Abstract
Background
There are many factors that may affect the learning curve for total hip arthroplasty (THA) and surgical approach is one of these. There has been renewed interest in the direct anterior approach for THA with variable outcomes reported, but few studies have documented a surgeon’s individual learning curve when using this approach.
Questions/purposes
(1) What was the revision rate for all surgeons adopting the anterior approach for placement of a particular implant? (2) What was the revision rate for surgeons who performed > 100 cases in this fashion? (3) Is there a minimum number of cases required to complete a learning curve for this procedure?
Methods
The Australian Orthopaedic Association National Joint Replacement Registry prospectively collects data on all primary and revision joint arthroplasty surgery. We analyzed all conventional THAs performed up to December 31, 2013, with a primary diagnosis of osteoarthritis using a specific implant combination and secondarily those associated with surgeons performing more than 100 procedures. Ninety-five percent of these procedures were performed through the direct anterior approach. Procedures using this combination were ordered from earliest (first procedure date) to latest (last procedure date) for each individual surgeon. Using the order number for each surgeon, five operation groups were defined: one to 15 operations, 16 to 30 operations, 31 to 50 operations, 51 to 100 operations, and > 100 operations. The primary outcome measure was time to first revision using Kaplan-Meier estimates of survivorship.
Results
Sixty-eight surgeons performed 5499 THAs using the specified implant combination. The cumulative percent revision at 4 years for all 68 surgeons was 3% (95% confidence interval [CI], 2.5–3.8). For surgeons who had performed over 100 operations, the cumulative revision rate was 3% (95% CI, 2.0–3.5). It was not until surgeons had performed over 50 operations that there was no difference in the cumulative percent revision compared with over 100 operations. The cumulative percent revision for surgeons performing 51 to 100 operations at 4 years was 3% (95% CI, 1.5–5.4) and over 100 operations 2% (95% CI, 1.2–2.7; hazard ratio, 1.40 [95% CI, 0.7–2.7]; p = 0.33).
Conclusions
There is a learning curve for the anterior approach for THA even when using a prosthesis combination specifically marketed for that approach. We found that 50 or more procedures need to be performed by a surgeon before the rate of revision is no different from performing 100 or more procedures. Surgeons should be aware of this initial higher rate of revision when deciding which approach delivers the best outcome for their patients.
Introduction
It is commonly understood that proficiency at a given task requires repetition and time, but the length of time needed to achieve competence is not known. Popular writers such as Malcolm Gladwell have posited the concept of “ten thousand hours” as a minimum [8]. “Learning curve” is typically defined as the rate of a person’s progress in gaining experience or new skills. Surgeons have typically referred to the number of cases needed to achieve a steady state of outcomes as the learning curve. The learning curve for surgical procedures, and in particular for THA, may depend on many variables. Surgeon experience and volume influence the result of hip and knee arthroplasty [2]. The type of prosthesis that is chosen may have a substantial impact on the outcome, independent of surgical ability [6]. Finally, surgical processes such as surgical approach and continuity of the operating room team may influence the learning curve for THA. The number of procedures that a surgeon needs to move off the learning curve is not known and may differ with different types of surgery [14].
The anterior approach for THA, although common in some centers for many years, has recently had a more widespread uptake throughout the world [11–13]. This may be the result of the perception that there is faster recovery, less pain, and potentially a reduced risk of dislocation with the anterior approach [17]. Several studies, however, have demonstrated a higher rate of complications when comparing the anterior approach to THA and have suggested that this is the result of a learning curve for the technique [4, 5, 15, 18]. Although the learning curve is usually associated with a surgeon early in his or her career, changing prostheses or approach may well result in a different outcome.
The Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) tracks all arthroplasties performed in Australia and has previously developed a method to identify prostheses or combinations with a higher than anticipated rate of revision [7]. The results are published in the AOANJRR Annual Report. In 2009 the Versafit/Quadra-H combination (Medacta, Castel San Pietro, Swizterland) was reported as having an 11-fold rate of revision in the first 2 weeks of surgery [1], which was much higher than expected. This rate of revision reduced over the next 3 years and in 2012 the combination was no longer identified as an outlier [2]. The Quadra H is a tapered titanium stem with a proximal plasma coating designed for metaphyseal engagement. The Versafit cup is a plasma-coated hemispherical titanium cup of standard design. Both were specifically marketed for insertion with a dedicated direct anterior approach, which was performed in 95% of all procedures. Using data from the AOANJRR on the use of this prosthesis combination, we sought to answer the following questions: (1) What was the revision rate for all surgeons adopting the anterior approach for placement of a particular implant? (2) What was the revision rate for surgeons who performed > 100 cases in this fashion? (3) Is there a minimum number of cases required to complete a learning curve for this procedure?
Materials and Methods
The AOANJRR prospectively collects data at the time of surgery for primary and revision joint arthroplasty from all hospitals in Australia. Procedures reported to the Registry are crossvalidated with independently collected state health department data in a sequential multilevel matching process, which enables almost 100% data collection. Data are also matched biannually with the Department of Health and Ageing’s National Death Index to obtain information on the date of death.
The first Quadra-H/Versafit procedure with a known code linked to a surgeon was performed on July 11, 2007. Our analysis was restricted to all primary conventional THAs performed from this date up to December 31, 2013, with a diagnosis of osteoarthritis using the Quadra-H/Versafit combination.
Sixty-eight surgeons used the Quadra-H/Versafit combination and performed a total of 5499 procedures. Fifteen surgeons used the combination only once and 50% of surgeons performed 14 operations or less. To look at the learning curve, we examined data only from those surgeons performing more than 100 procedures with this combination. Thus, our data set for the learning curve analysis includes 13 surgeons performing 4138 procedures.
Procedures using this combination were ordered from earliest (first procedure date) to latest (last procedure date) for each individual surgeon. Using the order number for each surgeon, five operation groups were defined: one to 15 operations, 16 to 30 operations, 31 to 50 operations, 51 to 100 operations, and > 100 operations. The primary outcome measure was time to first revision and reasons for revision and types of revision were recorded. Results were also analyzed by year the surgeon first used the combination. At the time of this study the Registry did not collect specific data on the type of approach. Because the Quadra-H/Versafit was performed with the aid of a specific leg holder and distraction table (Medacta), the company kept records and provided a representative at each case. These cases were checked by the senior author (MS) to verify that 95% of the Quadra-H/Versafit prostheses were inserted through an anterior approach. There were 635 procedures recorded for surgeons who had performed 15 or less operations with 32 revisions. There were 2838 procedures recorded for surgeons who had performed more than 100 operations with 31 revisions (Table 1).
Table 1.
Revision rates of Quadra-H/Versafit total conventional hip replacement by operation group (all surgeons)
| Number of operations | Number revised | Total number | Observation years | Revisions/100 observation years (95% CI) |
|---|---|---|---|---|
| 1–15 operations | 32 | 635 | 1872 | 1.71 (1.17–2.41) |
| 16–30 operations | 14 | 475 | 1270 | 1.10 (0.60–1.85) |
| 31–50 operations | 20 | 570 | 1263 | 1.58 (0.97–2.44) |
| 51–100 operations | 19 | 981 | 1678 | 1.13 (0.68–1.77) |
| > 100 operations | 31 | 2838 | 4466 | 0.69 (0.47–0.99) |
| Total | 116 | 5499 | 10550 | 1.10 (0.91–1.32) |
CI = confidence interval.
There were no metal on metal bearing surface articulations recorded by the Registry for this prosthesis.
Statistical Analysis
The Registry uses Kaplan-Meier estimates of survivorship to describe the time to the first revision of an arthroplasty with censoring at the time of death or closure of the database at the time of analysis. The unadjusted cumulative percent revision with an accompanying 95% confidence interval (CI) was calculated with use of unadjusted pointwise Greenwood estimates. Hazard ratios were calculated using Cox proportional hazards models adjusting for age and sex and were used to compare the rate of revision between groups. The assumption of proportional hazards was checked analytically for each model; if the interaction between the predictor and the log of the postoperative time was significant in the standard Cox model, then a time-varying model was used. All tests were two-tailed at the 5% of level of significance. Statistical analysis was performed using SAS software version 9.3 (SAS Institute Inc, Cary, NC, USA).
Results
The cumulative percent revision at 4 years for all surgeons was 3% (95% CI, 2.5–3.8). The total number of revisions performed was 116. The most common reason for revision was for fracture, which occurred in 34 hips (29%) followed by loosening, dislocation, and infection (Table 2). The cumulative percent revision at 4 years for surgeons who had performed 15 procedures or less was 6% compared with 2% for surgeons who performed over 100 procedures (Table 3).
Table 2.
Revision diagnosis of Quadra-H/Versafit total conventional hip
| Quadra-H/Versafit | |||
|---|---|---|---|
| Revision diagnosis | Number | Percent revision | Percent primary |
| Fracture | 34 | 29 | 0.6 |
| Loosening/lysis | 26 | 22 | 0.5 |
| Prosthesis dislocation | 16 | 14 | 0.3 |
| Infection | 15 | 13 | 0.3 |
| Leg length discrepancy | 4 | 3 | 0.1 |
| Other | 21 | 18 | 0.5 |
| Number of revisions | 116 | 100 | 2.3 |
Table 3.
Numbers at risk and cumulative percent revision for the operation groups
| Operation group | 1 year | 2 years | 3 years | 4 years | 5 years | |
|---|---|---|---|---|---|---|
| 1–15 operations | CPR | 3 (2–5) | 4 (3–6) | 6 (4–8) | 6 (4–8) | 6 (4–8) |
| Number at risk | 548 | 433 | 298 | 191 | 91 | |
| 16–30 operations | CPR | 3 (2–5) | 3 (2–5) | 3 (2–5) | 3 (2–5) | 3 (2–5) |
| Number at risk | 415 | 272 | 172 | 105 | 47 | |
| 31–50 operations | CPR | 3 (1–4) | 4 (2–6) | 5 (3–7) | 5 (3–7) | |
| Number at risk | 427 | 259 | 187 | 97 | ||
| 51–100 operations | CPR | 2 (1–3) | 2 (1–3) | 2 (1–4) | 3 (2–5) | |
| Number at risk | 561 | 359 | 211 | 86 | ||
| > 100 operations | CPR | 1 (1–1) | 1 (1–2.0) | 2 (1–3) | 2 (1–3) | |
| Number at risk | 1764 | 960 | 332 | 80 |
Ninety-five percent confidence intervals shown in parentheses; CPR = cumulative percent revision.
There were 13 surgeons who had performed more than 100 operations using the Quadra-H/Versafit. These surgeons had therefore passed through all stages of the analysis and it could therefore truly be said to be representative of the learning curve for the anterior approach using the Quadra-H/Versafit combination. For the 13 surgeons who performed > 100 cases, the overall cumulative percent revision at 4 years was 3% (95% CI, 2.0–3.5).
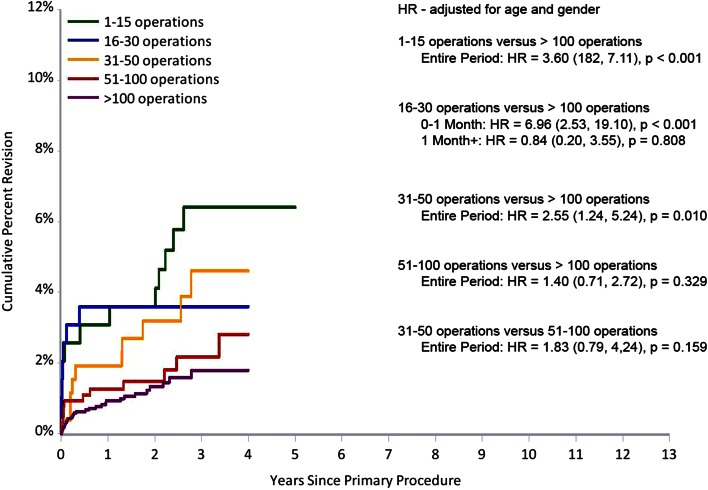
The cumulative percent revision at 4 years for their first 15 cases was 6% (95% CI. 3.7–11.0) and for greater than 100 operations 2% (95% CI, 1.2–2.7; hazard ratio, 3.6 [95% CI, 1.8–7.1]; p < 0.001). It was not until surgeons had performed over 50 operations that there was no difference in the cumulative percent revision compared with over 100 operations. The cumulative percent revision for surgeons performing 51 to 100 operations at 4 years was 3% (95% CI, 1.5–5.4) and over 100 operations 2% (95% CI, 1.2–2.7; hazard ratio 1.40 [95% CI, 0.7–2.7]; p = 0.33; Fig. 1).
Fig. 1.
This figure demonstrates the cumulative percent revision of the Quadra-H/Versafit total conventional hip replacement by operation group (surgeons with at least 100 operations).
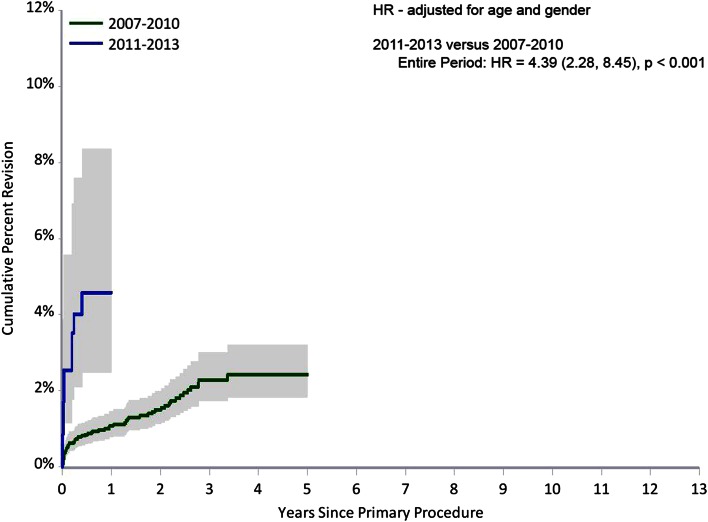
For surgeons performing over 100 operations with this combination, there was a higher rate of revision for those surgeons who started the surgery between 2011 and 2013 compared with 2007 to 2010 (hazard ratio 4.4; 95% CI, 2.3–8.5; p < 0.001; Fig. 2).
Fig. 2.
This figure demonstrates the cumulative percent revision of the Quadra-H/Versafit total conventional hip replacement by year the surgeon first used the combination (surgeons with at least 100 operations). HR = hazard ratio.
Discussion
The learning curve can be defined as the number of times a task must be repeated before a steady state is reached. We had the opportunity to look at the learning curve for the anterior approach because a particular implant was specifically marketed as an anterior approach hip. This study has demonstrated a higher rate of revision for patients undergoing the anterior approach to the hip using the Quadra-H/Versafit combination for the first 50 cases. This is true for all surgeons performing the procedure but importantly also for surgeons who have progressed through a learning curve and have performed more than 100 procedures. There were surgeons who may have only performed a few operations and may have decided to stop the procedure because of complications. The Registry believes that the higher rate of revision was not the result of the actual prosthesis but because of its insertion through a new approach.
Limitations
There are limitations to this study performed with data from the Registry. The outcome measure used was time to first revision. The Registry does not have information on dislocation or other complications that did not lead to revision nor information on length of stay, levels of perioperative pain, nor function. However, early revision is a devastating result for a patient and may outweigh any other perceived benefits. Thus, the true complication rate may be substantially higher than what we describe, particularly if early dislocations and periprosthetic fractures were managed without surgery. We also cannot be certain that all procedures with the Quadra-H/Versafit combination were performed through the anterior approach. Crosschecking the data with company records by the senior author showed that at least 95% of procedures were performed through the direct anterior approach. Therefore, there could be some cases that had lateral or posterior approaches. At the time of this data collection, the Registry did not collect specific data related to the surgical approach for THA. The authors believe that this however is unlikely to affect the analysis. Furthermore, because we report on the learning curve for those surgeons who persevered with over 100 cases, we cannot draw conclusions regarding the experience of those practitioners who abandoned either the approach or the implant in question. Although we report only on one particular implant combination, the design features of these implants are common to many widely used components, and we do not believe that our results are unique to these devices.
There is conflicting data published on the results of the anterior approach for THA for all surgeons performing this procedure. The Registry previously identified a higher than expected rate of revision for this combination, especially in the early period after surgery. The cumulative percent revision for the anterior approach for all surgeons is higher than for other approaches to THA as reported in the AOANJRR Annual Report [3]. There was a higher rate of revision for periprosthetic fracture in the Quadra-H/Versafit group compared with the revision diagnosis previously published for other conventional THAs [3]. This may have reflected difficulties with the preparation and insertion of the femoral stem.
A recent systematic review and meta-analysis comparing anterior and posterior approaches for THA demonstrated no clear superiority of either approach [10]. The primary outcome measure was validated patient-reported outcomes focused on pain and function. Data were not presented on rates of revisions between the two groups although the authors did state that they excluded two articles in which the “learning curve” for the anterior approach was used. It is not clear whether other articles reviewed stated whether the anterior approach was evaluated for the surgeons’ first cases.
We have shown that more experienced surgeons have a lower rate of revision. Surgeons who started the procedures between 2007 and 2010 tended to be more experienced than those surgeons who started in 2011 and this may explain the higher rate of revision. A previous study from the Registry has shown that surgical experience is related to outcome [3]. Poehling-Monaghan et al. [16] reported on a study of 222 patients comparing the direct anterior with the miniposterior THA. Two surgeons performed exclusively either approach and had extensive prior experience before the study started (over 300 procedures with the anterior approach). There were no differences between the two groups in length of stay, operative or in-hospital complications, or maximum distance walked in the hospital. Based on the data, this comparison effectively compared this procedure when the surgeon had passed the learning curve.
The learning curve can only be evaluated by following surgeons as they progress and perform more procedures. The learning curve is not the overall result of the rate of revision, number of complications, or length of stay after a certain number of procedures. We have shown that for surgeons who have performed more than 100 procedures, their rate of revision reduced from 6% for the first 15 procedures compared with 2% after their first 100. Surgeons needed to perform over 50 procedures to reach a rate of revision no different from performing over 100 procedures.
Our study confirms the findings of others, although it differs in the number of patients treated. Goytia et al. [9] evaluated the learning curve for the anterior approach to THA by studying 73 patients undergoing 81 consecutive procedures. They stated that surgical proficiency (surgical time, blood loss) improved after 40 cases and surgeons using this approach should expect a substantial learning period. Muller et al. [15] examined a consecutive series of 150 THA implanted with the anterior approach during the introduction of the technique and retrospectively analyzed the data after a minimum of 5 years. The 5-year survival rate for any implant revised was 95%. However, for the first 20 cases, it was 79% and for the next 130 cases 97%. The authors stated that the adoption of the anterior approach temporarily exposed patients to a higher risk of implant revision. They stated half of the perioperative complications occurred within the first 20 cases of the senior surgeon introducing the technique and these occurred within the first year. Spaans et al. [19] matched 46 patients using the direct anterior approach with 46 control subjects operated on using the posterolateral approach and found a higher complication rate. They did not demonstrate any improvement after 46 cases.
This study differed in that we were able to accurately measure the reduction in the revision rate over several time periods as the surgeon moved through their individual learning curve. This does raise the question of how many patients a surgeon would like to expose to a learning curve, especially if good results and a low complication rate can be achieved by other means [19].
Conclusions
This study has shown the effect of the learning curve for THA using a new surgical approach by analyzing the rate of revision using data from a national registry. The Quadra-H/Versafit combination implanted through a direct anterior approach using a leg holder requires 50 or more procedures to be performed by a surgeon before the rate of revision is no different from 100 or more procedures. Surgeons should be aware of this initial higher rate of revision when deciding which approach delivers the best outcome for their patients.
Acknowledgments
We thank the AOANJRR and the hospitals, orthopaedic surgeons, and patients whose data made this work possible. The Australian Government funds the AOANJRR through the Department of Health and Ageing.
Footnotes
The Australian Government funds the AOA NJRR through the Department of Health and Aging.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
References
- 1.Australian Orthopaedic Association National Joint Replacement Registry Annual Report. Adelaide, Australia: AOA; 2009. Available at: https://aoanjrr.dmac.adelaide.edu.au/annual-reports-2009. Accessed February 2, 2015.
- 2.Australian Orthopaedic Association National Joint Replacement Registry Annual Report. Adelaide, Australia :AOA; 2012. Available at: https://aoanjrr.dmac.adelaide.edu.au/annual-reports-2012. Accessed February 2, 2015.
- 3.Australian Orthopaedic Association National Joint Replacement Registry Annual Report. Adelaide, Australia: AOA; 2013. Available at: https://aoanjrr.dmac.adelaide.edu.au/annual-reports-2013. Accessed March 20, 2015.
- 4.Christensen CP, Karthikeyan T, Jacobs CA. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplasty. 2014;29:1839–1841. doi: 10.1016/j.arth.2014.04.036. [DOI] [PubMed] [Google Scholar]
- 5.D’Arrigo C, Speranza A, Monaco E, Carcangiu A, Ferretti A. Learning curve in tissue sparing total hip replacement: comparison between different approaches. J Orthop Traumatol. 2009;10:47–54. doi: 10.1007/s10195-008-0043-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Steiger RN, Graves SE, Hang J, Davidson D, Miller L. Five year results of the ASRTM XL Acetabular System and the ASRTM Hip Resurfacing System: analysis from Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am. 2011;93:2287–2293. doi: 10.2106/JBJS.J.01727. [DOI] [PubMed] [Google Scholar]
- 7.de Steiger RN, Miller LN, Davidson DC, Ryan P, Graves SE. Joint Registry approach for identification of outlier prostheses. Acta Orthop. 2013;84:348–352. doi: 10.3109/17453674.2013.831320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gladwell M. Outliers, the Story of Success. 1st ed. New York, NY, USA: Little, Brown and Company; Hachett Book Group; November 2008.
- 9.Goytia RN, Jones LC, Hungerford MW. Learning curve for the anterior approach total hip arthroplasty. J Surg Orthop Adv. 2012;21:78–83. doi: 10.3113/JSOA.2012.0078. [DOI] [PubMed] [Google Scholar]
- 10.Higgins BT, Barlow DR, Heagerty NE. Anterior vs posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J Arthroplasty. 2015;30:419–434. doi: 10.1016/j.arth.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 11.Jaret P. A new approach to hip surgery. The New York Times; March 18, 2013. Available at: http://well.blogs.nytimes.com/2013/03/18/faster-recovery-from-hip-surgery/?_php=true&_type=blogs&_r=0. Accessed February 5, 2014.
- 12.Kennon RE, Keggi JM, Wetmore RS, Zatorski LE, Huo MH, Keggi KJ. Total hip arthroplasty through a minimally invasive anterior surgical approach. J Bone Joint Surg Am. 2003;85(Suppl 4):39–48. doi: 10.2106/00004623-200300004-00005. [DOI] [PubMed] [Google Scholar]
- 13.Masonis J, Thompson C, Odum S. Safe and accurate: learning the direct anterior total hip arthroplasty. Orthopedics. 2008;31(Suppl 2):1417–1426. [PubMed] [Google Scholar]
- 14.Matsen KL. New technology: safety, efficacy, and learning curves. Clin Orthop Relat Res. 2014;472:1080–1085. doi: 10.1007/s11999-013-3413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muller DA, Zingg PO, Dora C. Anterior minimally invasive approach for total hip replacement: five-year survivorship and learning curve. Hip Int. 2014;24:277–283. doi: 10.5301/hipint.5000108. [DOI] [PubMed] [Google Scholar]
- 16.Poehling-Monaghan KL1, Kamath AF, Taunton MJ, Pagnano MW. Direct anterior versus miniposterior THA with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res. 2014 Aug 1 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 17.Siguier T, Siguier M, Brumpt B. Mini-incision anterior approach does not increase dislocation rate: a study of 1037 total hip replacements. Clin Orthop Relat Res. 2004;426:164–173. doi: 10.1097/01.blo.0000136651.21191.9f. [DOI] [PubMed] [Google Scholar]
- 18.Spaans AJ, van den Hout JAAM, Bolder SBT. High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop. 2012;83:342–346. doi: 10.3109/17453674.2012.711701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spaans AJ, van den Hout JAAM, Bolder SBT. Correspondence on high complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop. 2013;84:116–117. doi: 10.3109/17453674.2013.773412. [DOI] [PMC free article] [PubMed] [Google Scholar]