Abstract
Fungal keratitis accounts for 6–53% of all cases of ulcerative keratitis in variable studies. The majority of cases are due to septate fungi. The abnormal cornea in cases of dry eye syndrome, chronic ulceration, erythema multiform and possibly HIV infection is infected more commonly with Candida, most commonly Candida albicans. Candida parapsilosis affects neonates and intensive care unit (ICU) patients and it has been recently found with increasing frequency. In a previous study on mycotic keratitis in our tertiary eye hospital, filamentous fungi were more commonly isolated than yeasts. We are presenting 2 successive cases of corneal graft infection by Candida parapsilosis referred to us from another eye center to attract the attention of ophthalmologists and health workers to such an infection.
Keywords: Candida parapsilosis, Corneal graft, Keratitis
Introduction
Fungal infection of the cornea may constitute 6–53% of all cases of ulcerative keratitis and the majority follow trauma with plant material.1, 2 Clinically, it is recognized by coarse granular corneal infiltrate within 24–36 h after trauma. The vast majority are caused by septate filamentous fungi, however compromised corneas are subject to yeast infection: usually Candida species.2
Case reports
Case 1
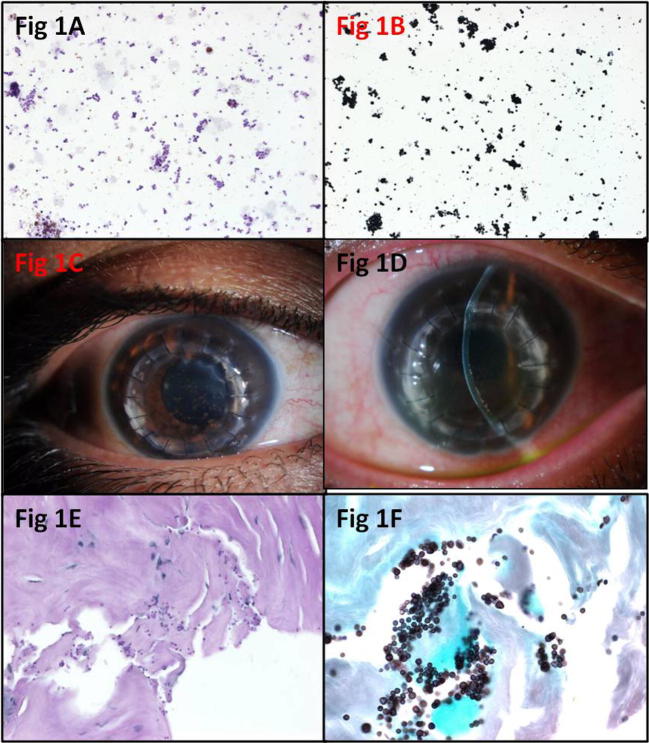
A 33-year-old Saudi male, known case of keratoconus presented to a private eye center 1 year ago (early 2014) and underwent penetrating keratoplasty (PKP) in the right eye with no complications. He developed mild haze at the edge of the graft 1 month post PKP followed by anterior chamber (AC) reaction and pigmented keratic precipitates (KPs). There was no definite infiltrate at that time. The AC tap showed pigment laden macrophages, dispersed pigment and yeast forms (Fig. 1a and b). He was started on amphotericin B topically and was referred to our hospital with VA 20/400 OD which improves to 20/300 with PH and IOP of 24 mmHg, OD (with the use of anti-glaucoma medications). Slit lamp examination (SLE) of his right eye showed whitish infiltrate versus scar at the junction of the graft, deep AC with +4 cells and no further view. (Fig. 1c). He was started on Voriconazole 1% eye drops QID, Predforte drops q 4 h daily tapered over 2 weeks and Timolol twice daily to control his IOP, all OD. Follow up showed increasing infiltrate (Fig. 1d) and the patient was admitted for corneal biopsy which further confirmed the presence of these yeast in the areas of infiltrate (Fig. 1e and f). The yeast forms proved by culture to be Candida parapsilosis.
Figure 1.
(A) Smear of the aqueous showing dispersed pigment and yeast forms (Original magnification ×400 Periodic Acid Schiff PAS). (B) The yeast forms (original magnification ×1000 Gomori Methenamine silver GMS, oil). (C) The clinical appearance of the right eye corneal graft at presentation. (D) The follow up appearance of the graft on medications. (E) The corneal biopsy tissue showing yeast forms with Periodic Acid Schiff stain (original magnification ×400 PAS). (F) The yeast forms confirmed by staining with Gomori Methenamine silver (original magnification ×1000 GMS, oil).
Case 2
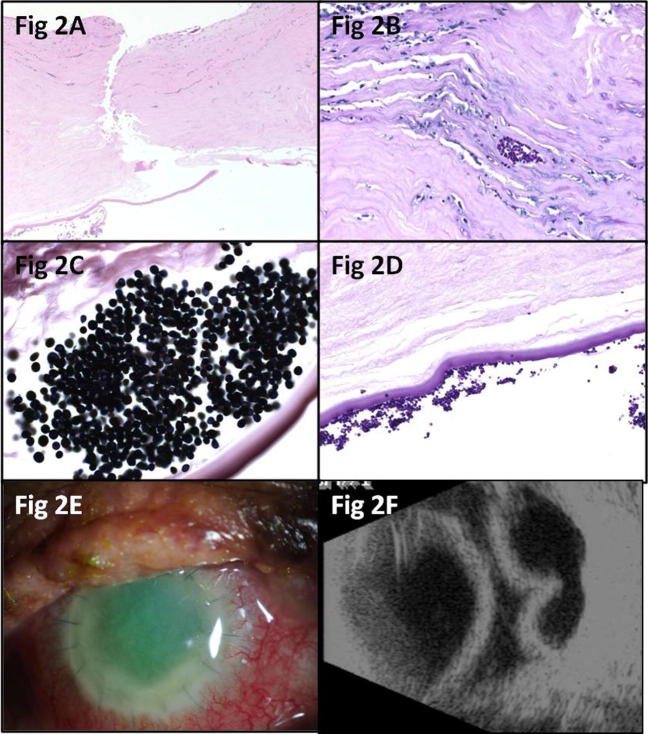
An 82-year-old Saudi male presented for the first time to King Khaled Eye Specialist Hospital (KKESH) in 2011 with phthisical left globe because of corneal scarring secondary to chicken pox infection in childhood. He also had immature cataract with light perception (LP) vision on the right. Systemically he was known to have diabetes and bronchial asthma. He underwent PKP, extracapsular cataract extraction (ECCE) and posterior chamber (PC) intraocular lens (IOL) implantation in the right eye with guarded prognosis elsewhere in December 2012. His graft failed after 1 year. He had another PKP in early 2014 -in the same eye center of case 1- and developed a persistent epithelial defect for which medial tarsorrhaphy and Amniotic membrane transplant (AMT) were performed. He presented to KKESH in May 2014 with poor vision of counting fingers (CF) in the right eye, IOP of 16 mmHg and persistent epithelial defect involving 85% of the graft which was hazy. Remnant of AMT was seen centrally. Other findings included: intact sutures, deep AC with AC reaction (not specified) and an iris fixated PC IOL. The patient was admitted and a therapeutic PKP was performed in June 2014 and the tissue of the second graft was submitted for both microbiology and tissue diagnosis. The histopathologic examination of the previous corneal graft showed sub-acute keratitis and numerous yeast forms mainly at the periphery of the graft, within the posterior stroma and retrocorneal collection of yeast forms along Descemet’s membrane (Fig. 2a–d). His last follow up showed VA of HM, soft right eye with hazy graft, +1 flare in the AC, but no sign of active infection. He also developed choroidal detachment which was managed by choroidal drainage (Fig. 2e and f). The culture revealed the same type of Candida species.
Figure 2.
(A) Lower magnification histopathologic photo of the second case corneal graft ulceration (original magnification ×100 Hematoxylin & Eosin H&E). (B) Pockets of yeast forms at the graft edge (original magnification ×400 Periodic Acid Schiff PAS). (C) The yeast forms with Gomori Methenamine silver stain, (original magnification ×1000, GMS, oil). (D) Retrocorneal yeast forms along Descemet’s membrane (original magnification ×400 Periodic Acid Schiff PAS). (E) The clinical appearance of the hazy therapeutic corneal graft of the right eye. (F) The ultrasound of the right eye showing post-operative choroidal detachment.
Discussion
Fungal keratitis accounts for 6–53% of all cases of ulcerative keratitis in variable studies and the majority of cases are due to septate fungi.1, 2 The abnormal cornea in cases of dry eye syndrome, chronic ulceration, erythema multiform and possibly HIV infection is infected more commonly with Candida.2 In a small series of spontaneous ulcerative keratitis in immunocompromised patients 3 out of the 5 infected corneas (in 4 cases) were caused by Candida albicans.3 These cases were known intravenous drug abusers with proved HIV or AIDS in 3 out of the 4 cases. None of them had any predisposing factor for ulcerative keratitis and no history of trauma, contact lens wear or ocular surface disease.
Uncommon Candida species such as Candida lipolytica and Candida humicola have been reported in post-traumatic keratitis.4, 5 In regard to corneal graft fungal infections in the form of infectious crystalline keratoplasty, several Candida species have been identified including Candida guilliermondii and parapsilosis.6, 7 The most commonly isolated yeast in infections generally is Candida albicans however it seems that Candida parapsilosis is found with increasing frequency.8 Candida parapsilosis affects neonates and intensive care unit (ICU) patients. It has affinity for foreign material with infections being related to peritoneal dialysis catheters, central lines, prosthetic heart valves and other indwelling access devices. As a result Candida parapsilosis is found to be increasingly responsible for outbreaks in hospitals with the hands of healthcare workers being the predominant environmental source.9, 10
Fungi secrete enzymes which are important for pathogenesis: phospholipases and proteases but the relationship between Candida parapsilosis virulence and phospholipases phenotype is unclear. On the other hand the surface adherence capacity of Candida has been found to be linked to the formation of biofilms.11 This adhesion feature seems to be critical in yeast pathogenesis especially for Candida parapsilosis as the organism is thought to be acquired from exogenous sources then adheres to devices and finally invades the host. Kuhn and his co-authors found predominant clonality of Candida parapsilosis in their outbreak isolates cultured from blood or catheter as well as at least one health worker hand isolate. Therefore they considered their outbreak to have nosocomial environmental origin.10 They also showed that the outbreak clone produced more biofilm than all other strains.10
The diagnosis of fungal infections in the ophthalmic practice requires: establishment of the presence of pathology, obtaining tissue to visualize the fungus and isolation of the responsible fungus, particularly by culture. The culture result in both our cases originating from the same outside eye center (one from aqueous and the other from both aqueous and corneal tissue) confirmed Candida parapsilosis and no other pathogens. In regard to fungal infections of corneal grafts, Al-Assiri and his co-authors recommended routine fungal cultures of the donor rims at the time of PKP as an important diagnostic tool to allow identification of potential organisms that might be transmitted to the graft leading to a late-onset graft infection by fungi such as Candida glabrata in their reported case.12
In a previous study on mycotic keratitis in our institution (during the period: 2006–2009), filamentous fungi were more commonly isolated than yeasts accounting for 71.3% (Aspergillus being the commonest followed by Fusarium) compared to 28.7% yeast infection most commonly by Candida species.12 In that study 5 cases of Candida parapsilosis were identified, however the infection was associated with other virulent pathogens in all these cases.13
In regard to the management, combination of surgery and antifungal drug is the usual therapeutic modality for most of eye fungal infections.2 Fungal keratitis is usually treated with topical antifungals such as Natamycin and Amphotericin B and may require the use of Azoles especially for Candida keratitis. Finally debridement and surgical intervention may be eventually required such as in our second case which was treated by PKP.2 In addition, prophylactic antifungal therapy implementation following PKP has been recommended in donor rim culture-positive cases.12
In conclusion, although we had only 2 successive cases within a short period of time originating from a single eye center (and not an outbreak), we believe that these are considered to be nosocomial infections. The corresponding eye care facility should be alerted for possible screening of their health workers. The practice of obtaining fungal cultures of donor corneal rims at the time of PKP has been also recommended.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Thomas P. Mycotic Keratitis – an underestimated mycosis. J Med Vet Mycol. 1994;32:235–256. doi: 10.1080/02681219480000321. [DOI] [PubMed] [Google Scholar]
- 2.Klotz S.a., Penn C.C., Negvesky G.j., Butrus S.I. Fungal and parasitic infections of the eye. Clin Microbiol Rev. 2000;13(4):662–685. doi: 10.1128/cmr.13.4.662-685.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Artistimuno B., Nirankari V.S., Hemady R.k., Rodrigues M.M. Spontaneous ulcerative keratitis in immunocompromised patients. Am J Ophthalmol. 1993;115(2):202–208. doi: 10.1016/s0002-9394(14)73924-8. [DOI] [PubMed] [Google Scholar]
- 4.Nitzulescu V., Nicalescu M. Ophthalmopathy determined by Candida humicola. Arch Roum Pathol Exp Microbiol. 1975;34:357–361. [PubMed] [Google Scholar]
- 5.Nitzulescu V., Nicalescu M. Three cases of ocular candidiasis caused by Candida lipolytica. Arch Roum Pathol Exp Microbiol. 1976;35:269–272. [PubMed] [Google Scholar]
- 6.Ainbinder D.j., Parmley V.C., Mader T.H., Nelson M.L. Infectious crystalline keratopathy caused by Candida guilliermondii. Am J Ophthalmol. 1997;125(5):723–724. doi: 10.1016/s0002-9394(98)00024-5. [DOI] [PubMed] [Google Scholar]
- 7.Rhem M.V., Wilhelmus K.R., Fornt R.L. Infectious crystalline keratopathy caused by Candida parapsilosis. Cornea. 1996;15:543–544. [PubMed] [Google Scholar]
- 8.Safdar A., perlin D.S., Armstrong D. Hematogenous infections due to the Candida parapsilosis, changing trends in fungemic patients at a comprehensive cancer center during the last four decades. Diag Microbiol Infect Dis. 2002;44:11–16. doi: 10.1016/s0732-8893(02)00423-6. [DOI] [PubMed] [Google Scholar]
- 9.Lupetti A., Tavanti A., Dabini P., Ghelardi E., Corsihi V., Merusi I. Horizontal transmission of Candida parapsilosis candidemia in a neonatal intensive care unit. J Clin Microbiol. 2002;40:2363–2369. doi: 10.1128/JCM.40.7.2363-2369.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuhn D.M., Mukherjee P.K., Clark T.A., Pujol C., Chandra J., Hajjeh R.A. Candida parapsilosis characterization in an outbreak setting. Emerg Infectious Disease. 2004;10(6):1074–1081. doi: 10.3201/eid1006.030873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramage G., Vande Walle K., Wickes B.L., Lopez-Ribot J.L. Biofilm formation by Candida dubliniensis. J Clin Microbiol. 2001;239:3234–3240. doi: 10.1128/JCM.39.9.3234-3240.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Assiri A., Al-Jastaneiah S., Al-Khalaf A., Al-Fraikh H., Wagoner M.D. Late onset donor-to-host transmission of Candida glabrata following corneal transplantation. Cornea. 2006;25(1):123–125. doi: 10.1097/01.ico.0000164777.80879.07. [DOI] [PubMed] [Google Scholar]
- 13.Alkatan H., Athmanathan S., Canites C.C. Incidence and microbiological profile of mycotic keratitis in a tertiary care eye hospital: a retrospective analysis. Saudi J Ophthalmol. 2012;26(2):217–221. doi: 10.1016/j.sjopt.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]