Abstract
Open globe injury (OGI) is a severe form of eye trauma estimated at 2-3.8/100,000 in the United States. Most pediatric cases occur at home and are the result of sharp object penetration. The aim of this article is to review the epidemiology, diagnosis, management, and prognosis of this condition by conducting a systematic literature search with inclusion of all case series on pediatric OGI published between 1996 and 2015. Diagnosis of OGI is based on patient history and clinical examination supplemented with imaging, especially computed tomography when indicated. Few prospective studies exist for the management of OGI in pediatric patients, but adult recommendations are often followed with success. The main goals of surgical management are to repair the open globe and remove intraocular foreign bodies. Systemic antibiotics are recommended as medical prophylaxis against globe infection, or endophthalmitis. Other complications are similar to those seen in adults, with the added focus of amblyopia therapy in children. Severe vision decline is most likely due to traumatic cataracts. The ocular trauma score, a system devised to predict final visual acuity (VA) in adults, has proven to be of prognostic value in pediatric OGI as well. Factors indicating poor visual prognosis are young age, poor initial VA, posterior eye involvement, long wound length, globe rupture, lens involvement, vitreous hemorrhage, retinal detachment, and endophthalmitis. A thorough understanding of OGI and the key differences in epidemiology, diagnosis, management, and prognosis between adults and children is critical to timely prevention of posttraumatic vision loss early in life.
Keywords: Amblyopia, eye trauma, open globe, pediatric trauma, surgery, visual impairment
INTRODUCTION
Trauma to the eye is a leading cause of monocular blindness worldwide, especially in developing countries.[1,2] About 2.4 million eye injuries occur in the United States annually, of which 35% are in children.[3] Although 95% of all ocular injuries do not require admission,[4] open compared to closed globe injuries in children are generally more severe and associated with more complications and surgical procedures, longer hospitalization times, and poorer visual prognoses.[2,5,6,7,8,9,10,11] This review summarizes the demographics and injury characteristics of pediatric open globe injury (OGI) and suggests a plan for diagnosis, management, and predicting outcome in these patients.
METHODS
For this literature review, PubMed was searched for combinations of the clusters of keywords: pediatric, paediatric, children; eye, ocular; trauma, injury; open globe, globe rupture, laceration, intraocular foreign body (IOFB), penetrating, perforating. One keyword/phrase from each cluster was used, unless repeated. All English-language case series consisting of ≥5 patients published between January 1996 and January 2015 were included. Results are synthesized in Tables 1 and 2 and Supplementary Table 1.
Table 1.
Incidence of concurrent ocular conditions with OGI* in children
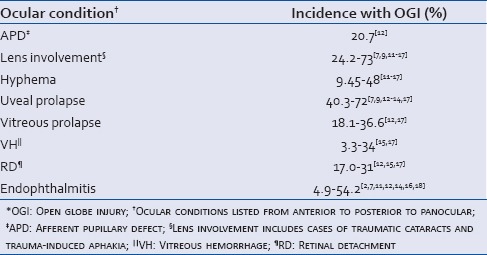
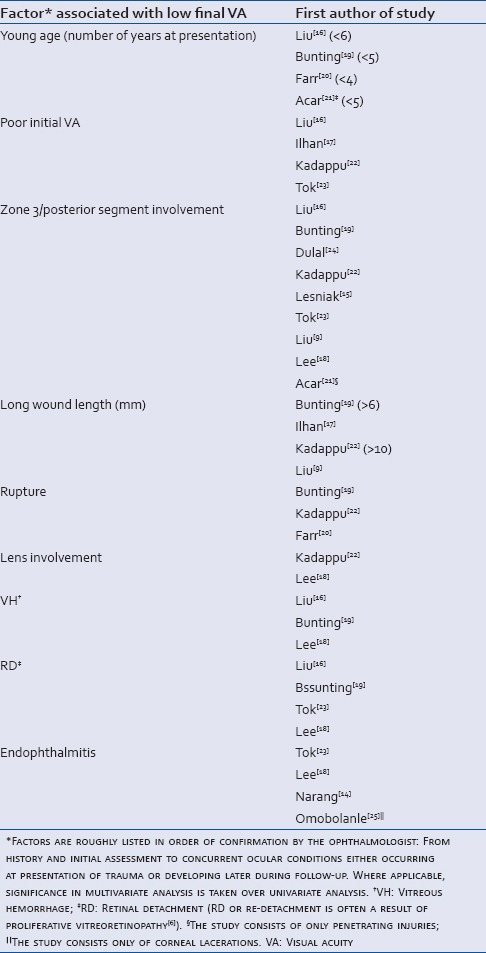
Table 2.
Factors significantly associated with a lower final VA from corroborating studies
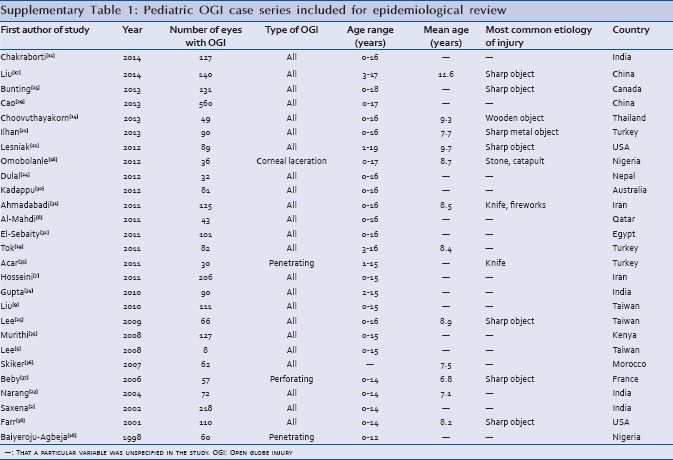
Supplementary Table 1.
Pediatric OGI case series included for epidemiological review
NOMENCLATURE
Following a standardized approach,[26,27] we define an OGI as a full-thickness mechanical injury to the cornea and/or sclera. The two types of OGI are ruptures and lacerations. Ruptures result from blunt trauma causing a full-thickness defect at the weakest point of the eye wall. Lacerations, the result of a sharp object entering the globe, are further classified as penetrating (only an entrance wound or same entrance/exit wound) or perforating (separate entrance and exit wounds) injuries. A separate category indicates the presence of an IOFB [Figure 1].
Figure 1.
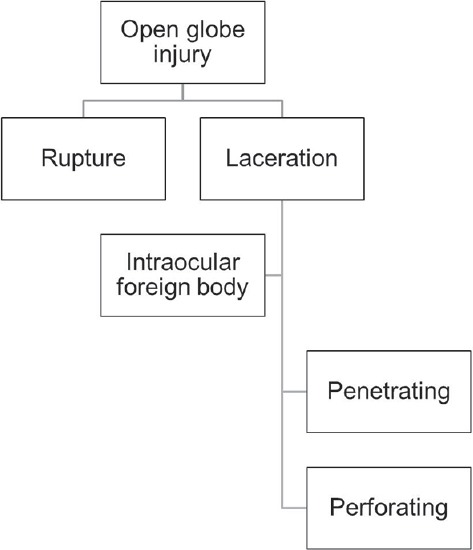
Open globe injury classification system.
OGI can also be categorized by zone of injury. Zone 1 includes the cornea and limbus. Zone 2 extends from the limbus to the anterior 5 mm of sclera, and Zone 3 extends posterior to Zone 2.[27,28]
DEMOGRAPHICS AND NATURE OF INJURY
As assessed by large-scale studies, the mean age for pediatric OGI during the last two decades ranges from 7.7 to 11.6 years [Supplementary Table 1].
The ratio of males to females presenting with OGIs ranges from 1.9:1 to 5.1:1,[10,13,14,15,16,17,18,19,22,23,25,30,31,36] though there is no significant difference across these studies in the incidence of right versus left eye affected. Pediatric OGI cases most frequently are caused by sharp objects such as knives[7,15,16,17,18,19,20,21,30,33,39] making penetrating injury the most common.[14,15,18,22,23] The majority of injuries occur at home.[7,16,17,24,29,30,38,40] In some developing countries, outdoor and street injuries are more common.[13,14] Other accidental causes of OGI in children have been documented,[41,42,43,44,45,46,47,48,49] as well as cases of abuse or assault.[15,50] Globally, fireworks during cultural celebrations are a common cause of pediatric OGI.[7,16,30,51,52]
Penetrating trauma is consistently the most common form of OGI in children at hospitals across the world, ranging from 48.4% to 83% of all OGIs, followed by rupture (9.9-34%) and IOFB presence (4.0-16.1%), with perforation being least common type of injury (1.2-4%).[2,7,9,11,13,14,15,16,17,18,20,22,23] Zone 1 injuries are also the most common form of OGI in pediatric patients (44-79%),[2,11,13,14,15,16,17,18,22,23] whereas Zone 3 injuries are associated with worse visual prognosis [Figure 2 and Table 2].
Figure 2.
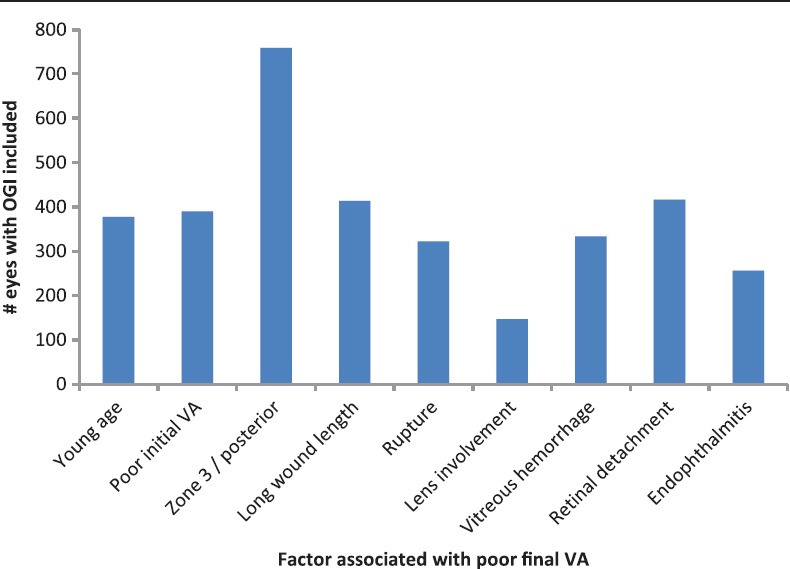
Number of eyes with open globe injury in confirmatory studies collated from Supplementary Table 1 showing significantly worse final visual acuity associated with certain factors. OGI: Open globe injury; VA: Visual acuity.
HISTORY AND EXAMINATION
Clinical examination
During initial assessment of any patient following ocular trauma, life-threatening conditions are first stabilized before evaluating the globe. Taking a complete history is crucial: IOFB is suspected with a history of the explosion, gunshot wound, or sharp object entering the eye, and appropriate imaging should be requested (see “Diagnostic imaging”).
Physicians must be opportunistic in assessing OGI in infants and children due to their limited ability to cooperate. If possible, obtain an initial visual acuity (VA), assess for an afferent pupillary defect (APD), delineate confrontational visual fields, and determine the degree of ocular motility for orbital injuries. The conjunctiva, cornea, sclera, anterior chamber, iris, angle, and lens are examined using a slit-lamp. In infants or uncooperative patients, an exam under anesthesia may need to be performed. One should have a high clinical suspicion for occult scleral laceration if the exam discloses hemorrhagic chemosis, intraocular pressure (IOP) <10 mmHg, abnormally deep/shallow anterior chamber, or peaked pupil. Rarely, occult OGI can present with nonspecific redness and irritation after a self-sealing corneal wound or if there is a small scleral perforation (e.g., induced by a dart).[32,34] If the diagnosis of OGI is obvious, IOP measurements and pupillary dilation should be avoided to decrease the risk of further extruding intraocular contents. Fundoscopy is performed without scleral depression.[35]
Other ocular signs commonly associated with pediatric OGI are hyphema, vitreous hemorrhage (VH), uveal/vitreous prolapse, cataract, lens subluxation, irido-dialysis, retinal detachment (RD), APD, or infection [endophthalmitis; Table 1].
Diagnostic imaging
OGI is generally diagnosed by history and clinical examination alone. Diagnostic imaging should be conducted to assess the presence of an IOFB if suspected[2,28,37,53,54,55] and to evaluate the extent of globe damage. The main imaging modalities used are computerized tomography (CT) and B-scan ultrasonography (US); rarely, X-ray, and magnetic resonance imaging (MRI) are used.
Computerized tomography
In one study, CT was 94.9% sensitive for IOFB detection.[56] It is highly sensitive for metallic IOFBs, and slightly less so but still more sensitive than MRI for glass. While metal and glass are hyperdense on CT, wooden fragments appear hypodense unless covered with lead-containing paint and can increase in radiodensity over days.[57] In pediatric patients, due to the possibility of motion artifact and the potentially harmful dose of radiation delivered to the lens during each CT scan,[58,59] ophthalmologists may use alternative methods such as US to confirm clinical suspicion of OGI.[60]
B-scan ultrasonography
B-scan is a rapid, cost-efficient method that can be useful in diagnosing OGIs, especially in assessing posterior segment integrity.[56] B-scan has been shown to have lower sensitivity in detecting IOFBs masked by intraocular air when compared to CT,[56,58] but one study of 427 B-scan reports showed 100% positive predictive value for diagnosis of RD and IOFB.[61] We recommend B-scan in compliant pediatric patients only when performed with extreme caution by an experienced technician or physician after primary globe closure to avoid further extrusion of intraocular contents.[60]
X-ray
Globe pathology may be detected incidentally on plain films. The speed, availability, and low cost of X-ray makes it valuable in detecting metallic IOFB or orbital fracture only in the absence of more advanced imaging modalities and when OGI cannot be clinically confirmed or ruled out.[62]
Magnetic resonance imaging
MRI is only used to detect nonmetallic IOFBs, especially when a wooden IOFB seen as an ambiguous hypodensity on CT can be mistaken for air.[60] It is critical to definitively rule out the presence of a metallic IOFB, as well as any other magnetic metal in or on the patient, before ordering an MRI. Ferromagnetic material (e.g., nickel, iron, cobalt) will be displaced by the magnets in the MRI whereas other metals (e.g., tantalum) will not.
TREATMENT
If OGI is suspected, a rigid eye shield, supported by the orbital bones and not the soft tissues of the globe, should be placed over the injured eye after clinical examination for protection. Antibiotics, analgesics, and possibly anti-emetics should then be administered. A tetanus shot should be given if there is incomplete or uncertain history of recent immunization. Limited activity is recommended until surgical repair.[62,63]
Broad-spectrum intravenous antibiotics with adequate ocular penetration are initiated as prophylaxis against endophthalmitis. Cefazolin, a first-generation cephalosporin, can be used as a first-line antibiotic. If IOFB is suspected, the patient should be admitted for a course of intravenous vancomycin and ceftazidime.[7,15,22,34,64,65]
Surgical management
The main goals of surgical OGI management are to emergently close primary wounds, reposition prolapsed ocular contents or debride if extruded for more than 24 h,[66] remove IOFBs, and treat or prevent complications with the ultimate goal of preserving VA.[28]
Primary globe repair is performed similarly as with cases of adult OGI.[67] The integrity of the cornea, limbus, and sclera should be maximally restored with intraoperative attention to reforming the anterior chamber and, if possible, avoiding distortion of the visual axis. Corneoscleral tissue grafts can be used for large open wounds that cannot be sutured closed.
During primary closure, anterior chamber IOFBs should be removed, and emergent pars plana vitrectomy (PPV) performed by a retina specialist in cases with confirmed posterior segment IOFB.[37,68,69] If a retina specialist is not available, emergent globe repair may be performed before transferring the patient emergently for retina surgery.
Intravitreal vancomycin (1 mg/0.1 cc) and ceftazidime (2.25 mg/0.1 cc) can be considered during IOFB removal,[65,70] but intracameral injections for endophthalmitis prophylaxis have not been tested in prospective trials in children. Decreased risk of endophthalmitis has only been shown in one prospective trial involving adult patients presenting with penetrating injuries and IOFBs who received prophylactic intravitreal injections of 40 μg of gentamicin sulfate and 45 μg of clindamycin, while risk was not decreased in patients on the regimen without an IOFB.[70,71]
COMPLICATIONS
Amblyopia
In children, amblyopia is a major concern after OGI due to the often lengthy period of visual rehabilitation and therapy. Depending on the extent of injury, visual potential may be poor and amblyopia will further negatively affect the visual prognosis. Prevention of amblyopia has been studied extensively, with patching of the uninjured eye as the gold standard of therapy, along with atropine if the uninjured eye is hyperopic.[18,34,72,73,74,75] The patient should be concurrently managed by a pediatric ophthalmologist following primary repair. Traumatic cataracts associated with corneal laceration are the most common cause for severe, refractory VA decline in children's eyes after OGI.[51,76]
Endophthalmitis
Endophthalmitis is a severe complication of OGIs and is associated with a significantly worse final VA,[14,18,23] necessitating proper prophylaxis, and aggressive management [Figure 2]. Compared with an incidence of 0.9-18.4% in adults, the incidence of posttraumatic endophthalmitis after OGI ranged from 4.9% to 54.2% in children [Table 2].[64,70,77,78,79,80,81,82,83,84,85] Trauma is one of the most common causes of endophthalmitis in this population.[86] Risk factors for traumatic endophthalmitis include presence of an IOFB, injury in a rural setting, wound contamination with organic matter,[80] primary wound closure delayed for longer than 24 h postinjury, and involvement of the lens capsule.[7,14,37,87]
The microbiological spectrum of posttraumatic endophthalmitis includes Gram-positive normal skin flora, e.g., Staphylococcus epidermis; as well as more virulent species, e.g., Bacillus sp. Streptococcus is the most commonly isolated organism in pediatric patients, versus Staphylococcus in adults.[65,88,89] Fungal infection can occur in association with organic matter, such as tree branch injury. Soil-contaminated injuries carry an increased risk of infection with Bacillus sp. and Clostridium sp., both of which are highly virulent organisms.
Retinal detachment
RD in the setting of an OGI in children is also associated with a worse visual prognosis, particularly if the injury involves Zone 3 [Figure 2 and Table 2].[90] Surgical management of RD in children after OGI has been shown to improve visual prognosis.[6,91] PPV followed by silicone oil infusion provides a relatively clear view for the patient without needing postoperative face-down positioning in contrast to gas tamponade,[92] thus minimizing noncompliance. However, silicone oil changes the refractive status of the eye, inducing hyperopia.
Vitreous hemorrhage
VH is commonly seen with posterior segment injuries. Vitrectomy can be delayed for 2-3 weeks in cases of VH without RD; however, if VH is visually significant, observation must be balanced with the risk of amblyopia.[69] PPV should be considered for VH within 7-14 days of OGI, particularly if Zone 2 or 3 is involved, to prevent tractional RD.[93]
Corneal opacities
Posttraumatic corneal opacities can be due to scarring or band keratopathy. These conditions should be managed aggressively with definitive surgical treatment, especially when the central visual axis is involved, to prevent amblyopia.[94]
Sympathetic ophthalmia
Sympathetic ophthalmia is a rare condition in which an autoimmune response causes granulomatous panuveitis in the uninjured sympathizing eye as well as in the injured eye. Its incidence after trauma has been reported to be rare (<1%) even in pediatric patients.[95] The standard initial treatment is high-dose systemic corticosteroids often followed by steroid-sparing agents, with immunosuppressant therapy for refractory cases. Advances in medical management have dramatically decreased the need for prophylactic secondary enucleation or evisceration;[28,96] should enucleation be needed or desired, e.g., for cosmetic reasons, it may be necessary to place a conformer to insure proper orbital bone growth.[97] Enucleation and conformer placement often are managed by an ophthalmic plastic surgeon and oculist.
Toxicity due to chronic intraocular foreign body
An IOFB can go undetected for many years after OGI. Metal IOFBs are typically the most toxic, so a high clinical suspicion for occult IOFB is needed in patients with a history of OGI and signs of IOFB toxicity as detailed below.[55] Definitive treatment for chronic IOFB toxicity is removal of the offending IOFB.
Copper IOFB toxicity is called chalcosis bulbi. An IOFB composed of more than 85% copper can produce an intense inflammatory response including hypopyon and may present as sterile fulminant endophthalmitis.[98] IOFBs with lower copper content can show green discoloration of Descemet's membrane, a red-brown cataract, and uveitis progressing to phthisis.[65] Iron IOFB toxicity, termed siderosis bulbi, can induce retinal degeneration with progressive vision loss[99] and retinal vascular change.[98] An early sign is mydriasis progressing to rapidly increasing IOP. Decreased B waves are seen on the electroretinogram.[100,101]
PROGNOSIS
The rate of successful treatment after pediatric OGI, defined as having a final VA of 20/40 or better, is between 54% and 56.5% in industrialized countries[9,19,22] with a less favorable prognosis in nonindustrialized countries (15.5-25.7%).[2,14,16,31] Table 2 and Figure 2 summarize the factors significantly associated with a low final VA in pediatric OGI patients in more than one case series. Common causes of persistently low final VA in children who sustained OGI are residual corneal opacity and amblyopia.[5]
Systems for prediction
Various scoring systems have been devised to predict final VA in ocular trauma. Kuhn et al.[102] developed the ocular trauma score (OTS) in 2002 from the large-scale eye injury registries of Hungary and the United States, with poor initial VA, rupture, endophthalmitis, perforation, RD, and APD listed as factors negatively affecting the score and thus final predicted VA.
To devise a prospectively validated system for VA prognosis in OGI, Schmidt et al.[103] proposed a classification and regression tree (CART) model in 2008 on 221 OGI patients to measure vision survival (light perception or better) versus no vision, and minimal to severe vision loss (20/400 or better) versus profound vision loss.
Most recently, a pediatric OTS (POTS) was formulated that de-emphasized VA in predicting visual prognosis due to the difficulty in ascertaining an accurate initial VA in the youngest patients, a point also raised by other investigators.[18,21] Acar et al.[21] provided an equation to determine the POTS in patients in whom initial VA was unable to be obtained, doubling the weight of age and zone of injury in the score calculation. It also eliminated APD from the list of associated ocular pathologies that would deduct raw points from the total score and, thus, predict a poorer prognosis. APD has been associated with false positives due to severe hyphema or severe VH.[66]
Studies have shown that the OTS is an accurate prognostic indicator for pediatric OGIs,[15,19,29,104] more so than either POTS[19,104] or CART.[105]
CONCLUSIONS
The pediatric population composes nearly 35% of all ocular trauma cases in the United States, despite a 17% decline in pediatric cases from 1990 to 2009 in the United States.[38] Boys sustain more OGIs than girls, and the most frequent mode of injury is penetration with sharp objects. OGIs occur more in children at home than anywhere else. Systems of classifying ocular trauma remain largely the same in pediatric as in adult patients, with Zone 1 being the most frequently affected region in pediatric OGI.
OGI diagnosis is clinical, with CT and US indicated to rule out IOFB and to visualize the posterior segment, respectively. Prophylactic antibiotics typically used include cefazolin or vancomycin plus ceftazidime in cases of IOFB. Emergent primary globe repair must be done to close the wound, remove IOFBs, and reposition prolapsed tissue. In addition to treating structural and infectious complications, management of pediatric OGI is focused on preventing amblyopia, because patient compliance with patching is generally low even at the expense of vision recovery. Traumatic cataracts secondary to corneal laceration are the most common cause for severe, refractory VA decline in children's eyes post-OGI. The number one organism isolated in pediatric OGI-associated endophthalmitis is Streptococcus.
Although devised for adults, the OTS has been shown to be an effective tool to gauge final VA after OGI in children as well. Factors indicating poor visual prognosis are young age, poor initial VA, posterior eye involvement, long wound length, globe rupture, lens involvement, VH, RD, and endophthalmitis.
Additional large-scale prospective studies are needed to improve evidence-based management of OGI for timely prevention of posttraumatic vision loss early in life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol. 1992;20:95–8. doi: 10.1111/j.1442-9071.1992.tb00718.x. [DOI] [PubMed] [Google Scholar]
- 2.Saxena R, Sinha R, Purohit A, Dada T, Vajpayee RB, Azad RV. Pattern of pediatric ocular trauma in India. Indian J Pediatr. 2002;69:863–7. doi: 10.1007/BF02723708. [DOI] [PubMed] [Google Scholar]
- 3.Prevent Blindness America. The Scope of the Eye Injury Problem. 2010. Available from: http://www.preventblindness.org/sites/default/files/national/documents/fact_sheets/FS93_ScopeEyeInjury.pdf .
- 4.May DR, Kuhn FP, Morris RE, Witherspoon CD, Danis RP, Matthews GP, et al. The epidemiology of serious eye injuries from the United States eye injury registry. Graefes Arch Clin Exp Ophthalmol. 2000;238:153–7. doi: 10.1007/pl00007884. [DOI] [PubMed] [Google Scholar]
- 5.Lee CH, Su WY, Lee L, Yang ML. Pediatric ocular trauma in Taiwan. Chang Gung Med J. 2008;31:59–65. [PubMed] [Google Scholar]
- 6.Sheard RM, Mireskandari K, Ezra E, Sullivan PM. Vitreoretinal surgery after childhood ocular trauma. Eye (Lond) 2007;21:793–8. doi: 10.1038/sj.eye.6702332. [DOI] [PubMed] [Google Scholar]
- 7.Hosseini H, Masoumpour M, Keshavarz-Fazl F, Razeghinejad MR, Salouti R, Nowroozzadeh MH. Clinical and epidemiologic characteristics of severe childhood ocular injuries in Southern Iran. Middle East Afr J Ophthalmol. 2011;18:136–40. doi: 10.4103/0974-9233.80702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Mahdi HS, Bener A, Hashim SP. Clinical pattern of pediatric ocular trauma in fast developing country. Int Emerg Nurs. 2011;19:186–91. doi: 10.1016/j.ienj.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 9.Liu ML, Chang YS, Tseng SH, Cheng HC, Huang FC, Shih MH, et al. Major pediatric ocular trauma in Taiwan. J Pediatr Ophthalmol Strabismus. 2010;47:88–95. doi: 10.3928/01913913-20100308-06. [DOI] [PubMed] [Google Scholar]
- 10.Abbott J, Shah P. The epidemiology and etiology of pediatric ocular trauma. Surv Ophthalmol. 2013;58:476–85. doi: 10.1016/j.survophthal.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Chakraborti C, Giri D, Choudhury KP, Mondal M, Datta J. Paediatric ocular trauma in a tertiary eye care center in Eastern India. Indian J Public Health. 2014;58:278–80. doi: 10.4103/0019-557X.146297. [DOI] [PubMed] [Google Scholar]
- 12.Altintas L, Altintas O, Yüksel N, Pirhan D, Ozkan B, Caglar Y. Pattern of open eye injuries in Northwest Turkey: A retrospective study. Ulus Travma Acil Cerrahi Derg. 2011;17:334–9. [PubMed] [Google Scholar]
- 13.Skiker H, Laghmari M, Boutimzine N, Ibrahimy W, Benharbit M, Ouazani B, et al. Open globe injuries in children: Retrospective study of 62 cases. Bull Soc Belge Ophtalmol. 2007;306:57–61. [PubMed] [Google Scholar]
- 14.Narang S, Gupta V, Simalandhi P, Gupta A, Raj S, Dogra MR. Paediatric open globe injuries. Visual outcome and risk factors for endophthalmitis. Indian J Ophthalmol. 2004;52:29–34. [PubMed] [Google Scholar]
- 15.Lesniak SP, Bauza A, Son JH, Zarbin MA, Langer P, Guo S, et al. Twelve-year review of pediatric traumatic open globe injuries in an urban U.S. population. J Pediatr Ophthalmol Strabismus. 2012;49:73–9. doi: 10.3928/01913913-20110712-02. [DOI] [PubMed] [Google Scholar]
- 16.Liu X, Liu Z, Liu Y, Zhao L, Xu S, Su G, et al. Determination of visual prognosis in children with open globe injuries. Eye (Lond) 2014;28:852–6. doi: 10.1038/eye.2014.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ilhan HD, Bilgin AB, Cetinkaya A, Unal M, Yucel I. Epidemiological and clinical features of paediatric open globe injuries in Southwestern Turkey. Int J Ophthalmol. 2013;6:855–60. doi: 10.3980/j.issn.2222-3959.2013.06.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee CH, Lee L, Kao LY, Lin KK, Yang ML. Prognostic indicators of open globe injuries in children. Am J Emerg Med. 2009;27:530–5. doi: 10.1016/j.ajem.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Bunting H, Stephens D, Mireskandari K. Prediction of visual outcomes after open globe injury in children: A 17-year Canadian experience. J AAPOS. 2013;17:43–8. doi: 10.1016/j.jaapos.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 20.Farr AK, Hairston RJ, Humayun MU, Marsh MJ, Pieramici DJ, MacCumber MW, et al. Open globe injuries in children: A retrospective analysis. J Pediatr Ophthalmol Strabismus. 2001;38:72–7. doi: 10.3928/0191-3913-20010301-07. [DOI] [PubMed] [Google Scholar]
- 21.Acar U, Tok OY, Acar DE, Burcu A, Ornek F. A new ocular trauma score in pediatric penetrating eye injuries. Eye (Lond) 2011;25:370–4. doi: 10.1038/eye.2010.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kadappu S, Silveira S, Martin F. Aetiology and outcome of open and closed globe eye injuries in children. Clin Experiment Ophthalmol. 2013;41:427–34. doi: 10.1111/ceo.12034. [DOI] [PubMed] [Google Scholar]
- 23.Tok O, Tok L, Ozkaya D, Eraslan E, Ornek F, Bardak Y. Epidemiological characteristics and visual outcome after open globe injuries in children. J AAPOS. 2011;15:556–61. doi: 10.1016/j.jaapos.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 24.Dulal S, Ale JB, Sapkota YD. Profile of pediatric ocular trauma in mid western hilly region of Nepal. Nepal J Ophthalmol. 2012;4:134–7. doi: 10.3126/nepjoph.v4i1.5865. [DOI] [PubMed] [Google Scholar]
- 25.Omobolanle AA, Henrietta N. Pattern of paediatric corneal laceration injuries in the University of Port Harcourt teaching hospital, Rivers State, Nigeria. BMC Res Notes. 2012;5:683. doi: 10.1186/1756-0500-5-683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuhn F, Morris R, Witherspoon CD, Mester V. The Birmingham Eye Trauma Terminology system (BETT) J Fr Ophtalmol. 2004;27:206–10. doi: 10.1016/s0181-5512(04)96122-0. [DOI] [PubMed] [Google Scholar]
- 27.Pieramici DJ, Sternberg P, Jr, Aaberg TM, Sr, Bridges WZ, Jr, Capone A, Jr, Cardillo JA, et al. The ocular trauma classification group. A system for classifying mechanical injuries of the eye (globe) Am J Ophthalmol. 1997;123:820–31. doi: 10.1016/s0002-9394(14)71132-8. [DOI] [PubMed] [Google Scholar]
- 28.Augsburger JJ, Corrêa ZM. Vaughan & Asbury's General Ophthalmology. 18th ed. New York: McGraw-Hill; 2011. [Last accessed on 2014 Jul 17]. Ophthalmic trauma. Available from: http://accessmedicine.mhmedical.com.proxy.libraries.rutgers.edu/book.aspx?bookid=387 . [Google Scholar]
- 29.Cao H, Li L, Zhang M, Li H. Epidemiology of pediatric ocular trauma in the Chaoshan Region, China, 2001-2010. PLoS One. 2013;8:e60844. doi: 10.1371/journal.pone.0060844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahmadabadi MN, Alipour F, Tabataei SA, Karkhane R, Rezaei H, Ahmadabadi EN. Sharp-object-induced open-globe injuries in Iranian children admitted to a major tertiary center: A prospective review of 125 cases. Ophthalmic Res. 2011;45:149–54. doi: 10.1159/000319546. [DOI] [PubMed] [Google Scholar]
- 31.Baiyeroju-Agbeja AM, Olurin-Aina OI. Penetrating eye injuries in children in Ibadan. Afr J Med Med Sci. 1998;27:13–5. [PubMed] [Google Scholar]
- 32.Acuna OM, Yen KG. Outcome and prognosis of pediatric patients with delayed diagnosis of open-globe injuries. J Pediatr Ophthalmol Strabismus. 2009;46:202–7. doi: 10.3928/01913913-20090706-04. [DOI] [PubMed] [Google Scholar]
- 33.Mansouri M, Faghihi H, Hajizadeh F, Rasoulinejad SA, Rajabi MT, Tabatabaey A, et al. Epidemiology of open-globe injuries in Iran: Analysis of 2,340 cases in 5 years (report no 1) Retina. 2009;29:1141–9. doi: 10.1097/IAE.0b013e3181a395ac. [DOI] [PubMed] [Google Scholar]
- 34.Tsui E, Salcone EM. Corneal trauma in a 6-year-old boy. JAMA. 2012;307:1970–1. doi: 10.1001/jama.2012.3457. [DOI] [PubMed] [Google Scholar]
- 35.Gayer S, Tutiven J. Anesthesia for pediatric ocular surgery. Ophthalmol Clin North Am. 2006;19:269–78. doi: 10.1016/j.ohc.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 36.Choovuthayakorn J, Patikulsila P, Patikulsila D, Watanachai N, Pimolrat W. Characteristics and outcomes of pediatric open globe injury. Int Ophthalmol. 2014;34:839–44. doi: 10.1007/s10792-013-9890-8. [DOI] [PubMed] [Google Scholar]
- 37.Castellarin AA, Pieramici DJ. Open globe management. Compr Ophthalmol Update. 2007;8:111–24. [PubMed] [Google Scholar]
- 38.Pollard KA, Xiang H, Smith GA. Pediatric eye injuries treated in US emergency departments, 1990-2009. Clin Pediatr (Phila) 2012;51:374–81. doi: 10.1177/0009922811427583. [DOI] [PubMed] [Google Scholar]
- 39.Karaman K, Znaor L, Lakos V, Olujic I. Epidemiology of pediatric eye injury in Split-Dalmatia County. Ophthalmic Res. 2009;42:199–204. doi: 10.1159/000232403. [DOI] [PubMed] [Google Scholar]
- 40.Armstrong GW, Kim JG, Linakis JG, Mello MJ, Greenberg PB. Pediatric eye injuries presenting to United States emergency departments: 2001-2007. Graefes Arch Clin Exp Ophthalmol. 2013;251:629–36. doi: 10.1007/s00417-011-1917-0. [DOI] [PubMed] [Google Scholar]
- 41.Krott R, Bartz-Schmidt KU, Heimann K. Laceration of the eye with a fishing hook. Br J Ophthalmol. 1999;83:1194. doi: 10.1136/bjo.83.10.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jalali S, Das T, Majji AB. Hypodermic needles: A new source of penetrating ocular trauma in Indian children. Retina. 1999;19:213–7. [PubMed] [Google Scholar]
- 43.Kimia A, Lee L, Shannon M, Capraro A, Mays D, Johnston P, et al. Holiday ornament-related injuries in children. Pediatr Emerg Care. 2009;25:819–22. doi: 10.1097/PEC.0b013e3181c33109. [DOI] [PubMed] [Google Scholar]
- 44.Chang JH, Mills RA, Pater J, Crompton JL. Case series of cat-scratch-inflicted full-thickness corneal lacerations and a review of the literature. Clin Experiment Ophthalmol. 2012;40:669–74. doi: 10.1111/j.1442-9071.2012.02783.x. [DOI] [PubMed] [Google Scholar]
- 45.Schrader WF, Gramer E. Open globe injuries induced by glass bottles containing carbonated drinks. Graefes Arch Clin Exp Ophthalmol. 2010;248:313–7. doi: 10.1007/s00417-009-1145-z. [DOI] [PubMed] [Google Scholar]
- 46.Stubbs AJ, Aburn NS. Penetrating eye injury from a rigid infant pacifier. Aust N Z J Ophthalmol. 1996;24:71–3. doi: 10.1111/j.1442-9071.1996.tb01555.x. [DOI] [PubMed] [Google Scholar]
- 47.Pahk PJ, Adelman RA. Ocular trauma resulting from paintball injury. Graefes Arch Clin Exp Ophthalmol. 2009;247:469–75. doi: 10.1007/s00417-008-0985-2. [DOI] [PubMed] [Google Scholar]
- 48.Bhavsar AR, Chen TC, Goldstein DA. Corneoscleral laceration associated with passenger-side airbag inflation. Br J Ophthalmol. 1997;81:514–5. doi: 10.1136/bjo.81.6.513b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ball DC, Bouchard CS. Ocular morbidity associated with airbag deployment: A report of seven cases and a review of the literature. Cornea. 2001;20:159–63. doi: 10.1097/00003226-200103000-00009. [DOI] [PubMed] [Google Scholar]
- 50.Skarbek-Borowska SE, Campbell KT. Globe rupture and nonaccidental trauma: Two case reports. Pediatr Emerg Care. 2011;27:544–6. doi: 10.1097/PEC.0b013e31821dc702. [DOI] [PubMed] [Google Scholar]
- 51.Xu YN, Huang YS, Xie LX. Pediatric traumatic cataract and surgery outcomes in eastern China: A hospital-based study. Int J Ophthalmol. 2013;6:160–4. doi: 10.3980/j.issn.2222-3959.2013.02.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patel R, Mukherjee B. Crash & burn: Ocular injuries due to fireworks. Semin Ophthalmol. 2014:1–6. doi: 10.3109/08820538.2014.962157. [DOI] [PubMed] [Google Scholar]
- 53.Lecuona K. Assessing and managing eye injuries. Community Eye Health. 2005;18:101–4. [PMC free article] [PubMed] [Google Scholar]
- 54.Ryan SJ, Schachat AP, Wilkinson CP, Hinton DR, Sadda SR, Wiedemann P. 5th ed. New York: Elsevier; 2013. Retina. [Google Scholar]
- 55.Raina UK, Kumar V, Kumar V, Sud R, Goel N, Ghosh B. Metallic intraocular foreign body retained for four years — An unusual presentation. Cont Lens Anterior Eye. 2010;33:202–4. doi: 10.1016/j.clae.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 56.Patel SN, Langer PD, Zarbin MA, Bhagat N. Diagnostic value of clinical examination and radiographic imaging in identification of intraocular Foreign bodies in open globe injury. Eur J Ophthalmol. 2012;22:259–68. doi: 10.5301/EJO.2011.8347. [DOI] [PubMed] [Google Scholar]
- 57.Yamashita K, Noguchi T, Mihara F, Yoshiura T, Togao O, Yoshikawa H, et al. An intraorbital wooden foreign body: Description of a case and a variety of CT appearances. Emerg Radiol. 2007;14:41–3. doi: 10.1007/s10140-007-0597-x. [DOI] [PubMed] [Google Scholar]
- 58.Fielding JA. The assessment of ocular injury by ultrasound. Clin Radiol. 2004;59:301–12. doi: 10.1016/j.crad.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 59.Perisinakis K, Raissaki M, Theocharopoulos N, Damilakis J, Gourtsoyiannis N. Reduction of eye lens radiation dose by orbital bismuth shielding in pediatric patients undergoing CT of the head: A monte carlo study. Med Phys. 2005;32:1024–30. doi: 10.1118/1.1881852. [DOI] [PubMed] [Google Scholar]
- 60.Kubal WS. Imaging of orbital trauma. Radiographics. 2008;28:1729–39. doi: 10.1148/rg.286085523. [DOI] [PubMed] [Google Scholar]
- 61.Andreoli MT, Yiu G, Hart L, Andreoli CM. B-scan ultrasonography following open globe repair. Eye (Lond) 2014;28:381–5. doi: 10.1038/eye.2013.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kuhn FP, Pieramici DJ. Vol. 64. New York: Thieme; 2002. Ocular Trauma: Principles and Practice; pp. 241–2. [Google Scholar]
- 63.Trief D, Adebona OT, Turalba AV, Shah AS. The pediatric traumatic hyphema. Int Ophthalmol Clin. 2013;53:43–57. doi: 10.1097/IIO.0b013e3182a129fd. [DOI] [PubMed] [Google Scholar]
- 64.Narang S, Gupta V, Gupta A, Dogra MR, Pandav SS, Das S. Role of prophylactic intravitreal antibiotics in open globe injuries. Indian J Ophthalmol. 2003;51:39–44. [PubMed] [Google Scholar]
- 65.Bhagat N, Nagori S, Zarbin M. Post-traumatic infectious endophthalmitis. Surv Ophthalmol. 2011;56:214–51. doi: 10.1016/j.survophthal.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 66.Agrawal R, Shah M, Mireskandari K, Yong GK. Controversies in ocular trauma classification and management: Review. Int Ophthalmol. 2013;33:435–45. doi: 10.1007/s10792-012-9698-y. [DOI] [PubMed] [Google Scholar]
- 67.Yonekawa Y, Chodosh J, Eliott D. Surgical techniques in the management of perforating injuries of the globe. Int Ophthalmol Clin. 2013;53:127–37. doi: 10.1097/IIO.0b013e3182a12b01. [DOI] [PubMed] [Google Scholar]
- 68.Yeh S, Colyer MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol. 2008;19:225–33. doi: 10.1097/ICU.0b013e3282fa75f1. [DOI] [PubMed] [Google Scholar]
- 69.Saxena S, Jalali S, Verma L, Pathengay A. Management of vitreous haemorrhage. Indian J Ophthalmol. 2003;51:189–96. [PubMed] [Google Scholar]
- 70.Ahmed Y, Schimel AM, Pathengay A, Colyer MH, Flynn HW., Jr Endophthalmitis following open-globe injuries. Eye (Lond) 2012;26:212–7. doi: 10.1038/eye.2011.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Soheilian M, Rafati N, Mohebbi MR, Yazdani S, Habibabadi HF, Feghhi M, et al. Prophylaxis of acute posttraumatic bacterial endophthalmitis: A multicenter, randomized clinical trial of intraocular antibiotic injection, report 2. Arch Ophthalmol. 2007;125:460–5. doi: 10.1001/archopht.125.4.460. [DOI] [PubMed] [Google Scholar]
- 72.Woodruff G, Hiscox F, Thompson JR, Smith LK. Factors affecting the outcome of children treated for amblyopia. Eye (Lond) 1994;8(Pt 6):627–31. doi: 10.1038/eye.1994.157. [DOI] [PubMed] [Google Scholar]
- 73.Taylor K, Powell C, Hatt SR, Stewart C. Interventions for unilateral and bilateral refractive amblyopia. Cochrane Database Syst Rev. 2012;4:CD005137. doi: 10.1002/14651858.CD005137.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bai H, Meng X, Wang D, Han J. Treatment for amblyopia after surgery for cataract and vitreoretina in pediatric ocular trauma. Eye Sci. 2013;28:68–72. [PubMed] [Google Scholar]
- 75.DeSantis D. Amblyopia. Pediatr Clin North Am. 2014;61:505–18. doi: 10.1016/j.pcl.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 76.Zaidman G, Ramirez T, Kaufman A, Palay D, Phillips R, Medow N. Successful surgical rehabilitation of children with traumatic corneal laceration and cataract. Ophthalmology. 2001;108:338–42. doi: 10.1016/s0161-6420(00)00524-8. [DOI] [PubMed] [Google Scholar]
- 77.Cebulla CM, Flynn HW., Jr Endophthalmitis after open globe injuries. Am J Ophthalmol. 2009;147:567–8. doi: 10.1016/j.ajo.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 78.Andreoli CM, Andreoli MT, Kloek CE, Ahuero AE, Vavvas D, Durand ML. Low rate of endophthalmitis in a large series of open globe injuries. Am J Ophthalmol. 2009;147:601–8.e2. doi: 10.1016/j.ajo.2008.10.023. [DOI] [PubMed] [Google Scholar]
- 79.Duch-Samper AM, Menezo JL, Hurtado-Sarrió M. Endophthalmitis following penetrating eye injuries. Acta Ophthalmol Scand. 1997;75:104–6. doi: 10.1111/j.1600-0420.1997.tb00263.x. [DOI] [PubMed] [Google Scholar]
- 80.Essex RW, Yi Q, Charles PG, Allen PJ. Post-traumatic endophthalmitis. Ophthalmology. 2004;111:2015–22. doi: 10.1016/j.ophtha.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 81.Hooi SH, Hooi ST. Open-globe injuries: The experience at Hospital Sultanah Aminah, Johor Bahru. Med J Malaysia. 2003;58:405–12. [PubMed] [Google Scholar]
- 82.Jonas JB, Knorr HL, Budde WM. Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology. 2000;107:823–8. doi: 10.1016/s0161-6420(00)00079-8. [DOI] [PubMed] [Google Scholar]
- 83.Sabaci G, Bayer A, Mutlu FM, Karagül S, Yildirim E. Endophthalmitis after deadly-weapon-related open-globe injuries: Risk factors, value of prophylactic antibiotics, and visual outcomes. Am J Ophthalmol. 2002;133:62–9. doi: 10.1016/s0002-9394(01)01320-4. [DOI] [PubMed] [Google Scholar]
- 84.Schrader WF. Epidemiology of open globe eye injuries: Analysis of 1026 cases in 18 years. Klin Monbl Augenheilkd. 2004;221:629–35. doi: 10.1055/s-2004-813254. [DOI] [PubMed] [Google Scholar]
- 85.Zhang Y, Zhang MN, Jiang CH, Yao Y, Zhang K. Endophthalmitis following open globe injury. Br J Ophthalmol. 2010;94:111–4. doi: 10.1136/bjo.2009.164913. [DOI] [PubMed] [Google Scholar]
- 86.Khan S, Athwal L, Zarbin M, Bhagat N. Pediatric infectious endophthalmitis: A review. J Pediatr Ophthalmol Strabismus. 2014;51:140–53. doi: 10.3928/01913913-20140507-01. [DOI] [PubMed] [Google Scholar]
- 87.Junejo SA, Ahmed M, Alam M. Endophthalmitis in paediatric penetrating ocular injuries in Hyderabad. J Pak Med Assoc. 2010;60:532–5. [PubMed] [Google Scholar]
- 88.Alfaro DV, Roth DB, Laughlin RM, Goyal M, Liggett PE. Paediatric post-traumatic endophthalmitis. Br J Ophthalmol. 1995;79:888–91. doi: 10.1136/bjo.79.10.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19:227–34. doi: 10.1111/1469-0691.12118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang NK, Chen YP, Yeung L, Chen KJ, Chao AN, Kuo YH, et al. Traumatic pediatric retinal detachment following open globe injury. Ophthalmologica. 2007;221:255–63. doi: 10.1159/000101928. [DOI] [PubMed] [Google Scholar]
- 91.Feng X, Feng K, Hu Y, Ma Z. Clinical features and outcomes of vitrectomy in pediatric ocular injuries-eye injury vitrectomy study. Indian J Ophthalmol. 2014;62:450–3. doi: 10.4103/0301-4738.120222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Szurman P, Roters S, Grisanti S, Aisenbrey S, Rohrbach JM, Warga M, et al. Primary silicone oil tamponade in the management of severe intraocular foreign body injuries: An 8-year follow-up. Retina. 2007;27:304–11. doi: 10.1097/01.iae.0000237685.99713.83. [DOI] [PubMed] [Google Scholar]
- 93.Sebag J. Anomalous posterior vitreous detachment: A unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol. 2004;242:690–8. doi: 10.1007/s00417-004-0980-1. [DOI] [PubMed] [Google Scholar]
- 94.Meier P. Combined anterior and posterior segment injuries in children: A review. Graefes Arch Clin Exp Ophthalmol. 2010;248:1207–19. doi: 10.1007/s00417-010-1414-x. [DOI] [PubMed] [Google Scholar]
- 95.Kumar K, Mathai A, Murthy SI, Jalali S, Sangwan V, Reddy Pappuru R, et al. Sympathetic ophthalmia in pediatric age group: Clinical features and challenges in management in a tertiary center in Southern India. Ocul Immunol Inflamm. 2014;22:367–72. doi: 10.3109/09273948.2013.841958. [DOI] [PubMed] [Google Scholar]
- 96.Chu XK, Chan CC. Sympathetic ophthalmia: To the twenty-first century and beyond. J Ophthalmic Inflamm Infect. 2013;3:49. doi: 10.1186/1869-5760-3-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Birgfeld C, Gruss J. The importance of accurate, early bony reconstruction in orbital injuries with globe loss. Craniomaxillofac Trauma Reconstr. 2011;4:121–8. doi: 10.1055/s-0031-1279673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Parke DW, 3rd, Flynn HW, Jr, Fisher YL. Management of intraocular foreign bodies: A clinical flight plan. Can J Ophthalmol. 2013;48:8–12. doi: 10.1016/j.jcjo.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 99.Lim LT, Shankar V, Blum RA, Hammer HM. Long-standing iron-containing intraocular foreign body without siderosis. Clin Exp Optom. 2011;94:387–8. doi: 10.1111/j.1444-0938.2010.00561.x. [DOI] [PubMed] [Google Scholar]
- 100.Sangermani C, Mora P, Mancini C, Vecchi M, Gandolfi SA. Ultrasound biomicroscopy in two cases of ocular siderosis with secondary glaucoma. Acta Ophthalmol. 2010;88:e1–2. doi: 10.1111/j.1755-3768.2009.01521.x. [DOI] [PubMed] [Google Scholar]
- 101.Ballantyne JF. Siderosis bulbi. Br J Ophthalmol. 1954;38:727–33. doi: 10.1136/bjo.38.12.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The ocular trauma score (OTS) Ophthalmol Clin North Am. 2002;15:163–5. doi: 10.1016/s0896-1549(02)00007-x. [DOI] [PubMed] [Google Scholar]
- 103.Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115:202–9. doi: 10.1016/j.ophtha.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 104.Schörkhuber MM, Wackernagel W, Riedl R, Schneider MR, Wedrich A. Ocular trauma scores in paediatric open globe injuries. Br J Ophthalmol. 2014;98:664–8. doi: 10.1136/bjophthalmol-2013-304469. [DOI] [PubMed] [Google Scholar]
- 105.Yu Wai Man C, Steel D. Visual outcome after open globe injury: A comparison of two prognostic models — The ocular trauma score and the classification and regression tree. Eye (Lond) 2010;24:84–9. doi: 10.1038/eye.2009.16. [DOI] [PubMed] [Google Scholar]


