Abstract
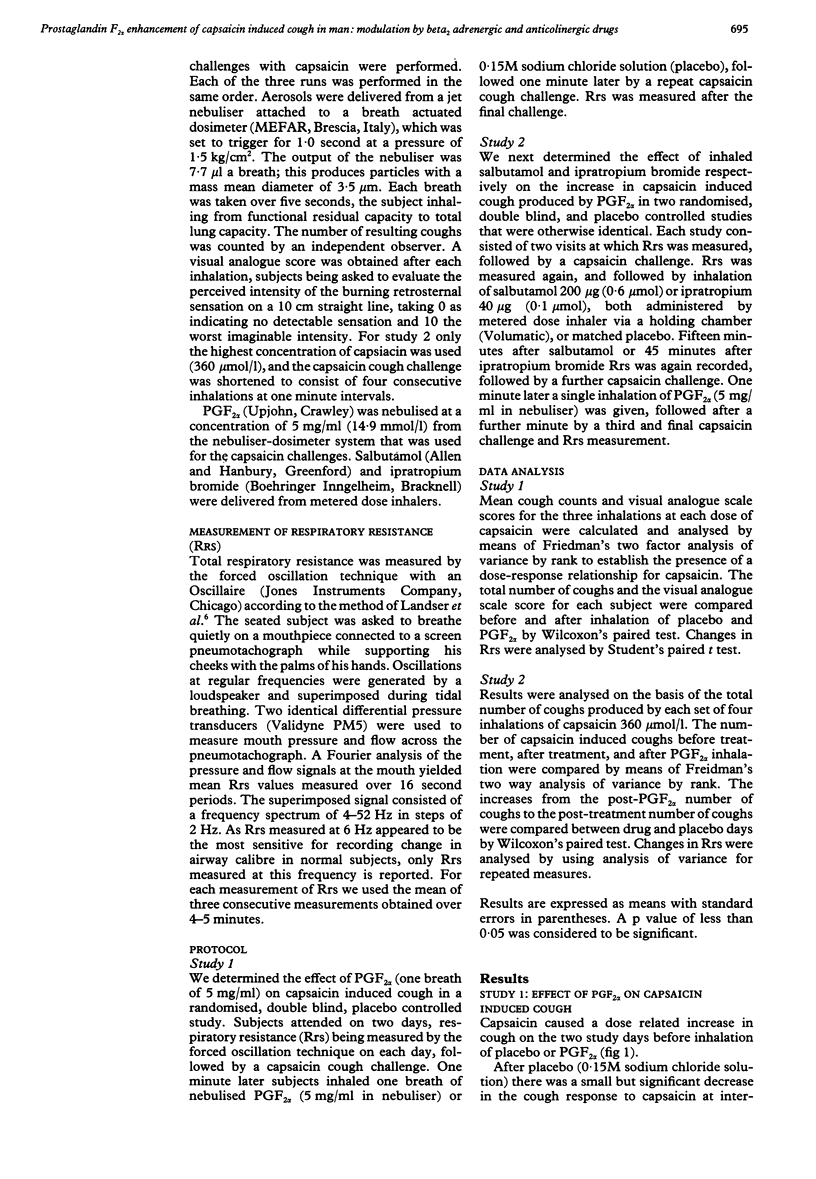
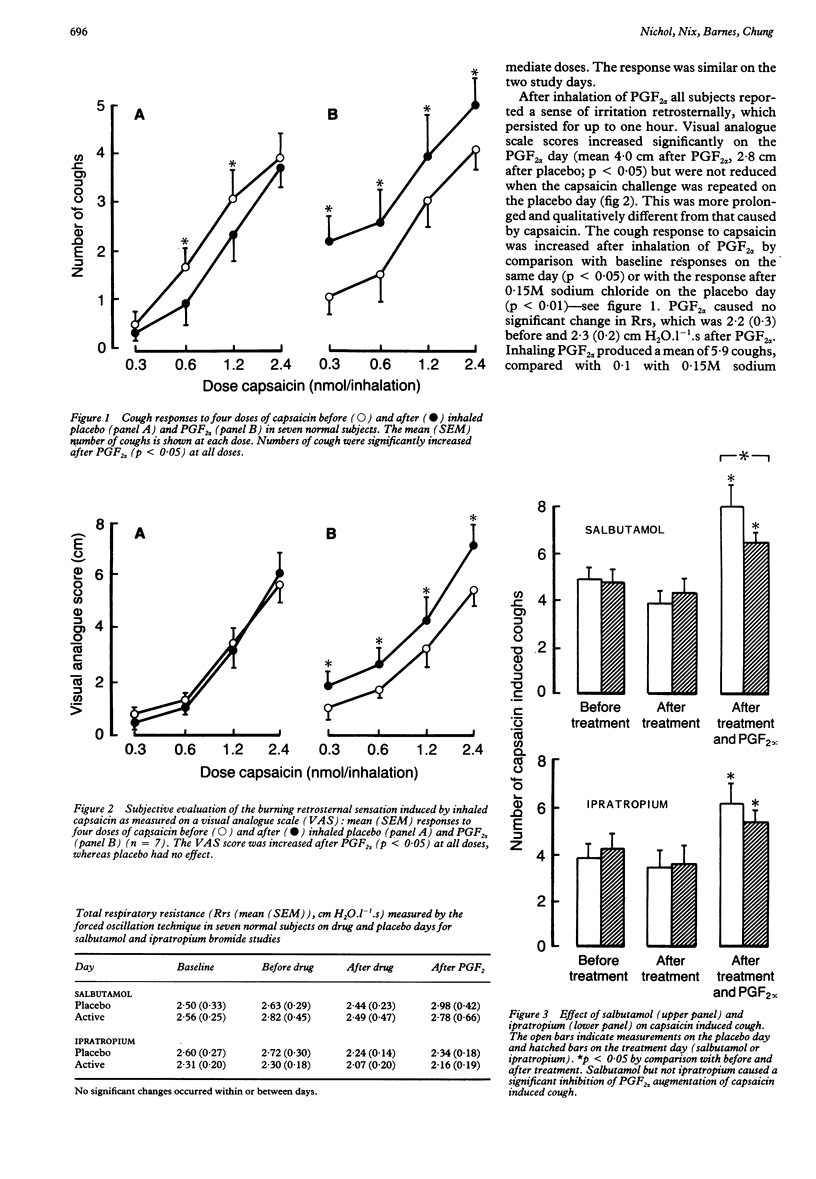
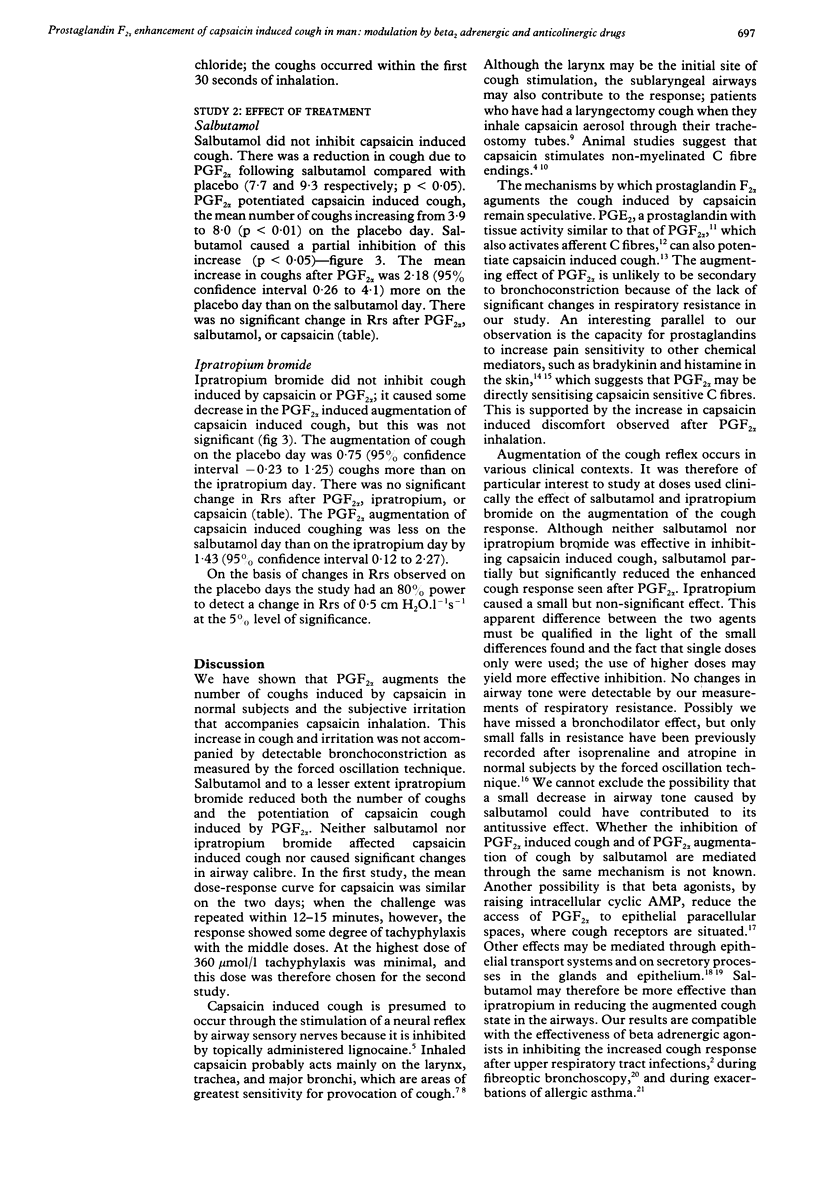
The effect of inhaled prostaglandin (PG) F2 alpha on the response to the inhaled tussive agent capsaicin was investigated in normal subjects. Seven subjects inhaled three breaths of four doses of capsaicin (0.3, 0.6, 1.2, and 2.4 nmol) before and immediately after inhaling PGF2 alpha (0.1 mumol) or placebo (0.15M NaCl) on separate days. The numbers of capsaicin induced coughs were greater after PGF2 alpha (mean 42.3 coughs) than after 0.15M sodium chloride (30.1). Visual analogue scores (0-10 on a 10 cm continuous scale) showed that capsaicin was more irritant after PGF2 alpha than after saline. Total respiratory resistance (Rrs), measured by the forced oscillation technique, was unaltered throughout the study. A double blind, placebo controlled study of the effects of inhaled salbutamol (200 micrograms, 0.6 mumol) and ipratropium bromide (40 micrograms, 0.1 mumol) on cough induced by capsaicin (2.4 nmol) and by PGF2 alpha (0.1 mumol) and on PGF2 alpha augmented, capsaicin induced coughing was performed in seven subjects. Neither drug had any effect on capsaicin induced coughing. Salbutamol reduced coughing due to PGF2 alpha (mean 7.7 coughs after salbutamol, 9.3 after placebo) but ipratropium bromide did not (mean 6.9 coughs after ipratropium bromide, 6.6 after placebo). Salbutamol also inhibited the augmentation of the capsaicin induced cough that followed inhalation of PGF2 alpha (mean augmentation 1.9 coughs after salbutamol, 4.1 after placebo), whereas ipratropium bromide did not (augmentation 1.7 coughs after ipratropium bromide, 2.7 after placebo). No changes in Rrs were seen after PGF2 alpha or either drug. Thus salbutamol reduces PGF2 alpha induced cough and the augmentation of capsaicin induced cough that follows PGF2 alpha.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Choudry N. B., Fuller R. W., Pride N. B. Sensitivity of the human cough reflex: effect of inflammatory mediators prostaglandin E2, bradykinin, and histamine. Am Rev Respir Dis. 1989 Jul;140(1):137–141. doi: 10.1164/ajrccm/140.1.137. [DOI] [PubMed] [Google Scholar]
- Coleridge H. M., Coleridge J. C., Baker D. G., Ginzel K. H., Morrison M. A. Comparison of the effects of histamine and prostaglandin on afferent C-fiber endings and irritant receptors in the intrapulmonary airways. Adv Exp Med Biol. 1978;99:291–305. doi: 10.1007/978-1-4613-4009-6_32. [DOI] [PubMed] [Google Scholar]
- Coleridge H. M., Coleridge J. C. Impulse activity in afferent vagal C-fibres with endings in the intrapulmonary airways of dogs. Respir Physiol. 1977 Apr;29(2):125–142. doi: 10.1016/0034-5687(77)90086-x. [DOI] [PubMed] [Google Scholar]
- Collier H. O., Schneider C. Nociceptive response to prostaglandins and analgesic actions of aspirin and morphine. Nat New Biol. 1972 Apr 5;236(66):141–143. doi: 10.1038/newbio236141a0. [DOI] [PubMed] [Google Scholar]
- Collier J. G., Fuller R. W. Capsaicin inhalation in man and the effects of sodium cromoglycate. Br J Pharmacol. 1984 Jan;81(1):113–117. doi: 10.1111/j.1476-5381.1984.tb10750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello J. F., Dunlop L. S., Gardiner P. J. Characteristics of prostaglandin induced cough in man. Br J Clin Pharmacol. 1985 Oct;20(4):355–359. doi: 10.1111/j.1365-2125.1985.tb05077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis B., Marin M. G., Yee J. W., Nadel J. A. Effect of terbutaline on movement of Cl- and Na+ across the trachea of the dog in vitro. Am Rev Respir Dis. 1979 Sep;120(3):547–552. doi: 10.1164/arrd.1979.120.3.547. [DOI] [PubMed] [Google Scholar]
- Duffey M. E., Hainau B., Ho S., Bentzel C. J. Regulation of epithelial tight junction permeability by cyclic AMP. Nature. 1981 Dec 3;294(5840):451–453. doi: 10.1038/294451a0. [DOI] [PubMed] [Google Scholar]
- Ellul-Micallef R. Effect of terbutaline sulphate in chronic "allergic" cough. Br Med J (Clin Res Ed) 1983 Oct 1;287(6397):940–943. doi: 10.1136/bmj.287.6397.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Empey D. W., Laitinen L. A., Jacobs L., Gold W. M., Nadel J. A. Mechanisms of bronchial hyperreactivity in normal subjects after upper respiratory tract infection. Am Rev Respir Dis. 1976 Feb;113(2):131–139. doi: 10.1164/arrd.1976.113.2.131. [DOI] [PubMed] [Google Scholar]
- Irwin R. S., Corrao W. M., Pratter M. R. Chronic persistent cough in the adult: the spectrum and frequency of causes and successful outcome of specific therapy. Am Rev Respir Dis. 1981 Apr;123(4 Pt 1):413–417. doi: 10.1164/arrd.1981.123.4.413. [DOI] [PubMed] [Google Scholar]
- Lundberg J. M., Saria A. Capsaicin-induced desensitization of airway mucosa to cigarette smoke, mechanical and chemical irritants. Nature. 1983 Mar 17;302(5905):251–253. doi: 10.1038/302251a0. [DOI] [PubMed] [Google Scholar]
- Lándsér F. J., Nagles J., Demedts M., Billiet L., van de Woestijne K. P. A new method to determine frequency characteristics of the respiratory system. J Appl Physiol. 1976 Jul;41(1):101–106. doi: 10.1152/jappl.1976.41.1.101. [DOI] [PubMed] [Google Scholar]
- Manço J. C., Hyatt R. E., Rodarte J. R. Respiratory impedance in normal humans: effects of bronchodilatation and bronchoconstriction. Mayo Clin Proc. 1987 Jun;62(6):487–497. doi: 10.1016/s0025-6196(12)65475-5. [DOI] [PubMed] [Google Scholar]
- Nicholls M. G., Gilchrist N. L. Sulindac and cough induced by converting enzyme inhibitors. Lancet. 1987 Apr 11;1(8537):872–872. doi: 10.1016/s0140-6736(87)91663-1. [DOI] [PubMed] [Google Scholar]
- Phipps R. J., Williams I. P., Richardson P. S., Pell J., Pack R. J., Wright N. Sympathomimetic drugs stimulate the output of secretory glycoproteins from human bronchi in vitro. Clin Sci (Lond) 1982 Jul;63(1):23–28. doi: 10.1042/cs0630023. [DOI] [PubMed] [Google Scholar]
- Sant'Ambrogio G. Information arising from the tracheobronchial tree of mammals. Physiol Rev. 1982 Apr;62(2):531–569. doi: 10.1152/physrev.1982.62.2.531. [DOI] [PubMed] [Google Scholar]
- Vesco D., Kleisbauer J. P., Orehek J. Attenuation of bronchofiberscopy-induced cough by an inhaled beta 2-adrenergic agonist, fenoterol. Am Rev Respir Dis. 1988 Oct;138(4):805–806. doi: 10.1164/ajrccm/138.4.805. [DOI] [PubMed] [Google Scholar]
- WIDDICOMBE J. G. Receptors in the trachea and bronchi of the cat. J Physiol. 1954 Jan;123(1):71–104. doi: 10.1113/jphysiol.1954.sp005034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zurier R. B. Prostaglandins, inflammation, and asthma. Arch Intern Med. 1974 Jan;133(1):101–110. [PubMed] [Google Scholar]


