Abstract
This empirical study examines the association between substance abuse, mental illness, health behaviors and different patterns of homelessness among recently released, HIV-infected jail detainees. Using longitudinal data from a 10-site study, we examine correlates of homelessness, transitions to and from stable housing and the effect of housing on HIV treatment outcomes. Based on our analysis, we found evidence that the transitions from homelessness are closely associated with a reduction in the use of alcohol and illicit drugs, a decline in drug addiction severity, and an improvement in mental health. In addition, we found evidence that disparities in the housing status contributed substantially to the observed gap in the HIV treatment outcomes between homeless and non-homeless patients, including in achievement of virological suppression over time.
Keywords: HIV, Jail, Incarceration, Homelessness, Substance abuse, Case management, Longitudinal cohort study
Introduction
Incarceration, including the revolving door through jails and prisons, contributes to poor HIV treatment outcomes through a number of different mechanisms [1]. Important among these is the disruption of social networks, [2–4] resulting in destabilized housing [5] and increased HIV-risk taking behaviors [4]. Incarceration of HIV-infected drug users prevents entrance into social service and rehabilitation programs, resulting in social destabilization in which these individuals have limited effective treatment opportunities [6, 7]. Additionally, inadequate access to and provision of treatment for mental illness and lack of social support puts them at a greater risk of recurrent drug use [8]. The lack of enabling resources, combined with predisposing conditions such as substance use disorders (SUDs), conspire to negatively impact HIV treatment outcomes [9–11]. For HIV-infected drug users, recidivism and poor continuity of care upon release result in poor clinical outcomes and thwart public health efforts [12, 13].
A sixth of all people living with HIV/AIDS (PLWHA) in the United States cycle through prison or jail annually, with nearly all doing so initially through a jail [14]. Therefore, reducing the vulnerability of the recently released HIV-infected jail detainees is a crucial component of coordinating post-release services and promoting optimal HIV treatment outcomes. Jail detainees, often released without a transitional plan, frequently face unstable housing circumstances, problems finding employment and loss of medical and social entitlements. Indeed, compared to their housed counterparts, homeless HIV-infected individuals who enter jail experience poor HIV treatment outcomes before incarceration [5]. The interdependence between incarceration and housing instability, drug and alcohol use, mental health and HIV poses many challenges for designing effective interventions that result in improved social and health outcomes [6].
Homelessness and incarceration are syndemic and mutually reinforcing of poor treatment outcomes. Depending on location, available estimates suggest that between 23 % and 68 % of homeless individuals have a history of incarceration [15, 16]. Similarly, among the criminal justice population, between 10 % and 50 % experienced homelessness at some point in the year prior to incarceration [17].
In studies that have analyzed the relationship between homelessness and retention in HIV care, unstable housing and homelessness have been shown to be associated with poor adherence to HIV medications and increased risk of death among PLWHA [18–20]. Compared with individuals who are stably housed, homeless individuals are particularly more likely to experience worse HIV health outcomes, including viral load and CD4 count determinations [18–20]. These findings reflect decreased access to and utilization of HIV care and ART and, for those who are prescribed ART, lower levels of adherence due to underlying mental illness and high rates of SUDs among those who return to the community [21, 22].
Innovative community programs like the “Housing First” model that prioritize housing over other enabling resources, reflect the notion that once a person is provided with a stable place to live, all other factors, including health, are improved [20, 23, 24]. Transitional services for persons returning to the community from incarceration have demonstrated improved health outcomes when housing was incorporated [11, 25]. Further confirmation of this approach, however, is urgently needed for those with HIV infection to help policy makers and service providers to design and implement better interventions.
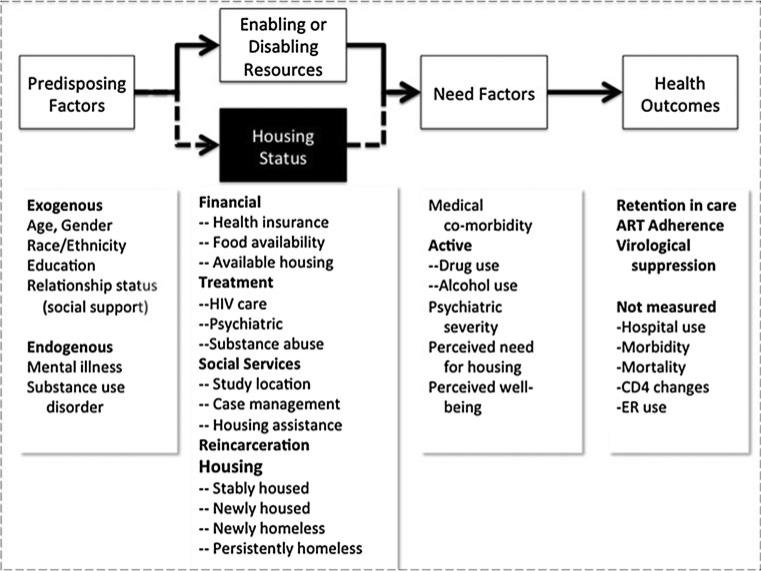
The Behavioral Model for Vulnerable Populations [5, 26] is a theoretical approach to incorporate a complex array of factors, including homelessness, that contributes to healthcare utilization and specific treatment outcomes. A depiction of this model is provided in Fig. 1 and described elsewhere for homeless populations [5].
Fig. 1.
Behavioral model for vulnerable populations: adaptation for homeless outcomes (Color figure online)
Data collected from the Health Resources and Services Administration's Special Project of National Significance (HRSA-SPNS) Enhancing Linkages to HIV Primary Care Services Jail Settings Initiative (EnhanceLink) program was examined to assess the following aims: (1) to examine factors that influence homelessness among HIV-infected recently released jail detainees at baseline and 6 months post-release; (2) identify factors that are associated with transitions to and from stable housing; and (3) assess the gap in HIV-related healthcare engagement that results from the individual's housing status. Additional details about the services provided at each site [27], retention in HIV care [28] and substance abuse treatment outcomes [29] are described elsewhere.
Data and Sample Selection
The ten-site EnhanceLink initiative assessed an array of innovative interventions delivered to HIV-infected jail detainees who were transitioning to the community across ten geographically diverse U.S. communities [27].
Although eligibility criteria differed slightly across sites, the study was generally restricted to HIV-infected detainees aged 18 years or older. New York, for example, excluded subjects who required independent case management services for mental illness, while Chicago included only women. From January 2008 to November 2011, 1,270 subjects underwent informed consent and were enrolled.
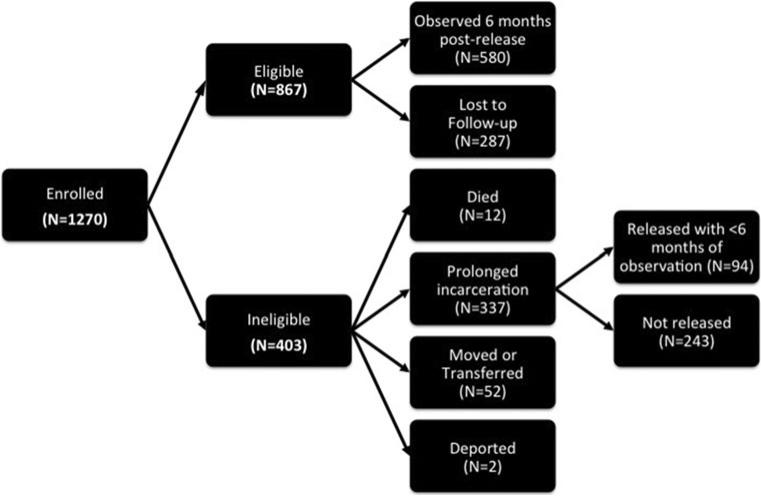
Among these, 403 (31.7 %) subjects were excluded from the analytical sample, including individuals who: (1) remained incarcerated and/or transferred to prison (N = 243); (2) were released from jail near the end of the study and did not have a full 6 months of post-release evaluation (N = 94); (3) died (N = 12); (4) moved away from the catchment area and were unavailable for follow-up (N = 26); (5) were administratively transferred to non-participating institutions (N = 26); or (6) were deported (N = 2). Compared to the 867 subjects who remained in the sample, excluded participants were more likely to be male and less like to be married or be in a stable relationship, and less likely to be re-incarcerated (most commonly because they were never released). Factors commonly associated with poor retention in care, such as substance abuse, medical co-morbidity, lack of previous HIV care engagement and baseline housing status, however, were not statistically different in the analytic and excluded samples, suggesting that bias was not introduced as a result of exclusion. Of the 867 subjects in the final analytic sample, 580 (66.9 %) also had data at the six-month evaluation (Fig. 2).
Fig. 2.
Disposition of study participants (Color figure online)
The Institutional Review Board at Rollins School of Public Health at Emory University and Abt Associates approved the multisite study, and each site's IRB approved and oversaw individual site involvement. A certificate of confidentiality was also obtained for the study.
Study Instruments and Variable Definitions
Data were collected by each of the sites and entered into a common electronic database. Baseline data covered the current incarceration and immediate pre-incarceration periods and were collected through structured interviews at the time of incarceration; jail-based medical chart reviews of the detainees were compiled while the detainees remained incarcerated. Follow-up data provided by each site covered the interim period over the 6 months following release from jail, and included a structured interview, clinic based medical chart review, and case manager reports of community-based services provided.
Homelessness was defined previously by self-report if the subject indicated that they were either homeless or if they indicated that in the previous 30 days they had slept in a shelter, the street or a park, an empty building, a bus station or in some other public space [5]. The variable was measured at baseline and in 6-month post-release period. Independent variables were gleaned from our conceptual framework, the Behavioral Model for Vulnerable Populations, that have previously been used to study homeless populations [5, 30, 31]. The independent variables, aside from health beliefs that were not measured, are included in Fig. 1, and are measured at the baseline and in the end of the 6 month post-release period as well.
As a proxy for predisposing factors and as control for heterogeneity, a number of self-reported baseline demographic variables were included such as age, gender, race and ethnicity, educational level and relationship status. Being in a relationship was defined based on whether the individual reported being married or in a committed relationship. Drug use and mental disorders were by self-report from the Addiction Severity Index, 5th Edition (ASI). Specifically, the information on respondent's recent drug use history (30 days prior to the interview at baseline and 6 months) was also included with an emphasis on cocaine, heroin and alcohol. In addition to drug use, several measures of mental health were also included for all participants in the analysis: a measure of whether the subjects reported experiencing severe depression or anxiety in the 30 days leading up to the interview (baseline and 6 months) and whether the subject was diagnosed with bipolar disorder while incarcerated. In addition, the 12-item Short Form of the Medical Outcomes Study (SF-12) was used to assess health-related quality of life (HRQoL). Composite sub-scores from this instrument assessed physical and mental well-being as continuous variables and were included in the analysis for the two time periods that were assessed.
The enabling resources included health insurance status at the time of incarceration and food insecurity. Food insecurity was defined based on self-reported gaps in food consumption (longer than 2 days) in the 30 days prior to the baseline assessment and 6 month assessment.
Need factors often include measures of disease severity and health beliefs about illness. We, therefore, included substance abuse severity and active medical conditions among the covariates for the baseline as well as the 6 month follow-up period. To assess substance abuse severity, the ASI composite score for drugs was calculated based on the data on the consumption of heroin, cocaine, methadone, non-prescribed opiates, barbiturates, amphetamines, cannabis, hallucinogens, and multiple drugs, as well as subjects’ perceptions about importance of drug treatment and severity of the subject's addiction [32]. A cutoff of 0.12 was employed based on existing literature demonstrating 85 % sensitivity and 86 % specificity at this threshold [33]. Alcohol use severity was calculated from the ASI using a cutoff value of 0.15, based on literature demonstrating 86 % sensitivity and 80 % specificity associated with alcohol dependence [32–35]. The severity of mental illness was ascertained from the ASI psychiatric component and was analyzed as a dichotomous variable with a cutoff of 0.22 since this threshold previously was demonstrated to have 90 % specificity and 71 % sensitivity in identifying mental illness [32, 33, 35]. In addition, whether any psychiatric medications were prescribed in the 30 days leading up to the interview was included as a binary indicator. Other medical co-morbidities were based on self-report if the subject indicated that they had been diagnosed for the condition.
Indicators measuring re-incarceration, as reported in the first month following the release from jail as well as the six-month follow up, were used to monitor individuals who returned to jail. Other health outcomes assessed in our analysis included: whether the participant self-reported being on ART, and virologic suppression (<400 copies/mL). Adherence was measured using the visual analog scale [36] and high levels of adherence were defined as having taken 95 % or more of the doses in the 7 days prior to incarceration.
Statistical Methods
Missing Data
On average, less than 7 % of selected data missing at the baseline was also missing at the 6 months. In addition, approximately 33 % of the sample did not have a follow-up interview at 6 months. To address concerns about missing data, a series of multiple imputations were performed using a Markov Chain Monte Carlo (MCMC) simulation conditional on the variables that were observed. Our analysis showed that with 20 imputed data sets the relative efficiency attained was 99 %. We used Rubin's rules to combine the results from various imputations in each of our analyses [37].
While the Missing at Random (MAR) assumption cannot be tested directly [38], we performed sensitivity analysis by examining the performance of the models exhibiting departures from the MAR assumption. Overall, we can report that the results were robust and not sensitive to the MAR assumption. As a further assessment of robustness and an alternative to multiple imputation procedure, we estimated a series of Heckman's sample selection correction models and found that the key parameters in the Heckman's type models were poorly identified, allowing us not to report the results from these models.
Aim 1: Factors Associated with Homelessness
To assess the relationship between housing status and the selected covariates, several logistic regressions were estimated. First, we performed cross sectional analysis for each of the two assessments (i.e. baseline and 6 months) predicting the probability of being homeless as a function of the independent covariates at each of the time points. The covariates with a P ≤ 0.10 in the univariate analysis, as determined by the Wald test, were included in multivariate analysis. In addition, Akaike Information Criterion (AIC) were used to discriminate among the multivariate models. The χ2 test was used to assess the overall goodness-of-fit assessing the null hypothesis that the logistic model is not appropriate for these data.
Aim 2: Dynamic Transitions Between Homelessness & Housing
In the second part of the analysis we examined the association between the change in various covariates between the two time points (baseline and 6 months) and the transition to and from stable housing. Initially we restricted our sample to those individuals who were homeless at baseline, and estimated a logistic regression predicting the probability that the individuals were housed at six-months. Again, P values from the univariate model, and the AIC were used to select the final model specification. The χ2 test was used to assess the overall goodness-of-fit. Then we repeated the analysis for the sample which was housed at baseline and analyzed the transitions from stable housing in the same manner.
Aim 3: Counterfactual Analysis of the Effect of Housing on HIV-Care Outcomes
To assess the gap in the engagement in HIV-care among housed and homeless individuals, we employed a validated propensity score matching method [39], which has the advantage of allowing us to draw causal inference using observational studies [40–43]. In this case, we used the propensity score analysis to investigate the size and the scope of the difference in selected HIV treatment outcomes that were due to the differences in housing status. In the first step, we estimated the probability that each individual in our sample was homeless at baseline and at 6 months, using the model we identified for the first aim. Then we used the nearest-neighbor algorithm to match the individuals based on their propensity score and then computed the average difference among individuals in each of the four outcomes: access to HIV-care provider, receipt of ART, ≥95 % ART adherence, and virological suppression. We computed Abadie and Imbens standard errors, which are meant to correct for the shortcomings of the bootstrap method [44, 45]. We initially performed the analysis for baseline data, and then repeated the analysis using 6-month data. Last, we tested the sensitivity of the MAR assumption by using a conservative estimate of participation in the HIV care by replacing missing observations with negative (zero) outcomes. We also tested the sensitivity of the matching algorithm by using several methods such as nearest neighbor with calipher ([46]), Mahalanobis matching ([47, 48]) and a kernel based method ([49]). The results were robust and similar across the selected class of estimators. All statistical analyses were conducted using STATA v.12 [50].
Results
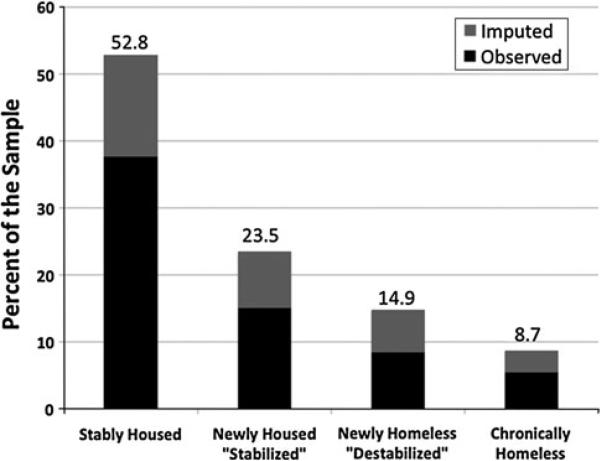
The baseline for all participant characteristics for those with baseline and 6-month data are provided in Table 1. Most subjects were male, black, unmarried, in their 40s, had not completed high school and were using cocaine in the 30 days prior to incarceration; 38 % of the respondents in the full sample (and 35 % of the individuals who had 6 months of data) were homeless at baseline. At six-month assessment, however, the percentage of homeless subjects declined to 21 %. After accounting for attrition, homelessness decreased among this population between preincarceration and 6 months post-release. The decline in homelessness resulted primarily because the number of individuals who became housed within 6 months is larger than the number of individuals who lost their housing within the same time period (Fig. 3).
Table 1.
Comparison of baseline demographic and risk behavior characteristics of HIV-infected jail detainees stratified by attrition status
| Characteristics | Total | Observed at 6 months* |
Unobserved at 6 months* |
P value | ||
|---|---|---|---|---|---|---|
| N = 867 |
N = 580 |
N = 287 |
||||
| N | % | N | % | |||
| Homeless status | 334 | 205 | 35.3 | 129 | 44.9 | <0.01 |
| Mean age (SD) | 42.9 | 43.7 | (8.3) | 41.5 | (9.6) | <0.01 |
| Gender | ||||||
| Male | 586 | 415 | 71.6 | 171 | 59.6 | <0.01 |
| Female | 281 | 165 | 28.4 | 116 | 40.4 | <0.01 |
| Race and ethnicity | ||||||
| Non-Hispanic White | 137 | 92 | 15.9 | 45 | 15.7 | 0.52 |
| Non-Hispanic Black | 504 | 326 | 56.2 | 178 | 62.8 | 0.87 |
| Hispanic | 203 | 151 | 26 | 52 | 18.1 | <0.01 |
| Other | 27 | 11 | 1.9 | 16 | 5.6 | <0.01 |
| Relationship status | ||||||
| In a stable relationship | 283 | 198 | 34.1 | 85 | 29.6 | 0.18 |
| Not in a relationship | 584 | 382 | 44.9 | 202 | 70.4 | <0.01 |
| Education | ||||||
| Less than high school | 443 | 283 | 48.8 | 160 | 55.7 | 0.05 |
| High school | 290 | 204 | 35.2 | 86 | 30 | 0.13 |
| Above high school | 134 | 93 | 16 | 41 | 14.3 | 0.5 |
| Food insecurity | 321 | 200 | 34.5 | 121 | 42.2 | 0.03 |
| Re-incarcerated | 256 | 226 | 39 | 30 | 10.5 | <0.001 |
| Engagement in HIV care | ||||||
| Usual HIV care provider | 642 | 464 | 80.0 | 178 | 62.02 | <0.01 |
| Prescribed ART (as % eligible) | 442 | 317 | 54.7 | 125 | 43.55 | <0.01 |
| 95 % adherence to ART (as % eligible) | 260 | 197 | 34.0 | 63 | 21.95 | <0.01 |
| Viral suppression (VL < 400) | 275 | 188 | 32.4 | 87 | 30.31 | <0.01 |
| Health insurance status | 649 | 467 | 80.2 | 182 | 63.4 | <0.01 |
| Co-morbidities | ||||||
| Depression/anxiety | 488 | 316 | 54.5 | 172 | 59.9 | 0.12 |
| Prescribed psychiatric medication | 221 | 151 | 26.0 | 70 | 24.4 | 0.60 |
| Bipolar disorder (diagnosed in jail) | 103 | 72 | 12.4 | 31 | 10.8 | 0.49 |
| Chronic Hepatitis C | 327 | 232 | 40.0 | 95 | 33.1 | 0.05 |
| Substance use in the 30 days pre-incarceration | ||||||
| Heroin | 232 | 161 | 27.8 | 71 | 24.7 | 0.34 |
| Cocaine | 465 | 298 | 51.4 | 167 | 58.2 | 0.06 |
| Alcohol | 250 | 159 | 27.4 | 91 | 31.7 | 0.19 |
| Addiction severity index | ||||||
| Drugs | 589 | 375 | 64.7 | 214 | 74.6 | 0.04 |
| Alcohol | 572 | 369 | 63.6 | 203 | 70.7 | 0.21 |
| Psychiatric | 463 | 301 | 51.9 | 162 | 56.4 | 0.17 |
| Quality of life—physical health: mean (SD) | 90.9 | 46.1 | (11.9) | 44.8 | (12.0) | 0.69 |
| Quality of life—mental health: mean (SD) | 80.7 | 40.2 | (12.3) | 40.5 | (12.8) | 0.55 |
| Services received | ||||||
| Housing coordinator | 274 | 202 | 34.8 | 72 | 25.1 | <0.01 |
| Sites (anonymous) | ||||||
| 1 | 62 | 34 | 5.9 | 28 | 9.8 | 0.04 |
| 2 | 44 | 20 | 3.4 | 24 | 8.4 | <0.01 |
| 3 | 324 | 226 | 39 | 98 | 34.1 | 0.17 |
| 4 | 58 | 37 | 6.4 | 21 | 7.3 | 0.61 |
| 5 | 37 | 25 | 4.3 | 12 | 4.2 | 0.93 |
| 6 | 56 | 51 | 8.8 | 5 | 1.7 | <0.01 |
| 7 | 77 | 38 | 6.6 | 39 | 13.6 | <0.01 |
| 8 | 66 | 41 | 7.1 | 25 | 8.7 | 0.39 |
| 9 | 81 | 56 | 9.7 | 25 | 8.7 | 0.65 |
| 10 | 62 | 52 | 9.0 | 10 | 3.5 | 0.03 |
The frequencies are based on actual data and estimates from a multiple imputation procedure
Observed at 6 months means the individuals had the 6 month interview, and unobserved means that they did not have the 6 month interview
Fig. 3.
Patterns of housing from baseline to 6 months after release from jail (N = 867) (Color figure online)
Aim 1: Factors Associated with Homelessness
A comparison among factors that were associated with homelessness across time reveals several patterns. First homeless individuals were more likely to report a lack of enabling resources such as health insurance, food availability and housing. Second, homeless individuals were more likely to be re-incarcerated after the release from jail. The analysis of enabling resources at the community level reveals that the average service utilization rate was approximately 38 % among homeless and non-homeless in the full sample. Homeless participants were no more likely to use the community-based services than the non-homeless. One notable exception, however, was appointments made with a housing coordinator. Clients who were homeless at baseline were more likely to meet with a housing coordinator within one month of release than non-homeless clients.
In addition homeless individuals were more likely to report active drug use, especially cocaine, and were more likely to report higher levels of drug and alcohol use severity. For example, the conditional odds of active cocaine use on being homeless are 66 % higher than the odds of a non-user being homeless at baseline and 173 % higher after 6 months.
In addition, homeless PLWHA are more likely to have mental illness, especially depression and anxiety. For example, the conditional odds of an individual with high psychiatric severity being homeless are almost 50 % higher than conditional odds of being homeless for an individual who has no psychiatric severity. The results indicate that the health outcomes and the quality of physical and mental scores among the homeless are worse than among the individuals who were housed at baseline and 6 months post-release (Table 2).
Table 2.
Factors associated with homelessness at baseline and 6 months post-release
| Covariates | Baseline (N = 867) |
6 months (N = 867) |
||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted |
Adjusted |
Unadjusted |
Adjusted |
|||||
| Odds ratio | (95 % CI) | Odds ratio | (95 % CI) | Odds ratio | (95 % CI) | Odds ratio | (95 % CI) | |
| Age | 0.98 | (0.96, 0.99) | * | 1.00 | (0.97, 1.02) | * | ||
| Gender | ||||||||
| Female | Referent | |||||||
| Male | 0.65 | (0.48, 0.87) | * | 0.84 | (0.56, 1.24) | * | ||
| Race | ||||||||
| Non-Hispanic White | Referent | * | ||||||
| Non-Hispanic Black | 1.19 | (0.79, 1.77) | * | 0.82 | (0.49, 1.35) | * | ||
| Hispanic | 0.85 | (0.53, 1.35) | * | 0.85 | (0.46, 1.56) | * | ||
| Other | 1.29 | (0.53, 3.10) | * | 1.37 | (0.41, 4.54) | * | ||
| Relationship status | ||||||||
| In a relationship | 0.67 | (0.49, 0.90) | * | 0.55 | (0.35, 0.83) | 0.40 | (0.23, 0.69) | |
| Not in a relationship | Referent | Referent | Referent | |||||
| Educational level completed | ||||||||
| Less than high school | 1.14 | (0.84, 1.55) | * | 1.34 | (0.87, 2.06) | * | ||
| High school | Referent | |||||||
| Above high school | 0.66 | (0.42, 1.02) | * | 0.97 | (0.54, 1.72) | * | ||
| Food insecurity | 6.50 | (4.77, 8.83) | 5.54 | (3.97, 7.73) | 6.40 | (3.81, 10.7) | 4.15 | (2.22, 7.74) |
| Reincarcerated | 1.23 | (0.91, 1.65) | * | 1.07 | (0.70, 1.62) | * | ||
| Health insurance status | 0.47 | (0.34, 0.64) | 0.53 | (0.35, 0.81) | 0.54 | (0.31, 0.92) | * | |
| Depression/anxiety (last 30 days) | 2.03 | (1.52, 2.70) | * | 5.11 | (3.25, 8.02) | * | ||
| On psychiatric medication (last 30 days) | 1.33 | (0.97, 1.81) | * | 1.53 | (0.99, 2.35) | * | ||
| Bipolar disorder | 1.68 | (1.11, 2.54) | * | 1.43 | (0.82, 2.47) | * | ||
| Chronic Hepatitis C | 0.97 | (0.73, 1.29) | * | 0.99 | (0.67, 1.46) | * | ||
| Heroin use (last 30 days) | 1.09 | (0.79, 1.48) | * | 2.64 | (1.48, 4.70) | * | ||
| Cocaine use (last 30 days) | 2.19 | (1.64, 2.91) | 1.66 | (1.18, 2.31) | 3.61 | (2.22, 5.87) | 2.73 | (1.48, 5.01) |
| Alcohol use (last 30 days) | 1.42 | (1.05, 1.92) | * | 2.71 | (1.63, 4.48) | * | ||
| Drug use severity | 2.30 | (1.66, 3.18) | * | 3.11 | (1.82, 5.31) | * | ||
| Alcohol use severity | 2.36 | (1.72, 3.23) | * | 2.45 | (1.54, 3.90) | * | ||
| Psychiatric severity | 2.11 | (1.58, 2.81) | 1.49 | (1.03, 2.15) | 3.78 | (2.48, 5.75) | 1.75 | (1.01, 3.00) |
| Quality of life—physical health | 0.98 | (0.97, 0.99) | 0.99 | (0.97, 1.00) | 0.98 | (0.96, 0.99) | * | |
| Quality of life—mental health | 0.97 | (0.96, 0.98) | * | 0.95 | (0.92, 0.96) | * | ||
| Sites (anonymous) | ||||||||
| 1 | Referent | |||||||
| 2 | 2.06 | (1.03, 4.10) | 1.11 | (0.50, 2.43) | 1.37 | (0.60, 3.10) | 1.22 | (0.50, 2.99) |
| 3 | 3.85 | (1.77, 8.36) | 2.27 | (0.89, 5.76) | 1.11 | (0.43, 2.85) | 1.21 | (0.42, 3.46) |
| 4 | 1.19 | (0.58, 2.44) | 1.22 | (0.53, 2.78) | 2.02 | (0.80, 5.10) | 1.66 | (0.61, 4.47) |
| 5 | 3.12 | (1.54, 6.31) | 2.32 | (1.04, 5.15) | 1.78 | (0.79, 4.02) | 1.35 | (0.52, 3.46) |
| 6 | 0.95 | (0.56, 1.62) | 1.28 | (0.69, 2.34) | 0.27 | (0.12, 0.59) | 0.44 | (0.18, 1.02) |
| 7 | 1.13 | (0.54, 2.34) | 0.77 | (0.34, 1.73) | 1.56 | (0.68, 3.57) | 1.40 | (0.55, 3.51) |
| 8 | 4.59 | (1.98, 10.5) | 3.69 | (1.42, 9.55) | 2.43 | (0.92, 6.42) | 1.85 | (0.58, 5.87) |
| 9 | 1.20 | (0.59, 2.40) | 0.71 | (0.31, 1.57) | 1.13 | (0.49, 2.55) | 0.90 | (0.37, 2.16) |
| 10 | 1.26 | (0.64, 2.44) | 0.84 | (0.39, 1.82) | 1.16 | (0.45, 2.98) | 0.62 | (0.20, 1.81) |
| P value from χ2-goodness-of-fit test (smallest) | 0.39 | 0.11 | ||||||
| AIC (median) | 947.50 | 766.50 | ||||||
Figures in bold are significant at 5 % level
Variables excluded from the final multivariate model based on best-fit AIC
Aim 2: Dynamic Transitions Between Homelessness & Housing
The analysis of homelessness dynamics provides important insights into factors that contribute to stabilization of the lives of PLWHA (Table 3). Improvements in the enabling resources such as provision of basic needs, access to food, substance abuse treatment and health insurance are associated with increased likelihood of homeless individuals finding stable housing within 6 months of post release. While improvements in drug use severity, especially decreases in heroin and cocaine use, are significantly associated with transitions into stable housing, the associations do not remain as robust after controlling for other independent variables.
Table 3.
Factors associated with a transition from homelessness to new housing within 6 months (N = 331)
| Covariates | Unadjusted |
Adjusted |
||
|---|---|---|---|---|
| Odds ratio | (95 % CI) | Odds ratio | (95 % CI) | |
| Food insecurity: went for >2 days without food | ||||
| Never: no at baseline, no at 6 months | 7.24 | (2.94, 17.8) | 4.54 | (1.88, 10.9) |
| Improvement: yes at baseline, no at 6 months | 9.39 | (3.78, 23.3) | 5.86 | (2.34, 14.6) |
| Deterioration: no at baseline; yes at 6 months | 2.20 | (0.45, 10.5) | Referent | |
| Persistent: yes at baseline, yes at 6 months | Referent | Referent | ||
| Alcohol use (30 days prior to the interview) | ||||
| Never: no at baseline, no at 6 months | 3.83 | (1.38, 10.5) | 2.92 | (1.30, 6.53) |
| Improvement: yes at baseline, no at 6 months | 3.62 | (1.11, 11.7) | 2.39 | (0.87, 6.60) |
| Deterioration: no at baseline; yes at 6 months | 0.86 | (0.18, 3.99) | Referent | |
| Persistent: yes at baseline, yes at 6 months | Referent | Referent | ||
| Cocaine use (30 days prior to the interview) | ||||
| Never: no at baseline, no at 6 months | 3.74 | (1.68, 8.29) | * | |
| Improvement: yes at baseline, no at 6 months | 3.96 | (1.89, 8.30) | * | |
| Deterioration: no at baseline; yes at 6 months | 1.29 | (0.40, 4.09) | * | |
| Persistent: yes at baseline, yes at 6 months | Referent | * | ||
| Heroin use (30 days prior to the interview) | ||||
| Never: no at baseline, no at 6 months | 2.17 | (0.79, 5.89) | * | |
| Improvement: yes at baseline, no at 6 months | 3.53 | (1.14, 10.9) | * | |
| Deterioration: no at baseline; yes at 6 months | 0.45 | (0.06, 3.05) | * | |
| Persistent: yes at baseline, yes at 6 months | Referent | * | ||
| Depression (30 days prior to the interview) | ||||
| Never: no at baseline, no at 6 months | 2.72 | (1.32, 5.57) | Referent | |
| Improvement: yes at baseline, no at 6 months | 3.67 | (1.51, 8.85) | 1.89 | (0.80, 4.42) |
| Deterioration: no at baseline; yes at 6 months | 0.47 | (0.17, 1.25) | Referent | |
| Persistent: yes at baseline, yes at 6 months | Referent | Referent | ||
| Drug use severity (above a specified threshold) | ||||
| Never: no at baseline, no at 6 months | 2.08 | (0.98, 4.38) | Referent | |
| Improvement: yes at baseline, no at 6 months | 3.04 | (1.48, 6.21) | 1.60 | (0.77, 3.30) |
| Deterioration: no at baseline; yes at 6 months | 0.65 | (0.16, 2.49) | Referent | |
| Persistent: yes at baseline, yes at 6 months | Referent | Referent | ||
| Alcohol use severity (above a specified threshold) | ||||
| Never: no at baseline, no at 6 months | 4.28 | (1.78, 10.2) | * | |
| Improvement: yes at baseline, no at 6 months | 2.26 | (1.24, 4.09) | * | |
| Deterioration: no at baseline; yes at 6 months | 1.77 | (0.50, 6.28) | * | |
| Persistent: yes at baseline, yes at 6 months | Referent | * | ||
| Psychiatric severity (above a specified threshold) | ||||
| Never: no at baseline, no at 6 months | 2.92 | (1.49, 5.70) | * | |
| Improvement: yes at baseline, no at 6 months | 2.18 | (1.06, 4.46) | * | |
| Deterioration: no at baseline; yes at 6 months | 0.92 | (0.35, 2.37) | * | |
| Persistent: yes at baseline, yes at 6 months | Referent | * | ||
| Health insurance status | ||||
| Never: no at baseline, no at 6 months | Referent | Referent | ||
| Improvement: no at baseline; yes at 6 months | 1.46 | (0.51, 4.17) | Referent | |
| Deterioration: yes at baseline, no at 6 months | 2.31 | (0.55, 9.55) | Referent | |
| Persistent: yes at baseline, yes at 6 months | 2.83 | (1.10, 7.21) | 1.63 | (0.80, 3.30) |
| AIC (median) | 376.40 | |||
| P value from χ2-goodness of fit test (median) | 0.27 | |||
Figures in bold are significant at P < 0.05
Variables excluded from the final multivariate model based on the AIC criteria
The analysis also reveals that those individuals who were more likely to continue using cocaine and heroin and were more likely to experience deteriorations in their mental health after being released from jail were also more likely to have lost their housing and experienced “destabilization” after jail release (Table 4).
Table 4.
Factors associated with a housing destabilization within 6 months (N = 536)
| Covariates | Unadjusted |
Adjusted |
||
|---|---|---|---|---|
| Odds ratio | (95 % CI) | Odds ratio | (95 % CI) | |
| Food insecurity: went for >2 days without food | ||||
| Never: no at baseline, no at 6 months | Referent | Referent | ||
| Improvement: yes at baseline, no at 6 months | 1.85 | (0.86, 3.93) | Referent | |
| Deterioration: no at baseline; yes at 6 months | 7.45 | (3.42, 16.2) | 3.47 | (1.44, 8.37) |
| Persistent: yes at baseline, yes at 6 months | 4.40 | (1.36, 14.2) | 2.01 | (0.54, 7.48) |
| Alcohol use (30 days prior to the interview) | ||||
| Never: no at baseline, no at 6 months | Referent | * | ||
| Improvement: yes at baseline, no at 6 months | 0.94 | (0.43, 2.02) | * | |
| Deterioration: no at baseline; yes at 6 months | 2.47 | (0.81, 7.45) | * | |
| Persistent: yes at baseline, yes at 6 months | 1.93 | (0.68, 5.43) | * | |
| Cocaine use (30 days prior to the interview) | ||||
| Never: no at baseline, no at 6 months | Referent | Referent | ||
| Improvement: yes at baseline, no at 6 months | 1.04 | (0.49, 2.17) | Referent | |
| Deterioration: no at baseline; yes at 6 months | 2.39 | (0.77, 7.38) | Referent | |
| Persistent: yes at baseline, yes at 6 months | 4.01 | (1.80, 8.91) | 3.06 | (1.30, 7.21) |
| Heroin use (30 days prior to the interview) | ||||
| Never: no at baseline, no at 6 months | Referent | * | ||
| Improvement: yes at baseline, no at 6 months | 0.58 | (0.23, 1.45) | * | |
| Deterioration: no at baseline; yes at 6 months | 2.59 | (0.75, 8.85) | * | |
| Persistent: yes at baseline, yes at 6 months | 2.69 | (1.07, 6.69) | * | |
| Depression (30 days prior to the interview) | ||||
| Never: no at baseline, no at 6 months | Referent | Referent | ||
| Improvement: yes at baseline, no at 6 months | 1.13 | (0.34, 3.66) | Referent | |
| Deterioration: no at baseline; yes at 6 months | 7.69 | (2.56, 23.0) | 5.37 | (1.91, 15.1) |
| Persistent: yes at baseline, yes at 6 months | 5.39 | (2.40, 12.1) | 3.99 | (1.95, 8.14) |
| Drug use severity (above a specified threshold) | ||||
| Never: no at baseline, no at 6 months | Referent | * | ||
| Improvement: yes at baseline, no at 6 months | 0.90 | (0.38, 2.10) | * | |
| Deterioration: no at baseline; yes at 6 months | 2.91 | (0.73, 11.5) | * | |
| Persistent: yes at baseline, yes at 6 months | 2.73 | (1.30, 5.71) | * | |
| Alcohol use severity (above a specified threshold) | ||||
| Never: no at baseline, no at 6 months | Referent | * | ||
| Improvement: yes at baseline, no at 6 months | 1.02 | (0.49, 2.09) | * | |
| Deterioration: no at baseline; yes at 6 months | 1.32 | (0.33, 5.12) | * | |
| Persistent: yes at baseline, yes at 6 months | 2.07 | (0.90, 4.72) | * | |
| Psychiatric severity (above a specified threshold) | ||||
| Never: no at baseline, no at 6 months | Referent | * | ||
| Improvement: yes at baseline, no at 6 months | 2.22 | (0.85, 5.73) | * | |
| Deterioration: no at baseline; yes at 6 months | 5.57 | (2.09, 14.7) | * | |
| Persistent: yes at baseline, yes at 6 months | 4.33 | (2.07, 9.03) | * | |
| Health insurance status | ||||
| Never: no at baseline, no at 6 months | 2.10 | (0.812, 5.36) | * | |
| Improvement: no at baseline; yes at 6 months | 1.67 | (0.50, 5.62) | * | |
| Deterioration: yes at baseline, no at 6 months | 2.89 | (1.15, 7.23) | * | |
| Persistent: yes at baseline, yes at 6 months | Referent | * | ||
| AIC (median) | 378.40 | |||
| P value from χ2-goodness of fit test (Median) | 0.40 | |||
Figures in bold are significant at 5 % level
Variables excluded from the final multivariate model based on the AIC criteria
Aim 3: Counterfactual Analysis of the Effect of Housing on HIV-Care Outcomes
Propensity score matching indicated that housing status had a significant effect on engagement in HIV treatment at the baseline and after 6 months. Based on potential outcomes framework, we estimated in Table 5 that individuals experiencing homelessness were less likely to have been engaged in HIV care as measured by (1) having an HIV care provider (2) take any ART in the past week and (3) achieving ≥95 % ART adherence. The effect was particularly strong in the baseline sample, and was not statistically significant in the 6 month data.
Table 5.
Counterfactual analysis of the effect of homelessness on HIV treatment outcomes
| Outcomes | Baseline |
6 months |
||||||
|---|---|---|---|---|---|---|---|---|
| Inferred outcome if all individuals were housed (%) | Inferred Outcome if all individuals were homeless (%) | Average difference in outcome due to housinga (%) | P value | Inferred outcome if all individuals were housed (%) | Inferred outcome if all individuals were homeless (%) | Average difference in outcome due to housinga (%) | P value | |
| Usual HIV care provider | 78.6 | 66.2 | 12.3 | 0.02 | 87.8 | 85.8 | 2.0 | 0.881 |
| Receipt of ART | 57.9 | 46.0 | 12.0 | 0.02 | 77.6 | 69.0 | 8.6 | 0.129 |
| High (>95 %) ART adherence | 35.0 | 25.2 | 9.9 | 0.04 | 51.2 | 43.0 | 8.2 | 0.224 |
| Viral suppression | 33.4 | 27.3 | 6.1 | 0.23 | 56.6 | 41.0 | 15.6 | 0.03 |
In the program evaluation literature this is also known as the “Average Treatment Effect”
*Figures in bold are significant at 5 % level
While there were no significant average differences in the inferred probability of virological suppression at the baseline, by 6 months we estimated that average difference in virological suppression between homeless and housed was as high as 15.6 % (56.6 % vs. 41.0 %). Once we controlled for attrition, the percent of individuals who were virologically suppressed increased in the entire sample, yet the results indicate that housed individuals were able to attain virological suppression in larger frequencies than individuals who experienced homelessness in the post-release period. Additional simulations indicated that the gap in HIV treatment outcomes of homeless and housed individuals was neither sensitive to the missing data assumption nor to the choice of matching algorithm.
Discussion
In this large, multisite study of released HIV-infected jail detainees, homelessness is common and dynamic. Though dynamic, transition to and from homelessness following incarceration was associated with a complex array of interrelated factors, including mental illness, recurrent drug use and availability of basic needs. The multifaceted interactions between homelessness and incarceration present critical challenges for engagement in HIV care and persistence in HIV treatment. In this sample, high levels of addiction severity, drug use itself, and psychiatric disorders were strongly correlated with homelessness, suggesting a particular need for diagnosing, treating and ensuring continuity of treatment along with provision of additional social support for PLWHA after release from jail. The findings confirm those from the pre-incarceration period from this same cohort, suggesting that services should be initiated and continued from the time of entry into jail and maintained continuously thereafter [5].
HRQoL for both physical and mental well-being was significantly worse for the homeless. The high prevalence of depression and psychiatric disorders among the homeless population underscores the importance of diagnosis and treatment. Treatment of mental illness has been demonstrated to improve retention in care and HIV outcomes in other settings and it stands to reason that it would hold true for this population as well [26]. Moreover, for newly housed participants, the levels of depression, anxiety, and psychiatric severity improved over time, while those who lost housing (became destabilized), experienced deterioration in their depression and heightened psychiatric severity. This suggests that the housing status and psychiatric health may be interrelated and reinforce each other.
The correlations between the improvements of food security, health insurance and homelessness underscore the importance of addressing basic needs first, since these appear to be prerequisite to attaining higher needs, like engagement in HIV care, that often complicate the lives of destabilized persons transitioning from jail. These findings therefore lend empirical support to the theory of hierarchy of needs [51]. Struggles with food insecurity and lack of housing have been shown to interfere with linkages to services and continuity of care [30].
We found evidence that homeless individuals are less likely to have an usual HIV provider, less likely to be prescribed ART, and after 6 months, are less likely to be virally suppressed than individuals who are fully housed. The implication of the gap in HIV treatment engagement suggests that the vulnerability of the homeless individuals translates into inferior outcomes in the longer run, and even though the full sample has improvements in HIV care engagement over time, the improvements are not uniformly distributed between homeless and housed individuals. Findings here for the post-release period highlight the importance of providing a number of critical enabling resources to the vulnerable population of homeless individuals to ensure continuity of care.
The analysis of transitions from homelessness to housing reveals that SUDs, chronic and relapsing conditions, are closely associated with chronic homelessness. In this case, reducing substance use relapse itself and lowering addiction severity is directly correlated with reductions in homelessness. According to our findings, those individuals who reduce their consumption of heroin and cocaine are more likely to transition out of chronic homelessness while those who relapse back to drug use are more likely to remain chronically homeless. These results highlight the crucial role of evidence-based drug treatment for PLWHA in jails. Moreover, it lends empirical support for the effective treatment of alcohol use disorders as part of a transitional plan [52]. In the case of individuals with opioid or alcohol dependence, the use of medication-assisted therapies, such as methadone, buprenorphine or extended release naltrexone may be used for treating opioid dependence [6, 7, 22] and extended-release naltrexone for alcohol use disorders [53] may provide benefit. The fact that a complex array of factors were associated with homelessness reinforces the need to create and test multifaceted interventions in order to achieve optimal outcomes.
Linkage services play an important role in the retention and participation of clients in the health care system and ART adherence. Our finding of poor engagement in HIV and other treatment services and high attrition rates from care, implies that the existing post-release array of community services, primarily case management, has considerable room for improvement.
There remain several limitations to this longitudinal study. First, given the non-random sample in the observational study, the causal pathways between variables are challenging, as the causal relationships likely run in several directions and may be related to unobserved heterogeneity. For example, the individuals who experience depression and have SUDs may not be able to find housing or work because of the lack of financial resources (e.g. first and last month's rent) and prevailing barriers to meaningful employment due to criminal record. This may in turn compound worsened sense of despair, depression and anxiety, which negatively influence motivation for seeking stable housing.
The measure of homelessness, which is based on self-report is itself problematic for several reasons. First of all, the measure might be underestimating the number of individuals experiencing homelessness in the 6-month interval, since the question only addresses the 30 days prior to the interview. The analysis of the variable based on the housing needs identified by the case manager reveals that nearly 44 % of those individuals who were “non-homeless” at baseline, identified a need for housing within one month of release, while 55 % of homeless individuals did not reveal a need for the housing. This suggests that the homeless status could be measured with error and, as a result, lead to a bias in our estimates.
Another limitation is that modeling propensity scores can only account for observed covariates. Unobserved factors that may influence homelessness are not accounted for in the matching procedure. Even though our sample is large enough and the overlap between “treatment” and “control” groups are significant, there may still be hidden bias due to unobserved heterogeneity.
Despite these limitations, the EnhanceLink evaluation provides crucial insight into what is needed to improve outcomes of some of the most medically and socially vulnerable individuals in society—PLWHA who are transitioning from jail. In order to achieve parity for these individuals, a complex array of services are needed, including stable housing, to optimize HIV treatment outcomes. Such interventions have the high likelihood to improve health and well-being for the individual, but to additionally improve outcomes for society.
Conclusions
The vulnerability of the released PLWHA transitioning from jail is particularly acute and complex, as such individuals must overcome a myriad of social, health and economic problems including homelessness, substance abuse, mental illness, declining physical HRQoL and unmet basic needs. Addressing fundamental housing needs is an essential factor in promoting HIV treatment adherence and positive outcomes among this population.
Acknowledgments
Enhancing Linkages to HIV Primary Care Services Initiative is a HRSA-funded Special Project of National Significance. Funding for this research was also provided through career development grants from the National Institute on Drug Abuse (K24 DA017072, FLA), research grants from the National Institute on Alcohol Abuse and Alcoholism (R01 AA018944, FLA). Assistance was also provided by Emory Center for AIDS Research (CFAR, P30 AI050409, ACS). The funding sources played no role in study design, data collection, data analysis, data interpretation, writing of the manuscript or the decision to submit the paper for publication.
Contributor Information
Alexei Zelenev, Section of Infectious Diseases, AIDS Program, Department of Internal Medicine, Yale University School of Medicine, 135 College Street, Suite 323, New Haven, CT 06510, USA.
Ruthanne Marcus, Section of Infectious Diseases, AIDS Program, Department of Internal Medicine, Yale University School of Medicine, 135 College Street, Suite 323, New Haven, CT 06510, USA.
Artem Kopelev, Section of Infectious Diseases, AIDS Program, Department of Internal Medicine, Yale University School of Medicine, 135 College Street, Suite 323, New Haven, CT 06510, USA.
Jacqueline Cruzado-Quinones, New York City Department of Public Health, New York, NY, USA.
Anne Spaulding, Emory University, Atlanta, GA, USA.
Maureen Desabrais, Baystate Medical Center, Springfield, MA, USA Maureen.Desabrais@baystatehealth.org.
Tom Lincoln, Baystate Medical Center and Tufts University School of Medicine, Springfield, MA, USA Thomas.Lincoln@bhs.org.
Frederick L. Altice, Section of Infectious Diseases, AIDS Program, Department of Internal Medicine, Yale University School of Medicine, 135 College Street, Suite 323, New Haven, CT 06510, USA Yale University School of Public Health, New Haven, CT, USA, frederick.altice@yale.edu.
References
- 1.Maru DS, Basu S, Altice FL. HIV control efforts should directly address incarceration. Lancet Infect Dis. 2007;7(9):568–9. doi: 10.1016/S1473-3099(07)70190-1. [DOI] [PubMed] [Google Scholar]
- 2.Wallace R. Social disintegration and the spread of AIDS—II. Meltdown of sociogeographic structure in urban minority neighborhoods. Soc Sci Med. 1993;37:887–96. doi: 10.1016/0277-9536(93)90143-r. [DOI] [PubMed] [Google Scholar]
- 3.Wallace RG. AIDS in the HAART era: New York's heterogeneous geography. Soc Sci Med. 2003;56(6):1155–71. doi: 10.1016/s0277-9536(02)00121-1. [DOI] [PubMed] [Google Scholar]
- 4.Thomas JC. From slavery to incarceration: social forces affecting the epidemiology of sexually transmitted diseases in the rural South. Sex Transm Dis. 2006;33(Suppl 7):S6–10. doi: 10.1097/01.olq.0000221025.17158.26. [DOI] [PubMed] [Google Scholar]
- 5.Chen NE, Meyer JP, Avery AK, Draine J, Flanigan TP, Lincoln T, Spaulding AC, Springer SA, Altice FL. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS Behav. 2011 doi: 10.1007/s10461-011-0080-2. doi:10.1007/s10461-011-0080-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications of adequate transitional care for HIV-infected prisoners: five essential components. Clin Infect Dis. 2011;53(5):469–79. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Fried-land GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):59–79. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harrison LD, Harrison LD. The revolving prison door for drug-involved off enders: challenges and opportunities. Crime Delinq. 2001;47:462–85. [Google Scholar]
- 9.Hopper K. Reckoning with homelessness. Cornell University Press; Ithaca: 2002. [Google Scholar]
- 10.Metraux S, Metzger DS, Culhane DP. Homelessness and HIV risk behaviors among injection drug users. J Urban Health. 2004;81(4):618–29. doi: 10.1093/jurban/jth145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang SW, Kirst MJ, Chiu S, Tolomiczenko G, Kiss A, Cowan L, et al. Multidimensional social support and the health of homeless individuals. J Urban Health. 2009;86(5):791–803. doi: 10.1007/s11524-009-9388-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of antiretroviral therapy among HIV-infected prisoners: reincarceration and the lack of sustained benefit after release to the community. Clin Infect Dis. 2004;38(12):1754–60. doi: 10.1086/421392. [DOI] [PubMed] [Google Scholar]
- 13.Pai NP, Estes M, Moodie EE, Reingold AL, Tulsky JP. The impact of antiretroviral therapy in a cohort of HIV infected patients going in and out of the San Francisco county jail. PLoS ONE. 2009;4(9):e7115. doi: 10.1371/journal.pone.0007115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Courtenay-Quirk C, Pals SL, Kidder DP, Henny K, Emshoff JG. Factors associated with incarceration history among HIV-positive persons experiencing homelessness or imminent risk of homelessness. J Community Health. 2008;33(6):434–43. doi: 10.1007/s10900-008-9115-7. [DOI] [PubMed] [Google Scholar]
- 16.Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving doors: imprisonment among the homeless and marginally housed population. Am J Public Health. 2005;95(10):1747–52. doi: 10.2105/AJPH.2005.065094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Metraux S, Caterina R, Cho R. Incarceration and homelessness. In: Dennis D, Locke G, Khadduri L, editors. Toward understanding homelessness: the 2007 national symposium on homelessness research. US Department of Housing & Urban Development; Washington, DC: 2008. [Google Scholar]
- 18.Kidder DP, Wolitski RJ, Campsmith ML, Nakamura GV. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007;97(12):2238–45. doi: 10.2105/AJPH.2006.090209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwarcz SK, Hsu LC, Vittinghoff E, Vu A, Bamberger JD, Katz MH. Impact of housing on the survival of persons with AIDS. BMC Public Health. 2009;9:220. doi: 10.1186/1471-2458-9-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolitski RJ, Kidder DP, Pals SL, Royal S, Aidala A, Stall R, Holtgrave DR, Harre D, Courtenay-Quirk C. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493–503. doi: 10.1007/s10461-009-9643-x. [DOI] [PubMed] [Google Scholar]
- 21.Baillargeon J, Giordano TP, Rich JD, Wu ZH, Wells K, Pollock BH, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–57. doi: 10.1001/jama.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Springer SA, Chen S, Altice FL. Improved HIV and Substance abuse treatment outcomes for released HIV-infected prisoners: the impact of buprenorphine treatment. J Urban Health. 2010;87(4):592–602. doi: 10.1007/s11524-010-9438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Milaney KP. The 6 dimensions of promising practice for case managed supports to end homelessness, part 1: contextualizing case management for ending homelessness. Prof Case Manag. 2011;16(6):281–7. doi: 10.1097/NCM.0b013e31821ee840. [DOI] [PubMed] [Google Scholar]
- 24.Tull T. The source. Vol. 13. University of California; The National Abandoned Infants Assistance Resource Center; Berkeley: 2004. The “housing first” approach for families affected by substance abuse. [Google Scholar]
- 25.Wang EA, Hong CS, Samuels L, Shavit S, Sanders R, Kushel MB. Transitions clinic: creating a community-based model of health care for recently released California prisoners. Public Health Rep. 2010;125:171–177. doi: 10.1177/003335491012500205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–302. [PMC free article] [PubMed] [Google Scholar]
- 27.Draine J, Ahuja D, Altice FL, Arriola KJ, Avery AK, Beckwith KG, et al. Strategies to enhance linkages between care for HIV/ AIDS in jail and community settings. AIDS Care. 2011;23(3):366–77. doi: 10.1080/09540121.2010.507738. [DOI] [PubMed] [Google Scholar]
- 28.Althoff AL, Zelenev A, Meyer JP, Fu J, Brown SE, Vagenas P, Avery AK, Cruzado-Quiñones J, Spaulding AC, Altice FL. Correlates of retention in HIV care after release from jail: results from a multi-site study. AIDS Behav. 2012 doi: 10.1007/s10461-012-0372-1. doi:10.1007/s10461-012-0372-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krishnan A, Wickersham JA, Chitsaz E, Springer SA, Jordan AO, Zaller N, Altice FL. Post-release substance abuse outcomes among HIV-infected jail detainees: results from a multisite study. AIDS Behav. 2012 doi: 10.1007/s10461-012-0362-3. doi:10.1007/s10461-012-0362-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–20. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 32.McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, Carise D. The addiction severity index at 25: origins, contributions and transitions. Am J Addict. 2006;15(2):113–24. doi: 10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- 33.Rikoon SH, Cacciola JS, Carise D, Alterman AI, McLellan AT. Predicting DSM-IV dependence diagnoses from Addiction Severity Index composite scores. J Subst Abuse Treat. 2006;31(1):17–24. doi: 10.1016/j.jsat.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 34.McLellan AT, Luborsky L, Woody GE, O'Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. J Nerv Ment Dis. 1980;168(1):26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Calsyn DA, Saxon AJ, Bush KR, Howell DN, Baer JS, Sloan KL, et al. The Addiction Severity Index medical and psychiatric composite scores measure similar domains as the SF-36 in substance-dependent veterans: concurrent and discriminant validity. Drug Alcohol Depend. 2004;76(2):165–71. doi: 10.1016/j.drugalcdep.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 36.Giordano TP, Guzman D, Clark R, Charlebois ED, Bangsberg DR. Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clin Trials. 2004;5(2):74–9. doi: 10.1310/JFXH-G3X2-EYM6-D6UG. [DOI] [PubMed] [Google Scholar]
- 37.Rubin D. Multiple imputation for non-response in surveys. Wiley; New York: 1987. [Google Scholar]
- 38.Jaeger M. Machine learning: ECML 2006, No. 4212. Springer; Berlin: 2006. On testing the missing at random assumption. [Google Scholar]
- 39.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41. [Google Scholar]
- 40.Wooldridge JM. Econometric analysis of cross section and panel data. MIT Press; Cambridge: 2002. [Google Scholar]
- 41.Guo S, Fraser M. Propensity score analysis: statistical methods and applications. Sage; Thousand Oaks: 2009. [Google Scholar]
- 42.Rubin DB. Estimating causal effects of treatments in randomized and nonrandomized studies. J Educ Psychol. 1974;66(5):688–701. [Google Scholar]
- 43.Rubin DB. Direct and indirect causal effects via potential outcomes. Scand J Stat. 2004;31(2):161–70. [Google Scholar]
- 44.Abadie A, Imbens G. On the failure of the bootstrap for matching estimators. Econometrica. 2008;76(6):1537–57. [Google Scholar]
- 45.Abadie A, Imbens G. Large sample properties of matching estimators for average treatment effects. Econometrica. 2006;74:235–67. [Google Scholar]
- 46.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33–8. [Google Scholar]
- 47.Rubin DB. Matching methods that are equal percent bias reducing: some examples. Biometrics. 1976;32:109–20. [Google Scholar]
- 48.Cochran W, Rubin D. Controlling bias in observational studies. Sankhyā. 1973;35:417–46. [Google Scholar]
- 49.Heckman J, Ichimura H, Todd P. Matching as an econometric evaluation estimator. Rev Econ Stud. 1998;65(2):261–94. [Google Scholar]
- 50.Stata: Release 12. [Computer program] StataCorp LP.; College Station, TX: 2011. [Google Scholar]
- 51.Maslow AH. Toward a psychology of being. 3rd ed. Wiley; New York: 1998. [Google Scholar]
- 52.Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2011;112(3):178–93. doi: 10.1016/j.drugalcdep.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Springer SA, Azar MM, Altice FL. HIV, alcohol dependence, and the criminal justice system: a review and call for evidence-based treatment for released prisoners. Am J Drug Alcohol Abuse. 2011;37(1):12–21. doi: 10.3109/00952990.2010.540280. [DOI] [PMC free article] [PubMed] [Google Scholar]