Abstract
Background
Modern ceramic-on-ceramic bearings have become attractive alternatives to conventional polyethylene in total hip arthroplasty (THA) as a result of their low wear and minimal particle production. However, 28-mm heads in ceramic-on-ceramic bearing couples have been associated with ceramic fracture. To address these issues, 32-mm and larger ceramic heads with a titanium-alloy sleeve have been introduced, although limited data are available on their durability and clinical outcomes.
Questions/purposes
We determined (1) the survivorship of the primary ceramic-on-ceramic THA using a 32-mm ceramic head with a titanium-alloy sleeve at a minimum followup of 5 years; (2) Harris hip scores; (3) the incidence of ceramic fracture and noisy hip; and (4) the proportion of hips showing radiographic evidence of osteolysis.
Methods
From November 2005 to August 2009, we performed 301 ceramic-on-ceramic THAs using a 32-mm ceramic head with a titanium-alloy sleeve in 270 patients. Of these, 12 patients (12 hips [4%]) died from problems unrelated to surgery and 13 patients (15 hips [5%]) were lost during followup before a minimum of 5 years had been reached, leaving 245 patients who had 274 THAs with a minimum followup of 5 years (mean, 6.5 years; range, 5–9 years) in this retrospective analysis. During the study period, 30% (301 of 997 hips) were performed with this articulation based on the operating surgeon’s discretion. The mean patient age at the time of surgery was 55 years (range, 16–82 years). All operations were performed at a single center. All of the ceramic implants were hot isostatic-pressed, laser-marked, proof-tested third-generation alumina. We determined the implant survival, Harris hip scores, incidence of ceramic fracture or noisy hips (based on a questionnaire), and presence of osteolysis.
Results
The survival rate of ceramic-on-ceramic bearings in primary THA using a 32-mm ceramic head with a titanium-alloy sleeve was 98% (95% confidence interval, 96%–100%) at 9 years. The Harris hip score improved from a mean of 47 points preoperatively to 93 points at last followup. One ceramic head fractured at 6 years postoperatively. No ceramic liners fractured. Audible hip clicking and squeaking were identified in four hips and one hip, respectively. Osteolysis was detected in three hips, but none had symptoms.
Conclusions
Primary ceramic-on-ceramic THA using a 32-mm ceramic head with a titanium-alloy sleeve has a survivorship of 98% at 9-year followup. Nevertheless, surgeons should be aware of the potential risks of ceramic fracture, noise, and osteolysis associated with the use of a ceramic head with a titanium-alloy sleeve.
Level of Evidence
Level IV, therapeutic study.
Introduction
Conventional polyethylene is associated with wear-induced osteolysis and/or loosening at long-term followup in THA [17]. Thus, two principal approaches have been advocated: improving the polyethylene or using a hard-on-hard bearing [19]. In addition to reducing the prospect of polyethylene wear, hard-on-hard bearings provide options for larger femoral head sizes, to increase the head-neck ratio and the ROM before which impingement occurs, effectively reducing dislocation rates [5, 20]. However, metal-on-metal bearings with large femoral heads have been associated with unacceptably high rates of revision and potentially extensive soft tissue damage, leading to serious disability [1, 6]. Thus, ceramic-on-ceramic bearings have become popular [29].
Modern ceramic-on-ceramic bearings have low wear and minimal particle production, and as a result have become attractive alternatives that are commonly recommended for young and active patients [13, 35]. However, the frequency of ceramic head fracture associated with one design of a short-neck modular alumina femoral head was 1.4% [14], and until recently, the most commonly used size for a ceramic head was 28 mm, and 28-mm heads might be at the risk of dislocation and femoral head fracture [2, 4, 14, 28]. Nonuniform contact between the ceramic head and the metal taper increases the risk of a ceramic head fracture [14], and the presence of small debris between the ceramic head and the metal taper results in a reduction in the load to fracture [34]. In addition, several case studies have shown that the implantation of a ceramic head on a damaged taper may result in premature fracture of the ceramic head [14, 23, 25]. Because unexpected or undetected damage on the taper or the presence of any contaminant between the metal taper and ceramic head during primary THA increases the risk of a ceramic head fracture [34], an absolutely clean interface is of primary importance. A ceramic head with a titanium-alloy sleeve was introduced to solve such issues by minimizing the alteration in the interface between the ceramic head and the metal taper. The application of the titanium-alloy sleeve in a primary ceramic-on-ceramic THA has the advantages of protecting the taper from unexpected damage or contamination and, hence, reduces the risk of a ceramic head fracture. To our knowledge, no other studies to date have reported on the application of a ceramic head with a titanium-alloy sleeve for primary THA.
We therefore sought to determine (1) the survivorship of the primary ceramic-on-ceramic THA using a 32-mm ceramic head with a titanium-alloy sleeve at a minimum followup of 5 years; (2) Harris hip scores; (3) the incidence of ceramic fracture and noisy hip; and (4) the proportion of hips showing radiographic evidence of osteolysis.
Materials and Methods
From November 2005 to August 2009, we performed 997 cementless THAs in 891 patients. During the study period, we used third-generation alumina ceramic-on-ceramic bearings in all hips. Of these, 30% (301 of 997 THAs) were performed with a 32-mm ceramic head with a titanium-alloy sleeve combined with a proximal modular stem in 270 patients. The other 696 THAs were performed with a 28-mm or 32-mm ceramic head with no titanium-alloy sleeve combined with either a proximal modular stem or grit-blasted tapered wedge stem in 621 patients. The decision for use of a 32-mm ceramic head with a titanium-alloy sleeve was at the operating surgeon’s discretion. There were no general indications for selecting the bearing surface during the study period. Of the 270 patients (301 hips) managed with a 32-mm ceramic head with a titanium-alloy sleeve, 12 patients (12 hips [4%]) died from problems unrelated to surgery and 13 patients (15 hips [5%]) were lost during followup before a minimum of 5 years had been reached, and none of the 12 patients who died or of the 13 lost patients had undergone revision or reoperation before the last followup. The remaining 245 patients (274 hips) constituted the study cohort. There were 160 men and 85 women. The mean age at the time of the index surgery was 55 years (range, 16–82 years), and the mean body mass index was 25 kg/m2 (range, 15–36 kg/m2). The mean followup was 6.5 years (range, 5–9 years). The most common diagnosis was primary coxarthrosis or coxarthrosis after hip dysplasia (46%) (Table 1). Institutional review board approval was obtained for this study.
Table 1.
Initial diagnoses
| Initial diagnosis leading to THA | Number of hips (N = 274) |
|---|---|
| Primary coxarthrosis or coxarthrosis after hip dysplasia | 125 |
| Osteonecrosis of the femoral head | 105 |
| Femoral neck fracture | 13 |
| Sequelae of Legg-Calvé-Perthes | 10 |
| Ankylosing spondylitis | 7 |
| Sequelae of infection | 7 |
| Multiple epiphyseal dysplasia | 4 |
| Miscellaneous conditions | 3 |
All of the index arthroplasties were performed at one institution by one of two high-volume hip arthroplasty surgeons (Y-SP, Y-WM) through an anterolateral approach. For all patients, the THA involved a 32-mm ceramic head (BIOLOX® forte; CeramTec AG, Plochingen, Germany) with a titanium-alloy sleeve that was preassembled at the factory. As a result, no contaminant was found on the contact surface between the ceramic head and the metal sleeve (Fig. 1). The acetabular components were the Duraloc® option cup (DePuy/J&J, Warsaw, IN, USA; n = 263) and Plasmacup® SC (Aesculap AG & Co, Tuttlingen, Germany; n = 11). The femoral components were the S-ROM® stem (DePuy/J&J) in all hips.
Fig. 1.

Photograph of a 32-mm ceramic head (BIOLOX® forte; CeramTec AG, Plochingen, Germany) with a titanium-alloy sleeve designed to fit the Morse taper of an S-ROM stem (DePuy/J&J, Warsaw, IN, USA).
Clinical and radiological evaluation was performed preoperatively, at 6 weeks, 3 months, 6 months, and 1 year postoperatively and annually thereafter. The clinical outcomes were assessed using Harris hip scores [7] during each visit, and a Harris hip score of ≥ 90 points was considered to be an excellent outcome; 80 to 89 points was a good outcome; 70 to 79 points was a fair outcome; and < 70 points was a poor outcome. Each patient completed a questionnaire that included the items regarding any noise had occurred since the time of the operation and if so, whether the noise was a squeaking, clicking, or any other noises as well as the frequency and reproducibility of the noise, activities associated with the noise, awareness of the noise by other people, any pain associated with the noise, and effect of the noise on the quality of life. The radiological evaluations consisted of an AP and crosstable lateral radiographs. These radiographs were reviewed at the final followup by two independent observers (S-JL, S-PJ) with respect to the stability of the acetabular and the femoral components and the presence of the osteolysis. Cup loosening was defined as the presence of a radiolucent line around the entire circumference, a change in the inclination of the angle of at least 5°, or a migration of at least 2 mm [9]. Stem loosening was defined as a complete radiolucent line, a progressive axial subsidence of > 3 mm, or a shift in the varus or valgus [3]. Osteolysis was defined as a periprosthetic cystic or scalloped lesion with a diameter exceeding 2 mm that had not been present on the immediate postoperative radiographs [11].
A survivorship analysis was performed by using a Kaplan-Meier estimator with an endpoint of revision for any reason, and patients who were lost to followup were regarded as censored cases. The statistical analysis was performed using IBM SPSS Statistics Version 22.0 (IBM Corp, Somers, NY, USA).
Results
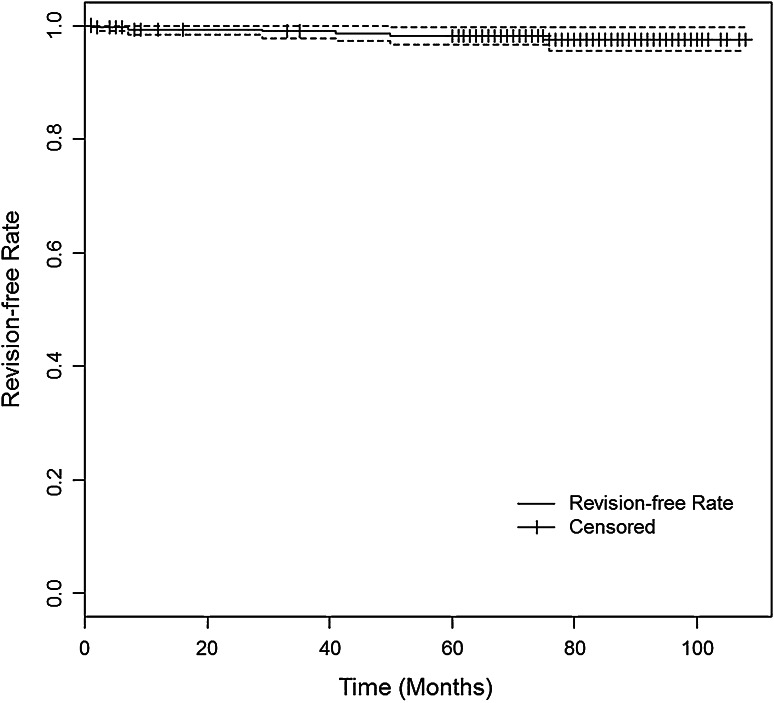
The Kaplan-Meier survivorship for ceramic-on-ceramic bearings in primary THA using a 32-mm ceramic head with a titanium-alloy sleeve, with an endpoint of revision for any reason, was 98% (95% confidence interval [CI], 96%–100%) at 9 years (Fig. 2).
Fig. 2.
The Kaplan-Meier survival curve with a revision for any reason as an endpoint is shown. The dotted lines indicate the 95% CI.
The mean Harris hip score improved from 47 points (range, 17–77 points) preoperatively to 93 points (range, 45–100 points) at the time of the final followup. The outcome was categorized as good to excellent in 97% of the hips, fair in five hips, and poor in four hips. Of the nine hips in the fair or poor category, three hips had a deep infection, two hips had a femoral stem loosening, one hip had a peroneal nerve palsy, one hip had a ceramic head fracture, and the other two had been diagnosed as having iliopsoas tendonitis by ultrasonography.
One patient (0.4%) sustained a fracture of the ceramic femoral head 6 years postoperatively, without any obvious trauma history, and the fracture involved a 32-mm diameter +0 component used on an S-ROM stem (DePuy/J&J) with a Plasmacup SC (Aesculap AG & Co). During revision, the metal taper was protected by the titanium-alloy sleeve that had been inserted during the primary THA. No ceramic liner fracture was seen during followup.
The incidence of an audible hip noise at the last followup was identified in five (1.8%) of the 274 hips. One of the patients produced a squeaking sound when rising from a sitting or squatting position and the other four produced an intermittent clicking sound while walking. The hip noise was not associated with any pain or any modification in the daily activities of any patient. Furthermore, no patient could reproduce the noise and required revision.
Periprosthetic osteolysis was detected in three hips (1.1%), but none of these hips showed pain or any signs of inflammation, and the erythrocyte sedimentation rate and the C-reactive protein values were within normal limits (Fig. 3). All acetabular components showed radiographic evidence of osseointegration at the last followup. Two (0.7%) of 274 hips showed radiographic signs of loosening of the femoral stem, and both had a 9-mm small-diameter stem. The revision surgery took place at 29 and 45 months, respectively, and these stems were observed to have fibrous ingrowth.
Fig. 3.
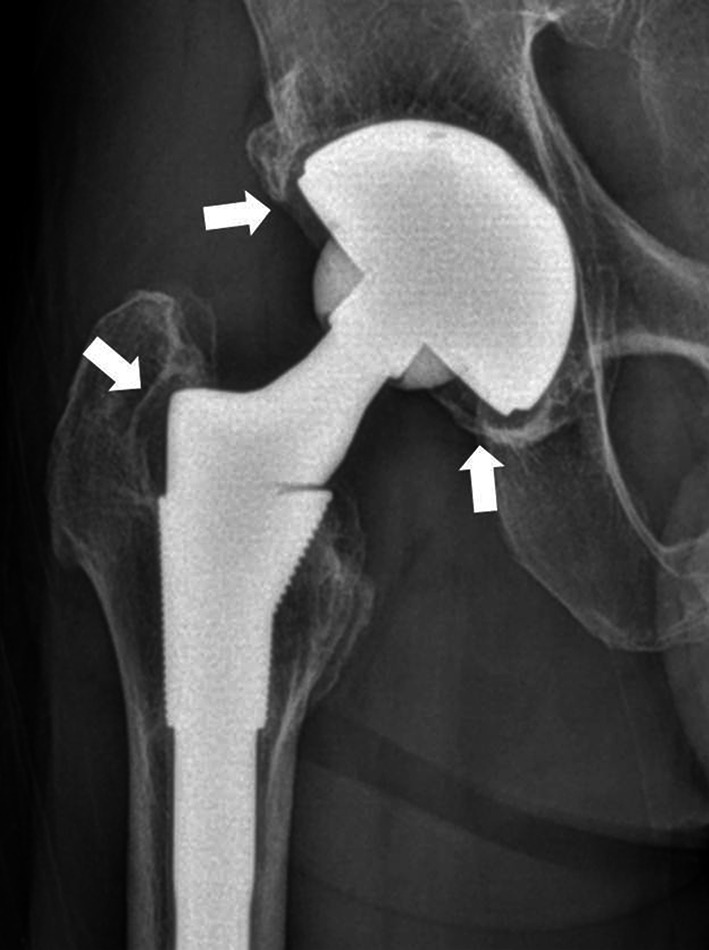
AP radiograph of the right hip showing osteolytic lesions about the acetabular cup and the greater trochanter 6 years after the index operation. Arrows indicate osteolytic lesions.
Discussion
The ceramic head with a titanium-alloy sleeve offers a modular solution for a damaged taper in revision hip surgery, and a few studies have discussed the outcomes of revision THA using this system [8, 10, 12, 32]. However, this system also can be used in primary THA, and it may reduce the risk of a ceramic head fracture by minimizing the alterations in the interface between the metal taper and the ceramic head. We therefore determined (1) the survival rate of the primary ceramic-on-ceramic THA using a 32-mm ceramic head with a titanium-alloy sleeve at a minimum followup of 5 years; (2) Harris hip scores; (3) the incidence of ceramic fracture and noisy hip; and (4) the proportion of hips showing radiographic evidence of osteolysis.
Our study has several limitations. First, this study is limited by its retrospective nature and by the lack of a control group. During the study period, only 30% of patients received a 32-mm ceramic head with a titanium-alloy sleeve and implant selection was primarily at the operating surgeon’s discretion. There were no general indications for selecting the bearing surface during the study period and the rationale for choice of implant could not be ascertained from this retrospective review. Therefore, there is the potential for selection bias and it is impossible to draw conclusions regarding the outcomes of this design compared with another design in a similar group of patients. However, this is the first large series reporting on the results of application of a 32-mm ceramic head with titanium-alloy sleeve in primary THA. Second, the length of followup was not uniform for all patients. However, all patients with implants had a minimum of 5 years followup and the mean followup was 6.5 years. This length of followup allowed us to determine the medium-term outcomes in this population. Third, we evaluated periprosthetic osteolysis on plain radiographs. CT scans would be more sensitive to detect the presence and extent of osteolysis [26], but it was not used in this study. Fourth, data have been obtained from 32-mm third-generation ceramic heads with titanium-alloy sleeves. Although the incidence of a ceramic head fracture is very low (0.4%) in our series, a larger (36 mm or greater) ceramic head with a metal sleeve made of a fourth-generation ceramic is currently available on the market. Lastly, we studied only one design of femoral stem combined with a 32-mm sleeved ceramic head and therefore cannot generalize our findings to all third-generation alumina ceramic-on-ceramic hip prostheses.
We determined the survivorship for ceramic-on-ceramic bearings in primary THA using a 32-mm ceramic head with a titanium-alloy sleeve was 97.5% at 9 years. Several reports have discussed using a ceramic head with a titanium-alloy sleeve in revision hip arthroplasty [8, 10, 12, 32]. Jack et al. [10] reported on the isolated acetabular revision of 165 hips that were followed for a mean of 5 years with a 97% survival rate for acetabular components at 8 years. Kim et al. [12] also reported on an isolated acetabular revision of 53 hips followed for a mean of 6 years with a 94% survival rate for acetabular components (Table 2).
Table 2.
Results of reports of ceramic-on-ceramic THA using a ceramic head with a titanium-alloy sleeve
| Study | Type of arthroplasty | Number of hips | Type of ceramics | Head size (mm) | Mean age (years) | Mean followup (years) | Audible hip noise (%) | Ceramic fracture (%) | Osteolysis (%) | Dislocation (%) | Survival rate |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Thorey et al. [32] | Revision THA | 91 | BIOLOX delta | 28, 32, 36, 40, 44* | 64.1 | 2.1 | 0 | 0 | 0 | 1 (1.1) | NR |
| Helwig et al. [8] | Isolated acetabular revision | 47 | BIOLOX delta | NR | 61.0 | 2.2 | NR | 0 | 0 | NR | NR |
| Jack et al. [10] | Isolated acetabular revision | 165 | Alumina 100 and BIOLOX delta 65 | 28(4):32(131):36 (30) | 65.5 | 4.8 | NR | 2 head fracture in alumina (1.2) | 0 | 4 (2.4) | 96.6% for acetabular component at 8.3 years |
| Kim et al. [12] | Isolated acetabular revision | 53 | BIOLOX forte | 32 (all) | 49.9 | 5.7 | 2 squeakings and 5 clickings (13) | 0 | 0 | 0 | 94.3% for acetabular component |
| Current study | Primary THA | 274 | BIOLOX forte | 32 (all) | 55.1 | 6.5 | 1 squeaking and 4 clickings (1.8) | 1 head fracture (0.4) | 3 (1.1) | 2 (0.7) | 97.5% at 9 years |
* Exact number of hips is not reported; NR = not reported.
We found that the mean Harris hip score was 93 points at a mean followup of 6.5 years. Our results were comparable to those in other reports of THA using 32-mm third-generation alumina ceramic-on-ceramic bearings [18, 21, 30, 31]. The mean Harris hip score has ranged from 89 to 97 points at a mean followup of 8.1 years (range, 6.2–12.9 years) (Table 3).
Table 3.
Clinical results of reports of 32-mm alumina ceramic-on-ceramic THA
| Study | Number of hips | Head size (number of hips) | Type of fixation | Mean age (years) | Mean followup (years) | Harris hip score (points) |
|---|---|---|---|---|---|---|
| Lusty et al. [21] | 301 | 32-mm (278), 28-mm (23) | Cementless | 58 | 6.5 | 95 |
| Solarino et al. [30] | 35 | 32-mm (all) | Hybrid | 66 | 6.7 | 97 |
| Solarino et al. [31] | 68 | 32-mm (all) | Hybrid | 50 | 12.9 | 91 |
| Lee et al. [18] | 60 | 32-mm (all) | Cementless | 50 | 6.2 | 89 |
| Current study | 274 | 32-mm (all) | Cementless | 55 | 6.5 | 93 |
In our series of ceramic-on-ceramic primary THA with a 32-mm ceramic head with a titanium-alloy sleeve, one (0.4%) ceramic head was fractured. Jack et al. [10] reported a 1.2% fracture rate, both in a 32-mm alumina ceramic head with a metal sleeve, after isolated acetabular revision. The rates of ceramic head fracture for 28-mm alumina-on-alumina ceramic bearings of up to 1.4% have been reported in primary THA [14]. We found that alumina ceramic head fracture occurs even after the use of a 32-mm ceramic head with a titanium-alloy sleeve. Although a very low incidence of ceramic head fracture was observed, our findings suggest that patients should be informed of this problem when considering a THA using a 32-mm ceramic head with a titanium-alloy sleeve. Another concern regarding the use of ceramic bearings is that noise (squeaking or clicking) can occur. The incidence of squeaking ranged from 0% to 18% in various studies [27, 33, 35]. We identified five hips (1.8%) with noise after the use of a 32-mm ceramic head. Four of these produced an intermittent clicking noise and one produced squeaking. None was associated with any pain or any modification in daily activities, and none required revision surgery.
One major concern of using a ceramic head with a titanium-alloy sleeve is the formation of a metal-to-metal interface between the sleeve and the taper. Several reports have documented high revision rates as a result of corrosion at the cone/taper interface after large-diameter metal-on-metal THAs [15, 16, 22]. In our series, periprosthetic osteolysis was detected in 1.1% (three of 274 hips), but none of these hips showed any pain or any signs of infection. Although we did not record the levels of metal ions or revise the hips with osteolysis, a recent in vitro study has demonstrated that a large ceramic head with a metal sleeve does not have an effect on the corrosion between the metal sleeve and the metal taper [24]. It is currently unclear whether there is fretting corrosion and trunnion wear in a sleeved ceramic head in vivo.
To the best of our knowledge, our study may be the first to report on the clinical outcomes of using a 32-mm ceramic head with a titanium-alloy sleeve for a primary ceramic-on-ceramic THA. We found a survival rate of 97.5% at 9 years, and our observations support the continued use of a 32-mm ceramic head with a titanium-alloy sleeve in primary THA. However, ceramic head fractures may still occur, although with a very low incidence rate. Long-term observation is also required for periprosthetic osteolysis whether it comes from corrosion/fretting between the taper and sleeve. Additional understanding could be gleaned from retrieval analysis of failed cases with osteolysis. Our findings also suggest that surgeons should be aware of the potential risks of ceramic fracture, noise, and osteolysis that are associated with the use of a ceramic head with a titanium-alloy sleeve. Further followup is required before a definite judgment can be made regarding the long-term outcomes.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bozic KJ, Browne J, Dangles CJ, Manner PA, Yates AJ, Jr, Weber KL, Boyer KM, Zemaitis P, Woznica A, Turkelson CM, Wies JL. Modern metal-on-metal hip implants. J Am Acad Orthop Surg. 2012;20:402–406. doi: 10.5435/JAAOS-20-06-402. [DOI] [PubMed] [Google Scholar]
- 2.Callaway GH, Flynn W, Ranawat CS, Sculco TP. Fracture of the femoral head after ceramic-on-polyethylene total hip arthroplasty. J Arthroplasty. 1995;10:855–859. doi: 10.1016/S0883-5403(05)80087-7. [DOI] [PubMed] [Google Scholar]
- 3.Campbell AC, Rorabeck CH, Bourne RB, Chess D, Nott L. Thigh pain after cementless hip arthroplasty. Annoyance or ill omen. J Bone Joint Surg Br. 1992;74:63–66. doi: 10.1302/0301-620X.74B1.1732268. [DOI] [PubMed] [Google Scholar]
- 4.D’Antonio J, Capello W, Manley M, Bierbaum B. New experience with alumina-on-alumina ceramic bearings for total hip arthroplasty. J Arthroplasty. 2002;17:390–397. doi: 10.1054/arth.2002.32183. [DOI] [PubMed] [Google Scholar]
- 5.Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, Della Valle CJ, Gross AE. The Frank Stinchfield Award: Dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res. 2012;470:351–356. doi: 10.1007/s11999-011-2146-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graves SE, Rothwell A, Tucker K, Jacobs JJ, Sedrakyan A. A multinational assessment of metal-on-metal bearings in hip replacement. J Bone Joint Surg Am. 2011;93(Suppl 3):43–47. doi: 10.2106/JBJS.K.01220. [DOI] [PubMed] [Google Scholar]
- 7.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An endresult study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–55. [PubMed] [Google Scholar]
- 8.Helwig P, Konstantinidis L, Hirschmüller A, Bernstein A, Hauschild O, Südkamp NP, Ochs BG. Modular sleeves with ceramic heads in isolated acetabular cup revision in younger patients-laboratory and experimental analysis of suitability and clinical outcomes. Int Orthop. 2013;37:15–19. doi: 10.1007/s00264-012-1735-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hodgkinson JP, Shelley P, Wroblewski BM. The correlation between the roentgenographic appearance and operative findings at the bone-cement junction of the socket in Charnley low friction arthroplasties. Clin Orthop Relat Res. 1988;228:105–109. [PubMed] [Google Scholar]
- 10.Jack CM, Molloy DO, Walter WL, Zicat BA, Walter WK. The use of ceramic-on-ceramic bearings in isolated revision of the acetabular component. Bone Joint J. 2013;95:333–338. doi: 10.1302/0301-620X.95B3.30084. [DOI] [PubMed] [Google Scholar]
- 11.Joshi RP, Eftekhar NS, McMahon DJ, Nercessian OA. Osteolysis after Charnley primary low-friction arthroplasty: a comparison of twomatched paired groups. J Bone Joint Surg Br. 1998;80:585–590. doi: 10.1302/0301-620X.80B4.7361. [DOI] [PubMed] [Google Scholar]
- 12.Kim Y, Kim YH, Hwang KT, Choi IY. Isolated acetabular revision with ceramic-on-ceramic bearings using a ceramic head with a metal sleeve. J Arthroplasty. 2014;29:2420–2423. doi: 10.1016/j.arth.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 13.Kim YH, Choi Y, Kim JS. Cementless total hip arthroplasty with ceramic-on-ceramic bearing in patients younger than 45 years with femoral-head osteonecrosis. Int Orthop. 2010;34:1123–1127. doi: 10.1007/s00264-009-0878-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koo KH, Ha YC, Jung WH, Kim SR, Yoo JJ, Kim HJ. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008;90:329–336. doi: 10.2106/JBJS.F.01489. [DOI] [PubMed] [Google Scholar]
- 15.Kwon YM, Fehring TK, Lombardi AV, Barnes CL, Cabanela ME, Jacobs JJ. Risk stratification algorithm for management of patients with dual modular taper total hip arthroplasty: consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons and the Hip Society. J Arthroplasty. 2014;29:2060–2064. doi: 10.1016/j.arth.2014.07.029. [DOI] [PubMed] [Google Scholar]
- 16.Langton DJ, Sidaginamale R, Lord JK, Nargol AVF, Joyce TJ. Taper junction failure in large-diameter metal-on-metal bearings. Bone Joint Res. 2012;1:56–63. doi: 10.1302/2046-3758.14.2000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 18.Lee YK, Ha YC, Koo KH. Comparison between 28 mm and 32 mm ceramic-on-ceramic bearings in total hip replacement. Bone Joint J. 2014;96:1459–1463. doi: 10.1302/0301-620X.96B11.34358. [DOI] [PubMed] [Google Scholar]
- 19.Lehil MS, Bozic KJ. Trends in total hip arthroplasty implant utilization in the United States. J Arthroplasty. 2014;29:1915–1918. doi: 10.1016/j.arth.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 20.Lombardi. AV Jr, Skeels MD, Berend KR, Adams JB, Franchi OJ. Do large heads enhance stability and restore native anatomy in primary total hip arthroplasty? Clin Orthop Relat Res. 2011;469:1547–1553. [DOI] [PMC free article] [PubMed]
- 21.Lusty PJ, Tai CC, Sew-Hoy RP, Walter WL, Walter WK, Zicat BA. Third-generation alumina-on-alumina ceramic bearings in cementless total hip arthroplasty. J Bone Joint Surg Am. 2007;89:2676–2683. doi: 10.2106/JBJS.F.01466. [DOI] [PubMed] [Google Scholar]
- 22.Meyer H, Mueller T, Goldau G, Chamaon K, Ruetschi M, Lohmann CH. Corrosion at the cone/taper interface leads to failure of large-diameter metal-on-metal total hip arthroplasties. Clin Orthop Relat Res. 2012;470:3101–3108. doi: 10.1007/s11999-012-2502-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park MS, Yoon SJ, Yoo MJ. Repeated ceramic head fracture after ceramic-on-ceramic total hip arthroplasty. J Korean Hip Soc. 2012;24:59–64. doi: 10.5371/jkhs.2012.24.1.59. [DOI] [Google Scholar]
- 24.Preuss RHK, Flohr M, Streicher RM. Fretting corrosion and trunnion wear-is it also a problem for sleeved ceramic heads? Semin Arthroplasty. 2012;23:251–257. doi: 10.1053/j.sart.2013.01.008. [DOI] [Google Scholar]
- 25.Pulliam IT, Trousdale RT. Fracture of a ceramic femoral head after a revision operation: a case report. J Bone Joint Surg Am. 1997;79:118–121. doi: 10.2106/00004623-199701000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Puri L, Wixson RL, Stern SH, Kohli J, Hendrix RW, Stulberg SD. Use of helical computed tomography for the assessment of acetabular osteolysis after total hip arthroplasty. J Bone Joint Surg Am. 2002;84:609–614. doi: 10.2106/00004623-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 27.Restrepo C, Matar WY, Parvizi J, Rothman RH, Hozack WJ. Natural history of squeaking after total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2340–345. doi: 10.1007/s11999-009-1223-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schroder D, Bornstein L, Bostrom MP, Nestor BJ, Padgett DE, Westrich GH. Ceramic-on-ceramic total hip arthroplasty: incidence of instability and noise. Clin Orthop Relat Res. 2011;469:437–442. doi: 10.1007/s11999-010-1574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sedrakyan A, Graves S, Bordini B, Pons M, Havelin L, Mehle S, Paxton E, Barber T, Cafri G. Comparative effectiveness of ceramic-on-ceramic implants in stemmed hip replacement: a multinational study of six national and regional registries. J Bone Joint Surg Am. 2014;96(Suppl 1):34–41. doi: 10.2106/JBJS.N.00465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Solarino G, Piazzolla A, Mori CM, Moretti L, Patella S, Notarnicola A. Alumina-on-alumina total hip replacement for femoral neck fracture in healthy patients. BMC Musculoskelet Disord. 2011;12:32. doi: 10.1186/1471-2474-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Solarino G, Piazzolla A, Notarnicola A, Moretti L, Tafuri S, De Giorgi S, Moretti B. Long-term results of 32-mm alumina-on-alumina THA for avascular necrosis of the femoral head. J Orthop Traumatol. 2012;13:21–27. doi: 10.1007/s10195-011-0174-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thorey F, Sakdinakiattikoon M, Thiengwittayaporn S, Windhagen H. Early results of revision hip arthroplasty using a ceramic revision ball head. Semin Arthroplasty. 2011;22:284–289. doi: 10.1053/j.sart.2011.09.008. [DOI] [Google Scholar]
- 33.Walter WL, Yeung E, Esposito C. A review of squeaking hips. J Am Acad Orthop Surg. 2010;18:319–326. doi: 10.5435/00124635-201006000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Weisse B, Affolter C, Stutz A, Terrasi GP, Köbel S, Weber W. Influence of contaminants in the stem-ball interface on the static fracture load of ceramic hip joint ball heads. Proc Inst Mech Eng H. 2008;222:829–835. doi: 10.1243/09544119JEIM374. [DOI] [PubMed] [Google Scholar]
- 35.Yoon HJ, Yoo JJ, Yoon KS, Koo KH, Kim HJ. Alumina-on-alumina THA performed in patients younger than 30 years: a 10-year minimum followup study. Clin Orthop Relat Res. 2012;470:3530–3536. doi: 10.1007/s11999-012-2493-2. [DOI] [PMC free article] [PubMed] [Google Scholar]