Abstract
Background
Dislocation is a major complication after primary total hip arthroplasty (THA), but little is known about the potential relationships between bearing materials and risk of dislocation. Dislocation within the first year after surgery is typically related to either surgical error or patient inattention to precautions, but the reasons for dislocation after the first year are often unclear, and whether ceramic bearings are associated with an increased or decreased likelihood of late dislocation is controversial.
Questions/purposes
The purpose of this study was to use a national registry to assess whether the choice of bearings–metal-on-polyethylene (MoP), ceramic-on-polyethylene (CoP), ceramic-on-ceramic (CoC), or metal-on-metal (MoM)–is associated with differences in the risk of late dislocation.
Methods
Data from primary THAs were extracted from the New Zealand Joint Registry over a 10-year period. The mean age of patients was 69 years (SD ± 12 years), and 53% were women. The median followup in this population was 7 years (range, 1–13 years). The surgical approach used was posterior in 66% of THAs, lateral in 29%, and anterior in 5%. The primary endpoint was late revision for dislocation with “late” defined as greater than 1 year postoperatively. A total of 73,386 hips were available for analysis: 65% MoP, 17% CoP, 10% CoC, and 7% MoM. In general, patients receiving CoC and MoM bearings were younger compared with patients receiving CoP and MoP bearings.
Results
Four percent of the hips were revised (3130 THAs); 867 THAs were revised for dislocation. Four hundred seventy THAs were revised for dislocation after the first postoperative year. After adjusting for head size, age, and surgical approach, only CoP (hazard ratio [HR], 2.10; p = 0.021) demonstrated a higher proportion of revision, whereas MoP did not (HR, 1.76; 95% p = 0.075). There were no differences of revisions for dislocation in the CoC (HR, 1.60; p = 0.092) and MoM cohorts (HR, 1.54; p = 0.081).
Conclusions
Dislocation is a common reason for revision after THA. The relationships between bearing materials and risk of revision for late dislocation remain controversial. This large registry study demonstrated that bearing surface had little association with the incidence of late dislocation. Future studies with longer followups should continue to investigate this question.
Level of Evidence
Level III, therapeutic study.
Introduction
Dislocation is a major complication after THA. In the 2014 New Zealand Joint Registry report, dislocation has been identified as the most common reason for primary THA revision ahead of aseptic loosening of the acetabular component and femoral component [21]. The incidence of dislocation is highest in the first year after surgery and then continues at a relatively constant rate over the life of the arthroplasty [2, 5]. Recurrent dislocation is a frequent reason for revision [20]. Surgical approach, component orientation, offset reconstruction, femoral head size, and patient neurological status are common factors associated with a potential risk of dislocation [3, 13].
Little is known about the potential relationships between bearing materials and risk of dislocation. Limited availability of options for stem offset adjustments and acetabular liner design are considered potential causes of increased risk of dislocation in ceramic THAs [6, 15]. Bader et al. [1] found no difference in forces required to dislocate a THA in vitro when using bearing surfaces of different materials. However, ceramic bearings showed higher instability when the cup was implanted in a position causing impingement between the stem and liner. In a long-term study, Hernigou et al. [9] found that alumina-on-alumina bearing couples decrease the cumulative risk of late dislocation as compared with alumina-on-polyethylene (PE). On the other hand, Sexton et al. [20] from the Australian Orthopaedic Association National Joint Replacement Registry reported a higher rate of revision for dislocation in ceramic-on-ceramic THAs than in metal-on-PE THAs in some subgroups of patients. Risk factors for dislocation are thought to differ between early and late events with patient and mechanical factors playing a larger role in early dislocation and biological factors affecting late dislocation [7, 11]. In this article, we elected to define a late dislocation requiring revision occurring 1 year after the index surgery.
The objective of this New Zealand National Registry study was to assess whether the choice of bearings–metal-on-polyethylene (MoP), ceramic-on-polyethylene (CoP), ceramic-on-ceramic (CoC), or metal-on-metal (MoM)–is associated with differences in the risk of late dislocation.
Materials and Methods
We extracted data on all primary THAs between January 1, 1999, and December 31, 2012, from the New Zealand National Joint Registry. This registry has a hospital compliance of 98%, and data are validated against the New Zealand Health Information Service. During this time, 81,972 primary THAs were carried out in New Zealand. The mean age of the patients undergoing primary THA was 69 years (SD ± 12) and 53% were women. Osteoarthritis was the indication for surgery in 88% of hips. All diagnoses for primary THA were included in this study. The approach used was posterior in 65% of THAs, lateral in 28%, and anterior in 4%. Surgeon grade was recorded from 2005 onward with the majority of THAs performed by consultant surgeons (87%). The bearing surfaces included 8177 (10%) CoC, 14,093 (17%) CoP, 461 (0.5%) ceramic-on-metal, 5910 (7%) MoM, and 53,331 (65%) MoP. All CoC bearings were 28 mm in diameter or bigger.
There were 73,386 hips at 1 year postoperatively, 65,387 hips at 2 years postoperatively, 42,086 hips at 5 years postoperatively, and 12,967 hips at 10 years postoperatively. The median followup was 7 years (range, 1–13 years).
The cumulative proportion of patients revision-free for dislocation of primary THAs at Years 1, 2, 5, and 10 was estimated using the Kaplan-Meier method. The mortality rate of patients included in this study over the median of 7 years followup is 2%. We therefore elected not to carry out competitive risk analysis. The primary endpoint was late revision for dislocation with late defined as greater than 1 year postoperatively. Thus, the primary analysis was performed on data excluding the first postoperative year. The overall, unadjusted dislocation revision rates for each bearing combination type were compared using the log rank test, where the adjusted risk ratios for age, head size, and surgical approach were calculated using the Cox regression model. An additional analysis was performed on data including the first postoperative year. For all analyses, a two-tailed p value < 0.05 was considered significant. Of note, observed component-years are defined as the number of registered primary THAs multiplied by the number of years each component has been in place. Revision rate/100 component-years reflects the yearly revision rate as a percent and is derived by dividing the number of prostheses revised by the observed component-years multiplied by 100.
Results
Three thousand one hundred thirty THAs (4%) were revised for any cause with a rate of 0.70 per 100 component-years, and 867 (1.1%) were revised for dislocation with a rate of 0.19 per 100 component-years. Four hundred seventy (0.65%) hips were revised for dislocation after the first postoperative year with a rate of 0.11 per 100 component-years. CoC bearings had the lowest proportion of revisions in the observation period after the first postoperative year (38%) compared with CoP (63%), MoM (48%), and MoP (54%) (Table 1). We found that there was little association in this series between bearing type and late dislocation after adjusting for head size, age, and surgical approach. Overall, only CoP THAs (hazard ratio [HR], 2.10; p = 0.021) had a higher proportion of revisions, whereas MoP did not (HR, 1.76; 95% p = 0.075). There were no differences of revisions for dislocation in the CoC (HR, 1.60; p = 0.092) and MoM THAs (HR, 1.54; p = 0.081).
Table 1.
Time to revision for dislocation by bearing surface*
| Bearing surface | Time to revision for dislocation | Total number | |
|---|---|---|---|
| < 1 year | ≥ 1 year | ||
| Number (%) | Number (%) | ||
| Ceramic-on-ceramic | 26 (62) | 16 (38) | 42 |
| Ceramic-on-polyethylene | 58 (37) | 98 (63) | 156 |
| Metal-on-metal | 25 (52) | 23 (48) | 48 |
| Metal-on-polyethylene | 288 (46) | 333 (54) | 621 |
| Total | 397 (46) | 470 (54) | 867 |
* The ceramic-on-ceramic couple had the highest proportion of revisions during the first postoperative year and the smallest proportion of revisions after the first postoperative year.
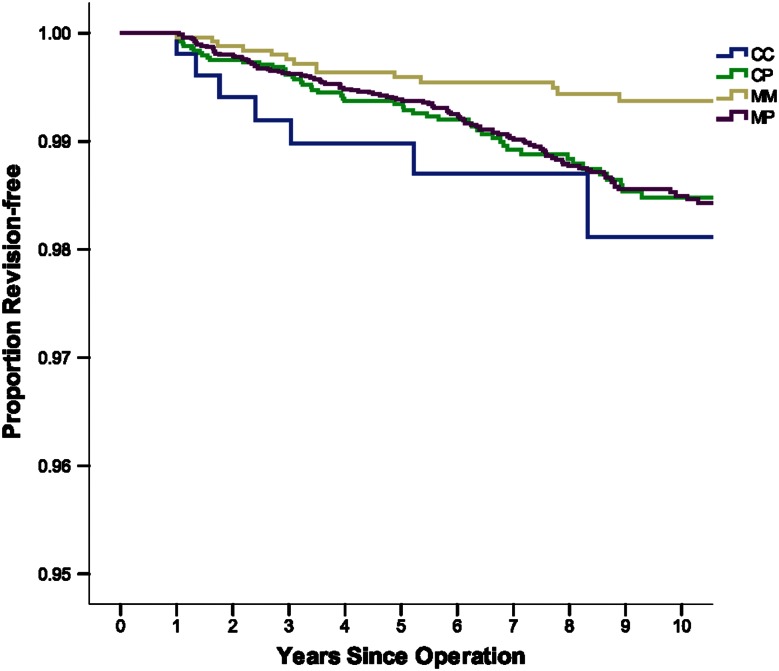
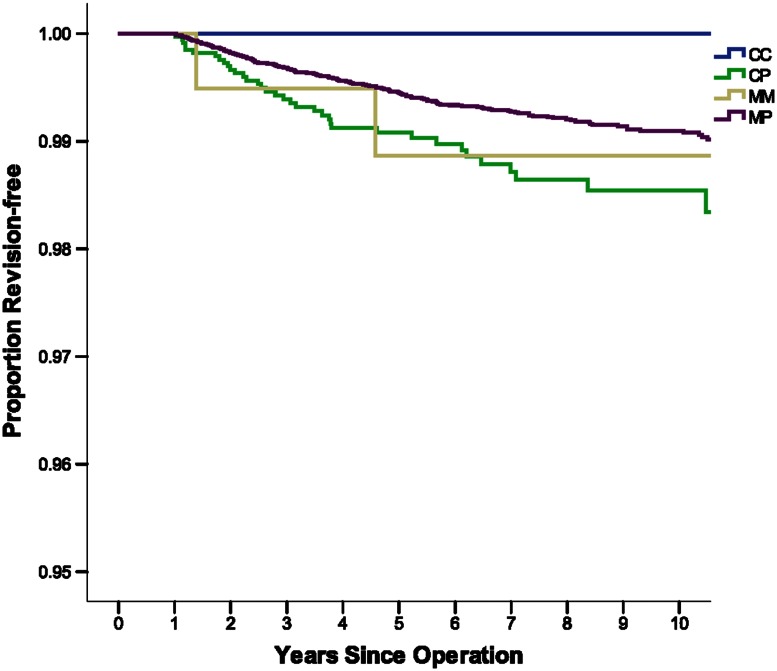
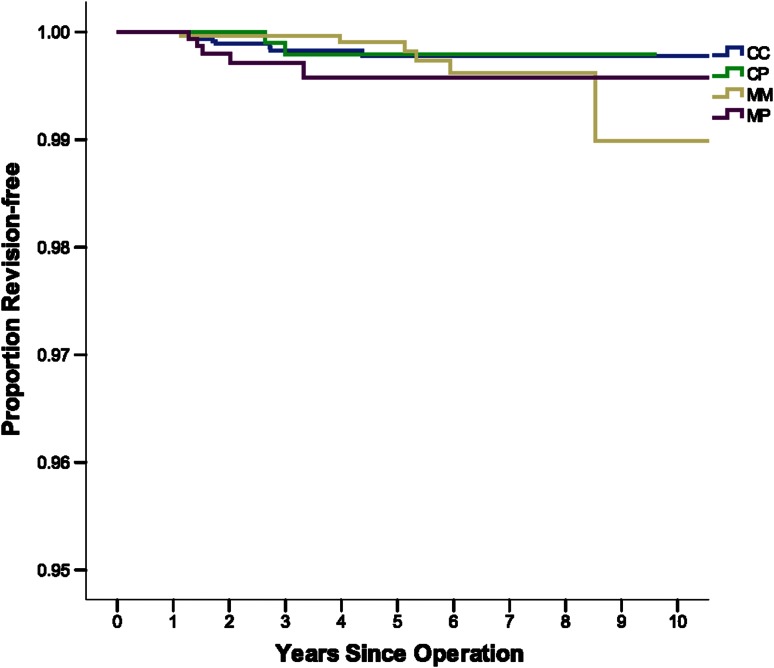
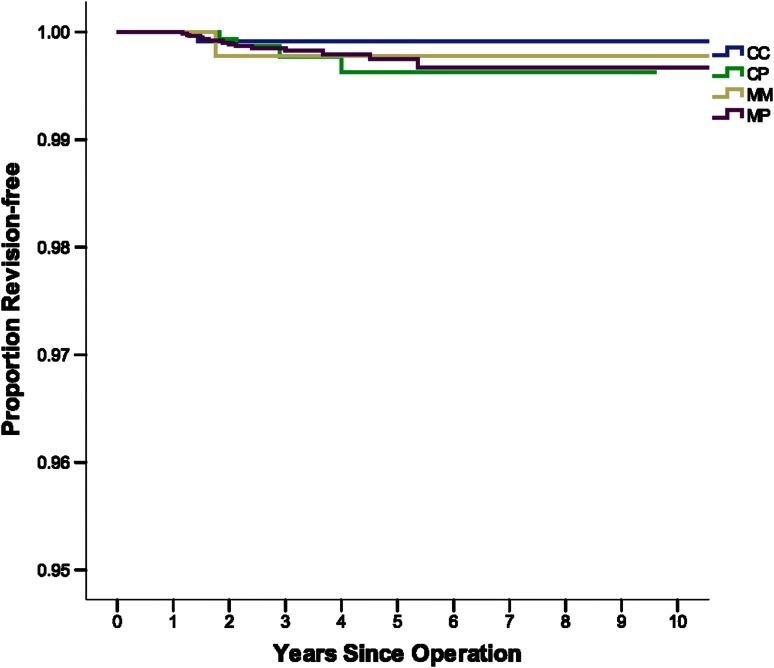
There were more revisions for late dislocation in CoC THAs than for MoM THAs in younger patients and smaller head size (< 65 years, 28 mm) (HR, 0.29; 95% confidence interval [CI], 0.12–0.71; p = 0.014) (Fig. 1). There were no other statistically significant differences for CoC THAs when stratified by age and head size. However, there were no revisions of CoC THAs in older patients with small head size (≥ 65 years, 28 mm) (Fig. 2). Also, CoC and CoP THAs showed the lowest revision rate in younger patients with large femoral head size (< 65 years, > 28 mm) (Fig. 3). Finally, CoC THAs showed the lowest revision rate in older patients with large femoral head size (≥ 65 years, > 28 mm) (Fig. 4).
Fig. 1.
This figure shows the proportion revision-free for dislocation from 1 year after THAs by bearing surface adjusted for femoral head size ≤ 28 mm and age < 65 years. CC = ceramic-on-ceramic; CP = ceramic-on-PE; MM = metal-on-metal; MP = metal-on-PE. CC showed the highest revision rate (100 components/year 0.20; CI, 0.08–0.42).
Fig. 2.
This figure shows the proportion revision-free for dislocation from 1 year after THAs by bearing surface adjusted for femoral head size ≤ 28 mm and age ≥ 65 years. CC = ceramic-on-ceramic; CP = ceramic-on-PE; MM = metal-on-metal; MP = metal-on-PE. CC showed the lowest revision rate (no revisions).
Fig. 3.
This figure shows the proportion revision-free for dislocation from 1 year after THAs by bearing surface adjusted for femoral head size > 28 mm and age < 65 years. CC = ceramic-on-ceramic; CP = ceramic-on-PE; MM = metal-on-metal; MP = metal-on-PE. CC showed the lowest revision rate (0.04 100 components/year; CI, 0.02–0.07) after CoP (0.03 100 components/year; CI, 0.00–0.13).
Fig. 4.
This figure shows the proportion revision-free for dislocation from 1 year after THAs by bearing surface adjusted for femoral head size > 28 mm and age ≥ 65 years. CC = ceramic-on-ceramic; CP = ceramic-on-PE; MM = metal-on-metal; MP = metal-on-PE. CC showed the lowest revision rate (100 components/year 0.02; CI, 0.00–0.12).
The analysis was repeated with the inclusion of early dislocation revisions. When adjusted by head size, age, and approach, there were again no differences between the bearing surfaces.
Discussion
Dislocation after THA constitutes a prominent reason for revision surgery [5, 20, 21]. Early dislocation is frequently associated with patient and mechanical factors, whereas late dislocation can be associated with biological factors [7, 11]. Although multiple studies have focused on risk factors for late dislocation, bearing surfaces have not been extensively scrutinized and outcomes are controversial [12]. A recent clinical trial showed that CoC bearing couples decrease the cumulative risk of late dislocation as compared with CoP [9]. The Australian Orthopaedic Association National Joint Replacement Registry reported a higher rate of revision for dislocation in CoC THAs than in MoP THAs in some subgroups of patients [20]. Alumina ceramic is a histologically inert biomaterial, and the limited articular wear debris generated in THA stimulates a fibrocytic reaction that can increase the stability of the joint pseudocapsule [4, 14, 18]. In this study, we asked whether articular bearings are associated with an increased or decreased likelihood of late dislocation. In this cohort of 73,386 THAs analyzed over a period of 13 years, only 470 THAs (0.65%) required revision for late dislocation. After adjusting for age, femoral head size, and surgical approach, bearing surface had little association with late dislocation risk; CoP showed the highest rates of revision. CoC and MoM did not show any difference compared with MoP. On the other hand, younger patients (< 65 years) and smaller head size (≤ 28 mm) showed high rates of revision with CoC. A similar finding is reported by the Australian Registry [20].
The retrospective nature of this study carries inherent limitations. Our data are based on the clinical practice of a relatively small group of orthopaedic surgeons. The group included 211 surgeons with an average number of 37 THAs/surgeon carried out in 2013 [21]. During the 13-year observation period, an increasing number of THAs was carried out in New Zealand using crosslinked PE. In this study, we did not stratify the analysis according to PE quality. Most CoC THAs had a femoral head diameter of ≥ 28 mm (6228 [91%]). No ceramic heads with diameter of less than 28 mm were used, and the large majority of all ceramic components (Biolox Forte and Delta ceramic) were from one single manufacturer (Ceramtec, Plochingen, Germany). Our analysis did not include separate analysis of 32-mm and more than 32-mm heads. The Finnish registry [12] compared revision rates for THA dislocation versus femoral head size. There was a 40% reduction of revision with 32-mm compared with 28-mm head diameter. However, increasing the head size to 36 mm did not show any difference. Other possible factors involved in risk of dislocation such as body mass index, activity status, and comorbidities were only recently included in the registry database and were not analyzed in this study. It is prudent to keep in mind the timeframe of data collection, because the design of bearing surfaces change over time, in particular the PE cup liner. In this study, liners with high offset, a lipped design, and a semiconstrained design were not stratified for analysis. Analysis of bilateral THAs as independent observations is a potential statistical flaw of the study. However, less than 4% of all THAs was carried out under the same anesthetics and therefore possibly using the same implant [21]; the majority of bilateral THAs carried out at different time points had different bearing surfaces (different age of the patient and time of surgery, different surgeons and hospitals, and different indications). For this reason, we feel that including bilateral THAs as independent endpoints in this study was permissible. Another potential limitation of this study is related to the controversy on the definition of early and late dislocation with cutoffs ranging from 3 months, 1 year, 2 years, and 5 years [10, 17]. However, most first-time dislocations occur within 1 year after primary THAs [2]. In our study, 366 of 836 (44%) primary THAs were revised for dislocation within the first postoperative year. Risk factors for dislocation are thought to differ between early and late events with patient and mechanical factors playing a larger role in early dislocation and biological factors affecting late dislocation [7, 11]. We elected to define late as dislocation requiring revision occurring 1 year after the index surgery. Thus, we possibly included in the analysis hips with instability related to reasons such as implant malposition rather than to instability secondary to inflammatory changes with joint capsule dissociation.
We incorrectly expected a reduced revision rate for late dislocation in CoC THAs assuming that the local biological response to ceramic debris produces a healthy joint pseudocapsule with increased mechanical strength. Our hypothesis was based on a number of observations: (1) the periarticular fibrous tissue reaction to ceramics originally described by Boutin et al. [4] differs from the inflammatory reaction to metal and PE [22]; (2) alumina ceramic is one of the most histologically inert biomaterials, and the limited articular wear debris generated in THA stimulates a fibrocytic reaction around the prosthesis [14, 16]; (3) MoP pseudocapsules exhibited higher levels of inflammatory markers than their CoC counterparts [18]; (4) analysis of excised pseudocapsules in CoC THAs showed small numbers of macrophages, few foreign body-type giant cells, and occasional lymphocytes, whereas PE components promoted extensive foreign body-type inflammatory changes [8, 19]; and (5) in a bilateral primary THA study, Hernigou et al. [9] used CoC couples on one side and CoP couples on the contralateral side, always with 32-mm femoral heads. The cumulative number of dislocations (126 patients, 252 hips) at a minimum of 27 years in CoP hips was higher (n = 31) compared with CoC hips (n = 4). Late dislocation was defined as greater than 2 years postoperatively; 28 occurred in the CoP hips and none occurred in the CoC cohort of hips. The authors also found increased capsular thickness in CoC hips when compared with CoP hips.
Despite these findings, this study showed no advantage of using CoC in regard to reduction of risk of revision for late dislocation and showed that CoP had the poorest results in this context.
Sexton et al. [20] from the Australian registry analyzed 110,239 primary THAs with a total of 862 (0.78%) revisions for dislocation. The baseline characteristics, including indication for surgery, gender, and age distribution, were similar to our study. However, the study covered a shorter period of time, and the surgical approach was not considered for multivariate analysis. In the New Zealand Registry, the posterior approach shows a higher THA revision rate when compared with the direct-lateral approach [21]. In the Australian Registry paper, CoC bearing surfaces had a lower risk of requiring revision resulting from dislocation than did MoP and CoP surfaces with a followup of up to 7 years. However, in the group of CoC THAs with the head diameter of 28 mm and age < 65 years and with the head diameter of > 28 mm and age > 65 years, there was a higher rate of revision for dislocation than with other bearing combinations. In the present study, we also found high rates of revision for late dislocation in younger patients (< 65 years) with 28-mm head diameter and CoC bearings. The limited length of head options, the lack of liners with eccentric offset, and the small bearing diameter are possible factors associated with this finding observed in both registries.
In conclusion, this large registry study demonstrated that bearing surfaces had little association with the incidence of revision for late dislocation. The biologic response to ceramic particles in the joint space with increased capsular thickness and fibrosis and the related assumption of reduced risk for revision after late dislocation remain a controversial topic. In our opinion, with the current knowledge, there is no reason to conclude that CoP is an inferior or superior bearing surface. Future studies with longer followup should continue to investigate this query.
Acknowledgments
We thank Professor Chris Frampton, University of Otago, Christichurch, New Zealand, for the statistical analysis, and Tony Hobbs, New Zealand arthroplasty Registry, Christichurch, New Zealand, for providing the database of this study. We also thank all New Zealand orthopaedic surgeons that are participating to the Hip Arthroplasty Registry.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
This work was performed at the University of Auckland, Auckland, New Zealand.
References
- 1.Bader R, Steinhauser E, Zimmermann S, Mittelmeier W, Scholz R, Busch R. Differences between the wear couples metal-on-polyethylene and ceramic-on-ceramic in the stability against dislocation of total hip replacement. J Mater Sci Mater Med. 2004;15:711–718. doi: 10.1023/B:JMSM.0000030214.79180.13. [DOI] [PubMed] [Google Scholar]
- 2.Berry DJ, von Knoch M, Scheck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 3.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87:762–769. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 4.Boutin P, Christel P, Dorlot J, Meunier A, de Roquancourt A, Blanquaert D, Herman S, Sedel L, Witvoet J. The use of dense alumina-alumina ceramic combination in total hip replacement. J Biomed Mater Res. 1988;22:1203–1232. doi: 10.1002/jbm.820221210. [DOI] [PubMed] [Google Scholar]
- 5.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:130–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 6.Colwell CW, Jr, Hozack WJ, Mesko JW, D’Antonio JA, Bierbaum BE, Capello WN, Jaffe WL, Mai KT. Ceramic-on-ceramic total hip arthroplasty early dislocation rate. Clin Orthop Relat Res. 2007;465:155–158. doi: 10.1097/BLO.0b013e31815072e4. [DOI] [PubMed] [Google Scholar]
- 7.Daly PJ, Morrey BF, Minnesota R. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74:1334–1343. [PubMed] [Google Scholar]
- 8.Esposito C, Maclean F, Campbell P, Walter WL, Walter WK, Bonar SF. Periprosthetic tissues from third generation alumina-on-alumina total hip arthroplasties. J Arthroplasty. 2013;28:860–866. doi: 10.1016/j.arth.2012.10.021. [DOI] [PubMed] [Google Scholar]
- 9.Hernigou P, Homma Y, Pidet O, Guissou I, Hernigou J. Ceramic-on-ceramic bearing decreases the cumulative long-term risk of dislocation. Clin Orthop Relat Res. 2013;471:3875–3882. doi: 10.1007/s11999-013-2857-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Itokawa T, Nakashima Y, Yamamoto T, Motomura G, Ohishi M, Hamai S, Akiyama M, Hirata M, Hara D, Iwamoto Y. Late dislocation is associated with recurrence after total hip arthroplasty. Int Orthop. 2013;37:1457–1463. doi: 10.1007/s00264-013-1921-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knoch MV, Berry DJ, Harmsen WS, Morrey BF. Late dislocation after total hip arthroplasty. J Bone Joint Surg Am. 2002;84:1949–1953. doi: 10.2106/00004623-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Kostensalo I, Junnila M, Virolainen P, Remes V, Matilainen M, Vahlberg T, Pulkkinen P, Eskelinen A, Makela KT. Effect of femoral head size on risk of revision for dislocation after total hip arthroplasty: a population-based analysis of 42,379 primary procedures from the Finnish Arthroplasty Register. Acta Orthop. 2013;84:342–347. doi: 10.3109/17453674.2013.810518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kung PL, Ries MD. Effect of femoral headsize and abductors on dislocation after revision THA. Clin Orthop Relat Res. 2007;465:170–174. doi: 10.1097/BLO.0b013e318159a983. [DOI] [PubMed] [Google Scholar]
- 14.Lerouge S, Huk O, Yahia LH, Witvoet J, Sedel L. Ceramic-ceramic and metal-polyethylene total hip replacements: comparison of pseudomembranes after loosening. J Bone Joint Surg Br. 1997;79:135–139. doi: 10.1302/0301-620X.79B1.6621. [DOI] [PubMed] [Google Scholar]
- 15.Murphy SB, Ecker TM, Tannast M. Two- to 9-year clinical results of alumina ceramic-on-ceramic THA. Clin Orthop Relat Res. 2006;453:97–102. doi: 10.1097/01.blo.0000246532.59876.73. [DOI] [PubMed] [Google Scholar]
- 16.Prudhommeaux F, Hamadouche M, Nevelos J, Doyle C, Meunier A, Sedel L. Wear of alumina-on-alumina total hip arthroplasties at a mean 11-year followup. Clin Orthop Relat Res. 2000;379:113–122. doi: 10.1097/00003086-200010000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Pulido L, Restrepo C, Parvizi J. Late instability following total hip arthroplasty. Clin Med Res. 2007;5:139–142. doi: 10.3121/cmr.2007.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sedel L, Simeon J, Meunier A, Villette J, Launay S. Prostaglandin E2 level in tissue surrounding aseptic failed total hips. Arch Orthop Trauma Surg. 1992;111:255–258. doi: 10.1007/BF00571519. [DOI] [PubMed] [Google Scholar]
- 19.Sedel L, Walter WL, Pitto RP. Ceramic-on-ceramic THA: do the advantages outweigh the limitations? Clin Orthop Relat Res. 2014;472:2927–2931. doi: 10.1007/s11999-014-3665-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sexton SA, Walter WL, Jackson MP, De Steiger R, Stanford T. Ceramic-on-ceramic bearing surface and risk of revision due to dislocation after primary total hip replacement. J Bone Joint Surg Br. 2009;91:1448–1453. doi: 10.1302/0301-620X.91B11.22100. [DOI] [PubMed] [Google Scholar]
- 21.The New Zealand Joint Registry: fifteen year report: January 1999 to December 2013. Available at: http://www.nzoa.org.nz/nz-joint-registry. Accessed June 2015.
- 22.Willert HG, Bertram H, Buchhorn GH. Osteolysis in alloarthroplasty of the hip: the role of ultra-high molecular weight polyethylene wear particles. Clin Orthop Relat Res. 1990;258:95–107. [PubMed] [Google Scholar]