Abstract
Background Both the dorsal and the volar portion of the scapholunate interosseous ligament (SLIL) are major stabilizers of the scapholunate (SL) joint. Most reconstruction methods to restore SL stability do not address the volar constraints and frequently fail to reduce the SL gapping. Wrist arthroscopy allows a complete evaluation of the SL interval, accompanying ligament status, and associated SL advanced collapse (SLAC) wrist changes. It enables simultaneous reconstruction of the dorsal and palmar SL ligaments anatomically with the use tendon graft in a boxlike structure.
Materials and Methods From October 2002 to June 2012, the treatment method was applied in 17 patients of chronic SL instability of average duration of 9.5 months (range 1.5–18 months). There were three Geissler grade 3 and 14 grade 4 instability cases. The average preoperative SL interval was 4.9 mm (range 3–9 mm). Dorsal intercalated segment instability (DISI) deformity was present in 13 patients. Six patients had stage 1 SLAC wrist change radiologically. Concomitant procedures were performed in four patients.
Description of Technique With the assistance of arthroscopy and intraoperative imaging as a guide, a combined limited dorsal and volar incision exposed the dorsal and palmar SL interval without violating the wrist joint capsule. Bone tunnels of 2.4 mm were made on the proximal scaphoid and lunate. A palmaris longus tendon graft was delivered through the wrist capsule and the bone tunnels to reduce and connect the two bones in a boxlike fashion. Once the joint diastasis is reduced and any DISI malrotation corrected, the tendon graft was knotted and sutured on the dorsal surface of the SL joint extra-capsularly in a shoe-lacing manner. The scaphocapitate joint was transfixed with Kirschner wires (K-wires) to protect the reconstruction for 6–8 weeks.
Results The average follow-up was 48.3 months (range 11–132 months). Thirteen returned to their preinjury job level. Eleven patients had no wrist pain, and six had some pain on either maximum exertion or at the extreme of motion. The average total pain score was 1.7/20 compared with the preoperative score of 8.3/20. The postoperative average total wrist performance score was 37.8/40, with an improvement of 35%. The average extension range improved for 13%, flexion range 16%, radial deviation 13%, and ulnar deviation 27%. Mean grip strength was 32.8 kg (120% of the preoperative status, 84% of the contralateral side). The average SL interval was 2.9 mm (range 1.6–5.5 mm). Recurrence of a DISI deformity was noted in four patients without symptoms. Ischemic change of proximal scaphoid was noted in one case without symptoms or progression. There were no major complications. All patients were satisfied with the procedure and outcome.
Conclusion Our method of reconstructing both the dorsal and volar SL ligament, in a minimally invasive way, is a logical and effective technique to improve SL stability. The potential risk of ischemic necrosis of the carpal bone is minimized by preservation of the scaphoid blood supply, the small size of the bone tunnels created, and the inclusion of the capsule at the reconstruction site.
Keywords: wrist arthroscopy, scapholunate ligament, SL dissociation, wrist surgery, tendon graft
Scapholunate (SL) dissociation is the most common carpal instability.1 Numerous surgical techniques have been described to restore or improve the stability of the SL joint and to retard and prevent the progression to arthritis. These procedures included various forms of capsulodesis, static or dynamic tenodesis, ligament reconstruction employing tendon weaving, bone-retinaculum-bone reconstruction, and the reduction and association of the scaphoid and lunate (RASL) procedure. Nevertheless, it is difficult to create a vertical tether between the distal and proximal carpal row and to the distal radius without impairing normal wrist kinematics and midcarpal joint motion. Recurrent or persistent gapping, tendon loosening, technical difficulty, limited motion and grip strength, and fracturing of or through drill holes have been reported.2 3 4 5 6 7 8 9 10 11 Furthermore, most methods provide only dorsal and uni-planar reconstructions.
Many studies have emphasized the importance of the volar ligaments.12 13 14 15 It is logical and more ideal to restore both the dorsal and volar component of the SL ligament. In one biomechanical study Yi et al used a palmaris longus tendon to pass through drill holes in the anteroposterior plane of the scaphoid and the lunate. The SL diastasis was effectively reduced to normal, and the scaphoid and lunate contact pressure on the radius and the scaphoid-to-lunate contact ratio were significantly improved after the reconstruction.16 Zdero used bovine tendons passing through double bone tunnels of the scaphoid and lunate in 19 cadaveric wrists.17 There was no difference in the mechanical property from the normal wrists. These cadaveric study results support the clinical application of a combined dorsal and volar SL ligament reconstruction.
In 2002, we developed an arthroscopic assisted technique to reconstruct both the dorsal and volar SL ligament simultaneously using a free tendon graft in a boxlike structure without violating the major blood supply to the scaphoid and soft tissue envelope (Fig. 1). The indication was subacute and chronic SL dissociation of 6 weeks or beyond. Both dynamic and static instabilities were appropriate, as long as the SL diastasis and dorsal intercalated segmental instability (DISI) deformity were reducible, as confirmed arthroscopically and radiologically.
Fig. 1.
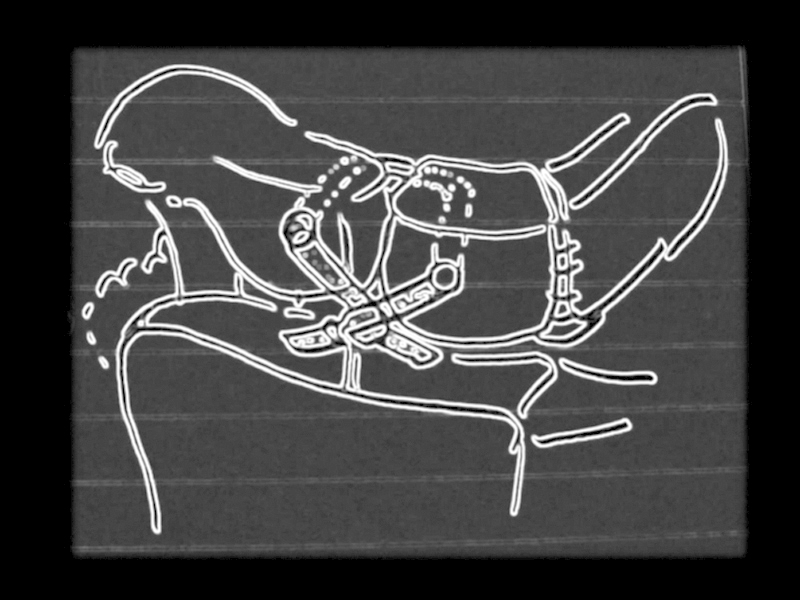
Simultaneous reconstruction of the dorsal and palmar SL ligaments anatomically with the use of tendon graft in a boxlike structure.
Materials and Patients
From October 2002 to June 2012, 17 patients with SL dissociation underwent an arthroscopic assisted SL ligament reconstruction. There were 15 male and 2 female patients. The mean age was 42 (range 26–60 years). The dominant wrist was involved in all patients. The mean duration from injury to treatment was 9.5 months (range 1.5–28 months). Nine were injured in sports activities, three had a fall on outstretched hands, and three were injured in road traffic accidents. Workers' compensation was involved in five patients. All patients had chronic dorsal or dorsoradial wrist pain occurring especially at the extremes of motion and on exertion, and eight had subjective weakness and a sense of instability with painful clicking. The physical examination revealed tenderness at or around the SL interval in all cases. The Watson's test was positive in 11 out of the 17 cases.
All patients were assessed by an occupational therapist before the operation and at regular intervals postoperatively, using an author-generated wrist score (Fig. 2).18 The mean preoperative total wrist performance score was 28/40 (range 13 to 36), and mean total pain score in performing the activities of daily living (ADL) tasks was 8.3/20 (range 1–18). The average wrist active extension range was 53° (range, 10–71°), flexion range 45° (range 10–76°), radial deviation 16° (range 5–25°), ulnar deviation 26° (range 10–43°). A visual analogue scale (VAS) for pain at daily maximum exertion averaged 6.2/10 (range 1–9). The power grip strength averaged 27.3 kg, which was 74% of the contralateral side.
Fig. 2.
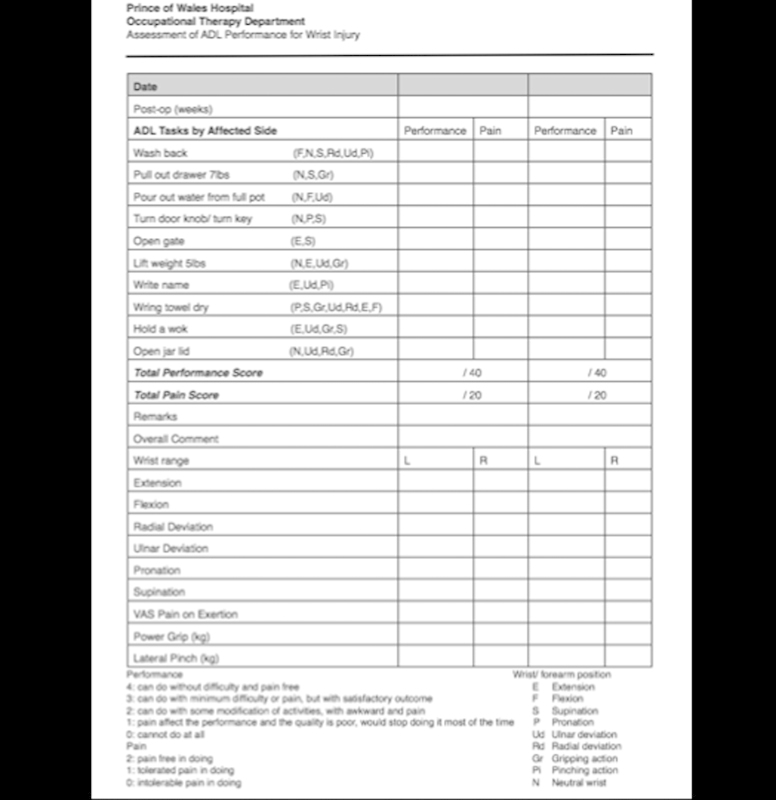
Record sheet of the wrist function assessment performed by an occupational therapist. It consists of 5 elements, which are performance evaluation, pain evaluation, wrist range of motion, pain VAS, and grip and pinch strength.
The SL interval was evaluated with a mini C-arm. The widest SL interval was documented and compared with the contralateral side. The mean SL gapping was 4.9 mm (range 3–9 mm). A true SPC (scaphoid-pisiform-capitate) lateral view was taken to assess the SL and capitolunate (CL) angles. The average SL angle was 85° (range, 52–102°), CL angle was 3.4° (range 0–20°). A DISI deformity was present in 13 patients, with an SL angle of more than 70°. A SLAC wrist stage I degeneration consisting of radial styloid narrowing was identified in six patients. Arthroscopy was performed in all cases. The SL instability was rated as a Geissler grade III in 3 cases and grade IV in 14 cases. Other findings at arthroscopy included radial styloid synovitis in 15, STT joint synovitis in 11, radial styloid cartilage degeneration in 10, a scaphoid fossa chondral lesion in 1, a lunate fossa chondral lesion in 3, a chondral defect of proximal scaphoid in 4, a chondral defect of proximal lunate in 2, a degenerative tear of the radioscaphocapitate and long radiolunate ligaments in 2, and a triangular fibrocartilage complex (TFCC) tear in 6. Concomitant procedures were performed in 7 cases, including TFCC débridement in 3, ulnar shortening osteotomy in 2, arthroscopic TFCC reconstruction in 1, and arthroscopic osteochondral grafting in 1.
Surgical Techniques
Diagnostic wrist arthroscopy under portal site local anesthesia can be performed prior to the definitive surgery when the SL dissociation cannot fully account for the wrist pain.19 This helps to evaluate the cause of the chronic wrist pain, confirm the status of the SL ligaments, evaluate the reducibility of the SL diastasis, and assess the cartilage and the SLAC changes.
The surgery was performed under general anesthesia or regional block. The patient was placed in a supine position with the arm suspended in a wrist traction tower under 10–13 lb of traction. The tourniquet was not initially inflated. 1:200,000 dilution of adrenaline was injected in the portal sites to reduce bleeding. Continuous saline irrigation of the joint was achieved with a bag of 3 L of normal saline instilled under gravity. Radiocarpal joint arthroscopy was performed initially through the 3–4 and 4–5 portals with 6U for outflow, followed by midcarpal joint (MCJ) arthroscopy through the midcarpal radial (MCR) and midcarpal ulnar (MCU) portals. Small transverse incisions were made along the skin creases for better scar appearance. A 1.9-mm or 2.7-mm arthroscope was used. The joint was inspected systematically and the findings documented. A synovectomy and radial styloidectomy was performed at the same time if necessary using a 2-mm shaver and 2.9-mm burr. Intra-articular fibrosis was resected with a shaver to improve the wrist motion and to facilitate a reduction of the SL malalignment and DISI deformity.
The tourniquet was then inflated and the reconstructive procedure was performed. A 2-cm transverse incision was extended from slightly radial to the 3–4 portal toward the 4–5 portal (Fig. 3). The extensor retinaculum was split along its oblique fibers. The extensor digitorum communis (EDC) was retracted ulnarly to expose the lunate. Radially the interval between the extensor carpi radialis brevis (ECRB) and the extensor carpi radialis longus (ECRL) was identified, which usually corresponded well to the ideal position of the scaphoid tunnel. Volarly, a transverse incision was made along the proximal wrist crease from the ulnar border of the palmaris longus to the ulnar border of the flexor carpi radialis (FCR) tendon (Fig. 4). A palmaris longus free graft was harvested by use of a tendon stripper. The anterior forearm fascia was incised. The interval between the flexor carpi radialis tendon and the finger flexor tendons and median nerve was entered to reach the volar wrist joint capsule. Both the volar and dorsal wrist joint capsules were preserved without violation. The wrist was then ready for bone tunnel preparation.
Fig. 3.
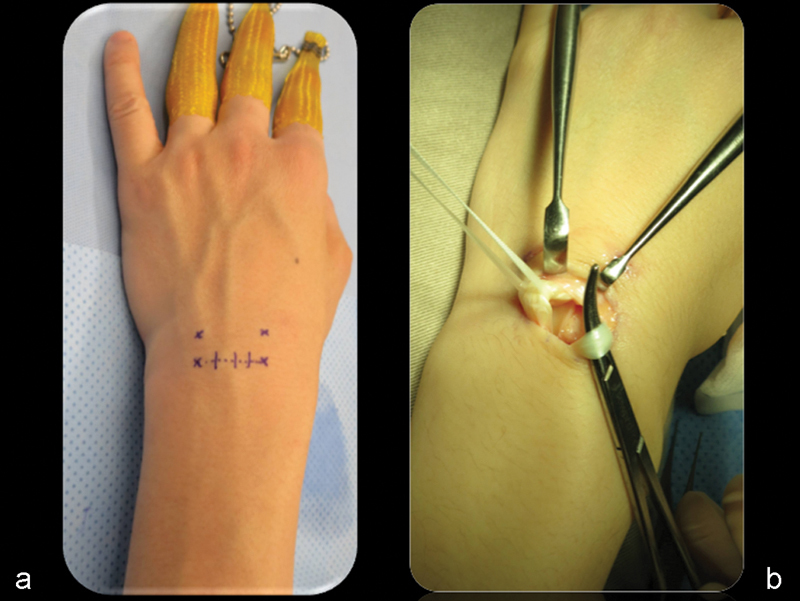
(a) Through a dorsal incision, (b) the extensor tendons are retracted, exposing the dorsal wrist capsule.
Fig. 4.
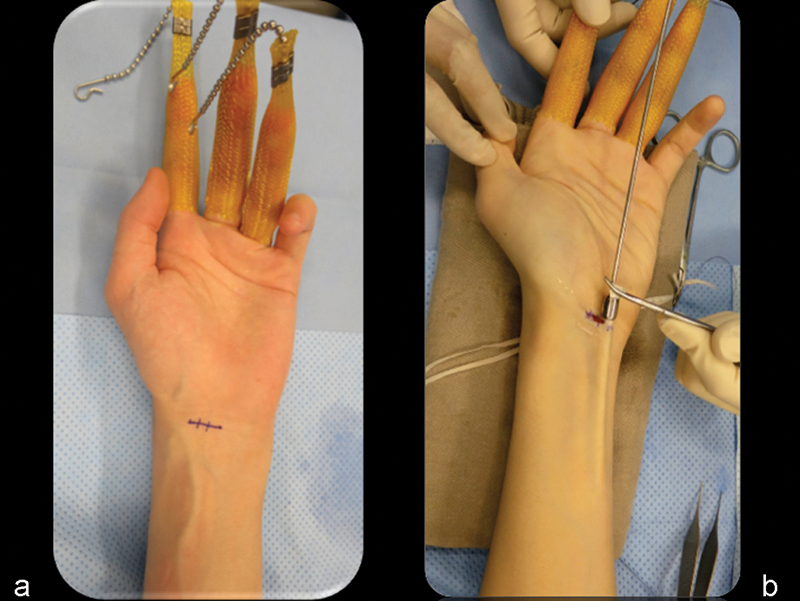
(a) Through a volar incision, (b)the PL graft can be harvested with the use of a tendon stripper.
The hand was examined fluoroscopically. If there was a DISI deformity, the extended posture of the lunate was corrected by flexing the wrist to restore the normal radiolunate angle, and the radiolunate joint was transfixed with a 1.6-mm Kirschner wire (K-wire) inserted percutaneously through the distal radius. The radiolunate (RL) pin was inserted in the ulnar half of the lunate to avoid conflict with the lunate bone tunnel. The wrist was then extended passively to correct the flexion deformity of the scaphoid and to restore a normal SL angle. If this was not possible, an additional arthroscopic release of the fibrosis around the scaphoid and lunate was performed. If the DISI deformity was still irreducible, then the SL reconstruction was abandoned (Fig. 5). Through the dorsal incision, the EDC tendons were retracted ulnarly, and a 1.1-mm guide pin was inserted using a drill guide under fluoroscopic guidance into the lunate. When the radius and lunate were well aligned with the RL pin, the path of the guide pin should be perpendicular to the long axis of the lunate; that is, parallel to the line joining the tip of the volar and dorsal lips of the lunate. The guide pin was about 2–3 mm from the bone margin and then was advanced toward the volar cortex. With the flexor tendons and median nerve, including the palmar cutaneous branch, carefully retracted ulnarly, the guide pin was was used to perforate the volar cortex of the lunate and exit through the volar wound (Fig. 6). Another guide pin was then inserted into the scaphoid through the interval between the ECRB and ECRL tendons. It was placed parallel to the lunate guide pin if the SL angle was corrected. Otherwise, it entered slightly more distal to the guide pin entry site of the lunate and was directed proximally and volarly, to provide a better counter-rotational force on the scaphoid to correct the flexion deformity (Fig. 7). With the the FCR tendon retracted radially, the scaphoid pin exited through the volar wound. Thenthe lunate and scaphoid tunnels were sequentially expanded with cannulated drill bits from 2.0 to 2.4 or 2.7 mm depending on the thickness of the palmaris longus graft. The smallest diameter drill hole for the smooth passage of the tendon graft was used, to avoid iatrogenic fracture or avascular necrosis. The free tendon graft was delivered through the bone tunnels with a 2-mm arthroscopic grasper, from the volar side of the scaphoid to dorsal, and from the volar aspect of the lunate to dorsal (Fig. 8). The tendon graft was passed outside the capsule to cross the SL interval so that the reconstruction also helped to tighten the capsule and the extrinsic ligaments, which conferred added stability to the SL joint.
Fig. 5.
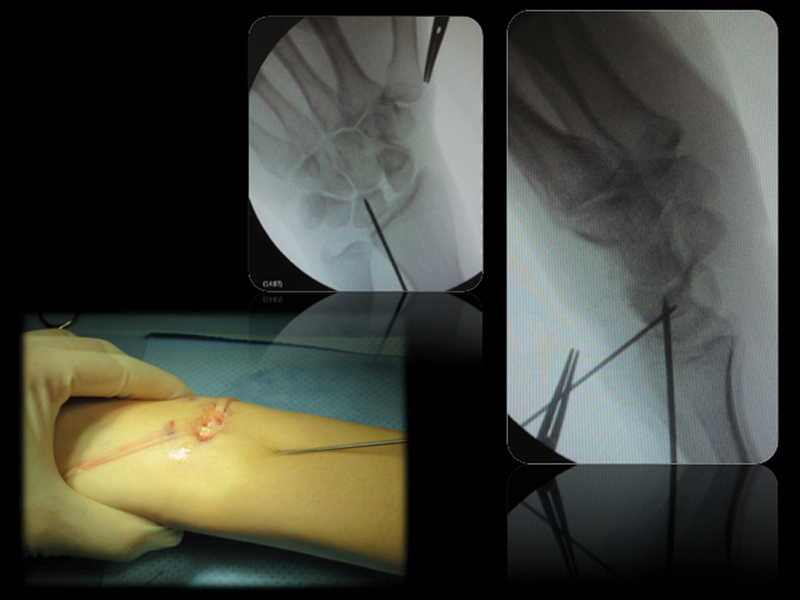
A DISI deformity of lunate is reduced by the Linscheid maneuver. The radiolunate joint is transfixed with a 1.6-mm K-wire with the lunate in a netural position. Another K-wire is positioned to prepare the lunate tunnel from a dorsal to volar direction.
Fig. 6.
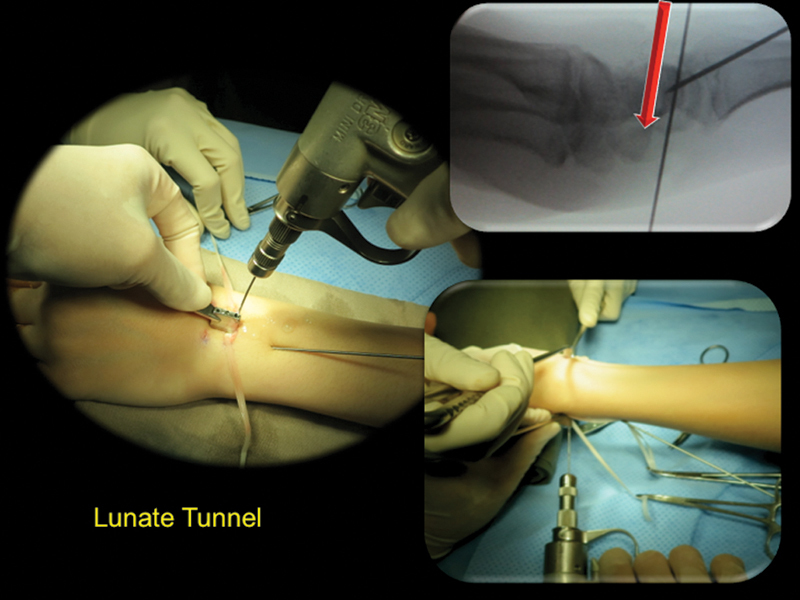
Preparation of the lunate tunnel with a K-wire inserted through the dorsal capsule from dorso-proximal to volar-distal direction.
Fig. 7.
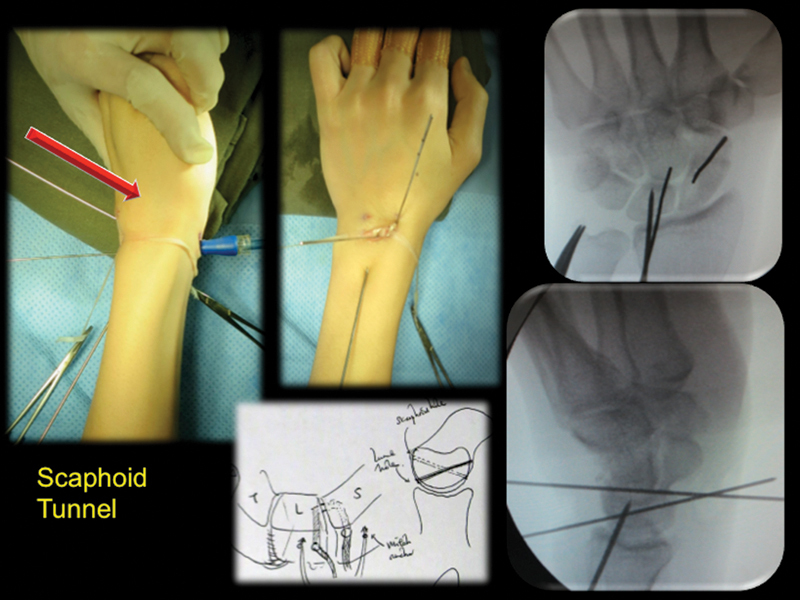
Preparation of the scaphoid tunnel with a K-wire inserted through the dorsal capsule from dorso-distal to volar-proximal direction.
Fig. 8.

A PL tendon graft is delivered through the wrist capsule and the bone tunnels to reduce the two bones in a boxlike fashion.
The MCJ was then inspected through either the MCR or MCU portal. The RL pin was then withdrawn from the lunate so that the lunate was mobile. With manual traction of the two ends of the tendon graft, any SL gapping or step-off was corrected. Any interposed tissue in the SL interval that prevented a complete reduction was excised arthroscopically. The reduction was be facilitated by using a large bone reduction clamp between the scaphoid and triquetrum. The tendon graft was maximally tensioned and tied in a shoelace manner over the dorsal capsule and secured with 2–0 nonabsorbable sutures (Fig. 9). SL stability was confirmed arthroscopically and fluoroscopically. The tendon graft was then tied once more and sutured. Two K-wires were inserted through a small incision in the anatomic snuffbox region to transfix the scaphocapitate (SC) joint to protect the reconstructed ligament during the healing process (Fig. 10). The K-wires were cut short and buried underneath the skin. Additional suture anchors were placed at the dorsal bone tunnels for the scaphoid and lunate for additional graft fixation. The radiolunate pin was then advanced to maintain the lunate reduction if necessary. The tendon knot was then sutured to the adjacent dorsal joint capsule and the extensor retinaculum was repaired. The tourniquet was released for hemostasis. The wound was closed with absorbable sutures. A bulky dressing and a scaphoid plaster slab were applied with wrist in a neutral position and the thumb in neutral palmar abduction.
Fig. 9.
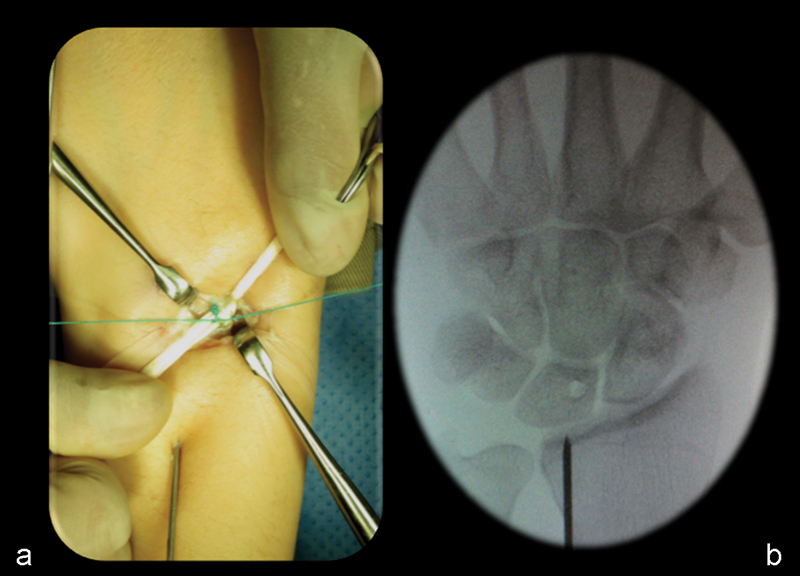
(a) The tendon graft is knotted and sutured under maximal tension on the dorsal surface of the SL joint extra-capsularly in shoelace manner. (b) Note the reduction of the SL interval on X-ray.
Fig. 10.

(a,b) The scaphocapitate joint is transfixed with 1.1-mm K-wires to protect the ligament reconstruction.
The wrist was immobilized in a short arm thumb spica cast for 6 weeks. The RL pin was removed at the beginning of the third week. The cast was then changed to a thumb spica splint for an additional 2 weeks, at which time gentle wrist mobilization was allowed out of the splint. The SC pins were removed at the beginning of the ninth week. The splint was worn at nighttime for another 4–6 weeks. Gradual wrist range of motion exercises under physiotherapy supervision were started after the pin removal. Gradual strengthening exercises were started at the beginning of the thirteenth week after surgery.
Results
The average follow-up was 48.3 months (range 11–132). Thirteen patients were able to return to their pre-injury job level, and four had some restriction at work. Eleven patients did not have any wrist pain at any time. Three had some wrist pain on maximum exertion. Four had some wrist pain at the extreme of motion. None of them had any wrist pain at rest. The average total pain score was 1.7/20 in performing the 10 ADL tasks, compared with the preoperative score of 8.3/20. VAS of pain at daily maximum exertion averaged 1.8/10 (preoperative 6.2/10). None of the patients had any tenderness at the SL interval. The Watson's test was negative in all. The average wrist extension improved 13% (postoperative active extension range 60.1°), flexion 16% (post-operative active flexion range 52°), radial deviation 13% (postoperative range 18°), and ulnar deviation 27% (postoperative range 33°). The postoperative average total wrist performance score was 37.8/40, with an improvement of 35%. The mean grip strength was 32.8 kg, which was 120% of the preoperative status and 84% of the contralateral side. Radiographically the average SL interval was 2.9 mm (range 1.6–5.5 mm, preoperative average 4.9 mm). In 15 patients, there was no difference in the SL interval at the time of K-wire removal from that at the final follow-up (Figs. 11 12 13 14 15) A recurrence of DISI deformity was noted in four patients. There was no further progression of degenerative changes in the six patients with SLAC stage 1, though 2 had more prominent radial styloid beaking.
Fig. 11.
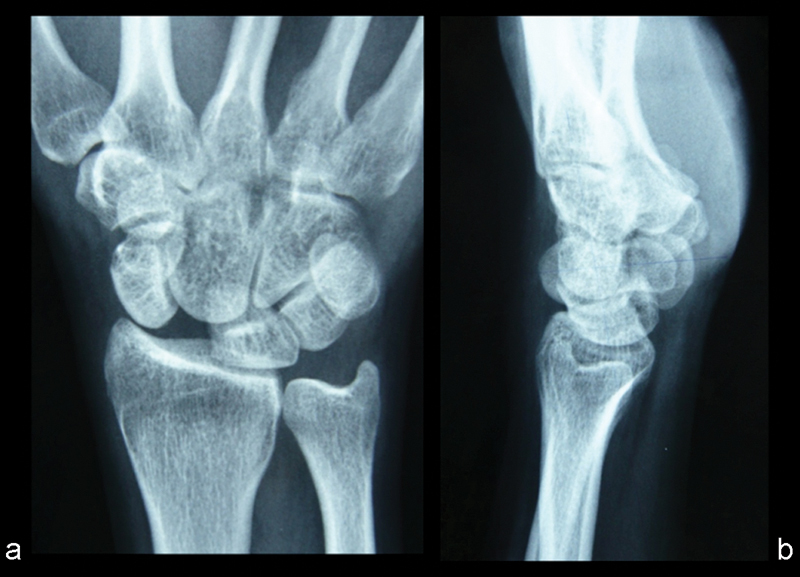
A 43-year-old man developed right wrist pain and swelling 1 year after injury at a tennis game. (a,b) X-rays showed a widely dissociated SL joint and a severe DISI deformity with dorsal subluxation of the proximal scaphoid. The SL interval measured 8.4 mm.
Fig. 12.
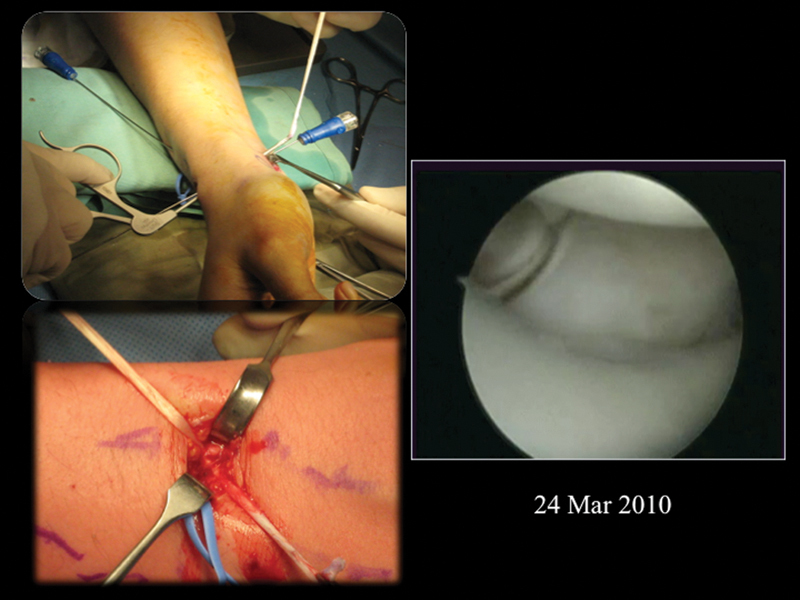
The patient underwent an arthroscopic assisted box reconstruction of the SL ligament with a PL graft on March 24, 2010. Arthroscopy showed a well-reduced and stable SL joint.
Fig. 13.
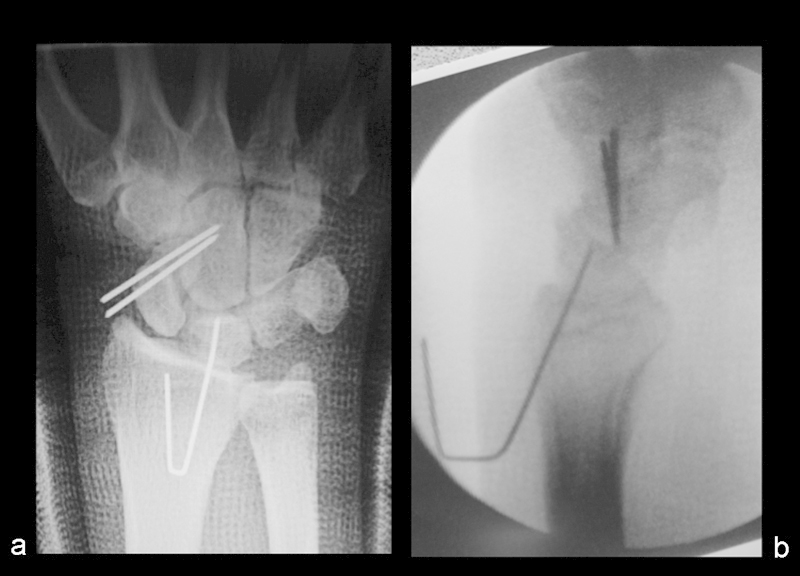
(a,b) The postop X-ray demonstrated a well-reduced SL joint and correction of the DISI deformity.
Fig. 14.

(a,b) A follow-up X-ray after 5 years showed a well-maintained SL joint alignment with no arthritic change.
Fig. 15.

Follow-up pictures of the patient on March 3, 2015, showed minimal scar and a good range of wrist motion.
There was no infection or neurovascular complication in the series. One patient was noted to have an early recurrence of the SL diastasis at 2 weeks. Exploration revealed slackening of the tendon graft; therefore a retensioning was performed. One patient early in our series developed moderate ischemia of the proximal pole of the scaphoid on follow-up. This was a case in which a large drill hole was made (2.9 mm) close to the bone margin. The proximal scaphoid resorbed slightly with time. The SL interval increased from intraoperative 1.5 mm to 3 mm at 1-year postoperative, but there was no further SL gapping at 9.5 years after the operation (Fig. 16). The patient was symptom-free and had an improvement of grip strength of 45% and was 44% stronger than the uninjured side. The wrist performance score improved from a preoperative level of 31/40 to 39/40, and VAS of pain from 6/20 to 1/20.
Fig. 16.
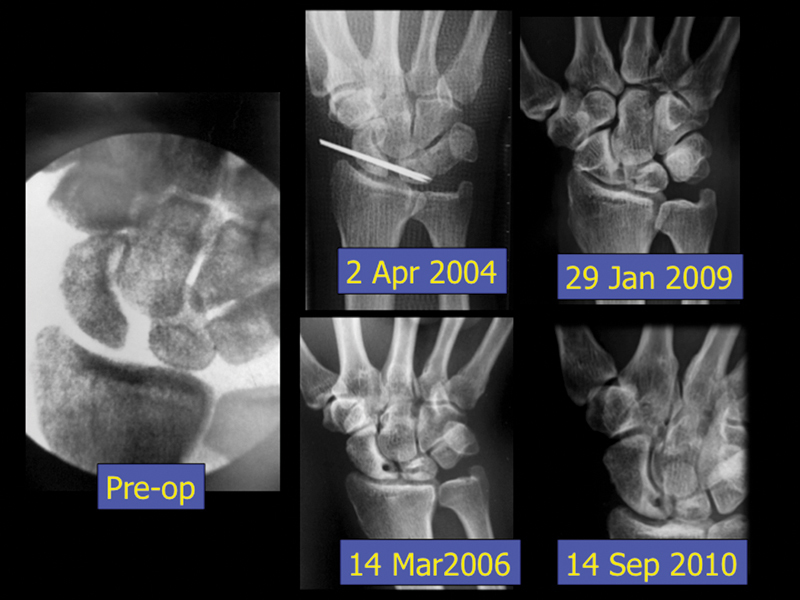
Serial X-rays showed no progression of the ischemia of the proximal scaphoid in one patient.
Discussion
The idea of bone tunnel reconstruction of SL ligament is not a new one. In 1975, Dobyns used a portion of tendon to pass through anteroposterior bone tunnels in the proximal pole of the scaphoid and lunate to reconstruct the SL linkage.20 Stability was obtained by tightly looping the tendon graft across the scaphoid and lunate. However, creating drill holes across poorly vascularized areas of bone in an open fashion severely compromised their blood supply and resulted in fractures and avascular necrosis. This approach was subsequently abandoned. Our current arthroscopic assisted technique does not require dissection of the joint capsule and hence preserves the carpal blood supply. Fibrotic scar around the scaphoid and lunate is released arthroscopically. This minimally invasive technique helps to minimize the soft tissue dissection and decrease the risk of avascular necrosis, promote healing of the reconstructed SL ligament, and hasten the postoperative rehabilitation.
Our results demonstrated an improvement in the wrist range of motion, which differs from the results of other SL reconstruction techniques. We did not need to advance the dorsal joint capsule as in dorsal capsulodesis, which inevitably jeopardizes the wrist flexion motion.2 21 22 23 24 25 26 27 The FCR acts to protect the scaphoid from rotary subluxation by supinating the scaphoid and pronating the lunate. Preserving the FCR in our method theoretically helps to preserve a dynamic stabilizer of the SL joint and to eliminate the tether between the radius and scaphoid, which could affect the wrist extension range. Recurrent SL gapping is very common in some series reports,3 and our results also failed to demonstrate a perfect reduction of all the SL intervals. The range of postoperative SL interval was from 1.6 mm to 5.5 mm, though a reduction of the SL interval from an average 4.9 mm to 2.9 mm was achieved. Replacing a ligament with a tendon cannot truly replicate the unique anatomy of the SL complex. However, maintenance of the SL interval was found in 15 patients after the K-wire removal at 8 weeks. Reconstructing both the volar and dorsal ligaments is expected to be more effective at maintaining the SL interval than the more common dorsal reconstructions.
Many cadaveric results support the role of both dorsal and volar SL ligament in SL stability and the rewarding biomechanical results of reconstruction of both.16 17 20 Several promising clinical results from restoring the volar SL ligament, such as Marcuzzi, who treated six patients by reconstructing both the dorsal and volar SL ligament with very good clinical outcomes.28
There are several possible pitfalls. Spearing the tendon graft while pinning the SL joint could potentially injure and weaken the tendon graft and should be avoided. Pinning the SC joint might cause irritation or injury to the superficial radial nerve. Use of a wide-bore needle as a protective sheath is recommended. The diameter of the bone tunnels should match that of the PL graft. The size of the bone tunnel should be limited to under 2.5 mm in most patients. An adequate distance from the bone margins should be observed. Excessive resistance in the tunnel during graft insertion might weaken the graft. Soaking the tendon graft in normal saline swells the graft and produces higher tunnel resistance. Graft pretensioning might be helpful to prevent secondary slackening. Creating a drill hole through a small carpal bone can lead to iatrogenic fracture and avascular necrosis.
Conclusion
Our method of reconstructing both the dorsal and volar SL ligaments, in a minimally invasive way, is a logical and effective technique to improve the SL stability. The potential risk of ischemic necrosis of the carpal bone can be minimized by the preservation of blood supply, the small size of the bone tunnels created, and the inclusion of the capsule at the reconstruction site. Our intermediate-term results demonstrate the ability to improve patients' symptoms, improve strength and range of motion, and retard the progression of arthritis.
Footnotes
Conflict of Interest None
References
- 1.Daniels J M II, Zook E G, Lynch J M. Hand and wrist injuries: Part I. Nonemergent evaluation. Am Fam Physician. 2004;69(8):1941–1948. [PubMed] [Google Scholar]
- 2.Moran S L, Ford K S, Wulf C A, Cooney W P. Outcomes of dorsal capsulodesis and tenodesis for treatment of scapholunate instability. J Hand Surg Am. 2006;31(9):1438–1446. doi: 10.1016/j.jhsa.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Linscheid R L, Dobyns J H. Treatment of scapholunate dissociation. Rotatory subluxation of the scaphoid. Hand Clin. 1992;8(4):645–652. [PubMed] [Google Scholar]
- 4.Almquist E E, Bach A W, Sack J T, Fuhs S E, Newman D M. Four-bone ligament reconstruction for treatment of chronic complete scapholunate separation. J Hand Surg Am. 1991;16(2):322–327. doi: 10.1016/s0363-5023(10)80120-0. [DOI] [PubMed] [Google Scholar]
- 5.Brunelli G A, Brunelli G R. A new technique to correct carpal instability with scaphoid rotary subluxation: a preliminary report. J Hand Surg Am. 1995;20(3 Pt 2):S82–S85. doi: 10.1016/s0363-5023(95)80175-8. [DOI] [PubMed] [Google Scholar]
- 6.Van Den Abbeele K L, Loh Y C, Stanley J K, Trail I A. Early results of a modified Brunelli procedure for scapholunate instability. J Hand Surg [Br] 1998;23(2):258–261. doi: 10.1016/s0266-7681(98)80191-5. [DOI] [PubMed] [Google Scholar]
- 7.Talwalkar S C, Edwards A TJ, Hayton M J, Stilwell J H, Trail I A, Stanley J K. Results of tri-ligament tenodesis: a modified Brunelli procedure in the management of scapholunate instability. J Hand Surg [Br] 2006;31(1):110–117. doi: 10.1016/j.jhsb.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 8.Chabas J F, Gay A, Valenti D, Guinard D, Legre R. Results of the modified Brunelli tenodesis for treatment of scapholunate instability: a retrospective study of 19 patients. J Hand Surg Am. 2008;33(9):1469–1477. doi: 10.1016/j.jhsa.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Elias M, Lluch A L, Stanley J K. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am. 2006;31(1):125–134. doi: 10.1016/j.jhsa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 10.Glickel S Z, Millender L H. Ligamentous reconstruction for chronic intercarpal instability. J Hand Surg Am. 1984;9(4):514–527. doi: 10.1016/s0363-5023(84)80102-1. [DOI] [PubMed] [Google Scholar]
- 11.Taleisnik J. Vol. 27. St Louis: Mosby; 1978. Wrist anatomy function and injury. American Academy of Orthopaedic Surgeons Instructional Course Lectures; pp. 61–87. [Google Scholar]
- 12.Mayfield J K. Patterns of injury to carpal ligaments. A spectrum. Clin Orthop Relat Res. 1984;(187):36–42. [PubMed] [Google Scholar]
- 13.Meade T D, Schneider L H, Cherry K. Radiographic analysis of selective ligament sectioning at the carpal scaphoid: a cadaver study. J Hand Surg Am. 1990;15(6):855–862. doi: 10.1016/0363-5023(90)90003-a. [DOI] [PubMed] [Google Scholar]
- 14.Dunn M J, Johnson C. Static scapholunate dissociation: a new reconstruction technique using a volar and dorsal approach in a cadaver model. J Hand Surg Am. 2001;26(4):749–754. doi: 10.1053/jhsu.2001.26025. [DOI] [PubMed] [Google Scholar]
- 15.Short W H, Werner F W, Sutton L G. Dynamic biomechanical evaluation of the dorsal intercarpal ligament repair for scapholunate instability. J Hand Surg Am. 2009;34(4):652–659. doi: 10.1016/j.jhsa.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 16.Yi I S, Firoozbakhsh K, Racca J, Umeda Y, Moneim M. Treatment of scapholunate dissociation with palmaris longus tendon graft: a biomechanical study. Univ Pennsylvania Orthop J. 2000;13:53–59. [Google Scholar]
- 17.Zdero R, Olsen M, Elfatori S. et al. Linear and torsional mechanical characteristics of intact and reconstructed scapholunate ligaments. J Biomech Eng. 2009;131(4):41009. doi: 10.1115/1.3005149. [DOI] [PubMed] [Google Scholar]
- 18.Ho P C, Tse W I, Wong C WY, Chow E C. Arthroscopic osteochondral grafting for radiocarpal joint defects. J Wrist Surg. 2013;2(3):212–219. doi: 10.1055/s-0033-1351788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ong M T, Ho P C, Wong C W, Cheng S H, Tse W L. Wrist arthroscopy under portal site local anesthesia (PSLA) without tourniquet. J Wrist Surg. 2012;1(2):149–152. doi: 10.1055/s-0032-1326726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dobyns J H Linscheid R L Chao E YS Weber E R Swanson G E Traumatic instability of the wrist In Instructional Course Lectures, The American Academy of Orthopaedic Surgeons. Vol. 24, pp. 182-199 St. Louis: C. V. Mosby; 1975 [Google Scholar]
- 21.Szabo R M. Scapholunate ligament repair with capsulodesis reinforcement. J Hand Surg Am. 2008;33(9):1645–1654. doi: 10.1016/j.jhsa.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 22.Azura L Ahmad T S Kamarul T A modified Blatt dorsal capsulodesis in the treatment of dynamic scapholunate instability Med J Malaysia 200661(Suppl B):51–54. [PubMed] [Google Scholar]
- 23.Moran S L, Cooney W P, Berger R A, Strickland J. Capsulodesis for the treatment of chronic scapholunate instability. J Hand Surg Am. 2005;30(1):16–23. doi: 10.1016/j.jhsa.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 24.Deshmukh S C, Givissis P, Belloso D, Stanley J K, Trail I A. Blatt's capsulodesis for chronic scapholunate dissociation. J Hand Surg [Br] 1999;24(2):215–220. doi: 10.1054/jhsb.1998.0183. [DOI] [PubMed] [Google Scholar]
- 25.Muermans S, De Smet L, Van Ransbeeck H. Blatt dorsal capsulodesis for scapholunate instability. Acta Orthop Belg. 1999;65(4):434–439. [PubMed] [Google Scholar]
- 26.Uhl R L, Williamson S C, Bowman M W, Sotereanos D G, Osterman A L. Dorsal capsulodesis using suture anchors. Am J Orthop. 1997;26(8):547–548. [PubMed] [Google Scholar]
- 27.Gajendran V K, Peterson B, Slater R R Jr, Szabo R M. Long-term outcomes of dorsal intercarpal ligament capsulodesis for chronic scapholunate dissociation. J Hand Surg Am. 2007;32(9):1323–1333. doi: 10.1016/j.jhsa.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 28.Marcuzzi A, Leti Acciaro A, Caserta G, Landi A. Ligamentous reconstruction of scapholunate dislocation through a double dorsal and palmar approach. J Hand Surg [Br] 2006;31(4):445–449. doi: 10.1016/j.jhsb.2006.02.009. [DOI] [PubMed] [Google Scholar]


