Abstract
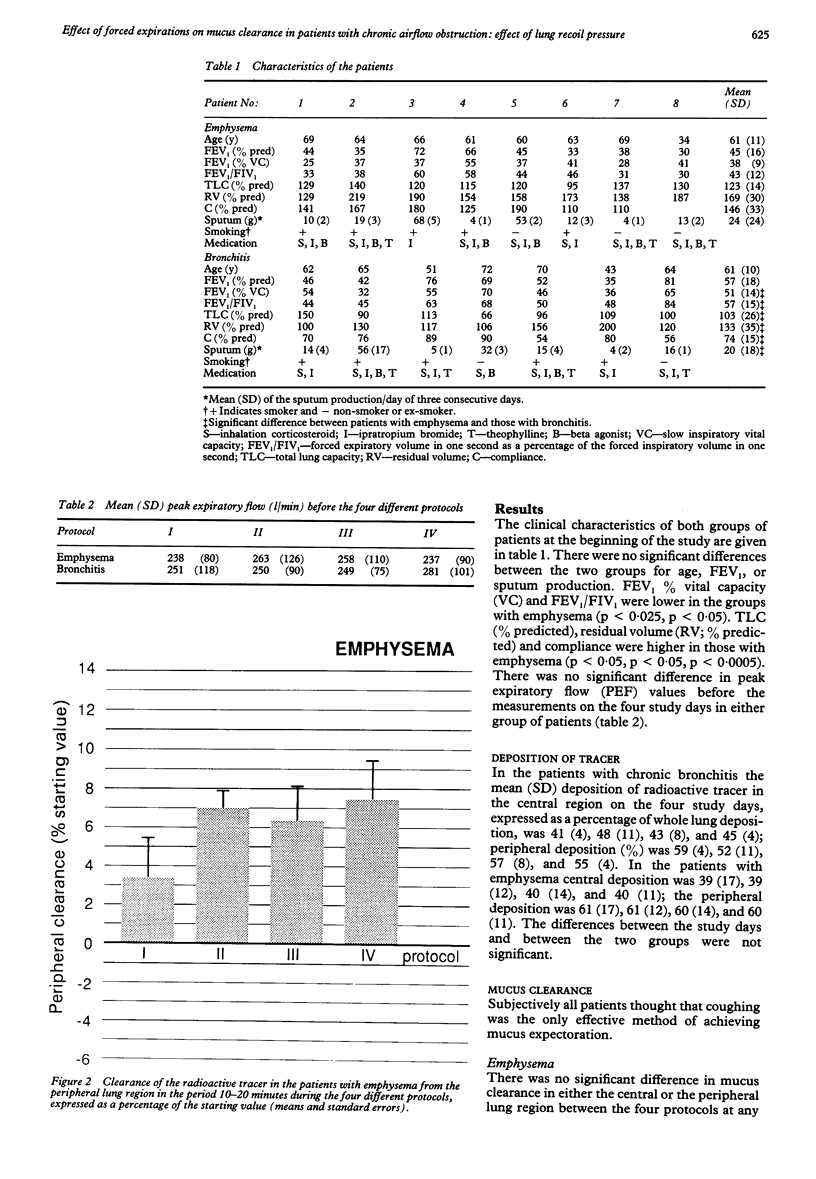
Spontaneous mucus clearance and the effect of forced expirations and coughing on mucus clearance were investigated in eight patients with chronic airflow obstruction and low elastic recoil pressure (emphysema group: mean FEV1 45% predicted) and in seven patients with chronic airflow obstruction and normal elastic recoil pressure (chronic bronchitis group: mean FEV1 57% predicted). Mucus clearance was measured in a central and a peripheral lung region by a radioactive aerosol tracer technique. Spontaneous mucus clearance from the peripheral lung region was higher in the patients with emphysema than in those with chronic bronchitis. There was no difference in central mucus clearance between the two groups. Mucus clearance from the peripheral lung region increased significantly during forced expirations and coughing in the patients with chronic bronchitis but not in those with emphysema. It is concluded that in patients with chronic airflow obstruction and regular sputum production spontaneous peripheral mucus clearance is greater in those with decreased elastic recoil pressure. Physiotherapy that includes forced expirations and coughing can enhance mucus clearance in such patients when elastic recoil pressure is normal but is unlikely to be effective when elastic recoil pressure is decreased.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Camner P., Mossberg B., Philipson K. Tracheobronchial clearance and chronic obstructive lung disease. Scand J Respir Dis. 1973;54(5):272–281. [PubMed] [Google Scholar]
- Clarke S. W., Jones J. G., Oliver D. R. Resistance to two-phase gas-liquid flow in airways. J Appl Physiol. 1970 Oct;29(4):464–471. doi: 10.1152/jappl.1970.29.4.464. [DOI] [PubMed] [Google Scholar]
- Dawson S. V., Elliott E. A. Wave-speed limitation on expiratory flow-a unifying concept. J Appl Physiol Respir Environ Exerc Physiol. 1977 Sep;43(3):498–515. doi: 10.1152/jappl.1977.43.3.498. [DOI] [PubMed] [Google Scholar]
- Kim C. S., Rodriguez C. R., Eldridge M. A., Sackner M. A. Criteria for mucus transport in the airways by two-phase gas-liquid flow mechanism. J Appl Physiol (1985) 1986 Mar;60(3):901–907. doi: 10.1152/jappl.1986.60.3.901. [DOI] [PubMed] [Google Scholar]
- Kirilloff L. H., Owens G. R., Rogers R. M., Mazzocco M. C. Does chest physical therapy work? Chest. 1985 Sep;88(3):436–444. doi: 10.1378/chest.88.3.436. [DOI] [PubMed] [Google Scholar]
- Langlands J. The dynamics of cough in health and in chronic bronchitis. Thorax. 1967 Jan;22(1):88–96. doi: 10.1136/thx.22.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leith D. E. Cough. Phys Ther. 1968 May;48(5):439–447. doi: 10.1093/ptj/48.5.439. [DOI] [PubMed] [Google Scholar]
- Mead J., Turner J. M., Macklem P. T., Little J. B. Significance of the relationship between lung recoil and maximum expiratory flow. J Appl Physiol. 1967 Jan;22(1):95–108. doi: 10.1152/jappl.1967.22.1.95. [DOI] [PubMed] [Google Scholar]
- Mossberg B., Philipson K., Camner P. Tracheobronchial clearance in patients with emphysema associated with alpha1-antitrypsin deficiency. Scand J Respir Dis. 1978 Feb;59(1):1–7. [PubMed] [Google Scholar]
- Prato F. S., Vinitski S. Radiation dose calculations for inhalation of Tc-99m sulfur colloid radioaerosol. J Nucl Med. 1983 Sep;24(9):816–821. [PubMed] [Google Scholar]
- Pryor J. A., Webber B. A. An evaluation of the forced expiration technique as an adjunct to postural drainage. Physiotherapy. 1979 Oct;65(10):304–307. [PubMed] [Google Scholar]
- Pryor J. A., Webber B. A., Hodson M. E., Batten J. C. Evaluation of the forced expiration technique as an adjunct to postural drainage in treatment of cystic fibrosis. Br Med J. 1979 Aug 18;2(6187):417–418. doi: 10.1136/bmj.2.6187.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutland J., Griffin W. M., Cole P. J. Human ciliary beat frequency in epithelium from intrathoracic and extrathoracic airways. Am Rev Respir Dis. 1982 Jan;125(1):100–105. doi: 10.1164/arrd.1982.125.1.100. [DOI] [PubMed] [Google Scholar]
- Simon G., Pride N. B., Jones N. L., Raimondi A. C. Relation between abnormalities in the chest radiograph and changes in pulmonary function in chronic bronchitis and emphysema. Thorax. 1973 Jan;28(1):15–23. doi: 10.1136/thx.28.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton P. P., Parker R. A., Webber B. A., Newman S. P., Garland N., Lopez-Vidriero M. T., Pavia D., Clarke S. W. Assessment of the forced expiration technique, postural drainage and directed coughing in chest physiotherapy. Eur J Respir Dis. 1983 Jan;64(1):62–68. [PubMed] [Google Scholar]
- Verboon J. M., Bakker W., Sterk P. J. The value of the forced expiration technique with and without postural drainage in adults with cystic fibrosis. Eur J Respir Dis. 1986 Sep;69(3):169–174. [PubMed] [Google Scholar]
- van der Schans C. P., Piers D. A., Postma D. S. Effect of manual percussion on tracheobronchial clearance in patients with chronic airflow obstruction and excessive tracheobronchial secretion. Thorax. 1986 Jun;41(6):448–452. doi: 10.1136/thx.41.6.448. [DOI] [PMC free article] [PubMed] [Google Scholar]