Abstract
Objective
To characterize exposure histories and respiratory disease among surface coal miners identified with progressive massive fibrosis from a 2010 to 2011 pneumoconiosis survey.
Methods
Job history, tenure, and radiograph interpretations were verified. Previous radiographs were reviewed when available. Telephone follow-up sought additional work and medical history information.
Results
Among eight miners who worked as drill operators or blasters for most of their tenure (median, 35.5 years), two reported poor dust control practices, working in visible dust clouds as recently as 2012. Chest radiographs progressed to progressive massive fibrosis in as few as 11 years. One miner’s lung biopsy demonstrated fibrosis and interstitial accumulation of macrophages containing abundant silica, aluminum silicate, and titanium dust particles.
Conclusions
Overexposure to respirable silica resulted in progressive massive fibrosis among current surface coal miners with no underground mining tenure. Inadequate dust control during drilling/blasting is likely an important etiologic factor.
Inhalation of respirable coal mine dust causes coal workers’ pneumoconiosis—a chronic, irreversible occupational lung disease. Progressive massive fibrosis (PMF) is a debilitating, advanced form of pneumoconiosis. The Federal Coal Mine Health and Safety Act of 1969 (Coal Act) established the federal permissible exposure limit (PEL) of 2.0 mg/m3 for respirable coal mine dust in underground and surface coal mines and mandated regular inspections of surface and underground mines, in an effort to prevent coal workers’ pneumoconiosis. Under the Coal Act, the Mine Safety and Health Administration (MSHA) required a reduced dust limit if the silica content in a dust sample exceeds 5%, effectively establishing a respirable silica PEL of 100 μg/m3. MSHA conducts periodic inspections at coal mines to assess compliance with these PELs. In 2014, MSHA issued a new rule1 reducing the PEL for coal mine dust to 1.5 mg/m3.
The Coal Act also established a health surveillance system, administered by the National Institute for Occupational Safety and Health (NIOSH), designed to detect pneumoconiosis among working underground coal miners by offering periodic chest radiographs. Miners are not charged for participation in this voluntary program. Under Part 90 of the Coal Act, miners with evidence of pneumoconiosis are offered the opportunity to transfer to a less dusty occupation at the mine (if one exists).
In 2012, there were more than 50,000 surface coal miners in the United States—44.3% of the coal mining workforce. Nevertheless, the benefits of pneumoconiosis surveillance under the Coal Act were not extended to surface miners until 2014. Consequently, surface miners did not generally have access to free periodic chest radiographs, and much less is known about the prevalence of dust-related lung disease in this group.
Surface coal mining has generally been considered less dusty than underground mining; however, highwall drills at surface mining operations can generate large quantities of respirable dust containing significant levels of crystalline silica. Working as a surface driller is a recognized risk factor for pneumoconiosis.2–6 Drill operators and workers in the vicinity of the drill may experience exposure to hazardous dust levels. Table 1 summarizes results from dust sampling conducted by MSHA inspectors for drill operators and the blasting crew at surface coal mines.7 Many of the samples exceeded the MSHA PEL, and most were above the NIOSH-recommended exposure limit (50 μg/m3).
TABLE 1.
Percentage of MSHA Inspector Samples Collected From 1995 to 2012 With Excessive Silica7
| Highwall Drill Operator
|
Blaster/Shooter/Shotfirer
|
||||
|---|---|---|---|---|---|
| >100 μg/m3,* | >50 μg/m3,† | >100 μg/m3,* | >50 μg/m3,† | ||
| n | % | % | n | % | % |
| 2250 | 33.7 | 68.4 | 372 | 19.1 | 68.8 |
MSHA permissible exposure limit.
NIOSH recommended exposure limit.
Infrequent surveys conducted during the past 40 years have documented pneumoconiosis among US surface miners, generally at lower prevalence and less severity when compared with underground miners during the same periods.3–5,8 In 2010 to 2011, the mobile examination unit from the NIOSH Enhanced Coal Workers’ Health Surveillance Program (ECWHSP) traveled to 16 states with active surface coal mines and offered surface miners a free chest radiograph.9 Pneumoconiosis was found among 2.0% of the 2328 screened miners with at least 1 year of mining tenure. Twelve miners had radiographic changes consistent with PMF. Nine of these 12 miners reported no underground mining tenure.9 The objective of this study was to further characterize the work and medical histories of these miners who worked exclusively at surface mines and developed advanced pneumoconiosis.
METHODS
Potential cases of PMF from surface coal mine work were identified during the 2010 to 2011 ECWHSP survey. Chest radiographs were interpreted using the standardized International Labour Office classification system10 as previously described.9 A determination of PMF was made when at least two B Readers identified the presence of large opacities (≥1 cm) consistent with pneumoconiosis (category A, B, or C).10 Cases were excluded if the miner reported prior underground mining tenure.
Age, mining tenure, job history, and radiograph interpretations reported during the 2010 to 2011 survey were reviewed. Prior radiographs on file with the NIOSH were reviewed, if available. Potential sources of prior radiographs include the National Study of Coal Workers’ Pneumoconiosis (1969 to 1988)11 (survey of underground miners, however, surface miners were not discouraged from participating), and MSHA’s Miners’ Choice Program (1999 to 2002)8 (survey of underground and surface miners). Smoking status was not collected during the ECWHSP survey. Initial contact with miners was attempted by telephone. If a miner could not be reached, a follow-up letter was sent. If the miner was deceased, the next-of-kin was interviewed. Informed consent was obtained before all interviews. The study was approved by the NIOSH institutional review board (HSRB 12-DRDS-07XP).
Telephone interviews sought to confirm the miner’s occupational history, including mining tenure, work practices, other occupational exposures, respiratory health, and smoking status. Investigators requested the release of relevant medical records, including prior chest radiographs. One miner’s lung biopsy was reevaluated by an expert lung pathologist (JLA). One miner had been diagnosed with sarcoidosis, not a form of pneumoconiosis, and was excluded from the follow-up.
RESULTS
For Miners 1 to 5, data were limited to results from the ECWHSP field survey and prior radiographs (Miners 2 and 3). Telephone interviews were completed by Miners 6, 8, and 9, and Miner 7’s next-of-kin. Medical records were reviewed for Miners 7 and 8. During the telephone interview, Miner 9 reported a previous physician diagnosis of sarcoidosis. He had worked as a supervisor at a surface mine for 30 years, but reported no other relevant occupational dust exposure. Although silicosis can be clinically similar to sarcoidosis, we were unable to review the medical findings, and thus omitted Miner 9 as a PMF case.
The remaining eight cases were non-Hispanic, white males with a median age of 56 years. The mean surface mining tenure was 32.9 years (median, 35.5 years; range, 10 to 40 years). All miners’ radiographs demonstrated category A or B PMF; the background small opacity profusion category ranged from 1/0 to 2/3.
Case Studies
Miners 1 to 5
Miners 1 to 5 worked for a majority of their careers as drillers or driller/blasters (Table 2). Miner 2 had a chest radiograph at the age of 31 years (30 years before his ECWHSP radiograph), which did not show evidence of pneumoconiosis. Miner 3 had a radiograph at the age of 47 years (10 years before his ECWHSP radiograph), which showed small opacity profusion category 2/1 but no large opacities, documenting progression to PMF over the course of 10 years. Miners 1 to 4 could not be reached by telephone, but according to Social Security Administration records they were alive at the time of follow-up. Miner 5 confirmed his mining job history but declined to complete the telephone interview.
TABLE 2.
Summary of Case Information From Surface Coal Miners With Progressive Massive Fibrosis
| Miner | Age* | Total Years of Tenure | Months of Follow-Up† | Longest-Held Mining Job and Length
|
ECWHSP Survey Radiograph
|
Previous Radiograph
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Job | Years | Profusion | PMF Category | Remarks‡ | Age, yrs | Profusion | PMF Category | ||||
| 1 | 54 | 33 | 29 | Driller§ | 33 | 2/2 | A | 2 | – | – | – |
| 2 | 61 | 36 | 31 | Driller | 33 | 1/0 | B | 2 | 31 | 0/0 | No PMF |
| 3 | 57 | 37 | 29 | Driller/blaster | 37 | 2/2 | B | 1, 3 | 47 | 2/1 | No PMF |
| 4 | 55 | 35 | 29 | Driller | 34 | 2/3 | A | 1 | – | – | – |
| 5 | 53 | 34 | 19 | Driller | 23 | 2/1 | A | 1 | – | – | – |
| 6 | 53 | 10 | 26 | Blaster | 9 | 1/1 | A | 2, 3 | – | – | – |
| 7 | 60 | 40 | 11¶ | Driller | 40 | 1/1 | A | 2 | 27 | 0/0 | No PMF |
| 8 | 57 | 38 | 28 | Driller | 38 | 2/1 | A | 1 | 46 | 0/0 | No PMF |
Age of the miner on the day of ECWHSP radiograph.
Number of months from the day of ECWHSP radiograph to the most recent vital status confirmation.
Remarks: 1= ECWHSP radiograph showed bilateral large opacities typical of PMF; 2 = ECWHSP radiograph showed a unilateral large opacity; 3 = ECWHSP radiograph showed evidence of emphysema.
Miner 1 reported working 33 years in surface coal mine drilling but did not provide a complete job history.
Miner 7 was deceased at the time of our follow-up.
ECWHSP; Enhanced Coal Workers’ Health Surveillance Program; PMF, progressive massive fibrosis.
Miner 6
Miner 6 reported 9 years of work as a contract blaster at surface coal mines, and 1 year as a haul truck operator, driller, and maintenance worker for a coal company before his survey chest radiograph showing PMF. As a contract blaster, he reported many days on which he worked for several hours in dust clouds generated by drilling rigs. He asserted that the contract employer did not provide either a respiratory protection program or training about dust hazards, and he did not recall any personal dust sampling. In contrast, during the 1 year he worked as a mining company employee, Miner 6 described regular use of dust collectors and air-conditioned cabs, and he perceived lower dust exposure compared with his years of contract work. The mining company had also performed dust measurements to assess compliance with regulations. Miner 6 did report exposure to intermittent dust clouds during the use of compressed air on equipment maintenance and blowing dust out of filters.
Before surface mining, Miner 6 had worked for 21 years in fiberglass production, with exposure to resin and formaldehyde, but he denied exposures to processes that would be expected to generate significant respirable dust. Radiographic abnormalities (but not PMF) have been associated with work in fiberglass manufacturing.12
Miner 6 reported progressive exertional dyspnea, but denied other respiratory symptoms such as chronic cough or phlegm. He had smoked approximately one pack of cigarettes per day for 32 years. We were not able to review Miner 6’s medical records.
Miner 7
Miner 7 was 60 years old at the time of his radiograph and had worked as a surface coal drill operator for 40 years. He denied having any other dusty jobs. A chest radiograph at the age of 27 years showed no evidence of pneumoconiosis. Miner 7’s wife (next-of-kin) reported that the drills he operated early in his career did not have cabs, and his clothing was usually covered in dust. During the last few years of his tenure, he worked in air-conditioned cabs under less dusty conditions and dust exposures were periodically measured. He would not be required to operate the drill if the air conditioner in the drill cab was not operational.
The ECWHSP survey radiograph for Miner 7 was classified as PMF category A and was also suspicious for cancer of the lung or pleura. He had smoked cigarettes throughout his adult life. A transbronchial lung biopsy was obtained from the left upper lobe, near the lesion classified as PMF. The tissue was labeled benign in the contemporaneous medical records. Nevertheless, Miner 7 was subsequently diagnosed with adenocarcinoma in the right lung. Although the left lung lesion remained radiographically stable, the miner died of metastatic cancer 11 months after his participation in the ECWHSP.
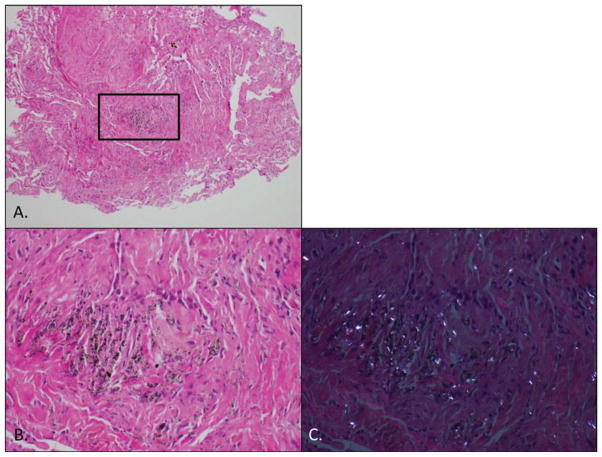
NIOSH obtained the tissue blocks and slides of the left upper lobe lung biopsy. The tissue included bronchial wall, mucosa, and some adjacent lung parenchyma. Further specialized histopathologic analysis revealed the interstitial accumulation of macrophages, containing a mixture of opaque and birefringent dust associated with some fibrosis (Fig. 1). With polarized light imaging, the particles were predominantly strongly birefringent, consistent with silicates, as well as numerous weakly birefringent particles consistent with silica (Fig. 1C).
FIGURE 1.
(A) A small biopsy taken near the PMF lesion is visualized under light microscopy (H&E stain). The black box indicates the region viewed at higher power in images B and C. (B) Image viewed using bright-field light microscopy. (C) The same image viewed using polarized light imaging, where silica (weakly birefringent) and silicates (strongly birefringent) refract the polarized light and show up brighter than the surrounding lung tissue and other materials. Also, it shows fibrosis (collagen is very weakly birefringent). This same tissue is shown in Figure 2. H&E, hematoxylin and eosin; PMF, progressive massive fibrosis.
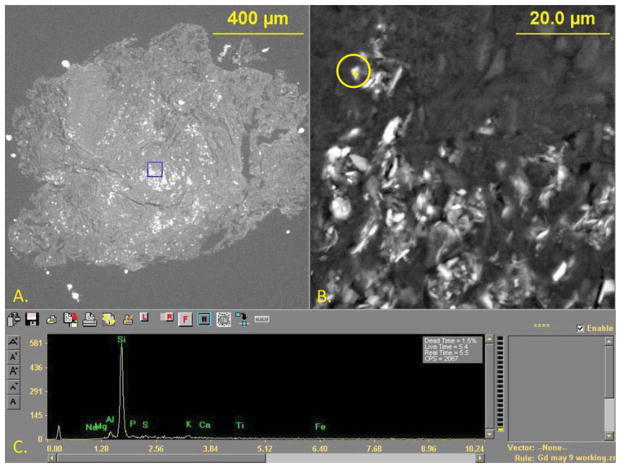
Scanning electron microscopy with energy dispersive x-ray spectroscopy was used to characterize the inorganic particles in situ in the macrophages within the tissue paraffin block, avoiding further destruction of the tissue sample.13 Figure 2 shows a region of the tissue that was analyzed with an example of the results from one particle. Of the 335 particles from two pieces of the parenchymal tissue analyzed, 12.2% were silica, 82.4% aluminum silicates, and 4.5% titanium dioxide. No other types of particles were found with any frequency. No evidence of malignancy was seen. Classical macules of coal workers’ pneumoconiosis, silicotic nodules, or tissue consistent with PMF were not captured by the biopsy. According to Miner 7’s wife, an autopsy documented coal workers’ pneumoconiosis; however, we were unable to obtain the autopsy report or any preserved tissue.
FIGURE 2.
An example of a particle analyzed using SEM/EDS. (A) A small biopsy taken near the PMF lesion is visualized using SEM. This is the same portion of tissue visualized in Figure 1. The box indicates the region viewed at higher power in image B, showing hundreds of individual particles in macrophages. (B) Particle circled in yellow with a yellow cross-hair was individually analyzed to yield the EDS spectrum shown in image C. (C) The EDS spectrum peak indicating the analyzed particle is silica (showing only an elemental peak for silicon). EDS, energy dispersive x-ray spectroscopy; PMF, progressive massive fibrosis; SEM, scanning electron microscopy.
Miner 8
Miner 8 received a chest radiograph at the age of 46 years, which did not have evidence of pneumoconiosis (Fig. 3A). His ECWHSP radiograph (age of 57 years) was classified as small opacity profusion category 2/1, with category A PMF in a typical pattern of bilateral upper lung zone lesions (Fig. 3B). He worked his entire career as a drill operator at a variety of operations, including surface coal mines, road construction, and rock quarry operations. The road construction work would often be fulfilling more than one purpose (eg, road construction and surface coal removal on the same site).
FIGURE 3.
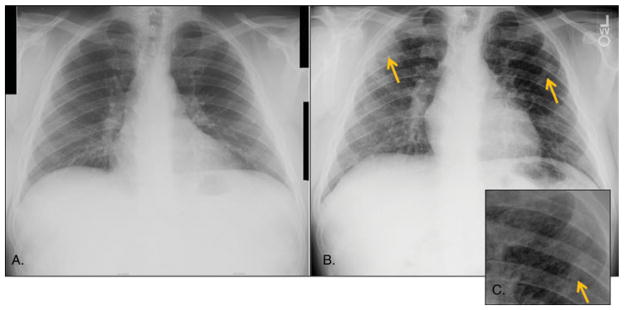
Miner 8’s chest radiographs. (A) A digitized copy of the radiograph that was taken at the age of 46 years and had no evidence of pneumoconiosis (small opacity profusion category 0/0 and no evidence of PMF). (B) Digital radiograph taken in NIOSH’s mobile surveillance unit 11 years later, at the age of 57 years, and was classified as small opacity profusion category 2/1 and PMF category A. Yellow arrows point to locations of PMF lesions. (C) Magnification of the indicated PMF lesion in the left lung. PMF, progressive massive fibrosis.
Miner 8 described variable but often very dusty working conditions. Many of the drills he operated did not have effective dust collectors. Frequently, drills did not have cabs; a drill designed for wet drilling (not equipped with a cab or dry dust collector) was regularly operated without water. On drills with cabs, the air-conditioning system was often in poor operating condition, and dust would recirculate inside the cab. On early model drills, it was frequently necessary to open cab doors to avoid the dust and extreme heat emitted by the drill machinery. At times, to avoid extreme heat or dust, he left the cab while drilling. To document his assertions, he provided photographs illustrating the working conditions he experienced at surface mines throughout his career. These showed workers exposed to clouds of dust at the drill site (Fig. 4 representative examples). Miner 8 reported that personal dust sampling was done a few times per year when federal mine inspectors were on the job site, but he denied existence of a respiratory protection program or of being informed of dust sampling results.
FIGURE 4.
Photographs taken at the worksite by Miner 8. (A) Taken in 1981 at a surface coal mine, it shows a dust cloud enveloping the operator’s cab on a surface drill. (B) Taken in 2010 at a surface coal mine, it shows a cloud of dust around an Ingersoll Rand 45 drill and a worker to the left of the haul truck. (C) Taken in 2012 at a surface coal mine, it shows three miners enveloped in a dust cloud loading drill holes to blast overburden.
At the age of 56 years, Miner 8 began having shortness of breath and cough with moderate physical activity. Previously, he had been physically active and without symptoms, and had never smoked. After receiving a report of PMF on his survey radiograph, he sought medical care. His lung function was found to be significantly reduced and exhibited a restrictive pattern: forced expiratory volume in 1 second was 75%, forced vital capacity was 69%, and total lung capacity was 62% of the predicted reference values. Cardiopulmonary exercise testing revealed a low partial pressure of oxygen (pO2) at peak exercise and no evidence of any cardiac limitation. His physician diagnosed him with severe silicosis with PMF and advised him to leave mining.
Could Lung Cancer Explain These Cases?
Because large opacities in miners may represent either PMF or lung cancer, we evaluated the background presence of small opacities, the location of the large lesions, and the follow-up time (time from ECWHSP survey to the most recent confirmation of vital status) among the eight surface miner cases. In all cases, the miners’ radiographs demonstrated a background of small opacities consistent with pneumoconiosis. Miners 3, 4, 5, and 8 had bilateral large opacities, a classic indicator of PMF, and all four remained alive after 19 to 29 months of follow-up. Miners 1, 2, and 6 had unilateral lesions, but these three also remained alive after at least 26 months. Although Miner 7 died of progressive adenocarcinoma 11 months after participating in the survey, a left lung biopsy showed dust-related changes but no malignancy, and his left lung lesion remained radiographically stable throughout his subsequent course. Taken together, the findings do not support lung cancer as an explanation for the radiographic abnormalities in these surface coal miners.
DISCUSSION
This contemporary case series describes eight US surface coal miners with radiographic findings of PMF—the most severe and lethal form of pneumoconiosis. Although the prevalence of pneumoconiosis among surface miners is generally assumed to be less than among underground coal miners,8,9 recent investigations have documented advanced forms of pneumoconiosis among surface miners who reported only surface coal mining tenure. Furthermore, two cases progressed quickly (<11 years) to PMF, similar to the rapidly progressive pneumoconiosis pattern than has been recently observed among underground coal miners in central Appalachia.13–15 All eight cases presented here worked a majority of their mining careers in drilling or blasting. When dust controls at surface mining operations are insufficient, blast hole drills can generate a substantial amount of respirable dust, exposing the drill operator, members of the blasting crew, and surrounding workers to hazardous conditions. Dust measurements at surface coal mines (Table 1) have continued to show excessive silica exposures in drilling and blasting operations.
Several of these miners reported little to no training on the hazards of dust. One miner described minimal attention to health hazards while he was working as a contract employee, but a more comprehensive approach after he began working directly for a mine operator. The miners indicated that working conditions had improved during their careers, but described a persistent tacit understanding to “get the job done” regardless of the working conditions.
Strengths of this study include vital status follow-up on all cases, the availability of prior radiographs in four cases and follow-up clinical histories in three cases, the photographic documentation of work conditions, and the unique analysis of lung histopathology and dust content in one case. A major limitation is the absence of confirmatory medical records, telephone interviews, or any further pathology tissue samples to review for five miners.
CONCLUSIONS
Even though all of the miners in this study worked their entire careers under the provisions of the 1969 Coal Act, study results show that severe forms of pneumoconiosis continue to occur in miners whose occupational exposure occurred exclusively through surface coal mining work. Supplemental information provided by some participants indicated that dust controls were often insufficient at their worksites. Given that surface coal miners make up a substantial portion (44%) of the coal mining workforce, the case series results and ongoing silica overexposures documented by MSHA sampling highlight the need to reduce respirable dust exposures at surface mining operations and demonstrate the need for including surface miners in routine respiratory health surveillance.
On April 23, 2014, the MSHA announced a new rule aimed at better protecting coal miners’ health. The new rule becomes effective on August 1, 2014, and implements multiple changes that will lead to reduced dust exposures for mine workers. Some of the key components impacting surface miners in this new rule include (1) determining noncompliance on the basis of a single full-shift sample collected by the MSHA, (2) requiring mine operators to take immediate corrective action when an overexposure occurs, (3) expanding compliance sampling requirements for mine operators, (4) allowing for the use of a Continuous Personal Dust Monitor (provides near real-time information on wearer dust exposures) for the collection of compliance samples, (5) extending medical surveillance and Part 90 transfer rights to surface miners, and (6) expanding medical surveillance by including pulmonary function testing and symptom assessment.1 Finally, on August 1, 2016, the rule reduces the federal PEL for respirable dust from 2.0 to 1.5 mg/m3. This rule is a significant step, especially for surface miners, in MSHA’s campaign to protect the health of all US coal miners and “End Black Lung.”16
Acknowledgments
The Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health and State University of New York (SUNY) Upstate Medical University supported the salaries of the authors, and no other funding was obtained. This work was performed as part of their work; no nongovernmental funding supported this work. The analytical electron microscope instrumentation at SUNY was partially supported by a grant from New York State Development’s Division of Science, Technology and Innovation.
The authors thank Travis Markle, Shanna Clark, and the Coal Workers’ Health Surveillance Program Team, as well as Drs Robert Cohen and Kristin Yeoman for helpful feedback during the preparation of the article.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention or the National Institute for Occupational Safety and Health.
The authors declare no conflicts of interest.
References
- 1.U.S. Department of Labor; Mine Safety and Health Administration (MSHA) [Accessed May 2014];Lowering Miners’ Exposure to Respirable Coal Mine Dust, Including Continuous Personal Dust Monitors. Available at https://s3.amazonaws.com/public-inspection.federalregister.gov/2014-09084.pdf.
- 2.Parker J, Lapp N, Banks D. Surface coal mine drillers and silicosis: the ten year West Virginia experience. Am Rev Respir Dis. 1989;139:A490. [Google Scholar]
- 3.Amandus HE, Hanke W, Kullman G, et al. A re-evaluation of radiological evidence from a study of US strip coal miners. Arch Environ Health. 1984;39:346–351. doi: 10.1080/00039896.1984.10545861. [DOI] [PubMed] [Google Scholar]
- 4.Amandus HE, Petersen MR, Richards TB. Health status of anthracite surface coal miners. Arch Environ Health. 1989;44:75–81. doi: 10.1080/00039896.1989.9934379. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Silicosis screening in surface coal miners—Pennsylvania, 1996–1997. MMWR Morb Mortal Wkly Rep. 2000;49:612–615. [PubMed] [Google Scholar]
- 6.Banks DE, Bauer MA, Castellan RM, et al. Silicosis in surface coalmine drillers. Thorax. 1983;38:275–278. doi: 10.1136/thx.38.4.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Department of Labor; Mine Safety and Health Administration (MSHA) Program Evaluation and Information Resources: MSHA Standardized Information System. Arlington, VA: Data downloaded August 19, 2013. [Google Scholar]
- 8.Centers for Disease Control and Prevention. Pneumoconiosis prevalence among working coal miners examined in federal chest radiograph surveillance programs—United States, 1996–2002. MMWR Morb Mortal Wkly Rep. 2003;52:336–340. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Pneumoconiosis and advanced occupational lung disease among surface coal miners—16 States, 2010–2011. MMWR Morb Mortal Wkly Rep. 2012;61:431–434. [PubMed] [Google Scholar]
- 10.International Labour Office. Guidelines for the Use of the ILO International Classification of Radiographs of Pneumoconioses. Geneva, Switzerland: International Labour Office; 2002. [Google Scholar]
- 11.Centers for Disease Control and Prevention. Pneumoconiosis in coal miners: NIOSH research and surveillance. MMWR CDC Surveill Summ. 1983;32:39SS–42SS. [PubMed] [Google Scholar]
- 12.Kilburn K, Warshaw R. Difficulties of attribution of effect in workers exposed to fiberglass and asbestos. Am J Ind Med. 1991;20:745–751. doi: 10.1002/ajim.4700200605. [DOI] [PubMed] [Google Scholar]
- 13.Wade WA, Petsonk EL, Young B, et al. Severe occupational pneumoconiosis among West Virginian coal miners: one hundred thirty-eight cases of progressive massive fibrosis compensated between 2000 and 2009. Chest. 2011;139:1458–1462. doi: 10.1378/chest.10-1326. [DOI] [PubMed] [Google Scholar]
- 14.Antao VC, Petsonk EL, Sokolow LZ, et al. Rapidly progressive coal workers’ pneumoconiosis in the United States: geographic clustering and other factors. Occup Environ Med. 2005;62:670–674. doi: 10.1136/oem.2004.019679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Petsonk EL, Rose C, Cohen R. Coal mine dust lung disease. New lessons from old exposure. Am J Respir Crit Care Med. 2013;187:1178–1185. doi: 10.1164/rccm.201301-0042CI. [DOI] [PubMed] [Google Scholar]
- 16.Mine Safety and Health Administration. MSHA End Black Lung Act Now. 2014. [Google Scholar]