Abstract
Purpose
Visual performance following toric intraocular lens implantation for cataract with moderate and severe astigmatism.
Setting
Cataract services, Shroff Eye Centre, New Delhi, India.
Design
Case series.
Method
This prospective study included 64 eyes of 40 patients with more than 1.50 dioptre (D) of pre-existing corneal astigmatism undergoing phacoemulsification with implantation of the AcrySof® toric IntraOcular Lens (IOL). The unaided visual acuity (UCVA), best corrected visual acuity (BCVA), residual refractive sphere and refractive cylinders were evaluated. Toric IOL axis and alignment error was measured by slit lamp method and Adobe Photoshop (version 7) method. Patient satisfaction was evaluated using a satisfaction questionnaire at 3 months.
Results
The mean residual refractive astigmatism was 0.57 D at the final follow-up of 3 months. Mean alignment error was 3.44 degrees (SD = 2.60) by slit lamp method and 3.88 degrees (SD = 2.86) by Photoshop method. Forty-six (71.9%) eyes showed misalignment of 5 degrees or less, and 60 (93.8%) eyes showed misalignment of 10 degrees or less. The mean log MAR UCVA at 1st post-op day was 0.172 (SD = 0.02), on 7th post-op day was 0.138 (SD = 0.11), and on 30th post-op day was 0.081 (SD = 0.11). The mean log MAR BCVA at three months was −0.04 (SD = 0.76).
Conclusion
We believe that implantation of AcrySof® toric IOL is an effective, safe and predictable method to correct high amounts of corneal astigmatism during cataract surgery.
Keywords: Toric IOL, Moderate and severe astigmatism
Introduction
Refractive errors, especially uncorrected ones, are among the most common causes of visual impairment in the world; the World Health Organization estimates this population to be around 153 million.1 Also, it has been estimated that 15–29% of patients with cataract have more than 1.5 dioptres (D) of pre-existing astigmatism.2, 3
Apart from correcting corneal astigmatism with spectacles and contact lenses, treatment options include excimer laser refractive procedures such as photorefractive keratectomy, laser in situ keratomileusis, and laser-assisted subepithelial keratomileusis; astigmatic keratotomy using limbal or corneal relaxing incisions; opposite clear corneal incisions (OCCI); and toric IOL.4 But the potential complications of incisional keratotomy have been the limitations.5 Surgeons considering OCCI have to take into account factors such as age, magnitude, and the depth and length of the incisions.6
In the recent years, two major developments in cataract surgery have contributed to a significant improvement in visual outcomes. One is the shift to smaller incisions and the other, management of corneal astigmatism, intraoperatively using toric IOLs.
The evolution of cataract surgery techniques and advancements in IOLs have blurred the line between refractive and cataract surgery. Improved technologies as well as patients’ higher expectations have heightened the importance of treating postoperative residual refractive error, which can be the cause of increased night vision complaints. This in addition to accurate intraocular lens (IOL) power calculations, has led to cataract surgery now being commonly referred to as refractive cataract surgery. It is seen that the implantation of toric IOL at the time of cataract removal is a predictable, single step procedure to minimize residual refractive error.4
The Acrysof® toric IOL is one of the most commonly used toric IOLs in cataract surgery.
It is a 13.0 mm single piece foldable modified-L haptic injectable lens with a 6.0 mm optic and natural blue-light filtering technology. These are made of hydrophobic acrylic material, with stable force haptic design for rotational stability. The superior rotational stability is directly related to the haptic design in which the knee of the haptic absorbs the entire force of the capsular bag as it contracts. It is designed with 3 reference dots on each side that mark the axis of the cylinder on the posterior surface. Intraocular lens spherical power is available from +6.00 to +30.00 D. This IOL has shown to be effective in reducing relative astigmatism and providing good uncorrected visual outcomes and spectacle independence for distance vision.
In our series, we determine the efficacy and alignment error of Acrysof® toric IOL for correcting pre-existing corneal astigmatism in cataract patients in Indian population. The IOL models used were the SN60T series namely T4, T5, T6, T7, T8, and T9 which correct 1.03 D, 1.55 D, 2.06 D, 3.08 D, 3.60 D, and 4.11 D respectively at the corneal plane.
Patients and methods
Study design and patient population
This prospective study comprised of 64 eyes of 40 patients with moderate and severe corneal astigmatism presenting to the outpatient department of Shroff Eye Centre, New Delhi, from October 2011 to June 2012. The study was registered with the institutional review board and an approval was obtained from the ethics committee. The ethics committee comprised of Head of Department, Cataract and IOL services, Director of Shroff Eye Centre and Academic Director, Shroff Eye Centre. All these cases underwent a conventional phacoemulsification under peribulbar anaesthesia with implantation of Alcon AcrySof® toric intraocular lens by a single surgeon, NMS. Patients with regular corneal astigmatism more than 1.5 D, pre-senile and senile cataract were included. Patients with any previous intra-ocular surgery, abnormal iris or pupil deformation, macular degeneration or retinopathy, severe dry eyes, and irregular astigmatism were excluded.
Preoperative assessment
A detailed history was taken to exclude any ocular pathology. All patients underwent preoperative ocular examination including Slit Lamp Examination, intraocular pressure measurement (by Nidek, NT4000 Auto Non Contact Tonometer), keratometry (using IOLMaster), Axial length measurement (using IOLMaster), IOL power (calculation using 3rd or 4th generation formula (wherever applicable)), Schirmer’s test (using Schirmer strips No. 41 Whatmann filter paper), Specular Microscopy (using SP 3000P specular microscope), and fundus examination (by Indirect Ophthalmoscopy). Toric IOL model, alignment axis and anticipated residual astigmatism were calculated using web-based toric IOL calculator program available at http://www.acrysoftoriccalculator.com. Patient was counselled regarding the procedure along with a formal written consent; the possible need for spectacles after the procedure is that the results may not be 100% and small degree of residual cylinder may occur.
Prior to surgery, the eye was anesthetized with 0.5% proparacaine drops. The patient was seated in the upright position and made to fixate at a distance target. A bubble marker (ASICO AE-2791TBL) was used for marking the reference marks for identifying the 3-, 6- and 9-o’clock positions on the limbus (Fig. 1(a)). The patient was made to sit while applying the reference marks to compensate for the possible cyclotorsion which may occur on lying supine. When the bubble was in between the two vertical lines, it indicated that the 3- and 9-wedges of the marker were truly horizontal (Fig. 1(a)). A special Gentian Violet pen was used to ink the wedges. This pen stood up to the pre-operative prepping, was flexible, smudges proof and was packed individually in sterile peel pouch. The marker was gradually advanced towards the eye while the examiner ensured the bubble was in the central position when the wedges make contact with the limbus.
Figure 1.

(a) Bubble marker (ASICO AE-2791TBL) being used with the patient in upright Seated position and (b) reference marks at 0°, 90° and 180°.
Surgical technique
Intra-operatively, a temporal limbal incision (2.75 mm) was made. A 5.5 mm capsulorhexis with 360° peripheral coverage of the IOL optic was performed so as to achieve “shrink wrap” effect which maintains good long term IOL centration. This was followed by cortical cleavage hydrodissection and nuclear rotation. Nucleotomy was performed using a “Stop and Chop” phacoemulsification technique followed by cortical clean-up. The Alcon AcrySof® toric IOL was implanted with an injector system, and rotated appropriately to align the reference marks on the IOL surface with the corneal marks. Careful attention was given to correct axis positioning of the IOL at the time of surgery and meticulous removal of residual viscoelastic material after IOL insertion was done to reduce the possibility of misalignment. The incision was adequately hydrated to ensure closure.
Postoperatively, the patients were followed up in the outpatient department at Shroff Eye Centre on postoperative days 1, 7, 30 and 90.
The following parameters were assessed:
-
(1)
Unaided visual acuity (UCVA) at days 1, 7, 30 and best corrected visual acuity (BCVA) at days 30 and 90 were assessed by a single observer, JF.
-
(2)
Slit lamp examination on all postoperative visits to check anterior chamber reaction by Hogan’s criteria, was assessed by a single observer, JF.
-
(3)
The achieved IOL alignment at 3 months was analysed by aligning the slit beam of the slit lamp with the marks denoting the axis of the IOL after pupillary dilation, and was performed by single masked observer, AK (Fig. 2(a)). In addition, slit lamp photographs were analysed using tools in Adobe Photoshop (version 7.0) and were taken by a single masked observer, RD. The amount of alignment error of each eye was calculated. A pre-operative photograph with the reference marks was imported in the Adobe Photoshop. Using the “Single Row Marquee Tool” a straight line was placed on the image adjacent to the limbal reference marks. Using the “Transform Tool”, straight line was rotated in such a manner so as to align through the reference marks on the limbus. The amount of rotation (clockwise or anticlockwise) was noted from the “Set Rotation” dialogue box (Fig. 2(b)). The amount of alignment error (in degrees) induced was noted by both slit-lamp method and Photoshop method.
-
(4)
Patient satisfaction was evaluated by a questionnaire at the 3 month follow-up was documented by a single observer, JF.
Figure 2.
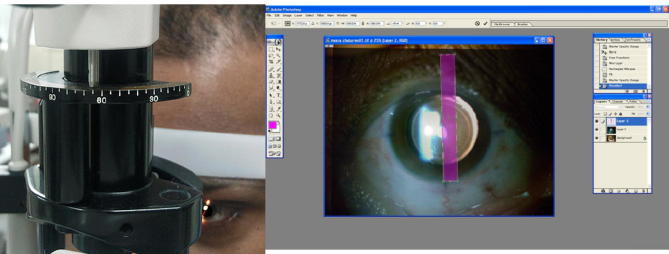
(a) Achieved IOL alignment at 3 months being analysed by aligning the slit-LAMP BEAM with the IOL Marks after pupillary dilation. (b) Straight edge of a transparent rectangle aligned with the marks denoting the IOL plus axis.
Statistical analysis
Data analysis was done using descriptive analysis and frequency distribution to analyse age, sex, eye distribution, type of cataract preoperatively, most common model of toric intraocular lens implanted, anterior chamber reaction postoperatively and contrast sensitivity.
Paired t test and Pearson correlation were used to correlate between corneal cylinder before and after toric Intraocular Lens implantation.
Wilcoxon sign rank test and Paired t test were also applied to find change in uncorrected visual acuity on days 1, 7 and 30 and also change in preoperative best corrected visual acuity with that on days 30 and 90.
Statistical analysis was performed using SPSS for Windows software (version 15.0, SPSS, Inc.). The level of statistical significance was a P value less than .05.
Results
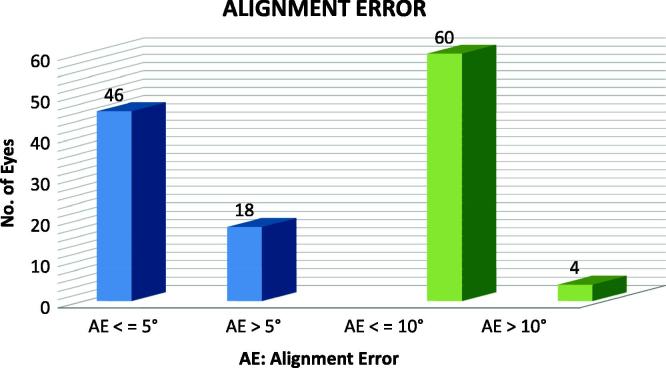
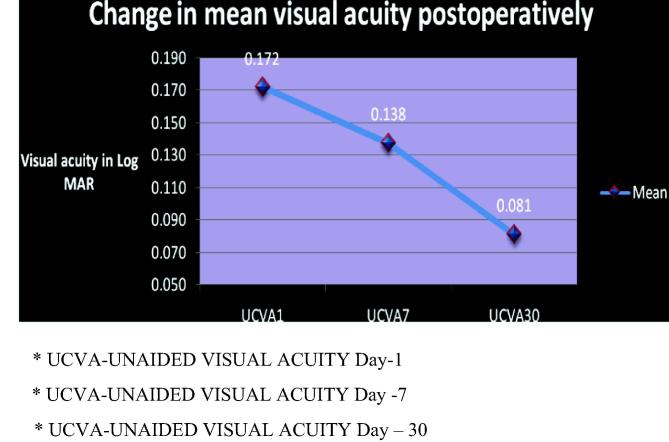
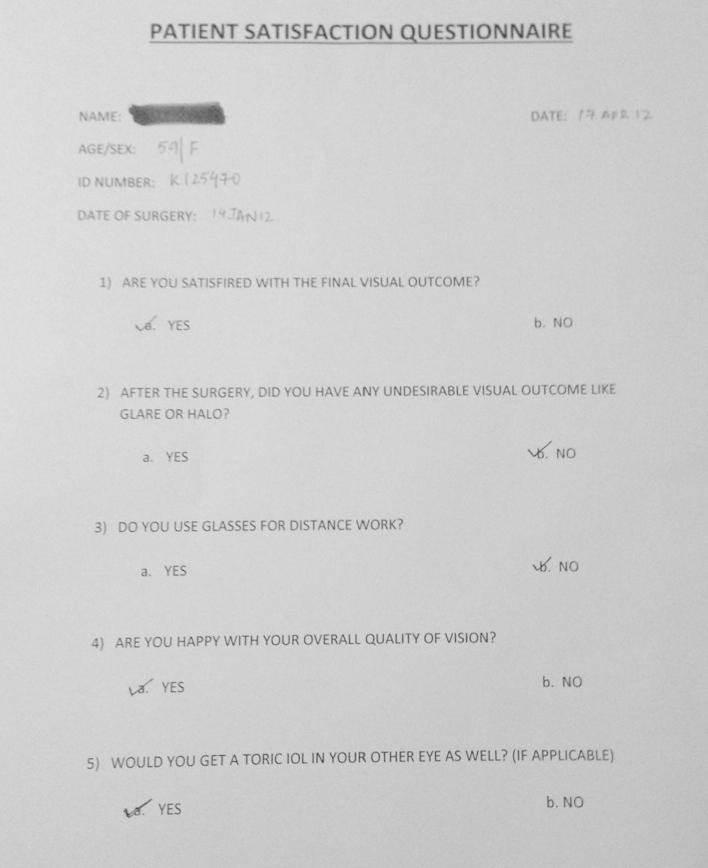
The mean age in our study was 64.09 years (SD = 11.688), with maximum number of patients being in age group of 55 years or younger (27.5%, n = 11). Four out of these patients were having pre-senile cataracts. In our study we had 60% of males (n = 24) and 40% of females (n = 16). The mean axial length in our study was 23.97 mm (SD = 0.91) (Table 1). The maximum number of toric IOLs was used in T4 model which was implanted in 22 eyes (34.38%) followed by T5 model in 18 eyes (28%) (Table 2). The mean preoperative cylinder was found to be 2.5403 (SD = 0.9046) whereas mean postoperative absolute final cylinder was reported as 0.5703 (SD = 0.28). This change was found to be statistically significant using Paired t test (p = 0.00) (Table 3). The mean postoperative alignment error was found to be 3.43 degrees (SD = 2.6) on slit lamp examination while it was calculated to be 3.87 degrees (SD = 2.8) on Adobe Photoshop in our study group (Fig. 3). In our study, 46 (71.9%) eyes showed misalignment of 5 degrees or less, and 60 (93.8%) eyes showed misalignment of 10 degrees or less (Fig. 4). Four patients had misalignment of more than 10 degrees, two had UCVA of 20/30 at 1 month and BCVA of 20/25 at end of 3 months with −0.75 D. The other two patients had UCVA of 20/25 at 1 month and BCVA of 20/20 at end of 3 months with −1.25 D. The mean log MAR visual acuity (unaided) on first postoperative day was 0.172, which showed a sloping trend to 0.138 at Day 7 and then 0.081 at Day 30. The difference in log MAR visual acuity between the three groups is statistically significant with p < 0.05 in all three groups, namely UCVA day 1, UCVA day 2, and UCVA day 3 (Fig. 5). The difference in mean visual acuity of pre-op best corrected visual acuity and best corrected acuity at Day 30 and Day 90 was analysed in our study. Also, difference in BCVA Day 30 and Pre-op BCVA (p = 0.00), difference in BCVA Day 90 and Day 30 (p = 0.02), and difference in BCVA Day 90 and Pre-op BCVA (p = 0.00) were found to be statistically significant (Table 4). Patient satisfaction questionnaire showed that 34 patients (85%) were satisfied with their UCVA. Thirty-six patients (90%) did not complain of any undesirable visual phenomenon such as glare or haloes. Six patients (15%) were prescribed correction for distance vision. All patients (100%) were happy with the quality of vision.
Table 1.
Preoperative patient demographic data.
| Characteristics | Values |
|---|---|
| Eyes | 64 |
| Patients | 40 |
| Mean age | 64.09 (SD = 11.69) |
| Sex (Male/Female) | 24/16 |
| Average corneal cylinder (pre-op) | 44.19 (SD = 0.27) |
| Mean axial length | 23.97 mm (SD = 0.17) |
| Mean intraocular pressure | 15.6 mmHg (SD = 2.6) |
| Specular microscopy count | 2401.78 cells/mm2 |
| Schirmer’s test | 12.47 mm (SD = 5.55) |
| Intraocular lens power | 19.30 D (SD = 2.45) |
Table 2.
Models of toric IOLS used.
| Model | N = No. of eyes | Percentage (%) |
|---|---|---|
| T4 | 22 | 34.38 |
| T5 | 18 | 28.13 |
| T6 | 12 | 18.75 |
| T7 | 4 | 6.25 |
| T8 | 4 | 6.25 |
| T9 | 4 | 6.25 |
Table 3.
Mean pre-operative cylinder and absolute postoperative cylinder.
| Mean | N = No. of eyes | Std. deviation | |
|---|---|---|---|
| K cylinder | 2.5403 | 64 | .9046 |
| Absolute final cylinder | .5703 | 64 | .2856 |
Figure 3.
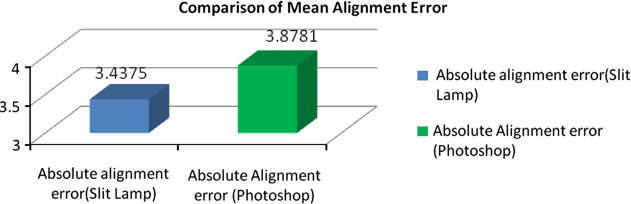
Mean postoperative alignment error slit lamp versus Adobe Photoshop.
Figure 4.
Alignment error of ⩽5° and ⩽10° and number of eyes in each group.
Figure 5.
Change in unaided visual acuity (UCVA) on days 1, 7, and 30.
Table 4.
Best corrected visual acuity-pre-operative period, at day 30 and day 90.
BCVA_pre – best corrected visual acuity pre-operative.
BCVA30 – best corrected visual acuity day – 30.
BCVA90 – best corrected visual acuity day – 90.
Discussion
Accurate positioning of a toric IOL is the most important factor determining the efficacy of the astigmatism correction.7 Although precise axis alignment is critical to good outcomes of toric IOL implantation, misalignment of toric IOLs remains a major barrier to the optimization of postoperative results.8
In our prospective study, we have studied the visual performance following toric IOL implantation for cataract with moderate and severe corneal astigmatism in 64 eyes of 40 patients with pre-senile and senile cataract. The mean residual refractive astigmatism was 0.57 D (SD = 0.29 D) at the final follow-up, which was at 3 months. This was similar to the study done by Bauer et al. where the residual refractive astigmatism was less than 0.75 D in 74% of the eyes and less than 1.00 D in 91% of the eyes.4 Also, the mean postoperative cylinder was 0.92 D with STAAR AA4203 toric IOL and 0.53 D with AcrySof® SN60T toric IOL, in a comparative study done by Chang in the USA.5 A study by Ruhswurm et al. showed that the mean astigmatism was reduced to 0.84 D.9 The residual refractive cylinder was less than 0.75 D in 62% of the eyes and less than 1.00 D in 81% of the eyes.10 Other studies have also shown similar results. A study done in Australia had a mean postoperative cylinder of 0.81 (SD = 0.59).7
The visual improvement after toric IOL implantation in our study was comparable to other studies. Uncorrected visual acuity (UCVA) was checked on 1st, 7th and 30th postoperative day. The mean log MAR UCVA at 1st post-op day was 0.172 (SD = 0.02), on 7th post-op day was 0.138 (SD = 0.11), and on 30th pos-op day was 0.081 (SD = 0.11).
Application of paired t test indicated that implantation of a toric intraocular lens elicited a statistically significant change in uncorrected visual acuity on Day 7 compared with Day 1 (baseline) as t (31) = 2.775, p = 0.009.
A statistically significant difference in visual acuity is also elicited on Day 30 compared with Day 7 as t (31) = 4.447, p = 0.00.
Similarly, a statistically significant difference in uncorrected visual acuity is observed on Day 30 compared with Day 1 as t (31) = 4.473, p = 0.00.
These results confirm the importance of implanting AcrySof® toric IOL as an effective and safe method to correct high amounts of corneal astigmatism during cataract surgery.
In our study, we found a mean alignment error of 3.44 degrees (SD = 2.60) by slit lamp method and 3.88 degrees (SD = 2.86) by Photoshop method.
Also, we found that 46 (71.9%) eyes showed misalignment of 5 degrees or less, and 60 (93.8%) eyes showed misalignment of 10 degrees or less. Sixty-four (100%) eyes showed misalignment of 15 degrees or less.
Initially the U.S. Food and Drug Administration (FDA) trial results showed a mean misalignment of less than 4 degrees.11 These results were correlating with other studies done around the world. In one study done in Spain, mean toric IOL axis rotation was 3.63 degrees (SD 3.11).12 Another study done in Australia showed mean IOL misalignment by slit lamp to be 2.55 degrees (SD = 2.76) by slit lamp method and 2.65 degrees (SD = 1.98) by internal map method.7
A likely reason for the improved rotational stability of the AcrySof® toric IOL is the stronger tendency for its hydrophobic acrylic material to adhere to the capsule. This ‘tackiness’ is in contrast to the slippery surface of a plate-haptic silicone IOL, which has shown to be far less adherent to the posterior capsule in animal studies.13 Additional clinical advantages of the AcrySof® toric IOL are its more popular single-piece acrylic design and the presence of a truncated posterior edge.14
The mean log MAR BCVA at one month was −0.02 (SD = 0.08) and at three months was −0.04 (SD = 0.76). In the study by Mendicute et al., all eyes achieved 0.1 BCVA or better.12 The mean BCVA of the study by Visser et al. was 0.81 (SD = 0.21)10 and by Carey et al. was −0.01 (SD = 0.12).7 Chang in his comparative study found BCVA of >0.3 in 92% of STAAR toric IOLs and 94% of AcrySof® toric IOLs.5
At the end of our study, patient satisfaction was assessed using Patient Satisfaction Questionnaire (Fig. 6). The questionnaire consisted of a set of 5 closed ended questions, which were given to the patients on their last visit. The questionnaire was formed to understand the satisfaction level of the patients after the surgery. All patients were happy with the overall quality of their vision. No redialing of the IOL was required in any of the patient.
Figure 6.
Patient satisfaction questionnaire.
Conclusion
We believe that the implantation of an AcrySof® toric IOL is an effective, safe and predictable method to correct high amounts of corneal astigmatism during cataract surgery. No undesirable visual phenomenon such as glare or haloes was noted in the study group. Slight residual refractive error was well tolerated by the patients. Careful attention to correct axis positioning of the IOL at the time of surgery and meticulous removal of residual viscoelastic material after IOL insertion will help reduce rate of rotation. In the end, the key to accurate results lies in proper patient selection, accurate biometry and right surgical technique.
Conflict of interest
The authors declared that there is no conflict of interest.
Financial disclosure
No author has a financial or proprietary interest in any material or method mentioned.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.World Health Organization Fact file. Blindness and Visual Impairment. <http://www.who.int/features/factfiles/vision/02_en.html> [accessed 11.10.09].
- 2.Hoffer K.J. Biometry of 7500 cataractous eyes. Am J Ophthalmol. 1980;90:360–368. doi: 10.1016/s0002-9394(14)74917-7. [DOI] [PubMed] [Google Scholar]
- 3.Ninn-Pedersen K., Stenevi U., Ehinger B. Cataract patients in a defined Swedish population 1986–1990. II. Preoperative observations. Acta Ophthalmol (Copenh) 1994;72:10–15. doi: 10.1111/j.1755-3768.1994.tb02729.x. [DOI] [PubMed] [Google Scholar]
- 4.Bauer N.J.C., de Vries N., Webers C.A.B., Hendrikse F., Nuijts R.M.M.A. Astigmatism management in cataract surgery with the Acrysof toric intraocular lens. J Cataract Refract Surg. 2008;34:1483–1488. doi: 10.1016/j.jcrs.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 5.Chang D.F. Comparative rotational stability of single-piece open-loop acrylic and plate-haptic silicone toric intraocular lens. J Cataract Surg. 2008;34:1842–1847. doi: 10.1016/j.jcrs.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 6.Mendicute J., Irigoyen C., Ruiz M., Illarramendi I., Ferrer-Blasco T., Montés-Micó R. Toric intraocular lens versus opposite clear corneal incisions to correct astigmatism in eyes having cataract surgery. J Cataract Refract Surg. 2009;35:451–458. doi: 10.1016/j.jcrs.2008.11.043. [DOI] [PubMed] [Google Scholar]
- 7.Carey P.J., Leccisotti A., McGilligan V.E., Goodall E.A., Moore C.B.T. Assessment of toric intraocular lens alignment by a refractive power/corneal analyser system and slitlamp observation. J Cataract Refract Surg. 2010;36:222–229. doi: 10.1016/j.jcrs.2009.08.033. [DOI] [PubMed] [Google Scholar]
- 8.Jin H., Limberger I.J., Ehmer A., Guo H., Auffarth G.U. Impact of axis misalignment of toric intraocular lenses on refractive outcomes after cataract surgery. J Cataract Refract Surg. 2010;36:2061–2072. doi: 10.1016/j.jcrs.2010.06.066. [DOI] [PubMed] [Google Scholar]
- 9.Ruhswurm I., Scholz U., Zehetmayer H., Hanselmayer G., Vass C., Skorpik C. Astigmatism correction with a foldable toric intraocular lens in cataract patients. J Cataract Refract Surg. 2000;26:1022–1027. doi: 10.1016/s0886-3350(00)00317-5. [DOI] [PubMed] [Google Scholar]
- 10.Visser N., Ruíz-Mesa R., Pastor F., Bauer N.J.C., Nuijts R.M.M.A., Monté-Micó R. Cataract surgery with toric intraocular lens implantation in patients with high corneal astigmatism. J Cataract Refract Surg. 2011;37:1403–1410. doi: 10.1016/j.jcrs.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 11.Horn J.D. Status of toric intraocular lenses. Curr Opin Ophthalmol. 2007;18:58–61. doi: 10.1097/ICU.0b013e328011f9bf. [DOI] [PubMed] [Google Scholar]
- 12.Mendicute J., Irigoyen C., Aramberri J., Onadarra A., Montes-Mico R. Foldable toric intraocular lens for astigmatism correction in cataract patients. J Cataract Refract Surg. 2008;34(4):601–607. doi: 10.1016/j.jcrs.2007.11.033. [DOI] [PubMed] [Google Scholar]
- 13.Oshika T., Nagata T., Ishii Y. Adhesion of lens capsule to intraocular lenses of polymethylmethacrylate, silicone, and acrylic foldable materials: an experimental study. Br J Ophthalmol. 1998;82:549–553. doi: 10.1136/bjo.82.5.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang D.F. Single versus three piece acrylic IOL [editorial] Br J Ophthalmol. 2004;88:727–728. doi: 10.1136/bjo.2004.040063. [DOI] [PMC free article] [PubMed] [Google Scholar]