Abstract
To evaluate whether the use of traditional Chinese medicine (TCM; 中醫 zhōng yī) influences symptoms or functional outcomes in patients with osteoarthritis (OA) of the knee (膝關節炎 xī guān jié yán).
A systematic review of randomized control trials was conducted. Searches for studies in PubMed that were performed between 1965 and August 2013, and retrieved studies were subjected to reference screening. The types of studies included in our review were 1) placebo-based or comparative studies; 2) open label, single-blinded or double-blinded studies; 3) studies evaluating the efficacy of TCM for treating OA of the knee; and 4) studies evaluating only TCM or combination preparations. Trials were conducted with participants over 18 years of age with knee pain and at least three of the following characteristics: 1) an age greater than 50 years; 2) morning stiffness lasting for fewer than 30 min; 3) a crackling or grating sensation; 4) bony tenderness of the knee; 5) bony enlargement of the knee; or 6) no detectable warmth of the joint to the touch. Studies were rated for risk of bias and graded for quality.
After screening, 104 studies that satisfied the eligibility requirements were identified, and only 18 randomized control trials were included in the quantitative and qualitative synthesis. Upon review, we found “moderate-quality” evidence of effects from acupuncture (針灸 zhēn jiǔ) on pain, which was measured using a visual analogue scale, and physical function, which was measured using qigong (氣功 qì gōng) with motion. “Low-quality” evidence was found regarding the effects of acupuncture on physical function, and no evidence was found regarding the effects of herbal medicine on pain or physical function. Herbal patches (藥布 yào bù) appeared to affect pain and physical and function, but these effects were not found to be significant.
The initial findings included in this review suggest that acupuncture is a promising intervention according to the primary outcome measure, pain, and qigong with motion is an effective method for treating physical function. However, according to the Grades of Recommendation, Assessment, Development, and Evaluation criteria, only moderate-quality evidence was found in these studies. Further rigorous studies are warranted to investigate the application of TCM in treating OA of knee.
Keywords: osteoarthritis, knee, traditional Chinese medicine, acupuncture, qigong, massage
Graphical abstract
1. Introduction
Osteoarthritis (OA), originating from the Greek words “bone”, “joint”, and “inflammation”, is one of the most common causes of pain and disability in middle-aged and older people.1 OA is currently considered an inflammatory disorder of movable joints that is involved in several pathological features such as deterioration and abrasion of articular cartilage and formation of new bone at the articular surface and subchondral bone, resulting in limitation of joint movement.2, 3, 4 The incidence of symptomatic OA is likely to increase because of the aging population and obesity epidemic.5 In the United States, the prevalence of OA of the knee (膝關節炎 xī guān jié yán) is 10% in men and 13% in women in millions among adults 60 years of age or older in 2010.5 Radiographic evidence of OA generally appears in those over 65 years of age, approximately 80% of whom are over 75 years of age.6 OA is essentially an inflammatory disease, causing signs and symptoms of inflammation such as stiffness and joint effusion.4 OA causes articular cartilage loss, capsular stretching, muscle weakness, bony remodeling, synovitis, and ligament laxity, ultimately leading to malalignment of the knee joint. The abnormal structure resulting from OA causes abnormal focal stress in the knee joint and induces a vicious cycle of joint damage. The major complaint of patients with OA of the knee is pain derived from tearing of the patella-femoral joint, inflammation of soft tissue, and collection of synovial fluid.3, 7 Treatment of OA includes intraarticular corticosteroid injection, oral acetaminophen, capsaicin cane, and nonsteroidal antiinflammatory drugs (NSAIDs).8
According to the basic theory of traditional Chinese medicine (TCM; 中醫 zhōng yī), OA is an “impediment disease (痹病 bì bìng)”, which refers to a group of diseases resulting from “invasion of wind, cold, and dampness (風寒濕侵襲 fēng hán shī qīn xí)”.9 Mavrommtis et al (2012) reported that acupuncture (針灸 zhēn jiǔ) with etoricoxib reduced pain more than did sham acupuncture with etoricoxib or etoricoxib alone in patients with knee OA.10 Duhuo Jisheng Tang treatment for 4 weeks can reduce pain and stiffness and improve physical function in knee OA patients.11 Moxibustion (艾灸 ài jiǔ) is a traditional therapy to treat diseases through thermal stimulation by burning herb when the knee pain was due to “the invasion of the cold (風邪侵襲 fēng xié qīn xí)”.12 Herbal patch (藥布 yào bù) is made through the powder of the herbs, vegetable oil and excipient, like Componere Hydrargyrum (Shenyao), then cooling and coating with cloth or paper. Herbal patch is placed on the injured area or acupoint (穴位 xué wèi) for reducing “swelling and pain (腫痛 zhǒng tòng)”.13 Qigong (氣功 qì gōng) is an energy exercise and therapy that assume the existence of a “Qi (氣 qì)” circulating throughout the body and in the surrounding environment.14 Massage therapy (推拿 tuī ná) is that the doctor uses their hands to manipulate the patient's body to relax and “dredge the meridians (疏通經絡 shū tōng jīng luò)” and promote “Qi flowing and blood circulating (氣血循環 qì xuè xún huán)”.15 Therefore, the aim of the present study was to determine whether the use of TCM influences symptoms or functional outcomes in patients with OA of the knee through a systematic review of randomized control trials (RCTs) from the PubMed and MEDLINE databases.
2. Materials and methods
2.1. Data source and review process
The PubMed database was used to search for relevant studies conducted between 1965 and August 2013. The PubMed database comprises more than 23 million citations of biomedical literature from MEDLINE, life science journals, and online books. The articles used in our analysis were published in English, and the full text of these studies is available through PubMed Central and publisher web sites. The keywords in our study were osteoarthritis, traditional Chinese medicine (TCM; 中醫 zhōng yī), acupuncture (針灸 zhēn jiǔ), herb, e herbal patches (藥布 yào bù), moxibustion (艾灸 ài jiǔ), Massage therapy (推拿 tuī ná) and qigong (氣功 qì gōng). TCM indicates the use of acupuncture, herbs, herbal patches, moxibustion, massage therapy, or integration for treatment. The major keyword “osteoarthritis” was combined with the other keywords separately. For example, “((osteoarthritis) AND acupuncture) AND English [Language]” or (osteoarthritis) AND Traditional Chinese Medicine AND English [Language], to search relevant RCTs for all TCM treatments for OA. Articles satisfying the search criteria were entered into a review process, and the full texts collected according to the criteria were further reviewed.
2.2. Types of studies
Only RCTs with participants appropriately allocated into treatment and control groups were included in our study. RCTs that 1) were placebo-based or comparative; 2) were open label, single-blinded or double-blinded; 3) evaluated the efficacy of TCM in OA of the knee; or 4) evaluated TCM only or a combination of preparations were included.
2.3. Types of participants
The inclusion criteria referred Zhang and Jordan (2010)5 for participants were (1) an age >50 years and (2) symptoms and signs of OA of the knee. Patients with at least three of the following characteristics were considered to have typical symptoms and signs of OA: (A) morning stiffness lasting fewer than 30 min; (B) a crackling or grating sensation; (C) bony tenderness of the knee; (D) bony enlargement of the knee; and (E) no detectable warmth of the joint to the touch. The exclusion criteria were (1) OA secondary to other etiologies such as trauma, infection, and rheumatoid arthritis; (2) OA located at multiple sites, and inability of the treatment to target specific joints and (3) if those multiple sites included OA of knee.
2.4. Types of interventions
The types of interventions analyzed in our review were acupuncture or electroacupuncture (EA; 電針 diàn zhēn), herbs or formulas, herbal patches, moxibustion, qigong and massage therapy, according to the theory of TCM. Studies designed to treat OA by integrating TCM and modern medicine was also included. Studies involving laser acupuncture or acupuncture with local drug injections and nonclinical studies, such as animal and cell line studies, were excluded.
2.5. Types of outcome measurement
The studies analyzed in this review were required to include an assessment before and after intervention and a follow-up period. All studies applied tools for assessing the effectiveness of treatment, namely (1) tools for measuring pain intensity such as the Visual Analogue Scale (VAS) and Numeric Rating Scale (NRS) and (2) tools for measuring functional status or disability including the Western Ontario and McMaster Universities Arthritis Index (WOMAC), Short Form 36 (SF-36) health survey, and other reliable and valid methods. The timing of assessment was recorded, and the evaluations were blinded.
2.6. Risk-of-bias assessment and quality
The checklists of the Cochrane back review group were used as a methodological template to assess the risk of bias of individual RCTs. The methodological quality of trials was classified as “low”, “moderate”, and “high” by using a trial method adapted from previous guidelines (Table 1),16, 17 and studies rated equal or more than 6 of 12 were considered to have a low risk of bias.
Table 1.
Criteria for judging the quality of individual trials.
| High | >75% of the criteria have been fulfilled [≧10/12]. Where they have not been fulfilled the conclusions of the study or review are thought very unlikely to alter. |
| Moderate | 50–75% of the criteria have been fulfilled [6–9/12]. Those criteria that have not been fulfilled or not adequately described are thought unlikely to alter the conclusions. |
| Low | Less than 50% of the checklist criteria were fulfilled [<6/12]. The conclusions of the study are thought likely or very likely to alter. |
2.7. Quality of evidence
The overall quality of evidence was evaluated according to the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) criteria, as in previous research18 (Table 2). In brief, studies that were observational, limited, inconsistent, indirect, or imprecise or exhibited publication bias were considered to yield “low-quality” evidence. By contrast, studies that involved randomized trials and large effect sizes and showed evidence of a dose-response gradient were considered to provide “high-quality” evidence. Furthermore, when researchers attempted to eliminate all potential confounding factors, the results were considered high-quality evidence.
Table 2.
The evidence grading system applied in this review.
| High | At least 75% of the RCTs with no limitations of study design have consistent findings, direct and precise data and no known or suspected publication bias. |
| Moderate | One of the domains is not met. |
| Low | Two of the domains are not met. |
| Very low | Three of the domains are not met. |
| No evidence | No RCTs were identified that addressed this outcome. |
2.8. Data extraction
Data were analyzed and summarized using a standard form that comprised the following items: author/year/country, study design, participants, intervention, outcome measures, and results (Table 3, Table 4, Table 5, Table 6).
Table 3.
Osteoarthritis (OA) of the knee intervention with “Acupuncture (針灸 zhēn jiǔ)”.
| Basic information of researches | Participants | Intervention | Outcome assessment | Results | The risk of bias |
|---|---|---|---|---|---|
| Ng MM et al21 2003, Hong Kong, China (RCT) (Patient-blind) (Assessor-blind) |
N = 24 (diagnosed with OA knee) Inclusion criteria:
|
EA treatment (N = 8):
Subjects received general education on osteoarthritic knee care only |
|
|
10/12 (High) |
| Berman BM et al22 2004, USA (RCT) (Patient-blind) (Assessor-blind) |
N = 570 Inclusion criteria:
|
True acupuncture group (N = 190):
|
|
|
11/12 (High) |
| Tukmachi E et al23 2004, UK (RCT) |
N = 30 Inclusion criteria:
|
Group A (N = 9):
|
|
|
7/12 (Moderate) |
| Vas J et al24 2004, Spain (RCT) (Patient-blind) (Assessor-blind) |
N = 97 Inclusion criteria:
|
Intervention group (N = 48)
|
|
|
10/12 (High) |
| Witt C et al25 2005, Germany (RCT) (Patient-blind) |
N = 300 Inclusion criteria:
|
Acupuncture group (N = 150):
|
|
|
10/12 (High) |
| Scharf HP et al26 2006, Germany (RCT) (Patient-blind in TCA and sham) |
N = 1039 Inclusion criteria:
|
Conservative therapy (N = 342):
|
|
|
10/12 (High) |
| Williamson L et al27 2007, UK (RCT) (Patient-blind) (Assessor-blind) |
N = 181 (on the surgical list) Inclusion criteria:
|
Acupuncture group (N = 60):
|
|
|
10/12 (High) |
| Jubb RW et al28 2008, UK (RCT) (Patient-blind) |
N = 68 Inclusion criteria:
|
Acupuncture group (N = 34):
|
|
|
8/12 (Moderate) |
| Itoh K et al29 2008, Japan (RCT) (Patient-blind) (Assessor-blind) |
N = 30 (age >60 years, diagnosed OA according to ACR* criteria) Inclusion criteria:
|
Standard acupuncture (N = 10):
|
|
|
8/12 (Moderate) |
| Lu TW et al30 2010, Taiwan (RCT) (Patient-blind) |
N = 20 Inclusion criteria:
|
Experimental group (N = 10):
|
|
|
9/12 (Moderate) |
| Soni A et al31 2012, UK (RCT) (Parallel design) (Assessor-blind) |
N = 56 Inclusion criteria:
|
Acupuncture and exercise therapy (N = 28):
|
|
|
8/12 (Moderate) |
| Mavrommatis CI et al10 2012, Greece (RCT) (Patient-blind) (Assessor-blind) |
N = 120 Inclusion criteria:
|
Acupuncture and etoricoxib (N = 40):
All patients received 60 mg etoricoxib tablets once a day for 60 days. |
|
|
10/12 (High) |
*EA: electro-acupuncture.
*VAS: visual analogue scale.
*WOMAC: The Western Ontario and McMaster Universities Arthritis Index.
*ACR: American College of Rheumatology.
*K-L: Kellgren-Lawrence criteria.
Table 4.
Herbal patch for OA of the knee.
| Author/Year Country/Design |
Participants | Intervention | Outcome assessment | Results | The risk of bias |
|---|---|---|---|---|---|
| Wang X et al13 2012, China (RCT) (Patient-blind) (Assessor-blind) (Care giver-Blind) |
N = 150 Inclusion criteria:
|
FNZG (N = 60) Extraction mainly from Rhizoma Arisaematis, Radix Aconiti, Flos Caryophylli and nine herbs. SJG (N = 60) Extraction mainly from Rhizoma Arisaematis, Radix Aconiti, and fifteen herbs. Placebo patch (N = 30) Acrylic pressure-sensitive adhesive tape All patches had the same size of 10 cm × 13 cm and were matched with each other for taste, color, and package. |
|
|
10/12 (High) |
Table 5.
Herbs for OA of the knee.
| Author/Year Country/Design |
Participants | Intervention | Outcome assessment | Results | The risk of bias |
|---|---|---|---|---|---|
| Park SH et al32 2009, Korea (RCT) (Patient-blind) (Care giver-blind) |
N = 57 Inclusion criteria: (1)Age from 43 to 73 years, (2)Diagnosis according to ACR criteria, (3)K-L grade 1–2, (4)stop all analgesic medication and physical therapy for 1 week before study |
AIF group (N = 31) the formulation which contained 200 mg of AIF (Ginsenoside Rb1, stachyose and eleutheroside E), 192 mg of corn starch, 4 mg of HPMC, 4 mg of magnesium stearate in each capsule. Placebo group (N = 26) the formulation of 392 mg of corn starch, 4 mg of HPMC, 4 mg of magnesium stearate in each capsule. |
|
|
9/12 (Moderate) |
| Li XH et al33 2010, China (RCT) |
N = 100 Inclusion criteria: (1) diagnosis according to ACR criteria, (2) diagnosis in TCM according to Directing Principle for Clinical Research of New Chinese Drugs, (3) X-ray grading |
Treatment group (N = 50)
|
|
|
5/12 (Low) |
Table 6.
Qigong for OA of the knee.
| Author/Year Country/Design |
Participants | Intervention | Outcome assessment | Results | The risk of bias |
|---|---|---|---|---|---|
| Chen KW et al14 2008, USA (RCT) (Patient-blind) (Assessor-blind) |
N = 112 Inclusion criteria: (1)diagnosis according to ACR criteria at least 6 months prior to evaluation, (2)physical examination before the study to confirm the diagnosis, (3) agreed to maintain a stable analgesic dose during study |
EQT group (N = 60):
|
|
|
10/12 (High) |
| An B et al34 2008, China (RCT) |
N = 28 (diagnosis according to ACR criteria) Inclusion criteria: (1)symptoms at least 6 months before study, (2) no current exercise programe, (3) willingness to participate in the study |
Baduanjin intervention (N = 14):
|
|
|
5/12 (Low) |
| Lee HJ et al35 2009, Korea (RCT) (Assessor-blind) |
N = 41 Inclusion criteria: (1)K-L grade≧2 at least 6 months, (2) no current exercise programme, (3)age from 50 to 80 years. |
T'ai chi (太極拳 tài jí quán) (N = 28):
|
|
|
10/12 (High) |
3. Results
3.1. Study selection and exclusion
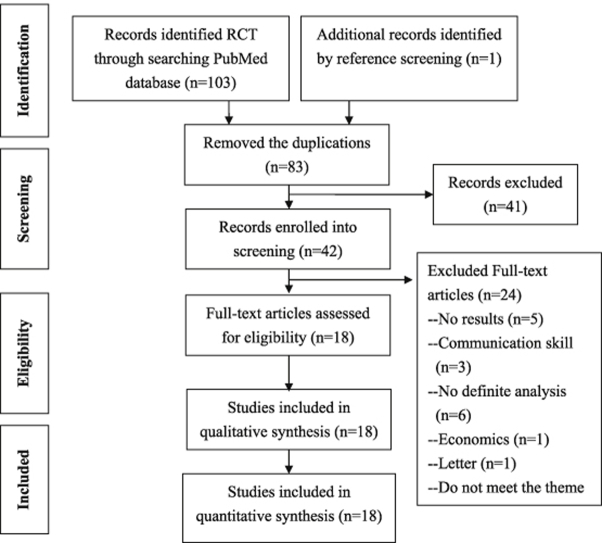
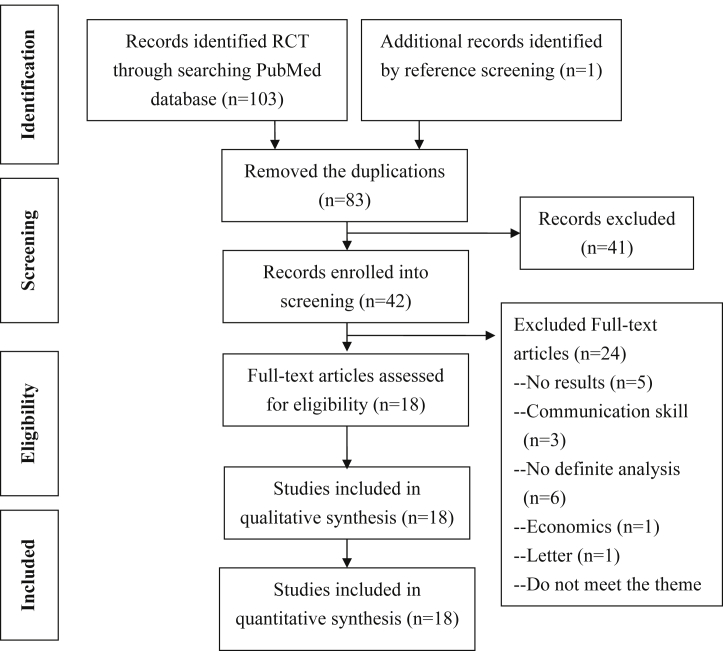
Studies were identified through PubMed according to the inclusion criteria. The protocol of data analysis and reasons for exclusion are summarized in Fig. 1. In summary, 104 studies were identified, and 21 studies were removed because of duplication. Eighty-three studies were screened again by reviewing the abstracts according to the inclusion and exclusion criteria. Studies that were impossible to include or exclude were retained until a full-text assessment could be conducted. Forty-two studies were included after assessing the descriptions of the full-text articles. Finally, 18 studies were included in our analysis (Table 3), and 24 studies were excluded because five studies did not include results, three related to communication skill, six lacked definite analyses, one focus in economics only, one was a letter, six were not relevant to the study objective, one related to a patient's expectations, and one lacked a discussion of a RCT. Twelve studies involved acupuncture (針灸 zhēn jiǔ) application10, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 (Table 3), one involved herbal patch (藥布 yào bù) application13 (Table 4), two involved herbal medicine application32, 33(Table 5), and three involved qigong (氣功 qì gōng) application for OA treatment14, 34, 35 (Table 6). No studies involvingmassage therapy (推拿 tuī ná), moxibustion (艾灸 ài jiǔ), or integrated therapy for OA were included in our analysis. Meta-analysis could not be conducted because of the heterogeneous study designs and treatment modalities of the included trials.
Fig. 1.
Flow diagram of inclusion and exclusion of articles (PRISMA 2009 Flow Diagram).
3.2. Risk of bias in the included studies
The risk of bias in the studies that we analyzed is shown in Table 1. Although 18 studies were described as randomized, nine lacked adequate randomization and concealed allocation, two lacked the inclusion of similar groups at the baseline, three lacked adequate or clear blinding, two lacked an acceptable dropout rate, five lacked an intention-to-treat analysis, three lacked adequate co-intervention, one lacked adequate compliance, one lacked an adequate timing outcome assessment, and one lacked adequate selective outcome reports.
Ten studies were considered to have high methodological quality (≧10/12), six had moderate methodological quality (6–9/12), and two had low methodological quality (<6/12). Seven studies with high methodological quality and five studies with moderate methodological quality involved acupuncture treatment. One study with moderate methodological quality and one study with low methodological quality involved herbal treatment. One study with high methodological quality involved herbal patch treatment. Two studies with high methodological quality and one study with low methodological quality involved qigong treatment (Table 7, Table 8, Table 9, Table 10).
Table 7.
Methodological quality assessment and risk-of-bias (Acupuncture (針灸 zhēn jiǔ)).
| Adequate randomization | Concealed allocation | Groups similar at baseline | Patient blinded | Care provider blinded | Outcome assessor blinded | Dropout rate described and acceptable | Intention to treat analysis | Co-interventions avoided or similar | Compliance acceptable | Timing outcome assessment similar | Report free of selective outcome reporting | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ng MM et al 2003 | Yes | Unclear | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10/12 |
| Berman BM et al 2004 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 11/12 |
| Tukmachi E et al 2004 | Yes | Yes | No | No | No | No | Yes | Yes | No | Yes | Yes | Yes | 7/12 |
| Vas J et al 2004 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes | 10/12 |
| Witt C et al 2005 | Yes | Unclear | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10/12 |
| Scharf HP et al 2006 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes | 10/12 |
| Williamson L et al 2007 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | 10/12 |
| Jubb RW et al 2008 | Unclear | Unclear | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | 8/12 |
| Itoh K et al 2008 | Unclear | Unclear | Yes | Yes | No | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | 8/12 |
| Lu TW et al 2010 | Unclear | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | 9/12 |
| Soni A et al 2012 | Yes | Yes | No | No | No | Yes | No | Yes | Yes | Yes | Yes | Yes | 8/12 |
| Mavrommatis CI et al 2012 | Yes | Yes | Yes | Yes | No | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | 10/12 |
Table 8.
Methodological quality assessment and risk-of-bias (Herbal patch).
| Adequate randomization | Concealed allocation | Groups similar at baseline | Patient blinded | Care provider blinded | Outcome assessor blinded | Dropout rate described and acceptable | Intention to treat analysis | Co-interventions avoided or similar | Compliance acceptable | Timing outcome assessment similar | Report free of selective outcome report in | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wang X et al 2012 | Unclear | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10/12 |
Table 9.
Methodological quality assessment and risk-of-bias (Herbal medicine).
| Adequate randomization | Concealed allocation | Groups similar at baseline | Patient blinded | Care provider blinded | Outcome assessor blinded | Dropout rate described and acceptable | Intention to treat analysis | Co-interventions avoided or similar | Compliance acceptable | Timing outcome assessment similar | Report free of selective outcome reporting | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Park SH et al 2009 | Unclear | Unclear | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | 9/12 |
| Li XH et al 2010 | Unclear | Unclear | Yes | Unclear | Unclear | Unclear | Yes | Yes | Unclear | Yes | Unclear | Yes | 5/12 |
Table 10.
Methodological quality assessment and risk-of-bias (Qigong (氣功 qì gōng)).
| Adequate randomization | Concealed allocation | Groups similar at baseline | Patient blinded | Care provider blinded | Outcome assessor blinded | Dropout rate described and acceptable | Intention to treat analysis | Co-interventions avoided or similar | Compliance acceptable | Timing outcome assessment similar | Report free of selective outcome reporting | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chen KW et al 2008 | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | 10/12 |
| An B et al 2008 | Unclear | Unclear | Yes | No | No | Unclear | No | No | Yes | Yes | Yes | Yes | 5/12 |
| Lee HJ et al 2009 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10/12 |
3.3. Effects of intervention
The effects of TCM intervention on knee OA (膝關節炎 xī guān jié yán) are summarized according to modality, namely acupuncture (Table 3), herbal patches (Table 4), herbs (Table 5), and qigong (Table 6).
3.3.1. Acupuncture treatment for OA
3.3.1.1. Acupuncture in pain control for OA
The eleven of 1210, 24, 26, 30, 31 studies have reported that acupuncture can reduce pain in patients with OA of the knee. Among these studies, nine (five high10, 21, 24, 25, 26 and four moderate quality23, 28, 29, 30) showed statistically significant pain reductions, and two (one high22 and one moderate quality31) showed non-significant pain reductions. One27 of 12 studies did not report a reduction in pain. Eight10, 21, 23, 24, 26, 28, 29, 30 of nine studies that showed statistically significant reductions in pain used the VAS or NRS for pain assessment and one25 study used the WOMAC pain scale.
Eight studies have demonstrated that acupuncture can significantly improve physical function in patients with knee OA.10, 22, 23, 24, 25, 26, 29, 30 Among these studies, five had high quality,10, 22, 24, 25, 26 and three had moderate quality.23, 29, 30 Seven (five high10, 22, 24, 25, 26 and two moderate23, 29 quality) of eight studies used the WOMAC for pain assessments. Only one30 of eight studies used gait analysis as its assessment for physical function.
3.3.2. Herbal patch
Only one high-quality study involving herbal patch treatment for OA was analyzed in our review.13 This study demonstrated that herbal patch treatment reduced pain and improved physical function, but these positive effects were not statistically significant. This study used the VAS for pain measurement and the WOMAC for functional assessment.
3.3.3. Herbs
Only one moderate-quality study involving the treatment of OA with herbs showed that herbs significantly reduced pain according to the VAS.23, 32 The other study involving herbal treatment of OA had low quality and did not show a significant pain reduction.21, 33
Regarding of physical function, the results were the same as those mentioned previously. Only one moderate-quality study on herbal therapy showed a significant increase in physical function according to the WOMAC.33
3.3.4. Qigong
Two studies showed a significant reduction in pain resulting from qigong treatment. One of these two studies provided high-quality evidence and used the McGill Pain Questionnaire as a pain scale.14 The other study provided low-quality evidence and used the WOMAC for pain measurement.34 One study35 included in this paper did not have an assessment of pain.
For improved physical function resulting from qigong treatment, one high-quality study showed an improvement in SF-36 and 6-m walking test significantly, but this improvement of WOMAC functional scale was not significant.35 Another high-quality study14 showed no improvement in physical function, and a low-quality study showed statistically significant improvements in physical function according to the WOMAC functional scale, 6-m walking test and ISKE (Isokinetic Strength of the Knee Extensors).34
3.4. Quality of evidence
Regarding the quality of evidence, no studies provided high-quality according to the GRADE criteria. Moderate-quality evidence supported reduced pain after a therapeutic course of acupuncture. Low-quality evidence supported improved function after acupuncture treatment or qigong. No evidence supported improved function after treatment with herbs or qigong. Because only one study regarding herbal patch treatment was analyzed, its quality of evidence could not be analyzed using the GRADE criteria (Table 11, Table 12, Table 13).
Table 11.
Acupuncture (針灸 zhēn jiǔ) for osteoarthritis of the knee (膝關節炎 xī guān jié yán) (GRADE).
| Number of studies | Design | Limitation | Inconsistency | Indirectness | Imprecision | Publication bias | Other considerations | Quality |
|---|---|---|---|---|---|---|---|---|
| Pain after treatment | ||||||||
| 12 | RCT | Serious limitationa | No serious inconsistencyb | No serious indirectnessc | No serious imprecision | Undetected | None | Moderate |
| Function after treatment | ||||||||
| 12 | RCT | Serious limitationa | Seriousd | No serious indirectnesse | No serious imprecision | Undetected | None | Low |
Three studies were unclear random sequence generation. Four were unclear allocation concealment. Two were inadequate Selection of participants to groups. Three were no intention-to-treat principle. Three were inadequate blinding. Only two studies did not have serious limitations.
Nine studies were consistent with acupuncture to relief pain after treatment and had significant differences. One study achieved pain release without significant differences. The results of two studies without serious limitations were no significant differences about pain release.
Five studies had similar populations (age, diagnosis and severity) but patients of twelve studies were all diagnosed osteoarthritis. Eight studies used VAS for estimate the pain of the knee and four used other method to evaluate the severity of the pain.
Seven studies were consistent with acupuncture to improve function and had significant differences. The others did not achieve improved function. One study without serious limitations had improved function with significant differences.
Five studies had similar populations (age, diagnosis and severity) and patients of twelve studies were all diagnosed osteoarthritis. Nine studies used WOMAC as their outcome measurement of the function of the knee.
Table 12.
Herbs for osteoarthritis of the knee (膝關節炎 xī guān jié yán) (GRADE).
| Number of studies | Design | Limitation | Inconsistency | Indirectness | Imprecision | Publication bias | Other considerations | Quality |
|---|---|---|---|---|---|---|---|---|
| Pain after treatment | ||||||||
| 2 | RCT | Serious limitationa | Serious inconsistencyb | Serious indirectnessc | Serious imprecisionc | Undetected | None | – |
| Function after treatment | ||||||||
| 2 | RCT | Serious limitationa | Serious inconsistencyd | Serious indirectnessc | Serious imprecisionc | Undetected | None | – |
Two studies had both unclear random sequence generation and allocation concealment.
Two studies both had decreased pain after treatment but no significant differences.
One study had no reliability and validity of the outcome measurement.
One study had improved function with statistic difference but the other without statistic difference.
Table 13.
Qigong (氣功 qì gōng) for osteoarthritis of the knee (膝關節炎 xī guān jié yán) (GRADE).
| Number of studies | Design | Limitation | Inconsistency | Indirectness | Imprecision | Publication bias | Other considerations | Quality |
|---|---|---|---|---|---|---|---|---|
| Pain after treatment | ||||||||
| 3 | RCT | Serious limitationa | Serious inconsistencyb | Serious indirectnessb | Serious imprecisionb | Undetected | None | – |
| Function after treatment | ||||||||
| 3 | RCT | Serious limitationa | No serious inconsistencyc | No serious indirectness | No serious imprecision | Undetected | None | Moderate |
One study had both unclear random sequence generation and allocation concealment. Two studies had no intention-to-treat analysis.
One study did not have pain score but had the WOMAC index that has a subscale of the pain scale. Two studies had decreased pain scale with significant differences.
Two studies had improved function without significant differences and one with significant differences.
4. Discussion
In this review, eighteen studies were included to determine the efficacy of TCM (中醫 zhōng yī) in patients with OA of the knee (膝關節炎 xī guān jié yán). We found that the studies involving acupuncture (針灸 zhēn jiǔ) and herbal patch (藥布 yào bù) treatments had lower risks of bias than those involving other TCM treatments. In addition, we found that studies involving acupuncture and herbal patch treatments had high methodological evidence regarding reduction of pain and improvement of physical function in patients with knee OA. By contrast, the risk of bias and quality of evidence regarding studies involving the application of herbal medicine for treating knee OA was inadequate because of methodological problems. No RCTs were conducted regarding the use of massage therapy (推拿 tuī ná) or moxibustion (艾灸 ài jiǔ), and RCTs should be developed for these treatments. Evidence regarding the effect of acupuncture on pain scores and the effect of qigong (氣功 qì gōng) on function scores was less conflicting.
Since the 1970s, acupuncture has become a prevalent therapy for pain.36, 37 In recent years, research has focused more on acupuncture than on other TCM treatments for pain control, and the quality of studies on acupuncture has improved. However, research on TCM therapies other than acupuncture for pain control remains insufficient. The results of our review show fewer RCTs on TCM, but acupuncture for treating knee OA pain could partially explain this phenomenon. In addition, most Chinese herbal medicines (中草藥 zhōng cǎo yào) are pure compounds, and few RCTs have applied herbal medicine and herbal patches to treat knee OA.34, 38 The decision to use acupuncture, massage therapy, or herbal medicine and patches for OA may correlate with the pathogenesis of OA and the aim of treatment. In general, acupuncture and massage therapy can alter muscle imbalance or fascial tension and reduce inflammation and pain in the early stages of OA,21, 23, 24, 26 whereas herbal medicines and patches can reduce inflammation locally but cannot alter abnormal alignment and the degenerative process.13, 32
4.1. Methodological considerations
Several factors contributed to a low quality of evidence or lack of evidence. Regarding acupuncture, three of 12 studies lacked clear random sequence generation, four lacked clear allocation concealment, two lacked adequate assignment of participants to groups, three lacked an intention-to-treat analysis, and three lacked adequate blinding. Only two studies did not have serious limitations. Although nine studies showed that acupuncture significantly relieved pain, two studies without serious limitations did not show significant pain relief following acupuncture. All patients in the 12 studies were diagnosed with OA, eight studies used the VAS as a pain scale, and four studies used the NRS to evaluate pain severity. Seven studies showed that acupuncture significantly improved physical function. The other studies did not show improved physical function. One study without serious limitations showed significantly improved physical function. The most critical study limitation among the analyzed studies was that most studies did not effectively explain processes for reducing bias.
Both studies on herbal medicine lacked clear random sequence generation and allocation concealment. Although both studies showed pain relief, neither could that show this pain relief was significant. Only one study showed significantly improved function. Currently, data are not sufficient to show a clear benefit of herbal medicine in patients with knee OA compared with controls.
Regarding qigong treatment, one of three studies lacked clear random sequence generation and allocation concealment, and two studies did not use an intention-to-treat analysis. One study did not determine a pain score, but used the WOMAC, which contains a subscale of the pain scale. Two studies showed that qigong treatment significantly reduced pain. Three studies showed improved physical function as a result of qigong treatment, but only one showed significantly improved physical function. According to our results, studies that showed improved physical function in patients treated with qigong had a moderate quality of evidence.
Regarding herbal patch treatment, only one study included random sequence generation and allocation concealment, but these processes were unclear. The bias was introduced. Although this study had a low risk of bias, more studies are required to eliminate the bias and increase the quality of evidence.
Despite 10 of 18 studies having high methodological quality (≧10/12), these studies were collectively flawed regarding random sequence generation, allocation concealment, compliance, and dropout rates. Our review findings were significantly influenced by these shortcomings. The quality of future RCTs must be improved to reduce bias in future reviews.
4.2. Review strengths and limitations
The literature search and selection procedure used in this review may have introduced bias. The literature search was conducted only in English, and only one database was used. Some RCTs may have been located in other databases or recorded in other languages. According to our selection procedure, the pathology of knee OA was not limited, and some patients developed OA as a result of trauma or infection rather than idiopathy or degeneration. These cases may have caused bias in our review. Patients with different demographics should be examined with caution.
Studies published after August 2013 or unpublished studies may have been omitted from our review. Using references from studies included in our review to identify other studies may have led to an overrepresentation of positive studies.
This review did not involve meta-analysis, and these studies should be divided into several categories according to various designs, for example, comparison between an experimental group and placebo or control groups, or comparison between an experimental group and standard treatment or control groups. If these studies were divided, we could compare them more effectively.
The studies included in our review were conducted between 1965 and 2013, and nearly all RCTs in the PubMed database involving TCM for knee OA were initially selected. After screening, 18 studies were included in our review.
4.3. Implications for health practice
OA of the knee is extremely prevalent among elderly people and interferes with their daily activities. Many elderly people cannot engage in daily activities including sports, shopping, and travel because of pain or the inability to walk. Furthermore, many elderly people visit hospitals or clinics because of pain and limited ranges of motion, causing a financial burden on the health care system in Taiwan. Current treatment options such NSAIDs, hyaluronic acid injection, and total knee arthroplasty are ineffective in treating OA. Glucosamine sulfate seems to be an alternative solution for treating OA, but evidence regarding its efficacy remains equivocal. TCM is another solution for treating OA.
According to our review, acupuncture seems to be effective for pain relief, and qigong seems effective for improving physical function. Only five papers10, 21, 24, 25, 26 have statistically significant about reducing pain and attach the high quality of methodological evidence. The usually used acupuncture points were local points including ST36, GB34, SP9, EX-LE5 (Xiyan), ST-35 (Dubi) and distant points are including LI4, SP6, KI3. The T'ai chi (太極拳 tài jí quán) is a low-impact, low-intensity and easy exercise with low drop-out rate, it can serve more activity for elderly patients with OA knee.35 Many mechanisms through which acupuncture exerts analgesic effects have been introduced. The major mechanisms that are currently accepted are the endogenous opiate mechanism and descending inhibitory mechanism.36, 39, 40 In support of this theory, evidence shows that the opioid antagonist naloxone blocks the analgesic effects of acupuncture.39, 41 Endogenous opioids are mediated by their μ, δ, and κ receptors, and the descending inhibitory pathway is mediated by its monoaminergic neurotransmitters and their receptors.42 In response to injury of the human body, the peripheral injury information is transmitted to substantia gelatinosa cells by primary afferent fibers, and the signal then ascends to the brain through the spinothalamic tract. Stimulation through EA could produce signals from the marginal cell tract that are transmitted to the brain through the spinothalamic tract.43, 44 Signals transmitted to the cortex and intrinsic dorsal neurons evoke cholinergic, ENKergic, and GABAergic neurons that can inhibit substantial gelatinosa cells.19, 36 The signal is then transmitted to the periaqueductal gray and nucleus raphe magnus to inhibit substantia gelatinosa cells by 5-HT. Another path from the cortex is the locus coeruleus. The signal from the locus coeruleus inhibits substantia gelatinosa cells and primary afferent fibers and enhances cholinergic, ENKergic, and GABAergic neurons through norepinephrine.36 Because these pathways originating from EA can inhibit nociceptive inputs from the periphery to higher areas in the CNS, acupuncture is useful for relieving pain.36
Qigong is effective for improving OA knee function and is the only treatment that requires moving patients' bodies and exercising their knee joints. Two of three qigong studies in our review involved – T'ai chi and Baduanjin (八段錦 bā duàn jǐn), and the other study involved external qigong therapy for which patients were not required to move their knees. T'ai chi and Baduanjin significantly improved function, but external qigong therapy did not significantly improve function. Compared with patients treated with acupuncture, patients treated with physical therapy had lower mean walking times, but this difference was nonsignificant.27 According to myofascial theory, pain from inflammation and friction of articular surfaces may induce muscle spasms around the joint, and the muscle spasms cause muscle ischemia. The ischemic soft tissue then causes more pain, which causes another muscle spasm.45, 46 Finally, a taut band and trigger point form, and the range of motion becomes limited. Limited range of motion and muscle spasms cause joint contractures and increase the difficulty of walking in elderly people. Low-impact, low-intensity exercise therapies, such as T'ai chi and Baduanjin, benefit elderly patients because these patients can stretch the muscles around the knees, such as the calf muscles and hamstrings, and break the pain-spasm-pain cycle.
Herbal medicine and patches are used to eliminate inflammation or improve circulation of the knees.13, 32 Park et al (2009) used AIF (Panax notoginseng (三七 sān qī), Rehmannia glutinosa Libosch (地黃 dì huáng), and Eleutherococcus senticosus (刺五加 cì wǔ jiā)) to treat OA knee and the VAS score and K-WOMAC decreased significantly. Li et al (2010) used recipe (Rhizoma Pinelliae (半夏 bàn xià), Arisaema cum Bile (膽南星 dǎn nán xīng), Rhizoma Chuanxiong (川芎 chuān xiōng), Radix Angelicae Sinensis (當歸 dāng guī), Radix Morindae Officinalis (巴戟天 bā jǐ tiān), Radix Paeoniae Alba (白芍 bái sháo), Rhizoma Atractylodis (蒼朮 cāng zhú), Rhizoma seu Radix Notopterygii (羌活 qiāng huó), Radix Angelicae Pubescentis (獨活 dú huó), Rhizoma Corydalis (延胡索 yán hú suǒ), Radix Astragali (黃耆 huáng qí) and Radix Achyranthis Bidentatae (懷牛膝 huái niú xī)) to heal OA knee and the decreased symptoms and effective rate were better in the treatment group but no statistic difference. Although these papers can improve symptoms, their quality evidence is no evidence and the methodological evidence is low to moderate.21, 23 The evidence regarding the effects of these therapies remains equivocal, and further study is required to prove their efficacy.
Other TCM therapies, such as massage therapy and manipulation, are oriental therapies, the effects of which can be studied further. We found that there were not many papers to study this area and we think this area needed to develop more rigorous studies. OA is a degenerative disease and always causes mal-alignment of the bone structure. In Taiwan, many elderly people with knee pain receive massage therapy and manipulation therapies to relieve pain and improve function. The mechanism of muscle spasm release involved in massage therapy and manipulation may be the same as that involved in active low-intensity muscle exercise, but massage therapy and manipulation are passive rather than active.
5. Conclusion
This was a systematic review investigating the evidence regarding TCM (中醫 zhōng yī) effectiveness in patients with OA of the knee (膝關節炎 xī guān jié yán). The initial findings of this review suggest that acupuncture (針灸 zhēn jiǔ) is a promising intervention according to the primary outcome measures of pain, and qigong (氣功 qì gōng) with motion is an effective method for treating physical function. However, based upon the GRADE criteria, the evidence for PNE is currently graded as moderate quality. This treatment approach should be investigated further to determine its most effective clinical use.
Conflict of interest
The authors have no conflicts of interest to declare.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
References
- 1.Buckwalter J.A., Mankin H.J. Articular cartilage: degeneration and osteoarthritis, repair, regeneration, and transplantation. Instr Course Lect. 1998;47:487–504. [PubMed] [Google Scholar]
- 2.Dequeker J., Luyten F.P. The history of osteoarthritis-osteoarthrosis. Ann Rheum Dis. Jan 2008;67:5–10. doi: 10.1136/ard.2007.079764. [DOI] [PubMed] [Google Scholar]
- 3.Felson D.T. Clinical practice. Osteoarthritis of the knee. N Engl J Med. Feb 23 2006;354:841–848. doi: 10.1056/NEJMcp051726. [DOI] [PubMed] [Google Scholar]
- 4.Pelletier J.P., Martel-Pelletier J., Abramson S.B. Osteoarthritis, an inflammatory disease: potential implication for the selection of new therapeutic targets. Arthritis Rheum. Jun 2001;44:1237–1247. doi: 10.1002/1529-0131(200106)44:6<1237::AID-ART214>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 5.Zhang Y., Jordan J.M. Epidemiology of osteoarthritis. Clin Geriatr Med. Aug 2010;26:355–369. doi: 10.1016/j.cger.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arden N., Nevitt M.C. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol. Feb 2006;20:3–25. doi: 10.1016/j.berh.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Goldring S.R., Goldring M.B. Clinical aspects, pathology and pathophysiology of osteoarthritis. J Musculoskelet Neuronal Interact. Oct–Dec 2006;6:376–378. [PubMed] [Google Scholar]
- 8.McAlindon T.E., Bannuru R.R., Sullivan M.C. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage/OARS, Osteoarthritis Research Society. Mar 2014;22:363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Regional Office for the Western P . World Health Organization; Manila, Philippines: 2007. WHO International Standard Terminologies on Traditional Medicine in the Western Pacific Region. Western Pacific Region. [Google Scholar]
- 10.Mavrommatis C.I., Argyra E., Vadalouka A., Vasilakos D.G. Acupuncture as an adjunctive therapy to pharmacological treatment in patients with chronic pain due to osteoarthritis of the knee: a 3-armed, randomized, placebo-controlled trial. Pain. Aug 2012;153:1720–1726. doi: 10.1016/j.pain.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Lai J.N., Chen H.J., Chen C.C., Lin J.H., Hwang J.S., Wang J.D. Duhuo jisheng tang for treating osteoarthritis of the knee: a prospective clinical observation. Chin Med. 2007;2:4. doi: 10.1186/1749-8546-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee S., Kim K.H., Kim T.H. Moxibustion for treating knee osteoarthritis: study protocol of a multicentre randomised controlled trial. BMC Complement Altern Med. 2013 Mar 13;13:59. doi: 10.1186/1472-6882-13-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang X., Cao Y., Pang J. Traditional chinese herbal patch for short-term management of knee osteoarthritis: a randomized, double-blind, placebo-controlled trial. Evid Based Complement Altern Med: eCAM. 2012;2012:171706. doi: 10.1155/2012/171706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen K.W., Perlman A., Liao J.G., Lam A., Staller J., Sigal L.H. Effects of external qigong therapy on osteoarthritis of the knee. A randomized controlled trial. Clin Rheumatol. 2008 Dec;27:1497–1505. doi: 10.1007/s10067-008-0955-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Y1 Cao, Zhan H., Pang J. Individually integrated traditional Chinese medicine approach in the management of knee osteoarthritis: study protocol for a randomized controlled trial. Trials. 2011 Jun 22;12:160. doi: 10.1186/1745-6215-12-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liddle S.D., Gracey J.H., Baxter G.D. Advice for the management of low back pain: a systematic review of randomised controlled trials. Man Ther. Nov 2007;12:310–327. doi: 10.1016/j.math.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Clarke C.L., Ryan C.G., Martin D.J. Pain neurophysiology education for the management of individuals with chronic low back pain: systematic review and meta-analysis. Man Ther. Dec 2011;16:544–549. doi: 10.1016/j.math.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Sodha R., Sivanadarajah N., Alam M. The use of glucosamine for chronic low back pain: a systematic review of randomised control trials. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2012-001167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baba H., Shimoji K., Yoshimura M. Norepinephrine facilitates inhibitory transmission in substantia gelatinosa of adult rat spinal cord (Part 1) effects on axon terminals of GABAergic and glycinergic neurons. J Am Soc Anesthesiol. 2000;92:473–484. doi: 10.1097/00000542-200002000-00030. [DOI] [PubMed] [Google Scholar]
- 20.Furlan A.D., Pennick V., Bombardier C., van Tulder M. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine. Aug 15 2009;34:1929–1941. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 21.Ng M.M., Leung M.C., Poon D.M. The effects of electro-acupuncture and transcutaneous electrical nerve stimulation on patients with painful osteoarthritic knees: a randomized controlled trial with follow-up evaluation. J Altern Complement Med. Oct 2003;9:641–649. doi: 10.1089/107555303322524490. [DOI] [PubMed] [Google Scholar]
- 22.Berman B.M., Lao L., Langenberg P., Lee W.L., Gilpin A.M., Hochberg M.C. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. Dec 21 2004;141:901–910. doi: 10.7326/0003-4819-141-12-200412210-00006. [DOI] [PubMed] [Google Scholar]
- 23.Tukmachi E., Jubb R., Dempsey E., Jones P. The effect of acupuncture on the symptoms of knee osteoarthritis–an open randomised controlled study. Acupunct Med: journal of the British Medical Acupuncture Society. Mar 2004;22:14–22. doi: 10.1136/aim.22.1.14. [DOI] [PubMed] [Google Scholar]
- 24.Vas J., Mendez C., Perea-Milla E. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. BMJ. Nov 20 2004;329:1216. doi: 10.1136/bmj.38238.601447.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Witt C., Brinkhaus B., Jena S. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. Jul 9-15 2005;366:136–143. doi: 10.1016/S0140-6736(05)66871-7. [DOI] [PubMed] [Google Scholar]
- 26.Scharf H.P., Mansmann U., Streitberger K. Acupuncture and knee osteoarthritis: a three-armed randomized trial. Ann Intern Med. Jul 4 2006;145:12–20. doi: 10.7326/0003-4819-145-1-200607040-00005. [DOI] [PubMed] [Google Scholar]
- 27.Williamson L., Wyatt M.R., Yein K., Melton J.T. Severe knee osteoarthritis: a randomized controlled trial of acupuncture, physiotherapy (supervised exercise) and standard management for patients awaiting knee replacement. Rheumatology (Oxford) Sep 2007;46:1445–1449. doi: 10.1093/rheumatology/kem119. [DOI] [PubMed] [Google Scholar]
- 28.Jubb R.W., Tukmachi E.S., Jones P.W., Dempsey E., Waterhouse L., Brailsford S. A blinded randomised trial of acupuncture (manual and electroacupuncture) compared with a non-penetrating sham for the symptoms of osteoarthritis of the knee. Acupunct Med: journal of the British Medical Acupuncture Society. Jun 2008;26:69–78. doi: 10.1136/aim.26.2.69. [DOI] [PubMed] [Google Scholar]
- 29.Itoh K., Hirota S., Katsumi Y., Ochi H., Kitakoji H. Trigger point acupuncture for treatment of knee osteoarthritis – a preliminary RCT for a pragmatic trial. Acupunct Med: journal of the British Medical Acupuncture Society. Mar 2008;26:17–26. doi: 10.1136/aim.26.1.17. [DOI] [PubMed] [Google Scholar]
- 30.Lu T.W., Wei I.P., Liu Y.H. Immediate effects of acupuncture on gait patterns in patients with knee osteoarthritis. Chin Med J. Jan 20 2010;123:165–172. [PubMed] [Google Scholar]
- 31.Soni A., Joshi A., Mudge N., Wyatt M., Williamson L. Supervised exercise plus acupuncture for moderate to severe knee osteoarthritis: a small randomised controlled trial. Acupunct Med: journal of the British Medical Acupuncture Society. Sep 2012;30:176–181. doi: 10.1136/acupmed-2012-010128. [DOI] [PubMed] [Google Scholar]
- 32.Park S.H., Kim S.K., Shin I.H., Kim H.G., Choe J.Y. Effects of AIF on knee osteoarthritis patients: double-blind, randomized placebo-controlled study. Korean J Physiol Pharmacol: official journal of the Korean Physiological Society and the Korean Society of Pharmacology. Feb 2009;13:33–37. doi: 10.4196/kjpp.2009.13.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li X.H., Liang W.N., Liu X.X. Clinical observation on curative effect of dissolving phlegm-stasis on 50 cases of knee osteoarthritis. J Tradit Chin Med = Chung i tsa chih ying wen pan/sponsored by All-China Association of Traditional Chinese Medicine, Academy of Traditional Chinese Medicine. Jun 2010;30:108–112. doi: 10.1016/s0254-6272(10)60024-6. [DOI] [PubMed] [Google Scholar]
- 34.An B., Dai K., Zhu Z. Baduanjin alleviates the symptoms of knee osteoarthritis. J Altern Complement Med. Mar 2008;14:167–174. doi: 10.1089/acm.2007.0600. [DOI] [PubMed] [Google Scholar]
- 35.Lee H.J., Park H.J., Chae Y. Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: a pilot, randomized, waiting list controlled trial. Clin Rehabil. Jun 2009;23:504–511. doi: 10.1177/0269215508101746. [DOI] [PubMed] [Google Scholar]
- 36.Kim W., Kim S.K., Min B.I. Mechanisms of electroacupuncture-induced analgesia on neuropathic pain in animal model. Evid Based Complement Alternat Med: eCAM. 2013;2013:436913. doi: 10.1155/2013/436913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization. Regional Office for the Western Pacific . World Health Organization; 2002. Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials; p. 81. [Google Scholar]
- 38.Lechner M., Steirer I., Brinkhaus B. Efficacy of individualized Chinese herbal medication in osteoarthrosis of hip and knee: a double-blind, randomized-controlled clinical study. J Altern Complement Med. Jun 2011;17:539–547. doi: 10.1089/acm.2010.0602. [DOI] [PubMed] [Google Scholar]
- 39.Pomeranz B., Chiu D. Naloxone blockade of acupuncture analgesia: endorphin implicated. Life Sci. Dec 1 1976;19:1757–1762. doi: 10.1016/0024-3205(76)90084-9. [DOI] [PubMed] [Google Scholar]
- 40.Takeshige C., Sato T., Mera T., Hisamitsu T., Fang J. Descending pain inhibitory system involved in acupuncture analgesia. Brain Res Bull. Nov 1992:617–634. doi: 10.1016/0361-9230(92)90131-g. [DOI] [PubMed] [Google Scholar]
- 41.Mayer D.J., Price D.D., Rafii A. Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone. Brain Res. Feb 1977;121:368–372. doi: 10.1016/0006-8993(77)90161-5. [DOI] [PubMed] [Google Scholar]
- 42.Ho K.Y., Tay W., Yeo M.C. Duloxetine reduces morphine requirements after knee replacement surgery. Br J Anaesth. Sep 2010;105:371–376. doi: 10.1093/bja/aeq158. [DOI] [PubMed] [Google Scholar]
- 43.Alexander G.M., Peterlin B.L., Perreault M.J., Grothusen J.R., Schwartzman R.J. Changes in plasma cytokines and their soluble receptors in complex regional pain syndrome. J Pain: official journal of the American Pain Society. Jan 2012;13:10–20. doi: 10.1016/j.jpain.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 44.Bing Z., Cesselin F., Bourgoin S., Clot A.M., Hamon M., Le Bars D. Acupuncture-like stimulation induces a heterosegmental release of Met-enkephalin-like material in the rat spinal cord. Pain. Oct 1991;47:71–77. doi: 10.1016/0304-3959(91)90013-N. [DOI] [PubMed] [Google Scholar]
- 45.Travell J., Rinzler S., Herman M. Pain and disability of the shoulder and arm: treatment by intramuscular infiltration with procaine hydrochloride. J Am Med Assoc. 1942;120:417–422. [Google Scholar]
- 46.Johansson H., Sojka P. Pathophysiological mechanisms involved in genesis and spread of muscular tension in occupational muscle pain and in chronic musculoskeletal pain syndromes: a hypothesis. Med Hypotheses. Jul 1991;35:196–203. doi: 10.1016/0306-9877(91)90233-o. [DOI] [PubMed] [Google Scholar]