Abstract
Herbal medicine, the backbone of traditional medicine, has played an important role in human health and welfare for a long period. Traditional therapeutic approaches of regional significance are found in Africa, South and Central America, China, India, Tibet, Indonesia, and the Pacific Islands. The considerable scientific significance and commercial potential of traditional medicines have resulted in increased international attention and global market demands for herbal medicines, especially Chinese herbal medicines. Herbal medicines currently are the primary form of health care for the poor in the developing countries, and also are widely used as a supplement or substitute for conventional drugs in developed countries. These traditional medicines have a pivotal role in the treatment of various ailments and more than 50% of drugs used in Western pharmacopoeia are isolated from herbs or derived from modifications of chemicals found in plants. Herbal medicines usually contain a complex mixture of various bioactive molecules, which make its standardization complicated, and there is little information about all compounds responsible for pharmacological activity. Several research papers have been published that claim pharmacological activity of herbal medicines but few are discussing the role of the exact phytoconstituent. Understanding the pharmacokinetic profile of such phytoconstituents is essential. Although there are research papers that deal with pharmacokinetic properties of phytoconstituents, there are a number of phytoconstituents yet to be explored for their kinetic properties. This article reviews the pharmacokinetic profile of 50 different therapeutically effective traditional medicinal plants from the year 2003 onward.
Keywords: Pharmacokinetics, Phytoconstituents, Traditional Chinese medicines (TCM), Traditional medicinal systems (TMS), ADME
Graphical abstract
1. Introduction
Herbal medicines are known to have a strong reputation throughout history and within every culture to provide first-line and basic health services for patients with numerous disease conditions. The roots of herbal medicine are at the very beginning of human history. These are the oldest form of medicine for welfare of mankind, and they play a paramount role in culture-specific traditional medicinal systems (TMS), i.e., Ayurveda (India) and traditional Chinese medicine (China). Herbal medicine is an umbrella term that encompasses an array of treatment options to supplement conventional and nonconventional therapies. Herbal medicine approaches are completely different from modern orthodox medicines. The historical background of herbal medicine begins with ethnopharmacology, a term introduced in 1967, which mainly deals with the scientific study of the traditional medicinal plants. It can be defined as ʻthe scientific study of materials used by ethnic and cultural groups as medicinesʼ and in most instances this is synonymous with the study of traditional medicine.1 Phytochemicals, phytomedicine, natural remedies, natural products and their chemistry, and various other subjects are present in the realm of herbal medicines and are beyond the scope of this article. Basically, medicinal plants are a huge source of chemical compounds, including primary and secondary metabolites, alkaloids, flavonoids, and lignin. These medicinal plants and their extracts yield promising leads (active principals) to further strengthen the medicinal system. These natural bioactive compounds play a central role in combating many human diseases. More than 50% of drugs used in Western pharmacopoeia are isolated from herbs or derived from modification of phytoconstituents.2 Recent studies have stated that 75–90% (developing world) and 80% (less developed/developing countries) of the current world population relies on the use of herbal medicines for their primary health care and other needs, which signifies the scope of TMS, where 85% of medicinal plants of TMS involve the use of plant extracts.3, 4 These phytochemicals show a more complex pharmacokinetic profile (the study of the time course of phytochemicals, absorption, distribution, metabolism, and excretion). This pharmacokinetic profile helps to elaborate the relationship between intensity and time course of pharmacology, the toxicological effects of phytochemicals in the human body, and extends the scope of the use and acceptance by different regulatory bodies. As pointed out by the World Health Organization, there is very limited knowledge about the chemical compositions, pharmacokinetics, pharmacodynamics, and metabolomics of TCM plants; the data about authentication, efficacy, and safety of TCM are known and are far from satisfactory to meet the required criteria for worldwide use.5 To provide satisfactory data about safety and efficacy of these medicinal plants and for pharmacokinetic profile, we have gathered information from various search engines and other possible sources from 2003 onward to provide a detailed picture on ADME parameters (absorption, distribution, metabolism, and excretion) of some phytoconstituents. The review elaborates pharmacokinetic profile of 50 medicinally important phytoconstituents from different medicinal plants.
2. Pharmacokinetic profile of drugs
2.1. Ammi visnaga L. (阿密茴香 ē mì huí xiāng)
Visnagin is a furanocoumarins derivative and one of the major constituents in Ammi visnaga L. (Apiaceae). It is commonly known as Khella. It was used by ancient Egyptians as a treatment for kidney stone disease. Visnagin has cardiovascular effects due to calcium channel blocking actions. Visnagin also has negative chronotropic and inotropic effects and reduces peripheral vascular resistance. Its extract prevents urolithiasis (kidney stone formation) by decreasing calcium oxalate crystal growth in the stone-forming rat model.
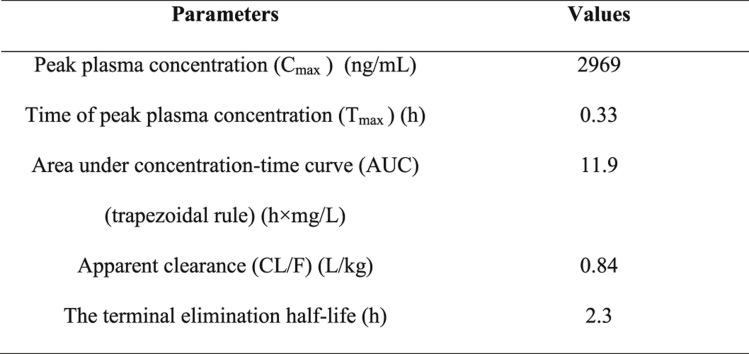
A sensitive and highly selective liquid chromatography-tandem mass spectrometry (LC-MS) method was used to determine visnagin in rat plasma. Chromatography was performed on a Phenomenex Synergi Max RP, (75 × 2.0 mm internal diameter [i.d.], 4 μm, Torrance, CA, USA) analytical column at ambient temperature. The mobile phase used for analysis was 0.1% formic acid, 5mM ammonium acetate in deionized water and methanol (15:85, v/v) delivered at a flow rate of 0.2 mL/min. For quantitative determination of visnagin in a rat plasma, a 50-μL sample is required. Pharmacokinetic parameters after oral administration of visnagin are provided in Table 1.6
Table 1.
Pharmacokinetic parameters after oral administration of visnagin.
| Parameters | Values |
|---|---|
| Peak plasma concentration (Cmax) (ng/mL) | 2969 |
| Time of peak plasma concentration (Tmax) (h) | 0.33 |
| Area under the concentration-time curve) (trapezoidal rule) (h × mg/L) | 11.9 |
| Apparent clearance (CL/F) (L/kg) | 0.84 |
| The terminal elimination half-life (h) | 2.3 |
2.2. Apium graveolens, Ligusticum sinensis, and Ligusticum wallichii (芹菜 qín cài), Ligusticum sinensis (藁本 gǎo běn) and Ligusticum wallichii (川芎 chuān xiōng)
3-n-Butylphthalide is a volatile chemical present in several plants including Apium graveolens, Ligusticum sinensis, and Ligusticum wallichii. In China 3-n-butylphthalide [(±)-NBP] may be a promising new drug for the treatment of ischemic cerebral diseases, such as stroke.
A high-performance liquid chromatography (HPLC)-mass spectrometry (MS)/MS with positive ionization mode was adopted to determine 3-n-butylphthalide in rat plasma. The system was equipped with an ACQUITY UPLCTM BEH C18 (50 × 2.1 mm i.d., 1.7 μm) column. Gradient mobile phase composed of acetonitrile (ACN) and water containing 0.1% formic acid was used. The separated compounds were detected by a Waters Tandem Quadrupole (TQ) Detector (Waters, Milford, MA). The column temperature, flow rate, and chromatographic run time per sample used was 35°C, 0.2 mL/min, and 3.0 minutes, respectively. The lower limit of quantification (LLOQ) value was 5.57 ng/mL. Pharmacokinetic parameters after intravenous administration of 3-n-butylphthalide (5 mg/kg) are provided in Table 2.7 3-n-Butylphthalide followed extensive metabolism in humans and produced four metabolites, i.e., 10-keto-NBP, 3-hydroxy-NBP, 10-hydroxy-NBP, and NBP-11-oic acid.8
Table 2.
Pharmacokinetic parameter of 3-n-butylphthalide after intravenous administration dose 5 mg/kg.
| Parameter | Values |
|---|---|
| AUC0-6h (ng·h/mL) | 1140.16 |
| Apparent volume of distribution (Vc) (L/kg) | 1.22 |
| Half-life (t1/2) (distribution) (h) | 0.098 |
| t1/2 (elimination) (h) | 2.62 |
| Clearance (Cl) (L/h kg) | 3.67 |
AUC = area under the concentration-time curve.
2.3. Atractylodes macrocephala Koidz (白朮 bái zhú)
Atractylodes macrocephala Koidz is one of the TCMs listed in Chinese pharmacopoeia. It exhibits antitumor, anti-inflammatory, and antibacterial properties. The anticancer effect of atractylenolide I has been proved in different cancer cells.
The HPLC-MS/MS method was reported for quantification of atractylenolide I in Wistar rat plasma after oral administration of the ethanolic (95%) extract of atractylodis. The MS was operated in the positive electrospray ionization (ESI) mode with multiple reaction monitoring (MRM). The LC system was equipped with a Phenomenex Gemini column (2.0 × 50 mm i.d., 5 μm, Phenomenex Company, CA, USA). The mobile phase consisted of a mixture of 0.1% formic acid in water and 0.1% formic acid in methanol. The flow rate was set at 0.4 mL/min, and column temperature and injection volume are 25°C and 10 μL, respectively. The limit of detection (LOD) and the limit of quantification (LOQ) are 0.6 ng/mL and 2.0 ng/mL, respectively. The pharmacokinetic parameters of atractylenolide I after oral administration of ethanolic (95%) atractylodis extract are presented in Table 3. The pharmacokinetic data indicate that atractylenolide I was absorbed very quickly in the body.
Table 3.
Pharmacokinetic parameters of atractylenolide I after oral administration of Atractylodis extract (20 g/kg) to rats (n = 6, mean ± standard deviation).
| Parameters | Values |
|---|---|
| Elimination rate constant (Ke) (/h) | 0.365 ± 0.06 |
| AUC0-T (μg h/L) | 22.2 ± 1.9 |
| AUC0-∞ (μg h/L) | 22.6 ± 1.8 |
| Tmax (h) | 0.81 ± 0.11 |
| Cmax (μg/L) | 7.99 ± 1.2 |
| Vc (l/kg) | 2768.6 ± 751.5 |
| Cl (l/h/kg) | 978.2 ± 117.3 |
| t1/2 (h) | 1.94 ± 0.27 |
AUC = area under the concentration-time curve; Cl = clearance; Cmax = peak plasma concentration; Tmax = time of peak plasma concentration.
When simultaneous determination for atractylenolide I, II, and III was performed in blank rat plasma, atractylenolide II was found in real samples, atractylenolide III was found in plasma at different time points, and the pharmacokinetic curve of atractylenolide III showed an irregular pattern.9
2.4. Artemisia annua L. (黃花蒿 huáng huā hāo)
Artemisia annua L. (annual wormwood) contains the antimalarial artemisinin. Aqueous preparations of the dried herb are included in the pharmacopoeia of the People's Republic of China for the treatment of fever and malaria.
A reverse-phase HPLC was used to determine artemisinin in blood samples of healthy male volunteers receiving 9 g of Artemisia annua L. The system is equipped with 250 × 4.6 mm Multophere RP-18, 5-μm column (Chromatography Service, Langenwehe, Germany). A linear gradient of 45–100% acetonitrile in water (20 minutes, 1 mL/min) was used. For online postcolumn derivatization, 0.3 M aqueous potassium hydroxide was added to the elute at a rate of 0.2 mL/min. The resulting mixture was passed through a 5-m steel capillary (0.5 mm internal diameter) immersed in a water bath of 70°C. Ultraviolet absorption was monitored at 289 nm. The pharmacokinetic parameters of artemisinin are provided in Table 4. The overall picture of pharmacokinetic data revealed that artemisinin plasma concentrations after intake of the given herbal tea are sufficient for clinical effects, but insufficient to recommend such preparations as equivalent substitutes for modern artemisinin drugs in malaria therapy.10
Table 4.
Pharmacokinetic parameters of artemisinin.
| Parameter | Values |
|---|---|
| Mean ± SD (ng/mL) (Maximum plasma concentration of artemisinin) | 240 ± 75 |
| Mean ± SD (ng/mL × h) (Area under the plasma concentration-time curve) | 336 ± 71 |
| Tmax (h) | 0.6 ± 0.2 |
| t1/2 (h) | 0.9 ± 0.2 |
SD = standard deviation; Tmax = time of peak plasma concentration.
2.5. Aristolochia fangchi (防己馬兜鈴 fáng jǐ mǎ dōu líng)
Aristolochic acids (AAs) are found primarily in the plant genera Aristolochia and Asarum. AAs exhibit anti-inflammatory, antitussive, and antiplatelet aggregation pharmacologic properties and they are also used as pain relievers. AAs have proved to be the major components that cause renal fibrosis problems. AAs are a mixture of structural-related 10-nitrophenanthrene 1-carboxylic acids, where AAI, the 8-methoxy-3,4- methylene dioxy derivative, and AAII, the 3,4-methylenedioxy derivative, are the major components in the Aristolochia species.
Ultra high-performance liquid chromatography (UHPLC)-MS/MS with a Quatro Micro triple-quadrupole mass spectrometer (Micromass, Manchester, UK) operating at positive ion electrospray mode has been reported to determine the pharmacokinetic parameters. The system was equipped with an Acquity BEH C18 column (100 × 2.1 mm i.d., 1.7 μm, Waters) for separation of aristolochic acids. The mobile phase was composed of 10mM ammonium formaten (pH 3.0) (solvent A) and ACN (solvent B). The gradient profile was 0–2 min: 34% B; 2–10.5 min: linear from 34% to 36% B; 10.5–10.6 min: linear from 36% to 34% B and then re-equilibrium of the column. The flow rate was kept at 0.3 mL/min. The column oven and autoinjection system are set at 40°C and 4°C respectively. Partial loop with needle over fill mode was used for sample injection, and the injection volume was 5 μL. The LOD was 0.14 ng/mL for AAI and 0.26 ng/mL for AAII. The pharmacokinetic parameters after single oral administration of 10 mg/kg standard in female Wistar rats are presented in Table 5.
Table 5.
Pharmacokinetic parameters after single oral administration of 10 mg/kg standard in female Wister rats.
| Parameter | AAI | AAII |
|---|---|---|
| T max (min) | 30 | 45 |
| C max (ng/mL−1) | 7249.3 | 77.7 |
| AUC (ng/mL−1 min) | 716,936.3 | 31,344.8 |
| t1/2 (min) | 234.6 | 800.7 |
| Rate constant (k) (min−1) | 0.003 | 0.0009 |
| Oral clearance (mL/min−1) | 2.9 | 66.0 |
AA = aristolochic acid; AUC = area under the concentration-time curve; Cmax = peak plasma concentration; Tmax = time of peak plasma concentration.
The pharmacokinetic data revealed that AAs could be quickly absorbed in the gastro-intestinal tract. The hepatic enzymes P450 1A1 and 1A2 help to detoxify AAI through the metabolism of AAI into less toxic metabolites aristolactam I (AL I).11
2.6. Anemarrhena asphodeloides (知母 zhī mǔ)
The Chinese herb named as Zhi-Mu, mangiferin (2-b-d-glucopyranosyl-1,3,6,7-tetrahydroxyxanthen-9-one) has been isolated from the herbal root of Anemarrhena asphodeloides Bung showing antioxidant, antiviral, and anticancer activity.
A HPLC tandem MS with in vivo microdialysis sampling method was used for continuous monitoring of free mangiferin in rat blood. Mangiferin was separated by a reverse-phase C microbore column (15031 mm) from dialysate within 10 minutes. The mobile phase consisted of 18 acetonitrile-0.05% phosphoric acid-tetrahydrofuran (10:75:15, v/v/v) with a flow rate of 0.05 mL/min. The wavelength of the UV detector was set at 257 nm. The LOQ and retention time are 0.05 mg/mL and 6.0 minutes, respectively. The pharmacokinetic parameters for mangiferin are provided in Table 6. The study results revealed that mangiferin cannot cross the blood-brain barrier because it was not detected in the bile and brain for all dosage treatments. Mangiferin metabolites are formed by methylation and phase II sulfation and glucuronidation are found in rat bile.12
Table 6.
Pharmacokinetic parameters following mangiferin administration (10, 30, and 100 mg/kg, intravenously) (± = 6).
| Parameters | 10 mg/kg | 30 mg/kg | 100 mg/kg |
|---|---|---|---|
| AUC (min mg/mL) | 122.9617.1 | 452.5639.8 | 2424.26196.7a |
| Half-life of slow distribution phase (t 1/2β) (min) | 28.563.5 | 35.063.5 | 47.864.1* 1/2,b |
| Steady-state volume of distribution (Vss) (L/kg) | 3.060.3 | 2.560.3 | 2.060.3 ss |
| Cl (mL/min/kg) | 90.161 2.6 | 69.166.5 | 43.264.3* |
| Mean residence time (min) | 35.062.52 | 35.962.8 | 45.864.8* |
AUC = area under the concentration-time curve; Cl = clearance.
* Denotes the, significantly different (p = 0.05) from the dose of 10 and 30 mg/kg (Student's t test) and SS denotes the steady-state.
Significantly different (p = 0.05) from the dose of 10 and 30 mg/kg (Student t test).
2.7. Baphicacanthus cusia (Nees) Bremek. (馬藍 mǎ lán), Polygonum tinctorium Ait. (蓼藍 liǎo lán) and Isatis indigotica Fort. (菘藍 sōng lán)13
Indirubin, a 3,20-bisindole isomer of indigo, exists in several medicinal plants such as Baphicacanthus cusia (Nees) Bremek, Polygonum tinctorium Ait., and Isatis indigotica Fort. It is one of the compounds that exhibits antileukemic action more specifically effective against chronic granulocytic leukemia. In addition, it is useful as an antiproliferative and an anti-inflammatory agent.
HPLC was adopted to determine the pharmacokinetic parameters of indirubin in a rat after intravenous and intraperitoneal administration. It was equipped with a Zirchrom Kromasil ODS column (200 × 4.6 mm i.d., 5 mm) and protected by a guard column (Phenomenex Security Guard TM, ODS, 4 × 3.0 mm, Cheshire, UK). The mobile phase contains a mixture of methanol-water (75:25, v/v). The flow rate and wavelength for detection are 1 mL/min and 289 nm at room temperature, respectively. The LLOQ was found to be 6.5 ng/mL. The mean pharmacokinetic parameters of indirubin after intravenous injections and intraperitoneal injections at doses 2.8, 5.6, and 5.6 mg/kg, respectively, in rats are provided in Table 7. The parent molecule of indirubin metabolized and excreted fast as compared with its metabolites. Indirubin showed a relatively low bioavailability of 8.40% in rats when it was intraperitoneally administered, and to enhance its therapeutic efficacy design of appropriate dosage form or delivery system or structural modification may be required.
Table 7.
Mean pharmacokinetic parameters of indirubin after intravenous injections at doses of 5.6 and 2.8 mg/kg and intraperitoneal injections at dose of 5.6 mg/kg in rats.
| Parameters | Doses |
||
|---|---|---|---|
| 5.6 mg/kg (i.v.) | 2.8 mg/kg (i.v.) | 5.6 mg/kg (i.p.) | |
| AUC0–N (ng h/mL) | 308 ± 750.0 | 130 ± 748.3 | 25.9 ± 74.9 |
| AUC0–t (ng h/mL) | 295 ± 745.2 | 124 ± 7 43.3 | 22.6 ± 75.2 |
| Cmax (ng/mL) | 201 ± 723.7 | 155 ± 717.7 | 20.87 ± 7.6 |
| Tmax (h) | 0.017 | 0.017 | 0.010 |
| Ke (h−1) | 0.670 ± 70.2 | 0.6837 ± 0.2 | 0.6407 ± 0.5 |
| t1/2 (h) | 1.0307 ± 0.2 | 1.0207 ± 0.2 | 1.08070 ± .4 |
| MRT (h) | 1.7507 ± 0.3 | 1.5107 ± 0 .3 | 0.7777 ± 1.1 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; i.p. = intraperitoneal; i.v. = intravenous; MRT = mean residence time; Tmax = time of peak plasma concentration.
2.8. Cudrania tricuspidata (Carr.) Bur. (柘樹 zhè shù)
Cudrania tricuspidata (Carr.) Bur. is a deciduous shrub or tree distributed over China, Korea, and Japan. The root of the plant is used for gastric carcinoma. Among the active compounds, cudratricusxanthone B (CXB) is found to be the most promising.
A HPLC-ESI-tandem MS was used to evaluate the pharmacokinetic characteristics of CXB after intravenous administration in the rat. The system was equipped with a Venusil XBP-PH C18 column (2.1 × 100 mm i.d., 5 μm) coupled with a Phenomenex C18 guard column (4.0 × 3.0 mm i.d., 5 μm) and the temperature was set at 40°C. The mobile phase was 0.5% formic acid in methanol at a flow rate of 0.3 mL/min. Acquisition of MS data for CXB and Internal standards was performed in positive ionization mode. The study used 5.0 mg/kg CXB in rats, which was administered via the tail vein. Blood samples (about 50 μL at 0.083 and 0.25 h, and about 200 μL at other points) are drawn from the retro-orbital plexus before dosing and at 0.083, 0.25, 0.5, 1, 2, 3, 4, 6, 9, 15, and 24 hours after dosing. The compartment model for pharmacokinetic parameters of CXB was chosen according to the lowest Akaike information criterion (AIC) value. The (AUC0-t) and infinity (AUC0-∞) are calculated using the linear trapezoidal rule with a noncompartment model, and other parameters are estimated with a three-compartment model. The method was sensitive with an LLOQ at 1.0 ng/mL for CXB using 100 μL of rat plasma. The pharmacokinetic parameters of CXB after a single intravenous administration are given in Table 8. CXB after a single intravenous administration indicate the rapid distribution followed by a slow elimination.14
Table 8.
The main pharmacokinetic parameters of CXB after a single intravenous administration of 5.0 mg/kg CXB in six male rats.
| Parameter | Value |
|---|---|
| Vc (L/kg) | 2.60 ± 1.88 |
| t1/2 pi (h) | 0.109 ± 0.058 |
| Half-life of rapid distribution phase (t1/2 α) (h) | 0.503 ± 0.173 |
| t1/2 β (h) | 8.17 ± 0.99 |
| K12 (1/h) | 1.38 ± 1.36 |
| k21 (1/h) | 2.24 ± 1.77 |
| k13 (1/h) | 1.17 ± 0.178 |
| k31 (1/h) | 0.113 ± 0.021 |
| k10 (1/h) | 4.53 ± 1.65 |
| Cl (L/kg/h) | 9.52 ± 1.73 |
| AUC0–t (ng h/mL) | 566.0 ± 76.4 |
| AUC0–∞ (ng h/mL) | 583.1 ± 79.7 |
AUC = area under the concentration-time curve; Cl = clearance.
2.9. Citrus depressa (Shiikuwasha) (扁實檸檬 biǎn shí níng méng), Citrus sinensis (oranges) (甜橙 tián chéng) and Citrus limon (lemons) (檸檬 níng méng)
Nobiletin (3′,4′,5,6,7,8,-hexamethoxyflavone) is a polymethoxylated flavone commonly found in citrus fruit peels such as Citrus depressa (shiikuwasa), Citrus sinensis (oranges), and Citrus limon (lemons). Nobiletin exhibits a wide range of activities such as anti-inflammatory, antitumor proliferation, antitumor invasion, and neuroprotective properties and also is helpful in treating Alzheimer disease. In addition, nobiletin also improves hyperglycemia, insulin resistance, and atherosclerosis. Nobiletin substantially improve oral bioavailability in comparison with other polyhydroxylated flavonoids.
HPLC coupled with Photodiode Array Detector (PDA) was used to quantification of nobiletin in rat plasma and brain tissue. The system was equipped with Lichro CART RP18 column (4.6 × 250 mm i.d., 5.0 μm). The system was run in isocratic mode with mobile phase consisting of potassium dihydrogen orthophosphate (pH 4.5; 0.04mM) and acetonitrile in ratio of 50:50, v/v. The flow rate and run time are 1.0 mL/min and 9.0 min, respectively, at 334 nm. The LLOQ is 0.05 ng/mL. The pharmacokinetics parameters of nobiletin in male S.D. rats following oral administration of nobiletin are provided in Table 9. Nobiletin get rapidly absorbed because of its lipophilic nature and high permeability. Elimination of nobiletin from the brain was slower in comparison with plasma. The AUC and t1/2 indicated that the brain exposure of nobiletin is approximately three times higher than the plasma.15
Table 9.
Selected pharmacokinetics parameters of nobiletin in male Sprague Dawley rats following oral administration of nobiletin at 50 mg/kg (n = 3/time point).
| Parameters | Plasma | Brain |
|---|---|---|
| AUC(0–t) (μg·h/mL) | 7.49 | 20.66 |
| AUC(0–∞) (μg·h/mL) | 7.84 | 23.20 |
| Cmax (μg·h/mL) | 1.78 | 4.20 |
| Tmax (h) | 1.00 | 1. 00 |
| Kel (1/h) | 0.39 | 0.06 |
| t1/2 (h) | 1.80 | 11.42 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; Tmax = time of peak plasma concentration; Kel = elimination rate constant.
2.10. Cynomorium songaricum Rupr. (鎖陽 suǒ yáng)
Cynomorium songaricum Rupr. (Suoyang) is one of the known medicinal parasitic plants from TCM. The catechins isolated from C. songaricum include catechin, epicatechin, and epicatechin gallate. Catechin and epicatechin are useful in atherosclerosis and cancer treatment, respectively.
The LC-MS/MS method was used for simultaneous determination of pharmacokinetic parameters catechin, epicatechin, and epicatechin gallate after oral administration of alcoholic C. songaricum extract in rats. The system was equipped with an Eclipse Plus (Agilent, USA) C18 (4.6 × 100 mm, 1.8 μm) column with a security guard C18 (2.1 × 12.5 mm i.d., 5 μm) column. The mobile phase involves formic acid aqueous solution (0.1%) (A) and acetonitrile (B) using a gradient elution of 20–44% B at 0–8 min, 44–80% B at 8–12 min, 80–20% B at 12–13 min, and the re-equilibration time of gradient elution is 5 minutes. The flow rate, column oven temperature, and injection volume are 0.3 mL/min, 25°C, and 10 μL, respectively. Cmax of catechin, epicatechin, and epicatechin gallate in rat plasma are 86.69 ± 38.65, 32.57 ± 15.00 and 36.93 ± 12.62 ng/mL whereas Tmax values are 0.15 ± 0.09, 0.20 ± 0.10 and 0.20 ± 0.13 hours, respectively. The LLOQ value is 2 ng/mL. The pharmacokinetic parameters of catechin, epicatechin, and epicatechin gallate after oral administration are provided in Table 10. Catechin, epicatechin, and epicatechin gallate demonstrated rapid absorption in rat plasma after oral administration of C. songaricum extracts.16
Table 10.
Pharmacokinetic parameters of catechin, epicatechin, and epicatechin gallate after oral administration of 15.25 g kg−1C. songaricum extract (n = 8, mean ± standard deviation).
| Parameters | Catechin | Epicatechin | Epicatechin gallate |
|---|---|---|---|
| MRT0–12 (h) | 3.98 ± 0.33 | 4.54 ± 0.66 | 3.85 ± 0.78 |
| T1/2 2α(h) | 0.33 ± 0.12 | 0.60 ± 0.34 | 0.51 ± 0.36 |
| T1/2 2β(h) | 6.38 ± 4.20 | 34.86 ± 25.30 | 4.70 ± 4.24 |
| AUC0–12 (ng h/mL) | 109.7 ± 57.0 | 67.66 ± 16.99 | 72.44 ± 49.93 |
| AUC 0-∞ (ng h/mL) | 154.0 ± 97.2 | 214.0 ± 161.7 | 91.01 ± 67.99 |
AUC = area under the concentration-time curve; MRT = mean residence time.
2.11. Curcuma longa L. (薑黃 jiāng huáng)
Curcumin (1,7-bis(4-hydroxy-3-methoxyphenyl)-1,6-heptadiene- 3,5-dione) is a phenolic substance derived from spice herb Curcuma longa L. Curcumin is widely used in the food industry as a natural food coloring agent and curry powder. In addition, curcumin has the anticancer, antiviral, and anti-infectious properties, anti-amyloidogenic effects, and wound healing qualities and it is also useful in treating Alzheimer disease.
A LC-MS/MS with an orthogonal Z-spray electrospray interface system was used to determine the pharmacokinetics and oral bioavailability of curcumin and demethoxy curcumin from C. longa. The system was equipped with a ZORBAX (Agilent, Palo Alto, CA, USA) Extend-C18 column (150 × 4.6 mm i.d., 5 μm). The system delivered a constant flow of 200 μL/min and the mobile phase consisted of 70% acetonitrile and 30% 1mM formic acid. The volume of injection was 10 μL. The LOD and LOQ of curcumin in the rat plasma are 1ng/mL and 5 ng/mL, respectively. It can also be used as an analytical tool for the quality control of various species of turmeric herbs. The pharmacokinetic data after curcumin administration are provided in Table 11.17 The extent of curcumin conjugation was greater in an intestine of human and in rat curcumin is widely conjugated in hepatic fraction. Intestinal and hepatic microsomes are responsible for curcumin glucuronide whereas curcumin sulfate, tetrahydrocurcumin, and hexahydro-curcumin were found as curcumin metabolites in intestinal and hepatic cytosol from humans and rats.18
Table 11.
Pharmacokinetic data after curcumin administration (10 mg/kg intravenously and 500 mg/kg by mouth) in rats.
| Parameters | Curcumin |
|
|---|---|---|
| 10 mg/kg, i.v. | 500 mg/kg, p.o. | |
| AUC (min μg/mL) | 7.2 ± 1.2 | 3.6 ± 0.6 |
| t1/2 β (min) | 28.1 ± 5.6 | 44.5 ± 7.5 |
| Cmax (μg/mL) | 0.36 ± 0.05 | 0.06 ± 0.01 |
| Tmax (min) | – | 41.7 ± 5.4 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; i.v. = intravenous; p.o. = by mouth; Tmax = time of peak plasma concentration.
3. Dicaffeoylquinic acids
Dicaffeoylquinic acids (DCQAs) are a class of natural polyphenolic compounds widely distributed in many herbs. 3,4-DCQA, 1,5-DCQA, 3,5-DCQA, and 4,5-DCQA are the typical analogs of DCQAs. Large amounts of such polyphenolic compounds have been extracted from Ainsliaea fragrans champ. (兔耳風 tù ěr fēng) These compounds exhibit various biological actions such as antibacterial, antiviral, anti-inflammatory, and antioxidative stress effects.
The HPLC-MS/MS method was used for simultaneous estimation of pharmacokinetic activity of four DCQAs in Dawley rat plasma. The system was equipped with an Agilent (Santa Clara, CA) ZORBAX SB-C18 column (150 × 2.1 mm i.d., 1.8 μm) (Agilent Technologies). The MS was operated in the negative mode. The mobile phase composed of acetonitrile (A) and water containing 0.1% formic acid (B) and it is eluted as follows: 0 min (23%, A), 2 minutes (23%, A), 3.5 minutes (10%, A), 5 minutes (20%, A), 10.5 minutes (20%, A), 14 minutes (70%, A), 14.01 minutes (23%, A), and 18 minutes (23%, A). The flow rate and column temperature were 0.2 mL/min and 30°C, respectively. The plasma sample was prepared using a liquid-liquid extraction method and the recovery rate for the four analytes was around 80%. The calibration curves are linear over a concentration range of 10.6–1060.0 ng/mL for 3,4-DCQA, 19.2–1920.0 ng/mL for 1,5-DCQA, 14.0–2900.0 ng/mL for 3,5-DCQA, and 9.7–970.0 ng/mL for 4,5-DCQA. The intraday and interday precision was less than 15% and the relative error (RE) was within ±15%. The four DCQAs were not stable after three complete freeze/thaw cycles (−80°C to 23°C). However, they were stable after long-term sample storage (−80°C for 30 days) and bench-top (23°C for 2 hours). The extracted samples on the auto sampler rack at 4°C are stable for 6 hours. The LLOQ was as follows: 10.6 ng/mL for 3,4-DCQA, 19.2 ng/mL for 1,5-DCQA, 14 ng/mL for 3,5-DCQA, and 9.7 ng/mL for 4,5-DCQA, which was sufficiently sensitive to measure relatively low concentrations of DCQA in plasma with a simple liquid-liquid extraction procedure using as little as 50 μL plasma. The typical plasma concentration-time profiles indicate that 3,4-DCQA, 3,5- DCQA, and 4,5-DCQA may transform to 1,5-DCQA in vivo because the content of 1,5-DCQA in the extract was very low.19
3.1. Dracaena cochinchinensis (龍血 lóng xuè)
Longxuejie is a resina moiety isolated from the Dracaena cochinchinensis (Lour.) S.C. Chen which is also called ʻdragon's bloodʼ in TCM. Longxuejie is clinically used in the treatment of cerebral arterial thrombosis, ischemic heart disease, and peptic ulcer. Loureirin B is the single active component isolated form of longxuejie that has shown good therapeutic actions.
A HPLC (Shimadzu LC-20AD, Japan) an ESI-sciex Q-trap TM MS was used to analyze the Loureirin B after oral administration of longxuejie. The MS was operated in the positive ESI mode with multiple reaction monitoring (MRM) at unit resolution. The system was equipped with an Agilent XDB-C18 column (4.6 × 50 mm i.d., 5 μm) maintained at 20°C. The mobile phase was composed of water containing 0.1% formic acid (A) and methanol containing 0.1% formic acid (B) and with flow rate of 0.4 mL/min. After oral administration of 16 g/kg longxuejie to rats through lavage, serial blood samples (0.3 mL) are collected by retro-orbital puncture at 0, 0.083, 0.17,0.33, 0.5, 0.75, 1, 2, 4, 6, 8, 12, and 18 hours, and then centrifuged at 5000 rpm for 5 minutes immediately afterward. All plasma samples are stored at −20°C until analysis. The concentration range of 0.08–100 ng/mL. The LOD and LOQ were 0.03 and 0.08 ng/mL, respectively. The pharmacokinetic parameters of loureirin B after oral administration of longxuejie are provided in Table 12.20 In this study, apart from free loureirin B, conjugated metabolites of loureirin B such as sulfate and glucoside metabolites were also detected in rat plasma samples, and the study suggests the necessity of further detailed study of the metabolites.
Table 12.
Pharmacokinetic parameters of loureirin B after oral administration of longxuejie (16 g/kg) to rats (n = 6, mean ± standard deviation.
| Parameters | Values |
|---|---|
| Kel (/h) | 0.365 ± 0.06 |
| t1/2 (h) | 1.94 ± 0.27 |
| T max (h) | 0.81 ± 0.11 |
| Cmax (μg/L) | 7.99 ± 1.2 |
| AUC0–T (μg h/L) | 22.2 ± 1.9 |
| AUC0–∞ (μg h/L) | 22.6 ± 1.8 |
| Cl (l/h/kg) | 978.2 ± 117.3 |
| Vc (l/kg) | 2768.6 ± 751.5. |
AUC = area under the concentration-time curve; Cl = clearance; Cmax = peak plasma concentration; Tmax = time of peak plasma concentration.
3.2. Dioscorea nipponica (穿龍薯蕷 chuān lóng shǔ yù)
Protodioscin (3-O-[α l-rhamnopyranosyl-(1→2)-{α l-rhamnopyranosyl (1→4)}-β-d-glucopyranosyl]-26-O-[β-d-glucopyranosyl]-(25R)-furost-5-ene-3β,26-diol) is a typical example of a furostanol saponin, which is isolated from the roots of Dioscorea nipponica Makino, and it also comprises Oriental vegetables and medicinal plants. Protodioscin is found to be one of the potent anticancer agents and in China its formulation is commercially available.
HPLC-tandem MS with positive ion detection mode was used to determine the pharmacokinetics of protodioscin after intravenous administration in rats. The system was equipped with a Carbosorb ODS-3 column (50 × 2.0mm i.d., 5 μm) and a security guard C18 guard column (4 × 2.0 mm i.d.) using a mobile phase of acetonitrile-water-formic acid (80:20:0.1, v/v/v). The liquid flow rate and column temperature are 0.2 mL/min and 30°C, respectively. The LLOQ was found to be about 20.0 ng/mL. The pharmacokinetic parameters of protodioscin in rats after intravenous administrations are provided in Table 13. The pharmacokinetic data indicate that proportional increase in the area under the plasma concentration-time curve with increasing protodioscin dose thus confirms the dose-dependent kinetic property.21
Table 13.
Pharmacokinetic parameters of protodioscin in rats after intravenous administrations.
| Parameter | Dose (mg/kg) |
||
|---|---|---|---|
| 0.5 | 1 | 3 | |
| t1/2 (min) | 78 ± 12 | 58 ± 11 | 27 ± 19 |
| kel (1/min) | 0.0089 ± 0.0056 | 0.012 ± 0.042 | 0.029 ± 0.009 |
| Cmax (μg/mL) | 70 ± 9 | 116 ± 15 | 378 ± 10 |
| Vss (mL/kg) | 71.6 ± 13 | 49 ± 21 | 23.5 ± 9 |
| Cl (mL/min/kg) | 0.637 ± 0.19 | 0.598 ± 0.05 | 0.681 ± 0.06 |
| AUC0-t (μg min/mL) | 732 ± 82 | 1406 ± 107 | 4196 ± 245 |
| AUC0–∞ (μg min/mL) | 785 ± 94 | 1673 ± 195 | 4406 ± 209 |
AUC = area under the concentration-time curve; Cl = clearance; Cmax = peak plasma concentration; Vss = volume of distribution at steady state.
3.3. Flos Lonicerae (金銀花 jīn yín huā)
Flos Lonicerae is one of the herbal plants reported in the literature about TCM. Various saponins are present in these plants, which are useful in alleviating acute fever, headache, pharyngodynia, respiratory infection, pyocutaneous disease, and epidemic disease and are also helpful in treating hepatic injury caused by acetaminophen, Cd and CCl4, and conspicuous depressant effects on swelling of ear croton oil.
A LC/MS with an ESI negative mode was used to determine the pharmacokinetic parameters of four saponins after oral administration. The system is equipped with an Agilent Zorbax C18 guard column (12.5 × 4.6 mm i.d., 5 μm) and a Shim-Pack CLC-ODS column (150 × 6.0 mm i.d., 5.0 μm). The mobile phase was composed of 0.2% acetic acid water (A) and acetonitrile (B) using a gradient elution of 27–29% (v/v) B at 0–6 minutes; 29–33% B at 6–14 minutes; 33–50% B at 14–20 minutes; 50–80% B at 20–30 minutes. The mobile phase flow rate, injection volume, and column temperature are 1.0 mL/min, 10 μL, and 25°C, respectively. To maintain the flow rate of 0.25 mL/min and to avoid differences in nebulization efficiency, a postcolumn split was used. The LOD and LOQ (pooled plasma samples) values were 0.00234, 0.00184, 0.00217, 0.000433, and 0.00772, 0.00606, 0.00716, and 0.00143 μg/mL, respectively. The pharmacokinetic parameters of the four saponins after oral (2 g extract/kg) administration are presented in Table 14. In this study double peaks were observed in both individual and mean plasma concentration curves of the four saponins except for macranthoside B. This type of diversity of pharmacokinetics of various components is influenced by the complicated interactions among compounds during the process of absorption, distribution, metabolism and excretion.22
Table 14.
Pharmacokinetic parameters of the four saponins after oral administration of 2 g extraction/kg, each value represents the mean ± standard deviation (n = 5).
| Compound | Cmax−1 (μg/mL) | Cmax−2 (μg/mL) | T max−1 (h) | T max−2 (h) | AUC0−t (μg/h/mL) |
|---|---|---|---|---|---|
| Macranthoidin B | 1.39 | 1.30 | 5 | 18 | 22.79 |
| Macranthoidin A | 1.88 | 2.35 | 5 | 18 | 39.01 |
| Dipsacoside B | 1.73 | 2.20 | 5 | 18 | 39.62 |
| Macranthoside B | 0.10 | 0.64 | – | 18 | 19.52 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; Tmax = time of peak plasma concentration.
3.4. Forsythia suspense (Thunb) (連翹 lián qiào)
Forsythiaside, a phenylethanoid glycoside, is the most abundant constituent in the fruit of Forsythia suspense (Thunb) Vahl. Forsythiaside is able to show the antipyretic, antidote, and anti-inflammatory properties in the treatment of various infections, especially acute upper respiratory tract complaints caused by viruses and/or bacterial infection.
A LC-MS/MS method was used to determine the pharmacokinetic and oral bioavailability of forsythiaside in rats. The system was equipped with a Thermo Hypersil reverse-phase C18 column (250 × 4.6 mm i.d., 5 μm, San Jose, CA, USA), which was eluted with a gradient mobile phase of acetonitrile (A) and water (B) both containing 0.2% formic acid. The solvent A was 15% (v/v) at the beginning and linearly increased to 35% over 7 minutes, and then returned to 15% by 3 minutes. The mobile phase was delivered at a flow rate of 1 mL/min and 40% of elute was introduced to an Applied Biosystem 3200 Q-Trap mass spectrometer (Foster City, CA, USA) with ESI source. The detection was performed by negative ion ESI in multiple reaction monitoring mode. To calculate the parameters in noncompartmental models and plasma concentration versus time profiles, Win-Nonlin software (Pharsight Corporation, Mountain View, CA, USA, (Version 2.1)) was used. The LOD and LOQ were 0.2 and 1.0 ng/mL, respectively, when 100 μL of plasma was used for assay. The pharmacokinetic parameters of forsythiaside in rats following intravenous and oral administration are presented in Table 15. From pharmacokinetic parameters it is clear that forsythiaside is rapidly absorbed into the circulation system and reached its peak concentration at around 20 minutes after oral administration but because of potential hydrolysis in the gastrointestinal tract, poor permeability through the intestinal epithelial membrane and first-pass effect in the liver might be responsible for the low bioavailability of the compound.23
Table 15.
Pharmacokinetic parameters of forsythiaside in rats following intravenous (20 mg/kg) and oral (100 mg/kg) administration.
| Parameters | The route of dosing |
|
|---|---|---|
| i.v. | Oral | |
| Cmax (ng/mL) | – | 122.2 ± 45.4 |
| Tmax (min) | 0.0 | 20.0 ± 0.0 |
| Initial plasma concentration (C0) (μg/mL) | 64.2 ± 36.1 | – |
| t1/2, λz (min) terminal elimination half-life | 76.8 ± 26.5 | 74.7 ± 13.3 |
| AUC0–t (μg min/mL) | 570.5 ± 69.4 | 13.9 ± 5.2 |
| AUC0–∞ (μg min/mL) | 570.8 ± 69.2 | 14.6 ± 5.7 |
| CL/F (mL/(min kg) | 35.5 ± 4.2 | 39.4 ± 15.9 |
| Volume of distribution (Vd), λz/F (L/kg) | 4.0 ± 1.8 | 4.2 ± 1.9 |
| Absolute bioavailability (F) (%) | – | 0.5 |
All data are expressed as mean ± standard deviation (n = 5).
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; i.v. = intravenous; Tmax = time of peak plasma concentration; CL/F = apparent plasma clearance.
3.5. Flos Lonicerae: Flos Lonicerae (金銀花 jīn yín huā)
Flos Lonicerae is one of several herbs present in TCM. It mainly consists of a series of water-soluble phenolic components. Chlorogenic acid is the main constituent of Flos Loniceae, which has been reported to have activity of suppressing the N-nitrosating reaction and inhibiting hepatic glucose 6-phosphatase.
A HPLC with UV detector was used to determine the pharmacokinetic parameters of Flos Lonicerae after administration of water extract to rabbits. The system was equipped at room temperature with an analytical column (MTPERSIL BDS C18, 250 × 4.6 mm i.d., 5 μm). The mobile phase consisted of a mixture of acetonitrile-0.2% H3PO4 (11:89, v/v) adjusted to pH 3.0 with sodium hydroxide (0.2 g/mL). The flow rate and method concentration range are 0.8 mL/min and 0.0500–1.00 μg/mL, respectively. The UV detector was set at 327 nm. The LOQ was 0.0500 μg/mL. The pharmacokinetic parameters after administration of Flos Lonicerae water extract to rabbits are presented in Table 16. After single-dose administration of Flos Lonicerae extract, two maximum concentrations of chlorogenic acid were observed in rabbit plasma. The study suggests the possible way of mechanism is by hepatoenteral circulation.24
Table 16.
Pharmacokinetic parameters obtained by analyzing plasma samples after administration of 10 mg/kg Flos Lonicerae extract to rabbits (n = 4).
| Parameters | Values |
|---|---|
| AUC (μg min/mL) | 140 ± 65.9 |
| Area under first moment curve (AUMC) (μg min2/mL) | 2.80 × 104 ± 1.73 × 104 |
| MRT (min) | 190 ± 38.3 |
| Variance of the mean residence time (VRT) (min.min) | 1.28 × 104 ± 2.66 × 103 |
| Kel (L/min) | 0.0130 ± 0.0023 |
| Tmax(min) | 34.7 ± 1.09 |
| Cmax (μg/mL) | 0.839 ± 0.350 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; MRT = mean residence time; Tmax = time of peak plasma concentration; Kel = elimination rate constant.
3.6. Ginkgo biloba (銀杏 yín xìng)
Ginkgo biloba is a TCM herb mostly used to treat various diseases. It contains mixtures of terpenoids and flavonoids. The flavonoids, including flavones (quercetin, kaempferol, and isorhamnetin) and flavonol glycosides are responsible for the free radical scavenging effects of G. biloba, whereas the ginkgolides are potent antiplatelet factor (PAF) antagonists. However, the oral bioavailability of flavonoids is relatively low because of their low liposolubility and poor solubility, which severely limits their ability to pass across the lipid-rich biological membranes, resulting in poor bioavailability. In order to improve the absorption of ginkgo flavonoids in vivo, Ginkgo biloba extract (GBE), G. biloba extract phospholipid complexes (GBP), and solid dispersions (GBS) are formulated.
HPLC composed of an LC-20AB with SPDM20A (Shimadzu) was used to determine the pharmacokinetic characteristics and bioavailability of isorhamnetin, quercetin, and kaempferol after oral administration of GBE, GBP, and GBS in rats. The system was equipped with a Hedera ODS-2 column (250 × 4.6 mm i.d., particle size 5 μm, Dalian Elite, China). The mobile phase composed of a mixture of methanol and 0.4% phosphoric acid (60:40, v/v). The flow rate and column temperature are 1.0 mL/min and 35°C, respectively. The wavelength of UV detector was set at 360 nm. Based on a signal-to-noise ratio (S/N = 10), the LLOQ for isorhamnetin, quercetin, and kaempferol were 0.039, 0.056, and 0.048 μg/mL, respectively. The main pharmacokinetic parameters of isorhamnetin, quercetin, and kaempferol in rats are presented in Table 17, Table 18, Table 19, respectively. In comparison with GBE, both GBS and GBP showed better bioavailability, and the bioavailability of GBP is more than that of GBS. The key parameter in G. biloba flavonoids is the modification of liposolubility to enhance their bioavailability.25
Table 17.
The main pharmacokinetic parameters of isorhamnetin in rats.
| Parameter | GBE | GBP | GBS |
|---|---|---|---|
| Ke (1/h) | 0.0321 | 0.1135 | 0.0644 |
| Absorption rate constant (Ka) (1/h) | 0.2034 | 1.0512 | 0.6374 |
| Tmax (h) | 7.21 | 4.32 | 6.16 |
| Cmax (ng/mL) | 195.96 | 672.29 | 291.57 |
| AUC (0∼T) (ng/h/mL) | 1153.66 | 2722.37 | 1738.889 |
| MRT (0∼T) (h) | 6.3332 | 5.1331 | 5.3233 |
| CL/F(s) (ng/h/(ng/mL)) | 0.00022 | 0.00037 | 0.00041 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; GBE = Ginkgo biloba extract; GBP = G. biloba extract phospholipid complexes; GBS = G. biloba extract solid dispersions; MRT = mean residence time; Tmax = time of peak plasma concentration; CL/F = Apparent clearance; Ke = elimination rate constant.
Table 18.
The main pharmacokinetic parameters of quercetin in rats.
| Parameter | GBE | GBP | GBS |
|---|---|---|---|
| Ke (1/h) | 0.0541 | 0.1909 | 0.1124 |
| Ka (1/h) | 0.6376 | 1.4162 | 1.3592 |
| Tmax (h) | 1.21 | 1.02 | 0.63 |
| Cmax (ng/mL) | 179.21 | 724.89 | 419.02 |
| AUC (0∼T) (ng/h/mL) | 1368.26 | 3321.05 | 2841.63 |
| MRT (0∼T) (h) | 5.4791 | 4.1442 | 4.6633 |
| CL/F(s) (ng/h/(ng/mL)) | 0.0015 | 0.0033 | 0.0038 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; GBE = Ginkgo biloba extract; GBP = G. biloba extract phospholipid complexes; GBS = G. biloba extract solid dispersions; MRT = mean residence time; Tmax = time of peak plasma concentration; CL/F = Apparent clearance; Ke = elimination rate constant.
Table 19.
The main pharmacokinetic parameters of kaempferol in rats.
| Parameter | GBE | GBP | GBS |
|---|---|---|---|
| Ke (1/h) | 0.1641 | 0.3412 | 0.2875 |
| Ka (1/h) | 0.2029 | 0.8891 | 0.5570 |
| Tmax (h) | 6.32 | 5.83 | 1.33 |
| Cmax (ng/mL) | 180.23 | 323.56 | 280.54 |
| AUC (0∼T) (ng/h/mL) | 1139.59 | 2228.21 | 1630.94 |
| MRT (0∼T) (h) | 6.1712 | 5.5662 | 5.3033 |
| CL/F(s) (ng/h/(ng/mL)) | 0.0013 | 0.0028 | 0.0017 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; GBE = Ginkgo biloba extract; GBP = G. biloba extract phospholipid complexes; GBS = G. biloba extract solid dispersions; MRT = mean residence time; Tmax = time of peak plasma concentration; CL/F = apparent clearance; Ka = absorption rate constant and Ke = elimination rate constant.
3.7. G. biloba extract
G. biloba extract is one of the known remedies for treatment of various conditions. The standard ginkgo biloba extract, (EGb 761), contains 22–27% flavonoids and 5–7% lactones. Aglycones comprise less than 0.1% in the extract. G. biloba extract is extensively used therapeutically to increase peripheral and cerebral blood flow as well as for the treatment of dementia. G. biloba extract was reported to show interactions with other drug categories such as antiplatelet, antidepressant, diuretic, and nonsteroidogenic anti-inflammatory drugs. In addition, it shows significant interaction with human cytochrome P450. Considering consumer safety the kinetic behavior of the flavonoids in vivo was studied using the following method.
A HPLC with a diode-array detector was used to determine the total flavonoids in plasma after intravenous administration of G. biloba. The system was equipped with a C18 (4.6 × 150 mm, 5 μm, Waters) column with a guard C18 (4 × 15 mm i.d., 5 μm) column. The mobile phase consisted of an acetonitrile-0.02 mol/L sodium dihydrogen phosphate solution, containing 0.2% phosphoric acid, pH-2.0, (35:65, V/V). The flow rate, column temperature and detection wavelength are 1.0 mL/min, 30°C, and 360 nm respectively. The injections are administered to 55 male Wistar rats at doses of 50 mg/kg (containing 18 mg/mL flavonoids) via the thigh venae. Blood was collected from abdominal aorta by heparinized needles and syringes after 15, 25, 30, 60, 90, 120, 240, 360, 480, 600, and 720 min of administration from five rats each time. Then the blood was centrifuged at 3000 g for 15 minutes to obtain the plasma samples, which are stored at −80°C until assaying. The detection limits are 20 ng/mL for quercetin, 20 ng/mL for kaempferol, and 50 ng/mL for isorhamnetin. The pharmacokinetic parameters are calculated using a two-compartment model. The initial concentration in the plasma was 171.22 μg/mL. The half-life of the flavonoids in the first compartment (distribution) the second compartment (elimination) are 0.07 hours and 4.51 hours, respectively, whereas AUC0-∞, apparent volume of distribution and total body clearance are found to be 1711.06 μg min/mL, 0.11 L/kg, and 10.52 mL/(min.kg), respectively. The coingestion of 120 mg of EGb 761 and 500 mg of metformin did not significantly affect the pharmacokinetic properties of metformin.26
3.8. Gardenia jasminoides (梔子花 zhī zǐ huā)
Geniposide is an iridoid glycoside extracted from the fruit of Gardenia jasminoides. It is a well-known TCM herbal plant. It is used to treat disorders of the liver and gallbladder and also is known for its antihyperbilirubinemic action. Long-term use of the Gardenia extract and geniposide could induce hepatic pigmentation in pigs and mice and produce a hepatotoxic effect, respectively.
A LC system was coupled with multiple microdialysis probes to determine the amount of geniposide in the blood, liver, brain, and bile of anesthetized rats. The system was equipped with a Nova-Pak (Waters, Milford, MA, USA) reverse-phase column RP-C18 (150 × 3.9 mm i.d.; 5 μm) at ambient temperature (24 ± 1 °C). The mobile phase consists of acetonitrile-methanol-5mM monosodium phosphate (pH 4.6; 5:15:80, v/v/v), and the flow rate of the mobile phase was 1 mL/min. The maximum UV absorbance for geniposide was set at a wavelength of 240 nm. Method helps to know the pharmacokinetics of geniposide and its influence by the treatment of acupuncture. The pharmacokinetic data on geniposide in rat blood following geniposide administration are presented in Table 20. The acupuncture does not affect the pharmacokinetics of the herbal ingredient geniposide. However, several questions remain, and the most important is, Do these results reveal the independent effects between acupuncture and the pharmacokinetics of herbs?27
Table 20.
Estimated pharmacokinetic data on geniposide in rat blood following geniposide administration (10, 30, and 100 mg kg−1, intravenously).
| Parameters | Geniposide 10 mg/kg−1 |
Geniposide 30 mg/kg−1 |
Geniposide 100 mg/kg−1 |
|||
|---|---|---|---|---|---|---|
| With out acupuncture | With acupuncture | Without acupuncture | With acupuncture | Without acupuncture | With acupuncture | |
| A. Blood | ||||||
| AUC (min μgml−1) | 417 ± 17 | 486 ± 59 | 1102 ± 32 | 1235 ± 128 | 4759 ± 601 | 4233 ± 411 |
| MRT (min) | 15 ± 1 | 15 ± 1 | 18 ± 1 | 17 ± 2 | 17 ± 2 | 17 ± 2 |
| Cl (ml min−1 kg−1) | 24 ± 1 | 22 ± 2 | 27 ± 1 | 26 ± 3 | 23 ± 3 | 25 ± 2 |
| B. Liver | ||||||
| AUC (min μgml−1) | 550 ± 107 | 637 ± 76 | – | – | – | – |
| MRT (min) | 16 ± 2 | 19 ± 3 | – | – | – | – |
| C. Bile | ||||||
| AUC (min μgml−1) | 1039 ± 136 | 1001 ± 90 | – | – | – | – |
| MRT (min) | 37 ± 2 | 39 ± 1 | – | – | – | – |
| AUC liver/AUC blood | 1.34 ± 0.27 | 1.41 ± 0.24 | – | – | – | – |
| AUC bile/AUC blood | 2.50 ± 0.33 | 2.10 ± 0.10 | – | – | – | – |
Data are expressed as mean ± standard error of the mean from six individual micro-dialysis experiments at each dose treatment.
AUC = area under the concentration-time curve; Cl = clearance; MRT = mean residence time.
4. Homoeriodictyol-7-O-b-d-glucopyranoside
Homoeriodictyol-7-O-b-d-glucopyranoside (flavone 4′,5,7-trihydroxy-3′-methoxy-7-b-d-glucopyranoside, HEDT-Glu) isolated from the TCM herb Viscum coloratum and Viscum album (槲寄生 hú jì shēng). HEDT-Glu can inhibit platelet aggregation induced by platelet-activating factor. Phytochemical investigations indicated that Viscum coloratum helps to shows the inhibitory effect on PAF and also the antioxidative activities.
A HPLC with UV detector was used to determine the pharmacokinetic parameters of HEDT-Glu (13.2 mg/kg) after intravenous injection. The system was equipped with a Diamonsil C18 column (200 × 4.6 mm i.d., 5 μm). A mobile phase consisted of methanol-water-glacial acetic acid (45:55:0.5, v/v/v). The flow rate, column temperature, and UV detector wavelength are 1.0 mL/min, 30°C, and 284 nm, respectively. HEDT-Glu identification was carried out by MS (Finnigan TSQ), 1H- and 13C-NMR spectra (Bruker AVANCE-300). The LOQ in plasma and tissue samples are 1 and 0.5 ng, respectively. The main pharmacokinetic parameters of HEDT-Glu, are presented in Table 21. Low levels of the HEDT-Glu remained in the blood even 5 hours after intravenous administration. When s cleared from the blood, it is distributed to the liver and small intestine.28
Table 21.
Pharmacokinetic parameters of HEDT-Glu Following after intravenous administration 13.2 mg·kg−1 HEDT-Glu in rats (n = 6).
| Parameters | Values |
|---|---|
| AUC | 16.04 ± 3.19 μ g·h·mL−1. |
| Elimination half-life at the α phases (t1/2,a) | 0.06 ± 0.01 h |
| Elimination half-life at the β phase (t1/2,b) phases | 1.27 ± 0.31 h |
| Ke | 9.78 ± 1.61 h−1 |
| CL | 0.85 ± 0.17 l·kg−1·h−1. |
AUC = area under the concentration-time curve; CL = clearance; Ke = elimination rate constant.
4.1. Helicia nilagirica Bedd (山龍眼 shān lóng yǎn)
Helicid is the main chemical constituent extracted from the herb Helicia nilagirica Bedd of TCM. It is used to treat neurasthenia, neurasthenia syndrome, and vascular headache. From clinical practice it was found that helicid has significant healing effects, with no side effects on patients.
LC-ESI-MS method with negative ionization mode was used for identification and quantification of helicid in rat plasma. The pharmacokinetic parameters are also determined in rats after intragastric administration of helicid with a single dose 50 mg/kg. The system was equipped with a Luna C18 column (150 × 2.00 mm i.d., 5 μm). A mobile phase composed of acetonitrile-0.1% ammonia solution (20:80, v/v) at a flow rate of 0.3 mL/min. The LLOQ was found to be 1 μg/L. The pharmacokinetic parameters of helicid after oral administration are presented in Table 22. The plasma concentration of helicid was much lower in humans in comparison with rats and dogs, which suggests the existence of species differences but there is no significant species difference between human and rats for the plasma protein binding of helicid.29
Table 22.
Pharmacokinetic parameter of helicid after oral administration of a single dose of 100 mg.
| Parameter | Values |
|---|---|
| Cmax (μ g/L) | 10.6 ± 3.11 |
| Tmax (h) | 1.08 ± 0.47 |
| t1/2 (h) | 5.27 ± 0.89 |
| AUC0−24 (μ g h/L) | 37.25 ± 5.33 |
| AUC0−∞ (μ g h/L) | 40.34 ± 6.04 |
| F (%) | 48.34 in rats and 22.85 in dogs |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; Tmax = time of peak plasma concentration; t1/2 = half life; F = absolute bioavailability.
5. Hawthorn (山楂 shān zhā)
Hawthorn (Crataegus) is widely used as a medicinal plant in folk and official medicine. There are about 16 species in China, where Crataegus Pinnatifida Bge. Var Major N. E. Br, and Crataegus Pinnatifida Bge. (山裏紅果 shān lǐ hóng guǒ) are the two major species, named as Shanlihong and Shanzha, respectively. Hawthorn leaves flavonoids (HLF) include many types of flavonoids, e.g., vitexin-4″-O-glucoside (VGL), vitexin-2″-O-rhamnoside (VRH), vitexin, vitexin-6″-O-acetyl, rutin, hyperoside, quercitrin, and quercetin.
The HPLC with UV detector was used to determine the pharmacokinetic parameters of HLF. The system was equipped with reverse-phase Diamonsil TM C18 (200 × 4.6 mm i.d., 5 μm) column in presence of a guard column (Easy Guard C18 Kit, 8 × 4 mm, Dikma Technologies Inc.). The mobile phase composed of methanol-acetonitrile-tetrahydrofuran-0.5% acetic acid (1:1:19.4:78.6, v/v/v/v). The flow rate, column temperature, and UV detection are 0.8 mL/min, 30°C, and 330 nm, respectively. The sample injection and plasma required for both compounds are 20 μL and 100 μL, respectively. The LOQs are 0.23 μg/mL for VGL and 0.36 μg/mL for VRH and the relative standard deviations (RSDs) for both compounds are less than 20%. The pharmacokinetic parameters and dose-linear pharmacokinetics are carried out by compartmental, statistical moment (i.e., noncompartmental) analysis and least squares regression analysis, respectively. With minimum AIC values, a three-compartment open pharmacokinetic model was proposed and validated through the DAS 2.0.1. The pharmacokinetic parameters for VGL and VRH after a single intravenous administration of HLF are provided in Table 23. From the results it is found that the plasma concentrations and AUC of VGL and VRH in rat plasma were proportional to the administrated doses.30
Table 23.
Pharmacokinetic parameters for VGL and VRH in SD rats (mean ± standard deviation, n = 6) after a single intravenous administration of Hawthorn leaves flavonoids.
| Pharmacokinetic parameter | VGL |
VRH |
||||
|---|---|---|---|---|---|---|
| 0.61 mg/kg | 1.22 mg/kg | 2.45 mg/kg | 1.40 mg/kg | 2.80 mg/kg | 5.60 mg/kg | |
| t1/2 α (h) | 0.028 ± 0.002 | 0.029 ± 0.006 | 0.031 ± 0.003 | 0.029 ± 0.002 | 0.03 ± 0.005 | 0.033 ± 0.004 |
| t1/2 β (h) | 0.251 ± 0.004 | 0.25 ± 0.037 | 0.265 ± 0.006 | 0.25 ± 0.01 | 0.246 ± 0.035 | 0.26 ± 0.006 |
| Half-life of elimination phase (t1/2 γ) (h) | 2.671 ± 0.087 | 2.416 ± 0.137 | 2.373 ± 0.068 | 2.325 ± 0.163 | 2.273 ± 0.095 | 2.176 ± 0.051 |
| Apparent volumes of distribution of the central compartments (V1) (L/kg) | 0.021 ± 0.004 | 0.024 ± 0.01 | 0.024 ± 0.005 | 0.020 ± 0.006 | 0.022 ± 0.008 | 0.022 ± 0.003 |
| CL (L/h/kg) | 0.096 ± 0.013 | 0.101 ± 0.014 | 0.097 ± 0.010 | 0.094 ± 0.01 | 0.0932 ± 0.013 | 0.089 ± 0.01 |
| AUC(0−t) (mg h/L) | 4.492 ± 0.54 | 9.337 ± 1.215 | 20.891 ± 2.489 | 10.892 ± 1.168 | 23.766 ± 3.447 | 51.71 ± 6.504 |
| AUC(0−∞) (mg h/L) | 5.60 ± 0.778 | 10.578 ± 1.507 | 21.605 ± 2.459 | 12.664 ± 1.387 | 26.324 ± 4.238 | 53.984 ± 6.615 |
| MRT(0−t) (h) | 1.268 ± 0. | 1.478 ± 0.032 | 1.73 ± 0.018 | 1.212 ± 0.016 | 1.45 ± 0.05 | 1.668 ± 0.012 |
| MRT(0−∞) (h) | 2.543 ± 0.225 013 | 2.269 ± 0.096 | 2.18 ± 0.054 | 2.123 ± 0.215 | 2.142 ± 0.108 | 2.11 ± 0.071 |
AUC = area under the concentration-time curve; MRT = mean residence time.
5.1. Huperzia serrata (Thumb) (千層塔 qiān céng tǎ)
Huperzia serrata (Thumb.) Trev. is a well-known TCM plant used to relieve contusions, strains, and swelling, and to treat schizophrenia. As the peripheral cholinergic effect are often observed as the main side effect for this herb in clinic practice, it was suggested that the active component from H. serrata might be studied as a new drug for the treatment of neurodegenerative disorder such as Alzheimer disease. Bis(12)-hupyridone (B12H), a homodimer by linking two hupyridone fragments derived from Hup A, is a promising candidate for acetylcholinesterase (AChE) inhibition. In addition, as a more potent and selective anti-AChE agent, chemically synthesized B12H can be more easily prepared for its further commercialization and clinical use.
A HPLC DAD system was used to determine the pharmacokinetic profiles of B12H after intravenous (5 mg/kg and 10 mg/kg) and intra peritoneal (20 mg/kg) administration to rats. The system was equipped with an Agilent Extend C-18 analytical column (250 × 4.6 mm i.d., 5 μm) and protected with an Agilent Extend C-18 guard-column (12.5 × 4.6 mm i.d., 5 μm) maintained at 25°C. The iso-cratical elution with a mobile phase of water-ACN-trifluoroacetic acid (TFA) (81:19:0.04, v/v/v) was used at a flow rate of 1.0mL/min for the separation of analytes. The UV detector wavelength was set at 229 nm. Pharmacokinetic parameters are calculated with a two-compartmental and/or noncompartmental approach. The LOD and LOQ of this method are 0.05 μg/mL and 0.1 μg/mL, respectively. The pharmacokinetic parameters are presented in Table 24. The pharmacokinetic data indicated that after extravascular injection B12H could be well absorbed and most of the administered drug could enter into the systemic circulation.31
Table 24.
Pharmacokinetic parameters were calculated with two-compartmental and/or noncompartmental approach. Absolute bioavailability (F) was calculated as the ratio of the dose-normalized AUC0→∞ after i.p. injection (10 or 20 mg/kg) to that after bolus intravenous injection (5 mg/kg) of B12H.
| Pharmacokinetic parameters | Route of administration |
||
|---|---|---|---|
| Intravenous |
Intraperitoneal |
||
| 5 mg/kg | 10 mg/kg | 20 mg/kg | |
| Λ z (L/min) | 0.0050 ± 0.0005 | 0.0045 ± 0.0009 | 0.0059 ± 0.0008 |
| AUC0→t (min μg/mL) | 62.62 ± 5.47 | 96.15 ± 20.67 | 219.92 ± 8.78 |
| AUC0→∞ (min μg/mL) | 82.50 ± 8.55 | 125.73 ± 28.92 | 266.12 ± 13.14 |
| MRT (h) | 2.67 ± 0.18 | 3.84 ± 0.37 | 3.14 ± 0.37 |
| Cmax (μg/mL) | – | 0.93 ± 0.23 | 1.91 ± 0.29 |
| tmax (min) | – | 9.33 ± 6.25 | 4.75 ± 2.36 |
| t1/2 (h) | 2.35 ± 0.29 | 2.63 ± 0.49 | 1.99 ± 0.29 |
| CL (L/(min kg)) | 0.061 ± 0.006 | 0.055 ± 0.016 | 0.093 ± 0.005 |
| Vd (L/kg) | 12.35 ± 1.24 | 12.09 ± 1.72 | 16.06 ± 1.86 |
| F (%) | – | 76.2 | 80.7 |
AUC = area under the concentration-time curve; MRT = mean residence time; Cmax = maximum blood concentration; tmax = time to peak concentration; t1/2 = elimination half-life; Vd = the volume of distribution; CL = total blood clearance; F = absolute bioavailability.
5.2. Isodon rubescens (Hemsl.) (冬凌草 dōng líng cǎo)
Isodon rubescens (Hemsl.) Hara (Labiatae) is a perennial herb, native to China. It is one of the folk remedies for respiratory and gastrointestinal bacterial infections, inflammation, and cancer. The different diterpenoids found in the plants are lasiodonin, oridonin, ponicidin, and rabdoternin A. These compounds are able to shows a variety of biological actions such as antitumor, antimicrobial, anti-inflammatory, anticatastrophe, and antioxidation effects.
HPLC-ESI-MS method with positive ionization mode was used to determine pharmacokinetic profiles four diterpenoids in rat plasma after the single oral administration of I. rubescens ethanolic extract. The system was equipped with a Diamonsil C18 (250 × 4.6 mm i.d., 5 μm) column. The mass spectrometer was operated in the chemical determination process, which was divided into three periods. A linear gradient elution of methanol containing 0.1% formic acid (A) and 0.1% [v/v] aqueous formic acid (B) was used for the separation. The solvent flow, column temperature, and total run time between injections are 0.8 mL/min, 25°C, and 13.5 minutes, respectively. Over the range from 0.0 to 10.5 min, lasiodonin, oridonin, and Internal Standards are easily detected. The pharmacokinetic parameters of the four diterpenoids after single oral administration of I. rubescens ethanolic extract are presented in Table 25, Table 26. All four diterpenoids shows good absorption with oral administration. They are easily detected in plasma after 10 minutes and eliminated quickly at a similar rate.32
Table 25.
Pharmacokinetic parameters of the four diterpenoids in six rats plasma after single oral administration of I. rubescens extract 10 mL/kg (n = 6).
| Pharmacokinetic parameter | Compound |
|||
|---|---|---|---|---|
| Lasiodonin | Oridonin | Ponicidin | Rabdoternin A | |
| Cmax (ng/mL) (means ± SD) | 1300.717 ± 365.53 | 1916.333 ± 307.20 | 1582.383 ± 307.20 | 385.011 ± 58.35 |
| Tmax (min) | 105 | 105 | 120 | 105 |
| t1/2 (min) (means ± SD) | 40.984 ± 9.12 | 45.147 ± 11.42 | 40.269 ± 9.05 | 58.04 ± 12.02 |
| K (1/min) (means ± SD) | 0.0177 ± 0.0045 | 0.0161 ± 0.0037 | 0.0179 ± 0.0035 | 0.0124 ± 0.0024 |
| AUC0–t (ng/min/mL) (means ± SD) | 96990.82 ± 26493.23 | 142768.30 ± 34344.80 | 115004.70 ± 15237.04 | 28958.63 ± 5530.37 |
| AUC0–1 (ng/min/mL) (means ± SD) |
97916.68 ± 5348.35 | 144527.30 ± 33606.69 | 116425.80 ± 15969.54 | 29522.15 ± 5348.35 |
AUC = area under the concentration-time curve; SD = standard deviation; Cmax = maximum blood concentration; Tmax = time to peak concentration; t1/2 = half-life.
Table 26.
Lower limit of quantification and limit of detection for given diterpenoids compounds.
| Compound | LLOQ (ng/mL) | LOD (ng/mL) |
|---|---|---|
| Lasiodonin | 2.24 | 0.540 |
| Oridonin | 4.92 | 0.826 |
| Ponicidin | 5.32 | 0.736 |
| Rabdotemin A | 1.36 | 0.432 |
5.3. Isatis indigotica L. (菘藍 sōng lán)
Indolinone [(E,Z)-3-(4-hydroxy-3,5-dimethoxybenzylidene) indolin-2-one], is an alkaloid present in the TCM different herbs. It is present in the dried roots of I. indigotica L. (Brassicaceae) (板藍根 bǎn lán gēn) and in leaves of I. tinctoria L (European woad) (板藍葉 bǎn lán yè). Indolinone is useful in the inhibition of mast cell degranulation as well as block immunoglobulin E (IgE) mediated degranulation of sensitized mast cells.
An UPLC-MS/MS method with positive ionization mode was used to determine the pharmacokinetic parameters after a single intravenous of indolinone in rats. The system was equipped with a Waters UPLC HSS T3 column (100 × 2.1 mm i.d., 1.8 μm) protected by an Acquity UPLC column in-line filter unit (0.2 μm in-line frit). Seal wash solvent was water-acetonitrile (70:30, v/v), weak and strong wash solvents was water-acetonitrile (50:50, v/v; containing 0.2% TFA) and acetonitrile-isopropanol-acetone (40:30:30, v/v/v; containing 0.2% TFA), respectively. The flow rate was set as 0.5 mL/min. The standard calibration curve of indolinone generated between 30.0 and 3000 ng/mL was found to be quadratic. The LOQ was found to be 30.0 ng/mL. Indolinone was found to be stable in rat plasma samples kept for 4 hours on the bench at room temperature, after three successive freeze/thaw cycles, and in processed plasma samples stored at circa 10°C for 4 days. The main pharmacokinetic parameters of indolinone calculated by noncompartmental analysis using Win-Nonlin software. The pharmacokinetic parameters after a single intravenous of indolinone in rats are presented in Table 27. The pharmacokinetic data indicate short half-life and a relatively high clearance.33
Table 27.
Pharmacokinetic parameters after a single intravenous dose of 2 mg/kg indolinone in rats (n = 4).
| Parameters | Mean | SE |
|---|---|---|
| C0 (ng/mL) | 5205 | 2232 |
| t1/2 (min) | 4.30 | 0.14 |
| Ke (1/h) | 9.53 | 0.21 |
| AUC0–last (ng h/mL) | 561 | 166 |
| AUC0–∞ (ng h/mL) | 568 | 162 |
| MRT (min) | 5.16 | 0.59 |
| Vz (L/kg) | 0.39 | 0.15 |
| CL (L/h/kg) | 3.38 | 1.46 |
Data were calculated using noncompartmental analysis.
AUC = area under the concentration-time curve; MRT = mean residence time; SE = standard error; C0 = Initial plasma concentration; t1/2 = half-life; CL = total blood clearance and Ke = elimination rate constant.
5.4. Mangifera indica (檬果 méng guǒ)
Mangiferin (1,3,6,7-tetrahydroxyxanthone-C-2-β-d-glucoside) is a natural glucosyl obtained from the TCM herb, Mangifera indica. Recently, it is found that mangiferin is a promising agent for oral diabetes treatment.
An ACQUITYTM UPLC/MS system (Waters Corp., Milford, MA, USA) at 4°C was used to determine the pharmacokinetic parameters of mangiferin after oral and intravenous administration. The mass spectrometer was equipped with TQD triple-quadrupole tandem mass spectrometer in positive ESI mode. The system was equipped with ACQUITY UPLCTM BEH C18 column (50 × 2.1 mm i.d., 1.7 μm), which is set at 35°C. Gradient elution of acetonitrile (A) and water containing 0.1% formic acid (B) is used as a mobile phase. The elution started with 90% B then the composition was linearly changed to 30% B over 0.5 minutes and maintained at the level for 1.4 minutes. Finally, the composition was returned to the initial composition over 0.1 minutes and maintained for 1.0 min. The oral bioavailability was found to be 1.2%. The LLOQ (0.02 and 0.4 μg/mL) was defined as the lowest concentration on the calibration curves. The pharmacokinetic parameters are calculated applying a noncompartmental model. The pharmacokinetic parameters of mangiferin after oral and intravenous administration to rats are presented in Table 28. The oral bioavailability of mangiferin was found to be 1.2%. To improve the oral bioavailability of mangiferin chemical and pharmaceutical modification may be useful.34
Table 28.
Pharmacokinetic parameters of mangiferin after oral and intravenous administration to rats.
| Parameter | Oral administration (n = 6) | Intravenous administration (n = 6) |
|---|---|---|
| AUC(0–t) (μg/L h) | 1855.0 ± 887.7 | 61184.1 ± 22471.4 |
| AUC(0–∞) (μg/L h) | 2036.2 ± 942.2 | 62065.2 ± 23013.2 |
| T1/2 (h) | 3.2 ± 0.6 | 0.9 ± 0.4 |
| Tmax (h) | 2.5 ± 0.8 | 0.083 |
| MRT0–t (h) | 4.3 ± 0.5 | 1.3 ± 0.2 |
| Cmax (μg/L) | 301.3 ± 133.0 | 67798.3 ± 31235.9 |
| CLz (L/h kg) | (13.95 ± 4.64) × F | 0.15 ± 0.04 |
AUC = area under the concentration-time curve; Cmax – peak plasma concentration; MRT = mean residence time; Tmax = time of peak plasma concentration.
5.5. Pueraria lobata (Willd) (大葛藤 dà gé téng)
Kakkalide (KA) is the major isoflavone found in extracts from the dried flower of Pueraria lobata (Willd.). It is one of the TCM herbal remedies for symptoms associated with excessive alcohol intake, such as drunkenness, headache, red face, and liver injury. Three known glucuronide metabolites are irisolidone-7-O-glucuronide (Ir-7G), tectorigenin-7-O-glucuronide (Te-7G), and 6-OH biochanin A-glucuronide (6-OH BiA-G). A LC-MS/MS was used to determine the pharmacokinetic parameters for KA and its metabolites in rat plasma. LC/MSD (Agilent 1100 Series) Trap was operated at negative ESI interface. The system was equipped with a Kromasil (Tianjin Scientific Instruments Co. Ltd., China) C18 column (4.6 × 200 mm i.d., 5 μm) at 35°C. The mobile phase was composed of acetonitrile containing 0.05% TFA (A) and water containing 0.05% TFA (B), eluted in a gradient way. For the identification of irisolidone, the mobile phase consisting of solutions A and B was run in isocratic mode in the ratio of 44:56 (v/v). The flow rate was 1.0 mL/min. The injection volume and detection wavelength are 20 μL and 265 nm, respectively. Pharmacokinetic parameters are determined by using noncompartmental analysis. The pharmacokinetic parameters for KA and its metabolites in rat plasma are presented in Table 29. After oral administration of KA in rats, Phase II metabolism occurs and it forms 13 different metabolites that are found in rat urine, in which irisolidone (Ir), tectorigenin (Te), irisolidone-7-O-glucuronide (Ir-7G), tectorigenin-7-O-sulfate (Te-7S), and tectorigenin-4′-O-sulfate (Te-4′S) were characterized. The AUC0−t values of the glucuronide metabolites are significantly greater than that of KA. KA metabolism in vivo may occur in different sites, first in the intestine and then in the liver, and future enterohepatic recirculation prolongs the elimination of these glucuronide metabolites.35
Table 29.
Pharmacokinetic parameters for kakkalide (oral 200 mg/kg−1) and its metabolites in rat plasma.
| Parameters | KA | Ir-7G | Te-7G | 6-OH BiA-G |
|---|---|---|---|---|
| Tmax (h) | 0.25 ± 0.00 | 34.0 ± 11.8 | 38.0 ± 9.0 | 36.0 ± 7.6 |
| Cmax (μg/mL) | 0.26 ± 0.17 | 2.73 ± 0.74 | 0.55 ± 0.22 | 2.33 ± 1.29 |
| AUC(0−t) (μg·h/mL) | 0.24 ± 0.16 | 65.2 ± 11.7 | 17.0 ± 4.7 | 54.9 ± 26.7 |
| AUC(0−∞) (μg·h/mL) | 0.25 ± 0.16 | 104.3 ± 38.2 | 27.2 ± 13.9 | 56.7 ± 25.7 |
| t1/2 (h) | 0.95 ± 0.52 | – | – | – |
| MRT(0−t) (h) | 1.22 ± 0.58 | 31.3 ± 6.0 | 40.5 ± 4.1 | 37.1 ± 4.6 |
| MRT(0−∞) (h) | 1.55 ± 0.72 | 46.1 ± 13.6 | 102 .3 ± 125.1 | 40.1 ± 6.4 |
| CLz/F (L/h/kg) | 1021.7 ± 486.5 | 2.18 ± 0.93 | 8.46 ± 2.81 | 4.21 ± 1.95 |
| Vz/F (L/kg) | 1388.3 ± 1061.0 | 55.6 ± 33.4 | 472.9 ± 442.0 | 91.0 ± 120.4 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; MRT = mean residence time; Tmax = time of peak plasma concentration; CL/F = apparent plasma clearance; t1/2 = half life.
5.6. Pueraria thomsonii (大葛藤 dà gé téng)
The isoflavone tectoridin is present in large quantities in the flowers of Pueraria thomsonii Benth, a TCM plant. It is useful in the treatment of various disorders such as diabetes, and excessive alcohol intake disorders such as drunkenness, headache, red face, and liver injury. Tectoridin possesses hepatoprotective, estrogenic, antihypolipidemic, antioxidative, and anti-inflammatory properties. The various metabolites of tectoridin are tectorigenin-7-Oglucuronide- 4′-O-sulfate (Te-7G-4′S), Te-7G-4′S, tectorigenin-7-Oglucuronide (Te-7G), and tectorigenin-7-O-sulfate (Te-7S).
A HPLC with UV detector was used to quantitatively determine the pharmacokinetic parameters of four tectoridin metabolites in rat plasma. The system was equipped with Kromasil C18 column (4.6 × 200 mm, 5 μm). The mobile phase comprising a gradient system of acetonitrile (A) and water containing 0.1% formic acid (B) at a flow rate of 0.8 mL/min at 35 °C as follows: a linear gradient of the mixture of solutions (A:B) from 12:88 (v/v) to 17:83 for 10 minutes, then maintained at 17:83 for 8 minutes, followed by a linear gradient of solutions (A:B) from 17:83 to 24:76 for 9 minutes, maintained at 24:76 for 5 minutes, and finally a linear gradient of solutions (A:B) from 24:76 to 50:50 for 28 minutes. The injection volume was 10 μL. To determine the metabolites, a mobile phase comprising a gradient system of acetonitrile containing 0.05% TFA (A) and water containing 0.05% TFA (B) at a flow rate of 0.8 mL/min as follows: a linear gradient of the mixture of solutions (A:B) from 14:86 to 20:80 for 19 minutes, followed by a linear gradient from 20:80 to 27:73 for 9 minutes, and from 27:73 to 42:58 for 19 minutes. The injection volume and detection wavelength are 20 μL and 264 nm, respectively. LLOQs and those for Te-7G, Te-7S and tectorigenin, and tectoridin are found to be 125, 200, 25, and 150 ng/mL, respectively. The pharmacokinetic parameters for tectoridin (200 mg/kg) metabolites in rat plasma after oral administration are presented in Table 30. The plasma concentrations of tectorigenin conjugated metabolites were higher than those of the tectorigenin aglycone, as it undergoes Phase II metabolism and forms glucuronide and sulfate conjugates, and a glucuronidesulfate bisconjugate. These conjugates also undergo enterohepatic recirculation. The extensive Phase II metabolism plays an important role in the pharmacokinetics of tectoridin and tectorigenin in vivo.36
Table 30.
Pharmacokinetic parameters for metabolites in rat plasma after oral administration of 200 mg/kg tectoridin.
| Parameters | Te-7G-4′S | Te-7G | Te-7S | Tectorigenin |
|---|---|---|---|---|
| Tmax (h) | 3.50 ± 1.87 | 3.17 ± 1.81 | 5.58 ± 3.07 | 4.92 ± 2.87 |
| Cmax (μmol/L) | 21.4 ± 13.8 | 20.5 ± 9.70 | 14.3 ± 3.30 | 8.67 ± 3.07 |
| AUC(0–t) (μmol/L) | 164 ± 52 | 184 ± 73 | 123 ± 63 | 72.0 ± 22.0 |
| AUC(0–∞) (μmol/L) | 197 ± 79 | 198 ± 78 | 199 ± 91 | 98.0 ± 47.7 |
| MRT(0–t) (h) | 9.79 ± 4.47 | 10.7 ± 4.30 | 8.12 ± 3.37 | 8.54 ± 2.01 |
| MRT(0–∞) (h) | 20.4 ± 16.7 | 13.7 ± 6.00 | 15.9 ± 7.12 | 12.5 ± 3.90 |
| CL/F (L/h/kg) | 2.13 ± 0.96 | 2.35 ± 0.76 | 3.28 ± 1.85 | 8.13 ± 3.57 |
| V/F (L/kg) | 31.3 ± 13.8 | 31.0 ± 23.1 | 37.9 ± 20.9 | 80.7 ± 33.1 |
Data are mean ± standard deviation (n = 6).
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; MRT = mean residence time; Tmax = time of peak plasma concentration; CL/F = apparent plasma clearance.
5.7. Paeonia suffruticosa (牡丹 mǔ dān)
Paeonol (2′-hydroxy-4′-methoxyacetophenone) is a major component in the medicinal herb Moutan Cortex, the root cortex of Paeonia suffruticosa A. (Paeoniaceae) (牡丹皮 mǔ dān pí). It is commonly prescribed for the treatment of pain and inflammatory ailments in Chinese medicine.
A HPLC-DAD method was used to determine pharmacokinetic profiling of pure paeonol including its metabolites and herbal preparation. The system was equipped with a Phenomenex ODS (250 × 4.6 mm i.d., 5 μm, Phenomenex Inc., USA) protected by a Security Guard Cartridge (C18, 4.0 × 3.0 mm i.d.; Phenomenex Inc.). The mobile phase composed of acetonitrile (A) and aqueous solution containing 0.1% formic acid (B) (pH adjusted to 3.5 ± 0.2 by triethylamine). At normal room temperature flow rate, injection volumes and wavelength for detection are 1.0 mL/min, 50 μL, and 270 nm, respectively. The LLOQ in rat plasma was found to be 0.15 μg/mL of paeonol. Pharmacokinetic parameters are calculated based on the noncompartment method. The pharmacokinetic parameters of paeonol in rat plasma after single oral administration of paeonol alone and paeonol contained in the herbal preparation Qingfu Guanjieshu (QFGJS) are presented in Table 31. After oral administration of paeonol and QFGJS in rats, five metabolites of paeonol, P1–P5, were identified in rat urine. The relative plasma concentration of these metabolites was found to be significantly higher in rats treated with QFGJS than those treated with pure paeonol at a comparable dose. Four metabolites, P2–P5, appeared as soon as 5 minutes after dosing and reached the maximum plasma concentrations in approximately 20 minutes. This study indicating that paeonol could quickly be metabolized into P2–P5 and circulate in the blood and/or the tissues and organs, but metabolite P1 is not found in plasma.37
Table 31.
Pharmacokinetic parameters of paeonol in rat plasma after single oral administration of paeonol alone and paeonol contained in the herbal preparation Qingfu Guanjieshu.
| Parameters | Paeonol |
QFGJS |
||
|---|---|---|---|---|
| 35 mg/kg | 70 mg/kg | 140 mg/kg | 3.89 g/kg | |
| Cmax (μg/mL) | 0.73 ± 0.07 | 2.02 ± 0.23 | 4.16 ± 0.50 | 8.61 ± 1.30** |
| Tmax (min) | 9.00 ± 2.45 | 5.00 ± 0.00 | 7.00 ± 2.00 | 5.00 ± 0.00 |
| T1/2 E phase (min) | 34.25 ± 3.91 | 34.18 ± 1.77 | 50.13 ± 4.11 | 38.25 ± 2.99 |
| T1/2 D/A phase (min) | 12.02 ± 1.73 | 12.74 ± 1.69 | 12.79 ± 1.81 | 11.66 ± 0.62 |
| T1/2 A phase (min) | 2.60 ± 0.53 | 1.92 ± 0.44 | 2.51 ± 0.38 | 1.58 ± 0.21 |
| MRT (min) | 51.62 ± 8.86 | 36.65 ± 2.18 | 56.14 ± 3.13 | 37.43 ± 2.58 |
| Vd (ml/kg) | 47,170 ± 5984 | 49,628 ± 6810 | 48,329 ± 6424 | 18,034 ± 1498* |
| CL/F (ml/(min kg)) | 1016.8 ± 167.7 | 1003.4 ± 110.5 | 761.0 ± 70.6 | 342.2 ± 39.8*** |
| AUC0−t (μg min/mL) | 40.66 ± 9.99 | 74.13 ± 8.68 | 188.50 ± 16.35 | 229.64 ± 27.38** |
| AUC 0−∞ (μg min/mL) | 40.72 ± 10.01 | 74.38 ± 8.77 | 189.22 ± 16.47 | 229.88 ± 27.46** |
Data are expressed as the mean ± standard error of the mean of 6 to 8 rats. Paeonol contained in QFGJS at dosage of 3.89 g/kg is equivalent to 70 mg/kg pure paeonol to rat. p is significantly different from that of the paeonol alone (at a dosage of 70 mg/kg) group by Student t test. *p < 0.05; **p < 0.01; ***p < 0.001.
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; MRT = mean residence time; QFGJS = Qingfu Guanjieshu; Tmax = time of peak plasma concentration; CL/F = apparent plasma clearance; Vd = volume of distribution; T1/2 = half life.
5.8. Pulsatilla koreana (白頭翁 bái tóu wēng)
Pulsatilla koreana Nakai (Ranunculaceae) is a traditional Korean herbal medicine used to treat amoebic dysentery and malaria. A standardized extract of P. koreana, SK-PC-B70M, improves scopolamine-induced impairments of memory consolidation and spatial working memory. Oleanolic-glycoside saponins, especially hederacolchiside E, are not only the major constituents but also the marker compounds for the SK-PC-B70M. Hederacolchiside E is an essential saponin that helps facilitate detailed pharmacokinetic study and also future preclinical or clinical investigation of SK-PC-B70M.
A LC-MS/MS with negative EIS was used to determine pharmacokinetic parameters of hederacolchiside E after oral administration. The system was equipped with a Hydrosphere C18 column (2.0 × 50 mm i.d., 3 μm; YMC Co., Ltd., Kyoto, Japan). Nitrogen (99.999%) was used as the nebulizing turbo spray and curtain gas, with the optimum values set at 60, 60, and 20 (arbitrary units), respectively. The HPLC mobile phases consisted of 0.1% formic acid: tetrahydrofuran (FA:THF) (90:10) (A) and acetonitrile:0.1% FA:THF (80:10:10) (B). A linear gradient program was used with flow rate of 0.5 mL/min. Solvent (B) was gradually increased 60% for 3 minutes, maintained for 0.5 minutes, and followed by a 1.5-minute re-equilibration. Injection volume and column oven temperature are 2 μL and 50°C, respectively. LLOQ and LOD are found to be 2 ng/mL in 20 μL of plasma and 0.5 ng/mL, respectively. Plasma concentration data were analyzed using a noncompartmental method. The pharmacokinetic parameters of hederacolchiside E after oral administration of SKPC- B70M in male Sprague Dawley rats are presented in Table 32. The pharmacokinetic data indicate the nonlinear pharmacokinetic pattern.38
Table 32.
Pharmacokinetic parameters of hederacolchiside E after oral administration of SKPC-B70M at a dose of 400 mg/kg in male Sprague Dawley rats.
| Parameter | SK-PC-B70M |
||
|---|---|---|---|
| 100 mg/kg | 200 mg/kg | 400 mg/kg | |
| AUC (μg h/mL) | 0.56 ± 0.10 | 1.27 ± 0.27 | 6.46 ± 4.1 |
| MRT (h) | 9.46 ± 0.61 | 10.1 ± 0.41 | 16.1 ± 2.3 |
| Tmax (h) | 0.38 ± 0.14 | 5.69 ± 4.13 | 11.5 ± 9.1 |
| Cmax (μg/mL) | 0.07 ± 0.04 | 0.13 ± 0.08 | 0.36 ± 0.11 |
| Tλ1/2 (h) | 31.1 ± 37.2 | 19.0 ± 18.5 | 28.9 ± 19.9 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; MRT = mean residence time; Tmax = time of peak plasma concentration; Tλ1/2 = terminal elimination half-life.
5.9. Rhizoma Corydalis Decumbentis (夏天無 xià tiān wú)
Tetrahydropalmatine, protopine, and palmatine are the chemical moieties found in TCM herb, i.e., Rhizoma Corydalis Decumbentis. It is commonly used for the treatment of hemiplegia, rheumatoid arthritis, and infantile residual paralysis, to counteract the effects of dementia and hepatotoxicity, and for pain relief.
A LC-ESI-MS with a positive ion mode was used for quantification and to determine the pharmacokinetic profile for the three alkaloids, tetrahydropalmatine, protopine, and palmatine, in rat plasma. The system was equipped with a Diamonsil C18 column (250 × 4.6 mm, i.d., 4.6 μm, Dikma Technologies, Beijing, China) and protected with an Easy Guard C18 guard column (5 × 4.6 mm i.d., 5 μm, Dikma Technologies) maintained at 25°C. The mobile phase consisted of acetonitrile-water (40:60, v/v) containing 5mM ammonium acetate and 0.2% glacial acetic acid. The flow rate was 0.2 mL/min. The LOQ value was found to be 1.00 ng/mL. The mean pharmacokinetic parameters of three alkaloids after oral administration of Rhizoma Corydalis Decumbentis extract to rats are presented in Table 33. The pharmacokinetic data indicate that the absorption of tetrahydropalmatine and palmatine is fast compared to that of protopine, and elimination of palmatine is slow.39
Table 33.
Mean pharmacokinetic parameters of three alkaloids after oral administration of Rhizoma Corydalis Decumbentis extract at 2.0 g kg−1 to rats (n = 6).
| Parameter | Tetrahydropalmatine | Protopine | Palmatine |
|---|---|---|---|
| t1/2 (h) | 6.68 ± 0.64 | 4.98 ± 1.64 | 12.84 ± 4.58 |
| Tmax (h) | 1.50 ± 1.14 | 3.50 ± 0.55 | 1.92 ± 0.74 |
| Cmax (ng/mL−1) | 435.8 ± 58.5 | 347.9 ± 51.51 | 8.53 ± 2.95 |
| MRT(0−t) (h) | 7.21 ± 0.21 | 7.36 ± 0.64 | 8.10 ± 1.07 |
| MRT(0−∞) (h) | 9.32 ± 0.58 | 8.84 ± 1.88 | 16.89 ± 6.27 |
| AUC(0−t) (ng/h/mL−1) | 3450.1 ± 480.9 | 2987.0 ± 354.0 | 57.85 ± 13.44 |
| AUC(0−∞) (ng/h/mL−1) | 3720.1 ± 498.3 | 3150.8 ± 482.8 | 77.58 ± 27.01 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; MRT = mean residence time; Tmax = time of peak plasma concentration; t1/2 = half life.
6. Rhein
Rhein (RE, 1,8-dihydroxy-3-carboxyanthraquinone) is an active ingredient extensively found in plants such as Aloe (蘆薈 lú huì), Rhubarb (大黃 dà huáng), and Cassitoral L. It is currently used for treating diabetic nephrosis in clinical practice and for broad pharmacological activities, including antitumor, anti-inflammatory, antibacterium, and renal protection properties. Esterification of free carboxyl group liberates two ester prodrugs of RE, i.e., rhein methylate (REM) and rhein ethylate (REE).
A HPLC with Shimadzu RF-10A fluorescence detector was used to perform the comparative pharmacokinetic study of RE, REM, and REE. The system was equipped with Shimadzu LC-10AT isocratic pump, Shimadzu SIL-10AD auto-injector, HS chromatography integrator, and a Hypersil ODS2 (4.6 × 250 mm, i.d. 5 μm, Dalian Elite Analytical Instruments Co., China), column at 40°C. The mobile phase was composed of a mixture of acetonitrile: methanol: 0.3% acetic acid (15:61:24, V/V/V) at a flow rate of 1.2 mL/min. The excitation and emission wavelengths are set at 440 nm and 520 nm, respectively. The retention time of RE, IS, REM, and REE was 4.2, 6.2, 6.8 and 8.6 minutes, respectively. LLOQ for RE, REM, and REE was 0.005, 0.020, and 0.020, respectively. The pharmacokinetic parameters of rhein are provided in Table 34. The carboxyl-esterification significantly reduced the net exposure amount of rhein in vivo, leading to its inaptitude in the development of drug precursors of RE.40
Table 34.
Pharmacokinetic parameter of rhein.
| Administration route | Parameters | RE | REM | REE |
|---|---|---|---|---|
| i.g. | Tmax (h) | 0.9 ± 0.1 | 6.7 ± 2.3* | 10.7 ± 2.3** |
| Cmax (mg/L) | 42.66 ± 14.41 | 0.058 ± 0.035** | 0.95 ± 0.090** | |
| t1/2ka (h) | 0.2 ± 0.1 | 4.1 ± 1.6* | 3.0 ± 0.5** | |
| t1/2 α (h) | 1.1 ± 0.8 | 5.7 ± 1.6* | 1.5 ± 0.6 | |
| t1/2 β (h) | 3.2 ± 0.6 | 6.0 ± 1.7** | 6.4 ± 1.0** | |
| CL/F (L/h/kg) | 0.78 ± 0.28 | 97.65 ± 66.61** | 5.21 ± 0.51* | |
| i.v. | AUC0-∞ (h·mg/L) | 80.28 ± 13.59 | 1.03 ± 0.76** | 12.79 ± 0.96* |
| t1/2α (h) | 0.1 ± 0.04 | 0.6 ± 0.4* | 0.2 ± 0.1 | |
| t1/2β (h) | 0.4 ± 0.1 | 3.8 ± 0.8** | 2.9 ± 1.6* | |
| CL/F (L/h/kg) | 0.36 ± 0.11 | 0.93 ± 0.54 | 1.95 ± 0.68* | |
| AUC0-∞ (h·mg/L) | 2.40 ± 1.15 | 0.84 ± 0.40* | 0.36 ± 0.092* | |
| F abs (%) | 33.5 | 15.2 | 2.9 |
*P < 0.05, **P < 0.01 versus RE group.
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; i.g. = intragastric administration; i.v. = intravenous; RE = rhein; REE = rhein ethylate; REM = rhein methylate; Tmax = time of peak plasma concentration.
6.1. Rhizoma Bolbostematts
Rhizoma Bolbostematts, widely used in TCM, is prepared from the bulb of Bolbostemma paniculatum (Maxim.) (土貝母 tǔ bèi mǔ) Franquet. It possesses well-documented anticancer, antiviral, anti-inflammatory, and immunosuppressive properties. Saponins are considered as main bioactive constituents. Among them, tubeimoside I is the main component in the saponins of R. Bolbostematts. Tubeimoside I, a triterpenoid saponin isolated from the tubers of B. paniculatum, showed potent antitumor and antitumor-promoting effects.
A LC/MS method was used to determine the pharmacokinetic parameters of tubeimoside I after administration via both intravenous and oral routes. The system was equipped with a triple quadrupole mass spectrometer with Turbo-Ion-Spray ion source (MDS Sciex Inc., Toronto, Canada) and a Waters Symmetry C18 reverse-phase column (150 × 2.1 mm i.d., 3.5 μm, Waters Inc.) with a SB-C18 guard column (20 × 4.0 mm i.d., 5 μm). The mobile phase composed of a mixture of acetonitrile and water containing 5μM sodium acetate (60:40, v/v). The flow rate and column temperature are 0.2 mL/min and 25°C, respectively. The LLOQ for tubeimoside I was 20 ng/mL in 0.1 mL rat plasma. The pharmacokinetic parameters are described by using a two- compartmental model. The pharmacokinetic parameters in rats after intravenous administration are presented in Table 35, Table 36. After the oral and intravenous administration of tubeimoside I in rats, it shows limited absorption in system circulation and was slowly eliminated.41
Table 35.
Pharmacokinetic parameters in rats after intravenous administration 5 mg/kg.
| Parameter | Animal no. |
Mean | SD | |||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| t1/2α (h) | 0.586 | 0.155 | 0.109 | 0.131 | 0.245 | 0.228 |
| t1/2β (h) | 5.34 | 9.43 | 5.47 | 6.56 | 6.70 | 1.90 |
| V (l/kg) | 0.101 | 0.162 | 0.092 | 0.070 | 0.106 | 0.039 |
| CL (l/(h kg)) | 0.053 | 0.117 | 0.075 | 0.073 | 0.080 | 0.027 |
| AUC0–24 (mg h/L) | 89.06 | 36.24 | 60.76 | 59.46 | 61.38 | 21.62 |
| AUC0–∞ (mg h/L) | 95.09 | 42.62 | 66.44 | 68.05 | 68.05 | 21.45 |
AUC = area under the concentration-time curve; SD = standard deviation; CL = clearance; t1/2 = half life.
Table 36.
Pharmacokinetic parameters in rats after oral administration at 50 mg/kg.
| Animal no. | 1 | 2 | 3 | 4 | Mean | SD |
|---|---|---|---|---|---|---|
| t1/2α (h) | 1.35 | 0.67 | 1.78 | 1.55 | 1.33 | 0.48 |
| t1/2β (h) | 1.53 | 8.41 | 1.95 | 1.59 | 3.37 | 3.37 |
| t1/2 ka | 0.046 | 0.491 | 1.225 | 1.310 | 0.768 | 0.606 |
| AUC0–8 (mg h/l) | 2.41 | 1.52 | 0.55 | 0.93 | 1.35 | 0.81 |
| AUC0–∞ (mg h/l) | 2.67 | 1.86 | 0.62 | 1.05 | 1.55 | 0.91 |
| Bioavailability (%) | 0.39 | 0.27 | 0.09 | 0.15 | 0.23 | 0.13 |
| Tmax (h) | 3.00 | 2.00 | 2.00 | 4.00 | 2.75 | 0.96 |
| Cmax (μg/L) | 1000.2 | 611.3 | 192.3 | 895.2 | 674.8 | 361.2 |
Where t1/2ka is for the half-life of the absorption.
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; SD = standard deviation; Tmax = time of peak plasma concentration; t1/2β = elimination half-life.
6.2. Rhizoma Chuanxiong (川芎 chuān xiōng)
Ligustilide is the most abundant bioactive ingredient in Rhizoma Chuanxiong, a TCM herb commonly used for the treatment of cardiovascular ailments.
HPLC with an Agilent Series 1100 diode array detector was used to determine pharmacokinetic parameters of ligustilide in rats. The system was equipped with a Waters Symmetry C18 column (150 × 4.6 mm i.d., 5 μm) coupled and a guard column (Waters Spherisorb S5 ODS2, 10 × 4.6 mm i.d.). The samples are eluted using a mobile phase containing 0.25% aqueous acetic acid, v/v (A), and methanol (B). Oral bioavailability was estimated to be 2.6% at the 500-mg/kg dose. Ligustilide was monitored at 284 nm. The pharmacokinetic parameters of ligustilide in rats after intravenous, intraperitoneal, and oral administration are presented in Table 37. Seven metabolites of ligustilide were identified, and three of them were unequivocally characterized as butylidenephthalide, senkyunolide I, and senkyunolide H. These three compounds also occurred naturally in the herb and are reported to be bioactive.
Table 37.
Pharmacokinetic parameters of ligustilide in rats after intravenous, intraperitoneal, and oral administration (n = 5).
| Pharmacokinetic parameter | Administration route and dose (mg/kg) |
||||
|---|---|---|---|---|---|
| i.v. |
i.p. |
p.o. |
|||
| 15.6 | 14.9a | 26 | 52 | 500 | |
| Tmax (h) | – | – | 0.05 ± 0.02 | 0.08 ± 0.01 | 0.36 ± 0.19 |
| Cmax (mg/L) | 13.19 ± 0.84 | 6.93 ± 0.60*** | 7.48 ± 1.10*** | 20.75 ± 2.55### | 0.66 ± 0.23*** |
| t1/2 (h) | 0.31 ± 0.12 | 0.22 ± 0.07 | 0.36 ± 0.05 | 0.44 ± 0.08# | 03.43 ± 1.01*** |
| AUC 0-μ (mg/L)b | 1.81 ± 0.24 | 0.79 ± 0.10** | 0.93 ± 0.07* | 1.77 ± 0.23# | 0.047 ± 0.012** |
| Vd/F (L/kg)c | 3.76 ± 1.23 | 5.62 ± 1.19 | 6.54 ± 1.56 | 6.32 ± 1.81 | 1641.9 ± 121.6*** |
| CL/F (L/h/kg)c | 9.14 ± 1.27 | 20.35 ± 3.05** | 16.90 ± 1.21** | 9.26 ± 1.04## | 411.1 ± 145.7*** |
| MRT (h) | 0.30 ± 0.07 | 0.19 ± 0.03 | 0.30 ± 0.05 | 0.41 ± 0.03 | 5.14 ± 1.56*** |
| F (%) | 45.7d | 51.7 | 97.7 | 2.6 | |
*p 0.05, **p 0.01, ***p 0.001, compared with i.v. dosing of the isolated ligustilide.
#p 0.05, ##p 0.01, ###p 0.001, compared with the lower i.p. dose of the isolated ligustilide.
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; i.p. = intraperitoneal; i.v. = intravenous; MRT = mean residence time; p.o. = by mouth; Tmax = time of peak plasma concentration; CL = Clearance; Vd = Volume of Distribution; F = Absolute bioavailability; t1/2 = Half life; CL/F = apparent plasma clearance; Vd/F = apparent volume of distribution based on the terminal phase.
Dose of ligustilide in 100 mg/kg of Chuanxiong extract.
Normalized with dose.
Data represent Vd and CL in the case of i.v. dosing of the isolated ligustilide.
Relative bioavailability compared with that of i.v. dosing of the isolated ligustilide.
The oral bioavailability of ligustilide was low (2.6%), which was partly because of extensive first-pass metabolism in the liver.42
6.3. Rabdosia rubescens (冬凌草 dōng líng cǎo): Isodon rubescens (Hemsl.) (冬凌草 dōng líng cǎo)
Oridonin is a diterpenoid compound obtained from the Rabdosia rubescens (Labiatae) plant. The herb has been used traditionally as a digesting agent and anti-inflammatory agent. Oridonin has also been detected in other herbs such as Isodon trichocarpus, Isodon Japonicus, and Isodon shikokianus. It exhibits anti-inflammation, antibacterial, and antitumor effects.
Reverse phase-HPLC was used to determine the concentrations and pharmacokinetic parameters after oridonin was injected in rat plasma. The system was equipped with analytical DIKMA ODS C18 column (200 × 4.6 mm, 5 μm) with a DIKMA ODS C18 (4.6 × 12.5 mm i.d.) precolumn. The mobile phase was composed of acetonitrile-0.01M ammonium acetate (0.5% acetic acid) (30:70, v/v). The flow rate, column temperature, and UV detector wavelength are 1.0 mL/min, 25°C, and 238 nm, respectively. After tail vein injection of oridonin at 12.5 mg/kg dose in rats, oridonin in plasma are determined for a series of time points within 24 hours. The LOD and LLOQ are found to be 0.025 and 0.05 μg/mL, respectively. The two-compartment open model was used to determine the plasma oridonin concentration-time curve. The pharmacokinetics parameters calculated for intravenous administration of oridonin in rat are presented in Table 38. The oridonin is distributed quickly and was eliminated slowly in rats. The volume of distribution indicates that it might accumulate in certain organs or metabolize in the plasma.43
Table 38.
Pharmacokinetics parameters calculated from the intravenous oridonin study in the rat.
| Parameter | Value |
|---|---|
| t1/2α (h) | 0.12 |
| t1/2β (h) | 6.06 |
| CL (L/kg/h) | 1.56 |
| AUC (μg h/mL) | 7.96 |
| Vd (L/kg) | 1.83 |
AUC = area under the concentration-time curve; CL = clearance; Vd = volume of distribution.
6.4. Saposhnikovia divaricata (Turcz) (防風 fáng fēng)
Fangfeng, the root of Saposhnikovia divaricata (Turcz.) Schischk., is listed as a high-grade drug, which means high effectiveness and little toxicity in TCM. It is widely applied for headache, febrility, vertigo, and arthralgia due to wind, cold, and dampness in China, Japan, and other Asian countries. Prim-O-glucosylcimifugin and 4-O-d-glucosyl-5-O-methylvisamminol are the two major active chromones isolated from Fanfeng, which possess the analgesic, anti-inflammatory effect and suppression of platelet aggregation, and they may possess potential clinical applications such as treating acute and dull aching, infarction, and anti-inflammatory conditions.
HPLS/MS was used to determine the pharmacokinetic parameters and simultaneous detection of prim-O-glucosylcimifugin and 4-O-d-glucosyl-5-O-methylvisamminol in rat plasma and urine after single oral administration of Fangfeng extract. The system was equipped with an Agilent TC-C18 column (150 × 4.6 mm i.d., 5 μm), and with an ODS security guard column (10 × 4.6 mm i.d., 5 μm, Zhonghuida Co., China). The gradient mobile phase was composed of a methanol-water mixture containing 0.1% formic acid with a flow rate of 0.8 mL/min. The LLOQ of prim-O-glucosylcimifugin and 4-O-d-glucosyl-5-O-methylvisamminol was 1.0 ng/mL and 1.5 ng/mL in plasma, 10 ng/mL and 15 ng/mL in urine, respectively. The percent of two drugs excreted in the urine over the dose administered was 49.42% and 56.69% following oral administration. The pharmacokinetic parameters of prim-O-glucosylcimifugin and 4-O-d-glucosyl-5-O-methylvisamminol in rats after oral administration of Fangfeng extract are presented in Table 39. In this study, other than mentioned chromones two metabolites are also found, which need to be studied in detail.44
Table 39.
Pharmacokinetic parameters of prim-O-glucosylcimifugin and 4-O-d-glucosyl-5-O methylvisamminol in rats after oral administration of Fangfeng extract.
| Parameters | Compounds |
|
|---|---|---|
| Prim-O-glucosylcimifugin | 4-O-d-glucosyl-5-O-methylvisamminol | |
| T1/2 (h) | 1.31 | 1.96 |
| Cmax (ng/mL) | 39.92 | 41.53 |
| Tmax (h) | 0.54 | 0.56 |
| AUC(0–t) (ng/mL h) | 66.77 | 65.65 |
| AUC(0–∞) (ng/mL h) | 75.63 | 73.05 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; Tmax = time of peak plasma concentration.
6.5. S. japonica, S. mileensis (青葉膽 qīng yè dǎn), and S. chirata
Different plants of Swertia spp. S. japonica, S. mileensis, and S. chirata (Gentianceae) are well known in TCM and other Asian countries. These plants exhibit hepatoprotective, antiedematogenic, antihypolidemic, anti-spastic, anticholinergic, antinociceptive, antibacterial, anti-inflammatory, and anti-oxidant properties.
A LC-MS/MS method was used to determine pharmacokinetic parameters and quantification of swertiamarin in rats after oral administration. The system was equipped with a G6410B triple quadrupole mass spectrometer (Agilent), an ESI source, and an Agilent ZORBAX ECLIPSE XDB-C18 (100 × 2.1mm i.d., 1.8 μm) column. The isocratic elution of mobile phase was composed of methanol and water containing 0.1% acetic acid (25:75, v/v). The flow rate, column temperature, and internal standards are 0.2 mL/min, 40°C, and gentiopicroside, respectively. Pharmacokinetic parameters are calculated by using a noncompartmental model. The LLOQ was 5 ng/mL within a linear range of 5–1000 ng/mL (n = 7, r2 ≥ 0.994), and the LOD was 1.25 ng/mL (S/N ≥ 3). The pharmacokinetic parameters of swertiamarin after oral administration in rats are presented in Table 40. The pharmacokinetic data revealed that swertiamarin was rapidly absorbed into the circulation system after oral administration but it showed a short half-life of 1.50 hours.45 The absolute bioavailability of swertiamarin is around 10.3%. After oral administration to rats, it was rapidly and widely distributed in tissues. High concentrations were found in the liver and kidney, indicating that swertiamarin was possibly absorbed in the liver and eliminated by the kidney.46
Table 40.
Main pharmacokinetic parameters of swertiamarin after oral administration of 20 mg/kg to rats (n = 6, mean ± standard deviation).
| Parameters | Mean ± SD |
|---|---|
| t1/2z (h) | 1.104 ± 0.229 |
| Vz/F (L/kg) | 9.637 ± 4.322 |
| CLz/F (L/h/kg) | 5.638 ± 2.151 |
| AUC0–∞ (μg/L h) | 3593.7 ± 985.4 |
| MRT0–∞ (h) | 1.929 ± 0.364 |
| Tmax (h) | 0.945 ± 0.136 |
| Cmax (μg/L) | 1920.1 ± 947.0 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; MRT = mean residence time; SD = standard deviation; Tmax = time of peak plasma concentration; CL/F = Apparent clearance; CL = Clearance; t1/2 = Half life.
6.6. Strychnos nux vomica L. (馬錢子 mǎ qián zǐ)
Semen Strychni is the dried mature seed of Strychnos nux vomica L., a tree native in India. In classic Chinese Materia Medicas, the herbal drug is listed as a toxic herb and its biological effects (pharmacological and toxic effects) are dose dependent, needing to be processed to reduce the toxicity before clinical uses required by Chinese medicine prescriptions. Processed Semen Strychni is clinically used as an important ingredient in various remedies of traditional herbal medicines to treat nervous diseases, vomiting, arthritis, and pain from trauma, and to promote blood circulation and remove blood stasis. The most abundant alkaloids existing in the processed Semen Strychni are strychnine and brucine, which have been reported to possess analgesic, anti-inflammatory, and antitumor effects despite their toxicity.
LC-ESI-MS with positive electrospray ionization was used for simultaneous determination of strychnine, brucine, and pharmacokinetic parameters after oral administration of processed Semen Strychni to Wistar rats. The system was equipped with a Waters Symmetry TM C18 column (100 × 4.6 mm i.d., 5 μm,) kept at 30°C. The mobile phase was composed of methanol, 20mM ammonium formate, and formic acid (32:68:0.68, v/v/v) with a flow rate of 0.4 mL/min. The mean maximum plasma concentrations of strychnine and brucine detected in the rats are 54.93 and 4.95 ng/mL, respectively. Higher sensitivity was offered, with LLOQ of 0.5 and 0.1 ng/mL for strychnine and brucine, respectively, requiring only 0.1 mL of plasma.47 When both strychnine and brucine are individually incubated with rat liver S9 fraction, strychnine N-oxide and brucine N-oxide are the two metabolites that result.48
6.7. Stellera chamaejasme L. (狼毒 láng dú)
Stellera chamaejasme L. (Thymelaeaceae) is one of the toxic TCM listed in the Chinese Pharmacopeia. In recent years, it has also been used for the treatment of intestinal, gastric, and pulmonary cancers. Chamaechromone is a major biflavone constituent in dried roots of S. chamaejasme. The plant also shows anti-inflammatory, antiviral, cytotoxic, and antioxidant activity because of its biflavones and flavonoids contents.
A LC-MS with a positive ESI in MRM mode was used to determine the pharmacokinetics and absolute bioavailability chamaechromone in rat plasma. The system was equipped with an Xbridge TM C18 column (2.1 × 50 mm i.d., 3.5 μm, Waters). The mobile phase consisted of methanol-water containing 0.1% formic acid with a gradient elution starting at 5% methanol and progressing linearly to 90% methanol over 5.0 minutes, then returning to 5% methanol. Total run time was 6 minutes. The mobile phase was delivered at a flow rate of 0.4 mL/min. Rats receive 100 mg/kg chamaechromone by oral administration or intravenous injection of 5 mg/kg via the tail vein to determine the plasma concentration of chamaechromone in rats. The LLOQ of chamaechromone was 8 ng/mL. The pharmacokinetic parameters of chamaechromone in rats following intravenous and oral administration are provided in Table 41. The absolute bioavailability of chamaechromone was found to be 8.9%. Its poor absorption may be due to poor permeability through the intestinal epithelial membrane and efficient metabolism in the intestine, which is a common reason for low bioavailability of flavanoid compounds.49
Table 41.
Pharmacokinetic parameters of chamaechromone in rats following intravenous (5 mg/kg) and oral (100 mg/kg) administration.
| Oral |
Intravenous |
||
|---|---|---|---|
| Parameters | Mean ± SD | Parameters | Mean ± SD |
| Cmax (ng/L) | 795.9 ± 14.6 | C max (ng/L) | 4300.7 ± 113.6 |
| Tmax (h) | 11.3 ± 0.8 | t 1/2α (h) | 0.47 ± 0.22 |
| t1/2 (h) | 30.0 ± 19.3 | t1/2β (h) | 19.5 ± 9.5 |
| AUC0–60 (ng h/L) | 6976.7 ± 1026.9 | CL (L/(h kg)) | 1202.1 ± 121.8 |
| AUC0–∞ (ng h/L) | 7388.6 ± 940.0 | AUC0–48 (ng h/L) | 3672.1 ± 225.4 |
| CL z/F (L/(h kg)) | 13,731.8 ± 1871.6 | AUC0–∞(ng h/L) | 4129.2 ± 231.8 |
| Vz/F (L/kg) | 277,476.2 ± 132,126.1 | K10 (1/h) | 0.72 ± 0.66 |
| MRT0–t (h) | 18.5 ± 0.675 | K12 (1/h) | 1.67 ± 2.34 |
| MRT0–∞ (h) | 22.3 ± 4.9 | K21 (1/h) | 0.185 ± 0.261 |
| F (%) | 8.9 | MRT0–t (h) | 8.1 ± 0.67 |
| – | – | MRT0–∞ (h) | 16.1 ± 3.6 |
All data are expressed as mean ± SD (n = 6).
AUC = are under the concentration curve; Cmax = peak plasma concentration; MRT = mean residence time; SD = standard deviation; Tmax = time of peak plasma concentration; CL/F = apparent clearance; CL = clearance; F = absolute bioavailability; t1/2 = half life.
6.8. Salvia miltiorrhiza Bge (丹參 dān shēn)
The Chinese medicine, danshen, is the dried root and rhizome of Salvia miltiorrhiza Bge (Labiatae). Traditionally, danshen is believed to be effective in eliminating blood stasis, relieving pain, promoting blood flow, and stimulating menstrual discharge as well as easing the mind. Magnesium lithospermate B (MLB) has been found to have strong antioxidative and free-radical scavenging effects.
The LC-MS/MS method was used to determine the pharmacokinetics of MLB after intravenous administration and also detect the serum concentrations of MLB in beagle dogs. The system was equipped with CAPCELL PAK C18 column (50 × 2 mm i.d., 5 μm) and a Phenomenex C18 guard column. The mobile phase composed of 56% water (containing a mass fraction of 0.5% formic acid) and 44% acetonitrile at a flow rate 0.25 mL/min for an isocratic elution at room temperature. The pharmacokinetic parameters of MLB after intravenous administration in beagle dogs are presented in Table 42. This study indicates that MLB is rapidly distributed and metabolized in tissues and at a high dose, it shows saturated distribution.50 The catechol O-methyltransferase is responsible for formation of four (M1-M4) methylated metabolites in rats. The rapid and high biliary excretion levels of these metabolites suggested that they could undergo enterohepatic circulation and that they might thereby be largely responsible for the pharmacological effects of MLB.51
Table 42.
Pharmacokinetic parameters of magnesium lithospermate B after intravenous administration in beagle dogs.
| Parameter | Dose/mg/kg |
||
|---|---|---|---|
| 3 | 6 | 12 | |
| C0 (/mg/L) | 24 ± 4 | 47 ± 12 | 107 ± 15 |
| AUC0-tn (/mg·min/L) | 109 ± 24 | 248 ± 55 | 582 ± 84 |
| AUC 0-∞ (/mg·min/L) | 109 ± 24 | 248 ± 55 | 583 ± 84 |
| MRT0-∞ (/min) | 16.3 ± 3.8 | 14.8 ± 2.9 | 14.0 ± 0.8 |
| k10 (/h) | 13.2 ± 2.1 | 11.6 ± 1.5 | 11.2 ± 1.3 |
| k12 (/h) | 5.2 ± 1.6 | 3.9 ± 2.2 | 3.1 ± 0.5 |
| k21 (/h) | 1.5 ± 0.5 | 1.4 ± 0.4 | 1.4 ± 0.3 |
| V/L (/kg) | 1.7 ± 0.5 | 1.6 ± 0.6 | 1.3 ± 0.3 |
| T1/2α (/min) | 2.2 ± 0.2 | 2.7 ± 0.5 | 2.9 ± 0.3 |
| T1/2β (/min) | 43 ± 9 | 42 ± 7 | 42 ± 10 |
| CL(/mL/min/kg) | 28 ± 5 | 26 ± 7 | 21 ± 3 |
n = 6. Mean ± SD.
AUC = area under the concentration-time curve; MRT = mean residence time; SD = standard deviation; C0 = initial plasma concentration; CL = clearance; t1/2 = half life.
6.9. Salvia miltiorrhiza Bunge (丹參 dān shēn): Salvia miltiorrhiza Bge (丹參 dān shēn)
R-(+)-β-(3,4-dihydroxyphenyl)-lactic acid [named danshensu (Dhpl)] and protocatechuic aldehyde (Pal) have been considered the major active constituents of Salvia miltiorrhiza Bunge (Labiatae). Danshen (roots) of the plant has been used in TCM to treat coronary diseases, particularly angina pectoris and myocardial infarction. This plant also exhibits anticoagulant, antiarteriosclerotic, anti-inflammatory, and antihypoxic qualities.
The HPLC/UV method was used to determine the pharmacokinetic parameters of Dhpl and Pal. The system was equipped with an inertsil ODS-3 C18 reverse-phase column (250 × 4.6 mm i.d., 5 μm) and protected by RP18 (5 μm) guard column (Dikma, Beijing, China). The mobile phase consisted of 0.02% phosphoric acid-acetonitrile (91:9, v/v). The flow rate was 1 mL/min and the UV-vis detector was set at 280 nm. The LOQ for Dhpl and Pal was found to be 1.43 and 0.12 μg/mL, respectively. The pharmacokinetic parameters are determined by using non- compartmental analysis. The pharmacokinetics parameters of Dhpl and Pal after oral administration are presented in Table 43. The double-peak phenomenon was observed in these pharmacokinetic data and it may be due to the hepatoenteral circulation and redistribution in tissues phenomenon.52
Table 43.
Pharmacokinetics parameters of Dhpl and Pal after oral administration, dose 10 g/kg.
| Parameter |
Radix Salviae miltiorrhizae extract |
|
|---|---|---|
| Dhpl | Pal | |
| MRT (h) | 3.43 ± 0.07 | 4.31 ± 0.06 |
| AUC 0-∞ (μg·h/mL) | 396.82 ± 17.27 | 15.64 ± 0.66 |
| Calibration curve (μg/mL) | 1.43–228.48 a determination coefficient (r) of 0.996 (n = 8) | 0.12–7.94 a determination coefficient (r2) of 0.994 (n = 8) |
| LOQ (μg/mL) | 1.43. | 0.12 |
AUC = area under the concentration-time curve; LOQ = limit of quantification; MRT = mean residence time.
6.10. Stephania tetrandra (粉防己 fěn fáng jǐ)
Tetrandrine is an important bisbenzyl isoquinoline alkaloid isolated from the bulbous root of Stephania tetrandra S Moore (Menispermaceae) of TCM. It is widely use as an anti-inflammatory, antiallergic, antioxidant, and antifibrogenetic agent, as well as in immunomodulation and inhibition of platelet aggregation In addition to these pharmacological effects, tetrandrine also exhibits liver toxicity in dogs when administered in high doses for a relatively long period.
The LC/MS/MS method was used to determine the pharmacokinetic parameters of tetrandrine in rat plasma when administered as a single oral dose (50 mg/kg) in six Sprague Dawley rats. The system was equipped with a Dikma Diamonsil-C18 analytical column (4.6 × 150 mm i.d., 5 μm, Dikma Technologies, Beijing, China) at 35°C. The mobile phase consisted of acetonitrile-methanol-ammonium formate aqueous solution (20mM) containing 0.3% formic acid (20:30:50, v/v/v). The flow and LLOQ are 0.3 ml/min and 5 ng/ml respectively. The pharmacokinetic parameters after single oral administration standard in female Wister rats are presented in Table 44.53
Table 44.
Pharmacokinetic parameters of tetrandrine after single oral administration of 50 mg/kg in six Sprague Dawley rats.
| Parameter | Tetrandrine (50 mg/kg) |
|---|---|
| Tmax (h) | 6.0 ± 1.8 |
| Cmax (ng/mL) | 237.1 ± 95.9 |
| AUC(0–72) (μg/mL) | 6279.2 ± 2411.5 |
| AUC0→∞) (μg/mL) | 7002.7 ± 2528.0 |
| T1/2 (h) | 20.6 ± 3.7 |
| ke (L/h) | 0.034 ± 0.006 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; Tmax = time of peak plasma concentration; Ke : elimination rate constant; t1/2 = half life.
6.11. Silybum marianum L. (水飛薊 shuǐ fēi jì)
Silybum marianum L., also known as milk thistle, is widely use in traditional European medicine. Silymarin, a polyphenolic flavonoid isolated from milk thistle, primarily consists of four isomeric mixtures of active flavonolignans: silychristin, silydianin, and two groups of diastereoisomeric flavonolignans, silibinin, and isosilibinin. Silymarin is clinically useful for the treatment of toxic hepatitis, fatty liver, cirrhosis, ischemic injury, radiation toxicity, and viral hepatitis. It is a strong antioxidant capable of scavenging unconjugated radicals.
The LC method was used to measure unconjugated silibinin and total silibinin in rat plasma and bile. The system was equipped with a LiChrosorb RP-18 column (250 × 4 mm i.d., 5 μm, Merck) protected by guard column (Purospher STAR RP-18e, 5 μm) at room temperature (24 ± 1 °C). The mobile phases consisted of acetonitrile-10mM monosodium phosphate (pH 5.45 adjusted with orthophosphoric acid) (50:50, v/v). The flow rate and detection wavelength are 1 mL/min and 288 nm, respectively. The oral bioavailability of silibinin in rats was estimated to be 0.73%. Pharmacokinetic calculations are performed on each individual set of data using by noncompartmental method. The AUC was calculated according to the linear trapezoidal method. The pharmacokinetic parameters after silibinin administration are presented in Table 45, Table 46. The polyphenolic silibinin potentially go through Phase II conjugated reaction with glucuronidation. The conjugated metabolites are more water soluble, and they are possible in due course excreted in the urine and bile. It leads to poor bioavailability of silibinin. The absolute oral bioavailability of silibinin in rats was found to be approximately 0.95%. This may be due to the high reactivity with Phase II conjugation and poor absorption rate. The distribution ratio of AUCbile/AUCblood of silibinin suggests that the hepatobiliary elimination of silibinin may be regulated by active transport.54
Table 45.
Pharmacokinetic parameters after silibinin administration (100 mg/kg, intravenously and 500 mg/kg by mouth) for blood.
| Parameters | Silibinin (100 mg/kg i.v.) |
Silibinin (500 mg/kg p.o.) |
||
|---|---|---|---|---|
| Unconjugated | Total | Unconjugated | Total | |
| AUC (min mg/mL) | 5.5 ± 0.73 | 35.5 ± 5.9 | 0.26 ± 0.07 | 7.17 ± 1.42 |
| Cmax (μg/mL) | 256 ± 36 | 239 ± 19 | 8.5 ± 2.6 | 76 ± 15 |
| t1/2 (min) | 68 ± 7.2 | 105 ± 29 | 12.2 ± 1.8 | 77 ± 3.2 |
| Tmax | 0 | 8.2 ± 4.5 | 11 ± 1.8 | 30 ± 4.7 |
Data are expressed as mean ± standard error of the mean (n = 6).
AUC = area under the concentration time curve; Cmax = peak plasma concentration; i.v. = intravenous; p.o. = by mouth.
Table 46.
Pharmacokinetic parameters after silibinin administration (100 mg/kg, intravenous and 500 mg/kg by mouth) for bile.
| Parameters | Unconjugated | Total |
|---|---|---|
| AUC (min mg/mL) | 11.1 ± 2.84 | 1202 ± 186 |
| Cmax (μg/mL) | 517 ± 85 | 7910 ± 2080 |
| t1/2 (min) | 33 ± 8.3 | 97 ± 28 |
| Tmax | 5.1 ± 1.0 | 50 ± 18 |
| AUC bile/AUC blood | 3.1 ± 0.95 | 30 ± 9.4 |
Data are expressed as mean ± standard error of the mean (n = 6).
AUC = area under the concentration time curve; Cmax = peak plasma concentration.
7. Steroidal glycoalkaloids
Solanum spp. are well known for their steroidal glycoalkaloid properties, and solamargine is one of the steroid alkaloid glycosides present in them. Solamargine is useful as an antitumor agent in cancers of the colon, lung, and breast.
The HPLC method coupled with Shimadzu LCMS-2010A quadrupole MS by an ESI interface was used to determine the pharmacokinetic parameters of solamargine in rats. The system was equipped with a Shim-Pack VPODS C18 column (150 × 2.0 mm i.d., 5 μm) with a gradient elution of the mobile phase system consisting of acetonitrile (A) and 0.02% formic acid (B). The temperature of the column and auto-sampler was kept constant at 40°C and 10°C, respectively. Pharmacokinetic parameters in rats are estimated by a compartmental method. The studied method was successfully applied to analyze rat plasma samples after intravenous injection of solamargine at 1.0, 2.0, and 4.0 mg/kg in rats, supporting its applicability to biosample assay. The pharmacokinetic parameters after a single intravenous dose of 1.0, 2.0, and 4.0 mg/kg solamargine in rats are presented in Table 47. The pharmacokinetic data indicate that elimination or biotransformation of solamargine occurred relatively quickly in rats.55
Table 47.
Pharmacokinetic parameters after a single intravenous dose of 1.0, 2.0, and 4.0 mg/kg solamargine in rats (n = 5).
| Parameters | Mean ± SD |
||
|---|---|---|---|
| 1.0 mg/kg | 2.0 mg/kg | 4.0 mg/kg | |
| The plasma concentration at 5min (C5) (ng/mL) | 538.54 ± 278.79 | 1094.37 ± 694.87 | 2483.40 ± 272.89 |
| Cl (L/kg h) | 3.81 ± 0.68 | 4.10 ± 1.23 | 3.97 ± 0.44 |
| Vd (L/kg) | 20.16 ± 10.34 | 19.78 ± 12.55 | 15.68 ± 6.19 |
| t1/2 (h) | 3.54 ± 1.50 | 3.29 ± 1.52 | 2.76 ± 1.10 |
| AUC0–t (ng h/mL) | 242.41 ± 65.68 | 482.36 ± 138.07 | 947.74 ± 124.76 |
| AUC0–∞ (ng h/mL) | 270.50 ± 54.66 | 526.92 ± 161.72 | 1018.91 ± 117.26 |
AUC = area under the concentration time curve; SD = standard deviation; Cl = clearance; Vd = volume of distribution; t1/2 = half life.
7.1. Stephania cepharantha (金線吊烏龜 jīn xiàn diào wū guī)
FK-3000 [6,7-di-O-acetylsinococuline] is isolated from Stephania delavayi Diels (地不容 dì bù róng) and Stephania cepharantha. It exhibits antiviral action against the human immunodeficiency virus and also anticarcinogenic action in e breast cancer. FK-3000 also exhibits cytotoxic (apoptosis induction) and cytostatic (cell cycle arrest) effects.
A LC-MS with positive ESI was used to determine the pharmacokinetic parameters of FK-3000. The system was equipped with reverse-phase Gemini column (3.0 × 150 mm i.d., 5 μm, Phenomenex) with Security Guard TM (3.0 × 4.0 mm i.d., Phenomenex). The mobile phase is composed of acetonitrile and 0.1% formic acid (85:15, v/v) at a flow rate of 0.2 mL/min. The injection volume was 30 μL. The assay just described was applied to a pharmacokinetic (PK) study of FK-3000 using oral administration at a dose of 20 mg/kg in male rats. The LLOQ was found to be 10 ng/mL with a wide linear dynamic range from 10 ng/mL to 10,000 ng/mL. An optimized chromatographic run time of 9 minutes per sample yielded symmetric peaks for FK-3000. AUC0-t was calculated by a linear trapezoidal method. The pharmacokinetic parameters of FK-3000 [6,7-di-O-acetylsinococuline] isolated from Stephania delavayi are presented in Table 48.56
Table 48.
Pharmacokinetic parameters of FK-3000 [6,7-di-O-acetylsinococuline] isolated from Stephania delavayi.
| Pharmacokinetic parameters | Mean ± SD |
|---|---|
| Tmax (h) | 0.20 ± 0.06 |
| T1/2 (h) | 1.79 ± 0.09 |
| Cmax (ng/mL) | 251.9 ± 168.2 |
| MRT (h) | 1.61 ± 0.33 |
| AUC0–6 h (ng h/mL) | 209.3 ± 42.0 |
| AUC0–∞ (ng h/mL) | 245.7 ± 40.5 |
AUC = area under the concentration time curve; Cmax = peak plasma concentration; MRT = mean residence time; SD = standard deviation; Tmax = time of peak plasma concentration.
7.2. Tripterygium wilfordii Hook F (TWHF) (雷公藤 léi gōng téng)
Triptolide is a highly oxygenated diterpenoid triepoxide, is the major component responsible for the immunosuppressive and anti-inflammatory effects of Tripterygium wilfordii Hook F (TWHF), and serves as the quality control standard for TWHF. It is commonly used in the treatment of rheumatoid arthritis and other autoimmune diseases. Triptolide has a small margin between therapeutic and toxic doses and shows serious toxicity in the digestive, urogenital, and blood circulatory systems when its levels rise beyond the upper limits.
The LC/MS method was used to determine the pharmacokinetic parameters of triptolide. The system was equipped with a Zorbax Extend-C18 analytical column (4.6 × 150 mm i.d., 5 μm, Agilent Technologies) protected by a ODS guard column (Security Guard, Phenomenex) at 40°C. The mobile phase was composed of acetonitrile/methanol/0.05% triethylamine aqueous solution (20:50:30, v/v/v) at a flow rate of 1 mL/min. Under these conditions, triptolide eluted at approximately 3.2 minutes and the internal standard at 4.0 minutes. All measurements are carried out using the negative ion atmospheric pressure chemical ionization (APCI) mode. LLOQ was found to be 1 ng/mL in rat plasma. The pharmacokinetic parameters of triptolide in rats after oral or intravenous administration of triptolide are presented in Table 49. The current pharmacokinetic data reveal that triptolide was metabolized extensively, eliminated rapidly, and also showed that the toxicity produced by the triptolide was lag behind the exposure concentration.57
Table 49.
Pharmacokinetic parameters of triptolide in rats after oral or intravenous administration of triptolide.
| Parameter | Oral dose/mg/kg |
Intravenous dose/mg/kg |
||
|---|---|---|---|---|
| 0.6 | 1.2 | 2.4 | 0.6 | |
| ka (L/min) | 0.37 ± 0.17 | 0.39 ± 0.16 | 0.251 ± 0.09 | – |
| ke (L/min) | 0.03 ± 0.01 | 0.04 ± 0.02 | 0.03 ± 0.01 | – |
| V/F (L/kg) | 0.32 ± 0.34 | 0.33 ± 0.30 | 0.22 ± 0.17 | 1.27 ± 0.25 |
| T1/2 ka (min) | 2.19 ± 0.92 | 2.06 ± 0.83 | 3.00 ± 0.87 | – |
| T1/2 ke (min) | 21.70 ± 3.00 | 16.81 ± 5.24 | 20.40 ± 3.75 | 15.10 ± 4.44 |
| AUC(0–tn) (mg/L min) | 7057.14 ± 1826.04 | 10445.67 ± 3178.42 | 14538.98 ± 5636.58 | 9791.18 ± 585.88 |
| Tmax (min) | 11.00 ± 2.24 | 10.00 ± 0.00 | 10.00 ± 0.00 | – |
| Cmax (mg/L) | 254.00 ± 47.34 | 446.65 ± 112.86 | 537.33 ± 143.34 | – |
| CL/F (L/min/kg) | 0.06 ± 0.02 | 0.06 ± 0.02 | 0.06 ± 0.03 | 0.06 ± 0.01 |
n = 6, mean ± standard deviation.
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; Tmax = time of peak plasma concentration; CL/F = apparent clearance; Ke = elimination rate constant; Ka = absorption rate constant; t1/2 = half life.
7.3. Tripterygium wilfordii (雷公藤 léi gōng téng): Tripterygium wilfordii Hook F (TWHF) (雷公藤 léi gōng téng)
Triptolide, a diterpenoid triepoxide compound, isolated from the roots of Tripterygium wilfordii Hook F (Celastraceae, TWHF) is also commonly known as Thunder God Vine. In TCM it is used to treat some autoimmune disorders such as rheumatoid arthritis, systemic lupus erythematosus, and skin diseases.
The liquid chromatography with atmospheric pressure chemical ionization mass spectrometry (LC-APCI-MS) method was used to determine the pharmacokinetic parameters of triptolide. The system was equipped with a Zorbax Extend-C18 analytical column (4.6 × 150 mm i.d., 5 μm) protected by a ODS guard column (Security Guard, Phenomenex) at 40°C. The mobile phase composed of acetonitrile/methanol/0.05% triethylamine aqueous solution (30:50:20, v/v/v) at a flow rate of 0.75 mL/min. Triptolide eluted at approximately 3.3 minutes and the internal standard (prednisolone) at 4.0 minutes. The LOQ and total run time are 0.5 ng/mL and 5 minutes, respectively. The pharmacokinetic study of six beagle dogs following intragastric administration at a single dose of 0.05 mg/kg triptolide solution are presented in Table 50.58
Table 50.
The pharmacokinetic study of six beagle dogs following i.g. administration at a single dose of 0.05 mg/kg triptolide solution.
| Parameter | Values |
|---|---|
| Cmax | 28.03 ± 11.76 ng/mL |
| Tmax | 0.96 ± 0.30 h |
| MRT0−tn | 3.00 ± 0.54 h |
| T1/2ka | 0.50 ± 0.38 h |
Cmax = peak plasma concentration; MRT = mean residence time; Tmax = time of peak plasma concentration.
7.4. Verbascum sinuatum (毛蕊花 máo ruǐ huā), Orobanche rapum (列當 liè dāng), Cistanche salsa G. Beck (肉蓯蓉 ròu cōng róng), and Plantago psyllium L (車前 chē qián), Olea europaea (橄欖 gǎn lǎn)
Acteoside is a phenylethanoid glycoside having water-soluble polyphenolic compounds, which are widely distributed in many medicinal plants, including Verbascum sinuatum, Orobanche rapum, Cistanches salsa (C.A. Mey) G. Beck, and Plantago psyllium L, Olea europaea. Acteoside shows neuroprotective action and attenuated scopolamine-induced memory impairments in mice. Acteoside and its aglycones protect glutamate-induced excitotoxicity in a primary culture of rat cortical cells.
The LC with amperometric detection and microdialysis sampling method was used to determine pharmacokinetic profile protein-unbound acteoside in rat blood. Acteoside and dialysates was separated by using a Phenomenex Gemini column (150 × 2.0 mm i.d., 5 μm) with its guard column (10 × 2.0 mm i.d.). The mobile phase comprised acetonitrile-50mM monosodium phosphate (pH 2.8, adjusting with 85% orthophosphoric acid) (17:83, v/v), and the flow rate of the mobile phase was 0.2 mL/min. The LOD and LOQ for acteoside were found to be 2 ng/mL and 5 ng/mL, respectively. The pharmacokinetic parameters of acteoside in rats after 10 mg/kg administration are presented in Table 51. The pharmacokinetic data indicate that acteoside was unable to be detected in the brain dialysate and it also was rapidly distributed in the body.59
Table 51.
Pharmacokinetic parameters of acteoside in rats after 10 mg/kg administration.
| Parameters | Estimated |
|---|---|
| A (μg/mL) | 71.9 ± 30.9 |
| B (μg/mL) | 2.9 ± 0.5 |
| α (L/min) | 0.14 ± 0.03 |
| β (L/min) | 0.02 ± 0.004 |
| t1/2α (min) | 5.0 ± 1.2 |
| t1/2β (min) | 28.5 ± 4.7 |
| AUC (min μg/mL) | 592.3 ± 124.7 |
| Vss (mL/kg) | 277.7 ± 185.8 |
| Cl (mL/min/kg) | 17.7 ± 4.5 |
Data expressed as mean ± standard deviation (n = 6); t1/2, α: distribution half-life; t1/2, β: elimination half-life.
AUC = area under the concentration-time curve; Cl = clearance; Vss = volume of distribution at steady state.
7.5. Zingiber officinale (薑 jiāng)
Ginger, the dried rhizome of Zingiber officinale Roscoe (Zingiberaceae), is not only a popular spice and flavoring agent in a variety of foods, but also is an important dietary supplement for nausea and motion sickness. In TCM, fresh or processed ginger has been used for the treatment of many ailments. Ginger mainly contains essential oil and oleoresin. Oleoresin is the nonvolatile pungent component, and the major constituents of oleoresin have been identified as 6-gingerol, 8-gingerol, 10-gingerol, and 6-shogaol, which is the corresponding dehydration product of 6-gingerol.
A HPLC-MS method with positive ionization interface was used to determine the pharmacokinetic parameters of ginger oleoresin. The system was equipped with an Agilent Zorbax StableBond-C18 column (4.6 × 50 mm i.d., 1.8 μm) and the temperature was set at 30°C. The mobile phases consisted of 0.1% formic acid water (A) and acetonitrile (B). The flow rate and injection volume are 1.0 mL/min, and 2 μL, respectively. Pharmacokinetic parameters are estimated using noncompartmental analysis. LLOQ of 6-gingerol 0.0104, 8-gingerol 0.00357, 10-gingerol 0.00920, and 6-shogaol 0.00738 μg/mL. The pharmacokinetic parameters after single oral administration of 300 mg/kg ginger oleoresin in five rats are presented in Table 52. 6-Gingerol shows 90% plasma protein binding in rats and also extensive first-pass metabolism. 6-gingerol could be readily conjugated with glycuronic acid in the alimentary tract in vivo. It is also the reason for the low bioavailability. The 6-gingerol glucuronide was identified from bile and urine as the primary metabolite of rats orally administered 6-gingerol. As per pharmacological and toxicological consideration, Phase II metabolism of gingerols is important. In plasma, 6-gingerol was found in its glucuronide form and 8-gingerol, 10-gingerol, and 6-shogaol were distributed into blood in free form.60
Table 52.
Estimated pharmacokinetic parameters after single oral administration of 300 mg/kg ginger oleoresin to five rats.
| Parameter | 6-Gingerol | 8-Gingerol | 10-Gingerol | 6-Shogaol |
|---|---|---|---|---|
| AUC(0-t) (μg/mL/h) | 1.689 ± 0.38 | 0.177 ± 0.025 | 0.222 ± 0.021 | 0.14 ± 0.011 |
| MRT(0-t) (h) | 1.776 ± 0.502 | 1.845 ± 0.169 | 1.84 ± 0.263 | 1.932 ± 0.592 |
| T1/2 (h) | 3.574 ± 1.994 | 1.08 ± 0.439 | 1.576 ± 1.03 | 1.127 ± 0.745 |
| Tmax (h) | 1.167 ± 0.764 | 0.833 ± 0.289 | 0.361 ± 0.141 | 1 ± 0.866 |
| Cmax (μg/L) | 0.933 ± 0.545 | 0.092 ± 0.018 | 0.156 ± 0.012 | 0.111 ± 0.041 |
| CL/F (L/h/kg) | 57.43 ± 22.359 | 60.59 ± 8.849 | 154.898 ± 101.852 | 133.652 ± 14.032 |
AUC = area under the concentration-time curve; Cmax = peak plasma concentration; MRT = mean residence time; Tmax = time of peak plasma concentration; CL/F = apparent plasma clearance; t1/2 = half life.
8. Conclusion
Numerous herbal medicines as phytoformulations, phytochemicals, nutraceuticals, and functional food currently are available to improve health. Active principle obtained from the plants are the moribund source of treatment against the wide range of the diseases and in near future it may supersedes the synthetic moieties. These herbal medicines are not restricted to a particular ailment. Because these medicines are used with increasing frequency to improve health, it is essential to know the pharmacokinetic profile of the aliment being treated. ADME plays a central role in promoting more rational use and to map pharmacological actions of such herbal aliments. This pharmacokinetic profile acts as a blueprint for the medicinal plant. These data help justify the therapeutic, toxicological, and clinical value of herbal medicines. Recent research corroborates traditional claims and justifies use of herbal medicines for the welfare of the human beings. This necessitates further study of the many facets of these wonderful traditional herbal medicines. To support herbal medicine research in the near future and to expand activities, the current review will help those who are involved in natural product research.
Conflicts of interest
All authors have no conflicts of interest to declare.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
References
- 1.Evans W.C. 16th ed. Saunders Elsevier; Philadelphia: 2009. Trease and Evans Pharmacogonasy. [Google Scholar]
- 2.De Smet P.A. Herbal remedies. N Engl J Med. 2002;347:2046–2056. doi: 10.1056/NEJMra020398. [DOI] [PubMed] [Google Scholar]
- 3.Robinson M., Zhang X. World Health Organization; Geneva, Switzerland: 2011. The World Medicines Situation. [Google Scholar]
- 4.Sivasankari B., Pitchaimani S., Anandharaj M. A study on traditional medicinal plants of Uthapuram, Madurai District, Tamilnadu, South India. Asian. Pac J Trop Biomed. 2013;3:975–979. doi: 10.1016/S2221-1691(13)60188-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . WHO; Geneva, Switzerland: 2000. General Guidelines for Methodologies on Research and Evaluation of Traditional Medicine; pp. 3–4. [Google Scholar]
- 6.Vanachayangkul P., Butterweck V., Frye R. Determination of Visnagin in rat plasma by liquid chromatography with tandem mass spectrometry and its application to in vivo pharmacokinetic studies. J Chromatogr B. 2009;877:653–656. doi: 10.1016/j.jchromb.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 7.Niu Z., Chen F., Sun J. High-performance liquid chromatography for the determination of 3-n-butylphthalide in rat plasma by tandem quadrupole mass spectrometry: application to a pharmacokinetic study. J Chromatogr B. 2008;870:135–139. doi: 10.1016/j.jchromb.2008.05.044. [DOI] [PubMed] [Google Scholar]
- 8.Diao X., Ma Z., Wang H. Simultaneous quantitation of 3-n-butylphthalide (NBP) and its four major metabolites in human plasma by LC-MS/MS using deuterated internal standards. J Pharm Biomed Anal. 2013;78–79:19–26. doi: 10.1016/j.jpba.2013.01.033. [DOI] [PubMed] [Google Scholar]
- 9.Li Y., Zhang Y., Wang Z., Zhu J., Tian Y., Chen B. Quantitative analysis of atractylenolide I in rat plasma by LC-MS/MS method and its application to pharmacokinetic study. J Pharm Biomed Anal. 2012;58:172–176. doi: 10.1016/j.jpba.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 10.Rath K., Taxis K., Walz G., Gleiter C., Li S., Heide L. Pharmacokinetic Study of Artemisinin after oral intake of a traditional preparation of Artemisinin Annua L. (Annua Wormwood) Am J Trop Med Hyg. 2004;70:128–132. [PubMed] [Google Scholar]
- 11.Kuo C., Lee C., Lin S. Rapid determination of aristolochic acids I and II in herbal products and biological samples by ultra-high-pressure liquid chromatography-tandem mass spectrometry. Talanta. 2010;80:1672–1680. doi: 10.1016/j.talanta.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Lai L., Lin L., Lin J., Tsai T. Pharmacokinetic study of free mangiferin in rats by microdialysis coupled with microbore high-performance liquid chromatography and tandem mass spectrometry. J Chromatogr A. 2003;987:367–374. doi: 10.1016/s0021-9673(02)01415-2. [DOI] [PubMed] [Google Scholar]
- 13.Deng X., Zheng S., Gao G., Fan G., Li F. Determination and pharmacokinetic study of indirubin in rat plasma by high-performance liquid chromatography. Phytomedicine. 2008;15:277–283. doi: 10.1016/j.phymed.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Pi E., Chen J., Huang J., Hou A. A fast and sensitive HPLC-MS/MS analysis and preliminary pharmacokinetic characterization of cudratricusxanthone B in rats. J Chromatogr B. 2010;878:1953–1958. doi: 10.1016/j.jchromb.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 15.Singh S., Wahajuddin, Tewari D., Patel K., Jain G. Permeability determination and pharmacokinetic study of nobiletin in rat plasma and brain by validated high-performance liquid chromatography method. Fitoterapia. 2011;82:1206–1214. doi: 10.1016/j.fitote.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Q., Wang W., Li J. Simultaneous determination of catechin, epicatechin and epicatechin gallate in rat plasma by LC-ESI-MS/MS for pharmacokinetic studies after oral administration of Cynomorium songaricum extract. J Chromatogr B. 2012;880:168–171. doi: 10.1016/j.jchromb.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 17.Yang K., Lin L., Tseng T., Wang S., Tsai T. Oral bioavailability of curcumin in rat and the herbal analysis from Curcuma longa by LC-MS/MS. J Chromatogr B. 2007;853:183–189. doi: 10.1016/j.jchromb.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Ireson C., Jones D., Orr S. Metabolism of the cancer chemopreventive agent curcumin in human and rat intestine. Cancer Epidem Biomar. 2002;11:105–111. [PubMed] [Google Scholar]
- 19.Sun Y., Xu L., Wang Q. High-performance liquid chromatography/tandem mass spectrometry for simultaneous determination of four dicaffeoylquinic acids in rat plasma. J Chromatogr B. 2012;903:177–181. doi: 10.1016/j.jchromb.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 20.Li Y., Li Y., Yang Z., Xin N., Deng Y. A sensitive LC-MS/MS method to quantify loureirin B in rat plasma with application to preclinical pharmacokinetic studies. J Pharm Biomed Anal. 2009;50:983–986. doi: 10.1016/j.jpba.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Wang T., Liu Z., Li J. Determination of protodioscin in rat plasma by liquid chromatography-tandem mass spectrometry. J Chromatogr B. 2007;848:363–368. doi: 10.1016/j.jchromb.2006.10.050. [DOI] [PubMed] [Google Scholar]
- 22.Chen C., Qi L., Yi L., Li P., Wen X. Liquid chromatography-mass spectrometry analysis of macranthoidin B, macranthoidin A, dipsacoside B, and macranthoside B in rat plasma for the pharmacokinetic investigation. J Chromatogr B. 2009;877:159–165. doi: 10.1016/j.jchromb.2008.11.043. [DOI] [PubMed] [Google Scholar]
- 23.Wang G., Pan R., Liao Y., Chen Y., Tang J., Chang Q. An LC-MS/MS method for determination of forsythiaside in rat plasma and application to a pharmacokinetic study. J Chromatogr B. 2010;878:102–106. doi: 10.1016/j.jchromb.2009.11.029. [DOI] [PubMed] [Google Scholar]
- 24.Yang H., Yuan B., Li L., Chen H., Li F. HPLC determination and pharmacokinetics of chlorogenic acid in rabbit plasma after an oral dose of Flos Lonicerae extract. J Chromatogr Sci. 2004;42:173–176. doi: 10.1093/chromsci/42.4.173. [DOI] [PubMed] [Google Scholar]
- 25.Chen Z., Sun J., Chen H. Comparative pharmacokinetics and bioavailability studies of quercetin, kaempferol and isorhamnetin after oral administration of Ginkgo biloba extracts, Ginkgo biloba extract phospholipid complexes and Ginkgo biloba extract solid dispersions in rats. Fitoterapia. 2010;81:1045–1052. doi: 10.1016/j.fitote.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 26.Jun H., Yunan Z., Chao M., Weiyu W., Dongming X., Lijun D. Acid Hydrolytic Method for determination of ginkgo biloba total flavonoids in rat plasma by HPLC for pharmacokinetic studies. Tsinghua Sci Technol. 2010;15:452–459. [Google Scholar]
- 27.Tseng T., Tsai T. Measurement of unbound geniposide in blood, liver, brain and bile of anesthetized rats: an application of pharmacokinetic study and its influence on acupuncture. Analytica Chimica Acta. 2004;517:47–52. [Google Scholar]
- 28.Zhao Y., Wang X., Zhao Y., Gao X., Bi K., Yu Z. HPLC determination and pharmacokinetic study of homoeriodictyol-7- O -b -D-glucopyranoside in rat plasma and tissues. Biol Pharm Bull. 2007;30:617–620. doi: 10.1248/bpb.30.617. [DOI] [PubMed] [Google Scholar]
- 29.Xie H., Jia Y., Tan Z. LC-MS/MS determination of helicid in human plasma and its application in pharmacokinetic studies. J Chromatogr B. 2011;879:3607–3611. doi: 10.1016/j.jchromb.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 30.Ma G., Jiang X., Chen Z., Ren J., Li C., Liu T. Simultaneous determination of vitexin-4′-O-glucoside and vitexin-2′-O-rhamnoside from hawthorn leaves flavonoids in rat plasma by HPLC method and its application to pharmacokinetic studies. J Pharm Biomed Anal. 2007;44:243–249. doi: 10.1016/j.jpba.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 31.Yu H., Li W., Cheung M. Development and validation of an HPLC-DAD method for bis(12)-hupyridone and its application to a pharmacokinetic study. J Pharm Biomed Anal. 2009;49:410–414. doi: 10.1016/j.jpba.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 32.Du Y., Liu P., Shi X. A novel analysis method for diterpenoids in rat plasma by liquid chromatography-electrospray ionization mass spectrometry. Anal Biochem. 2010;407:111–119. doi: 10.1016/j.ab.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 33.Oufir M., Sampath C., Butterweck V., Hamburger M. Development and full validation of an UPLC-MS/MS method for the determination of an anti-allergic indolinone derivative in rat plasma, and application to a preliminary pharmacokinetic study. J Chromatogr B. 2012;902:27–34. doi: 10.1016/j.jchromb.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 34.Han D., Chen C., Zhang C., Zhang Y., Tang X. Determination of mangiferin in rat plasma by liquid-liquid extraction with UPLC-MS/MS. J Pharm Biomed Anal. 2010;51:260–263. doi: 10.1016/j.jpba.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 35.Bai X., Qu J., Lu J., Kano Y., Yuan D. Pharmacokinetics of kakkalide and its main metabolites in rat plasma determined by HPLC-DAD and LC-MS. J Chromatogr B. 2011;879:395–402. doi: 10.1016/j.jchromb.2010.12.025. [DOI] [PubMed] [Google Scholar]
- 36.Qu J., Gao J., Sun J., Zhang L., Makino T., Yuan D. Pharmacokinetics of conjugated metabolites in rat plasma after oral administration of tectoridin. J Chromatogr B. 2012;902:61–69. doi: 10.1016/j.jchromb.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 37.Xie Y., Zhou H., Wong Y., Xu H., Jiang Z., Liu L. Study on the pharmacokinetics and metabolism of paeonol in rats treated with pure paeonol and an herbal preparation containing paeonol by using HPLC-DAD-MS method. J Pharm Biomed Anal. 2008;46:748–756. doi: 10.1016/j.jpba.2007.11.046. [DOI] [PubMed] [Google Scholar]
- 38.Yoo H., Lee S., Lim S. LC-MS/MS method for determination of hederacolchiside E, a neuroactive saponin from Pulsatilla koreana extract in rat plasma for pharmacokinetic study. J Pharm Biomed Anal. 2008;48:1425–1429. doi: 10.1016/j.jpba.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 39.Ma H., Wang Y., He T., Chang X., Pu X. Simultaneous determination of tetrahydropalmatine, protopine, and palmatine in rat plasma by LC-ESI-MS and its application to a pharmacokinetic study. J Pharm Biomed Anal. 2009;49:440–446. doi: 10.1016/j.jpba.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 40.Ying P., Jian-Guo S., Guang-Ji W. Pharmacokinetic study of rhein and its carboxyl-esterification derivatives in rats. Chin J Nat Med. 2009;7:228–233. [Google Scholar]
- 41.Liang M., Zhang W., Zhang C. Quantitative determination of the anticancer agent tubeimoside I in rat plasma by liquid chromatography coupled with mass spectrometry. J Chromatogr B. 2007;845:84–89. doi: 10.1016/j.jchromb.2006.07.053. [DOI] [PubMed] [Google Scholar]
- 42.Yan R., Ling Ko N. Pharmacokinetics and metabolism of ligustilide, a major bioactive component in Rhizoma Chuanxiong, in the rat. Drug Metab Dispos. 2007;36:400–408. doi: 10.1124/dmd.107.017707. [DOI] [PubMed] [Google Scholar]
- 43.Ge J., You-Wei W., Xiao-Cong L., Ji-Yue C. Determination of oridonin in rat plasma by reverse-phase high performance liquid chromatography. J Pharm Biomed Anal. 2007;43:793–797. doi: 10.1016/j.jpba.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 44.Dai J., Chen X., Cheng W. A sensitive liquid chromatography-mass spectrometry method for simultaneous determination of two active chromones from Saposhnikovia root in rat plasma and urine. J Chromatogr B. 2008;868:13–19. doi: 10.1016/j.jchromb.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 45.Li H., Peng X., He J. Development and validation of a LC-ESI-MS/MS method for the determination of swertiamarin in rat plasma and its application in pharmacokinetics. J Chromatogr B. 2011;879:1653–1658. doi: 10.1016/j.jchromb.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 46.Li H.L., He J.C., Bai M. Determination of the plasma pharmacokinetic and tissue distributions of swertiamarin in rats by liquid chromatography with tandem mass spectrometry. Arzneimittelforschung. 2012;62:138–144. doi: 10.1055/s-0031-1298021. [DOI] [PubMed] [Google Scholar]
- 47.Xu Y., Si D., Liu C. Determination of strychnine and brucine in rat plasma using liquid chromatography electrospray ionization mass spectrometry. J Pharm Biomed Anal. 2009;49:487–491. doi: 10.1016/j.jpba.2008.10.020. [DOI] [PubMed] [Google Scholar]
- 48.Chen X., Lai Y., Cai Z. Simultaneous analysis of strychnine and brucine and their major metabolites by liquid chromatography-electrospray ion trap mass spectrometry. J Anal Toxicol. 2012;36:171–176. doi: 10.1093/jat/bks004. [DOI] [PubMed] [Google Scholar]
- 49.Lou Y., Hu H., Liu Y. Determination of chamaechromone in rat plasma by liquid chromatography-tandem mass spectrometry: application to pharmacokinetic study. J Pharm Biomed Anal. 2011;55:1163–1169. doi: 10.1016/j.jpba.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 50.Li X., Yu C., Sun W. Pharmacokinetics of magnesium lithospermate B after intravenous administration in beagle dogs. Acta Pharmacol Sin. 2004;25:1402–1407. [PubMed] [Google Scholar]
- 51.Zhang Y., Akao T., Nakamura N. Magnesium lithospermate b is excreted rapidly into rat bile mostly as methylated metabolites, which are potent antioxidants. Drug Metab Dispos. 2004;32:752–757. doi: 10.1124/dmd.32.7.752. [DOI] [PubMed] [Google Scholar]
- 52.Ye G., Wang C., Li Y.Y., Ren H., Guo D.A. Simultaneous determination and pharmacokinetic studies on (3,4-Dihydroxyphenyl)-lactic acid and protocatechuic aldehyde in rat serum after oral administration of radix Salviae miltiorrhizae extract. J Chromatogr Sci. 2003;41:327–330. doi: 10.1093/chromsci/41.6.327. [DOI] [PubMed] [Google Scholar]
- 53.Song N., Zhang S., Li Q., Liu C. Establishment of a liquid chromatographic/mass spectrometry method for quantification of tetrandrine in rat plasma and its application to pharmacokinetic study. J Pharm Biomed Anal. 2008;48:974–979. doi: 10.1016/j.jpba.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 54.Wu J., Lin L., Hung S., Chi C., Tsai T. Analysis of silibinin in rat plasma and bile for hepatobiliary excretion and oral bioavailability application. J Pharm Biomed Anal. 2007;45:635–641. doi: 10.1016/j.jpba.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 55.Zheng X., Xu L., Liang Y. Quantitative determination and pharmacokinetic study of solamargine in rat plasma by liquid chromatography-mass spectrometry. J Pharm Biomed Anal. 2011;55:1157–1162. doi: 10.1016/j.jpba.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 56.Lee J., Chae Y., Lee K. Development of a LC-MS method for quantification of FK-3000 and its application to in vivo pharmacokinetic study in drug development. J Pharm Biomed Anal. 2012;70:587–591. doi: 10.1016/j.jpba.2012.05.030. [DOI] [PubMed] [Google Scholar]
- 57.Shao F., Wang G., Xie H., Zhu X., Sun J., Jiye A. pharmacokinetic study of triptolide, a constituent of immunosuppressive, Chinese herb medicine, in rRats. Biol Pharm Bull. 2007;30:702–707. doi: 10.1248/bpb.30.702. [DOI] [PubMed] [Google Scholar]
- 58.Shao F., Wang G., Sun J. Liquid chromatographic/mass spectrometry assay of triptolide in dog plasma and its application to pharmacokinetic study. J Pharm Biomed Anal. 2006;41:341–346. doi: 10.1016/j.jpba.2005.11.026. [DOI] [PubMed] [Google Scholar]
- 59.Wu Y., Tsai T., Lin L., Tsai T. Liquid chromatographic method with amperometric detection to determine acteoside in rat blood and brain microdialysates and its application to pharmacokinetic study. J Chromatogr B. 2007;853:281–286. doi: 10.1016/j.jchromb.2007.03.033. [DOI] [PubMed] [Google Scholar]
- 60.Wang W., Li C., Wen X., Li P., Qi L. Simultaneous determination of 6-gingerol, 8-gingerol, 10-gingerol and 6-shogaol in rat plasma by liquid chromatography-mass spectrometry: application to pharmacokinetics. J Chromatogr B. 2009;877:671–679. doi: 10.1016/j.jchromb.2009.01.021. [DOI] [PubMed] [Google Scholar]