Abstract
Background
Members of armed forces worldwide are considered to be very susceptible to sexually transmitted infections, thus falling into a high-risk group of blood donors regarding transfusion-transmissible infections. In the Serbian Military Medical Academy a significant number (44% for the period 2005–2013) of blood donations were from members of the Serbian Army. The aim of this study was to determine the significance of military blood donors for the safety of blood transfusion.
Material and methods
Between January 2005 and December 2013, a total of 155,479 blood donations were tested for hepatitis B virus (HBV), hepatitis C virus (HCV), human immunodeficiency virus (HIV) and syphilis using serological assays (enzyme immunoassays, chemiluminescent microparticle immunoassay and western blot) and molecular testing (polymerase chain reaction analysis).
Results
The percentage of blood donations positive for transfusion-transmissible infections in the estimated period was 0.38%, and the percentage of HBV, HCV, HIV and syphilis positive blood donations was 0.20%, 0.12%, 0.005% and 0.06%, respectively. During that period, the percentage of all transfusion-transmissible infections, and in particular of HBV and HCV, declined significantly. In contrast, the percentage of HIV and syphilis positive blood donations remained unchanged. Higher rates of positivity for transfusion-transmissible infections in blood donations from members of the Serbian Army were not found, especially after mandatory military service was abolished in 2009.
Discussion
The reported rate of positivity for transfusion-transmissible infections in blood donations from the Military Medical Academy was considered low. This information is of great significance for further implementation of public health measures.
Keywords: blood donations, members of armed forces, transfusion-transmitted infections
Introduction
Transfusion-transmitted infections (TTI) are still one of the most serious complications of blood transfusion1. They lead to chronic and life-threatening disorders, so a huge number of scientific researchers have focused on this problem in order to improve blood transfusion practice and, particularly, to improve the safety of blood transfusions. Although the prevalence of TTI varies depending on the investigated region and the level of economic development, mandatory serological screening for TTI in blood donors together with improved health care conditions have reduced TTI in most countries1.
According to Serbian health legislation, every blood donation is tested for four TTI: human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV) and Treponema pallidum (the cause of syphilis). With approximately 17,000 blood donations per year, the Institute for Transfusiology and Haemobiology of the Military Medical Academy (MMA) is one of the most important transfusion centres in Serbia where blood donations from both military personnel of the Serbian Army and from civilians are collected. Although there are many local blood transfusion centres in Serbia, where mandatory donor blood testing is performed, only the MMA and Serbian Blood Transfusion Institute, process blood collected throughout the country. Besides, the MMA is the only transfusion centre in which blood donations from military personnel of the Serbian Army are collected. The MMA is also one of the most important hospitals in Serbia, providing medical care for military, civilian, Serbian and foreign patients. The need for blood at the MMA is very large since about 20,000 surgical interventions are performed yearly. Interventions usually done at the MMA include solid organ and hematopoietic stem cell transplantations, which are among the most complicated interventions in Serbia. This makes estimation of the number of TTI-positive blood donations especially significant since more than 40% of blood donations at the MMA were from members of the Serbian Army. It is well-known that members of armed forces worldwide are particularly exposed to sexually transmitted infections2. In peacetime, the incidence of these infections among members of armed forces may be two to five times higher than among civilians, while it can be even 50 times higher during armed conflicts3. The participation of the Serbian armed forces in peacekeeping missions in many regions makes them susceptible to TTI and it is routine procedure to test the personnel for HBV, HCV and HIV after their missions. Within the last decade, only one survey of the prevalence of TTI among members of the Serbian Army was published4. That survey of 5,617 members of the Serbian Army, in the period 2007–2008, found no HIV-positive cases, while the prevalence of HBV, HCV and syphilis was 0.28%, 0.34% and 0.02%, respectively. Except for these data, there is no updated information on the prevalence of TTI among blood donors (military or civilians) in either Serbia or the majority of neighbouring countries. Croatia is the only neighbouring country in which the Institute for Transfusion Medicine provides current data about the prevalence of TTI5. Since the prevalence of TTI can change significantly in a relatively short period of time6, there is a constant need to get applicable data. There have been intensive population movements in the last decades in the region of former Yugoslav countries, but comparison with data published at that time might be of no help. In 2005, a reorganisation of the Serbian Army was started; this was accompanied by staff redundancy and significant changes in the age and education structure of the army with the prominent changes occurring in 2009/2010 with the abolishment of conscription (mandatory military service) in 2009. Such extensive changes could have affected the number of TTI-positive blood donations in the MMA. In this survey, we estimated the trend of TTI in the MMA in the period from 2005 to 2013. This information might be of significance for further implementation of public health measures in order to improve the safety of blood transfusions.
Materials and methods
A total of 155,479 blood donations were collected from military and civilian voluntary blood donors throughout Serbia and tested at the Institute for Transfusiology and Haemobiology, MMA, between January 2005 and December 2013. According to the Serbian National Regulation, militaries are professional members of the Ministry of Defence and Serbian Army (officers, non-commissioned officers and professional soldiers). Civilians are defined as all citizens of Serbia who are not active members of the Serbian Army. As required by the universal guidelines for blood donations in Serbia, blood donors are aged from 18 to 65 years old. Potential donors at high risk of having infections are recognised and excluded from blood donation procedures based on a self-exclusion questionnaire and medical-history evaluation. In the estimated period, serum samples of 155,479 blood donations were tested for HBV, HCV, HIV and syphilis. Tests were performed using commercially available kits according to the manufacturers’ instructions and algorithms for every marker tested separately. The blood donations were tested for TTI by first-line and latest-generation immunoenzyme assays, by confirmatory assays, and by nucleic acid amplification testing.
The percentages of total TTI, HBV-, HCV- and syphilis-positive donations (analogous to the prevalence) were calculated using the following equation:
The percentages of total TTI, HBV-, HCV- and syphilis-positive donations of repeated blood donors only (analogous to the incidence) were also calculated using the equation:
The Chi-square test (software available on http://www.quantpsy.org/chisq/chisq.htm webpage)7 was used to assess the significance of year-to-year fluctuations in the prevalence of TTI. Linear regression analysis (conducted in the OriginPro 8 programme [OriginLab, Northampton, MA, USA]) was used to establish the time course (trends) of the prevalence of TTI. P-values of <0.05 were considered statistically significant.
Results
Overall, 155,479 blood donations were collected at the MMA, Belgrade during 2005–2013. Of these, 309 blood donations were positive for HBV, 187 for HCV, 8 for HIV, and 93 for syphilis (Table I). No simultaneous infections with two or more agents were detected in any of the 597 positive blood donations. The percentage of infected blood samples in the study period was 0.38% while the percentages of HBV-, HBC-, HIV- and syphilis-infected blood donations were 0.20%, 0.12%, 0.005% and 0.06%, respectively (Table I). The year-to-year fluctuations in the overall prevalence of TTI and in the prevalences of HBV and HCV were statistically significant (Table I). Table II shows the data on the origin of the TTI-positive blood donations. According to these data, the percentages of TTI-positive blood donations from repeated blood donors were 0.0005% for total TTI, 0.0003% for HBV, 0.0001% for HCV, 0.00001% for HIV and 0.0001% for syphilis.
Table I.
Transfusion-transmissible infections in blood donations to the Military Medical Academy, Belgrade, Serbia during the period 2005–2013.
| Year | N. of blood units | Prevalence | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| HBV | HCV | HIV | Syphilis | ||||||
|
|
|||||||||
| N. | % | N. | % | N. | % | N. | % | ||
| 2005 | 18,073 | 51 | 0.28 | 30 | 0.17 | 1 | 0.006 | 8 | 0.04 |
| 2006 | 18,113 | 46 | 0.25 | 22 | 0.12 | 1 | 0.006 | 8 | 0.04 |
| 2007 | 19,084 | 40 | 0.21 | 29 | 0.15 | 1 | 0.005 | 13 | 0.07 |
| 2008 | 18,081 | 43 | 0.24 | 24 | 0.13 | 1 | 0.006 | 10 | 0.06 |
| 2009 | 17,166 | 36 | 0.21 | 33 | 0.19 | 1 | 0.006 | 13 | 0.08 |
| 2010 | 17,401 | 31 | 0.18 | 15 | 0.09 | 1 | 0.006 | 16 | 0.09 |
| 2011 | 14,440 | 24 | 0.17 | 14 | 0.10 | 0 | 0.000 | 8 | 0.06 |
| 2012 | 16,583 | 17 | 0.10 | 13 | 0.08 | 1 | 0.006 | 7 | 0.04 |
| 2013 | 16,538 | 21 | 0.13 | 7 | 0.04 | 1 | 0.006 | 10 | 0.06 |
|
| |||||||||
| Total | 155,479 | 309 | 0.20 | 187 | 0.12 | 8 | 0.005 | 93 | 0.06 |
|
| |||||||||
| p* | 0.002 | 0.001 | 0.9 | 0.6 | |||||
N: absolute number of positive blood donations; %: percentage of positive blood donations;
significance of year-to-year fluctuation, determined by the Chi-square test.
HBV: hepatitis B virus; HCV: hepatitis C virus; HIV: human immunodeficiency virus.
Table II.
Demographic data on blood donations positive for transfusion-transmissible infections at the Military Medical Academy, Belgrade, Serbia.
| HBV | HIV | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| 2005–2013 | 2005–2009 | 2010–2013 | 2005–2013 | 2005–2009 | 2010–2013 | |||||||
| Positive | 309 | (100) | 216 | (100) | 93 | (100) | 8 | 5 | 3 | |||
| Military status | ||||||||||||
| Military | 168 | (54) | 147 | (68) | 21 | (23) | 3 | 3 | 0 | |||
| Civilian | 141 | (46) | 69 | (32) | 72 | (77) | 5 | 2 | 3 | |||
| Sex | ||||||||||||
| Male | 298 | (96) | 209 | (97) | 89 | (96) | 7 | 4 | 3 | |||
| Female | 11 | (4) | 7 | (3) | 4 | (4) | 1 | 1 | 0 | |||
| Donor status | ||||||||||||
| New | 270 | (87) | 186 | (86) | 84 | (90) | 6 | 4 | 3 | |||
| Repeat | 39 | (13) | 30 | (14) | 9 | (10) | 2 | 1 | 0 | |||
| Donor age (years) | ||||||||||||
| 18–29 | 149 | (48) | 126 | (58) | 23 | (25) | 3 | 3 | 0 | |||
| 30–39 | 47 | (15) | 29 | (13) | 18 | (19) | 1 | 1 | 0 | |||
| 40–49 | 52 | (17) | 23 | (11) | 29 | (31) | 4 | 1 | 3 | |||
| 50–65 | 56 | (18) | 33 | (15) | 23 | (25) | 0 | 0 | 0 | |||
|
| ||||||||||||
| HCV | Syphilis | |||||||||||
|
| ||||||||||||
| Positive | 187 | (100) | 138 | (100) | 49 | (100) | 93 | (100) | 52 | (100) | 41 | (100) |
| Military status | ||||||||||||
| Military | 118 | (63) | 108 | (78) | 10 | (20) | 29 | (31) | 22 | (42) | 7 | (17) |
| Civilian | 69 | (37) | 30 | (22) | 39 | (80) | 64 | (69) | 30 | (58) | 34 | (83) |
| Sex | ||||||||||||
| Male | 173 | (93) | 130 | (94) | 43 | (88) | 81 | (87) | 46 | (88) | 35 | (85) |
| Female | 14 | (7) | 8 | (6) | 6 | (12) | 12 | (13) | 6 | (12) | 6 | (15) |
| Donor status | ||||||||||||
| New | 165 | (88) | 124 | (90) | 41 | (84) | 67 | (72) | 39 | (75) | 28 | (68) |
| Repeat | 22 | (12) | 14 | (10) | 8 | (16) | 26 | (28) | 13 | (25) | 13 | (32) |
| Donor age (years) | ||||||||||||
| 18–29 | 134 | (72) | 118 | (86) | 16 | (33) | 21 | (23) | 19 | (37) | 2 | (5) |
| 30–39 | 26 | (14) | 8 | (6) | 18 | (37) | 14 | (15) | 5 | (10) | 9 | (22) |
| 40–49 | 15 | (8) | 7 | (5) | 8 | (16) | 21 | (23) | 6 | (12) | 15 | (37) |
| 50–65 | 12 | (6) | 5 | (4) | 7 | (14) | 37 | (40) | 22 | (42) | 15 | (37) |
Data are reported as absolute numbers and percentages (%) of positive blood donations. For HIV positive blood donors, the percentage values were not calculated because of the small number. HBV: hepatitis B virus; HCV: hepatitis C virus; HIV: human immunodeficiency virus.
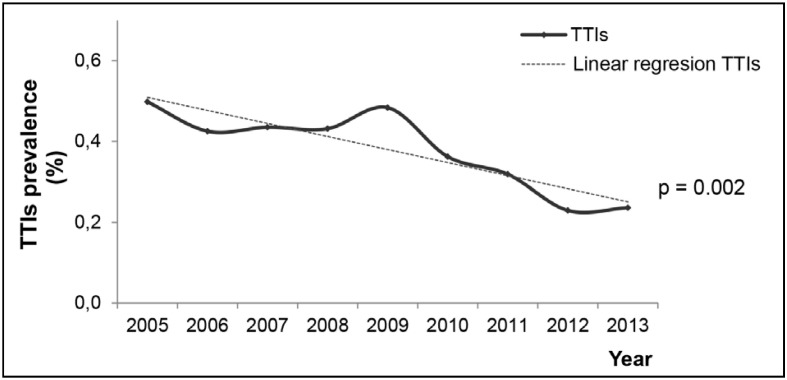
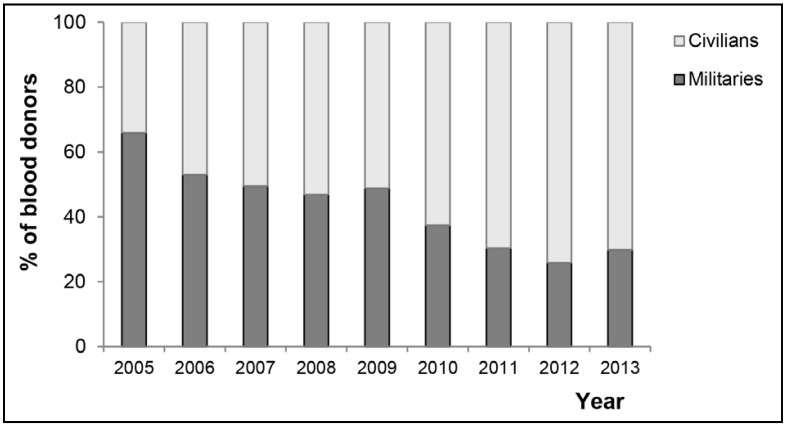
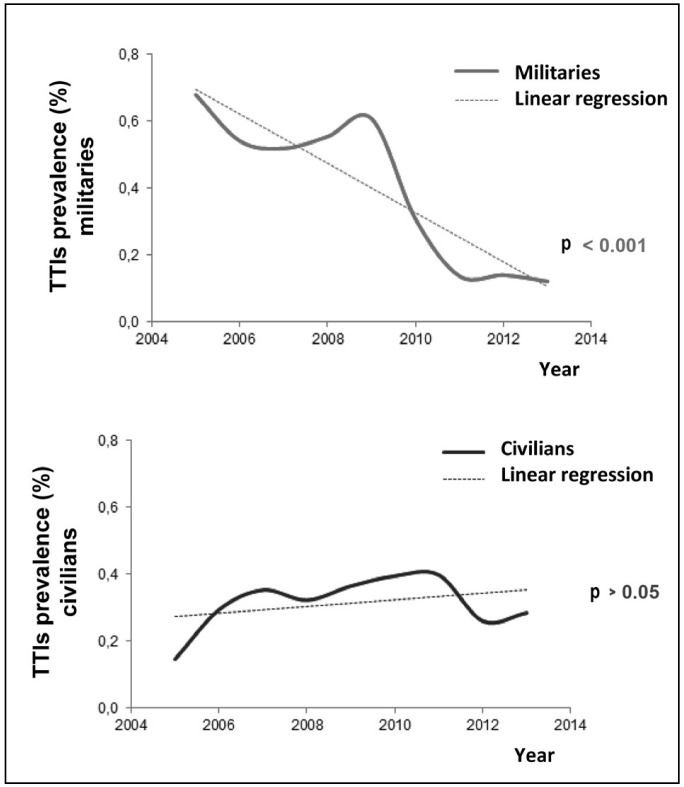
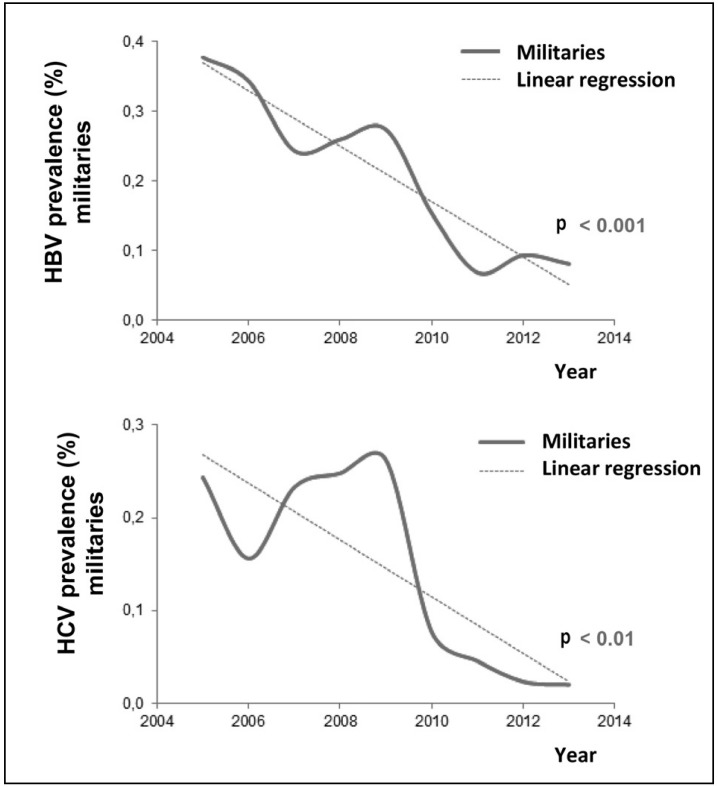
Over the study period, a significant declining trend in TTI- positivity was recorded (Figure 1) which was the result of decreasing numbers of HBV- and HCV-positive donations (Table I). The number of HIV-positive samples was stable, while a slight and statistically not significant increase in the number of syphilis-positive samples was found (Table I). According to the reorganisation of the Serbian armed forces, over the period 2005–2013, the contribution of blood donations from the army decreased from 65% to 30% (Figure 2). In the entire period considered, syphilis-positive samples were predominantly from civilians, while HBV- and HCV-positive samples were predominantly from military personnel (Table III). However, after conscription had been abolished (e.e the period from 2010–2013) positive samples for all the tested TTI were predominantly from civilians (Table III). Linear regression analysis confirmed no change in the percentage of TTI-positive blood donations from civilians (Figure 3). A statistically significant declining trend in the number of TTI-positive samples (Figure 3), in particular, for HBV and HCV, from military blood donors was observed in 2005–2013 (Figure 4). The strongest declining trend among this group of blood donors was detected after 2010, when conscription in Serbia was abolished.
Figure 1.
Declining percentage of blood donations positive for transfusion-transmissible infections (TTIs) over the period 2005–2013 in the Military Medical Academy, Belgrade, Serbia.
p: significance of the trend.
Figure 2.
Progressive decline of military personnel among blood donors at the Military Medical Academy, Belgrade, Serbia over the period 2005–2013.
Table III.
Percentage of transfusion-transmissible infections (TTIs) in blood donations from military or civilian blood donors at the Military Medical Academy, Belgrade, Serbia, before (2005–2009) and after (2010–2013) abolishing conscription (mandatory military service).
| 2005–2013 (%) | |||
|---|---|---|---|
|
| |||
| Militaries (N. 67,951) | Civilians (No 87,528) | p | |
| HBV | 0.25 | 0.16 | <0.001* |
| HCV | 0.17 | 0.08 | <0.001* |
| HIV | 0.006 | 0.005 | ns |
| Syphilis | 0.04 | 0.07 | <0.05* |
|
| |||
| Total TTIs | 0.47 | 0.32 | <0.001* |
|
| |||
| 2005–2009 (%) | |||
|
| |||
| Militaries (N. 42,683) | Civilians (N. 47,834) | p | |
|
| |||
| HBV | 0.31 | 0.16 | <0.001* |
| HCV | 0.23 | 0.07 | <0.001* |
| HIV | 0.006 | 0.005 | ns |
| Syphilis | 0.05 | 0.07 | ns |
|
| |||
| Total TTI | 0.59 | 0.31 | <0.001* |
|
| |||
| 2010–2013 (%) | |||
|
| |||
| Militaries (N. 20,117) | Civilians (N. 44,845) | p | |
|
| |||
| HBV | 0.10 | 0.36 | 0.08# |
| HCV | 0.04 | 0.20 | 0.06# |
| HIV | 0.005 | 0.004 | ns |
| Syphilis | 0.03 | 0.08 | 0.06# |
|
| |||
| Total TTI | 0.19 | 0.33 | <0.05 |
HBV: hepatitis B virus; HCV: hepatitis C virus; HIV: human immunodeficiency virus;
a statistically significant difference in TTIs positivity between military and civilian blood donations determined by the chi-square test; ns: not statistically significant;
difference close to statistical significance; N.: absolute number of blood donations in the corresponding group.
Figure 3.
Different trends in the percentages of infections positive for transfusion-transmissible infections (TTIs) in blood donations originating from militaries and civilians at the Military Medical Academy, Belgrade, Serbia in 2005–2013.
p: trend significances.
Figure 4.
Decreasing percentages of blood donations positive for HBV and HCV among donations from members of the Serbian armed forces, at the Military Medical Academy, Belgrade, Serbia in 2005–2013.
HBV: hepatitis B virus; HCV: hepatitis C virus.
Discussion
It is a common practice in Serbia to test blood donors for the presence of four widespread TTI: HBV, HCV, HIV and syphilis. Other agents “suspected” of being responsible for TTI (hepatitis E virus, West Nile virus, human herpes viruses, parvovirus B19, influenza virus, Listeria monocytogenes, Plasmodium, Toxoplasma, Leishmania, Trypanosoma)1 are not mandatorily tested for Serbia, in line with the practice in most other countries.
This study presents data on HCV-, HBV-, HIV- and syphilis-positive blood donations at the MMA, in the period from 2005 to 2013. According to data obtained from the central Serbian Blood Transfusion Institute (personal communication), the average number of blood donations per donor in the period 2010–2013 was 1.28. Although the number of positive blood donors should also be reported, it is considered that for transfusion practice (i.e., for organisation of blood transfusion centres, and planning of financial, technical and human resources) the percentage of positive donations could be more important.
In this study, covering the period from 2005 to 2013, we found that 0.38% (n=597) of blood donations at the MMA were positive for TTI; this can be considered a low percentage, according to Manzoor et al8. The recorded decreasing number of TTI-positive donations is in line with the global trend resulting from generally better control of sexually transmitted infections9 and the introduction of mandatory screening for TTI10.
In the investigated period (2005–2013), TTI-positive blood donations were predominantly from males, aged between 19 and 29 years old, who donated blood for the first time. The percentages of positive blood donations from civilians and from military personnel of the Serbian Army were similar (47% vs 53%). Analysis of the data for individual diseases showed that HBV- and HCV-positive blood donations were predominantly from members of the Serbian Army, whereas syphilis-positive ones were predominantly from civilians. Donations positive for TTI as a whole, HBV and HCV were predominantly from the youngest donors (19–29 years old), whereas syphilis-positive donations were from the oldest donors (50–65 years old). Abolishing conscription had a significant impact on the demographic characteristics of blood donors, leading to a significant increase in the percentage of civilian donors. Furthermore, in the period 2010–2013 the youngest age group (18–29 years) was not the largest contributor to HBV- and HVC-positive donations, accounting for 25% and 33% of such donations, respectively. Besides, this age group was “responsible” for only 5% of syphilis positive donations. With regard to the gender of the blood donors, only 6% of positive donations were from female blood donors. Such a result was expected, because of the predominance of males (more than 80%) among military personnel of the Serbian Army. Generally, in Serbia the number of women blood donors is low (25% according to unpublished data from the Serbian Blood Transfusion Institute, personal communication) and the MMA is not an exception to the general trend.
Although all blood donors in Serbia have to complete a screening questionnaire, they do not always give exact data, causing doubts about the credibility of the information11. Based on this fact, we decided to compare the prevalence of TTI recorded in our survey with the incidence of diseased citizens in Serbia, provided by our relevant institution, the “Dr. Milan Jovanovic Batut” Institute for Public Health, for the period 2005–201312. The recorded national incidences (expressed as percentages of newly detected cases) of HBV, HCV, HIV and syphilis for the investigated period were 0.007%, 0.009%, 0.0007% and 0.001%, respectively. The percentages of HBV-, HCV-, HIV- and syphilis-positive blood donations from repeat blood donors (which can be regarded as analogous to the national TTI incidences) were 0.0003%, 0.0001%, 0.00001% and 0.0001%, respectively, which could be regarded as low. These data allow us to conclude that, even though the blood donors included some people who provided false information regarding their risk behaviours and health status11, the general population of blood donors at the MMA could not be considered as a group at increased risk. The higher percentage of TTI-positive blood donations comparing to the percentage of newly detected cases of the disease (national incidence) is in accordance with World Health Organisation data indicating that approximately 70% of people with sexually transmitted infections get through without detectable symptoms of their diseases13.
Members of the armed forces have been described as a risk group for TTI2,14. However, the results of a Serbian survey in the period 2007–2008 showed that the rate of TTI-positive members of the Serbian armed forces was low (0.64%)4. Based on those results, the low number of TTI-positive blood donations at the MMA recorded in this survey was not a surprise, despite the high number of militaries among blood donors. We also expected that abolishing conscription in 2009 would have resulted in a decrease in TTI-positive blood donations, and for the percentage of TTI-positive blood donations to differ in the MMA from those recorded in Serbian civilian transfusion centres. In the Blood Transfusion Institute, the largest institute for blood transfusion in Serbia, there were 192,187 blood donors in the period 2010–2013 and the recorded percentages of HBV-, HCV-, HIV- and syphilis-positive donations were 0.09%, 0.06%, 0.005% and 0.04%, respectively. In the same period, the corresponding percentages in the MMA were 0.14%, 0.08%, 0.005% and 0.06%. The observed slight differences in TTI-positive blood donations between these two largest transfusion centres were nor statistically significant.
Information about the prevalence of TTI among blood donors as well as the number of TTI-positive blood donations in neighbouring countries is scarce. Only Croatia publishes yearly reports on the results of transfusion practice. In 2012, the prevalences of HBV-, HCV-, HIV- and syphilis-positive donations among 182,068 tested in that country were 0.009%, 0.003%, 0.003% and 0.004%, respectively5. In Romania for the period 2006–2008, among randomly chosen individuals, the average prevalence of HCV was 4.4%15. In the town of Stip in Macedonia, in the period 2001–2011 the prevalence rates of HBV, HCV, HIV and syphilis in blood donors were 1.32%, 0.45%, 0.003% and 0.10%, respectively16. In Albania, the reported overall prevalence rate of HBV in the period 2004–2006 was 9.5%17. The reported prevalences of HBV, HCV and HIV in Turkey in 2007 were 1.76%, 0.07%, and 0.008, respectively18. Until now, Balkan countries have been classified as countries of intermediate prevalence (0.5–2%) of HBV19. However, the results for at least Serbia and Croatia might now change this classification.
Data about the prevalence of TTI in military populations are scarce4,20,21,22,23. To our knowledge, except Serbia4, only Albania and Lithuania have provided TTI prevalence data for military personnel in the last decade. The reported prevalence of HBV among military personnel in Albania was 10.6%17 while that among Lithuanian army soldiers was 1.97%23.
Conclusions
According to the number blood donations found to be positive for the mandatorily tested transfusion-transmissible infections at the Military Medical Academy, Belgrade, Serbia, it could be concluded that the high number of members of the Serbian armed forces who donate blood at this institution does not pose a risk for Serbian transfusion practice.
Footnotes
Funding and resources
This work was supported by the Ministry of Defence of the Republic of Serbia (Grant VMA/06-10B.20) and by the Ministry of Education and Science of the Republic of Serbia (Grant n. 175062). We would like to thank to Dr. Milica Jovičić for providing data on the number of total blood donations and TTI positivity among them for 2010–2013.
Authorship contributions
DV designed the research, analysed data and prepared the manuscript; GK analysed data and prepared the manuscript; VI processed data, designed and prepared the manuscript; BB oversaw the project, analysed data and assisted with preparation of the manuscript.
The Authors declare no conflict of interest.
References
- 1.Barbara J, Eglin R. Introduction: transfusion-transmitted infections, then and now. In: Barbara J, Regan F, Contreras M, editors. Transfusion Microbiology. New York: Cambridge University Press; 2008. pp. 1–7. [Google Scholar]
- 2.Foreman M. Combat AIDS: HIV and the World’s Armed Forces. London: Healthlink Worldwide; 2002. [Google Scholar]
- 3.Rehn E, Sirleaf EJ. Women, War and Peace: The Independent Experts’ Assessment on the Impact of Armed Conflict on Women and Women’s Role in Peace-building. New York: United Nations Development Fund for Women; 2002. HIV/AIDS, Women and War; pp. 47–60. [Google Scholar]
- 4.Jadranin Z, Suljagic V, Todorovic V, et al. HIV/AIDS and other sexually transmitted infections among military members of the Armed Forces of Serbia. Vojnosanitetski Pregled. 2012;69:43–8. doi: 10.2298/vsp1201043j. [DOI] [PubMed] [Google Scholar]
- 5.Croatian Institute for Transfusion Medicine. Report on results of Transfusiology practice in Croatia for 2012. [Accessed on 02/09/2014]. Available at: http://www.hztm.hr/glasilo/53/izvjesce-o-rezultatima-rada.html.
- 6.Esteban JI, Sauleda S, Quer J. The changing epidemiology of hepatitis C virus infection in Europe. J Hepatol. 2008;48:148–62. doi: 10.1016/j.jhep.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 7.Preacher KJ. Calculation for the chi-square test: an interactive calculation tool for chi-square tests of goodness of fit and independence (Computer software [2001, April]) [Accessed on: 15/05/2014]. Available at: http://quantpsy.org.
- 8.Manzoor I, Hashmi N, Daud S, et al. Seroprevalence of transfusion transmissible infections (TTIs) in blood donors. Biomedica. 2009;25:154–8. [Google Scholar]
- 9.World Health Organization. Sexual and reproductive health. Report on global sexually transmitted infection surveillance. 2013. [Accessed on 23/07/2014]. Available at: http://www.who.int/reproductivehealth/publications/rtis/stis-surveillance-2013/en/
- 10.O’Brien SF, Yi Qi-L, Fan W, et al. Current incidence and estimated residual risk of transfusion-transmitted infections in donations made to Canadian Blood Services. Transfusion. 2007;47:316–25. doi: 10.1111/j.1537-2995.2007.01108.x. [DOI] [PubMed] [Google Scholar]
- 11.Balint B, Vucetic D, Todorovic-Balint M, et al. Safety improving by complementary serological and molecular testing combined with pathogen reduction of the donated blood in window period. Transfus Apher Sci. 2013;49:103–4. doi: 10.1016/j.transci.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 12.Institute of Public Health of Serbia. Dr Milan Jovanovic Batut. Health Statistical Yearbooks of Republic of Serbia. 2005–2012. [Accessed on 13/05/2014]. Available at: http://www.batut.org.rs/download/publikacije.
- 13.World Health Organization Media centre. Sexually transmitted infections (STIs) [Accessed on 15/06/2014]. Available at: http://www.who.int/mediacentre/factsheets/fs110/en/
- 14.Bond MM, Yates SW. Sexually transmitted disease screening and reporting practices in a military medical center. Mil Med. 2000;165:470–2. [PubMed] [Google Scholar]
- 15.Gheorghe L, Csiki IE, Iacob S, et al. The prevalence and risk factors of hepatitis C virus infection in adult population in Romania: a nationwide survey 2006–2008. J Gastrointestin Liver Dis. 2010;19:373–9. [PubMed] [Google Scholar]
- 16.Veresa V, Kamchev N, Shorova M, Delipetrov R. Incidence of HBsAg, anti HCV, anti-HIV and Treponema pallidum antibodies in blood donors of the eastern part of the Republic of Macedonia in the past 10 years [abstract] Bilt Transfuziol. 2012;58:139. [Google Scholar]
- 17.Resuli B, Prifti S, Kraja B, et al. Epidemiology of hepatitis B virus infection in Albania. World J Gastroenterol. 2009;15:849–52. doi: 10.3748/wjg.15.849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Acar A, Kemahli S, Altunay H, et al. The significance of repeat testing in Turkish blood donors screened with HBV, HCV and HIV immunoassays and the importance of S/CO ratios in the interpretation of HCV/HIV screening test results and as a determinant for further confirmatory testing. Transfus Med. 2010;20:152–9. doi: 10.1111/j.1365-3148.2009.00987.x. [DOI] [PubMed] [Google Scholar]
- 19.Velati C. Occult B hepatitis - still a risk for transfusions? Vox Sang. 2010;5:73–6. [Google Scholar]
- 20.Laguna-Torres VA, Aguayo N, Aguilar G, et al. HIV infection and high-risk behaviors in a Paraguayan military population. Int J STD AIDS. 2014;25:866–77. doi: 10.1177/0956462414523741. [DOI] [PubMed] [Google Scholar]
- 21.Rimoin A, Hoff N, Djoko C, et al. HIV infection and risk factors among the armed forces personnel stationed in Kinshasa, Democratic Republic of Congo. Int J STD AIDS. 2015;26:187–95. doi: 10.1177/0956462414533672. [DOI] [PubMed] [Google Scholar]
- 22.Lloyd J, Papworth E, Grant L, et al. Systematic review and meta-analysis of HIV prevalence among men in militaries in low income and middle income countries. Sex Transm Infect. 2014;90:382–7. doi: 10.1136/sextrans-2013-051463. [DOI] [PubMed] [Google Scholar]
- 23.Kupcinskas L, Petrauskas D, Petrenkiene V, Saulius K. Prevalence of hepatitis B virus chronic carriers and risk factors for hepatitis B virus infection among Lithuanian army soldiers. Mil Med. 2007;172:625–7. doi: 10.7205/milmed.172.6.625. [DOI] [PubMed] [Google Scholar]