Developing and administering a warfarin Patient Self-Management (PSM) education program for those with atrial fibrillation was feasible. There was improvement in PSM competency (34.9% to 95.3%) and high levels of self-reported comfort (100% prepared to self-manage warfarin and 93% comfortable changing doses on their own).
Abstract
Introduction:
Although improved anticoagulation therapy outcomes have been demonstrated in clinical trials evaluating warfarin patient self-management (PSM) programs, these studies did not provide detailed information regarding PSM program development and patient training.
Objective:
To evaluate the feasibility of and methods for developing and administering an education program to support a novel pilot warfarin PSM program.
Methods:
Patients receiving warfarin for atrial fibrillation were recruited to participate in a prospective, intervention-only, open-label pilot PSM program that released venipuncture international normalized ratio results to patients via a secure, online Web site. To support the pilot, a warfarin PSM education program with a dosing algorithm was developed and delivered to patients during a two-hour classroom session.
Main Outcome Measure:
A comparison of participants’ PSM competency test scores before and after attending the PSM program.
Results:
Forty-four patients attended the education program. The mean age of participants was 71 years and 50% were women. Patients declining study participation were older (p = 0.003) and had a greater burden of chronic disease (p = 0.005) than participants. Following PSM training, the mean competency score improved from 55.8% to 88.8% (p < 0.001), and the proportion achieving a passing score increased from 34.9% to 95.3% (p < 0.001). In the poststudy survey, 100% of responders perceived that PSM training prepared them to self-manage warfarin, and 92.9% of responders were comfortable changing warfarin doses on their own.
Conclusion:
Developing and administering a warfarin PSM education program for patients with atrial fibrillation was feasible. Improvement in PSM competency and high levels of self-reported comfort with warfarin PSM were identified.
INTRODUCTION
Vitamin K antagonists, such as warfarin, have been shown to decrease thromboembolic events.1 However, warfarin’s narrow therapeutic index necessitates frequent dosage adjustments on the basis of international normalized ratio (INR) results to optimize therapeutic efficacy (ie, prevent thrombosis) and to minimize the potential for adverse reactions (primarily bleeding).1
In traditional anticoagulation models, INRs are measured from blood obtained via venipuncture or fingerstick and the result is reported to anticoagulation providers.1 The patient then receives instructions on anticoagulant management from his or her anticoagulation provider.1 Patient self-management (PSM) is an alternative model of anticoagulation therapy delivery where the responsibility for warfarin dosage decision making is transferred to the patient once PSM competency has been demonstrated.2 Several meta-analyses of randomized, controlled trials comparing PSM with usual care reported a significant reduction in thromboembolic events associated with PSM with some also showing reductions in mortality.3–5 Self-adjustment of warfarin doses in randomized, controlled trials was typically accomplished by providing patients with a dosing algorithm to be used in conjunction with INR results derived from blood samples obtained via fingerstick and analyzed using point-of-care (POC) INR monitors.
Training is an essential component of PSM. PSM training programs ranging from 15 minutes to 2 half-days have been described in the literature,6–10 but detailed information regarding the development and content of such PSM training courses is scarce. Guidelines recommend PSM training programs provide patients with information on blood coagulation, warfarin drug interactions, monitoring with POC devices, evaluation of INR results and warfarin dose adjustments, signs and symptoms of bleeding and thrombosis, frequency of INR monitoring, record keeping, and information on travel and nutrition.11,12 However, these guidelines make no recommendations on delivery of this information, training program duration, or how to assess PSM competency at the conclusion of training.
The Clinical Pharmacy Anticoagulation and Anemia Service (CPAAS) at Kaiser Permanente Colorado (KPCO) provides comprehensive anticoagulation management services for approximately 9000 members. Blood for INR measurement is obtained by venipuncture at any of the 27 KPCO medical office laboratories without appointment. The results of INR testing are then reported to the ordering CPAAS practitioner through an electronic medical record and are simultaneously viewable by patients via a secure online messaging system. Traditional anticoagulation management by CPAAS in this model has demonstrated improved INR control and a reduction in the rate of anticoagulation therapy-related adverse events.13 Several small studies have demonstrated that PSM of warfarin results in INR control that is equivalent to that of specialized anticoagulation clinics,14,15 which indicates that this model could potentially be used in a large specialized anticoagulation service such as CPAAS. Although intensive intervention will always be required for complex and nonadherent patients, other models of anticoagulation management for relatively stable patients may benefit both patients and anticoagulation management staff.
The purpose of this study was to evaluate the feasibility and methods of developing and administering an education program to support a novel pilot warfarin PSM program whereby patients manage their own warfarin therapy using INRs measured from blood drawn by venipuncture at a medical office laboratory.
METHODS
Study Design and Setting
This was a descriptive study examining the feasibility and methods of developing and administering training for a warfarin PSM education program. The PSM pilot study occurred in two phases. The focus of this report is on the first phase, which consisted of developing the education program and recruiting and educating patients regarding warfarin PSM. The recruitment and training of patients occurred between January 2011 and February 2011. The second phase evaluating warfarin PSM outcomes is described in a separate report.16 Approval from the KPCO institutional review board was obtained for all study phases.
At KPCO, venipuncture-acquired INR results are routed electronically to the managing CPAAS pharmacist for assessment and clinical decision making. The patient is then informed of the INR result, the dose of warfarin to take, and the next INR assessment date via letter, telephone, or a secure online Web site (My Health Manager). My Health Manager allows patients to have access to health information, such as laboratory results, and to communicate via secure electronic mail with health care practitioners.
Study Participants
Eligible patients were 1) at least age 18 years; 2) receiving warfarin therapy for atrial fibrillation with 5 mg tablets, a goal INR range of 2.0 to 3.0, and at least 6 months of treatment before study recruitment; 3) willing to provide written informed consent; and 4) able to access My Health Manager. Patients were excluded if they 1) had a planned surgery/invasive procedure during the 3-month study period; 2) missed more than one ordered INR test within the 6 months before enrollment; 3) resided in a skilled nursing, assisted living, or long-term care facility; 4) had planned time away from the KPCO service area for more than 7 consecutive days during the 3-month study period; 5) had a gap in Health Plan membership exceeding 30 days in the 6 months before enrollment; 6) were non-English speaking; or 7) were deemed inappropriate for study participation by CPAAS program (eg, memory impairment, difficulty following instructions). To simplify development of a warfarin dosing algorithm, patients were also excluded if their warfarin dose was < 17.5 mg or > 70 mg per week.
Study Outcomes
The primary outcome was whether the education and competency assessment components of the program could be used to successfully train consenting participants in warfarin PSM. Training was deemed successful if the proportion of patients demonstrating PSM competency increased after the PSM education phase. Secondary outcomes included the assessment of participants’ perceptions of education program quality and ease of use of the warfarin dosing algorithm after completion of the 3-month PSM pilot phase. Characteristics of patients who agreed or declined to participate in the pilot were also compared.
Patient Self-Management Training Development Process
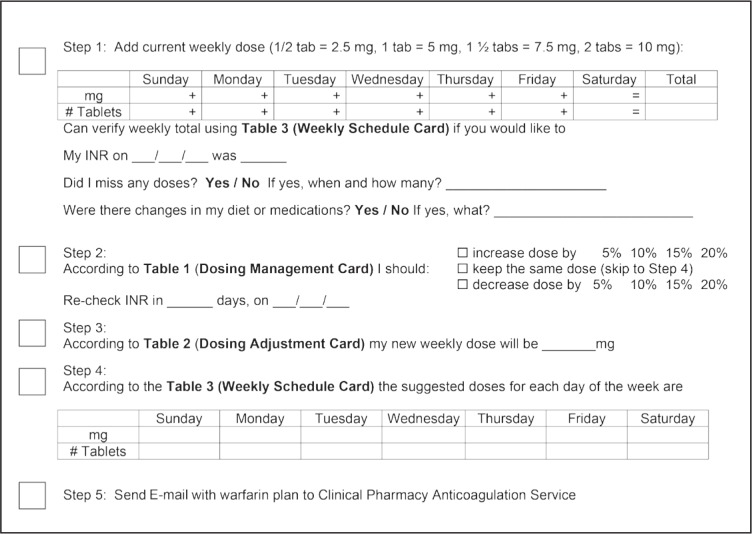
A warfarin PSM dosing algorithm consisting of three paper-based visual aids was developed. These aids consisted of a Dosage Management Card (Figure 1), a Dosage Adjustment Card (Figure 2), and a Weekly Schedule Card (Figure 3). These dosing aids were incorporated into a step-by-step PSM process as follows: 1) determining the total weekly warfarin dose in milligrams; 2) using the Dosage Management Card and current INR to determine how much to adjust the dose (0% to 20%) and when to obtain the next INR; 3) using the Dosage Adjustment Card to determine new weekly dose in milligrams; 4) using the Weekly Schedule Card to determine daily doses; and 5) relaying therapeutic plans to CPAAS pharmacists via a secure electronic message using My Health Manager. During the PSM training, patients learned how to use worksheets detailing the step-by-step process as an aid in dosing management decisions (Figure 4).
Figure 1.
Dosage management card.
INR = international normalized ratio; PT = prothrombin time.
Figure 2.
Dosage adjustment card.
Figure 3.
Weekly schedule card
Tab = tablet.
Figure 4.
Warfarin self-management worksheet/checklist
INR = international normalized ratio; tab = tablet.
A warfarin PSM competency assessment was developed and consisted of multiple-choice and short-answer questions. Four multiple-choice questions assessed knowledge of 1) the effect of vitamin K on INR, 2) recognizing and managing warfarin drug interactions, 3) distinguishing between serious and common bleeding complications, and 4) managing missed warfarin doses. Six short-answer questions assessed the following competencies: 1) adjusting warfarin doses on the basis of a low, slightly elevated, and significantly elevated INR; and 2) determining when to obtain a follow-up INR for each of these scenarios.
After providing informed consent, participants attended a 2-hour live training session before commencement of PSM. The competency test was administered to assess baseline knowledge before receiving education. During training, a slide presentation facilitated education regarding 1) warfarin; 2) obtaining INR results through My Health Manager; 3) adjusting warfarin doses using the 5-step process described above; 4) managing warfarin drug and dietary interactions; 5) managing missed warfarin doses; 6) responding to symptoms of bleeding and stroke; and 7) relaying therapeutic plans to CPAAS pharmacists using My Health Manager. Participants applied these principles to case-based problems, adjusting warfarin doses for various INRs, and making decisions on the basis of missed doses or drug/food interactions. At the end of the training session, the competency test was read-ministered with those participants achieving a score of at least 70% eligible to continue on to the PSM phase of the study.
Data Collection
Data regarding baseline patient characteristics for participants and nonparticipants were obtained via administrative data queries and included age, sex, risk factors for stroke and bleeding, time in therapeutic range during the 90-day pre-invitation phase, and length of time since enrollment in CPAAS. Information regarding household annual income and college education was collected administratively. A Chronic Disease Score, a measure of chronic illness burden, was calculated for all participants using administrative data from their pharmacy purchases in the six months before study enrollment.17,18
A postpilot survey aimed at assessing participant perceptions of the adequacy of the PSM training program was administered at the end of the PSM phase of the study using an online survey tool. This survey consisted of open-ended questions and 6 questions using a 5-point Likert-type scale with 1 being “Do Not Agree At All” and 5 being “Agree Completely.” A response of 4 or 5 was considered to be in agreement with the statement in question. The questions assessed the participants’ perceptions on 1) the quality of the training class and dosing cards and worksheets; 2) whether they were prepared for adjusting warfarin doses and managing drug interactions; 3) whether they understood more about warfarin after attending the class; and 4) class size.
Data Analysis
Descriptive statistics were used to summarize baseline characteristics. Pre- and posteducation session mean test scores and the proportion of participants who achieved a passing test score were compared using a paired t test and McNemar’s test, respectively. Differences in baseline patient demographic characteristics between participants and nonparticipants were compared using the χ2 test of association or Fisher exact test and Wilcoxon rank sum test, as appropriate. Alpha was set at 0.05. SAS, version 9.1.3 (SAS Institute, Cary, NC), statistical software was used for analyses.
RESULTS
Of 506 patients screened for enrollment, 167 were eligible to participate and 44 (26.3%) consented to enroll in the study (Figure 5). Participants in the PSM training were younger (70.6 vs 74.6 years, p = 0.003) and had lower mean Chronic Disease Score (6.7 vs 8.0, p = 0.005) but were otherwise similar to nonparticipants (Table 1).
Figure 5.
Patient disposition in study of patient self-management of warfarin.
INR = international normalized ratio
Table 1.
Patient characteristics by participation status
| Characteristic | Participant (n = 44) | Nonparticipant (n = 123) | p value |
|---|---|---|---|
| Mean age (median, SD)a | 70.6 (71, 6.9) | 74.6 (75, 8.1) | 0.003 |
| Female sex, n (%) | 22 (50) | 52 (42) | 0.424 |
| Risk factors, n (%)b | |||
| Prior thromboembolism | 1 (2) | 3 (2) | 0.951 |
| Prior stroke | 1 (2) | 5 (4) | 0.584 |
| Prior bleed | 3 (7) | 15 (12) | 0.324 |
| Cancer | 1 (2) | 3 (2) | 0.951 |
| Diabetes | 6 (14) | 24 (20) | 0.384 |
| Heart failure | 4 (9) | 21 (17) | 0.203 |
| Hypertension | 18 (41) | 66 (54) | 0.147 |
| Mean family income in $ for the patient’s Census Block (median $, SD)c | 68,126 (63,634; 24,450) | 66,559 (63,917; 23,871) | 0.810 |
| Mean percentage of persons in the patient’s Census Block with at least some college education (median %, SD)c | 25 (26, 5) | 24 (24, 6) | 0.839 |
| Mean percentage of INRs in therapeutic range (median %, SD)d | 79 (78, 20) | 80 (80, 18) | 0.572 |
| Mean length of time in days since enrollment in CPAAS (median days, SD)a | 1760 (1379, 1408) | 1663 (1481, 1181) | 0.981 |
| Mean Chronic Disease Score (median, SD) | 6.7 (6, 2.5) | 8.0 (8, 2.6) | 0.005 |
As of January 19, 2011.
Diagnosed in a medical office from July 1, 2010, through January 19, 2011.
Based on 2010 census data.
From laboratory results drawn in the 90 days before January 19, 2010.
CPAAS = Clinical Pharmacy Anticoagulation and Anemia Service; INR = international normalized ratio; SD = standard deviation.
A total of 13 two-hour training sessions were conducted to train the 44 participants. Class sizes ranged from 1 to 8 participants with 1 to 3 study team members present at each session. The mean pretest score was 55.8% (±19.5%) with only 15 participants (34.9%) achieving a passing score. One participant voluntarily withdrew from the study before taking the posteducation competency test and two participants voluntarily withdrew consent after successfully completing the posteducation competency test but before beginning the PSM phase of the study. After attendance at the PSM training program the absolute improvement in competency test scores and participants achieving a passing score were 33.0% and 60.4%, respectively (p < 0.001 for both) (Table 2).
Table 2.
Competency test result, N = 43
| Competency test | Score |
|---|---|
| Mean pre-education score, % (SD) | 55.8 (19.5) |
| Mean posteducation score, % (SD) | 88.8 (13.5) |
| Mean score change, % (SD) | 33.0 (19.2) |
| Patients with passing score | |
| Pre-education, no. (% of N) | 15 (34.9) |
| Posteducation, no. (% of N) | 41 (95.3) |
| Change in passing, no. (% of N) | 26 (60.4)a |
p < 0.001 compared with pre-education.
SD = standard deviation.
Twenty-eight of 39 (71.8%) participants completed the anonymous online survey assessing their perceptions of the training program and/or materials (Table 3). The majority of participants expressed favorable impressions of the training program. Preference for group vs one-on-one training sessions was mixed with a slight majority favoring group sessions.
Table 3.
Postpilot survey of perceptions of the patient self-management training by 28 participantsa
| Perception | Participants in agreement, % |
|---|---|
| The training class prepared me to manage warfarin on my own. | 100 |
| I prefer a group training class over one-on-one instruction. | 64.3 |
| The warfarin dosing cards and worksheets were easy to use. | 96.4 |
| I felt comfortable changing warfarin doses on my own. | 92.9 |
| I knew what I should do with my warfarin treatment when I changed one of my other medications. | 75 |
| I understand my warfarin treatment better after being in the study. | 89.3 |
Response rate was 71.8%.
DISCUSSION
We developed and implemented a program to train patients in warfarin PSM and successfully enrolled and trained 26.3% of eligible patients. Our program differed from other warfarin PSM programs in that INR results were acquired via venipuncture instead of POC devices and results were conveyed to participants using a secure online messaging system. Only one other small PSM pilot study utilizing venipuncture-based INR testing has been published to date.4 In that study INR results were relayed to patients via mail or in person.4 Such methods delay receipt of INR results compared with our study, where INR results from our secure online messaging system were released in real time.
Notably, the rate of eligible patients who enrolled in our study was similar to prior POC-based studies, suggesting that using venipuncture-based INR testing did not substantially increase acceptability of warfarin PSM.19 However, our findings do indicate that PSM using venipuncture INRs conveyed to patients via a secure online messaging system can be a viable method of warfarin therapy management for carefully selected patients provided these patients receive thorough PSM training.
For our pilot, study participation was limited by relatively strict inclusion and exclusion criteria. We studied only one indication for warfarin therapy using a single warfarin tablet strength to simplify development of the training material and dosing visual aids. Patients also were required to be active users of the secure online KPCO messaging system, further limiting our pool of eligible study participants. However, this criterion provided our pilot with patients who had access to their INR results the same day the test was performed, thus providing rapid INR results analogous to POC INR testing. In addition, because the most common reason for exclusion from our pilot was having missed more than one INR test in the previous six months, eligible patients were generally adherent to the demands of warfarin therapy monitoring.
We noted differences between patients who agreed to participate in the study and those declining participation. Participants were slightly younger and had lower burden of chronic disease than those who did not participate. We are unaware of any other PSM studies that compared patients agreeing and declining to participate; however, one study found that patients who completed PSM training were younger and more educated than patients who did not complete training.20 Patients responded positively to the training program; however, on the basis of the post-PSM survey, the portion of the PSM training focusing on management of drug interactions could be improved.
A potential barrier to widespread use of PSM is the initial time investment in training patients. Fifty-two study-staff hours were required to train 44 patients in PSM using our training method (including obtaining informed consent). Although current guidelines suggest classes with 3 to 6 participants,9,10 we found success with class sizes ranging up to 8 participants. Compared with PSM studies using POC machines, our program appeared to require less training time, probably in part because training patients to use POC devices for INR measurement was not required. In the future, to reduce the time commitment involved in PSM training, technology could be leveraged to create a Web-based PSM training program that patients could easily access from home. This would remove the need for patient travel and trainer travel and might decrease the time required to train patients in PSM. Providing opportunities for patients to ask questions in a Web-based training program might be challenging but could be achieved by using a live Webinar format. Although limited data exist for using Webinars for patient education, available data suggest that it may be a viable option.21
There were several limitations to our study. Because this was a pilot, the sample size was small and a control group was not employed. The external validity of our results may be influenced by the study setting and the requirement for access and ability to use a computer with Internet access. However, secure online messaging systems are becoming more common in integrated health care models, and according to 2013 US Census data, 74.4% of households have Internet access with this number steadily increasing over time.22 To this end, only 49 patients screened for our study did not meet inclusion criteria because they were not active on My Health Manager.
CONCLUSION
Developing and administering a focused education program and dosing algorithm for warfarin PSM using venipuncture INR results released through a secure Web site is feasible. The results of this pilot study may be used to inform the design of a randomized, controlled trial of this intervention compared with usual care practices.
Acknowledgments
Mary Corrado, ELS, provided editorial assistance.
Footnotes
Disclosure Statement
The authors of this article have no conflicts of interest to disclose.
This study was funded by the Kaiser Permanente Colorado Pharmacy Department.
References
- 1.Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G, American College of Chest Physicians Oral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e44S–88S. doi: 10.1378/chest.11-2292. DOI: http://dx.doi.org/10.1378/chest.11-2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ansell JE. Empowering patients to monitor and manage oral anticoagulation therapy. JAMA. 1999 Jan 13;281(2):182–3. doi: 10.1001/jama.281.2.182. DOI: http://dx.doi.org/10.1001/jama.281.2.182. [DOI] [PubMed] [Google Scholar]
- 3.Heneghan C, Ward A, Perera R, Self-Monitoring Trialist Collaboration et al. Self-monitoring of oral anticoagulation: systematic review and meta-analysis of individual patient data. Lancet. 2012 Jan 28;379(9813):322–34. doi: 10.1016/S0140-6736(11)61294-4. DOI: http://dx.doi.org/10.1016/S0140-6736(11)61294-4. [DOI] [PubMed] [Google Scholar]
- 4.Christensen TD, Johnsen SP, Hjortdal VE, Hasenkam JM. Self-management of oral anticoagulant therapy: a systematic review and meta-analysis. Int J Cardiol. 2007 May 16;118(1):54–61. doi: 10.1016/j.ijcard.2006.06.018. DOI: http://dx.doi.org/10.1016/j.ijcard.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Alamino JM, Ward AM, Alonso-Coello P, et al. Self-monitoring and self-management of oral anticoagulation. Cochrane Database Syst Rev. 2010 Apr 14;(4):CD003839. doi: 10.1002/14651858.CD003839.pub2. DOI: http://dx.doi.org/10.1002/14651858.CD003839.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Grunau BE, Wiens MO, Harder KK. Patient self-management of warfarin therapy: pragmatic feasibility study in Canadian primary care. Can Fam Physician. 2011 Aug;57(8):e292–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Khan TI, Kamali F, Kesteven P, Avery P, Wynne H. The value of education and self-monitoring in the management of warfarin therapy in older patients with unstable control of anticoagulation. Br J Haematol. 2004 Aug;126(4):557–64. doi: 10.1111/j.1365-2141.2004.05074.x. DOI: http://dx.doi.org/10.1111/j.1365-2141.2004.05074.x. [DOI] [PubMed] [Google Scholar]
- 8.Ansell JE, Patel N, Ostrovsky D, Nozzolillo E, Peterson AM, Fish L. Long-term patient self-management of oral anticoagulation. Arch Intern Med. 1995 Nov 13;155(20):2185–9. DOI: http://dx.doi.org/10.1001/archinte.1995.00430200066010. [PubMed] [Google Scholar]
- 9.Sawicki PT. A structured teaching and self-management program for patients receiving oral anticoagulation: a randomized controlled trial. Working Group for the Study of Patient Self-Management of Oral Anticoagulation. JAMA. 1999 Jan 13;281(2):145–50. doi: 10.1001/jama.281.2.145. DOI: http://dx.doi.org/10.1001/jama.281.2.145. [DOI] [PubMed] [Google Scholar]
- 10.Newall F, Monagle P, Johnston L. Home INR monitoring of oral anticoagulant therapy in children using the CoaguChek S point-of-care monitor and a robust education program. Thromb Res. 2006;118(5):587–93. doi: 10.1016/j.thromres.2005.08.004. DOI: http://dx.doi.org/10.1016/j.thromres.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 11.Ansell J, Jacobson A, Levy J, Völler H, Hasenkam JM, International Self-Monitoring Association for Oral Anticoagulation Guidelines for implementation of patient self-testing and patient self-management of oral anticoagulation. International consensus guidelines prepared by International Self-Monitoring Association for Oral Anticoagulation. Int J Cardiol. 2005 Mar 10;99(1):37–45. doi: 10.1016/j.ijcard.2003.11.008. DOI: http://dx.doi.org/10.1016/j.ijcard.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Fitzmaurice DA, Gardiner C, Kitchen S, Mackie I, Murray ET, Machin SJ, British Society of Haematology Taskforce for Haemostasis and Thrombosis An evidence-based review and guidelines for patient self-testing and management of oral anticoagulation. Br J Haematol. 2005 Oct;131(2):156–65. doi: 10.1111/j.1365-2141.2005.05739.x. DOI: http://dx.doi.org/10.1111/j.1365-2141.2005.05739.x. [DOI] [PubMed] [Google Scholar]
- 13.Witt DM, Sadler MA, Shanahan RL, Mazzoli G, Tillman DJ. Effect of a centralized clinical pharmacy anticoagulation service on the outcomes of anticoagulation therapy. Chest. 2005 May;127(5):1515–22. doi: 10.1378/chest.127.5.1515. DOI: http://dx.doi.org/10.1378/chest.127.5.1515. [DOI] [PubMed] [Google Scholar]
- 14.Cromheecke ME, Levi M, Colly LP, et al. Oral anticoagulation self-management and management by a specialist anticoagulation clinic: a randomised crossover comparison. Lancet. 2000 Jul 8;356(9224):97–102. doi: 10.1016/S0140-6736(00)02470-3. DOI: http://dx.doi.org/10.1016/S0140-6736(00)02470-3. [DOI] [PubMed] [Google Scholar]
- 15.McCahon D, Murray ET, Jowett S, et al. Patient self management of oral anticoagulation in routine care in the UK. J Clin Pathol. 2007 Nov;60(11):1263–7. doi: 10.1136/jcp.2006.044008. DOI: http://dx.doi.org/10.1136/jcp.2006.044008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simmons BJ, Jenner KM, Delate T, Clark NP, Kurz D, Witt DM. Pilot study of a novel patient self-management program for warfarin therapy using venipuncture-acquired international normalized ratio monitoring. Pharmacotherapy. 2012 Dec;32(12):1078–84. doi: 10.1002/phar.1139. DOI: http://dx.doi.org/10.1002/phar.1139. [DOI] [PubMed] [Google Scholar]
- 17.Clark DO, Von Korff M, Saunders K, Baluch WM, Simon GE. A chronic disease score with empirically derived weights. Med Care. 1995 Aug;33(8):783–95. doi: 10.1097/00005650-199508000-00004. DOI: http://dx.doi.org/10.1097/00005650-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Von Korff M, Wagner EH, Saunders K. A chronic disease score from automated pharmacy data. J Clin Epidemiol. 1992 Feb;45(2):197–203. doi: 10.1016/0895-4356(92)90016-g. DOI: http://dx.doi.org/10.1016/0895-4356(92)90016-G. [DOI] [PubMed] [Google Scholar]
- 19.Bloomfield HE, Krause A, Greer N, et al. Meta-analysis: effect of patient self-testing and self-management of long-term anticoagulation on major clinical outcomes. Ann Intern Med. 2011 Apr 5;154(7):472–82. doi: 10.7326/0003-4819-154-7-201104050-00005. DOI: http://dx.doi.org/10.7326/0003-4819-154-7-201104050-00005. [DOI] [PubMed] [Google Scholar]
- 20.Murray E, Fitzmaurice D, McCahon D, Fuller C, Sandhur H. Training for patients in a randomised controlled trial of self management of warfarin treatment. BMJ. 2004 Feb 21;328(7437):437–8. doi: 10.1136/bmj.328.7437.437. DOI: http://dx.doi.org/10.1136/bmj.328.7437.437. Erratum in: BMJ 2004 Mar;328(7439)563. DOI: http://dx.doi.org/10.1136/bmj.328.7439.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reinke LF, Griffith RG, Wolpin S, Donesky-Cuenco D, Carrieri-Kohlman V, Nguyen HQ. Feasibility of a webinar for coaching patients with chronic obstructive pulmonary disease on end-of-life communication. Am J Hosp Palliat Care. 2011 May;28(3):147–52. doi: 10.1177/1049909110376807. DOI: http://dx.doi.org/10.1177/1049909110376807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Computer and internet use [Internet] Washington DC: United States Census Bureau; 2014. Oct 27, [cited 2014 Dec 16]. Available from: www.census.gov/hhes/computer/. [Google Scholar]