAA had an OD of >0.8. Nonspecific background reactivity (NBR) was defined as the OD of viral antigen reacted against a constant normal control serum; acceptable NBR had an OD of <0.2. A satisfactory antigen was defined as that which had acceptable MAC-ELISA results, in which both the VSAA and NBR were within acceptable OD ranges. The highest antigen dilution with acceptable VSAA and NBR OD ranges was considered the working antigen dilution, and was a measure of functional antigen concentration.
2.7. Virus production for inactivation and concentration analyses
The optimal virus cell culture type and day of harvest were determined by the growth curves. A second batch was then made under the optimized conditions in four additional T150 cm2 flask(s). Supernatant was harvested and clarified at 2400 x g for 10 min at 4°C, and stored at −70°C with 20% FBS (Atlas Biologicals) until further analysis.
2.8. Virus inactivation methods
2.8.1. Beta-propiolactone (BPL)
Virus cell culture supernatants were thawed in a 44°C water bath with intermittent shaking. Aliquots of 15 ml were made and BPL (CTC Organics, Atlanta, GA) was added at final concentrations ranging from 0.1% to 0.3%. The BPL-treated aliquots were incubated for 24 hr at 4°C with moderate shaking on a refrigerated shaker plate. Mock-treated control virus supernatants (no addition of BPL) were incubated under the same conditions as the BPL-treated samples. Due to acidic BPL by-products, 7.5% sodium bicarbonate (Life Technologies) was added intermittently to adjust the pH (French, McKinney, 1964). Following BPL treatment the samples were stored at −70°C until further analysis. For hydrolysis analysis, samples were treated with 0.2% BPL and incubated for 24 h at 4°C with moderate shaking. Following BPL treatment, material that underwent hydrolysis was incubated at 37°C for 2 h, and then placed at −70°C until further analysis.
2.8.2. Gamma-irradiation
Gamma-irradiation was carried out at the CDC irradiation facility in Atlanta, GA using a cobalt-60 source with a 500 ml volume capacity. Based on previous experience inactivating alphaviruses, samples were irradiated with 6 Mrad (Goodman et al., 2014). Samples were maintained frozen on dry ice throughout shipping and the treatment process. Untreated control virus supernatants remained frozen without any exposure to gamma-irradiation.
2.9. Antigen Concentration
Antigen was concentrated after inactivation, as it had been determined empirically that antigen activity was lost if it was concentrated before inactivation. Inactivated cell culture supernatants were concentrated in Amicon Ultra-15 100kDa Centrifugal Filter Devices (Millipore, Billerica, MA) or Centricon Plus-70 100-kDa Centrifugal Filter Devices (Millipore) at 3500 x g for 10-45 min at 4°C. The final volume was adjusted with 0.1M trizma/BS buffer: 1.0M trizma pH 9.0 (Sigma-Aldrich) + borate saline solution pH 9.0 [1.5M sodium chloride (Daigger, Vernon Hills, IL), 0.5M boric acid (Fisher Scientific), 1.0N sodium hydroxide (Daigger)] to the desired concentration factor.
2.10. Viability assays
Two procedures were used to evaluate virus inactivation, as described previously (Goodman et al, 2014). Briefly, plaque titration of BPL-treated or gamma-irradiated antigen was performed in duplicate in 6-well plates on Vero cells, beginning at neat concentration, with a lower limit of detection (LLOD) of 10 PFU/ml. In addition, 100 μl of antigen was inoculated into duplicate T25 cm2 cell culture flasks containing Vero cells and passaged once a week for three weeks. Virus was considered inactivated if there was no detectable titer by plaque titration and if there was no detectable CPE in any of the three cell culture passages.
2.11. Lyophilization
Inactivated antigen was lyophilized in 250 μl aliquots in 2ml, 13mm Kimble serum vials (Kimble-Chase, Vineland, NJ) using a freeze-dry system (Labconco, Kansas City, MO). Samples were frozen at −70°C overnight, and then lyophilized for 18 hr at −30°C, then 6 hr at 30°C.
2.12. Antigen evaluation
A vial of lyophilized antigen was reconstituted and antigen performance was compared to reference suckling mouse brain antigen (SMB) in a panel of 12 archived de-identified EEEV IgM positive serum samples which had previously been tested in the ADB diagnostic laboratory by the CDC-microsphere immunoassay (MIA) and confirmed by PRNT (Basile et al., 2013; Beaty et al., 1995; Johnson et al. 2011). MIA results do not measure IgM titer; therefore, neutralization titers were used as a proxy to choose a range of high, medium, and low EEEV positive samples. Per the CDC protocol, samples were diluted 1:400 and tested in triplicate against the inactivated SINV/EEEV cell culture antigen or EEEV SMB antigen at their previously calculated working antigen dilutions of 1:40 and 1:80, respectively. Optical densities were averaged, and positive-to-negative (P/N) ratios were determined according to methods described previously (Martin et al., 2000).
3. Results
SINV/EEEV growth curves were performed first to determine the optimal cell culture type to use for subsequent antigen production. Next a small-scale batch of virus (two T150 flasks) was grown under the optimized cell culture conditions and used for inactivation and concentration analyses. Once the inactivation and concentration procedures were finalized, a large-scale batch of bulk antigen was made. Final processing included making aliquots and lyophilizing the antigen, and storage at −20°C. Antigen performance was evaluated at each step in production by the MAC-ELISA, and rated as acceptable or unacceptable based on VSAA and NBR. The viability of the antigen was assessed after initial inactivation and at final concentration to rule out residual infectivity. The chosen inactivation method was the one that completely inactivated the virus, had VSAA and NBR within the acceptable ranges, and had the highest working antigen dilution compared to the mock-treated or untreated virus.
3.1. SINV/EEEV growth curves
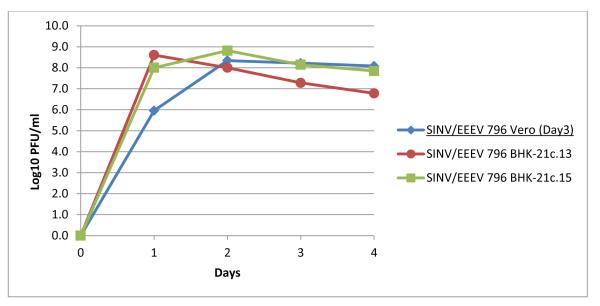
Virus was inoculated into T150 cm2 flasks containing Vero, BHK-21c.13, or BHK-21c.15 cells at a MOI of 0.001 and incubated for 4 days. Supernatant, 1 ml, was removed at 24 hr time points and tested by plaque titration and the EEEV MAC-ELISA. CPE was seen beginning on day 2 and was complete by days 3-4 (data not shown). Titers peaked by day 1-2 and were between 8 and 9 log10 PFU/ml in all cell types (Figure 1). However, none of the aliquots tested by the MAC-ELISA yielded acceptable VSAA despite the high titers obtained (data not shown).
Figure 1.
Growth of SINV/EEEV strain 796 in Vero, BHK-21c. 13, and BHK-21c.15 cells. T-150 cm2 flasks were inoculated with an MOI of 0.001 and incubated for 4 days. Underlined conditions indicate the optimal cell type and harvest day based on performance in the MACELISA.
3.2. SINV/EEEV inactivation
It had been shown previously that the VSAA of some alphaviruses increased after inactivation by BPL (French and McKinney, 1964; Goodman et al., 2014). Therefore, as proof of principle and despite the poor MAC-ELISA results, the remaining supernatant from the three growth curve flasks was collected on day 5 and treated with 0.3% BPL. The VSAA of the BPL-inactivated Vero cell culture supernatant increased and was acceptable out to a 1:3 dilution, but there was little increase of VSAA in the BHK-21c.13 and BHK-21c.15 cell culture supernatant (data not shown). Based on these preliminary results, a small-scale batch of SINV/EEEV was grown in Vero cells and harvested on day 3; this material was used for subsequent inactivation analyses.
Aliquots of SINV/EEEV supernatant from the small-scale material were treated with 0.1, 0.15, 0.2, 0.25, and 0.3% BPL (Table 1A). The SINV/EEEV VSAAs increased at all BPL concentrations compared to mock-treated virus, which had VSAA below the acceptable limit. All BPL concentrations completely inactivated the virus, and SINV/EEEV treated with ≤0.25% BPL produced acceptable MAC-ELISA results. These aliquots were then concentrated 50X using Amicon Ultra-15 centrifugal filters (Table 1A). Concentrated SINV/EEEV treated with ≤0.2% BPL had acceptable VSAA out to a 1:320 working antigen dilution; however, antigen treated with 0.1% BPL remained infectious.
Table 1.
SINV/EEEV antigen reactivity in the EEEV MAC ELISA following inactivation by BPL
| A. BPL treatment (small-scale) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antigen Dilution | VSAA | NBR | VSAA | NBR | VSAA | NBR | VSAA | NBR | VSAA | NBR | VSAA | NBR |
| 0.1% BPL | 0.15% BPL | 0.2% BPL | 0.25% BPL | 0.3% BPL | Mock-treated | |||||||
|
|
||||||||||||
| 1:2 | 1.995 | 0.156 | 2.151 | 0.478 | 1.960 | 0.578 | 1.640 | 0.534 | 1.159 | 0.450 ** | 0.215 | 0.029 |
| 1:4 | 1.192 | 0.075 | 1.357 | 0.103 | 1.157 | 0.099 | 0.999 | 0.072 | 0.713 | 0.083 | 0.208 | 0.025 |
| 1:8 | 0.812 | 0.045* | 0.885 | 0.055 | 0.724 | 0.045 | 0.593 | 0.039 | 0.437 | 0.039 | 0.118 | 0.022 |
| 1:16 | 0.537 | 0.038 | 0.537 | 0.041 | 0.416 | 0.038 | 0.346 | 0.031 | 0.277 | 0.032 | 0.063 | 0.021 |
| 1:32 | 0.428 | 0.030 | 0.315 | 0.030 | 0.274 | 0.029 | 0.197 | 0.030 | 0.204 | 0.025 | 0.027 | 0.024 |
| 1:64 | 0.219 | 0.036 | 0.196 | 0.026 | 0.155 | 0.024 | 0.123 | 0.024 | 0.129 | 0.025 | 0.022 | 0.022 |
| 0.1% BPL - 50X | 0.15% BPL - 50X | 0.2% BPL - 50X | 0.25% BPL - 50X | |||||||||
|
|
||||||||||||
| 1:10 | 2.271 | 0.189 | 1.155 | 0.920 | 1.081 | 2.034 | 1.034 | 2.617 | ||||
| 1:20 | 2.563 | 0.175 | 1.793 | 0.575 | 1.802 | 1.103 | 2.030 | 1.441 | ||||
| 1:40 | 2.165 | 0.104 | 2.534 | 0.346 | 2.573 | 0.730 | 2.322 | 0.804 | ||||
| 1:80 | 1.705 | 0.088 | 2.298 | 0.246 | 2.211 | 0.391 | 1.819 | 0.473 | ||||
| 1:160 | 1.263 | 0.070 | 1.787 | 0.164 | 1.627 | 0.243 | 1.140 | 0.238 | ||||
| 1:320 | 0.803 | 0.048 † | 1.200 | 0.089 | 0.953 | 0.108 | 0.658 | 0.127 | ||||
| B. BPL treatment (large-scale) | ||||
|---|---|---|---|---|
| Antigen Dilution | VSAA | NBR | VSAA | NBR |
| 0.2% BPL | 0.2% BPL | |||
| Unconcentrated | 12X Concentrated | |||
|
|
||||
| 1:10 | 0.547 | 0.064 | 2.009 | 0.487 |
| 1:20 | 0.269 | 0.051 | 1.117 | 0.245 † |
| 1:40 | 0.160 | 0.036 | 0.633 | 0.150 |
| 1:80 | 0.103 | 0.030 | 0.388 | 0.093 |
| 1:160 | 0.066 | 0.031 | 0.247 | 0.068 |
| 1:320 | 0.045 | 0.031 | 0.167 | 0.052 |
Abbreviations: VSAA, virus-specific antigen activity; NBR, nonspecific background reactivity.
OD readings in bold indicate the lowest dilution of antigen that yielded acceptable MAC ELISA results and was completely inactivated.
ODs in bold underlined italics indicate the dilution of antigen that yielded acceptable VSAA, but unacceptable NBR.
OD readings in bold italics indicate the dilution of antigen that yielded acceptable VSAA and NBR, but which was still infectious.
Based on the results from the SINV/EEEV small-scale inactivation and concentration experiment described above, and those from previous experiments that showed that 0.15% BPL was perhaps the borderline concentration that would completely inactivate alphaviruses, 0.2% BPL concentration was selected for inactivation of the SINV/EEEV large-scale batch in order to assure complete inactivation (Table 1B). The BPL-treated SINV/EEEV large-scale material was then concentrated 12X in a Centricon-70 centrifugal filter. The VSAA was acceptable out to a 1:20 working antigen dilution; however, during this scale-up process, the NBR rose above the acceptable limit (Table 1B). An aliquot of BPL-treated SINV/EEEV was incubated at 37°C for 2 h to assure complete hydrolysis of BPL. Hydrolyzed antigen NBR increased and VSAA decreased compared to the non-hydrolyzed antigen (data not shown). BPL, therefore, was not considered a suitable inactivation method for SINV/EEEV antigen production.
Gamma irradiation of SINV/EEEV small-scale material with 6 Mrad completely inactivated the virus. VSAA increased compared to untreated virus; acceptable MAC-ELISA results were obtained out to a 1:8 working antigen dilution (Table 2A). The antigen was then concentrated 25X in an Amicon Ultra-15 centrifugal filter, and yielded acceptable MAC-ELISA results out to a 1:80 working antigen dilution. The concentrated antigen remained non-infectious (Table 2A).
Table 2.
SINV/EEEV antigen reactivity in the EEEV MAC ELISA following inactivation by gamma-irradiation
| A. ɣ-treatment (small-scale) | ||||
|---|---|---|---|---|
| Antigen Dilution | VSAA | NBR | VSAA | NBR___ |
| 6 Mrad | Untreated___ | |||
|
|
||||
| Neat | 2.119 | 0.224 | 0.118 | 0.026 |
| 1:2 | 2.220 | 0.095 | 0.128 | 0.026 |
| 1:4 | 1.813 | 0.069 | 0.101 | 0.028 |
| 1:8 | 1.262 | 0.064* | 0.052 | 0.029 |
| 1:16 | 0.707 | 0.054 | 0.036 | 0.026 |
| 1:32 | 0.407 | 0.051 | 0.029 | 0.032 |
| 6 Mrad – 25X_ | ||||
| 1:10 | 1.958 | 0.382 | ||
| 1:20 | 1.441 | 0.092 | ||
| 1:40 | 1.160 | 0.051 | ||
| 1:80 | 0.818 | 0.044 | ||
| 1:160 | 0.477 | 0.034 | ||
| 1:320 | 0.300 | 0.038 | ||
| B. ɣ-treatment (large-scale) | ||||||
|---|---|---|---|---|---|---|
| Antigen Dilution | VSAA | NBR | VSAA | NBR___ | VSAA | NBR___ |
| 6 Mrad | 6 Mrad | 6 Mrad – 12X | ||||
| Unconcentrated | 12X Concentrated | Conc. – Lyophilized | ||||
|
|
||||||
| 1:10 | 0.771 | 0.062 | 2.060 | 0.149 | 1.573 | 0.098 |
| 1:20 | 0.433 | 0.047 | 1.802 | 0.085 | 1.324 | 0.068 |
| 1:40 | 0.245 | 0.042 | 1.228 | 0.062 | 0.883 | 0.053 |
| 1:80 | 0.147 | 0.040 | 0.746 | 0.053 | 0.522 | 0.048 |
| 1:160 | 0.086 | 0.034 | 0.429 | 0.047 | 0.313 | 0.046 |
| 1:320 | 0.060 | 0.029 | 0.245 | 0.038 | 0.182 | 0.042 |
Abbreviations: VSAA, virus-specific antigen activity; NBR, nonspecific background reactivity.
OD readings in bold indicate the lowest dilution of antigen that yielded acceptable MAC ELISA results and was completely inactivated.
Shaded boxes indicate the inactivation condition(s) used for final antigen production.
Large-scale SINV/EEEV supernatant was gamma-irradiated with 6 Mrad then concentrated 12X in a Centricon-70 centrifugal filter. The concentrated antigen was not infectious, and had acceptable MAC-ELISA activity out to a 1:40 working antigen dilution (Table 2B). Therefore, gamma irradiation was selected as the inactivation method for final, scaled-up SINV/EEEV antigen production. Aliquots of 0.25ml were made of the final product; the antigen was then lyophilized, sealed, and stored at −20°C. To test stability of the final product, one vial of the lyophilized antigen was removed from the freezer, reconstituted in 0.25 ml sterile water, and re-evaluated in the MAC-ELISA. The VSAA of the lyophilized antigen decreased slightly compared to non-lyophilized antigen, but the working antigen dilution remained at 1:40 (Table 2B).
3.3. SINV/EEEV evaluation
Performance of inactivated SINV/EEEV cell culture and EEEV SMB antigens was compared in a panel of 12 previously identified EEEV positive serum samples (Table 3). All results were positive in the MAC-ELISA using the SINV/EEEV antigen, and P/Ns were higher in 9 of 12 samples compared to EEEV SMB antigen. Two of the low-positive samples (samples 1 and 3) had negative results in the MAC-ELISA with the EEEV SMB antigen.
Table 3.
Comparison of SINV/EEEV cell culture and EEEV SMB antigen reactivity in the EEEV MAC-ELISA
| EEEV positive serum sample |
SINV/EEEV cell culture antigen - P/N |
EEEV SMB antigen - P/N |
|---|---|---|
| High positive 1 | 49.3 | 47.6 |
| High positive 2 | 61.4 | 74.5 |
| High positive 3 | 63.1 | 87.9 |
| High positive 4 | 56.2 | 53.3 |
| Medium positive 1 | 54.5 | 62.7 |
| Medium positive 2 | 54.5 | 53.0 |
| Medium positive 3 | 46.2 | 32.8 |
| Medium positive 4 | 53.5 | 41.1 |
| Low positive 1 | 4.9 | 1.2 |
| Low positive 2 | 12.3 | 3.5 |
| Low positive 3 | 4.9 | 1.8 |
| Low positive 4 | 12.8 | 4.7 |
Abbreviations: P/N, positive-to-negative ratio
MAC-ELISA interpretations: P/N < 2 = negative, P/N 2-3 = equivocal, P/N > 2 = positive
4. Discussion
EEEV is an enzootic arbovirus that circulates throughout eastern North America. Although only a few cases of EEEV infections in humans and unvaccinated horses are reported annually, EEEV infection is clinically indistinguishable from other neuroinvasive diseases and detection relies on laboratory-based surveillance. The EEEV MAC-ELISA is the primary serological test used to detect EEEV infection, confirmed by the neutralization assay with live virus. Viral antigens used in the ELISA generally are made from inactivated and concentrated live virus. EEEV is a select agent restricted, BSL-3 agent; therefore in order to make EEEV antigen from wild-type EEEV, a laboratory would need to have a BSL-3 facility and be registered with the select agent program.
SINV/EEEV is a recombinant virus in which the genes coding for the antigenic EEEV envelope proteins have replaced those of SINV in the SINV genome. SINV/EEEV can be used under BSL-2 conditions and is not under select agent restrictions. Previously, SINV/EEEV was shown to be neutralized similarly to wild-type EEEV in the PRNT (Johnson et al., 2011). Production of EEEV antigen from SINV/EEEV needed to be assessed to determine if the antigen would react appropriately to EEEV IgM in the MAC-ELISA, and to evaluate the stability of the chimeric virus particle proteins throughout the antigen production process of inactivation, concentration, and lyophilization. Using a previously described antigen production algorithm, the antigen production process and evaluation of SINV/EEEV in the MAC-ELISA, the end-use assay for this study, were described here (Goodman et al., 2014).
Peak SINV/EEEV titers from the growth curves were similar in all cell types, between 8 and 9 log10 PFU/ml, but none of the supernatant aliquots yielded acceptable VSAA in the EEEV MAC-ELISA. This lack of antigen activity prior to inactivation, and up to a tenfold increase in activity after inactivation, had been observed previously (French and McKinney, 1964; Goodman et al., 2014). Future experiments to investigate this include possible epitope mapping and x-ray crystallography to determine why there is a difference in antigen activity between infectious versus inactivated material. Therefore, production continued with inactivation by BPL at concentrations ranging from 0.1%-0.3%. SINV/EEEV was completely inactivated by ≥0.2% BPL, and although the VSAA was acceptable, the NBR was high, and increased to unacceptable levels after the antigen was concentrated 12X.
The increase in NBR following BPL treatment has been observed previously (Goodman et al., 2014). BPL is hydrolyzed in aqueous solution to β-hydroxypropionic acid (Perrin, Morgeaux, 1995). Sodium bicarbonate is added to the supernatant throughout the 24 hr inactivation process to neutralize the acid and preserve the VSAA, as acidity degrades the protein. In order to determine if there was residual BPL in the supernatant that might be causing the increase in NBR following BPL inactivation, the supernatant was incubated at 37°C for 2 hr to facilitate complete BPL hydrolysis, even though it had previously been shown that some VSAA is destroyed during hydrolysis, probably due to the rapid acidification of the supernatant heated to 37°C (Goodman et al., 2014). As expected, the VSAA of the SIN/EEEV did decrease following hydrolysis of the BPL. However, in contrast to previous observations, the NBR increased. Chemical inactivation with BPL is inexpensive and effective, but the quality of the final product is highly variable (Goodman et al., 2014). Therefore, BPL was not considered to be an acceptable method for inactivating SINV/EEEV because of the resultant high NBR.
Gamma irradiation is an alternative method of virus inactivation. At 6 Mrad, SINV/EEEV was completely inactivated, had higher VSAA compared to live virus, and lower NBR compared to BPL-inactivated antigen. Further processing by concentration and lyophilization did not alter the performance of the antigen in the end-use MAC-ELISA.
Comparison of SINV/EEEV cell culture antigen to EEEV SMB antigen using previously identified EEEV positive control serum samples demonstrated the acceptable performance of SINV/EEEV antigen in the EEEV MAC-ELISA. Indeed the sensitivity of the EEEV MACELISA was higher when the SINV/EEEV antigen was used, as IgM was detected in 2 low positive samples with the SINV/EEEV antigen, but not the EEEV SMB antigen.
In conclusion, EEEV antigen used in the diagnostic MAC-ELISA could be produced from SINV/EEEV under optimized conditions determined empirically. The final product derived from the recombinant SINV/EEEV had similar antigenicity and stability to antigen produced from wild-type alphaviruses (Goodman et al., 2014). The ability of non-select agent registered, BSL-2 laboratories to produce inactivated EEEV antigen by using recombinant SINV/EEEV will enhance the capacity of reference laboratories to provide these important diagnostic reagents.
Acknowledgments
We would like to thank Lyle Petersen, Wendi Kuhnert, Paul Simpson, and Kathi Kellar for their exceptional assistance in coordinating gamma-irradiation services between CDC-Fort Collins, CO and CDC-Atlanta, GA.
References
- Aguilar PV, Robich RM, Turell MJ, O’Guinn ML, Klein TA, Huaman A, Guevara C, Rios Z, Tesh RB, Watts DM, Olson J, Weaver SC. Endemic eastern equine encephalitis in the Amazon region of Peru. Am J Trop Med Hyg. 2007;76:293–98. [PubMed] [Google Scholar]
- Arrigo NC, Watts DM, Frolov I, Weaver SC. Experimental infection of Aedes sollicitans and Aedes taeniorhynchus with two chimeric sindbis/eastern equine encephalitis virus vaccine candidates. Am J Trop Med Hyg. 2008;78:93–97. [PMC free article] [PubMed] [Google Scholar]
- Basile AJ, Horiuchi K, Panella AJ, Laven J, Kosoy O, Lanciotti RS, Venkateswaran N, Biggerstaff BJ. Multiplex microsphere immunoassays for the detection of IgM and IgG to arboviral diseases. Plos One. 2013;8:1–16. doi: 10.1371/journal.pone.0075670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaty B, Calisher C, Shope R. Arboviruses. In: Lennette E, Lennette D, Lennette E, editors. Diagnostic procedures for viral, rickettsial, and chlamydial infections. American Public Health Association; Washington, DC: 1995. pp. 189–212. [Google Scholar]
- Brault AC, Powers AM, Chavez CL, Lopez RN, Cachon MF, Gutierrez LF, et al. Genetic and antigenic diversity among eastern equine encephalitis viruses from North, Central, and South America. Am J Trop Med Hyg. 1999;61:579–86. doi: 10.4269/ajtmh.1999.61.579. [DOI] [PubMed] [Google Scholar]
- Franklin RP, Kinde H, Jay MT, Kramer LD, Green EG, Chiles RE, et al. Eastern equine encephalomyelitis virus infection in a horse from California. Emerg Infect Dis. 2002;8:283–8. doi: 10.3201/eid0803.010199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French GR, McKinney RW. Use of Beta-Propiolactone in Preparation of Inactivated Arbovirus Serologic Test Antigens. J Immunol. 1964;92:772–8. [PubMed] [Google Scholar]
- Goodman CH, Russell BJ, Velez JO, Laven JJ, Nicholson WL, Bagarozzi DA, Jr., Moon JL, Bedi K, Johnson BW. Development of an algorithm for production of inactivated arbovirus antigens in cell culture. J Virol Methods. 2014;208:66–78. doi: 10.1016/j.jviromet.2014.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin DE. Alphaviruses. In: Knipe DM, Howley P.M. (Eds), editors. Fields Virology. Vol. 4. Lippincott, Williams, and Wilkins; New York, NY: 2001. pp. 917–62. [Google Scholar]
- Johnson BW, Kosoy O, Wang E, Delorey M, Russell B, Bowen RA, Weaver SC. Use of sindbis/eastern equine encephalitis chimeric viruses in plaque reduction neutralization tests for arboviral disease diagnostics. Clin Vacc Immun. 2011;18:1486–91. doi: 10.1128/CVI.05129-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert AJ, Martin DA, Lanciotti RS. Detection of North American eastern and western equine encephalitis viruses by nucleic acid amplification assays. J Clin Microbiol. 2003;41:379–385. doi: 10.1128/JCM.41.1.379-385.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin DA, Muth DA, Brown T, Johnson AJ, Karabatsos N, Roehrig JT. Standardization of immunoglobulin M capture enzyme-linked immunosorbent assays for routine diagnosis of arboviral infections. J Clin Micro. 2000;38:1823–6. doi: 10.1128/jcm.38.5.1823-1826.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monath TP, Lee CK, Julander JG, Brown A, Beasley DW, Watts DM, Hayman E, Guertin P, Makowiecki J, Crowell J, Levesque P, Bowick GC, Morin M, Fowler E, Trent DW. Inactivated yellow fever 17D vaccine: development and nonclinical safety, immunogenicity and protective activity. Vaccine. 2010;28:3827–40. doi: 10.1016/j.vaccine.2010.03.023. [DOI] [PubMed] [Google Scholar]
- Morris CD. Eastern equine encephalomyelitis. In: Monath TP, editor. The arboviruses: epidemiology and ecology III. CRC Press; Boca Raton, FL: 1988. pp. 293–98. [Google Scholar]
- Perrin P, Morgeaux S. Inactivation of DNA by β-propiolactone. Biologicals. 1995;23:207–11. doi: 10.1006/biol.1995.0034. [DOI] [PubMed] [Google Scholar]
- Powers A, Huang H, Roehrig J, Strauss E, Weaver S. Part II – The Positive Sense Single Stranded RNA Viruses: Togaviridae: Alphavirus. In: King AMQ, Adams MJ, Carstens EB, Lefkowitz EJ, editors. Virus taxonomy: classification and nomenclature of viruses: Ninth report of the International Committee on Taxonomy of Viruses. Elsevier Academic Press; San Diego, CA: 2012. pp. 1105–10. [Google Scholar]
- Tsai TF, Weaver SC, Monath TP. Alphaviruses. In: Richmann DD, Whitley RJ, Hayden FG, editors. Clinical Virology. ASM Press; Washington, DC: 2002. pp. 1177–210. [Google Scholar]
- Uittenbogaard JP, Zomer B, Hoogerhout P, Metz B. Reactions of β-propiolactone with nucleobase analogues, nucleosides, and peptides: implications for the inactivation of viruses. J Biol Chem. 2011;286:36198–214. doi: 10.1074/jbc.M111.279232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villari P, Spielman A, Komar N, McDowell M, Timperi RJ. The economic burden imposed by a residual case of eastern encephalitis. Am J Trop Med Hyg. 1995;52:8–13. doi: 10.4269/ajtmh.1995.52.8. [DOI] [PubMed] [Google Scholar]
- Wang E, Petrakova O, Adams AP, Aguilar PV, Kang W, Paessler S, Volk SM, Frolov I, Weaver SC. Chimeric sindbis/eastern equine encephalitis vaccine candidates are highly attenuated and immunogenic in mice. Vaccine. 2007;25:7573–81. doi: 10.1016/j.vaccine.2007.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver SC. Eastern equine encephalitis. In: Service MW, editor. The encyclopedia of arthropod-transmitted infections. CAB International; Wallingford, UK: 2001. pp. 151–59. [Google Scholar]
- Weaver SC, Tesh RB, Shope RE. Alphavirus infections. In: Guerrant RI, Walker DH, Weller PF, editors. Tropical infectious diseases principles, pathogens and practice. Churchill Livingstone; Philadelphia, PA: 1999. pp. 1281–87. [Google Scholar]