Abstract
Background
Infections such as common colds, influenza, acute upper respiratory infections, bacterial gastroenteritis, and urinary tract infections are usually diagnosed according to patients’ signs and symptoms. This study aims to develop a scale for the diagnosis of infectious diseases based on the six excesses (Liu Yin) etiological theory of Chinese medicine (CM) by the Delphi method.
Methods
A total of 200 CM-guided diagnostic items measuring signs and symptoms for infectious diseases were compiled from CM literature archives from the Han to Ming dynasties, CM textbooks in both China and Taiwan, and journal articles from the China Knowledge Resource Integrated Database. The items were based on infections and the six excesses (Liu Yin) etiological theory, i.e., Feng Xie (wind excess), Han Xie (coldness excess), Shu Xie (summer heat excess), Shi Xie (dampness excess), Zao Xie (dryness excess), and Huo Xie (fire excess). The items were further classified into the six excess syndromes and reviewed via a Delphi process to reach consensus among CM experts.
Results
In total, 178 items with a mean or median rating of 7 or above on a scale of 1–9 from a panel of 32 experts were retained. The numbers of diagnostic items in the categories of Feng (wind), Han (coldness), Shu (summer heat), Shi (dampness), Zao (dryness), and Huo (fire) syndromes were 15, 22, 25, 37, 17, and 62, respectively.
Conclusions
A CM-based six excesses (Liu Yin) evaluation and diagnosis (SEED) scale was developed for the evaluation and diagnosis of infectious diseases based only on signs and symptoms.
Background
Infections such as common colds, influenza, acute upper respiratory infections, bacterial gastroenteritis, and urinary tract infections are usually diagnosed according to patients’ signs and symptoms, while the diagnosis of pandemic infections such as influenza H1N1 [1–4] and H5N1 [5, 6] must be confirmed by expensive laboratory tests [7–9] or real-time RT-PCR assays of multiple specimens [10]. Pathogen testing in the laboratory might be of low sensitivity [11], and low accuracy in some cases [12–14], and above all time-consuming [15].
Chinese medicine (CM) can detect those infectious diseases mentioned above according to the etiological theory of Liu Yin (six excesses), i.e., Feng Xie (wind excess) representing varying temperature factors, Han Xie (coldness excess) representing falling temperature, Shu Xie (summer heat excess) representing rising temperature and humidity, Shi Xie (dampness excess) representing rising humidity, Zao Xie (dryness excess) representing falling humidity, and Huo Xie (fire excess) representing rising temperature [16, 17]. These Liu Yin (six excesses) collectively describe the circumstantial influences on Qi and Xue (blood), encompassing a number of CM diagnostic criteria checked by inquiry, inspection, olfaction, audition, percussion, palpation, and pulse examination (Fig. 1), and facilitate diagnostic and therapeutic decisions [18]. However, there has been no standard diagnostic assessment or measurement scales designed for infectious diseases based on the Liu Yin (six excesses) theory [19–28].
Fig. 1.
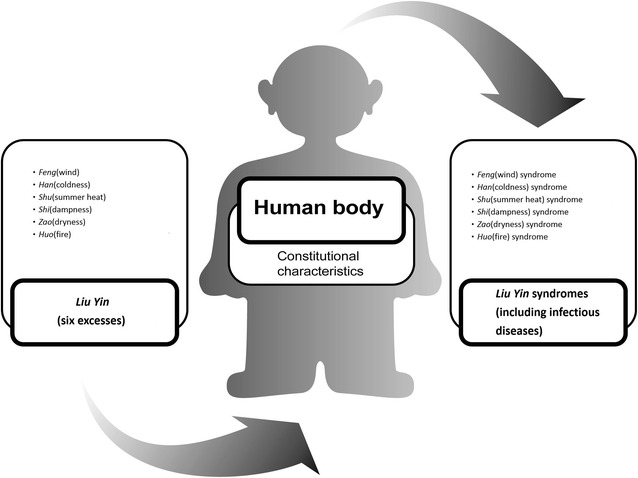
Infectious diseases were classifiable in CM according to the Liu Yin (six excesses), Feng (wind), Han (coldness), Shu (summer heat), Shi (dampness), Zao (dryness), and Huo (fire), and could be classified into Feng (wind), Han (coldness), Shu (summer heat), Shi (dampness), Zao (dryness), and Huo (fire) syndromes
This study aims to develop the six excesses (Liu Yin) evaluation and diagnosis (SEED) scale for infectious diseases based on the Liu Yin (six excesses) etiological theory in CM by a Delphi process among experts. The Delphi method aims to build consensus and generate ideas in research fields [29–41], and is useful for the establishment of diagnostic criteria in clinical medicine. It is a structured communication process to establish the definition of the syndromes, the diagnostic criteria or the staging of the diseases, and the suggested treatments in the medical guidelines [42–48].
Methods
The Delphi method [49] was used to achieve a group panel consensus on the diagnostic items for the Liu Yin (six excesses) syndromes among a panel of experts between 2007 and 2008. A nationally representative panel of Chinese medical experts were invited; only CM experts with good knowledge about CM and modern research methods with master or doctoral degrees, and more than 7 years of practicing experience were invited to join the Delphi panel. Based on this consensus, we carried out further statistical analyses for infectious diseases.
An interdisciplinary advisory board was formed by seven members, including five CM experts, one measurement methodologist, and one statistician. The advisory board selected the participants of the Delphi panel.
Representatives from various education backgrounds, medical disciplines, geographical distributions, and clinical experience were considered for the panel. Finally, a total of 32 CM experts meeting these criteria were invited, and all agreed to participate (Table 1). Of the 32 participants, 20 were from CM departments in medical centers, 6 were from district or regional teaching hospitals, and 6 were from private practices; 7 practiced in Northern region, 11 in central region, 6 in Southern region and 8 in other region. Twenty-one panelists held master degrees, 11 had doctoral degrees in medical sciences, and 26 panelists were teachers in academic institutions. The age (mean ± SD) of the panelists was 43 ± 7.0 years with a median of 42 years. The year of practicing experience (mean ± SD) was 11.3 ± 3.7 years with a median of 10 years.
Table 1.
Basic characteristics of the 32 CM experts
| Age, mean (SD), years | ||
| Average | 43 (SD = 7.0) | |
| Median | 42 | |
| Spectrum of practice, mean (SD), years | ||
| Average | 11.3 (SD = 3.7) | |
| Median | 10 | |
| Educational background, n (%) | ||
| Master degree | 21 (65.6 %) | |
| Doctorate degree | 11 (34.4 %) | |
| Geographic distribution, n (%) | ||
| Northern | 7 (21.9 %) | |
| Central | 11 (34.4 %) | |
| Southern | 6 (18.8 %) | |
| Other | 8 (25.0 %) | |
| Practice institution, n (%) | ||
| Medical centers | 20 (62.5 %) | |
| District teaching hospitals | 5 (15.6 %) | |
| Regional teaching hospitals | 1 (3.1 %) | |
| Private practices | 6 (18.8 %) | |
| Teaching in an academic institution, n (%) | ||
| Yes | 26 (81.3 %) | |
| No | 6 (18.8 %) | |
The Delphi process was iterative. We began with a systematic review of traditional CM literature including the Medicine Encyclopedia collected by Kentang Wang (AC1552–1639), 122 published modern textbooks, and 7364 journal articles from the China Knowledge Resource Integrated Database. The search keywords included: Feng (wind), Han (coldness), Shu (summer heat), Shi (dampness), Zao (dryness), Huo (fire), Wai-gan (external contraction), Liu Yin (six excesses), and Yin (excess), and we identified and compiled a pool of 200 diagnostic items for the Liu Yin (six excesses) syndromes. The CM experts categorized each of these 200 items into one of the Liu Yin (six excesses) syndromes, and the results were reviewed and face-validated by the same experts. The numbers of items for each Yin (excess) syndrome were: Feng (wind), 23; Han (coldness), 32; Shu (summer heat), 25; Shi (dampness), 40; Zao (dryness), 18; and Huo (fire), 62. We had mailed the items to the panelists and invited them to add any items; the numbers remained the same.
The classified items were then incorporated into the processes of the Delphi method and circulated via mail to the panelists for their ratings with follow-up phone calls within 2 weeks (Fig. 2). In stage 1, the panelists were asked to rate the appropriateness of each of the classified signs and symptoms on a scale of 1 (highly inappropriate) to 9 (highly appropriate). They were also instructed to provide reasons for the items they rated as “inappropriate”. In stage 2, the results for the mean rating and standard deviation of the individual items were mailed to the panelists, and they were asked again to provide and return their ratings after reviewing the results. The two-stage Delphi method are enough to saturate consensus [49–57], which cannot be maximized by increasing the number of round [58–64]. The progress was assessed by any reduction in the variability of judgments among the panelists. The level of consensus was quantified by the standard deviation of their ratings. After the two-stage Delphi method, the expert-rated diagnostic items with an average or median rating of 7 or above were considered to have face-validity and integrated into the standardized assessment. The cut point of 7.0 had been chosen because it highly represents panelists’ agreement as well as the estimated time required to complete the selected items by CM doctors is expected to be no more than 30 min.
Fig. 2.
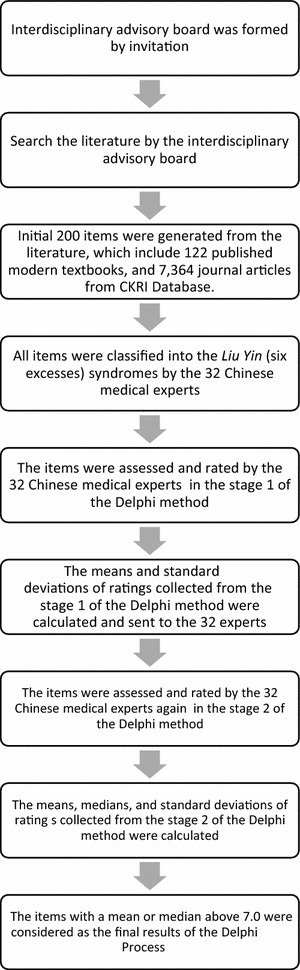
Flow chart of the Delphi process
Results
The mean, median and standard deviation of the ratings for each item from the first and second stages were calculated (Table 2). After the two-stage Delphi method, 15, 22, 25, 37, 17, and 62 diagnostic items with a rating of 7.0 or higher were retained in Feng (wind), Han (coldness), Shu (summer heat), Shi (dampness), Zao (dryness), and Huo (fire) syndromes, respectively. The standard deviations of all 178 retained items decreased from the first stage to the second stage because of the achieved agreement, with the following exceptions: “surging but weak pulse with dipped finger tip” (both 1.02) and “unclear head and eyesight” (1.01–1.06) in Shu (summer heat) syndrome; “edematous swelling in face and limbs” (both 1.10) and “unclear head and eyesight” (both 0.67) in Shi (dampness) syndrome; and “dry and yellow fur” (1.01–1.06) and “dry, yellow and white fur” (0.61–0.63) in Huo (fire) syndrome. However, the upward changes were relatively small.
Table 2.
Results of the two-stage Delphi method
| Syndrome | No. | Item | Stage 1 | Stage 2 | ||
|---|---|---|---|---|---|---|
| Mean (SD) | Median | Mean (SD) | Median | |||
| Feng (wind) syndrome | 1 | Aversion to winda | 8.03 (1.06) | 8 | 8.28 (0.96) | 8 |
| 2 | Floating pulsea | 7.63 (1.41) | 7 | 7.78 (0.87) | 7 | |
| 3 | Itchy throata | 7.25 (1.16) | 7 | 7.41 (0.80) | 7 | |
| 4 | Headachea | 7.09 (1.30) | 6 | 7.16 (0.51) | 6.5 | |
| 5 | Headache and painful stiffness in napea | 7.06 (1.34) | 7 | 7.06 (0.80) | 7 | |
| 6 | Floating and relaxed pulsea | 7.00 (1.42) | 6 | 7.28 (0.82) | 7 | |
| 7 | Clear snivela | 6.97 (1.23) | 7 | 7.09 (0.69) | 7 | |
| 8 | Sneezinga | 6.94 (1.34) | 5 | 7.13 (0.79) | 5 | |
| 9 | Pain at unfixed location | 6.88 (2.03) | 6 | 6.91 (1.09) | 6 | |
| 10 | Painful stiffness in nape and back | 6.84 (1.22) | 6 | 6.84 (0.95) | 5 | |
| 11 | Floating and rapid pulsea | 6.81 (1.42) | 7 | 7.19 (0.82) | 7 | |
| 12 | Generalized paina | 6.75 (1.59) | 7 | 7.06 (0.67) | 7 | |
| 13 | Nasal congestiona | 6.69 (1.31) | 7 | 7.13 (0.75) | 7 | |
| 14 | Cough, productivea | 6.59 (1.46) | 7 | 7.06 (0.67) | 7 | |
| 15 | Floating and weak pulsea | 6.53 (1.65) | 7 | 6.59 (1.07) | 7 | |
| 16 | Aches and pains in joints | 6.44 (1.39) | 5.5 | 6.69 (0.59) | 5 | |
| 17 | Generalized itching | 6.44 (1.68) | 5.5 | 6.44 (1.37) | 5 | |
| 18 | Thin white fur | 6.38 (1.79) | 6 | 6.50 (1.05) | 6 | |
| 19 | Pale red tongue | 6.28 (1.90) | 6 | 6.41 (0.98) | 6 | |
| 20 | Deviated eye and mouth | 6.16 (1.92) | 8 | 5.84 (1.44) | 8 | |
| 21 | Opisthotonosa | 5.63 (2.23) | 7 | 5.09 (1.40) | 7 | |
| 22 | Trismus (lockjaw)a | 5.53 (2.17) | 7 | 5.06 (1.37) | 7 | |
| 23 | Hemiplegia | 5.22 (2.35) | 6 | 5.13 (1.43) | 6 | |
| Han (coldness) syndrome | 1 | Aversion to colda | 8.22 (0.87) | 8.5 | 8.41 (0.61) | 8 |
| 2 | Floating and tight pulsea | 7.66 (1.10) | 7 | 7.78 (0.79) | 7 | |
| 3 | Preference for hot drinksa | 7.53 (1.37) | 7 | 7.53 (0.67) | 7 | |
| 4 | Clear phlegma | 7.53 (0.98) | 7 | 7.47 (0.57) | 7 | |
| 5 | Clear snivela | 7.41 (0.95) | 6 | 7.50 (0.67) | 7 | |
| 6 | A lot of clear and white phlegma | 7.38 (1.07) | 7 | 7.34 (0.60) | 7 | |
| 7 | Generalized paina | 7.13 (1.34) | 7 | 7.41 (0.67) | 7 | |
| 8 | Headache and painful stiffness in napea | 7.13 (1.18) | 7 | 7.28 (0.58) | 7 | |
| 9 | Shiveringa | 7.06 (1.37) | 7 | 7.22 (0.91) | 7 | |
| 10 | Ache in limbsa | 7.00 (1.39) | 7 | 7.28 (0.73) | 7 | |
| 11 | Cold body and limbsa | 7.00 (1.87) | 7 | 7.28 (0.96) | 7 | |
| 12 | Tight pulsea | 6.94 (1.39) | 6 | 7.13 (1.16) | 6 | |
| 13 | Aches and pains in jointsa | 6.88 (1.50) | 6 | 7.28 (0.58) | 6 | |
| 14 | White and moist fur | 6.88 (1.50) | 6 | 6.81 (1.00) | 6 | |
| 15 | Not thirstya | 6.84 (1.32) | 6 | 7.03 (0.93) | 6 | |
| 16 | White, moist and thin fura | 6.84 (1.51) | 7 | 6.94 (0.95) | 7 | |
| 17 | No desire to drink | 6.84 (1.27) | 6 | 6.81 (0.90) | 6 | |
| 18 | Clear urinea | 6.81 (1.64) | 7 | 6.78 (0.75) | 7 | |
| 19 | Painful stiffness in nape and backa | 6.78 (1.72) | 7 | 6.91 (0.95) | 7 | |
| 20 | White and thin fur | 6.78 (1.72) | 6 | 6.84 (0.95) | 6 | |
| 21 | Absence of sweatinga | 6.69 (1.64) | 7 | 7.13 (1.01) | 7 | |
| 22 | Cold feeling on nape and back | 6.69 (1.45) | 7 | 6.94 (0.76) | 6 | |
| 23 | Headachea | 6.63 (1.36) | 7 | 7.06 (0.95) | 8 | |
| 24 | Cough, productive | 6.53 (1.24) | 7 | 6.75 (0.72) | 6 | |
| 25 | White fur | 6.53 (1.78) | 7 | 6.59 (1.01) | 6 | |
| 26 | Sloppy stool | 6.50 (1.32) | 7 | 6.66 (1.00) | 6 | |
| 27 | Reversal cold of extremities | 6.50 (1.80) | 7 | 6.59 (1.24) | 6 | |
| 28 | White and slippery fura | 6.44 (1.63) | 7 | 6.50 (1.02) | 7 | |
| 29 | Nasal congestion | 6.38 (1.36) | 7 | 6.81 (0.63) | 6 | |
| 30 | Sneezing | 6.38 (1.34) | 6 | 6.81 (0.64) | 6 | |
| 31 | Lumbar pain or achea | 6.13 (1.54) | 8 | 6.53 (0.67) | 8 | |
| 32 | Breathlessnessa | 5.88 (1.52) | 7 | 6.22 (1.10) | 7 | |
| Shu (summer heat) syndrome | 1 | Thirstya | 7.97 (1.00) | 8 | 7.88 (0.71) | 8 |
| 2 | Fevera | 7.91 (1.09) | 8 | 8.00 (0.80) | 8 | |
| 3 | High fevera | 7.84 (1.05) | 8 | 7.88 (0.66) | 8 | |
| 4 | Profuse sweatinga | 7.81 (1.57) | 8 | 7.53 (0.92) | 7 | |
| 5 | Surging pulsea | 7.66 (0.94) | 8 | 7.66 (0.79) | 7 | |
| 6 | Fatiguea | 7.59 (1.21) | 7 | 7.72 (0.73) | 7 | |
| 7 | Aversion to heata | 7.56 (1.41) | 7 | 7.72 (0.73) | 7 | |
| 8 | Reddish yellow urinea | 7.56 (0.88) | 7 | 7.47 (0.67) | 7 | |
| 9 | Red tonguea | 7.53 (0.92) | 6 | 7.63 (0.66) | 6 | |
| 10 | Surging but weak pulse with dipped finger tipa | 7.53 (1.02) | 6 | 7.28 (1.02) | 6 | |
| 11 | Desire to drinka | 7.47 (1.41) | 7 | 7.53 (0.67) | 7 | |
| 12 | Unclear head and eyesighta | 7.44 (1.01) | 7 | 7.03 (1.06) | 7 | |
| 13 | Rapid pulsea | 7.34 (1.29) | 8 | 7.28 (0.68) | 8 | |
| 14 | Heavy or tired limbsa | 7.31 (1.38) | 8 | 7.25 (0.84) | 7 | |
| 15 | Reddened complexiona | 7.28 (0.85) | 7 | 7.22 (0.61) | 7 | |
| 16 | Preference for cold drinksa | 7.28 (1.51) | 7 | 7.13 (0.87) | 7 | |
| 17 | Shortness of urinea | 7.22 (1.04) | 6 | 7.06 (0.95) | 6 | |
| 18 | Red lipsa | 7.19 (0.74) | 7 | 7.19 (0.64) | 6 | |
| 19 | Agitationa | 7.13 (1.04) | 7 | 7.00 (0.76) | 7 | |
| 20 | Lethargya | 7.03 (1.26) | 7 | 6.78 (0.87) | 7 | |
| 21 | Dry tongue with little salivaa | 7.00 (0.95) | 8 | 7.09 (0.93) | 7 | |
| 22 | Anorexiaa | 6.81 (1.15) | 8 | 6.81 (0.90) | 8 | |
| 23 | Dizzinessa | 6.50 (1.22) | 8 | 6.47 (1.08) | 8 | |
| 24 | Stomach refluxa | 6.38 (1.07) | 7 | 6.34 (0.90) | 7 | |
| 25 | Headachea | 6.19 (1.51) | 7 | 6.38 (1.10) | 7 | |
| Shi (dampness) syndrome | 1 | Heavy or tired limbsa | 8.19 (0.86) | 7 | 8.09 (0.73) | 7 |
| 2 | Heavy-headednessa | 8.09 (0.86) | 8 | 8.06 (0.76) | 8 | |
| 3 | Fatiguea | 7.81 (0.90) | 7 | 7.81 (0.74) | 7 | |
| 4 | White and slimy fura | 7.75 (1.05) | 7 | 7.72 (0.68) | 7 | |
| 5 | Unclear head and eyesighta | 7.50 (0.67) | 8 | 7.50 (0.67) | 8 | |
| 6 | Viscous feeling in oral cavitya | 7.50 (0.95) | 7 | 7.47 (0.62) | 7 | |
| 7 | Thick and slimy fura | 7.47 (1.16) | 7 | 7.63 (0.79) | 7 | |
| 8 | Soggy pulsea | 7.41 (1.34) | 8 | 7.47 (1.02) | 8 | |
| 9 | Edematous swelling in face and limbsa | 7.41 (1.10) | 7 | 7.13 (1.10) | 7 | |
| 10 | Edema, generalized | 7.28 (1.53) | 6 | 6.94 (0.95) | 6 | |
| 11 | Rash | 7.25 (1.30) | 6 | 6.97 (1.09) | 6 | |
| 12 | Sloppy stoola | 7.22 (1.21) | 7 | 7.38 (0.61) | 7 | |
| 13 | Slippery pulsea | 7.19 (1.06) | 7 | 7.22 (0.79) | 7 | |
| 14 | Soggy and relaxed pulsea | 7.19 (1.35) | 7 | 7.19 (0.90) | 7 | |
| 15 | White and slippery fura | 7.19 (1.40) | 6 | 7.19 (0.74) | 6.5 | |
| 16 | No desire to drinka | 7.19 (1.23) | 6 | 7.00 (0.88) | 7 | |
| 17 | Yellow and slimy fura | 7.19 (1.18) | 7 | 6.97 (1.03) | 7 | |
| 18 | Slippery fura | 7.13 (1.43) | 7 | 7.16 (0.72) | 7 | |
| 19 | Soft stoola | 6.97 (1.36) | 6 | 7.22 (0.61) | 7 | |
| 20 | Anorexiaa | 6.97 (1.40) | 6 | 7.22 (0.71) | 6 | |
| 21 | Dizzinessa | 6.94 (1.46) | 7 | 7.13 (0.83) | 7 | |
| 22 | Lethargya | 6.94 (1.34) | 7 | 7.09 (0.89) | 7 | |
| 23 | White and moist fura | 6.94 (1.32) | 7 | 6.97 (0.78) | 7 | |
| 24 | Stool with dischargea | 6.94 (1.32) | 7 | 6.94 (0.72) | 7 | |
| 25 | Oppression in chesta | 6.91 (1.42) | 7 | 7.13 (0.83) | 7 | |
| 26 | White and moist fura | 6.91 (1.53) | 7 | 7.13 (0.75) | 7 | |
| 27 | Not thirstya | 6.91 (1.17) | 7 | 6.97 (0.78) | 7 | |
| 28 | Soggy and rapid pulsea | 6.91 (1.23) | 7 | 6.97 (0.90) | 7 | |
| 29 | Dyspepsia | 6.91 (1.42) | 7 | 6.81 (1.00) | 6 | |
| 30 | Jaundicea | 6.91 (1.47) | 7 | 6.78 (1.16) | 7 | |
| 31 | Mild fevera | 6.88 (1.31) | 7 | 7.09 (0.59) | 7 | |
| 32 | Stomach refluxa | 6.78 (1.24) | 8 | 6.84 (0.81) | 8 | |
| 33 | Gastric stuffinessa | 6.75 (1.46) | 7 | 7.06 (0.76) | 7 | |
| 34 | Vaginal dischargea | 6.75 (1.46) | 8 | 7.06(0.76) | 8 | |
| 35 | A lot of clear and white phlegma | 6.75 (1.34) | 7 | 7.00 (0.51) | 7 | |
| 36 | Aches and pains in jointsa | 6.72 (1.35) | 7 | 7.03 (0.47) | 7 | |
| 37 | White fura | 6.66 (1.49) | 7 | 6.91 (0.78) | 7 | |
| 38 | Vomitinga | 6.59 (1.24) | 7 | 6.56 (0.98) | 7 | |
| 39 | Ache in limbsa | 6.50 (1.32) | 7 | 6.72 (0.58) | 7 | |
| 40 | Generalized paina | 6.44 (1.48) | 6 | 6.75 (0.50) | 7 | |
| Zao (dryness) syndrome | 1 | Dry throata | 8.16 (0.72) | 8 | 8.17 (0.66) | 8 |
| 2 | Dry nasal cavitya | 8.06 (0.84) | 7 | 7.90 (0.49) | 6 | |
| 3 | Dry lipsa | 8.06 (0.88) | 8 | 7.79 (0.49) | 8 | |
| 4 | Dry skina | 7.84 (0.92) | 8 | 7.83 (0.54) | 8 | |
| 5 | Dry tongue with little fluida | 7.75 (1.05) | 8 | 7.66 (0.55) | 8 | |
| 6 | Cough, nonproductivea | 756 (1.08) | 6 | 7.62 (0.62) | 6 | |
| 7 | Thirstya | 7.38 (1.43) | 8 | 7.24 (0.83) | 7.5 | |
| 8 | Hard bound or dry stoola | 7.31 (1.28) | 7 | 7.14 (0.49) | 7 | |
| 9 | Sticky phlegma | 7.31 (1.03) | 7 | 7.14 (0.52) | 7 | |
| 10 | Dry, thin and white fura | 7.25 (1.34) | 7 | 7.17 (0.80) | 7 | |
| 11 | Dry, yellow and white fura | 7.25 (1.16) | 8 | 7.00 (0.89) | 8 | |
| 12 | Dry and yellow fura | 7.06 (1.29) | 7 | 6.79 (0.73) | 7 | |
| 13 | Desire to drinka | 7.00 (1.37) | 7 | 7.10 (0.86) | 7 | |
| 14 | Red tongue | 6.97 (1.58) | 6 | 6.90 (0.62) | 6 | |
| 15 | Hoarsenessa | 6.88 (1.21) | 7 | 7.00 (0.53) | 7 | |
| 16 | Pruritusa | 6.81 (1.38) | 7 | 7.10 (0.41) | 7 | |
| 17 | Dyscheziaa | 6.50 (1.34) | 7 | 6.59 (0.95) | 7 | |
| 18 | Cough, productivea | 6.28 (1.17) | 7 | 6.59 (0.82) | 7 | |
| Huo (fire) syndrome | 1 | High fevera | 7.97 (0.82) | 8 | 8.00 (0.57) | 8 |
| 2 | Fevera | 7.94 (1.08) | 8 | 7.97 (0.54) | 8 | |
| 3 | Rapid pulsea | 7.94 (1.19) | 8 | 7.84 (0.68) | 8 | |
| 4 | Heat intolerancea | 7.91 (0.86) | 7 | 7.94 (0.72) | 7 | |
| 5 | Thirstya | 7.91 (1.06) | 7 | 7.78 (0.61) | 7 | |
| 6 | Red tonguea | 7.88 (1.01) | 7 | 7.75 (0.67) | 7 | |
| 7 | Preference for cold drinksa | 7.69 (1.00) | 6 | 7.63 (0.66) | 6 | |
| 8 | Surging pulsea | 7.66 (1.18) | 7 | 7.56 (0.72) | 7 | |
| 9 | Reddish yellow urinea | 7.63 (1.01) | 7 | 7.59 (0.56) | 7 | |
| 10 | Sore throata | 7.56 (1.11) | 5 | 7.69 (0.69) | 5 | |
| 11 | Reddish eyea | 7.56 (1.01) | 7 | 7.56 (0.80) | 7 | |
| 12 | Desire to drinka | 7.56 (1.11) | 7 | 7.53 (0.57) | 7 | |
| 13 | Reddened complexiona | 7.56 (0.84) | 7 | 7.50 (0.72) | 6 | |
| 14 | Erythema, blister or ulcera | 7.53 (0.72) | 7 | 7.47 (0.98) | 7 | |
| 15 | Hard bound or dry stoola | 7.50 (1.19) | 7 | 7.44 (0.67) | 7 | |
| 16 | Agitationa | 7.50 (1.11) | 6 | 7.38 (0.71) | 6 | |
| 17 | Red lipsa | 7.47 (1.02) | 6 | 7.63 (0.71) | 6 | |
| 18 | Sore swollen guma | 7.47 (1.02) | 7 | 7.44 (0.76) | 6 | |
| 19 | Dry and yellow fura | 7.44 (0.56) | 7 | 7.47 (0.62) | 8 | |
| 20 | Hotness in chesta | 7.44 (1.01) | 7 | 7.38 (0.55) | 7 | |
| 21 | Red tip of tonguea | 7.44 (1.05) | 7 | 7.38 (0.71) | 7 | |
| 22 | Red tip and margin of tonguea | 7.44 (1.05) | 7 | 7.38 (0.71) | 7 | |
| 23 | Red dot on tonguea | 7.41 (1.07) | 8 | 7.41 (0.67) | 8 | |
| 24 | Floating and rapid pulsea | 7.38 (1.18) | 7 | 7.41 (0.67) | 7 | |
| 25 | Dry tongue with little fluida | 7.38 (1.01) | 7 | 7.31 (0.64) | 7 | |
| 26 | Dry, yellow and white fura | 7.38 (0.61) | 7 | 7.28 (0.63) | 7 | |
| Huo (fire) syndrome | 27 | Ulcer on tonguea | 7.34 (1.26) | 6 | 7.31 (0.74) | 6 |
| 28 | Aphthaa | 7.34 (1.15) | 8 | 7.28 (0.68) | 8 | |
| 29 | Hot feeling around anusa | 7.31 (1.09) | 7 | 7.28 (1.02) | 7 | |
| 30 | Dry lipsa | 7.31 (1.38) | 7 | 7.16 (0.57) | 7 | |
| 31 | Profuse sweatinga | 7.31 (1.00) | 8 | 7.06 (0.88) | 8 | |
| 32 | Purpuraa | 7.31 (1.28) | 7 | 7.06 (0.76) | 7 | |
| 33 | String-like and rapid pulsea | 7.28 (1.14) | 8 | 7.16 (0.63) | 7 | |
| 34 | Stinky diarrheaa | 7.28 (1.16) | 7 | 6.97 (0.61) | 7 | |
| 35 | Slippery and rapid pulsea | 7.22 (1.16) | 7 | 7.22 (0.61) | 7 | |
| 36 | Hotness in abdomena | 7.22 (1.21) | 7 | 7.19 (0.54) | 7 | |
| 37 | Dry throata | 7.22 (1.29) | 7 | 7.16 (0.57) | 6 | |
| 38 | Decreased urinationa | 7.22 (1.04) | 6 | 7.09 (0.69) | 6 | |
| 39 | Dysuriaa | 7.22 (0.97) | 7 | 6.91 (0.93) | 7 | |
| 40 | Skin wheala | 7.16 (0.92) | 8 | 7.16 (0.72) | 8 | |
| 41 | Yellow phlegma | 7.13 (1.24) | 7 | 7.22 (0.55) | 7 | |
| 42 | Epistaxisa | 7.13 (1.36) | 7 | 7.22 (0.66) | 7 | |
| 43 | Sudden and watery diarrheaa | 7.13 (1.01) | 7 | 6.97 (1.12) | 7 | |
| 44 | Yellow snivela | 7.06 (1.37) | 8 | 7.16 (0.63) | 7 | |
| 45 | Dyscheziaa | 7.06 (1.22) | 6.5 | 7.09 (0.64) | 6 | |
| 46 | Anguish in hearta | 7.03 (1.26) | 7.5 | 7.19 (0.64) | 7 | |
| 47 | Dry nasal cavitya | 7.00 (1.30) | 7 | 7.09 (0.53) | 7 | |
| 48 | Bitter taste in moutha | 7.00 (1.34) | 7 | 7.06 (0.80) | 7 | |
| 49 | Rasha | 6.97 (1.40) | 7 | 7.03 (0.69) | 7 | |
| 50 | Bloody stool with pusa | 6.97 (0.93) | 7 | 6.97 (1.09) | 7 | |
| 51 | Difficulty falling asleepa | 6.94 (1.32) | 7 | 7.09 (0.69) | 7 | |
| 52 | Delirious speecha | 6.84 (1.42) | 8 | 6.72 (0.99) | 8 | |
| 53 | Gingival bleedinga | 6.81 (1.40) | 7 | 6.91 (1.03) | 7 | |
| 54 | Nasal flaringa | 6.75 (1.46) | 7 | 6.81 (1.06) | 7 | |
| 55 | Difficulty maintaining sleepa | 6.72 (1.30) | 7 | 6.91 (0.59) | 7 | |
| 56 | Hemoptysisa | 6.69 (1.40) | 7 | 6.84 (0.85) | 7 | |
| 57 | Hematuriaa | 6.69 (1.49) | 7 | 6.66 (1.10) | 7 | |
| 58 | Headachea | 6.56 (1.32) | 8 | 6.41 (0.87) | 7 | |
| 59 | Hematemesisa | 6.44 (1.26) | 8 | 6.44 (0.94) | 8 | |
| 60 | Breathlessa | 6.34 (1.26) | 7.5 | 6.13 (0.94) | 7 | |
| 61 | Lethargya | 6.31 (1.60) | 7 | 6.31 (1.12) | 7 | |
| 62 | Tinnitusa | 5.84 (1.65) | 7 | 5.94 (0.91) | 7 | |
The translations were mainly according to “WHO International Standard Terminologies on Traditional Medicine in the Western Pacific Region [70]”
SD standard deviation
aThe 178 diagnostic items graded as 7.0 and above
The total number of retained items in each of the Liu Yin (six excesses) syndromes varied from 15 items in Feng (wind) syndrome to 62 items in Huo (fire) syndrome. All syndromes comprised two kinds of diagnostic items: subjective discomfort factors and objective examinations by the patients themselves or by clinicians. The diagnostic items for subjective discomfort included the following: items regarding sleeping, appetite, eyesight, and hearing; items regarding behavioral adjustments such as aversion, preference, anguish, and agitation; items regarding sensations of coldness, hotness, dryness, and bitterness; and items regarding feelings of pain, itch, ache, congestion, thirst, viscousness, oppression, fullness, stuffiness, heaviness, and tiredness. The diagnostic items for objective examinations included the following: general symptoms regarding complexion, eyes, lips, tongue, skin, snivel, stool, urine, phlegm, and awareness; physical responses such as breathlessness, coughing, shivering, sweating, sneezing, and vomiting; and appearance changes such as hemiplegia, deviated eyes and mouth, opisthotonos, trismus, and edema. In addition to the two kinds of diagnostic items, 4, 2, 3, 4, and 5 items of pulse examination were retained in Feng (wind), Han (coldness), Shu (summer heat), Shi (dampness), and Huo (fire) syndromes, respectively.
Some items were retained in more than one syndrome because of their overlapping contributions, as follows: “headache”, “generalized pain”, “clear snivel”, and “headache and painful stiffness in nape” in Feng (wind) and Han (coldness) syndromes; “floating and rapid pulse” in Feng (wind) and Huo (fire) syndromes; “aches and pains in joints” and “a lot of clear and white phlegm” in Han (coldness) and Shi (dampness) syndromes; “fatigue”, “heavy or tired limbs”, and “unclear head and eyesight” in Shu (summer heat) and Shi (dampness) syndromes; “thirsty”, “desire to drink”, and “dry tongue with little saliva” in Shu (summer heat), Zao (dryness), and Huo (fire) syndromes; “dry nasal cavity”, “dry lips”, “dry throat”, “hard bound or dry stool”, and “dry, yellow and white fur” in Zao (dryness) and Huo (fire) syndromes; and “aversion to heat”, “fever”, “high fever”, “profuse sweating”, “red lips”, “preference for cold drinks”, “agitation”, “shortness of urine”, “reddish yellow urine”, “red tongue”, “surging pulse”, and “rapid pulse” in Shu (summer heat) and Huo (fire) syndromes. Including these overlapping items, the SEED scale for infectious diseases, which captured the Liu Yin (six excesses) syndromes, was created and formatted as follows: Feng (wind), 15 items; Han (coldness), 22 items; Shu (summer heat), 25 items; Shi (dampness), 37 items; Zao (dryness), 17 items; and Huo (fire), 62 items. Following the integration of common items, a total of 102 diagnostic criteria conformed to the Liu Yin (six excesses) and covered the manifestations of the Liu Yin (six excesses) syndromes.
Discussion
This study codified the Liu Yin (six excesses) syndromes by the Delphi method with a panel of 32 CM experts. The 178 diagnostic items derived from the two-stage Delphi method combined information gleaned from CM classic textbooks, journal articles, and opinions of CM experts. All six syndromes encompassed diagnostic criteria regarding subjective discomfort and objective examinations, both were deemed essential for diagnostic judgment. Subjective discomfort was important for medical care considerations, while objective examinations were crucial for disease progress evaluations.
Common diagnostic items were present in different syndromes as a result of the same body responses to different Yin (excess). For example, “generalized pain” in Feng (wind) and Shi (dampness) syndromes results from obstructed circulation of Qi and Xue (blood) [65]. Common items combined with different signs or symptoms imply different body responses [66, 67]. “Fatigue” combined with “thirsty” was attributed to Shu Xie (summer heat excess), while “fatigue” combined with “not thirsty” was attributed to Shi Xie (dampness excess).
Five syndromes, except for Feng (wind) syndrome, comprised diagnostic items of tongue examinations for detecting the Qi and Xue (blood) status. Five syndromes, except for Zao (dryness) syndrome, comprised pulse examinations for instant diagnostic judgment in CM practice [68]. Clinical skills in pulse and tongue examinations were important for accurate assessment of signs and symptoms in the SEED scale [69], just as in CM clinical practice.
The 102 diagnostic criteria were checked by inquiry, inspection, olfaction, audition, percussion, palpation, and pulse examination to ensure complete consideration in medical care. Arrangement of these diagnostic items in a more systematic manner along with a designed record format for tongue and pulse examinations would be necessary for clinical practice. Practice manuals proposing the definition, description, and standardized process for each diagnostic criterion have also been developed for correct implementation.
The limitation of homogeneous education backgrounds is inevitable, since we excluded CM clinicians who had only practicing experience, but no postgraduate degrees from participating in the Delphi panel, as some research background would be required for understanding of the Delphi method and the statistical results circulated during the processes. The panelists’ average practicing experience of 11.7 years was considered to be a good representation of their clinical experience.
Because the Liu Yin (six excesses) syndromes were general categories, exploratory and confirmatory factor analyses were conducted to derive and validate the underlying structures of the SEED scale and to reveal the correlations among signs and symptoms. Future studies, including clinical observations to avoid item redundancy and to confirm the clinical practice of the SEED scale in infectious diseases, are required.
It’s the first scale based on the six excesses (Liu Yin) and constructed by the Delphi method; the CM experts epitomized the contents of CM literature and journal articles via the process. Future applications of the SEED scale in clinical practice, research and CM education are expected.
Conclusion
A CM-based SEED scale was developed for the evaluation and diagnosis of infectious diseases based on only signs and symptoms.
Authors’ contributions
YCS conceived and designed the study. PJC, TCL, LLC and JDL analyzed the data. PJC wrote the manuscript. TCL and CHC revised the manuscript. All authors read and approved the final manuscript.
Acknowledgements
This project was supported by Grant (number CCMP97-RD-113) from the Committee on Traditional Chinese Medicine and Pharmacy, Department of Health, Executive Yuan, Taiwan. The support of statistic analysis from the Biostatistics Center of China Medical University was also appreciated.
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Contributor Information
Pei-Jung Chiang, Email: aerin.chiang@vghtc.gov.tw.
Tsai-Chung Li, Email: tcli@mail.cmu.edu.tw.
Chih-Hung Chang, Email: chchang@northwestern.edu.
Li-Li Chen, Email: lily@mail.cmu.edu.tw.
Jun-Dai Lin, Email: jdlin@asia.edu.tw.
Yi-Chang Su, Email: sychang@mail.cmu.edu.tw.
References
- 1.Writing Committee of the WHO Consultation on Clinical Aspects of Pandemic Influenza Clinical aspects of pandemic 2009 influenza A (H1N1) virus infection. N Engl J Med. 2010;362(18):1708–1719. doi: 10.1056/NEJMra1000449. [DOI] [PubMed] [Google Scholar]
- 2.Miller E, Hoschler K, Hardelid P, Stanford E, Andrews N, Zambon M. Incidence of 2009 pandemic influenza A H1N1 infection in England: a cross-sectional serological study. Lancet. 2010;375(9720):1100–1108. doi: 10.1016/S0140-6736(09)62126-7. [DOI] [PubMed] [Google Scholar]
- 3.Baden LR, Drazen JM, Kritek PA, Curfman GD, Morrissey S, Campion EW. H1N1 Influenza A disease—information for health professionals. N Engl J Med. 2009;360(25):2666–2667. doi: 10.1056/NEJMe0903992. [DOI] [PubMed] [Google Scholar]
- 4.Echevarría-Zuno S, Mejía-Aranguré JM, Mar-Obeso AJ, Grajales-Muñiz C, Robles-Pérez E, González-León M, et al. Infection and death from influenza A H1N1 virus in Mexico: a retrospective analysis. The Lancet. 2009;374(9707):2072–2079. doi: 10.1016/S0140-6736(09)61638-X. [DOI] [PubMed] [Google Scholar]
- 5.Gambotto A, Barratt-Boyes SM, de Jong MD, Neumann G, Kawaoka Y. Human infection with highly pathogenic H5N1 influenza virus. Lancet. 2008;371(9622):1464–1475. doi: 10.1016/S0140-6736(08)60627-3. [DOI] [PubMed] [Google Scholar]
- 6.Webster RG, Govorkova EA. H5N1 influenza-continuing evolution and spread. N Engl J Med. 2006;355(21):2174–2177. doi: 10.1056/NEJMp068205. [DOI] [PubMed] [Google Scholar]
- 7.Blyth CC, Iredell JR, Dwyer DE. Rapid-test sensitivity for novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;361(25):2493. doi: 10.1056/NEJMc0909049. [DOI] [PubMed] [Google Scholar]
- 8.Oner AF, Bay A, Arslan S, Akdeniz H, Sahin HA, Cesur Y, et al. Avian influenza A (H5N1) infection in eastern Turkey in 2006. N Engl J Med. 2006;355(21):2179–2185. doi: 10.1056/NEJMoa060601. [DOI] [PubMed] [Google Scholar]
- 9.Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, et al. Avian influenza A (H5N1) infection in humans. N Engl J Med. 2005;353(13):1374–1385. doi: 10.1056/NEJMra052211. [DOI] [PubMed] [Google Scholar]
- 10.Abdel-Ghafar AN, Chotpitayasunondh T, Gao Z, Hayden FG, Nguyen DH, de Jong MD, et al. Update on avian influenza A (H5N1) virus infection in humans. N Engl J Med. 2008;358(3):261–273. doi: 10.1056/NEJMra0707279. [DOI] [PubMed] [Google Scholar]
- 11.Glezen WP. Prevention and treatment of seasonal influenza. N Engl J Med. 2008;359(24):2579–2585. doi: 10.1056/NEJMcp0807498. [DOI] [PubMed] [Google Scholar]
- 12.Stamm W, Wagner K, Amsel R, Alexander E, Turck M, Counts G, et al. Causes of the acute urethral syndrome in women. N Engl J Med. 1980;303(8):409–415. doi: 10.1056/NEJM198008213030801. [DOI] [PubMed] [Google Scholar]
- 13.Richards D, Toop L, Chambers S, Fletcher L. Response to antibiotics of women with symptoms of urinary tract infection but negative dipstick urine test results: double blind randomised controlled trial. BMJ. 2005;331(7509):143–146. doi: 10.1136/bmj.38496.452581.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poehling KA, Edwards KM, Weinberg GA, Szilagyi P, Staat MA, Iwane MK, et al. The underrecognized burden of influenza in young children. N Engl J Med. 2006;355(1):31–40. doi: 10.1056/NEJMoa054869. [DOI] [PubMed] [Google Scholar]
- 15.Lessler J, Reich NG, Brookmeyer R, Perl TM, Nelson KE, Cummings DA. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis. 2009;9(5):291–300. doi: 10.1016/S1473-3099(09)70069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang JL, Liu BY, Ma KW. Traditional Chinese medicine. Lancet. 2008;372(9654):1938–1940. doi: 10.1016/S0140-6736(08)61354-9. [DOI] [PubMed] [Google Scholar]
- 17.Peng J. Historical studies of the systems of diagnosis and treatment of exopathogenic diseases. Zhonghua Yi Shi Za Zhi. 1999;29(2):70–73. [PubMed] [Google Scholar]
- 18.Scheid V. The globalization of Chinese medicine. Lancet. 1999;354 (Suppl:SIV10). [DOI] [PubMed]
- 19.Zhang GG, Bausell B, Lao L, Handwerger B, Berman BM. Assessing the consistency of traditional Chinese medical diagnosis: an integrative approach. Altern Ther Health Med. 2003;9(1):66–71. [PubMed] [Google Scholar]
- 20.Zhang GG, Lee W, Bausell B, Lao L, Handwerger B, Berman B. Variability in the traditional Chinese medicine (TCM) diagnoses and herbal prescriptions provided by three TCM practitioners for 40 patients with rheumatoid arthritis. J Altern Complement Med. 2005;11(3):415–421. doi: 10.1089/acm.2005.11.415. [DOI] [PubMed] [Google Scholar]
- 21.Kalauokalani D, Sherman KJ, Cherkin DC. Acupuncture for chronic low back pain: diagnosis and treatment patterns among acupuncturists evaluating the same patient. South Med J. 2001;94(5):486–492. doi: 10.1097/00007611-200194050-00008. [DOI] [PubMed] [Google Scholar]
- 22.Birch S, Sherman K. Zhong Y acupuncture and low-back pain: traditional Chinese medical acupuncture differential diagnoses and treatments for chronic lumbar pain. J Altern Complement Med. 1999;5(5):415–425. doi: 10.1089/acm.1999.5.415. [DOI] [PubMed] [Google Scholar]
- 23.Lindahl MG, Barrett R, Peterson D, Zheng L, Nedrow A. Development of an integrative patient history intake tool: a Delphi study. Altern Ther Health Med. 2005;11(1):52–56. [PubMed] [Google Scholar]
- 24.Liu GP, Wang YQ, Dong Y, Zhao NQ, Xu ZX, Li FF, et al. Development and evaluation of an inquiry scale for diagnosis of heart system syndromes in traditional Chinese medicine. Zhong Xi Yi Jie He Xue Bao. 2009;7(1):20–24. doi: 10.3736/jcim20090103. [DOI] [PubMed] [Google Scholar]
- 25.Schnyer RN, Conboy LA, Jacobson E, McKnight P, Goddard T, Moscatelli F, et al. Development of a Chinese medicine assessment measure: an interdisciplinary approach using the Delphi method. J Altern Complement. 2005;11(6):1005–1013. doi: 10.1089/acm.2005.11.1005. [DOI] [PubMed] [Google Scholar]
- 26.Hogeboom CJ, Sherman KJ, Cherkin DC. Variation in diagnosis and treatment of chronic low back pain by traditional Chinese medicine acupuncturists. Complement Ther Med. 2001;9(3):154–166. doi: 10.1054/ctim.2001.0457. [DOI] [PubMed] [Google Scholar]
- 27.Sherman KJ, Cherkin DC, Hogeboom CJ. The diagnosis and treatment of patients with chronic low-back pain by traditional Chinese medical acupuncturists. J Altern Complement Med. 2001;7(6):641–650. doi: 10.1089/10755530152755199. [DOI] [PubMed] [Google Scholar]
- 28.Coeytaux RR, Chen W, Lindemuth CE, Tan Y, Reilly AC. Variability in the diagnosis and point selection for persons with frequent headache by traditional Chinese medicine acupuncturists. J Altern Complement Med. 2006;12(9):863–872. doi: 10.1089/acm.2006.12.863. [DOI] [PubMed] [Google Scholar]
- 29.Fitch K, Bernstein SJ, Aguilar MD, Burnand B, Lacalle JR, Lazaro P. The RAND/UCLA appropriateness method user’s manual: Natl Book Network 2000.
- 30.Dixon AE, Sugar EA, Zinreich SJ, Slavin RG, Corren J, Naclerio RM, et al. Criteria to screen for chronic sinonasal disease. Chest. 2009;136(5):1324–1332. doi: 10.1378/chest.08-1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang W, Doherty M, Leeb BF, Alekseeva L, Arden NK, Bijlsma JW, et al. EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: report of a task force of ESCISIT. Ann Rheum Dis. 2009;68(1):8–17. doi: 10.1136/ard.2007.084772. [DOI] [PubMed] [Google Scholar]
- 32.Sherman PM, Hassall E, Fagundes-Neto U, Gold BD, Kato S, Koletzko S, et al. A global, evidence-based consensus on the definition of gastroesophageal reflux disease in the pediatric population. Am J Gastroenterol. 2009;104(5):1278–1295. doi: 10.1038/ajg.2009.129. [DOI] [PubMed] [Google Scholar]
- 33.Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. The Lancet. 2005;366(9503):2112–2117. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (screening tool of older person’s prescriptions) and START (screening tool to alert doctors to right treatment) consensus validation. Int J Clin Pharmacol Ther. 2008;46(2):72–83. doi: 10.5414/CPP46072. [DOI] [PubMed] [Google Scholar]
- 35.Bowles KH, Holmes JH, Ratcliffe SJ, Liberatore M, Nydick R, Naylor MD. Factors identified by experts to support decision making for post acute referral. Nurs Res. 2009;58(2):115–122. doi: 10.1097/NNR.0b013e318199b52a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 37.Koekkoek B, van Meijel B, Schene A, Hutschemaekers G. A Delphi study of problems in providing community care to patients with nonpsychotic chronic mental illness. Psychiatr Serv. 2009;60(5):693–697. doi: 10.1176/ps.2009.60.5.693. [DOI] [PubMed] [Google Scholar]
- 38.Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, et al. Use of electronic health records in US hospitals. N Engl J Med. 2009;360(16):1628–1638. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 39.Tierney S, Fox JR. Chronic anorexia nervosa: a Delphi study to explore practitioners’ views. Int J Eat Disord. 2009;42(1):62–67. doi: 10.1002/eat.20557. [DOI] [PubMed] [Google Scholar]
- 40.Alahlafi A, Burge S. What should undergraduate medical students know about psoriasis? Involving patients in curriculum development: modified Delphi technique. BMJ. 2005;330(7492):633–636. doi: 10.1136/bmj.330.7492.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kassab S, Cummings M, Berkovitz S, van Haselen R, Fisher P. Homeopathic medicines for adverse effects of cancer treatments. Cochrane Database Syst Rev. 2009;(2):CD004845. doi:10.1002/14651858.CD004845.pub2 [DOI] [PMC free article] [PubMed]
- 42.Salliot C, Dernis E, Lavie F, Cantagrel A, Gaudin P, Wendling D, Claudepierre P, Flipo RM, Goupille PM, Le Loët X, Maillefert JF, Paul C, Saraux A, Schaeverbeke T, Tebib J, Combe B. Diagnosis of peripheral psoriatic arthritis: recommendations for clinical practice based on data from the literature and experts opinion. Joint Bone Spine. 2009;76(5):532–539. doi: 10.1016/j.jbspin.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 43.Taylor WJ, Shewchuk R, Saag KG, Schumacher HR, Jr, Singh JA, Grainger R, et al. Toward a valid definition of gout flare: results of consensus exercises using Delphi methodology and cognitive mapping. Arthritis Rheum. 2009;61(4):535–543. doi: 10.1002/art.24166. [DOI] [PubMed] [Google Scholar]
- 44.Murray PT, Devarajan P, Levey AS, Eckardt KU, Bonventre JV, Lombardi R, et al. A framework and key research questions in AKI diagnosis and staging in different environments. Clin J Am Soc Nephrol. 2008;3(3):864–868. doi: 10.2215/CJN.04851107. [DOI] [PubMed] [Google Scholar]
- 45.Guellac N, Niehues T. Interdisciplinary and evidence-based treatment guideline for juvenile idiopathic arthritis. Klin Padiatr. 2008;220(6):392–402. doi: 10.1055/s-0028-1086037. [DOI] [PubMed] [Google Scholar]
- 46.Graham B, Regehr G, Wright JG. Delphi as a method to establish consensus for diagnostic criteria. J Clin Epidemiol. 2003;56(12):1150–1156. doi: 10.1016/S0895-4356(03)00211-7. [DOI] [PubMed] [Google Scholar]
- 47.Pastor AC, Osman F, Teitelbaum DH, Caty MG, Langer JC. Development of a standardized definition for Hirschsprung’s-associated enterocolitis: a Delphi analysis. J Pediatr Surg. 2009;44(1):251–256. doi: 10.1016/j.jpedsurg.2008.10.052. [DOI] [PubMed] [Google Scholar]
- 48.Cheon JH, Kim ES, Shin SJ, Kim TI, Lee KM, Kim SW, et al. Development and validation of novel diagnostic criteria for intestinal Behcet’s disease in Korean patients with ileocolonic ulcers. Am J Gastroenterol. 2009;104:2492–2499. doi: 10.1038/ajg.2009.331. [DOI] [PubMed] [Google Scholar]
- 49.Campos F, Sousa A, Rodrigues V, Marques A, Queiros C, Dores A. Practical guidelines for peer support programmes for mental health problems. Rev Psiquiatr Salud Ment. 2014 doi: 10.1016/j.rpsm.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 50.Ferreira JJ, Santos AT, Domingos J, Matthews H, Isaacs T, Duffen J, et al. Clinical parameters and tools for home-based assessment of Parkinson’s disease: results from a Delphi study. J Parkinsons Dis. 2015;5(2):281–290. doi: 10.3233/JPD-140493. [DOI] [PubMed] [Google Scholar]
- 51.Loeffen EA, Mulder RL, Kremer LC, Michiels EM, Abbink FC, Ball LM, et al. Development of clinical practice guidelines for supportive care in childhood cancer-prioritization of topics using a Delphi approach. Support Care Cancer. 2014 doi: 10.1007/s00520-014-2559-7. [DOI] [PubMed] [Google Scholar]
- 52.Munck A, Mayell SJ, Winters V, Shawcross A, Derichs N, Parad R, et al. Cystic fibrosis screen positive, inconclusive diagnosis (CFSPID): a new designation and management recommendations for infants with an inconclusive diagnosis following newborn screening. J Cyst Fibros. 2015 doi: 10.1016/j.jcf.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 53.Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R. SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endosc. 2015 doi: 10.1007/s00464-015-4079-z. [DOI] [PubMed] [Google Scholar]
- 54.Roberts DM, Yates C, Megarbane B, Winchester JF, Maclaren R, Gosselin S, et al. Recommendations for the role of extracorporeal treatments in the management of acute methanol poisoning: a systematic review and consensus statement. Crit Care Med. 2015;43(2):461–472. doi: 10.1097/CCM.0000000000000708. [DOI] [PubMed] [Google Scholar]
- 55.Slade SC, Dionne CE, Underwood M, Buchbinder R. Standardised method for reporting exercise programmes: protocol for a modified Delphi study. BMJ Open. England: BMJ Publishing Group Limited; 2014. p. e006682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Suzuki Y, Fukasawa M, Nakajima S, Narisawa T, Keiko A, Kim Y. Developing a consensus-based definition of “Kokoro-no Care” or mental health services and psychosocial support: drawing from experiences of mental health professionals who responded to the Great East Japan Earthquake. PLoS Curr. 2015 doi: 10.1371/currents.dis.cfcbaf509711641ab5951535851e572e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Trevelyan EG, Turner WA, Robinson N. Developing an acupuncture protocol for treating phantom limb pain: a Delphi consensus study. Acupunct Med. England: BMJ Publishing Group Limited; 2015. pp. 42–50. [DOI] [PubMed] [Google Scholar]
- 58.James DJ, Warren-Forward HM. Development of consensus statements for pregnancy screening in diagnostic nuclear medicine: a delphi study. J Nucl Med Technol. United States: The Society of Nuclear Medicine and Molecular Imaging, Inc; 2015. pp. 74–79. [DOI] [PubMed] [Google Scholar]
- 59.Kunneman M, Pieterse AH, Stiggelbout AM, Marijnen CA. Which benefits and harms of preoperative radiotherapy should be addressed? A Delphi consensus study among rectal cancer patients and radiation oncologists. Radiother Oncol. 2015;114(2):212–217. doi: 10.1016/j.radonc.2014.11.034. [DOI] [PubMed] [Google Scholar]
- 60.Muller BG, van den Bos W, Brausi M, Futterer JJ, Ghai S, Pinto PA, et al. Follow-up modalities in focal therapy for prostate cancer: results from a Delphi consensus project. World J Urol. 2015 doi: 10.1007/s00345-014-1475-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Paneque M, Sequeiros J, Skirton H. Quality issues concerning genetic counselling for presymptomatic testing: a European Delphi study. Eur J Hum Genet. 2015 doi: 10.1038/ejhg.2015.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Strosberg JR, Fisher GA, Benson AB, Anthony LB, Arslan B, Gibbs JF, et al. Appropriateness of systemic treatments in unresectable metastatic well-differentiated pancreatic neuroendocrine tumors. World J Gastroenterol. 2015;21(8):2450–2459. doi: 10.3748/wjg.v21.i8.2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Temkin-Greener H, Ladwig S, Caprio T, Norton S, Quill T, Olsan T, et al. Developing palliative care practice guidelines and standards for nursing home-based palliative care teams: a Delphi study. J Am Med Dir Assoc. 2015;16(1):86 e1–86 e7. doi: 10.1016/j.jamda.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 64.Vilches-Moraga A, Arino-Blasco S, Verdejo-Bravo C, Mateos-Nozal J. University studies plan in geriatric medicine developed using a modified Delphi technique. Rev Esp Geriatr Gerontol. 2014 doi: 10.1016/j.regg.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 65.Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR, Lazaro P, et al. The RAND/UCLA appropriateness users manual. Santa Monica: RAND Institute; 2001. [Google Scholar]
- 66.Anonymous. Huangdi’s internal classic, before Han dynasty.
- 67.Hsiao CF, Tsou HH, Wu YJ, Lin CH, Chang YJ. Translation in different diagnostic procedures—traditional Chinese medicine and Western medicine. J Formos Med Assoc. 2008;107(12 Suppl):74–85. doi: 10.1016/S0929-6646(09)60011-5. [DOI] [PubMed] [Google Scholar]
- 68.O’Brien KA, Abbas E, Zhang J, Guo ZX, Luo R, Bensoussan A, et al. Understanding the reliability of diagnostic variables in a Chinese Medicine examination. J Altern Complement Med. 2009;15(7):727–734. doi: 10.1089/acm.2008.0554. [DOI] [PubMed] [Google Scholar]
- 69.Chiang PJ, Su YC, Liou DM. Acupuncture for chronic low back pain. N Engl J Med. 2010;363(18):1775–1776. doi: 10.1056/NEJMc1009789. [DOI] [PubMed] [Google Scholar]
- 70.WHO Regional Office for the Western Pacific. WHO international standard terminologies on traditional medicine in the Western Pacific Region. 2007.


