At a community hospital, 225 male and female patients, aged 38 to 90 years, undergoing elective total hip or knee replacement were randomly assigned to 1 of 3 groups (75 patients in each): “M” technique (M, a registered method of structured touch), guided imagery, or usual care. M showed the largest predicted decreases in both pain and anxiety between groups. There was no significant difference in narcotic pain medication use between groups. Patient satisfaction survey ratings were highest for M, followed by guided imagery.
Abstract
Context:
Postoperative management of pain after total joint arthroplasty remains a challenge despite advancements in analgesics. Evidence shows that complementary modalities with mind-body and tactile-based approaches are valid and effective adjuncts to reduce pain and anxiety postoperatively.
Objective:
To investigate the effectiveness of the “M” Technique (M), a registered method of structured touch using a set sequence and number of strokes, and a consistent level of pressure on hands and feet, compared with guided imagery and usual care, for the reduction of pain and anxiety in patients undergoing elective total knee or hip replacement surgery.
Methods:
Randomized controlled trial: M-TIJRP (MiTechnique and guided Imagery in Joint Replacement Patients [Mighty Junior P]). At a community hospital, 225 male and female patients, aged 38 to 90 years, undergoing elective total hip or knee replacement were randomly assigned to 1 of 3 groups (75 patients in each): M, guided imagery, or usual care. They were blinded to their assignment until the intervention.
Main Outcome Measures:
Reduction of pain and anxiety postoperatively. Secondary outcomes measured use of pain medication and patient satisfaction.
Results:
This study yielded positive findings for the management of pain and anxiety in patients undergoing elective joint replacement using M and guided imagery for 18 to 20 minutes compared with usual care. M showed the largest predicted decreases in both pain and anxiety between groups. There was no significant difference in narcotic pain medication use between groups. Patient satisfaction survey ratings were highest for M, followed by guided imagery.
Conclusion:
The benefit of M may be because of the specifically structured sequence of touch by competent caring, trained providers.
INTRODUCTION
Knee and hip arthroplasty causes patients to experience physical and emotional discomfort, most notably pain and anxiety. Joint arthroplasty is associated with substantial postoperative acute pain which, if uncontrolled, decreases early rehabilitation and long-term joint function.1
Patients facing surgery experience a disarray of emotion and a lack of feeling of control. The anxiety and pain experienced is associated with multi-system dysfunction, including altered cardiovascular-, neurosympathetic-, and endocrine-based responses. The anxiety experienced by patients affects respirations, pulse, and systolic blood pressure2 during the perioperative process, which may have a negative impact on recovery. Anxiety can slow the recovery process and has been found to be the only significant predictor of pain among patients undergoing total joint arthroplasty.3
Dalury et al4 wrote, “Failure to adequately control pain following total knee replacement induces pathophysiologic responses, which increase postoperative morbidity, hinder physiotherapy, increase anxiety, disrupt sleep patterns, and in general, decrease patient satisfaction and recovery.” According to the Joint Commission, pain is considered to be the “fifth vital sign” and adequate pain control is a “right” for all patients.4
Pellino and colleagues5 found that the postoperative use of nonpharmacologic measures resulted in the use of less opioid medication on postoperative Days 1 and 2, and patients showed a tendency for less anxiety compared with the usual care group. As perioperative analgesia shifts to integrate the use of complementary therapies into conventional practices, more physicians and nurses are becoming acquainted with various integrative approaches to preemptive analgesia, which have a positive effect in easing the recovery process.
The “M” Technique (M) is a registered method of structured touch created by Jane Buckle, PhD,6,7 who describes it as a series of gentle, slow, stroking movements done in a set sequence that causes the person being touched (receiver) to experience a greater sense of relaxation. The focus on repetitive sequences signals select areas of the brain, resulting in anxiety reduction and induction of prolonged relaxation.6 This gentle touch technique was developed for critically ill, fragile, or dying individuals, making it a valuable intervention in hospital and hospice settings. The level of pressure was confirmed by patients as a 3,7 with 10 being the deepest pressure.
In contrast to M, traditional massage, including light and rhythmic massage, provides no definition of pressure and aims to enhance blood and lymph flow. The anthropomorphic approach, including but not limited to rhythmic massage, complements the innate healing of the body using different hand techniques for different parts of the body to achieve different outcomes—without a clearly defined universal approach. M distinguishes itself from other massage techniques by using structured touch performed in a set pattern, sequence, and speed that never changes while involving the receiver in determining a consistent level of pressure.
Guided imagery describes any of various mind-focused techniques ranging from visualization and direct imagery-based suggestion through metaphor and storytelling. It affects almost all major physiologic control systems of the body, including respiration, heart rate, and blood pressure.8 Guided imagery has been shown to be an effective intervention for the reduction of anxiety and pain in surgical patients, also resulting in the decreased use of narcotic medications,9–11 which in one study was a decrease of nearly 50%.9 Antall and Kresevic10 note that guided imagery creates feelings of empowerment and relaxation, decreases anxiety and pain, increases endorphins, decreases blood loss, and decreases the use of pain medications in patients undergoing coronary artery bypass graft. A positive influence was also noted on recovery outcomes, pain, psychological well-being and patient satisfaction, distress, and length of stay.10 A study performed in patients undergoing total joint arthroplasty found guided imagery decreased levels of anxiety and pain at each time; however, the findings did not achieve overall significance between the groups.1
Guided imagery affects the autonomic balance of the body by refocusing the mind, resulting in physiologic relaxation by lowering sympathetic and increasing parasympathetic nervous system response through neurochemical and peptide changes. This intervention through a created vision of healing and relaxation is personalized, having an influence on emotions and effects on the limbic system and neuroendocrine axis. According to Gonzales and colleagues,12 “These connections between emotions and the modulation of pain support the theory that higher anxiety may affect an individual’s perception and coping with the pain experience.”
The authors of this study present the results of the “M” Technique, Guided Imagery, or Usual Care on Anxiety and Pain Pre- & Post-operatively in Elective Joint Replacement Patients” (M-TIJRP) study (ClinicalTrials.gov Identifier NCT01874379).12 On the basis of a literature review and the needs of patients undergoing elective hip and knee replacement surgery, the authors investigated the following hypotheses as primary and secondary outcome measures:
M and guided imagery would have an impact on the anxiety and pain of patients undergoing elective knee and hip replacements. Specifically at least half of the patients in each treatment group would experience at least a 50% decrease in anxiety and a 25% decrease in pain.
Both interventions would result in reduced use of pain medication and improvement of patient satisfaction scores.
METHODS
The study sample consisted of 225 patients scheduled for initial or subsequent elective hip or knee replacement surgery at Saint Clare’s Health System in Denville, NJ. Eligibility criteria included adults older than age 18 years undergoing elective knee or hip replacement who agreed to participate in the study regardless of medications or existing medical conditions. Hospital demographic analysis has shown a population consisting of 81% white, 9% Asian, 3% black, 1% American Indian, and 6% other race or ethnicity. Patients were excluded from the study if they presented with an active infection or open wound in the extremities, were unable to perceive touch in the hands and feet (eg, peripheral neuropathy), had an aversion to touch (expressed desire not to be touched or did not want to be touched), were not primarily English speaking, or did not have the ability to adequately understand a normal spoken voice (as defined by the Saint Clare’s Health System Audiology Department). During established “Patient Education for Total Hip or Total Knee Replacement” classes, patients were presented with the study plan. Patients who volunteered to be part of this study and met the criteria signed an informed consent form at the end of class.
Western institutional review board approval was obtained. The staff was introduced to the study design, interventions, and administration of the anxiety and pain scales. Care was taken that patients did not feel rushed when completing the survey.
The effect of specific interventions of M and guided imagery on anxiety and pain was studied using a controlled randomization method for all intervention groups through use of blinded envelopes containing the group letter A, B, or C, which were mixed and then drawn randomly. After administration of the initial Numeric Visual Anxiety Scale (NVAS), Pain Numeric Rating Scale (PNRS), and Hamilton Anxiety Scale, the assigned intervention groups were revealed.
M was performed on the hands and the feet for 18 to 20 minutes, with touch equally distributed among available extremities, paralleling the length of the guided imagery audio program and the duration of massage shown to be most effective at anxiety and pain reduction in previously reported studies. The level of pressure rendered in M is always 3 on a scale in which the maximum pressure is 10 as perceived by the recipient.7
The eight state-licensed massage therapists who participated in this study were trained in the consistent administration of Jane Buckle’s “M” Technique of the Hand and Foot7 and the use of the guided imagery equipment, and were familiar with patient intervention scripts. Each practitioner “settled” into the intent of the intervention, setting a relaxed tone and ensuring the patient’s comfort and centeredness to honor the mind and energy of the recipient.
The guided imagery program selected was Guided Meditation for Procedures or Surgery, created by Diane Tusek, RN, BSN.13 This selection was based on multiple opinions of reviewers noting it to be the most soothing and versatile, with less clinical and affirmation-focused dialogue.
This study was designed to integrate and evaluate M and guided imagery interventions in addition to usual care at 4 specific times during the hospital stay using the NVAS for anxiety and the PNRS for pain, administered before and after interventions. The Hamilton Anxiety Scale was administered at the same time as the NVAS before the first intervention and after the last intervention to validate findings with the NVAS. The 8 data points for collection were before and after the 4 intervention times: preoperative Day 0; postoperative Day 0, postoperative Day 1; and postoperative Day 2. A patient satisfaction questionnaire was completed at the time of discharge.
The potential for interruptions during the therapeutic intervention was explained to the patient beforehand. In addition, the massage therapist stated, “We may experience an interruption during this intervention, as this is being performed in a real-life scenario.”
Study Design
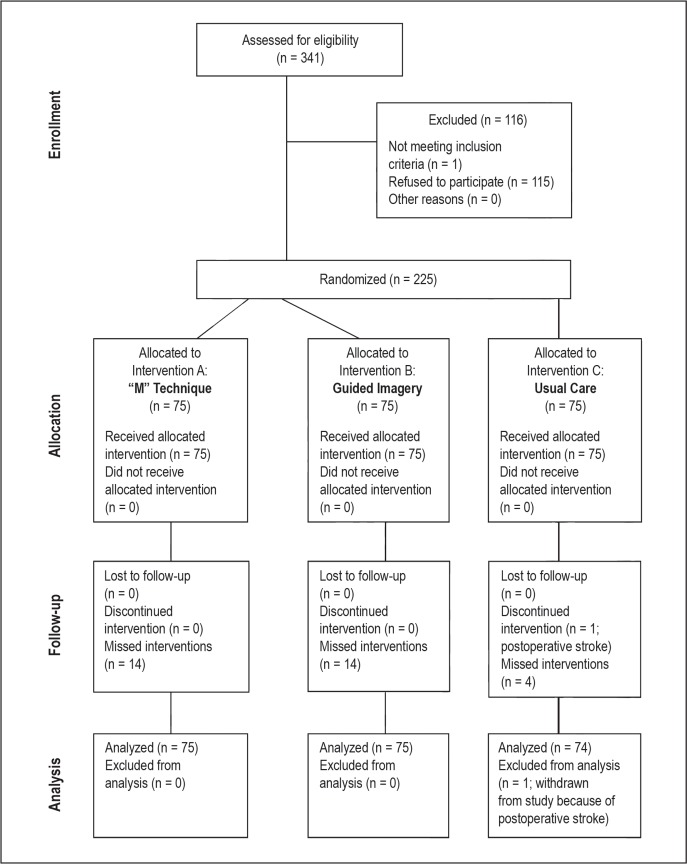
Figure 1 shows the study design.
Figure 1.
Flow diagram of study design.a
a Follows Consolidated Standards of Reporting Trials (CONSORT) 2010 (www.consort-statement.org).
Preoperative Day 0
After the same-day surgery nurse prepared the patient for surgery, permission and consent was secured from the patient. The massage therapist administered the NVAS and PNRS, followed by the Hamilton Anxiety Scale for all 3 groups. For Group A (M group), M was then administered to the patient’s hands and feet for 18 to 20 minutes, with touch equally divided between extremities according to availability. Any hand or foot accessed by intravenous lines was avoided. For Group B (guided imagery group), the therapist then instructed the patient on the guided imagery protocol and provided the patient with headphones and an MP3 player using 2 tracks for pre-operative guided imagery. The massage therapist monitored proper placement of headphones on the study patient, started the audio recording, and ensured that the volume was comfortable.
After interventions for Groups A and B, the NVAS and PNRS were administered after a pause of 30 to 60 seconds. For Group C (usual care group), the NVAS and PNRS were administered after an 18- to 20-minute wait. All documentation for interventions was recorded on individualized worksheets.
Postoperative Day 0
Once the patients were settled back into their rooms immediately after surgery and had been seen by the physical therapist for the first time, the massage therapist returned to administer the assigned intervention and the anxiety and pain scales before and after the intervention, consistent with the methods on preoperative Day 0.
Postoperative Days 1 and 2
Assigned interventions were performed after the first physical therapy session of the day. The Hamilton Anxiety Scale was administered to all groups on postoperative Day 2 after the final intervention, along with the NVAS and the patient satisfaction survey.
The primary objectives of this study were to determine if the M and guided imagery groups experienced a larger decrease in anxiety and pain than the usual care group, and to compare the two interventions. The usual care group was not anticipated to achieve the same extent of pain and anxiety decreases. These objectives were focused on intervention times 1 through 4 as previously described, and the assessment points for anxiety and pain were labeled as 1 through 8 surrounding intervention times.
The secondary objectives of this study were as follows: 1) to examine the trends of use of pain medication in all 3 groups and 2) to determine group patient satisfaction with their hospital experience as measured through a hospital preapproved patient satisfaction survey.
STATISTICAL ANALYSES
A sensitivity analysis assessment was done to determine the minimal detectable effect size with a sample size of 225, a power of 0.80, and an α level of 0.05. The model that was investigated is an analysis of covariance (ANCOVA) model with a main effect of treatment (ie, the effect of interest) with 3 covariates (eg, preintervention score on the outcome of interest, surgery type, and the type of medication used). As the ANCOVAs differed only by the outcome variable and the intervention point, only 1 sensitivity analysis was necessary to determine the minimal detectable effect. The result of this sensitivity analysis, performed by a free statistical power analysis software (G*Power 3; Heinrich Heine Universität; Düsseldorf, Germany),14 was that given the study design, an η2= 0.04 could be detected with 0.80 power. An η2 is calculated as the sum of squares treatment divided by the sum of squares total.
A separate ANCOVA was performed for each of the pre- and postintervention measurements using difference scores for pain and anxiety, resulting in 8 analyses. In addition, analysis was also performed to compare the initial preoperative Day 0 measurement with the final postoperative Day 2 measurement for both pain and anxiety. This was performed to determine whether the amount of pain and anxiety decreased over the duration of the study and to assess variation according to the patient’s treatment group. This resulted in 10 separate ANCOVA analyses.
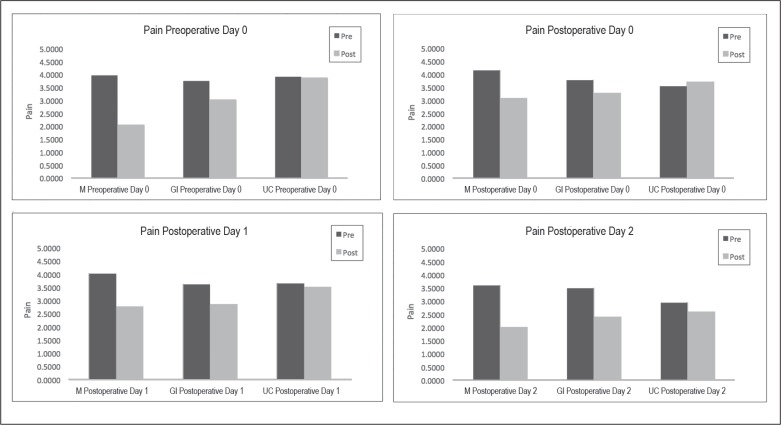
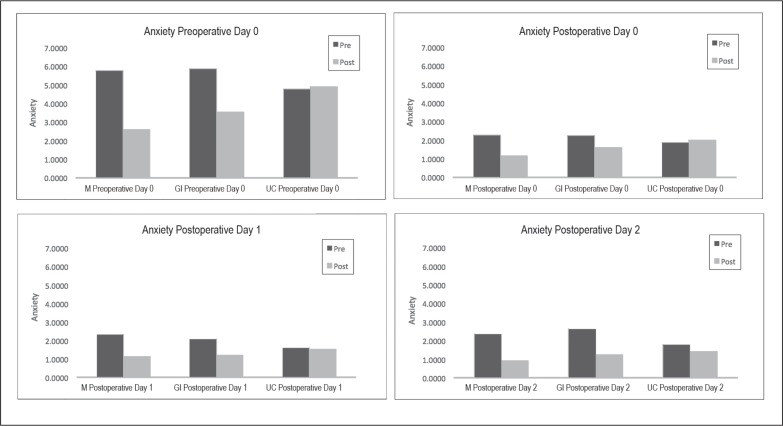
The predictors included in each of these analyses were the preintervention score on the outcome of interest, group, surgery type, and amount of medication used. These predictors were retained in the ANCOVA model regardless of their statistical significance, with significant predictors being presented and interpreted. (Full analysis of variance [ANOVA] tables are available from the authors on request.) All p values were corrected using the Bonferroni stepdown adjustment,15 accounting for all the p values involving group pairwise comparisons. This resulted in 30 comparisons: 3 for each of the 10 analyses. The 3 comparisons were M vs guided imagery, M vs usual care, and guided imagery vs usual care. The full list of adjusted and unadjusted p values is provided in Table 1. The covariates were excluded in the multiplicity control because they were not included in the family of tests. The family of tests is concerned only with all possible pairwise comparisons of the 3 groups; thus, the familywise error rate is controlled by employing the Bonferroni stepdown procedure.16 Descriptive statistics for all 8 of the pain and anxiety measurements are presented in Tables 2 and 3, and in graph form in Figures 2 and 3. For demonstration of the convergent validity of the NVAS with the Hamilton Anxiety Scale, the Hamilton Scale was also investigated using the ANCOVA.
Table 1.
Adjusted and unadjusted p values for pairwise comparisonsa
| Mean comparisonb | Outcome | Unadjusted | Bonferroni stepdown adjustment |
|---|---|---|---|
| Pain | |||
| Group A–B | Preoperative Day 0: pre- vs postintervention | < 0.0001 | < 0.0001 |
| Group A–C | Preoperative Day 0: pre- vs postintervention | < 0.0001 | < 0.0001 |
| Group B–C | Preoperative Day 0: pre- vs postintervention | 0.001 | 0.0188 |
| Group A–B | Postoperative Day 0: pre- vs postintervention | 0.0041 | 0.0648 |
| Group A–C | Postoperative Day 0: pre- vs postintervention | < 0.0001 | < 0.0001 |
| Group B–C | Postoperative Day 0: pre- vs postintervention | 0.0075 | 0.1056 |
| Group A–B | Postoperative Day 1: pre- vs postintervention | 0.0537 | 0.5369 |
| Group A–C | Postoperative Day 1: pre- vs postintervention | < 0.0001 | < 0.0001 |
| Group B–C | Postoperative Day 1: pre- vs postintervention | 0.0007 | 0.0135 |
| Group A–B | Postoperative Day 2: pre- vs postintervention | 0.0844 | 0.7599 |
| Group A–C | Postoperative Day 2: pre- vs postintervention | < 0.0001 | 0.0007 |
| Group B–C | Postoperative Day 2: pre- vs postintervention | 0.0115 | 0.1498 |
| Group A–B | Preoperative Day 0 vs postoperative Day 2 | 0.434 | 1 |
| Group A–C | Preoperative Day 0 vs postoperative Day 2 | 0.2885 | 1 |
| Group B–C | Preoperative Day 0 vs postoperative Day 2 | 0.7841 | 1 |
| Anxiety | |||
| Group A–B | Preoperative Day 0: pre- vs postintervention | 0.0059 | 0.0884 |
| Group A–C | Preoperative Day 0: pre- vs postintervention | < 0.0001 | < 0.0001 |
| Group B–C | Preoperative Day 0: pre- vs postintervention | < 0.0001 | < 0.0001 |
| Group A–B | Postoperative Day 0: pre- vs postintervention | 0.0901 | 0.7599 |
| Group A–C | Postoperative Day 0: pre- vs postintervention | < 0.0001 | 0.0018 |
| Group B–C | Postoperative Day 0: pre- vs postintervention | 0.0227 | 0.273 |
| Group A–B | Postoperative Day 1: pre- vs postintervention | 0.2907 | 1 |
| Group A–C | Postoperative Day 1: pre- vs postintervention | < 0.0001 | < 0.0001 |
| Group B–C | Postoperative Day 1: pre- vs postintervention | < 0.0001 | 0.001 |
| Group A–B | Postoperative Day 2: pre- vs postintervention | 0.4169 | 1 |
| Group A–C | Postoperative Day 2: pre- vs postintervention | < 0.0001 | 0.0016 |
| Group B–C | Postoperative Day 2: pre- vs postintervention | 0.0016 | 0.0276 |
| Group A–B | Preoperative Day 0 vs postoperative Day 2 | 0.5122 | 1 |
| Group A–C | Preoperative Day 0 vs postoperative Day 2 | 0.0401 | 0.4408 |
| Group B–C | Preoperative Day 0 vs postoperative Day 2 | 0.1605 | 1 |
These p values reflect application of the opioid equianalgesic conversion table.18
Group A = “M” Technique; Group B = guided imagery; and Group C = usual care.
Table 2.
Proportion of participants in each treatment group who experienced 25% pain decrease
| Mean differencea | No. | Proportion who met the criterion | Average change, %b |
|---|---|---|---|
| Guided imagery | |||
| Pain 2-Pain 1 | 51 | 0.235 | −26.6 |
| Pain 4-Pain 3 | 55 | 0.200 | −12.9 |
| Pain 6-Pain 5 | 63 | 0.222 | −25.3 |
| Pain 8-Pain 7 | 55 | 0.309 | −34.5 |
| Pain 8-Pain 1 | 50 | 0.620c | −31.1 |
| “M” Technique | |||
| Pain 2-Pain 1 | 59 | 0.542 | −53.0 |
| Pain 4-Pain 3 | 63 | 0.349 | −30.9 |
| Pain 6-Pain 5 | 64 | 0.313 | −36.1 |
| Pain 8-Pain 7 | 63 | 0.587 | −50.2 |
| Pain 8-Pain 1 | 58 | 0.724c | −50.3 |
| Usual care | |||
| Pain 2-Pain 1 | 52 | 0.019 | 2.2 |
| Pain 4-Pain 3 | 50 | 0.020 | 1.3 |
| Pain 6-Pain 5 | 64 | 0.078 | −4.1 |
| Pain 8-Pain 7 | 54 | 0.037 | −7.0 |
| Pain 8-Pain 1 | 53 | 0.679c | −20.1 |
Pain 2-Pain 1 surrounds preoperative Day 0, Pain 4-Pain 3 surrounds postoperative Day 0, etc.
Negative numbers indicate a decrease while positive numbers indicate an increase in pain.
There were no explicit expectations regarding the beginning and end of the study, but the corresponding proportion of patients had a percentage change larger than 25%.
Table 3.
Proportion of participants in each treatment group who experienced 50% anxiety decrease
| Mean differencea | No. | Proportion who met the criterion | Average change, %b |
|---|---|---|---|
| Guided imagery | |||
| Anxiety 2-Anxiety 1 | 65 | 0.431 | −42.8 |
| Anxiety 4-Anxiety 3 | 38 | 0.500 | −33.3 |
| Anxiety 6-Anxiety 5 | 38 | 0.526 | −47.6 |
| Anxiety 8-Anxiety 7 | 45 | 0.578 | −51.9 |
| Anxiety 8-Anxiety 1 | 64 | 0.906c | −78.7 |
| “M” Technique | |||
| Anxiety 2-Anxiety 1 | 67 | 0.657 | −55.6 |
| Anxiety 4-Anxiety 3 | 38 | 0.711 | −61.6 |
| Anxiety 6-Anxiety 5 | 47 | 0.745 | −67.4 |
| Anxiety 8-Anxiety 7 | 48 | 0.750 | −65.9 |
| Anxiety 8-Anxiety 1 | 66 | 0.909c | −85.0 |
| Usual care | |||
| Anxiety 2-Anxiety 1 | 62 | 0.016 | 5.4 |
| Anxiety 4-Anxiety 3 | 37 | 0.000 | 4.3 |
| Anxiety 6-Anxiety 5 | 33 | 0.121 | −0.7 |
| Anxiety 8-Anxiety 7 | 31 | 0.226 | −17.1 |
| Anxiety 8-Anxiety 1 | 62 | 0.855c | −76.3 |
Anxiety 2-Anxiety 1 surrounds preoperative Day 0, Anxiety 4-Anxiety 3 surrounds postoperative Day 0, etc.
Negative numbers indicate a decrease while positive numbers indicate an increase in anxiety.
There were no explicit expectations regarding the beginning and end of the study, but the corresponding proportion of patients had a percentage change greater than 50%.
Figure 2.
Mean pain scores for each of four measurements by treatment group.
GI = guided imagery; M = “M” Technique; pre = preintervention; post = postintervention; UC = usual care.
Figure 3.
Anxiety means for each of four measurement occasions separated by group.
GI = guided imagery; M = “M” Technique; pre = preintervention; post = postintervention; UC = usual care.
The secondary outcome of pain narcotic use was analyzed using ANOVA. An ANOVA was run with the main effects of group and medication. There was no need to define the medication type as a predictor because all medication dosages were calculated using an opioids-equianalgesic dosage conversion table. The ANOVA analysis was performed to determine if there were mean differences on patient satisfaction between the groups. All analyses were performed using SAS 9.2 software (SAS Institute Inc, Cary, NC).
RESULTS
A total of 225 patients were enrolled between November 2012 and June 2014. There were 75 participants randomly assigned to each intervention group. The study sample was 33.9% men (n = 76) and 66.1% women (n = 148). Of this sample, 31.3% (n = 70) underwent hip replacement, and 68.7% (n = 154) had knee replacement. Of the 4 intervention times for the 3 groups, there were 32 missed intervention times (14 for each of the intervention groups and 4 for the usual care group) because of various circumstances (eg, received late from recovery, patient refusal, adverse weather conditions, patient transfer requiring a higher level of care). This number reflects only 2% of the total number of points measured and thus is considered inconsequential.17
All participants assigned to a group were used in the analysis except one in the usual care group. Only three patients who took nonnarcotic medication were not included in the analyses. Otherwise, there was no attrition throughout the study, and there was no harm or unintended effects in any group.
Anxiety
The preintervention measure of anxiety and the group were significant predictors for the anxiety difference scores on the 4 measurement occasions (pre-operative Day 0, postoperative Day 0, postoperative Day 1, and postoperative Day 2). The general trends for the group were also the same although the pattern of statistical significance varied across the measurement occasions. The M group experienced the largest anxiety decreases, followed by guided imagery, which was followed by usual care. The initial levels of anxiety and group were significant predictors of the difference score on preoperative Day 0. Larger baseline anxiety resulted in larger predicted anxiety decreases, B = −0.375, p < 0.0001, and partial η2 (η2p) = 0.296. With use of the Bonferroni stepdown corrected p values, the M and guided imagery groups were predicted to experience significantly greater decreases in anxiety than the usual care group (p < 0.0001 and p < 0.0001, respectively; Table 1). Overall, the model explained 50.4% (adjusted R2 = 0.504) of the difference score variance, F5,202 = 43.078, p < 0.0001.
On postoperative Day 0, larger preintervention anxiety scores also resulted in larger predicted anxiety decreases, B = −0.335, p < 0.0001, and η2p = 0.208. The only significant difference on this occasion was between M and usual care (p = 0.0018). The overall model explained 26.5% of the variance in the difference scores, F5,197 = 15.545, p < 0.0001. On postoperative Day 1, for each additional unit increase in the preintervention anxiety, the amount of improvement increased by 0.273, B = −0.273, p < 0.0001, and η2p = 0.287. Both the M and guided imagery groups had significantly larger improvements than did the usual care group (p < 0.0001 and 0.0010, respectively) but were not significantly different from one another. This model explained 37.9% of the variance in the postoperative Day 1 difference scores, F5,207 = 26.0872, p < 0.0001. The postoperative Day 2 results followed a similar pattern, with larger preintervention anxiety scores predicting larger decreases in anxiety, B = −0.431, p < 0.0001, and η2p = 0.494. Once again, the M and guided imagery groups improved significantly more than the usual care group. This model explained 52.9% of the variance in the postoperative Day 2 difference scores, F5,205 = 48.130, p < 0.0001.
The improvement over the entire span of the study (baseline to postoperative Day 2 after intervention) did not follow a similar pattern of results. The only significant predictor was the level of preoperative Day 0 anxiety. Larger anxiety scores on preoperative Day 0 were associated with more improvement throughout the study. Although there was significant improvement during the course of the study, the group was not a significant predictor of the amount of improvement during the study period. This model explained 52.9% of the variance in the postoperative Day 2 difference scores, F5,200 = 76.573, p < 0.0001.
Pain
The preintervention measure of pain and the group were significant predictors for the pain difference scores on the 4 measurement occasions (preoperative Day 0, postoperative Day 0, postoperative Day 1, and postoperative Day 2). The predictors also showed the same trend for each of the measurement occasions; larger amounts of pain at the initial measurement on a particular day resulted in larger predicted pain decreases. The general trends for the group were also the same, although the pattern of statistical significance varied across the measurement occasions. The M group experienced the largest pain decreases, followed by guided imagery, which was followed by usual care. The statistics for each measurement occasion are presented in detail here.
Significant predictors of pain difference score on preoperative Day 0 were the initial levels of pain as well as the group. Specifically, larger baseline pain resulted in larger predicted pain decreases, B = −0.169 p < 0.0001, and η2p = 0.136. With use of the Bonferroni stepdown corrected p values, the M group was found to experience significantly greater decreases in pain than the guided imagery or usual care group (p < 0.0001 and p < 0.0001, respectively; Table 1). Overall, the model explained 36.70% (adjusted R2 = 0.36370) of the difference score variance, F5,202 = 25.034, p < 0.0001.
On postoperative Day 0, larger preintervention pain scores also resulted in larger predicted pain decreases, B = −0.091, p = 0.0014, and η2p = 0.050. On this occasion, the M group experienced significantly larger decreases in pain than did the usual care group (p < 0.0001). The overall model explained 18.8% of the variance in the difference scores, F5,197 = 10.345, p < 0.00001. Postoperative Day 1 had the same pattern of results; for each additional unit increase in the preintervention pain measurement on postoperative Day 1, the amount of improvement increased by 0.141, B = −0.141, p < 0.0001, and η2p = 0.087. Both the M and guided imagery groups had significantly larger improvements than did the usual care group (p < 0.0001 and 0.00135, respectively) but were not significantly different from one another. This model explained 18.9% of the variance in the postoperative Day 1 difference scores, F5,207 = 10.884, p < 0.0001. The postoperative Day 2 results followed a similar pattern, with larger preintervention pain scores predicting larger decreases in pain, B = −0.303, p < 0.0001, and η2p = 0.237. The only group differences in this situation were that the M group improved significantly more than the usual care group did. This model explained 30.6% of the variance in the postoperative Day 2 difference scores, F5,205 = 19.561, p < .0001.
The improvement during the entire span of the study (baseline to postoperative Day 2 after intervention) did not follow a similar pattern of results. Significant predictors were the type of surgery (knee vs hip; knees improved less, B = 0.818, p = 0.0192, η2p = 0.027), amount of medication used (B = 0.021, p = 0.0051, η2p = 0.039), and the baseline pain score (B = −0.811, p < 0.0001, η2 = 0.550). Specifically, the more medication taken resulted in less improvement, and those who had higher initial pain values were predicted to improve more. Although there was significant improvement over the course of the study, group was not a significant predictor of the amount of improvement over the study duration. This model explained 58.0% of the variance in the postoperative Day 2 difference scores, F5,200 = 57.573, p < 0.0001.
Secondary Analyses
With use of the Hamilton Anxiety Scale-derived difference scores as the outcome, the only significant predictor of the difference scores was the Hamilton scale’s initial score (B = −0.595, p < 0.0001). The amount of medicine taken, type of surgery, and group were not related to the Hamilton Anxiety Scale’s difference scores. This model explained 40.4% of the variance of these difference scores, F5,204 = 29.360, p < 0.0001. These results were very similar to the beginning vs the end-of-the-study results for the NVAS. The only significant predictor of the anxiety change from the beginning to the end of the study was the initial anxiety level (B = −0.772, p < 0.0001).
The amount of medicine taken, type of surgery, and group were not significant predictors of the NVAS. This model explained 64.8% of the variance in the NVAS difference scores. Statistically significant correlations between the Hamilton Anxiety Scale and NVAS measures at the beginning and end of the study also provided evidence for convergent validity of the 2 measures (r = 0.592 and 0.484, p < 0.0001, at the beginning and end of the study, respectively).
After using the opioid-equianalgesic dosages conversion table,18 there was not a significant difference in the amount of opioid medication taken between groups, F2,216 = 1.56, p = 0.213.
A 1-way ANOVA was performed for patient satisfaction, and findings revealed that there were significant differences between the groups, F2,214 = 30.75, p < 0.05. Specifically, the M group had higher satisfaction scores than the guided imagery or usual care group (p < 0.0001), and the guided imagery group had higher satisfaction scores than the usual care group (p = 0.0003). This p value was corrected using the Bonferroni stepdown adjustment. The mean satisfaction scores were as follows: 4.784, 4.250, and 3.781 for the M, guided imagery, and usual care groups, respectively. This model explained 21.6% of the variance in the satisfaction outcome.
DISCUSSION
The findings in this study demonstrate that M was effective during usual care for significant reduction of both anxiety and pain at nearly all intervention points when incorporated during routine perioperative conditions in patients undergoing elective knee and hip replacement. Accounting for 32 missed interventions did not result in a statistically significant impact on findings. The application of both mind-body (guided imagery) and touch interventions (M) demonstrated significant decreases in anxiety when looking at preoperative-to-discharge comparisons over usual care. M showed significant improvement over both guided imagery and usual care for decreased pain scores at intervention times 1 and 2 and had the largest predicted decreases in anxiety and pain at all intervention points. The only point that an intervention was unsuccessful at decreasing anxiety over usual care was guided imagery at intervention Point 2. This is speculated to have occurred because this intervention point added a variable of persistent effects of anesthesia, which has been linked to greater postoperative pain.19
According to Tusek, “… pain is a primary concern of patients, second only to the fear of death… .”20 The beneficial effect of M and guided imagery on pain in our study met expected outcomes and was found to be successful in decreasing pain scores at all intervention points exceeding the usual care group, largely correlating with our findings on anxiety. Other studies have also shown that fear and anxiety are proportionately linked to pain severity in perioperative patients.3,20,21
We found the use of narcotic pain medication did not vary among groups. These findings are in contrast with those of a study done using guided imagery in patients undergoing major colorectal surgery.11 Additionally, a prospective randomized trial involving 130 patients at the Cleveland Clinic Foundation found that requirements for analgesics were significantly reduced in guided imagery recipients undergoing elective abdominal surgeries.11 Surprisingly, M had no influence on the amount of pain medication used despite showing a greater reduction by global average percentage change and postintervention assessments.
The M group had higher satisfaction scores than both the guided imagery and usual care groups, and the guided imagery group had higher satisfaction scores than the usual care group on discharge. This finding coincides with the results of our primary outcome measures, which demonstrated that M produced the largest predicted decreases in anxiety and pain.
A major strength of this study is the success of applying integrative interventions under routine conditions. This unique aspect using guided imagery and M demonstrates the ability for widespread use of integrative therapies for patients in a variety of health care settings, even those viewed as being associated with high stress. Originally, M was intended for and studied for use in frail, elderly, end-of-life patients. This is, to our knowledge, the first study demonstrating the value of M as a therapeutic measure for the reduction of anxiety and pain in orthopedic patients undergoing elective joint replacement.
In this study, M focused on two of the most sensitive and connected areas of the body: the hands and feet. Stimulation of mechanoreceptors in the hands and the feet may result in pain inhibition by stimulating nonpainful nerve fibers. Noteworthy is that there is a recently discovered type of nerve fiber in the skin, the mechanoreceptive tactile C afferent, which carries signals via afferent pathways to the brain when the skin is stroked gently.22 Further elucidation of these receptors and the conditions under which they are stimulated could help to explain the differences in response to different types of light touch being used. Kinesthetic afferent pathways are also stimulated by skin stretch receptors in addition to normal muscle spindles for limb positioning and movement. It may be important to point out that kinesthetic pathways for the upper limbs ascend to the brain via the posterior columns without relaying in the spinal cord, whereas the lower limb pathways ascend via the Clarke column and the dorsal spinocerebellar tract and require crossover in the spinal cord.23 This information could potentially influence the therapeutic and perceived effect of different pressure levels from varying touch modalities used on the hands, feet, or both. Novel interoceptive receptors, which are 40% responsive to light touch, may play an integral role in patient response.24
Referring to the needs of the older population, the anthropologist Montagu comments,25 “The most important and neglected of these needs is the need for tactile stimulation.” He also stated that the elderly often have impaired hearing and vision as well as decreased mobility and vitality, which leaves them feeling helpless and vulnerable. However, through the emotional involvement of touch, Montagu25 asserted, we can reach through the isolation and communicate love, trust, affection, and warmth. Touch releases endorphins, peptides, and other neurochemicals that play a role in enhancing relaxation at a deep level via multiple mechanisms. A commonly understood mechanism about the action of endorphins is that they are neuropeptides that have an opioid effect via blocking the release of Substance P, a neurotransmitter known to play a major role in the sensation of pain.
Another explanation for the positive effects that massage or touch therapy has on pain is called the gate-control theory.26 This theory suggests that the pain signal takes longer to reach the brain than a pressure signal that is stimulated by touch and will “close the gate” to the pain stimulus.26 A meta-analysis by Moyer et al27 on massage therapy research suggested that the gate-control theory’s explanation for pain reduction was not supported by the data because of a “… failure to find a significant effect for the immediate assessment of pain … .” They note that improvement in anxiety and depression resulting from massage therapy may be caused by its influences on body chemistry and the psychological benefit of the therapist-client alliance.
The pain reduction benefit of M seems clearly related to a decrease in anxiety through many potential vehicles, including competent caring, physical comfort, and connectiveness through gentle repetitive motions, a calming touch on emotions, and likely by reasoning an energetic transference through intention. In our study the benefits of M for anxiety closely parallels the effectiveness rate of traditional psychotherapy.26 The body’s sensory network connects the physical to the emotional and mental through a complex interplay of nerves and chemicals relayed through the brain as the central feedback filter, implying a multidirectional influence based on the intervention being used and the patient’s individual experience. Evidence that massage therapy reduces pain and anxiety via one or a complex interplay of multiple psychophysiologic factors would reflect on the magnificence of the human construction and imply that there can be multiple approaches taken to obtain similar positive outcomes.
Acknowledging our incomplete understanding of the true nature of mind-body-spirit integration, this study demonstrates that M, a touch-based intervention, does reach multiple levels of a patient’s being and is an effective treatment option for the significant reduction of pain and anxiety in elective knee and hip replacement surgeries. Guided imagery, a mind-based intervention, showed positive outcomes on anxiety and pain reductions most likely by influencing the mind on a deeper or subconscious level.
Many efforts have been made by hospital personnel to ease a patient’s transition through the surgical process. However, these efforts have primarily focused on time management and efficiency on the part of the staff and have not necessarily taken into account the patient’s psychological comfort nor considered the effect this could have on his/her recovery. Patients are often at their most vulnerable just before surgery, with anticipation, elevated stress, and fear, and also immediately afterward when their energy is lower and their bodies are trying to accommodate after an invasive procedure. Concern, fear, and anxiety experienced by family members and friends who are present or even not present also can contribute to the patient’s anxiety. This stress, anxiety, and pain associated with surgery and recovery can increase complication rates and slow recovery times, resulting in longer hospital stays. In the last several years, substantial strides have been made in researching the effects of various integrative and complementary medicine techniques and their positive influence on patient health, including in the operative setting.
Vital signs were not included in this study as a data point because the usual hospital protocol for elective joint replacement is already replete with interruption during the entire recovery phase, resulting in potential stress, anxiety, and frustration. Favorable changes in blood pressure after massage28 and in systolic blood pressure and heart rate after the use of guided imagery29,30 have previously been noted.
Interruptions interfere with the relaxation and healing cycle. Previous studies largely segregated interventions so there were minimal or no interruptions and were less than realistic to the actual situation. Integrative therapies that can be routinely incorporated as part of the normal work flow of perioperative protocols ultimately result in substantial patient benefit using inexpensive, easily learned, and effective tools.
Armstrong et al31 showed that the combination of massage and guided imagery demonstrated a more pronounced effect on anxiety reduction compared with the massage-only group in a pilot study involving 55 patients undergoing cardiac catheterization. Studies of the importance of choice of integrative intervention could be based on patient response and preference, to either having a single intervention or having both administered in tandem or simultaneously. Future studies could be designed in which these 2 integrative modalities are combined, to determine the potential for synergistic effect. M could be initiated before guided imagery with the intention of engaging the patient through touch into the competent caring process. This would enhance the sense of connection and healing, increase patient comfort, decrease anxiety, and facilitate patient receptiveness to the input of a guided imagery program. A more intriguing possibility would be simultaneous administration of M and guided imagery initiated by brief touch to heighten integration of all the senses. Furthermore, patient selection from various guided imagery audio programs for connectedness with script, voice, and background sounds would likely be shown to be beneficial. Additionally, the use of guided imagery with consistent, uninterrupted administration of the audio program may have enhanced the predicted outcomes of this intervention to the already positive effect that we found in this study. Further investigations between the uses of guided imagery scripting using direct vs open (integrated) suggestion and the difference made by patient involvement in this choice will likely enhance the effects and benefits of this intervention. Guided imagery may possibly have had a better outcome if preparation began several days before the procedure, allowing for stronger brain entrainment. The initiation of integrative adjunctive therapy with M in the immediate pre-operative period may also subvert the necessity for advance preparation with the guided imagery program.
Inevitably, data showing increases in patient satisfaction, as seen in this investigation, would improve the reputation of the hospital in the community, be looked on favorably by insurers, improve staff and patient morale, and solidify the spiritualistic principles underlying humanistic care. Physicians, nurses, and staff who learn these modalities can also use them for themselves for their own health and wellness.
This study did not control for three concepts: intention, belief, and subtle energies. There is a healing intentionality associated with the practitioners who administered M beyond its unique form of structured touch, which is an unwritten part of their protocol. Practitioners “settle” into their routine at the start of the intervention, setting a relaxed tone, ensuring the patient’s comfort and centeredness, which influences the mind and energy of the recipient beyond touch alone. The consistent patient contact and touch alone of M would seem more resonant to the recipient than guided imagery on multiple levels. When a caregiver touches a patient, there is an inherent belief by the recipient that the caregiver “cares” as the recipient perceives the patient-centered competent caring being administered. Competent caring provided during interventions is integral to managing a patient’s anxiety and pain. Competence implies knowledge, skill, and intelligence, whereas caring provides the humanitarian aspect with positive intention and effect. Competent caring provided during interventions is a useful component and contributes to the reduction of anxiety, pain, and fears and the promotion of wellness.32 Extending this intentionality to all members of the health care team could create a more optimum healing environment.
Belief is a powerful factor in one’s perception and effect in response to an intervention. The observation of expressed disappointment by a small number of recipients in the study regarding their being randomly selected to one group rather than another indicated a sentiment owing to their individual preference toward an intervention. This recipient belief and sentiment could influence the outcome of the intervention, although this was not quantified in this study. Scott et al33 revealed that fulfillment of expectations in patients undergoing hip and knee replacement were shown to highly correlate with the degree of patient satisfaction. Having been chosen for one intervention while preferring to have another over the one chosen creates an expectation, which could decrease patient satisfaction ratings.
Subtle energies describe systems of energies that generally have eluded standard scientific measurement, yet the inherent belief in and common experience with them has been the basis of practice for all energy-healing practitioners. This energy, which can purportedly be perceived by healing practitioners, is inherent within, and it surrounds and extends beyond the intracellular and extracellular matrices of the body. All substances, including those related to human structure and functioning, are semiconductors and thus capable of transmitting vibration, which can convert to and transmit energy. Energetic vibrations perceived by the senses, including sound and touch, extend further than the physical realm. Oschman34 describes a continuum pathway conduction of energy, which is an atemporal cognition and response transmitting energy 10 to 20 times faster than sensory motor neurologic cognition and response. He further supports the concept of this energy being linked to the conduction of vibration being initiated on and transmitted through multiple levels, linking the physical and energetic fields. The implication is a continuum of effect on subtle energies on multiple planes interconnecting the mind, body, and spirit. Thus, positive intention, belief, and centeredness can be therapeutically transferred to a recipient for healing, transcending the constraints of time and space, and is currently being supported by sound scientific methodologic evidence.
Limitations
A potential limitation of the study was that therapists were directly involved in administration of the scales before and after interventions. In this regard, a proactive measure was taken to train all facilitators to a scripted discussion regarding the administration of scales, data collection, and patient satisfaction questionnaire completion. Limited funding also influenced this decision.
The study design did not control for environmental light or noise in Group C patients, as they were intended to represent the standard of care. Likewise, inherent interruptions remained routine for all groups and were not controlled for other than posting a sign indicating the study was in process.
Other limitations included lack of uniformity of the availability of all 4 extremities for M, not accounting for the timing of administration of pain medication in relation to initiation of the interventions, lack of documentation of patient touch sensation in feet postoperatively on Day 0, and expressed disappointment by clients in the randomized group (implying preconceived patient expectations and/or preferences for intervention type).
Data assessment for the comparative group distribution of comorbidities was not included. Because the scope of the study was limited to two days postoperatively, the identification of complications and final outcomes beyond discharge to home or a rehabilitation facility was not captured. Another limitation of the study was the lack of separation of subjects into distinct comparative groups between knee and hip surgery, which was not intended for this investigation.
Future Applications
Replication of this study would probably benefit patient care and obtain similar results. Recommendations for changes in the design include improved demographics of groups investigated, documentation of comorbid conditions, detailed analysis of pain medication use and timing relative to interventions, and additional personnel, not directly involved in interventions, for scale administration. Additionally, this study can be replicated in a community environment (eg, home and clinics), where the technique is taught to caregivers for those in need of adjunctive pain and anxiety relief. Future studies can also include combining touch/energy with mind-body interventions for potential augmentation of positive outcomes.
CONCLUSION
This study is the first we are aware of that demonstrates reduced anxiety and pain using M and guided imagery in patients undergoing elective joint replacement performed under routine conditions. We conclude that the underlying reason for the impressive benefit of M is the use of a specifically structured sequence of touch by the hands of competent caring, trained providers during the intervention process. Touch is an essential part of the competent caring process during an intervention because it is a vehicle for skillful interaction with intention, and it promotes wellness and healing. The creation of a healing, loving environment with intention on the part of all caregivers will help provide for optimal patient outcomes and satisfaction.
Acknowledgments
The author(s) acknowledge Saint Clare’s Health System; the orthopedic surgical staff; all study participants; and all health system staff involved in the study, including Serena Schmitz, CCRC, research coordinator; orthopedic educational facilitators and support staff for obtaining consent; Karen Koch, MS, BSN, CMSRN, ONC, Orthopedic Navigator; and John Diffily, Director of Rehabilitation Services. The following massage therapists at Saint Clare’s Hospital, Denville, NJ, participated in the study: Nancy Greuter, RN, LMT (Team Leader); Janice Dickson, LMT; Kristina Koski, LMT; Jillian Sinski, LMT; Elizabeth Sherpa, LMT, LAc; Margaret (Peggy) Burke, LMT; Karen Lumpuy, LMT; and Betty Surette, RN, LMT. Ms Sherpa also provided editing support.
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
This study received a $15,000 grant from Saint Clare’s Foundation, the charitable arm of the Saint Clare’s Health System, Denville, NJ; a donation from the Robert & Joan Dircks Foundation, Mountain Lakes, NJ; and $500 from the Amanda Munoz Fund from Saint Clare’s Foundation.
The author(s) have no conflicts of interest to disclose.
References
- 1.Thomas KM, Sethares KA. Is guided imagery effective in reducing pain and anxiety in the postoperative total joint arthroplasty patient? Orthop Nurs. 2010 Nov-Dec;29(6):393–9. doi: 10.1097/NOR.0b013e3181f837f0. DOI: http://dx.doi.org/10.1097/NOR.0b013e3181f837f0. [DOI] [PubMed] [Google Scholar]
- 2.Ko YL, Lin PC. The effect of using a relaxation tape on pulse, respiration, blood pressure and anxiety levels of surgical patients. J Clin Nurs. 2012 Mar;21(5–6):689–97. doi: 10.1111/j.1365-2702.2011.03818.x. DOI: http://dx.doi.org/10.1111/j.1365-2702.2011.03818.x. [DOI] [PubMed] [Google Scholar]
- 3.Montin L, Leino-Kilpi H, Katajisto J, Lepistö J, Kettunen J, Suominen T. Anxiety and health-related quality of life of patients undergoing total hip arthroplasty for osteoarthritis. Chronic Illn. 2007 Sep;3(3):219–27. doi: 10.1177/1742395307084405. DOI: http://dx.doi.org/10.1177/1742395307084405. [DOI] [PubMed] [Google Scholar]
- 4.Dalury DF, Lieberman JR, Macdonald SJ. Current and innovative pain management techniques in total knee arthroplasty. J Bone Joint Surg Am. 2011 Oct 19;93(20):1938–43. doi: 10.2106/JBJS.9320icl. DOI: http://dx.doi.org/10.2106/JBJS.9320icl. [DOI] [PubMed] [Google Scholar]
- 5.Pellino TA, Gordon DB, Engelke ZK, et al. Use of nonpharmacologic interventions for pain and anxiety after total hip and total knee arthroplasty. Orthop Nurs. 2005 May-Jun;24(3):182–90. doi: 10.1097/00006416-200505000-00005. DOI: http://dx.doi.org/10.1097/00006416-200505000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Buckle J, Newberg A, Wintering N, Hutton E, Lido C, Farrar JT. Measurement of regional cerebral blood flow associated with the M technique-light massage therapy: a case series and longitudinal study using SPECT. J Altern Complement Med. 2008 Oct;14(8):903–10. doi: 10.1089/acm.2007.0613. DOI: http://dx.doi.org/10.1089/acm.2007.0613. [DOI] [PubMed] [Google Scholar]
- 7.The ‘M’ technique: hand and foot DVD booklet. London, United Kingdom: RJ Buckle Associates LLC; 2010. p. 4. [Google Scholar]
- 8.Rakel D. Integrative medicine. 2nd ed. Philadelphia, PA: Saunders; 2007. p. 1032. [Google Scholar]
- 9.Tusek D, Church JM, Fazio VW. Guided imagery as a coping strategy for perioperative patients. AORN J. 1997 Oct;66(4):644–9. doi: 10.1016/s0001-2092(06)62917-7. DOI: http://dx.doi.org/10.1016/S0001-2092(06)62917-7. [DOI] [PubMed] [Google Scholar]
- 10.Antall GF, Kresevic D. The use of guided imagery to manage pain in an elderly orthopaedic population. Orthop Nurs. 2004 Sep-Oct;23(5):335–40. doi: 10.1097/00006416-200409000-00012. DOI: http://dx.doi.org/10.1097/00006416-200409000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Tusek DL, Church JM, Strong SA, Grass JA, Fazio VW. Guided imagery: a significant advance in the care of patients undergoing elective colorectal surgery. Dis Colon Rectum. 1997 Feb;40(2):172–8. doi: 10.1007/BF02054983. [DOI] [PubMed] [Google Scholar]
- 12.Gonzales EA, Ledesma RJ, McAllister DJ, Perry SM, Dyer CA, Maye JP. Effects of guided imagery on postoperative outcomes in patients undergoing same-day surgical procedures: a randomized, single-blind study. AANA J. 2010 Jun;78(3):181–8. [PubMed] [Google Scholar]
- 13.Tusek DL. Guided meditation for procedures or surgery: relax, relieve anxiety, sleep better, heal faster [audiobook] Solon, OH: Findaway World; 2009. Aug, [Google Scholar]
- 14.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analysis using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009 Nov;41(4):1149–60. doi: 10.3758/BRM.41.4.1149. DOI: http://dx.doi.org/10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 15.Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics. 1979;6(2):65–70. [Google Scholar]
- 16.Kutner M, Nachtsheim C, Neter J, Li W. Applied linear statistical models. 5th ed. Burr Ridge, IL: McGraw-Hill/Irwin; 2004. Aug, [Google Scholar]
- 17.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999 Mar;8(1):3–15. doi: 10.1177/096228029900800102. DOI: http://dx.doi.org/10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- 18.Opioids—equianalgesic dosages. Detroit, MI: GlobalRPh Inc; p. c1993. [updated 2015 Apr 10; cited 2015 Apr 10]. Available from: www.globalrph.com/narcotic.htm. [Google Scholar]
- 19.Hitti M. Anesthesia link to post-surgery pain [Internet] New York, NY: WebMD Health News; 2008. Jun 23, [cited 2015 May 4]. Available from: www.webmd.com/pain-management/news/20080623/anesthesia-link-to-postsurgery-pain. [Google Scholar]
- 20.Tusek DL, Cwynar R, Cosgrove DM. Effect of guided imagery on length of stay, pain and anxiety in cardiac surgery patients. J Cardiovasc Manag. 1999 Mar-Apr;10(2):22–8. [PubMed] [Google Scholar]
- 21.Vaughn F, Wichowski H, Bosworth G. Does preoperative anxiety level predict postoperative pain? AORN J. 2007 Mar;85(3):589–604. doi: 10.1016/S0001-2092(07)60130-6. DOI: http://dx.doi.org/10.1016/S0001-2092(07)60130-6. [DOI] [PubMed] [Google Scholar]
- 22.Morrison I. Gene-brain correlates of affective touch [abstract] [Internet] Philadelphia, PA: Positive Neuroscience; p. c2010. [cited 2012 Jan 14]. Available from: www.posneuroscience.org/abstract-geneBrai.html. [Google Scholar]
- 23.Proske U, Gandevia SC. The kinaesthetic senses. J Physiol. 2009 Sep 1;587(Pt 17):4139–46. doi: 10.1113/jphysiol.2009.175372. DOI: http://dx.doi.org/10.1113/jphysiol.2009.175372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blatman H. Lecture from the 2014 Integrative Healthcare Symposium. New York, NY. New York, NY: Integrative Healthcare Symposium; 2014. Feb, 2014. Fascia—the silent network: disorder, healing, and homeostasis [video of slide presentation] [Internet] pp. 20–22. [cited 2015 Apr 10]. Available from: http://fltwood.com/ihs_2014-02/scripts/sessions/22421.html. [Google Scholar]
- 25.Montagu A. Touching: the human significance of the skin. 3rd ed. New York, NY: Harper & Row Publishers Inc; 1986. pp. 395–6. [Google Scholar]
- 26.Field T. Touch for socioemotional and physical well-being: a review. Developmental Review. 2010 Dec;30(4):367–83. DOI: http://dx.doi.org/10.1016/j.dr.2011.01.001. [Google Scholar]
- 27.Moyer CA, Rounds J, Hannum JW. A meta-analysis of massage therapy research. Psychol Bull. 2004 Jan;130(1):3–18. doi: 10.1037/0033-2909.130.1.3. DOI: http://dx.doi.org/10.1037/0033-2909.130.1.3. [DOI] [PubMed] [Google Scholar]
- 28.Hernandez-Reif M, Field T, Krasnegor J, Hossain HT, Burman I. High blood pressure and associated symptoms were reduced by massage therapy. J Bodyw Mov Ther. 2000 Jan;4(1):31–8. DOI: http://dx.doi.org/10.1054/jbmt.1999.0129. [Google Scholar]
- 29.Toth M, Wolsko PM, Foreman J, et al. A pilot study for a randomized, controlled trial on the effect of guided imagery in hospitalized medical patients. J Altern Complement Med. 2007 Mar;13(2):194–7. doi: 10.1089/acm.2006.6117. DOI: http://dx.doi.org/10.1089/acm.2006.6117. [DOI] [PubMed] [Google Scholar]
- 30.Lin PC. An evaluation of the effectiveness of relaxation therapy for patients receiving joint replacement surgery. J Clin Nurs. 2012 Mar;21(5–6):601–8. doi: 10.1111/j.1365-2702.2010.03406.x. DOI: http://dx.doi.org/10.1111/j.1365-2702.2010.03406.x. [DOI] [PubMed] [Google Scholar]
- 31.Armstrong K, Dixon S, May S, Patricolo GE. Anxiety reduction in patients undergoing cardiac catheterization following massage and guided imagery. Complement Ther Clin Pract. 2014 Nov;20(4):334–8. doi: 10.1016/j.ctcp.2014.07.009. DOI: http://dx.doi.org/10.1016/j.ctcp.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 32.Rhodes MK, Morris AH, Lazenby RB. Nursing at its best: competent and caring. Online J Issues Nurs. 2011 Feb 23;16(2):10. DOI: http://dx.doi.org/10.3912/OJIN.VOL16No02PPT01. [PubMed] [Google Scholar]
- 33.Scott CE, Bugler KE, Clement ND, MacDonald D, Howie CR, Biant LC. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br. 2012 Jul;94(7):974–81. doi: 10.1302/0301-620X.94B7.28219. DOI: http://dx.doi.org/10.1302/0301-620X.94B7.28219. [DOI] [PubMed] [Google Scholar]
- 34.Oschman J. Energy medicine in therapeutics and human performance. Edinburgh, Scotland: Butterworth Heinemann; 2003. [Google Scholar]