Abstract
This study described the rate and predictors of Operation Enduring Freedom/Operation Iraqi Freedom active duty Army members’ enrollment in and use of Veterans Health Administration (VHA) services (linkage), as well as variation in linkage rates by VHA facility. We used a multivariate mixed effect regression model to predict linkage to VHA, and also calculated linkage rates in the catchment areas of each facility (n = 158). The sample included 151,122 active duty members who deployed to Iraq or Afghanistan and then separated from the Army between fiscal years 2008 and 2012. Approximately 48% of the active duty members separating utilized VHA as an enrollee within one year. There was significant variation in linkage rates by VHA facilities (31–72%). The most notable variables associated with greater linkage included probable serious injury during index deployment (odds ratio = 1.81), separation because of disability (odds ratio = 2.86), and various measures of receipt of VHA care before and after separation. Information about the individual characteristics that predict greater or lesser linkage to VHA services can be used to improve delivery of health care services at VHA as well as outreach efforts to active duty Army members.
INTRODUCTION
Over two million service members have been deployed to Afghanistan and Iraq during Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF). Several demographic and deployment-related characteristics differentiate these all-volunteer service members from those in earlier conflicts, including an increase in the portion of women, parents with young children, and deployment of Reserve Component (National Guard and Reserve) as well as active duty service members.1 As of 2010, approximately half of those deployed to Afghanistan and Iraq have been from the Army, with 56% of Army deployments by active duty and 44% by Reserve Component members.1 Compared to earlier conflicts, deployments to Iraq and Afghanistan have typically been longer, repeat deployments are frequent, and there may be limited breaks between deployments.2 There have been relatively high survival rates from serious injury, and common health issues include what are often considered “invisible wounds” of conflict—post-traumatic stress disorder, substance use disorders, depression, and symptoms associated with mild traumatic brain injury.1–7 Many have long-term health care needs, and it is important to anticipate the characteristics of veterans who may rely on the Veterans Health Administration (VHA) for some or all of their care.
To keep a fit and ready force during an era of conflict, access to a wide range of restorative health care services for service members is critical. During active duty, in addition to medical care received when deployed, members receive health care services on-base at military treatment facilities (MTFs) or clinics of the Department of Defense’s (DoD) Military Health System (MHS), and may be referred to private or VHA network providers as necessary. Active duty combat veterans who served after November 1998 are eligible to receive cost-free health care services from the VHA for 5 years after separation from the Army (Pub. L. No. 110-181). Those who enroll during this 5-year period remain eligible for VHA services after, but they may face copayments for services that are not service-connected based on their VHA priority group. To allocate resources, VHA has an eight-level priority system based on a member’s degree of service-related injury or disability, income, and other service characteristics.8
Access to VHA services is currently a top public policy concern, and it is a national priority to reduce real and perceived barriers to care.9 One important access area is whether veterans are enrolling in and utilizing (“linking” to) VHA care. Yet, there is limited literature about the characteristics or motivations of veterans who do or do not seek care at VHA. With respect to veterans who have not sought VHA care, a representative survey of all veterans revealed that they (not mutually exclusive categories): were unaware of benefits (42.3%), did not know how to apply for benefits (26.4%), did not need care (41.7%), used other health care sources (41.2%), and/or were never interested in getting care from VHA (30.0%).10 A survey specifically focused on OEF/OIF combat veterans who had received VHA services found that they experienced a variety of barriers to timely access to care.11 Despite these barriers, 95% of respondents would recommend care at VHA to other OEF/OIF veterans. Thus, it is critical to investigate manners in which we can improve linkage to VHA services.
The current study is a companion to a previous study that assessed the rate and predictors of VHA enrollment and care linkage for OEF/OIF Army Reserve Component members.12 Because of several administrative differences in the way Reserve Component and active duty members receive health care after deployment, it is not appropriate to conduct combined analyses. The purpose of this study of Army active duty members was to describe rates and predictors of linkage to VHA in the 365 days after separation in a cohort that had deployed and returned in fiscal years (FYs) 2008 to 2011. Although previous studies have examined rates of linkage, this is the first study to track a large cohort of active duty members who experienced a deployment to OEF/OIF after they separated from military service and to examine demographic, deployment, and health care–related predictors of linkage to VHA. We also uniquely described VHA facility-level variability in enrolling and serving veterans in their catchment areas. The information about patient, facility, and regional factors that are associated with higher and lower levels of linkage can be utilized to improve: access to needed services, local VA workforce planning and resource efforts, and joint DoD and VA planning efforts.
METHODS
This study is one component of the Substance Use and Psychological Injury Combat study (SUPIC), a longitudinal, observational study of Army service members who returned from deployment between FYs 2008 and 2011. Institutional review was conducted at Brandeis University, Stanford University, and the Human Research Protection Program of the Under Secretary of Defense for Personnel and Readiness. A description of the rationale, methods, and full SUPIC cohort are provided elsewhere.13 VHA linkage after separation is one outcome addressed by SUPIC, among other analyses that focus on outcomes specific to alcohol and drug misuse and psychological injury.14
Measures
The outcome variable was the receipt of any outpatient, inpatient, or residential health care from a VHA facility as an enrollee at least once during the 365 days after date of separation from the military that followed the index deployment. An index deployment is the first deployment ending in FYs 2008 to 2011 and matched to a Post-Deployment Health Assessment.13 We determined enrollment and utilization from the VHA National Patient Care Databases.
Predictor variables came from both DoD and VHA data. DoD data included: demographic characteristics from the Defense Enrollment Eligibility Reporting System; health care measures from the MHS Data Repository; and index deployment and separation date and reason derived from the Contingency Tracking System of the Defense Manpower Data Center.12 Predictor variables (measured at month before deployment unless indicated) included: age, gender, marital status, race/ethnicity, rank, number of deployments before index deployment, probable serious injury during index deployment, length of deployment, repeat deployment in the postindex year, cohort (FY of separation date—FYs 2008–2012), number of days between separation date and index deployment end date, separation code, and residence region. Separation codes included expiration of term of service, disability, behavioral, substance use disorder, unqualified, and other/not negative (including retirements).
Health care–related predictors came from the VHA National Patient Care Databases, and included: received preseparation VHA services as an enrollee in the VHA system (e.g., if previously served in the Army), received preseparation VHA services as a nonenrollee (e.g., through a services contract between DoD and VHA), and received postseparation VHA services as a nonenrollee (e.g., through a services contract between DoD and VHA). We used 5-digit zip codes and Google maps to estimate driving time to the nearest VHA facility with primary care services.
Data Analysis
We first calculated descriptive demographic, deployment, and health care statistics for the active duty Army members who separated during the observation period. We then used mixed effects logistic regression models to predict VHA utilization as an enrollee in the 365 days following separation, with a random effect for VHA facility (n = 158) to account for clustering of members within a facility. All considered predictors were included, and regression diagnostics, including an examination of variance inflation factors, were performed. Assumptions regarding linearity were examined and found to be reasonable for all continuous variables. Given the large sample size, we report odds ratios (ORs) and confidence intervals (CIs) rather than p-values. In addition to using logistic regression to analyze our dichotomous outcome variable, it would have been interesting to conduct a time-to-event analysis to better understand the timing of enrollment; however, this second analysis could not be conducted because our data did not meet the proportional hazards assumption of survival analysis.
To examine variation in linkage to VHA facilities, we assigned each member in the sample to one of the 158 major VHA facilities across the country. All VHA medical centers, clinics, and other settings of care are organized into one of these 158 organizational units. System monitoring and performance measurement is conducted at this level. We estimated the percentage (95% CI) of members in each VHA facility’s catchment area who received VHA services as an enrollee at any VHA facility using multivariate mixed effects regression models predicting utilization that control for other characteristics.
RESULTS
The demographic, deployment and separation, and health care characteristics of 151,122 active duty members who had been deployed to Iraq or Afghanistan and separated from the Army between FYs 2008 and 2012 are presented in Table I. The average age of these Army active duty members was approximately 26. Although the vast majority of members were men, approximately 1 out of 10 were female. About half of the group (49.75%) was married. A majority was non-Hispanic White (59.00%), followed by non-Hispanic African American (14.92%), Asian or Pacific Islander (13.39%), Hispanic (10.61%), and a very small portion of American Indian/Alaska Native (1.10%) and other races/ethnicities (0.98%).
TABLE I.
Background Characteristicsa of Army Active Duty Members (N = 151,122), with Index Deployment End Dates of FYs 2008–2011
| Categorical Variables | N (%) |
|---|---|
| Female | 16,107 (10.66) |
| Married | 75,184 (49.75) |
| Race/Ethnicity | |
| Non-Hispanic White | 89,162 (59.00) |
| Non-Hispanic African American | 22,549 (14.92) |
| Asian or Pacific Islander | 20,229 (13.39) |
| Hispanic | 16,035 (10.61) |
| American Indian/Alaska Native | 1,660 (1.10) |
| Other | 1,487 (0.98) |
| Rank | |
| Junior Enlisted | 101,133 (66.92) |
| Senior Enlisted | 37,873 (25.06) |
| Junior Officer | 15,422 (10.20) |
| Senior Officer | 2,940 (1.95) |
| Warrant Officer | 1,902 (1.26) |
| Probable Serious Injury During Indexb Deployment | 6,804 (4.50) |
| Repeat Deployment in the Postindex Year | 6,680 (4.50) |
| Separation Date Cohortc | |
| 2008 | 12,115 (8.02) |
| 2009 | 24,404 (16.15) |
| 2010 | 32,315 (21.38) |
| 2011 | 38,582 (25.53) |
| 2012 | 43,706 (28.92) |
| Received Preseparationd VHA Services as Enrollee in VHA System | 6,862 (4.54) |
| Received Preseparation VHA Services as Nonenrollee | 25,503 (16.88) |
| Separation Code | |
| Expiration of Term of Service | 72,849 (48.21) |
| Other, not Negative | 37,943 (25.11) |
| Disability | 15,422 (10.20) |
| Behavioral | 13,231 (8.76) |
| Substance Use Disorder | 6,796 (4.50) |
| Unqualified | 4,881 (3.23) |
| Residence Region at Index Deployment | |
| End Date | |
| South | 90,705 (60.02) |
| West | 36,737 (24.31) |
| Midwest | 12,179 (8.06) |
| Northeast | 11,501 (7.61) |
| Received Postseparation VHA Services as Nonenrollee | 14,037 (9.29) |
| Received Postseparation VHA Services as Enrollee in VHA System | 73,100 (48.37) |
| Continuous Variables | Mean (SD) |
| Age in Years | 26.07 (7.02) |
| Number of Deployments Before Index Deployment | 0.56 (0.81) |
| Length of Index Deployment (in Months) | 11.95 (5.02) |
| Gap (in Months) Between Separation Date and Index Deployment End Date | 17.08 (12.46) |
| Drive Time (in Hours) to Nearest VHA Facility | 0.56 (0.92) |
Measured at month before index deployment unless indicated.
Index refers to a deployment ending in FYs 2008–2011.
Cohort refers to FY of separation date.
Separation refers to a separation ending in FYs 2008–2012.
The majority of separated Army active duty members were junior enlisted (66.92%), followed by senior enlisted at 25.06%, and a small portion of junior officers (4.81%), senior officers (1.95%), and warrant officers (1.26%). On average, each Army active duty member was deployed 0.56 times before their index deployment (SD = 0.81). Index deployment lasted nearly a year (mean of 11.95 months; SD = 5.02). During their index deployment, about 4% had a probable serious injury—defined as receiving inpatient services within a MHS hospital immediately after deployment. Approximately 4% were deployed again within 1 year after returning from their index deployment. In each FY cohort, a greater portion of the active duty sample separated—8.02% in FY 2008, 16.15% in FY 2009, 21.38% in FY 2010, 25.53% in FY 2011, and 28.92% in FY 2012. On average, there was a gap of 17.08 months (or about 1.42 years) between members’ index deployment end and separation date. Reasons for separating from Army active duty included the end of their service term (48.21%), other—not negative (25.11%), disability (10.20%), behavioral (8.76%), substance use disorder (4.50%), and unqualified (3.23%). At the time of separation, most individuals (60.02%) resided in the South, with about one quarter (24.31%) in the West, and smaller portions in the Midwest (8.06%) and Northeast (7.61%).
Before separating, a small segment received VHA services as enrollees (4.54%), presumably with eligibility from other terms of service, and a larger portion received services as nonenrollees (16.88%; e.g., through TRICARE payment or other arrangements with DoD). After separation, approximately 9% received VHA services as a nonenrollee (e.g., through a service contract with DoD). For our main outcome variable, nearly half (48.4%) received VHA services as an enrollee within 12 months. On average, drive time to the nearest VHA facility was approximately 0.57 hours, with considerable variation (SD = 0.92).
In the logistic regression analysis (Table II), although most of the characteristics of Army active duty members were statistically significant predictors of VHA utilization as an enrollee (linkage) in the year following separation, here we focus on reporting the magnitude of the ORs given the large sample size. Most of the ORs hovered just above or below a value of 1, with some exceptions that are detailed here. When compared with junior enlisted, higher ranking service members had considerably lower odds of VHA linkage—senior enlisted (OR = 0.82), junior officer (OR = 0.73), senior officer (OR = 0.42), and warrant officer (OR = 0.62). Army active duty members had a much higher odds of VHA linkage if they had a probable serious injury during index deployment (OR = 1.81). The most notable OR for a reason for separation was for disability (OR = 2.86). Other considerably large ORs included receipt of additional health care before or after separation—received preseparation VHA services as enrollee (OR = 3.06), received preseparation VHA services as nonenrollee (OR = 1.45), and received postseparation VHA services as nonenrollee (1.68).
TABLE II.
Predictors of VHA Utilization as an Enrollee in the 365 Days after Separation for 151,122 Active Duty Members
| Parametera | OR (95% CI) |
|---|---|
| Demographic Characteristics | |
| Age in Years | 1.033 (1.030–1.035) |
| Female | 1.150 (1.110–1.192) |
| Married | 0.907 (0.886–0.928) |
| Race/Ethnicity (Non-Hispanic White as Reference) | |
| Non-Hispanic African American | 1.192 (1.155–1.231) |
| Asian or Pacific Islander | 0.958 (0.927–0.990) |
| Hispanic | 1.165 (1.124–1.207) |
| American Indian/Alaska Native | 0.997 (0.900–1.103) |
| Other | 0.971 (0.871–1.083) |
| Deployment and Separation Characteristics | |
| Rank (Junior Enlisted as Reference) | |
| Senior Enlisted | 0.816 (0.789–0.844) |
| Junior Officer | 0.732 (0.691–0.776) |
| Senior Officer | 0.419 (0.382–0.461) |
| Warrant Officer | 0.625 (0.563–0.693) |
| Length of Index Deployment (in Months) | 1.012 (1.009–1.014) |
| Number of Deployments Before Indexb Deployment | 1.021 (1.005–1.036) |
| Probable Serious Injury During Index Deployment | 1.812 (1.696–1.935) |
| Repeat Deployment in the Postindex Year | 0.947 (0.898–0.998) |
| Separation Date Cohortc (2008 as Reference) | |
| 2009 | 1.056 (1.009–1.105) |
| 2010 | 1.009 (0.965–1.055) |
| 2011 | 0.974 (0.931–1.020) |
| 2012 | 0.999 (0.951–1.050) |
| Gap (in Months) Between Separation Date and Index Deployment End Date | 1.001 (1.000–1.002) |
| Separation Code (Expiration of Term of Service as Reference) | |
| Other, not Negative | 0.627 (0.606–0.648) |
| Disability | 2.863 (2.728–3.004) |
| Behavioral | 0.928 (0.893–0.964) |
| Substance Use Disorder | 1.130 (1.074–1.189) |
| Unqualified | 1.363 (1.285–1.447) |
| Residence Region at Index Deployment | |
| End Date (West as Reference) | |
| South | 0.913 (0.835–0.998) |
| Midwest | 1.162 (1.045–1.293) |
| Northeast | 1.221 (1.084–1.377) |
| Health Care Characteristics | |
| Drive Time (in Hours) to Nearest VHA Facility | 0.979 (0.963–0.994) |
| Received Preseparationd VHA Services as Enrollee in VHA System | 3.056 (2.879–3.245) |
| Received Preseparation VHA Services as Nonenrollee | 1.454 (1.406–1.504) |
| Received Postseparation VHA Services as Nonenrollee | 1.680 (1.611–1.751) |
Measured at month before index deployment unless indicated.
Index refers to a deployment ending in FYs 2008–2011.
Cohort refers to FY of separation date.
Separation refers to a separation ending in FYs 2008–2012.
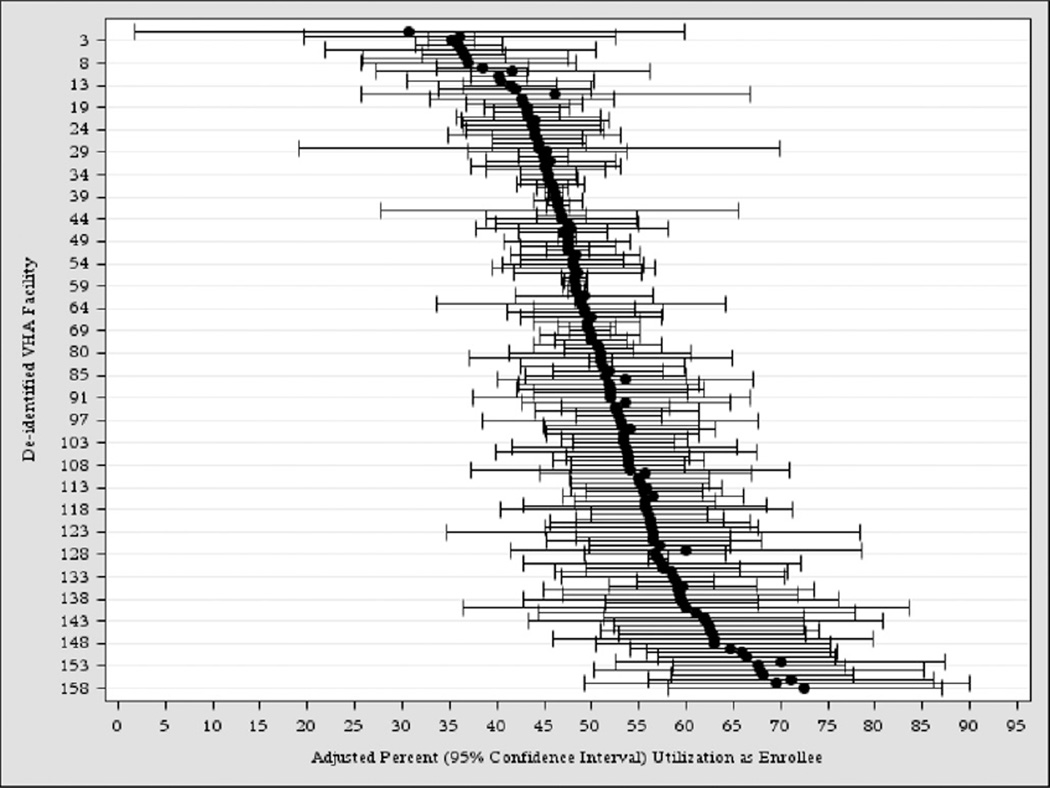
Wide variation existed in the portion (95% CI) of Army active duty members in each VHA facility’s catchment area who received any VHA services as an enrollee at any facility in the year following separation (Fig. 1). The results are adjusted for the background characteristics shown in Table II. Facility-level utilization as an enrollee in the year following separation ranged from 31 to 72%.
FIGURE 1.
Percent of active duty members with any VHA utilization as an enrollee in a VHA facility catchment area. Utilization measured in the year following member’s separation between FYs 2008 and 2012. Adjusted for characteristics shown in Table II.
DISCUSSION
The descriptive analysis found that 48.4% of OEF/OIF active duty Army members of recent deployment cohorts utilized VHA as an enrollee within 12 months following separation. This rate is similar to that reported in a companion article, which found that 56.9% of OEF/OIF Army National Guard and 45.7% of OEF/OIF Army Reserve members utilized VHA as an enrollee within 12 months after demobilizing (i.e., discharging) from an index deployment.11 Collectively, this work suggests that about half of OEF/OIF Army service members enroll in VHA and utilize services in the first year following eligibility (i.e., either demobilization for the Reserve Component or separation for active duty members).12 Although it is unknown what happens after our 1-year observation period, we plan to follow this cohort of OEF/OIF Army active duty members for up to 3 years following separation along with the OEF/OIF Army National Guard and Reserve members studied separately.12 We will reassess linkage rates longitudinally as well as predictors of delayed linkage.
In addition to finding similar linkage rates for Army active duty to National Guard and Reserve members, we found a remarkable range in linkage by facility for these three groups. By facility, between 31% and 72% of active duty members assigned to a facility’s catchment area utilized at least one VHA service at any facility as an enrollee within 365 days of separation (Fig. 1). This range was slightly narrower than we reported for National Guard (31%–89%) and Reserve (27%–81%) members after demobilization.12 We speculate that differences in these ranges could in part be explained by differences in access to employment-related insurance among Reserve Component members who might have returned to civilian deployment, or possibly to differences in identification with the military and veteran social role.
An important observation in this study is the wide range in linkage rates at the facility level for active duty members. Such large variation is also present in the National Guard and Reserve Components.12 Some potential explanations for these differences could be facility-level outreach, perceived quality at the facility level, facility-specific waiting lists and scheduling practices, and/or local availability of alternative health care services outside VHA. A more complete understanding of these issues requires additional research efforts that address whether or not these wide differences reflect veterans’ active choices to use or not use VHA, or the lack of information about resources at these facilities. This increased understanding of the sources of facility-level variation is critical for VHA to be a learning health care system, constantly adapting to meet the needs of veterans, and for DoD to assist with linking veterans to VHA when needed.
The predictors of linkage analyzed in the current study, particularly those related to deployment and separation characteristics, provide valuable information about the characteristics of Army active duty service members who do and do not link to VHA. A stronger tendency to link to VHA may reflect which groups have a greater interest in connecting to VHA and/or could signal good outreach to these groups by DoD and VHA. A lower tendency to link to VHA might highlight which groups need more information about services, do not currently need health care services, or are receiving care elsewhere.
There are four deployment or separation predictors that provide particularly helpful information about linkage (Table II). First, the lower linkage for service members with ranks above junior enlisted is not surprising given that they might be more likely to have access to health care outside VHA, e.g., through employer-sponsored health insurance. Second, the effect size was particularly large for the disability separation (OR = 2.86), which may reflect the importance of VHA for service members with high health care needs. Third, the direction of the effect for number of deployments before index deployment was found to be the opposite (negative) in the complementary analysis on Army National Guard and Reserve members.12 This may suggest that these previous deployments created more health care needs for Army active duty members, although they signify something quite different for Army National Guard and Reserve members. In a companion article on Army National Guard and Reserve members, the authors suggest that this lower odds of linkage is because of the “healthy warrior effect,”15 whereby members with better health would be predicted to be more likely to be deployed again and less likely to need VHA services after separation.12 Fourth, and in contrast, in all cases (for Army active duty, National Guard, and Reserve members), repeat deployment in the postindex year was associated with lower odds of linkage.12
With respect to health care characteristics, receipt of any other health care in VHA (preseparation as an enrollee or a nonenrollee as well as postseparation as a nonenrollee) was positively, statistically, and significantly associated with linkage (Table II). This is likely due to increased familiarity with the system before enrolling in and utilizing services at VHA.
A couple limitations of the study should be considered. First, some veterans seek and receive services (e.g., counseling) at VA Vet Centers,16 encounters that are not included in VHA administrative data. Thus, our estimates are a lower bound as we are missing a particular type of connection to VHA that may be helpful to veterans. Second, we only include indirect measures of medical need in our analyses, and more nuanced measures such as service-connected disability rating could be important.
To our knowledge, this study is the first to describe predictors of Army active duty enrollment in and utilization of VHA services. Information about the demographic, deployment, and health care factors that are positively and negatively associated with linkage can help both DoD and VHA target education and outreach to members both during active duty and after separation. On the one hand, the variables indicative of an already high connection to VHA (e.g., disability) may help VHA administration prospectively anticipate demands for health care based on characteristics of separating service members. On the other hand, a negative association with linkage provides DoD and VHA leaders with an opportunity to target specific outreach efforts to certain populations (e.g., Asian or Pacific Islander).
This work to improve linkage has begun by DoD and VHA, but there is room for improvement.17 For example, DoD and VHA have worked together to provide a seamless transition from MTFs to VHA through efforts such as having VHA social workers assigned to particular MTFs.18 Despite these projects, DoD and VHA have been criticized for problems with their collaborations, including barriers to sharing health information and not systematically identifying collaboration opportunities.19,20 Thus, more innovative and informed attempts to improve linkage, particularly for veterans most in need of VHA services, must be made. Improving communication between DoD and VHA as well as with service members may help veterans access valuable health care.
ACKNOWLEDGMENTS
We gratefully acknowledge Kennell and Associates for compiling the data used in these analyses, as well as Thomas V. Williams, the study’s Defense Health Agency, DoD, government project manager. This study was funded by the National Institute on Drug Abuse (R01DA030150) and supported by VA Health Services Research and Development (RCS-14-232) and the VA Office of Academic Affiliations. The Defense Health Agency’s Privacy and Civil Liberties Office, Army’s Office of the Surgeon General, and DoD Manpower Data Center provided access to data used in this study.
Footnotes
The opinions or assertions herein are the authors and do not necessarily reflect the views of the Department of Defense, Veterans Health Administration, or National Institutes of Health.
REFERENCES
- 1.National Research Council. Returning Home from Iraq and Afghanistan: Assessment of Readjustment Needs of Veterans, Service Members, and Their Families. Washington, DC: The National Academies Press; 2013. [accessed December 5, 2014]. Available at http://www.nap.edu/catalog/13499/returning-home-from-iraq-and-afghanistan-assessment-of-readjustment-needs. [PubMed] [Google Scholar]
- 2.Tanielian T, Jaycox LH. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008. [accessed December 5, 2014]. Available at http://www.rand.org/pubs/monographs/MG720.html. [Google Scholar]
- 3.Larson MJ, Wooten NR, Adams RS, Merrick EL. Military combat deployments and substance use: review and future directions. J Soc Work Pract Addict. 2012;12:6–27. doi: 10.1080/1533256X.2012.647586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Melcer T, Walker GJ, Galarneau M, Belnap B, Konoske P. Midterm health and personnel outcomes of recent combat amputees. Mil Med. 2010;175(3):147–154. doi: 10.7205/milmed-d-09-00120. [DOI] [PubMed] [Google Scholar]
- 5.Adams RS, Larson MJ, Corrigan JD, Horgan CM, Williams TV. Frequent binge drinking after combat-acquired traumatic brain injury among active duty military personnel with a past year combat deployment. J Head Trauma Rehabil. 2012;27(5):349–360. doi: 10.1097/HTR.0b013e318268db94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barlas FM, Higgins WB, Pflieger JC, Diecker K. 2011 Department of Defense Health Related Behaviors Survey of Active Duty Military Personnel. Fairfax, VA: ICF International; 2013. [accessed December 5, 2014]. Available at http://tricare.mil/tma/dhcape/surveys/coresurveys/surveyhealthrelatedbehaviors/downloads/Final%202011%20HRB%20Active%20Duty%20Survey%20Exec%20Summary.pdf. [Google Scholar]
- 7.Institute of Medicine. Substance Use Disorders in the U.S. Armed Forces. Washington, DC: The National Academies Press; 2013. [accessed December 5, 2014]. Available at http://www.nap.edu/catalog/13441/substance-use-disorders-in-the-us-armed-forces. [PubMed] [Google Scholar]
- 8.Department of Veterans Affairs. Priority Group Table. [accessed December 5, 2014]; Available at http://www.va.gov/healthbenefits/resources/priority_groups.asp.
- 9.Griffin D, Bronstein S, Cohen T. Obama signs $16 billion VA overhaul into law. [accessed December 5, 2014];CNN. 2014 Aug 7; Available at http://www.cnn.com/2014/08/07/politics/obama-va-bill/index.html. [Google Scholar]
- 10.Westat. Washington, DC: Department of Veterans Affairs; 2010. [accessed December 5, 2014]. National Survey of Veterans, Active Duty Service Members, Demobilized National Guard and Reserve Members, Family Members, and Surviving Spouses. Available at http://www.va.gov/vetdata/docs/SurveysAndStudies/NVSSurveyFinalWeightedReport.pdf. [Google Scholar]
- 11.Randall MJ. Gap analysis: transition of health care from Department of Defense to Department of Veterans Affairs. Mil Med. 2012;177(1):11–16. doi: 10.7205/milmed-d-11-00226. [DOI] [PubMed] [Google Scholar]
- 12.Harris AHS, Cheng C, Mohr BA, et al. Predictors of Army National Guard and Reserve members’ use of Veteran Health Administration health care after demobilizing from OEF/OIF deployment. Mil Med. 2014;179(10):1090–1098. doi: 10.7205/MILMED-D-13-00521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larson MJ, Adams RS, Mohr BA, et al. Rationale and methods of the Substance Use and Psychological Injury Combat Study (SUPIC): a longitudinal study of Army service members returning from deployment in FY 2008–2011. Subst Use Misuse. 2013;48(10):863–879. doi: 10.3109/10826084.2013.794840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larson MJ, Mohr BA, Adams RS, Wooten NR, Williams TV. Missed opportunity for alcohol problem prevention among Army active duty service members postdeployment. Am J Public Health. 2014;104:1402–1412. doi: 10.2105/AJPH.2014.301901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haley RW. Point: bias from the “healthy-warrior effect” and unequal follow-up in three government studies of health effects of the Gulf War. Am J Epidemiol. 1998;148(4):315–323. doi: 10.1093/oxfordjournals.aje.a009645. [DOI] [PubMed] [Google Scholar]
- 16.Rosen CS, Greenbaum MA, Fitt JE, Laffaye C, Norris VA, Kimerling R. Stigma help-seeking attitudes, and use of psychotherapy in veterans with diagnoses of posttraumatic stress disorder. J Nerv Ment Dis. 2011;199(11):879–885. doi: 10.1097/NMD.0b013e3182349ea5. [DOI] [PubMed] [Google Scholar]
- 17.Military Compensation and Retirement Modernization Commission. Arlington, VA: Military Compensation and Retirement Modernization Commission; 2015. [accessed February 2, 2015]. Report of the Military Compensation and Retirement Modernization Commission: Final Report. Available at http://www.mcrmc.gov/public/docs/report/MCRMC-FinalReport-29JAN15-HI.pdf. [Google Scholar]
- 18.General Accountability Office. Washington, DC: United States Government Accountability Office; 2006. [accessed December 5, 2014]. VA and DOD Health Care: Efforts to Provide Seamless Transition of Care for OEF and OIF Servicemembers and Veterans. Available at http://www.gao.gov/products/GAO-06-794R. [Google Scholar]
- 19.General Accountability Office. Washington, DC: United States Government Accountability Office; 2013. [accessed December 5, 2014]. Long History of Management Challenges Raises Concerns about VA’s and DOD’s New Approach to Sharing Health Information. Available at http://www.gao.gov/products/GAO-13-413T. [Google Scholar]
- 20.General Accountability Office. Washington, DC: United States Government Accountability Office; 2012. [accessed December 5, 2014]. Department-Level Actions Needed to Assess Collaboration Performance, Address Barriers, and Identify Opportunities. Available at http://gao.gov/products/GAO-12-992. [Google Scholar]