Abstract
Background
The incidence of acetabular fractures in osteoporotic patients is increasing. Immediate total hip arthroplasty (THA) has potential advantages, but achieving acetabular component stability is challenging and, at early followup, reported revision rates for loosening are high.
Questions/purposes
This study measured acetabular component stability and the initial surface contact achieved between the acetabular component and unfractured region of the pelvis after THA using an oversized acetabular component and cup-cage reconstruction.
Methods
Between November 2011 and November 2013, we treated 40 acute acetabular fractures in patients older than 70 years of age. Of these, 12 (30%) underwent immediate THA using an oversized acetabular component with screws inserted only into the ilium and a cup-cage construct. Postoperatively all patients were mobilized without weightbearing restrictions. Indications for immediate THA after acetabular fractures were displaced articular comminution deemed unreducible. Eleven of the 12 were prospectively studied to evaluate the initial stability of the reconstructions using radiostereometric analysis. One of the patients died of a pulmonary embolism after surgery, and the remaining 10 (median age, 81 years; range, 72–86 years) were studied. Of these, five were analyzed at 1 year and five were analyzed at 2 years. Acetabular component migration was defined as acceptable if less than the limits for primary THA that predict later loosening (1.76 mm of proximal migration and 2.53° of sagittal rotation). The contact surface between the acetabular component and ilium in direct continuity with the sacroiliac joint, and the ischium and pubis in direct continuity with the symphysis pubis, was measured on postoperative CT scans.
Results
At 1 year the median proximal migration was 0.83 mm (range, 0.09–5.13 mm) and sagittal rotation was 1.3° (range, 0.1°–7.4°). Three of the 10 components had migration above the suggested limits for primary THA at 1 year postoperatively. The contact surface achieved at surgery between the acetabular component and pelvis ranged from 11 to 17 cm2 (15%–27% of each component).
Conclusions
The majority of acetabular components in this cohort were stable despite the small contact surface achieved between the component and pelvic bone. Three of 10 migrated in excess of the limits that predict later loosening in primary THA but it remains to be seen whether these limits apply to this selected group of frail osteoporotic patients. We continue to use this technique routinely to treat patients with the same indications, but since the analysis of these data we have added screw fixation of the acetabular component to the ischial tuberosity and the superior pubic ramus.
Level of Evidence
Level IV, therapeutic study.
Introduction
The best treatment for osteoporotic acetabular fractures is not known. The incidence of acetabular fractures in older patients is increasing [6, 20], and these fractures are associated with high complication rates [4]. Open reduction and internal fixation (ORIF) is typically performed, but the difficulty in reconstruction, poor bone quality, and challenges in patient compliance often result in unfavorable outcomes [13, 16, 17]. These concerns and the less-than-satisfactory results of THA to treat posttraumatic arthritis after ORIF of acetabular fractures [5, 15, 26] have led to increasing interest in the use of THA in the acute phase after the fracture in selected patients [4, 5]. The published results of this treatment are difficult to interpret because the number of patients reported is small, the followup is short, and the techniques used for achieving and measuring acetabular component stability are variable [4, 5].
One of the challenges when performing THA for acute acetabular fractures is achieving acetabular component stability because the uncontained acetabular fragments preclude effective cement pressurization or press-fit cementless fixation of the acetabular component. This has led to early radiographic loosening being reported in up to 21% of cases [25]. As a result, several ancillary techniques have been reported, including Burch-Schneider antiprotrusion cages [32], cable fixation [18], plate fixation [24], and cup-cage construct [1]. Although not all papers reporting on the results of THA for acute acetabular fractures have reported early cup loosening, no study has used a sensitive radiographic method to assess acetabular component migration. Early migration is a well-established predictor for late aseptic loosening of primary acetabular components [11, 19]. However, plain radiographs cannot detect the suggested acceptable thresholds of 1.76 mm proximal migration and 2.53° sagittal rotation that may predict late aseptic loosening [19]. By contrast, radiostereometric analysis (RSA) is the most sensitive in vivo technique to assess prosthesis migration [9] and was the technique used to establish these thresholds [19].
Therefore, the primary aim of this study was to determine the early migration of the acetabular component in THA performed for acute osteoporotic acetabular fractures in our institution using RSA. Given that acetabular component stability has been associated with the size of the contact surface between the acetabular component and the host hip bone and that this contact is likely to be low when performing THA for acute acetabular fractures, the secondary aim was to measure this surface in these cases using postoperative CT scans.
Patients and Methods
This study, approved by the ethics committee of our institution (RAH protocol no. 060621), reports on a prospective case series of acute, displaced osteoporotic acetabular fractures treated with a primary THA using pelvic distraction and cup-cage reconstruction.
Between November 1, 2011, and November 30, 2013, we treated 40 patients older than 70 years of age with acetabular fractures. Of these, 12 (30%) were treated with immediate THA, all with a cup-cage construct and an oversized cup. Indications for immediate THA included a displaced associated fracture involving the anterior or both columns where the acetabular dome was not in direct connection with the sacroiliac joint/axial skeleton, irreducible articular comminution, protrusion of > 1 cm, and osteoporosis. Contraindications for immediate THA were fractures with < 1 cm of displacement, nonosteoporotic fractures, and patients who refused surgical treatment. Inclusion criteria for our study group included patients treated with immediate THA for acute acetabular fractures during November 2011 and 2013, acceptance to participate, and RSA of acetabular component migration. Exclusion criteria included refusal to participate and patients living more than 300 km from our center. Of our initial 12 patients treated with immediate THA, 11 patients, seven women and four men with a median age of 81 years (range, 76–87 years), satisfied the inclusion and exclusion criteria and were included in the study (Table 1). These 11 patients had the following fracture types according to the classification of Judet and Letournel [8]: anterior column posterior hemitransverse fracture (seven), associated both column fracture (three), and anterior column fracture (one).
Table 1.
Patient demographics, fracture classification, and length of hospital stay
| Patient number | Age (years) | Sex | Living status before injury | T-score (lumbar vertebrae) | Mechanism of injury | Fracture classification | Charlson Comorbidity Index | Length of hospital stay (days) | Length of hospital/rehabilitation stay after surgery (days) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 84 | F | Community dweller | −3.90 | LE | ACPHT | 4 | 12 | 9 |
| 2 | 86 | F | Community dweller | −4.34 | LE | ACPHT | 2 | 63 | 54 |
| 3 | 84 | F | Nursing home | −4.77 | LE | ABC | 2 | 16 | 8 |
| 4 | 81 | M | Community dweller | −3.76 | LE | ACPHT | 3 | 21 | 18 |
| 5 | 76 | M | Community dweller | −2.84 | HE (scooter) | AC | 2 | 14 | 8 |
| 6 | 79 | F | Community dweller | −4.97 | LE | ACPHT | 2 | 30 | 28 |
| 7 | 81 | F | Retirement village | −2.98 | LE | ABC | 1 | 17 | 10 |
| 8 | 87 | M | Community dweller | −3.17 | LE | ACPHT | 2 | 56 | 55 |
| 9 | 72 | M | Community dweller | −3.13 | HE (fall from 3-m height) | ABC | 2 | 26 | 16 |
| 10 | 75 | F | Community dweller | −2.68 | HE (MVA) | ACPHT | 0 | 25 | 19 |
| 11 | 86 | F | Community dweller | −6.06 | LE | ACPHT | 2 |
F = female; M = male; LE = low-energy (fall from standing height); HE = high energy (mechanism provided); MVA = motor vehicle accident; ACPTH = anterior column + posterior hemitransverse; ABC = associated both column; AC = anterior column.
The median Charlson Comorbidity Index [2] was 2 (range, 0–4). Median time to surgery from admission was 6 days (range, 1–10 days), and hospital/rehabilitation stay after surgery was 17 days (range, 8–55 days).
One patient died 7 days after surgery from a pulmonary embolism. Of the remaining 10 patients, there was no loss to followup and to date, five were analyzed out to 1 year and five were analyzed to 2 years.
All surgeries were performed through an extended posterior approach in which the superior gluteal bundle was exposed and protected throughout [27]. All reconstructions used an oversized trabecular metal acetabular component to achieve pelvic distraction and a cup-cage technique including screws inserted into the ilium. Briefly, after surgical exposure of the acetabulum, the articular cartilage was curetted away and the subchondral bone reamed using a reamer equal in diameter to that of the native acetabulum. We then placed sequentially larger trials until we identified the largest trial that fit the AP diameter of the pelvis without soft tissue impingement (Fig. 1).
Fig. 1A–C.
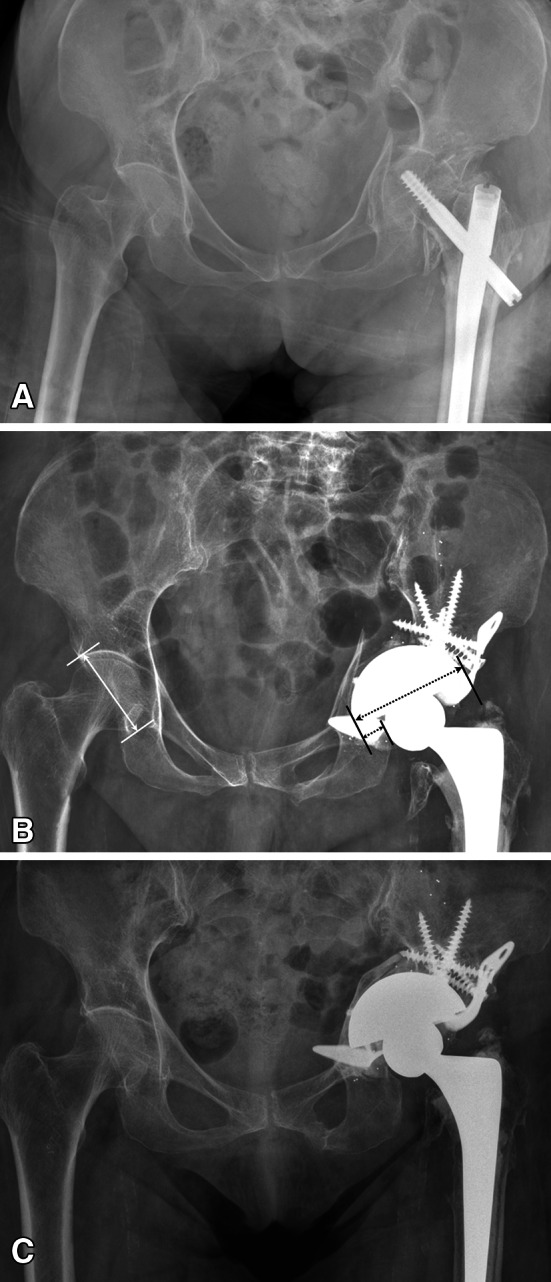
Preoperative (A), immediate postoperative (B), and 2 years postoperative (C) radiographs illustrating an acetabular fracture in the study—Case 3. (B) Note the difference between the diameter of the intact acetabulum (white solid arrow) and the diameter of the inserted acetabular component (long black dotted arrow) representing the degree of pelvic distraction (short black dotted arrow). (C) Note the pelvic discontinuity has been restored as the fracture healed.
After a femoral head autograft was inserted in the fracture site, we placed a revision TM acetabular component (Zimmer Inc, Warsaw, IN, USA) so that the rim spanned the gap between the intact ilium and the ischium. The acetabular component was then secured with screws in the ilioacetabular and sacroacetabular buttresses of the ilium [12, 28] by drilling additional holes, with a metal cutting burr, through the TM acetabular component near its rim. Once the cup was secured, we prepared the cage. Using a 2-cm osteotome, we created a slot in the ischium for insertion of the inferior flange of the cage. The appropriate size cage was then molded to fit the iliac wing and its inferior flange bent at approximately 90°. The inferior flange of the cage was inserted into the ischial slot while its superior flange was passed under the superior gluteal bundle and screwed into the ilium (Fig. 2).
Fig. 2.
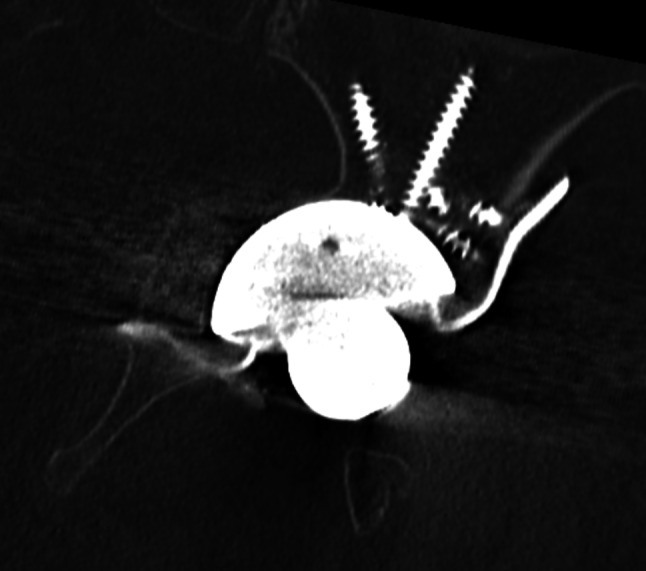
CT reconstruction image of the cup-cage construct used in Patient 3, illustrative for the reconstruction used in all patients in the study. Note the inferior flange of the cage in the ischium and the iliac fixation of the acetabular component with screws through the TM component and proximal flange of the cage.
Additional screws were inserted into the ilium by drilling holes through the cup-cage construct. After routine preparation of the femur, a trial reduction was performed to assess the optimal position of the liner in the cage, leg length, and stability using trial components. Using a metal cutting burr/disk, any prominent part of the cage interfering with the desired final position of the liner was removed. After inserting bone wax in the screw heads and graft in the empty holes of the TM acetabular component not covered by the cage, the liner was cemented in without pressurization in the late doughy phase. To allow for RSA analysis, up to 12 tantalum beads (0.8 mm diameter; RSA Biomedical, Umea, Sweden) were inserted in the stable parts of the ilium and the ischium.
After surgery all patients were encouraged to mobilize as tolerated without any imposed restrictions. Prophylactic antibiotics were given for the first 24 hours and deep vein thrombosis prophylaxis (Enoxaparin [Clexane®], 40 mg daily; Sanofi-Aventis Australia Pty Ltd, Macquarie Park, NSW, Australia) for 3 weeks.
Fracture healing was assessed on plain radiographs and was defined by bridging of the gap caused by the insertion of the oversized cup, uniting the supra- and infra-acetabular parts of the pelvic bone across the distracted pelvis.
Radiographic and RSA Analysis of Acetabular Component Stability
Plain AP and lateral radiographs and RSA radiographs were taken on the fourth postoperative day and then at 6 weeks, 3, 6, and 12 months and, for the five patients who reached 2 years followup at 24 months. For all RSA radiographic examinations, a uniplanar RSA setup with two radiographic tubes was used [3]. A room-mounted unit (Siemens Ysio Digital System; Siemens AG, Berlin, Germany) and a mobile radiographic unit (Shimadzu Art analog mobile machine; Shimadzu Medical Systems Ltd, Tokyo, Japan) were positioned with a 40° angle between the tubes. The calibration cage (Cage 43; RSA Biomedical) contained two 35 cm × 43-cm high-resolution digital radiographic cassettes (Agfa CR General plates; Agfa Healthcare, Mortsel, Belgium) with a focal length to the film of 1.6 m for each. The radiographic tubes were exposed simultaneously at 120 Kv and 16 mAs. The exposures were digitized with an AGFA Centricity CR SP1001 processor (AGFA Healthcare). Radiographs were analyzed using UmRSA software (Version 6.0 and UmRSA DICOM link; RSA Biomedical). Proximal migration and sagittal rotation of the acetabular component were determined in relation to reference markers that were inserted within an intact segment of the ilium. The limits used with the UmRSA software were 0.3 for the mean error of each rigid body and less than 250 for the condition number.
Acetabular component migration was defined as acceptable if it was less than the limits defined for primary THA that predict late loosening: 1.76 mm of proximal migration and 2.53° of sagittal rotation, respectively [19].
CT Measurement of Patient Bone Mineral Density and the Bone-implant Contact Surface
All patients underwent preoperative pelvic CT to assess fracture pattern, bone density, and to assist in preoperative planning. A postoperative pelvic CT was performed, on Day 4, to assess component position and host bone contact area. These examinations were performed using a high-resolution 128-slice CT scanner (Somatom Definition AS+; Siemens AG). CT scans of the hip were taken using a previously validated [30] CT protocol (140 kV, 200 mA, 0.75-second rotation speed, 1.25-mm slices, 1-mm feed). The reconstruction interval on coronal and sagittal images was 0.8 mm with a slice thickness of 1.25 mm. An extended scale technique [14] with a window level up to 30,710 Hounsfield units was used to suppress the resulting metal artifact. CT data were formatted in DICOM and then downloaded onto a Vitrea workstation (Vitrea Version 5.1; Vital Images Inc, Minnetonka, MN, USA). The quality of the CT images was additionally improved by adjustment of the window and level settings. The contact areas between pelvic bone and acetabular component were determined by one observer (RBS) traced on serial coronal CT slices with the use of a computer mouse and combined to give total contact distance. The total contact surface area was calculated by multiplying the total contact distance by the slice thickness. The surface area of the acetabular components (surface area of a hemisphere [A = 2π.r2]) was used to calculate the percentage of the bone-implant contact surface. Patient bone mineral density (BMD) was assessed on preoperative pelvic CT scans. Volumetric spinal BMD was measured at L4 and L5 using QCT Pro Bone Mineral Densitometry Software Version 5 (Mindways Software Inc, Austin, TX, USA) to determine patient T-scores.
This study was the first to measure migration of acetabular components to treat acetabular fractures using sensitive methods and therefore there was no historical data to base sample size calculation.
Results
Median proximal acetabular component migration at 1 year was 0.84 mm (range, 0.09–5.13 mm). Three acetabular components out of 10 had proximal migration or sagittal rotations above the suggested limits of migration for primary THA at 1 year (Table 2). Two acetabular components (Patients 3 and 4) had a proximal migration of 5.1 and 2.9 mm at 1 year, neither of which continued to migrate after 1 year (Fig. 3). However, one (Patient 4) did continue to rotate a further 2° between the 1- and 2-year examinations (Fig. 4). A third acetabular component (Patient 9) rotated 2.9° at 1 year, the majority of which occurred within the first 6 months. None of the five patients with 2-year followup had any additional proximal migration after 1 year above 0.2 mm (including the two acetabular components with the largest early migration). None of the patients whose component migration was above the acceptable threshold were symptomatic, and no patient is considered for revision. All fractures healed and all pelvic discontinuities restored by 6 months (Fig. 1).
Table 2.
Amount of acetabular distraction and contact between the acetabular component and the unfractured hip bone immediately after surgery and the acetabular component migration at 1-year followup
| Patient number | Native acetabular diameter (mm) | Cup diameter (mm) | Maximum possible acetabular distraction (mm) | Bone contact | Acetabular component migration relative to the ilium at 1 year | ||
|---|---|---|---|---|---|---|---|
| cm2 | Percent | Vertical translation (mm) | Sagittal rotation (°)* | ||||
| 1 | 49 | 64 | 15 | – | – | 0.43 | −1.3 |
| 2 | 51 | 64 | 13 | 15 | 25 | 0.41 | +0.3 |
| 3 | 44 | 64 | 20 | 16 | 27 | 5.13 | +7.4 |
| 4 | 59 | 76 | 17 | 17 | 20 | 2.87 | −2.2 |
| 5 | 49 | 68 | 19 | 17 | 25 | 0.66 | −1.3 |
| 6 | 47 | 62 | 15 | 14 | 26 | 1.17 | +1.9 |
| 7 | 58 | 70 | 12 | 11 | 15 | 0.41 | −0.1 |
| 8 | 54 | 70 | 16 | 12 | 16 | 1.22 | −0.2 |
| 9 | 53 | 72 | 19 | 17 | 22 | 1.01 | +2.9 |
| 10 | 52 | 68 | 16 | 12 | 18 | 0.09 | −0.9 |
* Positive rotation represents a decrease in inclination.
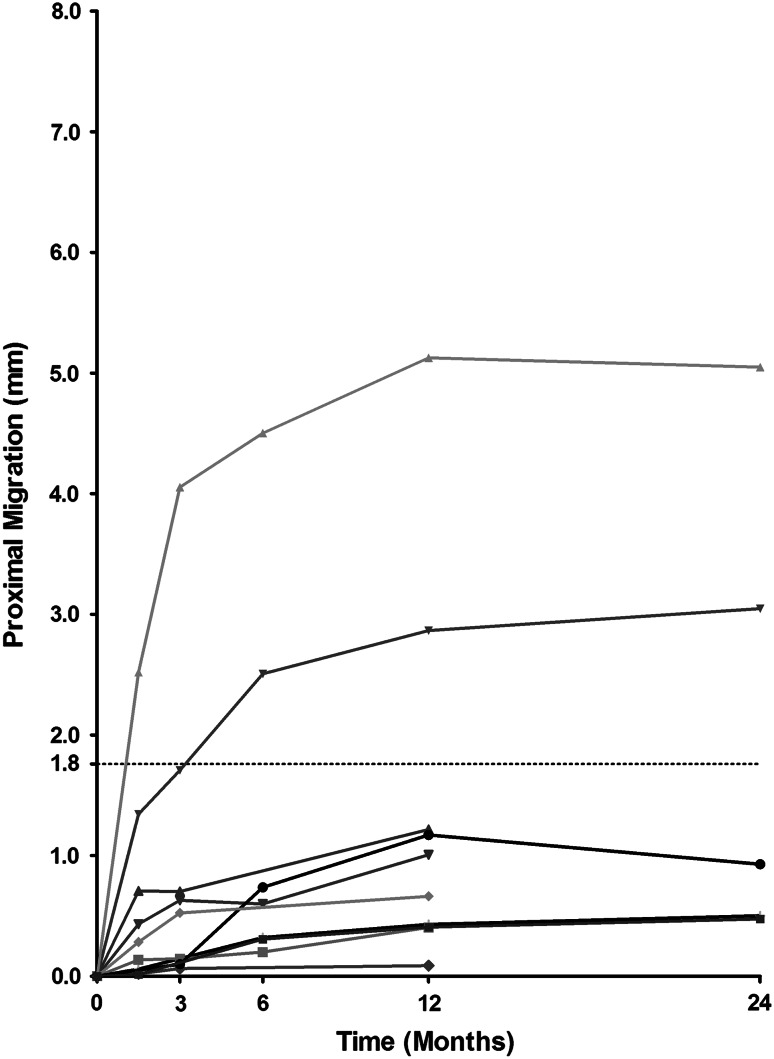
Fig. 3.
Superior migration of the acetabular components relative to the ilium over time. Note that two acetabular components (Patients 3 and 4) have migrated proximally more than 1.76 mm but that migration has stopped after 1 year.
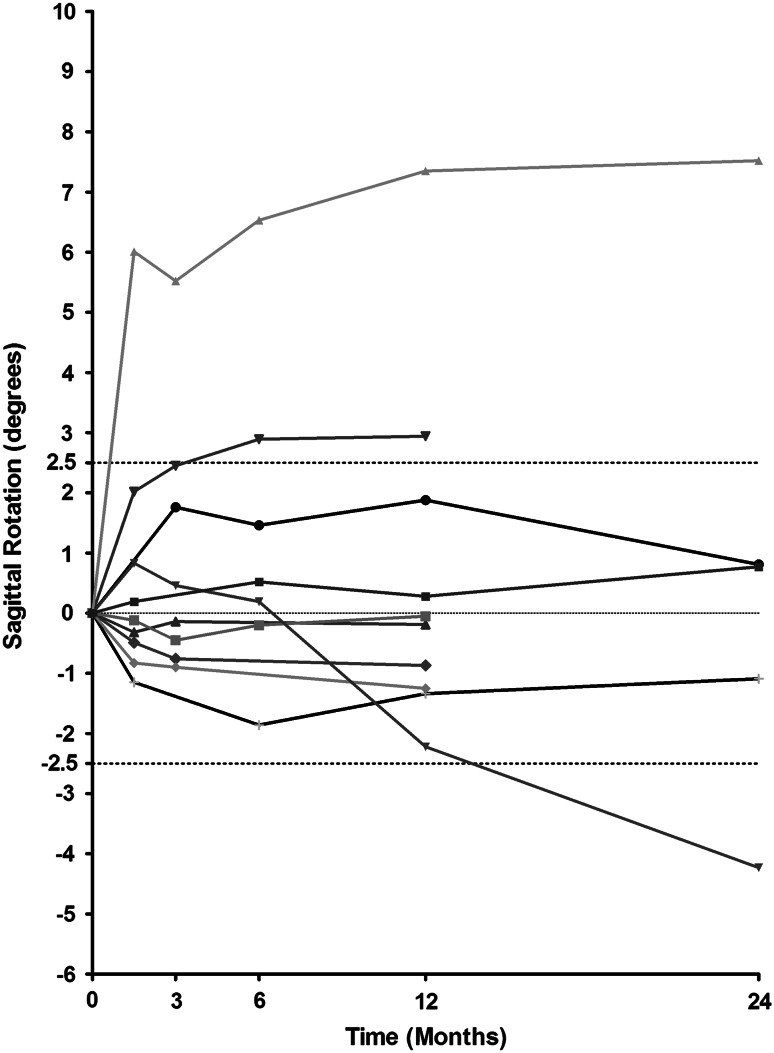
Fig. 4.
Sagittal rotation of the acetabular components relative to the ilium over time (positive rotation represents decrease in inclination). Note that two components have rotated more than 2.5° at 1 year (Patients 3 and 9). One cup (Patient 4) continued to rotate from 2.2° at 1 year to above the limit 4.2° at 2 years.
The contact surface achieved between the acetabular component and the unfractured region of the pelvis was small (Fig. 5) and measured between 8.5 and 17 cm2 or between 11% and 27% of the acetabular component surface (Table 2).
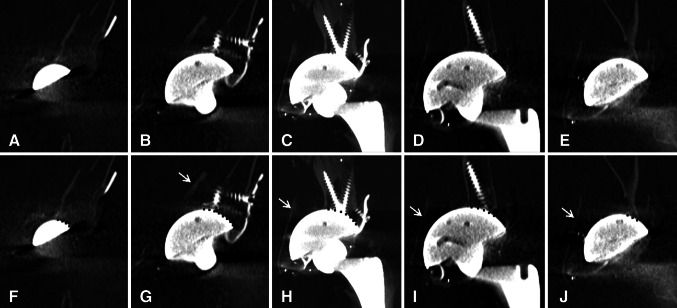
Fig. 5A–J.
Sequential anterior to posterior CT coronal reconstruction images of the acetabular reconstruction in Patient 3 illustrating the limited contact between the acetabular component and the unfractured host bone. Images A–E and F–J are identical with the ones in the lower row having contact surface marked by a dotted line. The fractured quadrilateral plate is pointed to by the white arrow.
Although not the focus of this article, the following complications were recorded before discharge: all patients had a low postoperative hemoglobin often requiring transfusion; two developed pulmonary embolism (including the patient who died), two developed pneumonia, two developed urinary tract infections, and two had postoperative confusion and delirium. There were no other late complications, including infections and dislocations, and all patients returned to their preinjury residence before 3 months after surgery.
Discussion
The incidence of acetabular fractures in osteoporotic patients and their acute management with THA are increasing. Achieving acetabular component stability in these cases is challenging and the reported risks of loosening and revision are high at early followup [25]. Pelvic distraction and cup-cage reconstruction have been previously used successfully in revision THA to treat pelvic discontinuity and severe acetabular defects [29]. Hence, we chose this technique to achieve initial acetabular component stability when performing THA for osteoporotic acetabular fractures. The only imaging method that allows early detection of acetabular component migration after THA is RSA, but to date, no study has investigated stability after THA for acute acetabular fractures using this sensitive and accurate technique. We found that in nine of the 10 patients investigated, the acetabular component stopped migrating at early followup. The migration of three acetabular components exceeded the limits known to predict later acetabular component loosening in primary THA performed for osteoarthritis [19].
This study has a number of limitations. First, the number of patients was small, a highly selected group treated in a tertiary center, and the followup short; durability of this approach will need to be established by continuing to follow these patients at longer term and by replicating these results in more patients and other centers. However, the use of a very sensitive measurement method, RSA, allows very detailed information to be gained from a small cohort in a short period of time. In line with a stepwise introduction of new treatments and the complexity of these cases, it is best that the development of new techniques is performed in highly specialized centers that have the ability not only to perform complex procedures, but also the ability to assess outcomes using the most accurate methods. It is important to note that if acetabular component migration was measured on plain radiographs, it is likely that all components would have been classified as stable and the pattern of migration remain unknown. Second, the limits of migration suggested for primary THA might not be applicable for this subgroup of patients who have multiple comorbidities, a limited life expectancy, and a smaller amount host bone available to achieve initial implant stability. Third, the study did not correlate the cup migration with the clinical outcomes in the patients investigated as a result of the small selective group of very frail patients included. It is very difficult to obtain clinical outcomes that are meaningful as a group beyond monitoring and reporting complications. However, in larger, future studies, clinical outcomes should be reported particularly when comparing various treatment methods. Fourth, the time from admission to surgery varied and this can affect outcomes. This variation was related to patient optimization in some cases and to the availability of surgical time in others. Fifth, it was not possible to measure migration of the acetabular component relative to the ischium because tantalum markers were often not visible on consecutive postoperative radiographs. Hence, only migration relative to the ilium is reported in this study. In future studies, better marker placement within the ischium will allow measurement of acetabular component migration relative to both the ilium and ischium, which will provide additional understanding of acetabular component stability. Sixth, the measurements of the surface contact between the acetabular component and unfractured pelvic bone may have been affected by the metal artifact. To minimize this effect, during measurement, any questionable area was included in the calculation of the total contact area. The ongoing improvements of metal artifact reduction techniques could improve such estimates in future studies.
The first aim of this study was to measure the early acetabular component stability after acute THA for osteoporotic acetabular fractures using an oversized acetabular component and cup-cage reconstruction. This was done using accurate methods as part of a stepwise introduction of a new surgical technique in our department. Early acetabular component migration has been shown to predict late loosening for both primary [11, 19] and, very recently, revision THA [10]. Three of 10 patients had acetabular component migration above suggested limits for primary THA. However, two of these components stabilized after 1 year with no further proximal migration or sagittal rotation. In a third patient, the component continued to rotate between 1 and 2 years suggesting it may be unstable. This is the first study that uses sensitive methods to measure early acetabular component migration in osteoporotic patients with displaced acetabular fractures treated with THA. Achieving initial cup stability is unquestionably more difficult than in most other primary THAs and, given the pelvic discontinuity, more difficult than in most revision THA. Therefore, the pattern of initial acetabular component migration might be very different after acute THA for acetabular fractures from those in other primary and some revision THAs. A different migration pattern has been previously reported for a subgroup of revision acetabular components treated with impaction bone grafting [21] despite the technique having good medium- to long-term results in cases with severe acetabular defects [7]. An RSA study reported a median proximal migration of 2.1 mm (range, 0.5–6.4 mm) at 2 years. The migration tended to stabilize before 1 year, but 33% of cups continued to migrate between 1 and 2 years after surgery [21], similar to the results reported in our study.
The second aim of this study was to measure the initial surface contact achieved between the acetabular component and unfractured region of the pelvis in our study group. Traditionally, the bone defects at revision THA guide and determine the reconstruction [22]. Less than 50% surface contact between acetabular components and the host pelvis is thought to unfavorably affect the outcomes of revision THA [7], but in two studies, surface contact was not an independent risk factor for migration and loosening [23, 31]. To date the contact surface between acetabular components and the pelvic bone has only been assessed by visual inspection before cup insertion [23, 31]. Such methods are quite crude and subject to significant bias and error. As CT has been validated for quantitative measurements of osteolysis around acetabular components [30], this method seems appropriate to be used to assess the surface contact between acetabular components and the pelvic bone. Our study has suggested that, in some cases, cup stability can be achieved even if the surface contact between the component and the host bone is very small. This is the first study to have measured contact surface achieved rather than visually approximating it as being more or less than a certain percent [23, 31].
The majority of acetabular components in this cohort was stable despite the small contact surface achieved between the component and pelvic bone. Three of 10 components migrated in excess of the limits that predict later loosening in primary THA. Although late loosening might be irrelevant in this selected group of frail osteoporotic patients, caution should be applied when planning to treat younger patients with acute acetabular fractures with this technique. We continue to use this technique routinely to treat patients with the same indications, but since the analysis of these data we have added screw fixation of the cup to the ischial tuberosity and the superior pubic ramus.
Footnotes
One or more of the authors (LBS, SAC, DWH) list the following relevant financial activities outside of this work and/or any other relationships or activities that readers could perceive to have influenced, or that give the appearance of potentially influencing, this manuscript: Zimmer Ltd (Warsaw, IN, USA) in the amount of USD 10,000 to USD 100,000.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Chana-Rodriguez F, Villanueva-Martinez M, Rojo-Manaute J, Sanz-Ruiz P, Vaquero-Martin J. Cup-cage construct for acute fractures of the acetabulum, re-defining indications. Injury. 2012;43(Suppl 2):S28–32. doi: 10.1016/S0020-1383(13)70176-1. [DOI] [PubMed] [Google Scholar]
- 2.Charlson MP, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 3.Chehade MJ, Solomon LB, Callary SA, Benveniste SH, Pohl AP, Howie DW. Differentially loaded radiostereometric analysis to monitor fracture stiffness: a feasibility study. Clin Orthop Relat Res. 2009;467:1839–1847. doi: 10.1007/s11999-009-0708-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD. Acetabular fractures in patients aged > 55 years: a systematic review of the literature. Bone Joint J. 2014;96:157–163. doi: 10.1302/0301-620X.96B2.32979. [DOI] [PubMed] [Google Scholar]
- 5.De Bellis UG, Legnani C, Calori GM. Acute total hip replacement for acetabular fractures: a systematic review of the literature. Injury. 2014;45:356–361. doi: 10.1016/j.injury.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010;92:250–257. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Cimbrelo E, Cruz-Pardos A, Garcia-Rey E, Ortega-Chamarro J. The survival and fate of acetabular reconstruction with impaction grafting for large defects. Clin Orthop Relat Res. 2010;468:3304–3313. doi: 10.1007/s11999-010-1395-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646. [PubMed] [Google Scholar]
- 9.Karrholm J, Gill RH, Valstar ER. The history and future of radiostereometric analysis. Clin Orthop Relat Res. 2006;448:10–21. doi: 10.1097/01.blo.0000224001.95141.fe. [DOI] [PubMed] [Google Scholar]
- 10.Klerken T, Mohaddes M, Nemes S, Karrholm J. High early migration of the revised acetabular component is a predictor of late cup loosening: 312 cup revisions followed with radiostereometric analysis for 2–20 years. Hip Int. 2015 Apr 27 [Epub ahead of print]. [DOI] [PubMed]
- 11.Krismer M, Stockl B, Fischer M, Bauer R, Mayrhofer P, Ogon M. Early migration predicts late aseptic failure of hip sockets. J Bone Joint Surg Br. 1996;78:422–426. [PubMed] [Google Scholar]
- 12.Letournel E, Judet R. Fractures of the Acetabulum. New York, NY, USA: Springer-Verlag; 1981. [Google Scholar]
- 13.Liebergall M, Mosheiff R, Low J, Goldvirt M, Matan Y, Segal D. Acetabular fractures. Clinical outcome of surgical treatment. Clin Orthop Relat Res. 1999;366:205–216. doi: 10.1097/00003086-199909000-00027. [DOI] [PubMed] [Google Scholar]
- 14.Link TM, Berning W, Scherf S, Joosten U, Joist A, Engelke K, Daldrup-Link HE. CT of metal implants: reduction of artifacts using an extended CT scale technique. J Comput Assist Tomogr. 2000;24:165–172. doi: 10.1097/00004728-200001000-00029. [DOI] [PubMed] [Google Scholar]
- 15.Makridis KG, Obakponovwe O, Bobak P, Giannoudis PV. Total hip arthroplasty after acetabular fracture: incidence of complications, reoperation rates and functional outcomes: evidence today. J Arthroplasty. 2014;29:1983–1990. doi: 10.1016/j.arth.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 16.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 17.Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003;407:173–186. doi: 10.1097/00003086-200302000-00026. [DOI] [PubMed] [Google Scholar]
- 18.Mouhsine E, Garofalo R, Borens O, Blanc CH, Wettstein M, Leyvraz PF. Cable fixation and early total hip arthroplasty in the treatment of acetabular fractures in elderly patients. J Arthroplasty. 2004;19:344–348. doi: 10.1016/j.arth.2003.08.020. [DOI] [PubMed] [Google Scholar]
- 19.Nieuwenhuijse MJ, Valstar ER, Kaptein BL, Nelissen RG. Good diagnostic performance of early migration as a predictor of late aseptic loosening of acetabular cups: results from ten years of follow-up with Roentgen stereophotogrammetric analysis (RSA) J Bone Joint Surg Am. 2012;94:874–880. doi: 10.2106/JBJS.K.00305. [DOI] [PubMed] [Google Scholar]
- 20.Ochs BG, Marintschev I, Hoyer H, Rolauffs B, Culemann U, Pohlemann T, Stuby FM. Changes in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU) Injury. 2010;41:839–851. doi: 10.1016/j.injury.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Ornstein E, Franzén H, Johnsson R, Sandquist P, Stefánsdóttir A, Sundberg M. Migration of the acetabular component after revision with impacted morselized allografts: a radiostereometric 2-year follow-up analysis of 21 cases. Acta Orthop Scand. 1999;70:338–342. doi: 10.3109/17453679908997821. [DOI] [PubMed] [Google Scholar]
- 22.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 23.Patel S, Sukeik M, Haddad FS. Initial implant stability predicts migration but not failure in cementless acetabular revision with bone grafting. J Arthroplasty. 2013;28:832–837. doi: 10.1016/j.arth.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 24.Rickman M, Young J, Trompeter A, Pearce R, Hamilton M. Managing acetabular fractures in the elderly with fixation and primary arthroplasty: aiming for early weightbearing. Clin Orthop Relat Res. 2014;472:3375–3382. doi: 10.1007/s11999-014-3467-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sarkar MR, Wachter N, Kinzl L, Bischoff M. Acute total hip replacement for displaced acetabular fractures in older patients. Eur J Trauma. 2004;5:296–304. doi: 10.1007/s00068-004-1351-7. [DOI] [Google Scholar]
- 26.Sierra RJ, Mabry TM, Sems SA, Berry DJ. Acetabular fractures: the role of total hip replacement. Bone Joint J. 2013;95:11–16. doi: 10.1302/0301-620X.95B11.32897. [DOI] [PubMed] [Google Scholar]
- 27.Solomon LB, Hofstaetter JG, Bolt MJ, Howie DW. An extended posterior approach to the hip and pelvis for complex acetabular reconstruction that preserves the gluteal muscles and their neurovascular supply. Bone Joint J. 2014;96:48–53. doi: 10.1302/0301-620X.96B1.31464. [DOI] [PubMed] [Google Scholar]
- 28.Solomon LB, Howie DW, Henneberg M. The variability of the volume of os coxae and linear pelvic morphometry. Considerations for total hip arthroplasty. J Arthroplasty. 2014;29:769–776. doi: 10.1016/j.arth.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 29.Sporer SM, Bottros JJ, Hulst JB, Kancherla VK, Moric M, Paprosky WG. Acetabular distraction: an alternative for severe defects with chronic pelvic discontinuity? Clin Orthop Relat Res. 2012;470:3156–3163. doi: 10.1007/s11999-012-2514-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stamenkov R, Howie D, Taylor J, Findlay D, McGee M, Kourlis G, Carbone A, Burwell M. Measurement of bone defects adjacent to acetabular components of hip replacement. Clin Orthop Relat Res. 2003;412:117–124. doi: 10.1097/01.blo.0000069001.16315.f4. [DOI] [PubMed] [Google Scholar]
- 31.Sternheim A, Backstein D, Kuzyk PR, Goshua G, Berkovich Y, Safir O, Gross AE. Porous metal revision shells for management of contained acetabular bone defects at a mean follow-up of six years: a comparison between up to 50% bleeding host bone contact and more than 50% contact. J Bone Joint Surg Br. 2012;94:158–162. doi: 10.1302/0301-620X.94B2.27871. [DOI] [PubMed] [Google Scholar]
- 32.Tidermark J, Blomfeldt R, Ponzer S, Soderqvist A, Tornkvist H. Primary total hip arthroplasty with a Burch-Schneider antiprotrusion cage and autologous bone grafting for acetabular fractures in elderly patients. J Orthop Trauma. 2003;17:193–197. doi: 10.1097/00005131-200303000-00007. [DOI] [PubMed] [Google Scholar]