Abstract
Background
Combined anteversion is the sum of femoral and acetabular anteversion and represents their morphological relationship in the axial plane. Few studies have investigated the native combined anteversion in patients with symptomatic dysplastic hips.
Questions/purposes
We hypothesized the following: (1) dysplastic hips have two distinct populations, which differ from each other and from normal hips in their combined anteversion; and (2) these populations differ clinically in terms of correlation between age of onset of symptoms and amount of anteversion.
Methods
We measured radiographic parameters by CT of 100 dysplastic hips in 76 patients who were symptomatic enough to undergo periacetabular osteotomy and of 50 normal hips in 44 patients who had CT scans as part of preparation for computer-navigated TKAs; these patients had no visible hip arthritis or dysplasia and no hip symptoms. Dysplastic hips were divided into the anteversion (83 hips) and retroversion groups (17 hips) based on acetabular version. Age at pain onset was determined from their medical charts.
Results
Combined anteversion in the anteversion group was greater than that in the retroversion and control groups: 47° ± 12°, 30° ± 16°, and 36° ± 9°, respectively. In the anteversion group, combined anteversion (r = −0.49; 95% confidence interval [CI], −0.66 to −0.27; p < 0.001) and femoral anteversion (r = −0.41; 95% CI, −0.60 to −0.19; p < 0.001) were associated with an earlier age at pain onset; however, no such relationships were observed in the retroversion group. After controlling for relevant potential confounding variables, we found that combined anteversion (hazard ratio [HR], 1.04; 95% CI, 1.01–1.07; p = 0.006) and Sharp angle (HR, 1.10; 95% CI, 1.02–1.17; p = 0.008) were associated with an earlier age of pain onset in the anteversion group.
Conclusions
These results suggest that not only lateral coverage of the femoral head, but also axial joint morphology is important for the development of pain in the anteversion group. Optimal combined anteversion should be considered during periacetabular osteotomy.
Level of Evidence
Level IV, prognostic study.
Introduction
Developmental dysplasia of the hip (DDH) is characterized by various morphological abnormalities such as acetabular dysplasia, decreased acetabular coverage of the femoral head, and excessive femoral anteversion [3, 16, 18]. These features result in abnormal joint stresses, leading to subsequent labral tears, articular cartilage degeneration, and early development of secondary hip osteoarthritis [2, 9, 15, 24, 25]. The severity of hip dysplasia has typically been determined by the degree of subluxation [21] and the extent of acetabular dysplasia.
Although hip deformities in the axial plane are also associated with the pathology of DDH, they have received less attention. We previously reported that, despite relatively better acetabular coverage, dysplastic hips with acetabular retroversion had earlier pain onset than those with acetabular anteversion [7]. This finding suggested a relationship between acetabular version and the pathogenesis of osteoarthritis. Combined anteversion is the sum of femoral and acetabular anteversion in the axial plane, and its role has not to our knowledge been evaluated.
We therefore sought to determine whether (1) dysplastic hips have two distinct populations, which differ from each other and from normal hips in their combined anteversion; and (2) these populations differ clinically in terms of correlation between age of onset of symptoms and amount of anteversion.
Patients and Methods
This retrospective study was approved by our institutional review board. We reviewed standard AP radiographs of the pelvis and pelvic CT images of 218 hips in 197 patients with symptomatic dysplastic hips obtained between January 2006 and June 2014 during preoperative assessment for periacetabular osteotomy. Hip dysplasia was defined as a lateral center-edge (CE) angle of Wiberg < 20° based on measurements using AP radiographs of the pelvis. Forty-nine hips were excluded because either their CT images were unavailable or did not include the knee to allow measurements of femoral anteversion. Forty-one hips that were scored as Grade 2 or worse according to the Tönnis osteoarthritis grading system [21] or that had visible osteophyte formation were excluded, because of concerns regarding the accuracy of measurements to be made. Fifteen hips in 10 patients with severe deformity of the femoral head, 12 hips in six patients with prior surgery, and one hip in one patient with severe pubic symphysis diastasis were excluded. The remaining 100 hips in 76 patients were included in this study. Eleven hips belonged to eight male patients and 89 hips belonged to 64 female patients. The average age of the patients at surgery was 38 years (range, 16–59 years) and all patients were skeletally mature. According to the classification system of Crowe et al. [4], all hips were classified as Type I. Nineteen hips in 15 patients had a history of nonoperative DDH treatment in childhood. From a review of the medical records, we determined the age at pain onset when the patients had continuous symptoms enough to consider periacetabular osteotomy. When the age at pain onset was unclear from this review, the patients were interviewed by one of us (YN) directly during their hospitalization for periacetabular osteotomy.
The control group included 50 hips of 44 patients with osteoarthritis of the knee. We examined AP pelvic radiographs and CT images of hips and pelvis routinely obtained during planning for TKA using a CT-based navigation system [14]. These individuals had no history of disease or articular symptoms in the hips, as indicated by a medical chart search and radiographic examination. All the subjects were women with an average age of 75 years (range, 52–87 years). Although the average age of the control group was higher than that of the dysplastic hip group, we confirmed that the control subjects had no degenerative changes in the hips or other hip abnormalities.
Pelvic CT (Aquilion; Toshiba, Tochigi, Japan) was performed following methods previously described [6]. Briefly, images were obtained at 2-mm intervals from the anterosuperior iliac spines to the inferior rim of the pelvis in combination with a 200-mm section of the midpoint of the knee. Data of the control subjects were obtained in 2-mm slices from a 100-mm section of the femoral head, a 200-mm section of the midpoint of the knee, and a 100-mm section of the distal part of the tibia in preparation for a CT-based navigation system of TKA [14].
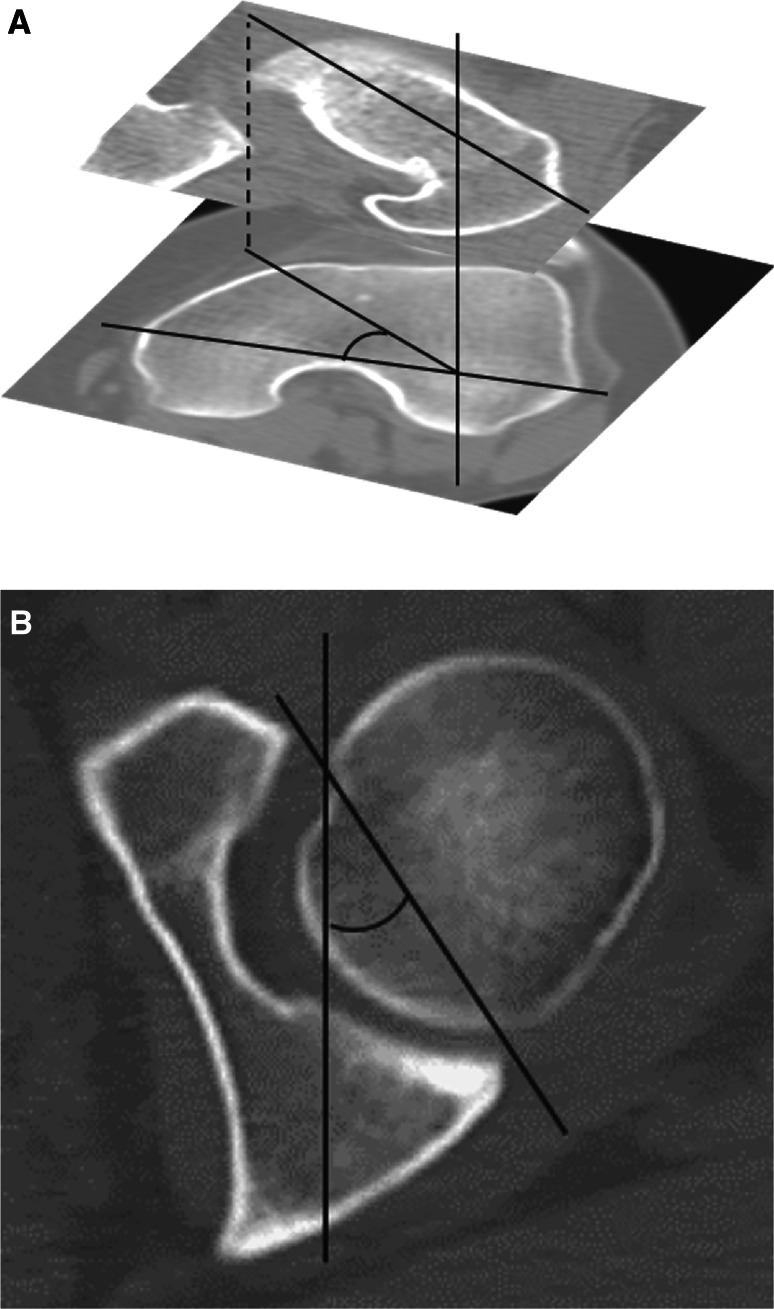
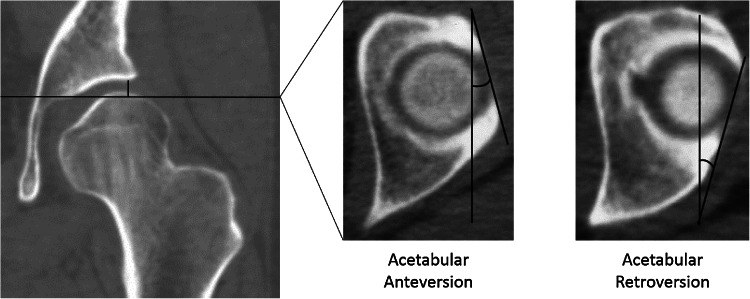
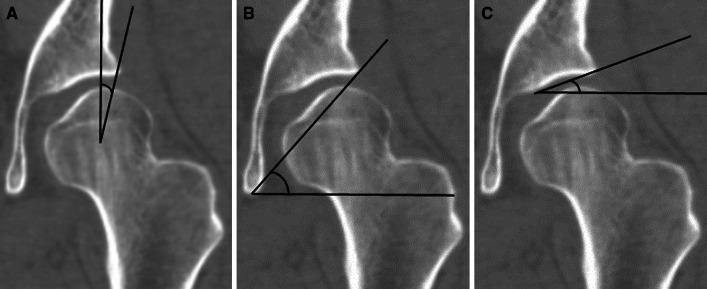
Multiplanar reconstruction of all images was performed using the image analysis software (3D Template; Kyocera Medical, Osaka, Japan). For the measurement of femoral anteversion, the femoral neck axis was defined using the single-slice method described by Sugano et al. [20]. The distal femoral condylar axis was measured using the transepicondylar axis, which is discernible in degenerated knees such as those of our control subjects. We defined the angle between the femoral neck axis and the transepicondylar axis as the femoral anteversion angle (Fig. 1A). On the acetabular side, we used the anterior pelvic plane [13] as a reference plane. We defined the acetabular anteversion angle [17] passing through the femoral head center as the angle created by the intersection of the line connecting the anterior and posterior edges of the acetabulum with a sagittal line (Fig. 1B). Native combined anteversion was calculated as the sum of femoral anteversion and acetabular anteversion. We divided the dysplastic hips into two groups following the method described by Jamali et al. [8] to eliminate the effect of pelvic tilt [23]. In particular, on the axial section 5 mm caudal to the acetabular roof, we measured the cranial anteversion angle to determine the presence of acetabular retroversion. We defined the anteversion group as comprising hips with a positive cranial anteversion angle and the retroversion group as those in which this angle was negative (Fig. 2). In the coronal plane passing through the femoral head center, we measured the lateral CE angle (Fig. 3A), Sharp angle (Fig. 3B), and acetabular roof obliquity (Fig. 3C).
Fig. 1A–B.
(A) The femoral anteversion angle was measured as an angle between the femoral neck axis and the transepicondylar axis. (B) The acetabular anteversion angle was measured as an angle formed by a line connecting the anterior and posterior edges of the acetabulum and a sagittal line on the axial plane passing through the center of the femoral head.
Fig. 2.
The cranial anteversion angle was measured as an angle formed by a line connecting the anterior and posterior edges of the acetabulum and a sagittal line on the axial plane 5 mm caudal to the acetabular roof. The anteversion group was defined as comprising hips with a positive cranial anteversion angle. The retroversion group was defined as those in which this angle was negative.
Fig. 3A–C.
(A) The lateral CE angle was measured as an angle formed by a line connecting the center of the femoral head and the lateral edge of the acetabulum and a sagittal line on the coronal plane passing through the center of the femoral head. (B) The Sharp angle was measured as an angle formed by a line connecting the lateral and inferior edges of the acetabulum and a horizontal line. (C) The acetabular roof obliquity was measured as an angle formed by a line connecting the medial edge of the sourcil and the lateral edge of the acetabulum and a horizontal line.
All measurements were performed by two observers (YK, MA) and were repeated in a blind manner at least 1 month after the first measurements. According to the standards for the kappa statistic proposed by Landis and Koch [10], intraobserver reliabilities of the femoral anteversion, acetabular anteversion, and combined anteversion, evaluated by using the intraclass correlation coefficient, were excellent (range, 0.92–0.97). Interobserver measurement reliabilities were also excellent (range, 0.88–0.91).
Statistical analysis was performed using JMP 9.0.2 (SAS Institute Inc, Cary, NC, USA). The Steel-Dwass test was used to compare the clinical data and radiographic parameters among the anteversion, retroversion, and control groups. Only one hip was randomly selected from each of the 24 patients who had bilateral hip pain in the same version group so that the statistical assumption of independent observation was fulfilled. To analyze the factors affecting age of onset of symptoms, we used the Spearman rank correlation coefficient with age at pain onset as the endpoint in each group. The Cox proportional hazard model was then applied to determine these factors contributing to age at pain onset. For all statistical analyses, p values < 0.05 were considered significant.
Results
Of the 100 dysplastic hips, 83 hips (83% [83 of 100]) had positive cranial anteversion angles (anteversion group) and the remaining 17 hips (17% [17 of 100]) had negative cranial anteversion angles (retroversion group). The anteversion group showed greater combined anteversion than the retroversion group (47° ± 12° versus 30° ± 16°; p < 0.001) and control group (47° ± 12° versus 36° ± 9°; p < 0.001), whereas no difference was noted between the retroversion and control groups (30° ± 16° versus 36° ± 9°; p = 0.24) (Table 1).
Table 1.
Radiographic and clinical parameters in the anteversion, retroversion, and control groups
| Parameter | Dysplastic hip group (100 hips) | Control group (50 hips) | |
|---|---|---|---|
| Anteversion group (83 hips) | Retroversion group (17 hips) | ||
| Femoral anteversion (°) (range) | 22 (−2 to 53)† | 16 (−11 to 40) | 14 (0–37) |
| Acetabular anteversion (°) (range) | 25 (12–37)*,† | 17 (6–25)† | 22 (8–35) |
| Combined anteversion (°) (range) | 47 (22–77)*,† | 30 (4–61) | 36 (19–67) |
| Lateral CE angle (°) (range) | 9 (−24 to 20)† | 13 (1–19)† | 39 (25–55) |
| Sharp angle (°) (range) | 49 (41–59)† | 47 (42–51)† | 36 (29–44) |
| Acetabular roof obliquity (°) (range) | 26 (10–44)*,† | 21 (15–31)† | 2 (−6 to 11) |
| BMI (kg/m2) (range) | 24 (17–31) | 23 (19–35)† | 25 (18–37) |
| Sex (male/female) | 10/73 | 1/16 | 0/50 |
| History of DDH treatment (yes/no) | 18/65 | 1/16 | 0/50 |
Values are expressed as mean with range in parentheses; *significant compared with retroversion group; †significant compared with control group; CE = center-edge; BMI = body mass index; DDH = developmental dysplasia of the hip.
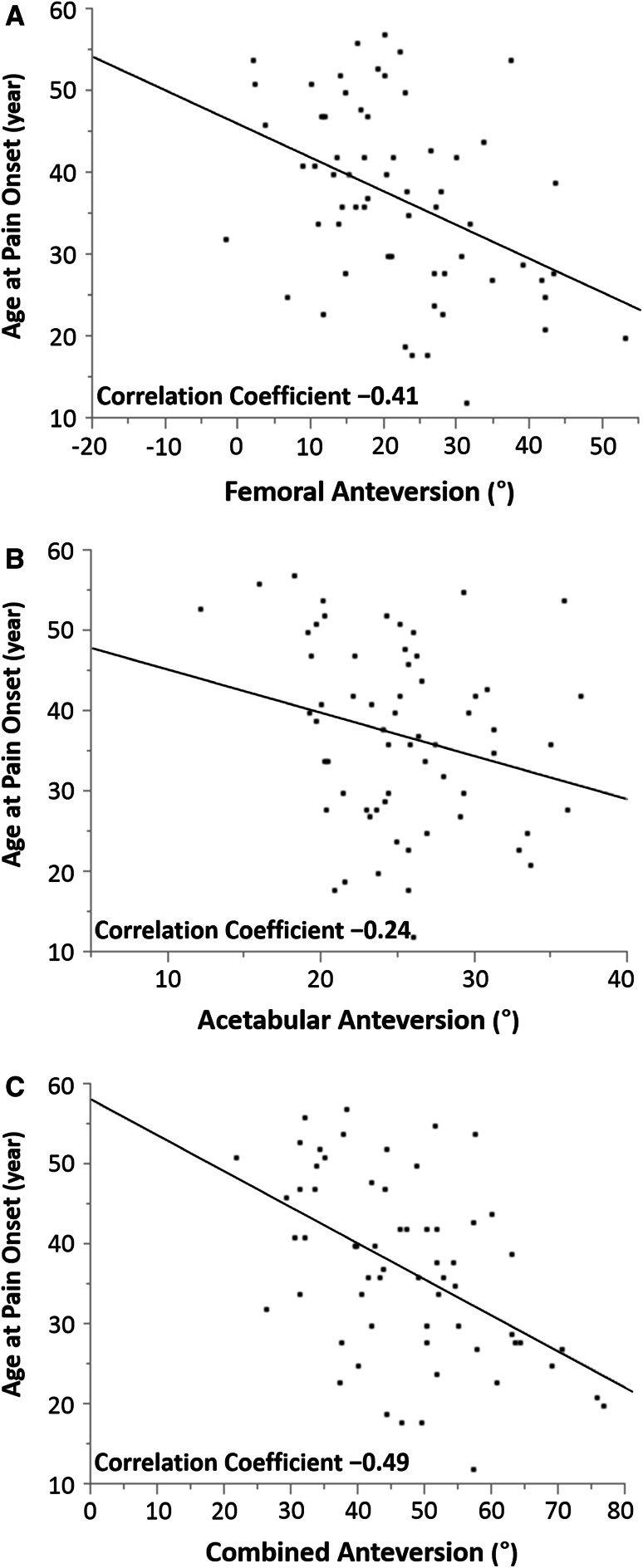
In the anteversion group, increased combined anteversion (r = −0.49; 95% confidence interval [CI], −0.66 to −0.27; p < 0.001) and femoral anteversion (r = −0.41; 95% CI, −0.60 to −0.19; p < 0.001) were associated with an earlier age at onset of pain (Table 2; Fig. 4); however, no such relationships were observed in the retroversion group (Table 3). After controlling for relevant potential confounding variables such as combined anteversion, Sharp angle, body mass index (BMI), and history of DDH treatment, we found that combined anteversion (hazard ratio [HR], 1.04; 95% CI, 1.01–1.07; p = 0.006) and Sharp angle (HR, 1.10; 95% CI, 1.02–1.17; p = 0.008) were associated with an earlier age of pain onset in the anteversion group (Table 4).
Table 2.
Correlation of age at pain onset with radiographic and clinical parameters in the anteversion group
| Parameter | Correlation coefficient | p value |
|---|---|---|
| Femoral anteversion | −0.41 | < 0.001 |
| Acetabular anteversion | −0.24 | 0.060 |
| Combined anteversion | −0.49 | < 0.001 |
| Lateral CE angle | 0.33 | 0.0090 |
| Sharp angle | −0.33 | 0.0098 |
| Acetabular roof obliquity | −0.24 | 0.060 |
| BMI | 0.25 | 0.051 |
CE = center-edge; BMI = body mass index.
Fig. 4A–C.
Graphs showing the correlation between age at pain onset and (A) femoral anteversion (r = −0.41, p < 0.001), (B) acetabular anteversion (r = −0.24, p = 0.060), and (C) combined anteversion (r = −0.49, p < 0.001) in the anteversion group.
Table 3.
Correlation of age at pain onset with radiographic and clinical parameters in the retroversion group
| Parameter | Correlation coefficient | p value |
|---|---|---|
| Femoral anteversion | −0.36 | 0.25 |
| Acetabular anteversion | 0.086 | 0.79 |
| Combined anteversion | −0.11 | 0.74 |
| Lateral CE angle | −0.61 | 0.035 |
| Sharp angle | 0.11 | 0.74 |
| Acetabular roof obliquity | 0.77 | 0.0037 |
| BMI | −0.17 | 0.59 |
CE = center-edge; BMI = body mass index.
Table 4.
Association between age at pain onset and potentially relevant risk factors in the anteversion group
| Parameter | HR | 95% CI | p value |
|---|---|---|---|
| Combined anteversion | 1.04 | 1.01–1.07 | 0.006 |
| Sharp angle | 1.10 | 1.02–1.17 | 0.008 |
| BMI | 0.93 | 0.84–1.01 | 0.096 |
| Sex (male/female) | 0.90 | 0.44–1.69 | 0.72 |
| History of DDH treatment (yes/no) | 0.83 | 0.29–2.15 | 0.76 |
HR = hazard ratio; CI = confident interval; BMI = body mass index; DDH = developmental dysplasia of the hip.
Discussion
Combined anteversion is the sum of femoral and acetabular anteversion and represents their morphological relationship in the axial plane. Although hip deformities in the axial plane are considered to be associated with the pathology of DDH, they have received less attention. We therefore sought to determine whether (1) dysplastic hips have two distinct populations, which differ from each other and from normal hips in their combined anteversion; and (2) these populations differ clinically in terms of correlation between age of onset of symptoms and amount of anteversion.
This study has several limitations. First, the normal subjects in the control group were older than the patients with dysplastic hips. However, because the normal subjects were asymptomatic and without morphological abnormalities that would suggest progression toward osteoarthritis, we considered them to be appropriate for the purpose of this study. There is also a view that only hips that remain asymptomatic in old age should be considered healthy [12]. Because the pelvis tends to tilt backward as a result of lumbar kyphosis in elderly patients, acetabular version may change. Thus, we also adjusted the pelvic tilt in reference to the anterior pelvic plane. Second, we retrospectively determined age at pain onset. In particular, we interviewed the patient regarding his or her history; however, this method depends on the patient’s subjective recollection and thus raises the possibility of inaccuracy. The onset of pain may be affected by not only hip morphology, but also other factors such as BMI or the levels of daily activity. Third, our results are representative only of Asian patients and therefore further studies are needed for patients of other ethnicities. Fourth, our patients are symptomatic enough to undergo major pelvic surgery. There may be many individuals with similar radiographs but no symptoms who never come to the attention of surgeons performing hip procedures. Thus, there may be a selection bias; however, it was difficult to justify taking CT of asymptomatic patients with dysplastic hips, and screening radiographs of the population at large would not be feasible.
We divided dysplastic hips into two groups based on the cranial acetabular version. The anteversion group included the majority of the patients (83%) and showed greater femoral anteversion compared with the retroversion group. We previously reported that the more acetabular anteversion was accompanied by the more femoral anteversion in this group [1]. The resultant combined anteversion in the anteversion group was greater than those in the retroversion and control groups; 47°, 30°, and 36°, respectively. In contrast, the acetabular retroversion was observed in 17% of the dysplastic hips in accordance with the previous studies: 17.2% by Li and Ganz [11] and 18% by Ezoe et al. [5]. Femoral anteversion and combined anteversion in this group were equivalent to those in the control group, and no correlation between acetabular and femoral anteversion was noted. Despite the less severe acetabular dysplasia compared with the anteversion group, age at pain onset in the retroversion group was earlier than that of the anteversion group. These findings support our hypothesis that the dysplastic hips have two distinct populations.
Tönnis and Heinecke [22] described the role of acetabular and femoral version (instability index) on the development of hip osteoarthritis. They mentioned that when decreased acetabular anteversion was combined with increased femoral anteversion or vice versa, the pathological consequences were compensated or diminished. In practice, however, increased femoral anteversion was often combined with the increased acetabular anteversion in our studies. Synergistically, increased combined anteversion was associated with an earlier age at onset of pain in the anteversion group. Sharp angle was also associated with an earlier age of pain onset, suggesting the important roles of both lateral coverage and combined anteversion on the pain onset in the anteversion group. In the retroversion group, earlier pain onset was observed regardless of the femoral anteversion. An earlier biomechanical study demonstrated the concentration of joint stress in the posterior region of the acetabulum during activities of daily living [19], and another found the peak pressures during postural change (standing up and sitting down) were located at the edge of the posterior wall of the acetabulum [26]. When posterolateral acetabular coverage is decreased as seen in the retroversion group, the increased stress concentrations at the same site during dynamic hip movement may contribute to the pain onset.
In conclusion, increased combined anteversion and Sharp angle were associated with an earlier age of pain onset in the anteversion group. These results suggest that not only lateral coverage of the femoral head, but also axial joint morphology (combined anteversion) is important for the development of pain in the anteversion group. Optimal combined anteversion should be considered during periacetabular osteotomy.
Acknowledgments
We thank Masanobu Ohishi MD, PhD, Satoshi Hamai MD, PhD, Masanobu Hirata MD, Daisuke Hara MD, Masayuki Kanazawa MD (Department of Orthopaedic Surgery, Graduate School of Medical Sciences, Kyushu University), and Junji Kishimoto (a statistician from the Digital Medicine Initiative, Kyushu University) for invaluable advice for this study.
Footnotes
The institution of the authors has received funding from Kyocera (Osaka, Japan), which is unrelated to this submitted work. One of the authors certifies that he (YN) received or may receive benefits, an amount less than USD 10,000 from Zimmer Japan (Tokyo, Japan) and Kyocera. This work was supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (No. 24592268 and 15K10450).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Akiyama M, Nakashima Y, Fujii M, Sato T, Yamamoto T, Mawatari T, Motomura G, Matsuda S, Iwamoto Y. Femoral anteversion is correlated with acetabular version and coverage in Asian women with anterior and global deficient subgroups of hip dysplasia: a CT study. Skeletal Radiol. 2012;41:1411–1418. [DOI] [PubMed]
- 2.Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Joint Surg Br. 2004;86:876–886. doi: 10.1302/0301-620X.86B6.14441. [DOI] [PubMed] [Google Scholar]
- 3.Anda S, Terjesen T, Kvistad KA, Svenningsen S. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr. 1991;15:115–120. doi: 10.1097/00004728-199101000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15–23. [PubMed] [Google Scholar]
- 5.Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88:372–379. doi: 10.2106/JBJS.D.02385. [DOI] [PubMed] [Google Scholar]
- 6.Fujii M, Nakashima Y, Sato T, Akiyama M, Iwamoto Y. Pelvic deformity influences acetabular version and coverage in hip dysplasia. Clin Orthop Relat Res. 2011;469:1735–1742. doi: 10.1007/s11999-010-1746-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fujii M, Nakashima Y, Yamamoto T, Mawatari T, Motomura G, Matsushita A, Matsuda S, Jingushi S, Iwamoto Y. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;92:895–903. doi: 10.2106/JBJS.I.00046. [DOI] [PubMed] [Google Scholar]
- 8.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the ‘cross-over-sign’. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 9.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- 10.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 11.Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–253. doi: 10.1097/01.blo.0000081934.75404.36. [DOI] [PubMed] [Google Scholar]
- 12.Mavcic B, Slivnik T, Antolic V, Iglic A, Kralj-Iglic V. High contact hip stress is related to the development of hip pathology with increasing age. Clin Biomech. 2004;19:939–943. doi: 10.1016/j.clinbiomech.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 13.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148–159. [PubMed] [Google Scholar]
- 14.Mizu-uchi H, Matsuda S, Miura H, Okazaki K, Akasaki Y, Iwamoto Y. The evaluation of post-operative alignment in total knee replacement using a CT-based navigation system. J Bone Joint Surg Br. 2008;90:1025–1031. doi: 10.1302/0301-620X.90B8.20265. [DOI] [PubMed] [Google Scholar]
- 15.Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict outcome. J Bone Joint Surg Am. 1995;77:985–989. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Murphy SB, Kijewski PK, Mills MB, Harless A. Acetabular dysplasia in the adolescent and adult. Clin Orthop Relat Res. 1990;261:214–223. [PubMed] [Google Scholar]
- 17.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 18.Noble PC, Kamaric E, Sugano N, Matsubara M, Harada Y, Ohzono K, Paravic V. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res. 2003;417:27–40. [PubMed] [Google Scholar]
- 19.Pedersen DR, Brand RA, Davy DT. Pelvic muscle and acetabular contact forces during gait. J Biomech. 1997;30:959–965. doi: 10.1016/S0021-9290(97)00041-9. [DOI] [PubMed] [Google Scholar]
- 20.Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr. 1998;22:610–614. doi: 10.1097/00004728-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 21.Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer; 1987. pp. 165–171. [Google Scholar]
- 22.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Wassilew GI, Heller MO, Diederichs G, Janz V, Wenzl M, Perka C. Standardized AP radiographs do not provide reliable diagnostic measures for the assessment of acetabular retroversion. J Orthop Res. 2012;30:1369–1376. doi: 10.1002/jor.22086. [DOI] [PubMed] [Google Scholar]
- 24.Wedge JH, Wasylenko MJ. The natural history of congenital disease of the hip. J Bone Joint Surg Br. 1979;61:334–338. doi: 10.1302/0301-620X.61B3.158025. [DOI] [PubMed] [Google Scholar]
- 25.Weinstein SL. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop Relat Res. 1987;225:62–76. [PubMed] [Google Scholar]
- 26.Yoshida H, Faust A, Wilckens J, Kitagawa M, Fetto J, Chao EY. Three-dimensional dynamic hip contact area and pressure distribution during activities of daily living. J Biomech. 2006;39:1996–2004. doi: 10.1016/j.jbiomech.2005.06.026. [DOI] [PubMed] [Google Scholar]