Introduction
Despite striking improvement in the prognosis and survival in patients with coronary artery disease (CAD), hypertension, and congenital heart disease, the prevalence of heart failure (HF) is still growing.1–3 HF is the most common cause of hospitalization after normal delivery - approximately 1 million patients are hospitalized annually for HF in the United States.4 Moreover, the prognosis of HF is relatively poor, with 25% mortality at 1 year and 50% mortality at 5 years (stage D HF: 80% mortality at 5 years) - worse than that of many cancers.1,2 The clinical profile, and outcome of HF in western population is well demonstrated after the release of several large registries such as Acute Decompensated Heart Failure National Registry (ADHERE) and the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF). 5–7 Based on data from ADHERE registry, lower systolic blood pressure (BP), elevated serum BUN and creatinine, hyponatremia, older age, presence of dyspnea at rest, and absence of chronic beta-blocker were identified as independent predictors of mortality.5,6 On the other hand, data on the prevalence and outcome of stroke in patients hospitalized for HF are very scarce and mainly driven from studies conducted in developed countries. Moreover, little systematic data exist regarding the clinical profile and management of HF patients in the Middle East population that have different ethnic, cultural, and socio-economic background. Hence, the Gulf Heart Association initiated and finalized the Gulf Acute Heart Failure Registry (Gulf CARE) to provide the first systematic report of the characteristics of acute HF (AHF) patients in this region.
Gulf CARE registry
The Gulf CARE is a prospective, multinational, multicentre registry aimed to describe the clinical characteristics, management, and outcomes of consecutive patients hospitalized with AHF to 47 hospitals in 7 Middle Eastern countries – Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, United Arab Emirates, and Yemen – between February and November 2012. The data has been recently published in the European Journal of Heart Failure in 2015.8 A total of 5005 patients, aged 59 ± 15 years, were enrolled. Fifty five percent of patients presented with acute decompensated chronic HF (ADCHF) while 45% had de novo AHF. Patients were followed up by telephone at 3 months and either by telephone or by a clinic visit at 1 year.
Sixty nine percent of patients had HF with reduced ejection fraction < 40% (HFrEF). The prevalence of hypertension was 61%, diabetes mellitus (DM) was 50%, CAD was 47%, and atrial fibrillation (AF) was 14%. CAD was the most prevalent aetiology (53%) followed by idiopathic dilated cardiomyopathy (18%), hypertensive heart disease (16%), and valvular heart disease (9%). At discharge, 71% and 78% of patients received beta-blockers and ACE inhibitors/ARBs, respectively. Less than 10% of patients had coronary intervention and/or device therapy. In-hospital mortality was 6.3%. The rate of re-hospitalization at 3 and 12 months were 18% and 40%, while cumulative mortality were 13% and 20% respectively. Patients with ADCHF were older (61 vs. 57 years; p < 0.001), and more likely to have a history of CAD (60% vs. 30%; P < 0.001), valvular heart disease (18% vs. 8%; p < 0.001), AF (17% vs. 6%; p < 0.001), hypertension (67% vs. 54%; p < 0.001), DM (54% vs. 44%; p < 0.001), hyperlipidemia (43% vs. 27%; p < 0.001), chronic kidney disease/dialysis (19% vs. 9%; p < 0.001), and prior stroke/transient ischemic attack (10.2% vs. 5.5%; p < 0.001) compared to those with de novo AHF. The median brain natruretic peptide (BNP) was significantly higher in de novo AHF patients than in those with ADCHF (1605 vs. 1154 pg/mL; p = 0.007).
A retrospective analysis of the Gulf CARE data was performed based on the presence or absence of prior stroke and the results were published in the British Medical Journal in 2015.9 The prevalence of prior stroke was 8.1 %. AHF patients with prior stroke were more likely to be older (66.5 vs. 59 years, p = 0.001), and to have hypertension (84.4% vs. 59.1%, p = 0.001), DM (69.3% vs. 48.1%, p = 0.001), AF (24.3% vs. 11.1%), CAD (62.9% vs. 45.3%, p = 0.001), peripheral arterial disease (15.1% vs. 13.5%, p = 0.001), left ventricle (LV) systolic dysfunction (56.4% vs. 44.6%, p = 0.001), and chronic kidney disease (28% vs. 13.7%, p = 0.001), and less likely to be smokers (16.1% vs. 22.6%, p = 0.003) compared to those with no history of stroke. Patients with prior stroke were more likely to require invasive (12.4% vs. 8.1%, p = 0.003) and non-invasive ventilations (15.3% vs. 8.9%, p = 0.001), and were also more likely to require inotropic support (21.8% vs. 15.1%, p = 0.001) and renal replacement therapy (2.5% vs. 4.5%, p = 0.02) compared to those without history of prior stroke. Therefore, patients with prior stroke had a longer hospital stay (p = 0.03) and a significantly higher 1-year mortality rate (32.7% vs. 23.2%, p = 0.001). In a multivariate regression model, stroke was identified as an independent predictor for in-hospital and 1-year mortality.
The risk of recurrent in-hospital stroke (2.0 vs. 11%, p = 0.001) and the 1-year mortality rate (30.1% vs. 36.8 %, p = 0.002) were significantly lower when the primary care provider was a cardiologist rather than an internist.
Discussion
Gulf CARE is the first systematic multinational registry of AHF patients in the Middle East. Data on the clinical profile, management, and outcome of HF in this region is very scarce, even though it is highly important to evaluate the magnitude of the problem and to guide management and future plans. Ethnicity may even affect the response to specific therapy, for example, the addition of a fixed-dose combination of hydralazine and isosorbide dinitrate to standard HF therapy offered particular efficacy and significantly lower mortality rate (6.2% vs. 10.2%, p = 0.02) in African Americans cohort with HFrEF10 (AHA guidelines Class I recommendations). Whether this benefit is evident in non-African Americans remains to be investigated.
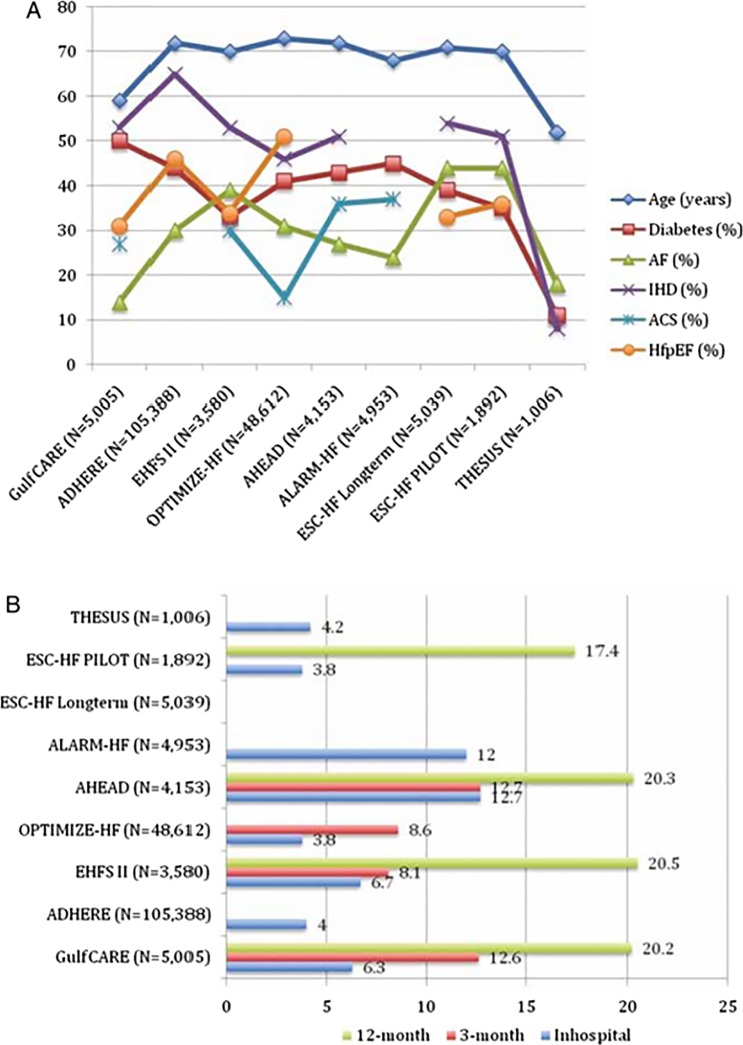
Gulf CARE registry was shortly released after the Heart function Assessment Registry Trial in Saudi Arabia (HEARTS) – the first prospective multicentre survey in the Kingdom of Saudi Arabia – that enrolled 2610 AHF patients and has been published in the European Journal of Heart Failure in 2014. As would be expected and in line with the findings of HEARTS registry, the clinical profile and management of AHF in this region differ from that in Western countries. Patients with AHF from this region are a decade younger (mean age in Gulf CARE: 59 years; HEARTS: 61.4 years) than Western patients (ADHERE: 72.4 years; OPTIMIZE-HF: 73.1 years) with a higher prevalence of DM (Gulf CARE: 50%; HEARTS: 64.1% while ADHERE: 44%, OPTIMIZE-HF: 41%) (Fig. 1). This could be explained by the lower life expectancy and the high prevalence of DM as a consequence of the sedentary unhealthy lifestyle and increased prevalence of visceral obesity in this region. The low prevalence of AF noticed in this registry may be also attributed to the younger age of the patients and low prevalence of valvular heart disease and alcohol consumption. HFrEF accounts for 69% of patients in Gulf CARE and 73% of patients in HEARTS registry which is higher than American registries (ADHERE: 54%, OPTIMIZA-HF: 49%). This could be explained by the high rates of CAD (53% in Gulf CARE, and 55.7% in HEARTS) which is the most prevalent cause of HF.
Figure 1.
(A) Demographic and clinical characteristics of different published heart failure registries. (B) Mortality in the different published heart failure registries. Adapted from Sulaiman et al. Eur. J. Heart Fail. 2015;17(4):374–84.
The 1-year mortality in AHF patients is 20% which is comparable to the mortality rate in HEARTS study and other registries in developed countries (Fig. 1). However, the 1-year re-hospitalization rate of 40% is very high compared with other registries, which may be attributed to the underutilization of coronary intervention and device therapy along with lack of proper outpatient surveillance and management in specialized heart failure clinics.
Heart failure and stroke
HF is associated with a 2 to 3-fold increased risk of ischemic stroke.11 Several mechanisms can link stroke to HF; (1) the high risk of thrombo-embolism related to the occurrence of AF or stasis of blood in dilated hypokinetic cardiac chambers and in peripheral blood vessels, (2) the hypercoagulable state and reduced fibrinolysis due to activation of the sympathetic nervous system and the renin-angiotensin-aldosterone system12, (3) endothelial dysfunction in HF13, (4) hypotension14, (5) underlying risk factors for the development of HF, such as hypertension and DM, can also predispose to atherosclerosis of carotid and cerebral arteries.
Little data exists also regarding the prevalence and outcome of stroke in patients hospitalized for HF. A meta-analysis of the incidence of stroke in patients with chronic HF reported 1.8% risk during the first year after diagnosis of HF with nearly 5% risk at 5 years post-diagnosis.15 In contrast to the low prevalence of prior stroke reported in patients with acute coronary syndrome (ACS) in the Middle East,16 history of stroke in patients hospitalized for AHF in Gulf CARE registry is relatively common (8.1%). Moreover, stroke was identified as an independent predictor for in-hospital and 1-year mortality. Hence, patients with prior stroke should be considered a higher risk group that may benefit from specialized care. The use of anticoagulants and antiplatelets in patients prior stroke is unfortunately very low in this registry during both hospitalization (20% and 29% respectively) and at discharge (22% and 41% respectively), which may explain the high rate of recurrent strokes and mortality. These rates are much lower than has been reported in a EUROASPIRE III survey where the use of antiplatelets or anticoagulants was 87.2%.17
On the other hand, the outcome of those patients is better when they are under care of cardiologists rather than internists. Cardiologists provided more evidence-based therapies, however selection bias may be the reason; patients with lower risk stroke were preferentially admitted under the care of cardiologists rather than internists.
Like other registries, Gulf CARE is an observational study in which unmeasured confounding biases mat exist. In addition, only few hospitals were involved in the registry in some countries; hence, the results might not be generalized.
What have we learned?
Gulf CARE data provides important insights into the clinical characteristics and patterns of care of patients with HF in the Middle East in order to improve patient management and outcomes. The findings highlight the importance of having our own registries and studies, not only depending on international guidelines that may not be suitable in certain circumstances to our different population. This indicates also a need for nationwide primary prevention and HF management programs to increase awareness and to combat this major healthcare problem.
References
- 1.Askoxylakis V, Thieke C, Pleger ST, Most P, Tanner J, Lindel K, Katus HA, Debus J, Bischof M. Long-term survival of cancer patients compared to heart failure and stroke: a systematic review. BMC Cancer. 2010;10:105. doi: 10.1186/1471-2407-10-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. ACCF/AHA Guideline for the Management of Heart Failure. Circulation. 2013;128(16):e240–e327. doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 3.Braunwald E. Heart Failure. JACC Hear. Fail. 2013;1(1):1–20. doi: 10.1016/j.jchf.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, RW, Turner MB. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 5.Adams KF, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Berkowitz RL, Galvao M, Horton DP. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE) Am. Heart J. 2005;149(2):209–216. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. J. Am. Coll. Cardiol. 2006;47(1):76–84. doi: 10.1016/j.jacc.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 7.Fonarow GC, Abraham WT, Albert NM, Gattis WA, Gheorghiade M, Greenberg B, O'Connor CM, Yancy CW, Young J. Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF): rationale and design. Am. Heart J. 2004;148(1):43–51. doi: 10.1016/j.ahj.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Sulaiman K, Panduranga P, Al-Zakwani I, Alsheikh-Ali AA, AlHabib KF, Al-Suwaidi J, Al-Mahmeed W, AlFaleh H, Elasfar A, Al-Motarreb A, Ridha M, Bulbanat B, Al-Jarallah M, Bazargani N, Asaad N, Amin H. Clinical characteristics, management, and outcomes of acute heart failure patients: observations from the Gulf acute heart failure registry (Gulf CARE) Eur. J. Heart Fail. 2015;17(4):374–384. doi: 10.1002/ejhf.245. [DOI] [PubMed] [Google Scholar]
- 9.Khafaji H, a R, Sulaiman K, Singh R, AlHabib KF, Asaad N, Alsheikh-Ali A, Al-Jarallah M, Bulbanat B, AlMahmeed W, Ridha M, Bazargani N, Amin H, Al-Motarreb A, AlFaleh H, Elasfar A, Panduranga P, Al Suwaidi J. Clinical characteristics, precipitating factors, management and outcome of patients with prior stroke hospitalised with heart failure: an observational report from the Middle East. BMJ. 2015;5(4):e007148. doi: 10.1136/bmjopen-2014-007148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor AL, Ziesche S, Yancy C, Carson P, D'Agostino R, Ferdinand K, Taylor M, Adams K, Sabolinski M, Worcel M, Cohn JN. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N. Engl. J. Med. 2004;351(20):2049–2057. doi: 10.1056/NEJMoa042934. [DOI] [PubMed] [Google Scholar]
- 11.Häusler KG, Laufs U, Endres M. Neurological aspects of chronic heart failure. Nervenarzt. 2011;82(6):733–742. doi: 10.1007/s00115-010-3093-6. [DOI] [PubMed] [Google Scholar]
- 12.Jug B, Vene N, Salobir BG, Sebestjen M, Sabovic M, Keber I. Procoagulant state in heart failure with preserved left ventricular ejection fraction. Int. Heart J. 2009;50(5):591–600. doi: 10.1536/ihj.50.591. [DOI] [PubMed] [Google Scholar]
- 13.Georgiadis D, Sievert M, Cencetti S, Uhlmann F, Krivokuca M, Zierz S, Werdan K. Cerebrovascular reactivity is impaired in patients with cardiac failure. Eur. Heart J. 2000;21(5):407–413. doi: 10.1053/euhj.1999.1742. [DOI] [PubMed] [Google Scholar]
- 14.Pullicino PM, McClure LA, Wadley VG. Blood pressure and stroke in heart failure in the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Stroke. 2009;40(12):3706–3710. doi: 10.1161/STROKEAHA.109.561670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Witt BJ, Gami AS, Ballman KV, Brown RD, Meverden RA, Jacobsen SJ, Roger VL. The incidence of ischemic stroke in chronic heart failure: a meta-analysis. J. Card. Fail. 2007;13(6):489–496. doi: 10.1016/j.cardfail.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 16.Albaker O, Zubaid M, Alsheikh-Ali AA, Rashed W, Alanbaei M, Almahmeed W, Al-Shereiqi SZ, Sulaiman K, Al Qahtani A, Al Suwaidi J. Early stroke following acute myocardial infarction: incidence, predictors and outcome in six Middle-Eastern countries. Cerebrovasc. Dis. 2011;32(5):471–482. doi: 10.1159/000330344. [DOI] [PubMed] [Google Scholar]
- 17.Heuschmann PU, Kircher J, Nowe T, Dittrich R, Reiner Z, Cifkova R, Malojcic B, Mayer O, Bruthans J, Wloch-Kopec D, Prugger C, Heidrich J, Keil U. Control of main risk factors after ischaemic stroke across Europe: data from the stroke-specific module of the EUROASPIRE III survey. Eur. J. Prev. Cardiol. 2014 doi: 10.1177/2047487314546825. doi: 10.1177/2047487314546825. [DOI] [PubMed] [Google Scholar]