Abstract
Background
Gender differences may exist in the symptom experience of patients with gastro-oesophageal reflux disease (GERD) who have a partial response to proton pump inhibitors (PPIs).
Objective
The purpose of this study was to analyse gender differences in partial responders to PPIs.
Methods
Patients with GERD who responded partially to PPIs (n = 580; NCT00703534) completed the Reflux Symptom Questionnaire 7-day recall (RESQ-7) and the Gastrointestinal Symptom Rating Scale (GSRS). Anxiety and depression were evaluated using the Hospital Anxiety and Depression Scale.
Results
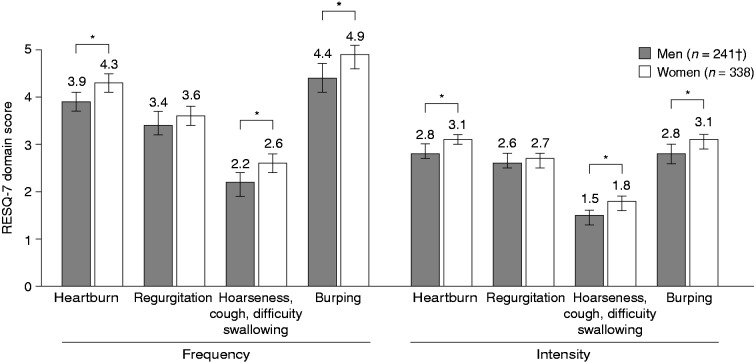
Women had significantly higher RESQ-7 domain scores than men for Heartburn (frequency: 4.3 vs 3.9; intensity: 3.1 vs 2.8), Burping (frequency: 4.9 vs 4.4; intensity: 3.1 vs 2.8) and Hoarseness, cough and difficulty swallowing (frequency: 2.6 vs 2.2; intensity: 1.8 vs 1.5), and had higher GSRS domain discomfort scores than men for Abdominal pain (3.51 vs 3.23), Indigestion (3.80 vs 3.45) and Constipation (2.69 vs 2.17) (all p < 0.05). Anxiety and depression were significantly more prevalent in women than in men.
Conclusion
In this population of partial responders, women had more frequent/intense heartburn and extra-oesophageal symptoms and more discomfort from abdominal pain, indigestion and constipation than men. Comorbid anxiety and depression may contribute to the increased symptom burden in women.
Keywords: Abdominal pain, extra-oesophageal symptoms, gender differences, gastro-oesophageal reflux disease, heartburn
Introduction
The cardinal symptoms of gastro-oesophageal reflux disease (GERD) are heartburn and regurgitation. Most individuals with GERD experience resolution of their reflux symptoms when on proton pump inhibitor (PPI) therapy, but partial response to PPI therapy is a growing problem in clinical practice.1
Some studies have suggested that there may be gender differences in the prevalence of partial response to PPIs.1–4 In a study conducted in patients newly diagnosed with GERD in primary care, partial symptomatic response to PPI therapy – identified using treatment change as a proxy – was associated with female gender (odds ratio (OR) 1.20; 95% confidence interval (CI): 1.05–1.37).2 In another study, conducted in patients with reflux oesophagitis and frequent heartburn, men were more likely than women to achieve heartburn resolution (OR 1.35; 95% CI: 1.14–1.59; p < 0.001).5 In an evaluation of four clinical trials including patients with GERD, the proportion of women with a partial symptomatic response to PPI therapy was higher than that in men, both in patients with and in those without reflux oesophagitis.4 Poorer treatment response was also associated with female gender in an open-label study of PPI therapy in patients with symptoms suggestive of GERD.3
Comorbid functional bowel disorders and psychological disorders add to the symptom burden in patients with GERD and have also been implicated in an impaired symptomatic response to PPI treatment.6–9 Irritable bowel syndrome (IBS), anxiety and depression are common comorbidities in the general population with GERD.10–13 The reported prevalence of IBS in some studies is as high as 35% in patients with GERD;13 the reported prevalence of anxiety in patients with GERD ranges from 25% to 32% and that of depression from 8% to 13%.10–12 In the general population, IBS, anxiety and depression are more common in women than in men.14,15
Partial PPI responders have similar upper gastrointestinal symptom patterns to patients with GERD who are not on PPI therapy, although partial responders experience more discomfort and, by definition, a poor response to PPIs.16 However, limited data exist on gender differences in the symptom experience of patients with GERD who have a partial response to PPI therapy. In addition, little is known about the prevalence in this population of functional disorders, anxiety and depression, which could contribute to the persistence of symptoms in men and women who are partial responders. The aim of this post hoc analysis was to determine whether symptom differences exist between men and women with a partial response to PPI therapy for GERD and to determine the roles of anxiety, depression and concomitant IBS.
Methods
Patients
Symptom reporting at enrolment was evaluated in partial responders to PPIs who took part in the Patient Reported Outcome (PRO) Validation Study (NCT00703534).17 Patients were eligible for inclusion if they had a history of GERD symptoms for at least six months and had received at least four weeks of individually optimised PPI therapy within the approved dose range for any GERD indication. Participants also needed to have a partial symptomatic response to PPI therapy, which was defined as persistent GERD symptoms (burning feeling behind the breastbone and/or unpleasant movement of material upwards from the stomach) of at least mild intensity on at least three days in the seven days before enrolment despite using a PPI. Patients whose symptoms had not improved at all on PPI therapy (i.e. non-responders) were excluded from the study. Individuals receiving twice-daily doses of PPI and those using prokinetic drugs were also excluded.
Participants were asked to complete the Reflux Symptom Questionnaire 7-day recall (RESQ-7), the Gastrointestinal Symptom Rating Scale (GSRS) and the Hospital Anxiety and Depression Scale (HADS) at enrolment.
Symptom measures
RESQ-7
The RESQ-7 is a PRO instrument with a one-week recall period that assesses symptom frequency and intensity. The RESQ-7 was validated in the current study sample for use in patients with GERD with a partial response to PPI therapy.18 The instrument consists of 13 items grouped into four domains: Heartburn (burning feeling behind the breastbone; pain behind the breastbone; heartburn; burning feeling in the centre of the upper stomach; pain in the centre of the upper stomach); Regurgitation (acid taste in the mouth; bitter taste in the mouth; unpleasant movement of material upwards from the stomach; stomach contents (liquid or food) moving upwards towards your throat or mouth); Hoarseness, cough and difficulty swallowing; and Burping.18 Symptom frequency is scored as the number of days during the previous seven days that each symptom is experienced (0, 1, 2, 3–4, 5–6 or daily). Symptom intensity is rated on a six-point scale, from 0 (did not have) to 5 (severe).
GSRS
The GSRS is a PRO instrument with a one-week recall. The scale assesses symptom severity using a seven-grade Likert scale, ranging from 1 (no discomfort at all) to 7 (very severe discomfort).19 The instrument consists of 15 items that are clustered into five domains: Reflux (heartburn; regurgitation); Abdominal pain (abdominal pain; hunger pains; nausea); Indigestion (rumbling; feeling bloated; burping; passing gas); Diarrhoea (diarrhoea; loose stools; urgent need for bowel movement); and Constipation (constipation; hard stools; feeling of incomplete bowel movement).
IBS criteria
IBS was assessed by the investigators using pre-specified questions based on the Rome II and Rome III diagnostic criteria for functional gastrointestinal disorders.20
Anxiety and depression
Anxiety and depression were evaluated using the HADS. The HADS is a 14-item PRO instrument comprising two seven-item subscales with a maximum possible score of 21. Scores lower than 8 were taken as indicating no disorder, scores of 8–10 as indicating a possible disorder, and scores of 11–21 as indicating a probable disorder.21
Ethical considerations
The study was performed in accordance with the Declaration of Helsinki and the International Conference on Harmonisation Good Clinical Practice guide. The study protocol was approved by a local or central Institutional Review Board before patient enrolment. All patients had to give their written informed consent before participation. All authors had access to the study data, and reviewed and approved the final manuscript.
Statistical analyses
Gender differences in patient demographics were assessed using the χ2 test with Yates’ correction. The non-parametric Wilcoxon test was used to analyse gender differences in mean domain frequency and intensity scores of the RESQ-7 and in mean domain discomfort scores of the GSRS. Adjustment for Rome III IBS criteria (yes/no) was performed using the stratified Wilcoxon test. Adjustment for Rome III IBS criteria (yes/no), and HADS anxiety and depression scores was performed using analysis of covariance.
Results
Patient demographics and PPI use
Data from all enrolled, eligible patients (n = 580) were included in the analysis. Demographic characteristics are summarised in Table 1, overall and separately by gender. The study population included more women than men. The proportion of patients with a history of reflux oesophagitis was significantly higher in men than in women. In contrast, a significantly higher proportion of women than men was on antidepressive medication.
Table 1.
Demographic characteristics of enrolled, eligible patients, overall and separately by gender
| Characteristic | Patients, n = 580 | Men, n = 242 (41.7%) | Women, n = 338 (58.3%) | p-valuea |
|---|---|---|---|---|
| Age, years | 48.2 (11.5) | 45.5 (11.6) | 50.0 (11.0) | NS |
| BMI, kg/m2 | 28.6 (3.8) | 28.7 (3.6) | 28.5 (4.2) | NS |
| History of reflux symptoms, years | 8.9 (8.1) | 8.8 (7.9) | 9.1 (8.2) | NS |
| History of reflux oesophagitis, n (%)b | ||||
| Yes | 97 (16.7) | 59 (24.4) | 38 (11.2) | <0.001 |
| No | 480 (82.8) | 180 (74.4) | 300 (88.8) | |
| History of hiatal hernia, n (%)b | ||||
| Yes | 144 (24.8) | 54 (22.3) | 90 (26.6) | NS |
| No | 184 (31.7) | 82 (33.9) | 102 (30.2) | |
| Use of antidepressant and anti-anxiety medications, n (%) | ||||
| Neuroleptics (NO5Ac) | 8 (1.4) | 3 (1.2) | 5 (1.5) | NS |
| Anxiolytics (NO5Bc) | 37 (6.4) | 10 (4.1) | 27 (8.0) | NS |
| Antidepressants (NO6Ac) | 117 (20.2) | 24 (9.9) | 93 (27.5) | <0.001 |
| Use of anti-insomnia medication, n (%) | ||||
| Hypnotics (NO5Cc) | 24 (4.1) | 7 (2.9) | 17 (5.0) | NS |
BMI: body mass index; NS: not significant.
Data are presented as mean (standard deviation) unless otherwise indicated.
Men vs women, χ2 test with Yates’ correction.
History of reflux oesophagitis and hiatal hernia was unknown in three and 252 patients, respectively.
World Health Organization Anatomical Therapeutic Chemical classification code.
Overall, 578 participants (99.7%) took a PPI in the four weeks before the study, of whom 577 took their PPI once daily: 516 individuals (89.4%) took their PPI in the morning; 59 (10.2%) took it in the evening; and 2 (0.3%) took it at another time (data were unavailable for one patient). Most patients (77.9% (n = 450)) used the maximum recommended PPI dose, and 73.0% (n = 422) had tried a different PPI with no improvement.
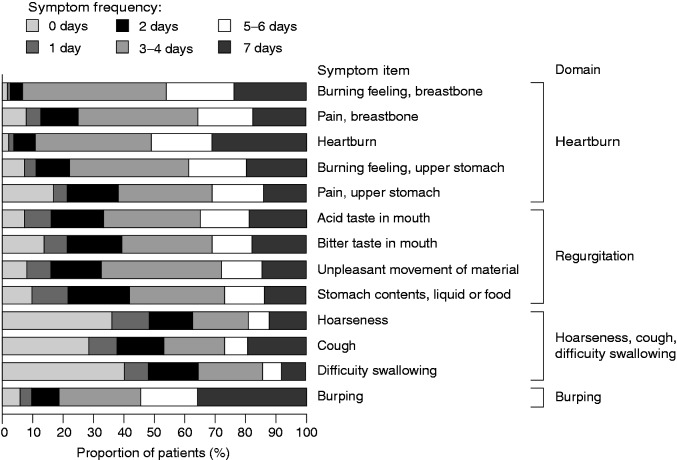
Overall symptom patterns
Baseline symptom frequencies per RESQ-7 item are shown in Figure 1. The most common symptoms reported to occur on a daily basis were burping and heartburn (occurring daily in 36% and 31% of patients, respectively). The most common items with moderately severe or severe intensity were heartburn (reported by 41% of patients), burping (34%) and burning feeling behind the breastbone (34%). Mean baseline intensity scores of the RESQ-7 were highest in the domains Heartburn and Burping (Table 2).
Figure 1.
Symptom frequencies per item at baseline in partial responders to proton pump inhibitor therapy, as assessed by the Reflux Symptom Questionnaire 7-day recall (RESQ-7) (n = 579; data were missing for one patient). Symptom frequency is scored on the RESQ-7 as the number of days during the previous seven days that each symptom is experienced (0, 1, 2, 3–4, 5–6 or 7 days).
Table 2.
Mean (95% confidence interval (CI)) item and domain intensity scores of the Reflux Symptom Questionnaire 7-day recall (RESQ-7)
| RESQ-7 domain/item | Mean (95% CI)a |
|---|---|
| Heartburn | 2.96 (2.88–3.03) |
| Burning feeling, breastbone | 3.16 (3.09–3.24) |
| Pain, breastbone | 2.86 (2.76–2.95) |
| Heartburn | 3.32 (3.23–3.40) |
| Burning feeling, upper stomach | 2.88 (2.78–2.97) |
| Pain, upper stomach | 2.58 (2.47–2.69) |
| Regurgitation | 2.64 (2.54–2.73) |
| Acid taste in mouth | 2.66 (2.55–2.77) |
| Bitter taste in mouth | 2.38 (2.27–2.49) |
| Unpleasant movement of material | 2.81 (2.70–2.91) |
| Stomach contents, liquid or food | 2.70 (2.59–2.80) |
| Hoarseness, cough, difficulty swallowing | 1.64 (1.54–1.74) |
| Hoarseness | 1.61 (1.48–1.73) |
| Cough | 1.77 (1.65–1.88) |
| Difficulty swallowing | 1.55 (1.43–1.67) |
| Burping | 2.96 (2.85–3.07) |
Data were missing for one patient.
Intensity is rated on the RESQ-7 using a six-point scale (0, did not have; 1, very mild; 2, mild; 3, moderate; 4, moderately severe; 5, severe).
Mean item and domain discomfort scores obtained using the GSRS are shown in Table 3. The highest scores were reported for the Reflux and Indigestion domains.
Table 3.
Mean (95% confidence interval (CI)) item and domain discomfort scores of the Gastrointestinal Symptom Rating Scale (GSRS)
| GSRS domain/item | Mean (95% CI)a |
|---|---|
| Reflux | 4.31 (4.21–4.40) |
| Heartburn | 4.42 (4.31–4.52) |
| Acid reflux | 4.20 (4.08–4.31) |
| Abdominal pain | 3.39 (3.30–3.49) |
| Abdominal pain | 4.04 (3.92–4.15) |
| Hunger pains | 3.46 (3.34–3.59) |
| Nausea | 2.68 (2.55–2.82) |
| Indigestion | 3.65 (3.54–3.76) |
| Rumbling | 3.28 (3.16–3.40) |
| Bloated | 3.67 (3.53–3.81) |
| Burping | 3.81 (3.67–3.94) |
| Passing gas | 3.85 (3.71–3.98) |
| Diarrhoea | 2.13 (2.02–2.23) |
| Diarrhoea | 1.93 (1.82–2.14) |
| Loose stools | 2.06 (1.95–2.17) |
| Urgent need for bowel movement | 2.39 (2.26–2.52) |
| Constipation | 2.48 (2.36–2.60) |
| Constipation | 2.45 (2.31–2.59) |
| Hard stools | 2.24 (2.11–2.36) |
| Feeling of incomplete bowel movement | 2.75 (2.61–2.89) |
Data were missing for three patients.
Degree of discomfort is rated on a scale of 1–7, where 1 = no discomfort at all; 7 = very severe discomfort.
Unadjusted gender differences in symptoms
Figure 2 shows mean RESQ-7 domain frequency and intensity scores separately by gender. Frequency and intensity scores for Regurgitation were similar in men and women. However, women reported significantly higher symptom frequency and intensity scores than men in the Heartburn, Burping, and Hoarseness, cough and difficulty swallowing domains of the RESQ-7.
Figure 2.
Mean domain frequency and intensity scores of the Reflux Symptom Questionnaire 7-day recall (RESQ-7), separately by gender. Symptoms are rated on the RESQ-7 using a six-point scale for frequency (0, did not have; 1, 1 day/week; 2, 2 days/week; 3, 3–4 days/week; 4, 5–6 days/week, 5, daily) and intensity (0, did not have; 1, very mild; 2, mild; 3, moderate; 4, moderately severe; 5, severe). Vertical bars represent 95% confidence intervals.
*p < 0.05 (non-parametric test: Wilcoxon test), †data were missing for one patient.
GSRS domain scores are shown separately by gender in Figure 3. Scores did not differ significantly in men and women in the Reflux and Diarrhoea domains. However, scores were significantly higher in women than in men in the Abdominal pain, Indigestion and Constipation domains.
Figure 3.
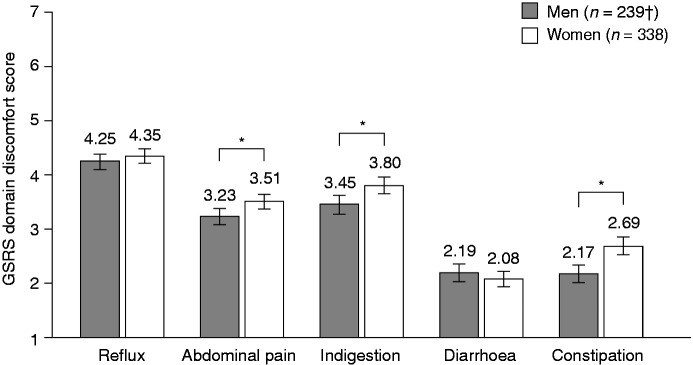
Mean domain discomfort scores of the Gastrointestinal Symptom Rating Scale (GSRS), separately by gender. Degree of discomfort is rated on a scale of 1–7, where 1 = no discomfort at all; 7 = very severe discomfort. Vertical bars represent 95% confidence intervals.
*p < 0.05 (non-parametric test: Mann–Whitney U test), †data were missing for three patients.
IBS
In total, 68 (11.7%) patients met the Rome II criteria for IBS and 63 (10.9%) met the Rome III criteria for IBS. Most participants (n = 54) who met the Rome II diagnostic criteria for IBS also met the Rome III diagnostic criteria for IBS. There was no statistical difference between men and women regarding the proportion of patients meeting Rome II and/or Rome III criteria.
Anxiety and depression
The prevalence rates for the three anxiety and depression score categories of the HADS (no disorder, possible and probable) are shown in Table 4, overall and separately by gender. Probable anxiety was present in 25.5% and probable depression in 8.5% of patients. Significantly more women than men had probable/possible anxiety and depression.
Table 4.
Prevalence of anxiety and depression, as assessed by the Hospital Anxiety and Depression Scale (HADS), overall and separately by gender
| No disorder, n (%) | Possible disorder, n (%) | Probable disorder, n (%) | p valuea (men vs women) | |
|---|---|---|---|---|
| Anxiety | ||||
| Overall (n = 576)b | 281 (48.8) | 148 (25.7) | 147 (25.5) | |
| Men (n = 240)b | 129 (53.8) | 65 (27.1) | 46 (19.2) | 0.044 |
| Women (n = 336)b | 152 (45.2) | 83 (24.7) | 101 (30.1) | |
| Depression | ||||
| Overall (n = 576)b | 435 (75.5) | 92 (16.0) | 49 (8.5) | |
| Men (n = 240)b | 192 (80.0) | 33 (13.8) | 15 (6.3) | 0.0035 |
| Women (n = 336)b | 243 (72.3) | 59 (17.6) | 34 (10.1) | |
Men vs women, χ2 test: no disorder vs possible/probable disorder.
Data were missing for two men and two women.
Scores<8 were taken as indicating no disorder, scores of 8–10 as indicating a possible disorder, and scores of 11–21 as indicating a probable disorder.
Potential influence of IBS, anxiety and depression on gender differences
Differences in RESQ-7 scores remained statistically significant after adjustment by presence or absence of IBS (Table 5). After adjustment for both IBS and HADS component scores, RESQ-7 score differences for frequency and severity of Hoarseness, cough and difficulty swallowing, and for intensity of Burping were no longer statistically significant (Table 5). IBS was statistically significant in most of the covariance analyses, potentially due to some correlation with the HADS sores. Of the two HADS score categories, depression was statistically significant in most of the analyses, but not anxiety.
Table 5.
Analyses of Reflux Symptom Questionnaire 7-day recall (RESQ-7) domain scores with p values with respect to gender
| Domain | No stratification or covariatea | Rome III IBS (yes/no)b | Anxiety and depression scores plus Rome III IBS (yes/no)c |
|---|---|---|---|
| Frequency scores | |||
| Heartburn | 0.015 | 0.026 | 0.044 |
| Regurgitation | 0.240 | 0.420 | 0.810 |
| Hoarseness, cough, Difficulty swallowing | 0.013 | 0.037 | 0.085 |
| Burping | 0.022 | 0.027 | 0.041 |
| Intensity scores | |||
| Heartburn | 0.017 | 0.024 | 0.027 |
| Regurgitation | 0.420 | 0.520 | 0.780 |
| Hoarseness, cough, difficulty swallowing | 0.016 | 0.035 | 0.071 |
| Burping | 0.009 | 0.011 | 0.063 |
IBS: irritable bowel syndrome.
Wilcoxon test. bStratified Wilcoxon test. cAnalysis of covariance.
Differences in GSRS scores remained statistically significant after adjustment for presence or absence of IBS, and differences in Diarrhoea domain scores became statistically significant on adjustment. After adjustment for both IBS and HADS component scores, GSRS score differences remained significant for Diarrhoea and were no longer significant for Abdominal pain.
Discussion
In this population of patients with GERD with a partial response to PPIs, symptoms of heartburn were significantly more frequent and significantly more intense in women than in men. Compared with men, women also had significantly more frequent and more intense extra-oesophageal symptoms (burping, hoarseness, cough and difficulty swallowing) and significantly more discomfort from abdominal pain, indigestion and constipation. Comorbid anxiety and depression among partial responders were more common in women than in men.
Partial symptomatic response to PPI therapy is seen more commonly in women than men with GERD.1–4 Among individuals with GERD, women are also more likely than men to have non-erosive reflux disease, whereas men are more likely than women to have reflux oesophagitis.4 The prevalence of partial response is higher in non-erosive reflux disease than in reflux oesophagitis,3,4 which may explain to some extent why partial response is associated with female gender. In our study population, more men than women had a history of reflux oesophagitis but, overall, most patients (82.8%) had a history of non-erosive reflux disease.
Although women had a higher heartburn burden than men in our study population of partial responders, frequency and intensity scores for regurgitation were similarly high in both sexes. This suggests that, while heartburn seems to respond less well to PPI therapy in women than in men, partial response of regurgitation to PPIs may be comparable in the two sexes. A lower overall response of regurgitation than heartburn to PPI therapy was observed in an analysis of two trials in patients with GERD and in a systematic review.22,23
Overall, prevalence rates for anxiety and depression in our study population were within the range previously reported for patients with GERD.10–12 However, the higher prevalence of anxiety and depression in women than men (as measured using the HADS) may have contributed to the increased symptom burden in women compared with men in our study population. Observed gender differences in heartburn, indigestion and constipation remained significant after adjustment for HADS scores (and IBS), indicating these are not explained by gender differences in the prevalence of anxiety and depression. However, adjustment for HADS scores and IBS resulted in loss of significance for the observed differences in extra-oesophageal symptoms and abdominal pain, with the depression (but not anxiety) score being statistically significant in most of the analyses, suggesting that gender disparities in the rates of depression may explain in part the observed differences in these symptoms.
Psychological stress has been shown to increase perception of heartburn and to worsen symptoms of GERD.24 In a population of patients with heartburn undergoing endoscopy, the presence of psychological stress was associated with a greater symptom burden before and after PPI therapy.25 High baseline HADS scores for anxiety and depression have also been shown to be associated with poor response to PPI treatment in patients with GERD symptoms.3
There is little information on the prevalence of IBS in patients who are partial responders to PPI therapy for GERD. In our study population, women had significantly more discomfort than men from abdominal pain, indigestion and constipation, while discomfort from diarrhoea did not differ significantly between the genders. However, the overall prevalence of IBS according to Rome II and/or III criteria was only slightly higher in women than in men and this difference was not statistically significant. Observed gender differences in abdominal pain, indigestion and constipation remained significant after adjustment for IBS, indicating that these are not explained by the presence of IBS comorbidity.
Modest gender differences in symptoms are also observed between men and women with IBS in general. For example, a recent meta-analysis showed that, compared with men with IBS, women with IBS were more likely to report constipation-related symptoms (OR 2.38; 95% CI: 1.45–3.92) and less likely to report diarrhoea-related symptoms (OR 0.45; 95% CI: 0.32–0.65).15 The overall prevalence of IBS in our study was similar to that reported in a large study of patients with GERD, in which the prevalence of IBS was 12.7% in patients with reflux oesophagitis and 18.3% in patients with non-erosive reflux disease.26 Earlier studies have reported higher prevalence rates of IBS in patients with GERD and it has been suggested that impaired health-related quality of life in these patients might be related to IBS rather than to GERD.13 Our results do not suggest that IBS is the major factor responsible for persistent symptoms in these patients. The gender differences in discomfort from abdominal pain suggest a higher prevalence of dyspepsia symptoms in women than men in our study, and symptoms that are related to non-GERD conditions such as functional dyspepsia are a possible reason for partial symptomatic response to PPI therapy.
Overall, 94% of patients in our study reported burping and more than one-third (36%) reported experiencing this symptom daily. The symptom frequency and intensity was higher in women than in men. Burping is associated with reflux events in patients with GERD;27–29 Kessing et al. used ambulatory 24-hour pH-impedance monitoring to show that patients with GERD are more likely to perceive liquid-containing gastro-oesophageal reflux events as burping than as heartburn or regurgitation.29 In that study, weakly acidic reflux episodes were just as likely as acid reflux episodes to be perceived as burping.28,29 Alongside symptoms more traditionally associated with GERD, burping may thus also need to be taken into account in clinical trials of anti-reflux therapies, particularly in partial responders to PPIs.
Hoarseness (reported by 64%) and cough (reported by 72%) were frequently reported symptoms in our population. Women had these symptoms at a higher frequency and intensity than men. These symptoms are difficult to assess as they may or may not be related to reflux disease. Therapeutic trials in partial responders will need to consider these symptoms in outcome measures. Gender differences in extra-oesophageal symptoms were also observed in an analysis based on the ProGerd study, which showed that, in patients with GERD, extra-oesophageal disorders were significantly more common in women than in men (OR 1.15; 95% CI: 1.03–1.30; p < 0.0178).30
Our study has several strengths and some weaknesses. It is one of the largest studies of partial responders to PPIs performed to date. Partial response to PPI therapy can be caused by incorrect disease diagnosis or poor adherence to therapy.31 In our study, the diagnosis was verified and PPI use was optimised by a gastroenterologist before entry into the study, decreasing the likelihood of these variables contributing to the population data. However, about 10% of participants took their PPI in the evening instead of in the morning and about 20% did not use the maximum recommended PPI dose, which may have increased the likelihood of persisting symptoms in these patients. A potential limitation of our study is that daily fluctuations in symptoms at baseline may not have been captured by the RESQ-7. For example, patients may have been influenced by their worst or most recent symptom experience when asked to report the average intensity of their symptoms during the 7-day recall period. The focus of our study was to determine the symptom profile of patients who have a partial response to PPI therapy and, therefore, patients were included based on GERD symptoms, without investigations such as endoscopy or pH measurements. While this is meaningful from a clinical standpoint, it does not provide insights into the mechanism of symptom generation (including extra-oesophageal symptoms) or into whether differences in symptom burden were affected by the presence of reflux oesophagitis, which has been shown in general population studies to be more common in men than women.32,33 Another limitation is that the investigation of gender differences was conducted as a post hoc analysis and was not the primary objective of the study.
In conclusion, the results of our study show that the remaining symptom burden in patients with GERD who have a partial response to PPI therapy is significantly higher in women than in men and includes burping, cough and hoarseness. The prevalence rates for anxiety and depression were significantly higher in women than in men, suggesting that these comorbidities contribute to the increased symptom burden in women with a partial PPI response.
Acknowledgements
Writing support was provided by Dr Anja Becher from Oxford PharmaGenesis Ltd, Oxford, UK, and was funded by AstraZeneca R&D, Mölndal, Sweden. Statistical support was provided by Tore Persson of AstraZeneca R&D, Mölndal, Sweden.
Funding
This study was funded by AstraZeneca R&D, Mölndal, Sweden.
Conflict of interest
N Vakil: consultancy fees from AstraZeneca, Ironwood Pharmaceuticals and Takeda Pharmaceutical; ownership interest in Meridian Bioscience. A Niklasson, H Denison, A Rydén: employees of AstraZeneca R&D, Mölndal, Sweden.
References
- 1.El-Serag H, Becher A, Jones R. Systematic review: Persistent reflux symptoms on proton pump inhibitor therapy in primary care and community studies. Aliment Pharmacol Ther 2010; 32: 720–737. [DOI] [PubMed] [Google Scholar]
- 2.Ruigomez A, Johansson S, Wernersson B, et al. Gastroesophageal reflux disease in primary care: Using changes in proton pump inhibitor therapy as an indicator of partial response. Scand J Gastroenterol 2012; 47: 751–761. [DOI] [PubMed] [Google Scholar]
- 3.Heading RC, Monnikes H, Tholen A, et al. Prediction of response to PPI therapy and factors influencing treatment outcome in patients with GORD: A prospective pragmatic trial using pantoprazole. BMC Gastroenterol 2011; 11: 52–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bytzer P, van Zanten SV, Mattsson H, et al. Partial symptom-response to proton pump inhibitors in patients with non-erosive reflux disease or reflux oesophagitis - a post hoc analysis of 5796 patients. Aliment Pharmacol Ther 2012; 36: 635–643. [DOI] [PubMed] [Google Scholar]
- 5.Labenz J, Armstrong D, Zetterstrand S, et al. Clinical trial: Factors associated with resolution of heartburn in patients with reflux oesophagitis–results from the EXPO study. Aliment Pharmacol Ther 2009; 29: 959–966. [DOI] [PubMed] [Google Scholar]
- 6.Mizyed I, Fass SS, Fass R. Review article: Gastro-oesophageal reflux disease and psychological comorbidity. Aliment Pharmacol Ther 2009; 29: 351–358. [DOI] [PubMed] [Google Scholar]
- 7.Becher A, El-Serag H. Systematic review: The association between symptomatic response to proton pump inhibitors and health-related quality of life in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2011; 34: 618–627. [DOI] [PubMed] [Google Scholar]
- 8.Zerbib F, Belhocine K, Simon M, et al. Clinical, but not oesophageal pH-impedance, profiles predict response to proton pump inhibitors in gastro-oesophageal reflux disease. Gut 2012; 61: 501–506. [DOI] [PubMed] [Google Scholar]
- 9.Wiklund I, Carlsson R, Carlsson J, et al. Psychological factors as a predictor of treatment response in patients with heartburn: A pooled analysis of clinical trials. Scand J Gastroenterol 2006; 41: 288–293. [DOI] [PubMed] [Google Scholar]
- 10.Piqué JM, Kulich KR, Vegazoc O, et al. Burden of gastroesophageal reflux disease. Evidence from a recent methodological study in Spain. Gastroenterol Hepatol 2004; 27: 300–306. [DOI] [PubMed] [Google Scholar]
- 11.Madisch A, Kulich KR, Malfertheiner P, et al. Impact of reflux disease on general and disease-related quality of life - evidence from a recent comparative methodological study in Germany. Z Gastroenterol 2003; 41: 1137–1143. [DOI] [PubMed] [Google Scholar]
- 12.Regula J, Kulich KR, Stasiewicz J, et al. Burden of illness in patients with reflux disease – evidence from a recent methodological study in Poland. Przeglad Epidemiologiczny 2005; 59: 75–85. [PubMed] [Google Scholar]
- 13.De Vries DR, Van Herwaarden MA, Baron A, et al. Concomitant functional dyspepsia and irritable bowel syndrome decrease health-related quality of life in gastroesophageal reflux disease. Scand J Gastroenterol 2007; 42: 951–956. [DOI] [PubMed] [Google Scholar]
- 14.Seedat S, Scott KM, Angermeyer MC, et al. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry 2009; 66: 785–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lovell RM, Ford AC. Effect of gender on prevalence of irritable bowel syndrome in the community: Systematic review and meta-analysis. Am J Gastroenterol 2012; 107: 991–1000. [DOI] [PubMed] [Google Scholar]
- 16.Vakil NB, Niklasson A, Denison H, et al. Symptom pattern in gastroesophageal reflux disease: Comparison with treatment-naïve patients suggests overlapping disease entities in partial responders to proton pump inhibitor therapy. Gastroenterology 2012; 142: S589–S590. [Google Scholar]
- 17.Vakil N, Björck K, Denison H, et al. Validation of the Reflux Symptom Questionnaire electronic diary in partial responders to proton pump inhibitor therapy. Clin Trans Gastroenterol 2012; 3: e7–e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ryden A, Denison H, Karlsson M, et al. Development and validation of a patient-reported outcome instrument in partial responders to proton pump inhibitors. Scand J Gastroenterol 2013; 48: 1018–1026. [DOI] [PubMed] [Google Scholar]
- 19.Dimenäs E, Glise H, Hallerbäck B, et al. Well-being and gastrointestinal symptoms among patients referred to endoscopy owing to suspected duodenal ulcer. Scand J Gastroenterol 1995; 30: 1046–1052. [DOI] [PubMed] [Google Scholar]
- 20.Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology 2006; 130: 1466–1479. [DOI] [PubMed] [Google Scholar]
- 21.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 22.Kahrilas PJ, Jonsson A, Denison H, et al. Regurgitation is less responsive to acid suppression than heartburn in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol 2012; 10: 612–619. [DOI] [PubMed] [Google Scholar]
- 23.Kahrilas PJ, Howden CW, Hughes N. Response of regurgitation to proton pump inhibitor therapy in clinical trials of gastroesophageal reflux disease. Am J Gastroenterol 2011; 106: 1419–1425. [DOI] [PubMed] [Google Scholar]
- 24.Fass R, Naliboff BD, Fass SS, et al. The effect of auditory stress on perception of intraesophageal acid in patients with gastroesophageal reflux disease. Gastroenterology 2008; 134: 696–705. [DOI] [PubMed] [Google Scholar]
- 25.Nojkov B, Rubenstein JH, Adlis SA, et al. The influence of co-morbid IBS and psychological distress on outcomes and quality of life following PPI therapy in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2008; 27: 473–482. [DOI] [PubMed] [Google Scholar]
- 26.Monnikes H, Heading RC, Schmitt H, et al. Influence of irritable bowel syndrome on treatment outcome in gastroesophageal reflux disease. World J Gastroenterol 2011; 17: 3235–3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hemmink GJ, Bredenoord AJ, Weusten BL, et al. Supragastric belching in patients with reflux symptoms. Am J Gastroenterol 2009; 104: 1992–1997. [DOI] [PubMed] [Google Scholar]
- 28.Kessing BF, Bredenoord AJ, Velosa M, et al. Supragastric belches are the main determinants of troublesome belching symptoms in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2012; 35: 1073–1079. [DOI] [PubMed]
- 29.Kessing BF, Bredenoord AJ, Velosa M, et al. Liquid-containing reflux events are more likely to be perceived as a belch than as heartburn or regurgitation. Gut 2011; 60: P0247–P0247. [Google Scholar]
- 30.Jaspersen D, Kulig M, Labenz J, et al. Prevalence of extra-oesophageal manifestations in gastro-oesophageal reflux disease: An analysis based on the ProGERD Study. Aliment Pharmacol Ther 2003; 17: 1515–1520. [DOI] [PubMed] [Google Scholar]
- 31.Dal-Paz K, Moraes-Filho JP, Navarro-Rodriguez T, et al. Low levels of adherence with proton pump inhibitor therapy contribute to therapeutic failure in gastroesophageal reflux disease. Dis Esophagus 2012; 25: 107–113. [DOI] [PubMed] [Google Scholar]
- 32.Ronkainen J, Aro P, Storskrubb T, et al. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: A Kalixanda study report. Scand J Gastroenterol 2005; 40: 275–285. [DOI] [PubMed] [Google Scholar]
- 33.Zagari RM, Fuccio L, Wallander MA, et al. Gastro-oesophageal reflux symptoms, oesophagitis and Barrett's oesophagus in the general population: Loiano-Monghidoro study. Gut 2008; 57: 1354–1359. [DOI] [PubMed] [Google Scholar]