Abstract
Background
5–10% of schoolchildren in Germany are absent from school without an excuse more than five times per year. We investigate the effectiveness of manual-based, multimodal cognitive behavioral therapy focusing on school-avoidant behavior and on the underlying mental disorders.
Methods
112 school avoiders were recruited from an outpatient child and adolescent psychiatric clinic and adaptively randomized into two treatment groups. The first group received manual-based multimodal treatment (MT), the second group treatment as usual (TAU) in the child and adolescent mental health care system. The primary outcome of the study was the percentage of classes attended in the five days prior to first measurement (before the intervention), as well as 6 and 12 months afterward. In each of these periods, school attendance was characterized as regular, partial, or none. Secondary outcomes were the severity of anxiety and depressive symptoms, self-efficacy, and quality of family life.
Results
In both treatment arms, the percentage of regular school attenders rose to about 60% in 6 months, regardless of the intervention (MT 60.6%, TAU 58.3%; odds ratio [OR] for changes over baseline 6.94, 95% confidence interval [CI] 3.98–12.12, p<0.001; OR for MT versus TAU 1.05, 95% CI 0.58–1.90, p = 0.875). The improvement persisted 12 months after inclusion.
Conclusion
In accordance with earlier studies, we found that manual-based multimodal treatment did not improve school avoidance to any greater extent than treatment as usual. Future studies should focus on the conditions for successful reintegration in school and on the differential indicators for outpatient versus inpatient treatment.
Absenteeism from school is associated with the risk of stopping one’s educational career (1) and is accompanied by an increased risk for failing school, unemployment, and mental disorders (2, 3). Five to 10% of German school students are absent from school to a substantial extent (>5 times unexcused absence/school year) (4, 5). School absenteeism that is accompanied by psychiatric symptoms is defined as school avoiding behavior (6– 8). All these factors contribute to the need to evaluate effective treatment strategies.
Two longitudinal studies reported successful outcomes for inpatient or outpatient cognitive behavioral therapy (CBT) with regard to psychopathology and school attendance. Walter et al. ([9], Germany) showed an increase in the proportion of regular school attenders to 87.1% subsequent to inpatient CBT. Heyne et al. ([10], Australia) achieved a school attendance rate of 40.5% in the outpatient setting. The patients primarily had anxiety and/or depressive disorders. According to Maric et al. (11), the improvements in the study reported by Heyne et al. (10) can partly be explained by the mediating effect of self-efficacy, which is associated with improved school performance (12).
To date, three randomized controlled trials (RCTs) have investigated the effects of CBT on school attendance. King et al. (13) showed that for patients with anxiety disorders, CBT was superior to waiting list conditions as regards school attendance (n=2×17 patients). Last et al. (14), however, found overall improvements in school attendance for patients with school phobia (separation anxiety), who were randomized to either CBT or psychoeducation treatment (n=32 and n=24), but they observed no differences between groups. A comparison between groups showed significantly stronger improvements in anxiety symptoms in patients in the psychoeducation group; depressive symptoms reduced significantly in the CBT group. A comparison of CBT, parent–teacher training, and a combination of both approaches for patients with primary anxiety disorder was undertaken by Heyne and colleagues in Australia (15) (n = 21 versus n = 20 versus n = 20; RCT). Differences between groups did not reach significance at 4.5 months after the end of the treatment.
The present study evaluated a multimodal, multiprofessional behavioral therapeutic treatment strategy (manual-based multimodal treatment [experimental group]) compared with treatment administered by child and adolescent psychiatrists in private practice in the regular mental health care system (treatment as usual [control group]). Before the start of treatment as well as at six and 12 months’ follow-ups we reviewed:
Primary outcome: proportion of school lessons attended within the five preceding school days (classified into no school attendance, partial school attendance, or regular school attendance)
Additional outcome variables: severity of the psychopathology, self-efficacy.
Methods
Design
The study has a randomized controlled parallel group design with three measurement points at six month intervals each. Patients were recruited from the clinical special outpatient department for children and adolescents with school avoiding behavior at the LVR-Hospital Essen. Box 1 lists the inclusion and exclusion criteria. On the basis of the RCTs conducted so far, we initially planned this study with a continuous outcome. We planned the number of cases on the basis of an assumed effect size of 0.25 for the treatment difference relating to the continuous outcome “proportion of school lessons attended within the five school days preceding the measurement point.” By using a sample size of 156 patients, the assumed between-group difference can be identified by using analysis of covariance (ANCOVA; F test) under consideration of the observed outcome at the previous measurement point as a covariate, and of a two-sided significance level of 5% and a power of 80% (G*Power, version 3.1.9.2). Patients were adaptively randomized centrally by an independent center (the Centre [sic] for Clinical Studies at Essen University Hospitals); they were stratified by sex and age younger/older than 15 years by using a biased coin method. Randomization was computer aided by the RITA (randomization in treatment arms [16]) program. The study was approved by the relevant ethics committee.
Box 1. Inclusion and exclusion criteria.
-
Inclusion criteria
School avoiders—that is, students who regularly miss school (at least three times in the six months before inclusion in the study) and who are absent for complete individual lessons at least
Age 6 up to (and including) 20 years
The child/adolescent is proficient enough in German for his/her participation in therapy to be feasible
Writing and reading skills
Written informed consent to participation in the study from the parents/caregivers/legal substitute
Subject participates in screening and complete pre-testing
The psychiatrist is released from the confidentiality requirement vis-à-vis the current form master and their successor in case of a change of class or school
A mental disorder has been confirmed (according to ICD-10)
-
Exclusion criteria
Intelligence quotient <70 (measured by using CFT 20-R)
Students with physicial disabilities and/or severe physical disorders (for example, heart failure, tumor disease)
Mentally healthy students
Students with a disorder according to chapter F2 of the ICD-10 (Schizophrenia, schizotypal, delusional, and other non-mood psychotic disorders) or at acute risk of self-harm or harming others
Students who are disinterested in school, who are school avoiders only in the sense that they show little interest in lessons and school and do not actively participate in lessons
Students who are regularly late for school but who do not miss individual lessons
Students who are kept out of school by their parents (for example, to conceal abuse or because of economic advantages)
Students who are not allowed to attend school owing to sanctions imposed by the school
Regular current psychotherapy that also focuses on school avoidance (not completed)
Intervention: Manual-based multimodal treatment
Patients in the manual-based multimodal treatment (experimental) group received multimodal treatment. The specified CBT is targeted at school avoidance and the underlying psychological disorder in equal measure. The manual comprises four modules (17), of which the module “cognitive behavioral therapy” is considered to be the most important. Since school avoiders are hard to motivate on the one hand, but present with a wide range of psychological/psychiatric disorders on the other hand, the main emphasis of the manual is placed on the motivational and planning phase of the treatment (Box 2; further information on the diagnostic evaluation and treatment according to the manual is in the eBox).
Box 2. Subject matter covered in the four modules of the school avoiders manual and study process.
-
Modules
-
Cognitive behavioral therapy
Indication: school avoidance and mental disorder
Frequency: up to two hours/week
Interventions (selection): school avoider specific exploration, multiprofessional case conceptualization (intervention 3), disorder-specific interventions from published behvioral therapy manuals which were adapted for school avoiders (for example [18, 19])
-
Family counseling
Indication: in the setting of the case conference
Frequency: usually one hour/week
Interventions (selection): family visits and counseling, supporting/strengthening parenting skills, accompanying students to school
-
School-related counseling
Indication: in the setting of the case conference
Frequency: usually one hour/week
Interventions (selection): giving advice on school career/education, case-related cooperative counseling/advice for teachers, accompanying students into the classroom
-
Psychoeducational exercise program
Indication: optional
Frequency: usually one hour/week
Interventions (selection): PC-aided sports games, improvement of social competencies, teaching coping strategies for everyday life
-
-
Therapy process
On average, cases were conceptualized (intervention 3) after 3.6 therapeutic sessions (mean: 41.6 days after the initial appointment; standard deviation 27.8 days). Six weeks after case conceptualization, the indication for inpatient treatment was defined in the setting of a case conference if the global assessment of psychosocial functioning according to ICD-10, axis VI, yielded a score of = 6 points.
17 patients of the manual-based multimodal treatment group dropped out of the therapy owing to insufficient motivation. In 20 patients, outpatient behavioral therapy was completed. After a one-year period, 19 patients were still receiving outpatient treatment. The average number of therapy sessions was 14.2, with parents sitting in as desired. The mean duration of treatment in patients with completed outpatient therapy was 23 weeks.
eBox. Further information on the diagnostic evaluation and manual-based multimodal treatment.
-
Standardized diagnostic evaluation
Diagnosis on the basis of the instrument “Diagnostic Interview for Mental Disorders in Children and Adolescents“ ([35, in German] for the standardized documentation of the diagnoses according to the ICD-10)
Use of the versions of the Diagnostic Interview for parents as well as for children
Standardized validation of the diagnoses by experienced case-managing clinicians in a consensus meeting
All interviewers underwent certified training in how to administer the instrument (Diagnostic Interview for Mental Disorders in Children and Adolescents)
-
Administering manual-based multimodal treatment
Two licensed psychologists with a diploma and three such psychologists undergoing advanced training in cognitive behavioral therapy, as well as a specialist in child and adolescent psychiatry and psychotherapy planned the behavioral therapy and administered it.
-
Adherence to the manual
Two raters who were not themselves administering therapy evaluated the therapeutic documentation by means of content analysis. They identified 86% of sessions as true to the manual (interrater reliability between r = 0.9 and r = 1.0).
Cases were conceptualized according to the manual in 95%.
The module “family counseling” included several supportive and educational interventions for parents and children. The interventions of the module “school-related conseling” included the school’s perspective on school avoidance, and the module “psychoeducational exercise program” aimed to strengthen students’ existing physical fitness and teach psychosocial competencies.
Intervention: Treatment as usual
Patients in the treatment as usual (control) group received a recommendation after the diagnostic evaluation had been completed to seek further treatment from one of 10 collaborating child and adolescent psychiatrists in private practice. Depending on the treating psychiatrist and on the psychiatric treatment approach, these patients (in accordance with the cooperation agreement) received within four weeks either psychodynamic, behavioral, or systemic therapy, and/or psychopharmacotherapy, initially in the outpatient setting.
Definition of study outcomes
The primary outcome was the ordinal-scale proportion of attended school lessons within the five days preceding the measurement points at the beginning of the study, after six months, and after 12 months. Owing to the distribution of the primary outcome (accumulations at 0 and 100%), we arranged—in a change to our original study protocol—the primary outcome into an ordinal scale, consisting of “no” (<10%), “partial” (≥10%+<90%), or “regular” ((≥90%) school attendance. The primary outcome as well as additional outcomes and measures are described in eTable 1.
eTable 1. Description of study outcomes and questionnaires.
| Outcome variable | Definition | Comments |
|---|---|---|
| Study outcomes | ||
| Relative proportion of school lessons attended in the five days preceding the survey | Categorized into
|
|
Psychopathology, externally rated:
|
Age-appropriate T scores for the overall severity grade of the CBCL |
|
Psychopathology, self rated (from the age of 12)
|
Age-appropriate T scores for the SCL-90-R subscales
|
|
General self efficacy:
|
Calculation of sum scores |
|
Family climate:
|
Use of subscale
|
|
Note: Because of space constraints we did not report additional outcomes, such as the proportion of regular school weeks over the period of the preceding 25 weeks. The exploratory analysis of the 25-week criterion does not contradict the results relating to the primary outcome
The above mentioned questionnaires to collect data on outcomes were administered at the first measurement point (T1), and at 6 months (T2) later, in a face to face interview. The same questionnaires were used for the telephone interview (T3), at 12 months after T1. In order to keep the extent of the assessment at T3 manageable, we did not use the version of the child behavior checklist 4–18 (CBCL) for parents; neither did we use the symptom checklist 90-R (SCL-90-R) except for the scales “depression” and “anxiety.”
Statistical analysis
We analyzed the data on the basis of the intention to treat cohort. The primary outcome was marginally modeled in a proportional odds model, based on the method of generalized estimating equations (GEE; [28]). To evaluate the treatment difference we included the baseline/follow-up measurement points (T1–T3) and the interaction between treatment and follow-up measurement point in the model. For the purposes of analyzing our secondary outcomes we examined the factors treatment, baseline/follow-up measurement points, and their interaction in a linear mixed model with an unstructured covariance matrix (29). We did not adjust for multiple testing, and all p values are strictly descriptive.
In order to analyze a possible bias to the results due to missing data, we compared non-response structures in both treatment groups, compared characteristics of patients with and without missing data, and, in addition to an analysis of all available cases (AAC; that is, T1–2, T1–3 or T1–2–3), we also evaluated imputed datasets. Under the assumption “missing not at random,” we assumed for the non-monotonic, missing data of the primary outcome the value “no school attendance” (worst case imputation). For the normally distributed additional outcomes, we multiply imputed under the assumption “missing at random” on the basis of the Markov Chain Monte Carlo (MCMC) technique ([30]; multiple imputations (MI); five imputations). Furthermore we applied the “last observation carried forward” (LOCF) approach to all outcomes. We analyzed our data by using the software package SAS, version 9.4.
Results
Recruitment and study dropouts
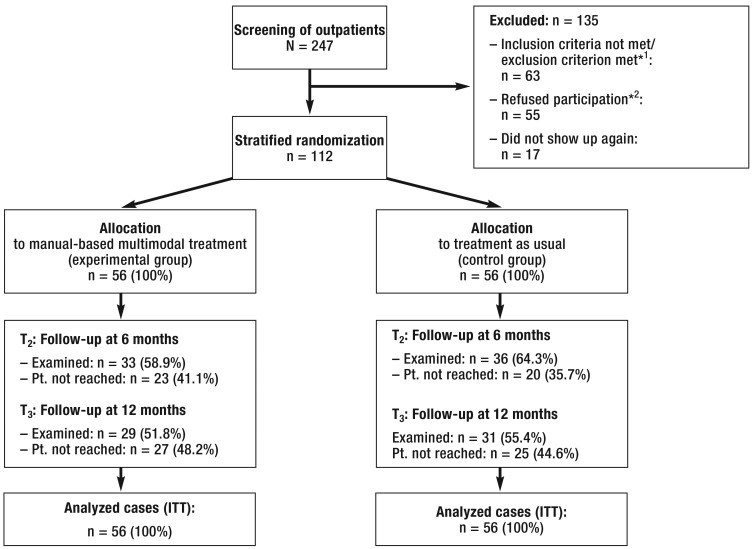
Between January 2011 and October 2012, 247 patients from the outpatient clinic for school avoiders and their main caregivers consecutively participated in a screening examination (Figure). 112 patients were included in the study.
Figure.
Recruitment and course of study (according to [31])
*1 No psychiatric disorder: n = 14 (22.2% of n = 63), intelligence quotient <70: n = 12 (19%), no missed lessons: n = 11 (17.5%),
at T1 in outpatient psychotherapy: n = 11 (17,5%), other: n = 15 (23.8%)
*2 Refused participation in the study because of the effort required as a result of the study conditions or therapy
ITT, intention to treat; Pt., patient
Our analyses of the dropouts did not show any differences (p>0.05) between regular study participants and dropouts with regard to variables such as age, sex, socioeconomic status, school attendance, psychopathology, or group membership. There were, however, indications that patients with externalizing disorders participated in the 1-year follow-up to a lesser degree than anticipated (χ 2= 5.133; p = 0.077).
Sociodemographic data, morbidity, and take-up
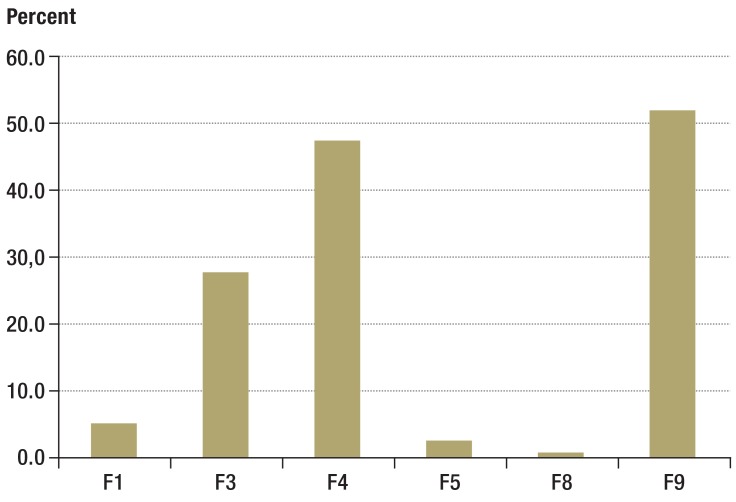
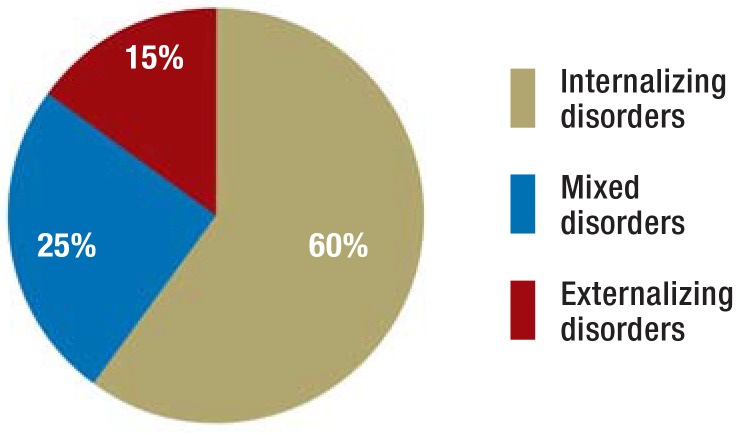
The mean age of the entire sample was 14.8 years (range 8.2–19.7 years). 34% of patients were female. The students came from all school types; 33% came from intermediate secondary schools and 33% from university preparatory high schools (eTable 2). We did not find any between-group differences regarding socioeconomic variables between the experimental group and the control group. In 51.8% of patients, a diagnosis of behavioral and emotional disorders with onset usually occurring in childhood and adolescence was made, followed by neurotic, stress-related, and somatoform (47.3%) and mood disorders (27.7%); eFigure 1; multiple diagnoses applied to 42.9% of patients. No differences between groups were seen for the diagnoses nor for the diagnostic criteria (eFigure 2).
eTable 2. Sociodemographic data.
| Manual-based multimodal treatment | Standard treatment | Total | |
|---|---|---|---|
| Mean age (SD) | 15.0 (2,4) | 14.6 (2,5) | 14.8 (2.5) |
| Female | 18 (32.1) | 20 (35.7) | 38 (33.9) |
| Male | 38 (67.9) | 36 (64.3) | 74 (66.1) |
| Socioeconomic status according to the Winkler index*1: n (%) | |||
|
22 (39.3) | 18 (32.1) | 40 (35.7) |
|
22 (39.3) | 22 (39.3) | 44 (39.3) |
|
11 (19.6) | 11 (19.6) | 22 (19.6) |
|
1 (1.8) | 5 (8.9) | 6 (5.4) |
| School type: n (%) | |||
|
4 (7.1) | 4 (7.1) | 8 (7.2) |
|
6 (10.7) | 1 (1.8) | 7 (6.3) |
|
7 (12.5) | 9 (16.1) | 16 (14.3) |
|
16 (28.6) | 21 (37.5) | 37 (33) |
|
20 (35.7) | 17 (30.4) | 37 (33) |
|
3 (5.4) | 1 (1.8) | 4 (3.5) |
|
0 | 3 (5.4) | 3 (2.7) |
| Class level: n | |||
|
7 | 7 | 7 |
|
9 | 8 | 8 |
|
10 | 10 | 10 |
Reported as means or patient numbers; reference value: N = 112; SD, standard deviation
*1Winkler index to identify the socioeconomic class of the parimary caregiver (36)
*2Includes the relevant school streams at comprehensive secondary schools
eFigure 1.
Psychiatric morbidity (ICD-10; multiple diagnoses are possible)
Notes:
F1 Mental and behavioral disorders due to psychoactive substance use
F3 Mood [affective] disorders
F4 Neurotic, stress-related and somatoform disorders
F5 Behavioral syndromes associated with physiological disturbances and physical factors
F8 Disorders of psychological development
F9 Behavioral and emotional disorders with onset usually occurring in childhood and adolescence
eFigure 2.
Rates of different clinical pictures by diagnostic criteria
Internalizing disorders—for example, depressive or anxiety disorders
Mixed disorders—for example, combination of mood [affective] disorder and conduct disorder or combined disorder of conduct and emotions
Externalizing disorders—for example, hyperkinetic disorder, conduct disorder
In the six months before inclusion in the study, two patients in the experimental group had spent a total of 49 days in inpatient psychiatric treatment; in the control group, one patient had spent 40 days in inpatient psychiatric treatment. Similarly, no differences were seen in the outpatient setting for the same time period with regard to the number of patients receiving therapy and the numbers of sessions attended. In the 1-year period after inclusion in the study, 8 patients in the experimental group spent a total of 593 days, and 13 patients from the control group spent 865 days, as inpatients in a psychiatric ward for children and adolescents. In the same period, the participants in the experimental group used 1219 hours (of which 1191 in the intervention setting) and in the control group, 221 hours, of outpatient psychiatric/psychotherapeutic treatment (eTable 3).
eTable 3. Use of hospital school and psychopharmacotherapy.
| Manual-based multimodal treatment | Treatment as usual | |||||
|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | |
| Use of hospital school*1 | ||||||
| n | 0 | 9 | 3 | 0 | 2 | 0 |
| Psychopharmacotherapy | ||||||
| N – total | 6*2 | 5 | 8 | 4*2 | 5 | 5*2 |
| Fluoxetine | 2 | 3 | 5 | 1 | 4 | 4 |
| Citalopram | 1 | 2 | 2 | 1 | – | 1 |
| Opipramol | 1 | – | – | – | – | – |
| Methylphenidate | 2 | – | 1 | 2 | 1 | 1 |
| Atomoxetine | 1 | – | – | 1 | – | – |
*1No difference between manual-based multimodal treatment and treatment as usual at T2 or T3 regarding school use for patients
*2n = 1 with double medication
Primary study outcome
The proportion of patients who did not attend school at all in the five days preceding T1 were 60.7% for the experimental group and 57.1% for the control group (AAC). The analysis of the treatment comparison (manual-based multimodal treatment [experimental group] versus treatment as usual [control group]) shows no difference for either treatment approach in terms of the regularity of school attendance for the observed time points. This is the case for the AAC analysis (odds ratio [OR] 1.05, 95% confidence interval [CI] 0.58 to 1.90) as well as for the evaluations using LOCF or worst case assumptions (OR 0.89, 95% CI 0.50 to 1.57; and OR 0.93, 95% CI 0.55 to 1.55, respectively).
The exploratory analysis indicates a treatment effect over time: the likelihood of increasing the frequency of school attendance at T2 is 6.9 times higher in the AAC analysis than at T1 (p<0.001). The comparison between T2 and T3 shows no change in the frequency of school attendance (OR 1.2, p = 0.708). The treatment effect between T1 and T2 is also found in the analyses under LOCF and the worst case assumptions, but the probabilities are less pronounced (T1 and T2: OR 3.5, p<0.001; and OR 1.8, p = 0.009, respectively). An interaction effect—time×group—was not observed.
Additional study outcomes
The following applies for the AAC analysis and the imputation methods LOCF and MI: the exploratory analysis of the treatment comparison (manual-based multimodal treatment [experimental group] versus treatment as usual [control group]) did not show pronounced differences for either of the imputation methods. The investigation of the treatment effect over time yielded the following results for all conditions of the analysis mentioned above: the comparison between T1 and T2 showed a reduction in the severity of the psychopathology (CBCL total value, depression, anxiety, the only exception is a trend for improvement to the “anxiety” variable in the experimental group under manual-based multimodal treatment) and a notable optimization of self-efficacy. From T2 and T3, improvements were seen in the quality of family life and in self-efficacy.
The interaction effect time×group assumed a p value of p ≤ 0.05 in the AAC and LOCF analysis only for the SCL-90-R scale “depression.” Patients in the experimental group reported a slight improvement in their depressive symptoms over time (by 2.9 points) (Table 1).
Table 1. Study outcomes by measurement point (all available cases).
| Manual-based multimodal treatment | Treatment as usual | Result of proportional odds and mixed linear models | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | T1 | T2 | T3 | T1 | T2 | T3 | Group: manual-based vs treatment as usual | Time point | Interaction: time × group | |
| T2 vs T1 | T3 vs T2 | |||||||||
| School visit during preceding week*1 | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | Odds ratio (95% CI) p value of χ 2 test | Odds ratio (95% CI) p value of χ 2 test | Odds ratio (95% CI) p value of χ 2 test | p value of χ 2 test |
| None | 60.7 (34) | 18.2 (6) | 13.8 (4) | 57.1 (32) | 19.4 (7) | 19.4 (6) | 1.05 (0.58 to 1.90)p=0.875 | 6.94(3.98 to 12.12) p < 0.001 | 1.15 (0.59 to 2.24)p = 0.623 | p = 0.760 |
| Partial | 26.8 (15) | 21.2 (7) | 20.7 (6) | 23.2 (13) | 22.2 (8) | 19.4 (6) | ||||
| Regular | 12.5 (7) | 60.6 (20) | 65.5 (19) | 19.6 (11) | 58.3 (21) | 61.3 (19) | ||||
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | MD (95% CI)p of t test | MD (95% CI)p of t test | MD (95% CI)p of t test | p of t test | |
| SCL-90-R depression* 2 | 52.7 (10.2)n = 44 | 49.8 (9.6)n = 30 | 48.4 (9.1)n = 27 | 49.8 (9.9)n = 40 | 43.2 (9.0)n = 28 | 47.3 (12.9)n = 25 | 1.26(–2.71 to 5.23) p = 0.531 | –5.27(–7.28 to [–3.26]) p < 0.001 | 1.85(–0.24 to 3.94) p = 0.083 | p = 0.018 |
| SCL-90-R anxiety *2 | 47.9 (10.7)n = 44 | 48.0 (11.4)n = 30 | 46.6 (10.2)n = 27 | 49.0 (10.7)n = 40 | 43.8 (9.7)n = 28 | 47.0 (12.8)n = 25 | –0.28 (–4.35 to 3.80) p = 0.893 | –3.37 (–5.77 to [–0.97]) p = 0.006 | 1.40 (–1.38 to 4.19) p = 0.320 | p = 0.434 |
| CBCL total score*3 | 64.5 (7.1)n = 51 | 56.6 (10.0)n = 38 | – | 65.3 (7.7)n = 50 | 56.6 (11.2)n = 38 | – | –0.10 (–3.11 to 2.92) p = 0.950 | –8.3 (–10.56 to 6.06) p < 0.001 | – | p = 0.923 |
| KINDL family climate*4 | 75.1 (18.1)n = 55 | 77.2 (24.2)n = 34 | 85.3 (14.2)n = 29 | 70.9 (22.3)n = 55 | 75.4 (22.1)n = 35 | 82.1 (20.5)n = 31 | 4.91 (–1.73 to 11.54) p = 0.145 | 3.82 (–1.28 to 8.92) p = 0.140 | 7.46 (1.94 to 12.99)p = 0.009 | p = 0.988 |
| GSE*4 | 15.1 (5.0)n = 47 | 18.0 (4.7)n = 31 | 20.5 (3.8)n = 27 | 15.6 (5.3)n = 44 | 18.9 (6.3)n = 29 | 20.2 (4.9)n = 27 | –0.34 (–2.15 to 1.47) p = 0.711 | 3.39 (2.20 to 4.59)p < 0.001 | 1.42 (0.21 to 2.63)p = 0.022 | p = 0.461 |
n, sample size; M, mean value; SD, standard deviation; MD, mean difference; 95% CI, confidence interval; p, p value (two-sided); SCL-90-R, symptom checklist-90-revised; CBCL, child behaviour checklist 4–18; KINDL-R, questionnaire to document children’s health-related quality of life; GSE, general self efficacy
*1Proportion of school avoiders who during the observation week were documented as having “no(ne)“ (<10%). “partial“ (≥ 10%, and < 90%) or “regular“ (≥ 90%) school visits. Students who regularly attended school at T 1 had regularly avoided lessons in the preceding 25 weeks.
*2Mean
*3Mean T score
*4Mean scale sum score
Discussion
As far as we are aware, this study is the first randomized controlled evaluation of the effectiveness of a multimodal, behavioral therapy–based treatment approach for school avoiders with a wide spectrum of diagnoses.
Limitations
In spite of not reaching our originally intended sample size because of the high screening dropout rate, the sample size is high compared with the cited RCTs. The distribution of the primary outcome variable (accumulation at 0 and 100%) had not been expected a priori in this form and therefore necessitated a change to our evaluation strategy, which indicates a reduced power of our study design because of the lower scaling level.
The limitations that reduce the representativeness of our study include the proportion of patients who dropped out of the screening (29.2% out of N = 247). It is possible that the low potential for change or a low motivation among some school avoiders requires that these students be visited on an outpatient basis (home visits, for example). The rapid chronification of school avoidance (32) is the reason for the absence of a waiting list group; however, King et al. (13) showed an improvement in rates of school attendance for CBT patients compared with waiting list patients, in whom school attendance rates did not change.
The dropout rate between follow-up points of 44.6% in the experimental group and 48.2% in the control group, 12 months after T1, may lead to biased results. The fact that no significant differences were found between patients who adhered to the study and those who dropped out could possibly be explained with a lower number of cases or a reduced power of the test. According to the available studies to date, we can assume that the extent of school avoidance in patients who were not reached by the follow-up remained the same (see for example [13]). Even so, we analyzed our data using a number of different assumptions and imputation methods. The most conservative assumption (worst case) assumed that patients who did not attend follow-up did not attend school at all.
Results for outcome variables
Contrary to expectations, no between-group differences were seen for the primary outcome. The results of the present study are therefore consistent with those reported by Last et al. (14) and Heyne et al. (15), who similarly did not find any differences between different treatment approaches. The data analysis under intention-to-treat (ITT) conditions possibly leads to a leveling-out of possibly existing differences between groups. Under all assumptions, the school attendance rate increases, especially in the first 6 months after the start of the treatment. It is possible that the odds of regular school attendance are subject to overestimates under the AAC assumption and to underestimates under the conservative worst case assumption. The LOCF analysis showed 3.5 times higher odds of attending school regularly again during the study period.
Under the supposition that 90% attendance at school can be classified as normal (13, 33), the proportion of school attenders in this study increased from 12.5% to 65.5% (experimental group, AAC, T1–3). These values are roughly consistent with the data from a meta-analysis of psychosocial interventions by Pina et al. (34) and in the three RCTs mentioned earlier, with the exception of the study reported by King et al. ([13], Table 2). In our study, 34 and 8 patients in the experimental group, and 36 and 13 patients in the control group, received outpatient or inpatient treatment in the year under observation.
Table 2. Comparison of randomized controlled trials investigating the treatment of school avoidance.
| King et al., 1998 (13) | Last et al., 1998 (14) | Heyne et al., 2002 (15) | Reissner et al. | |
|---|---|---|---|---|
| N (total) | 34 | 56 | 61 | 112 |
| Predominant type of disorder | Internalizing | Internalizing | Internalizing(Mixed) | InternalizingExternalizing Mixed |
| “Screening failures”*1 | Not reported | 47% | 27.4% | 54.7% |
| Dropout rate | 0% | 29% | 5% | 46.4% |
| Observation period | 3 months | 3.5 months | 4.5 months | 12 months |
| Response criterion | ≥ 95% school attendance | ≥ 95% school attendance | ≥ 90% school attendance | ≥ 90% school attendance |
| Response rate CBT | 82.3% | 65% | 60.3% | 65.5% (MT, AAC) |
| Differences between groups | CBT > waiting list*2 | CBT = psychoeducation | CBT = PTT = CBT+PTT | MT = TAU |
*1, potential
*2, higher school attendance rate in patients in CBT group
CBT, cognitive behavioral therapy; PTT, parent–teacher training; MT, manual-based multimodal treatment; TAU, treatment as usual; AAC, all available cases
Notable improvements were also seen for the additional outcomes in both groups, as early as in the first 6 months. Similarly to the study reported by Last et al. (14), the reduction of depressive symptoms over time was more pronounced in the experimental group. As the effect size of this difference in trend in the experimental group is small (Cohen’s d = 0.3), the results should be interpreted with caution.
Conclusion
The study shows at best a slight advantage for the patients treated according to the manual—with nominally, but not substantially, reduced healthcare costs in the first year under inclusion in the study (manual-based multimodal treatment: about €7200; treatment as usual: about €9300); Weschenfelder et al., in preparation). In addition to the analysis of conditional factors for a successful return to school, future RCTs with larger sample sizes are needed, in order better to understand the complexity of the issue. In order to increase effectiveness and lower costs, differential indications for outpatient versus inpatient treatment would be desirable.
Key Messages.
In all available studies including our own, 60–65% of school avoiders participated regularly in lessons after undergoing behavioral therapy; a similar proportion also attended school 12 months later.
The fact that only 35–40% of patients still did not, or only partially, attend school underlines the persistence of the problem, as well as the individual, familial, and societal implications.
To avoid chronification of the problem, affected parents should seek regular contact with teachers early on and initiate the diagnostic evaluation by a child and adolescent psychiatrist. The parents and the professional support system should not be discouraged by short-term setbacks during the course of the treatment.
Closer, structured cooperation between parents, school, youth services, the public order office, and child and adolescent psychiatrists might improve results. Schools as well as pediatricians and general practitioners in private practice should be supported to be able to provide optimized and more rapid diagnoses.
Because of the high non-participation rate in the treatment it may be concluded that low-threshold support services (for example, home visits with counseling) and more differentiated approaches of child and adolescent psychiatric treatment are required.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
The reported study was registered with the German Clinical Trials Register (DRKS-ID: DRKS00000738). The authors thank the federal state of North Rhine–Westphalia and the European Union for financial support (GW 187). Special thanks from the authors for realizing the study go to: H. Frey, J. Helmig, S.Kiessling, S. Mushoff-Küchenmeister, M. Schmitz, C. Ose, S. Spie, P. Vasen und A. Wertgen, as well as the collaborating child and adolescent psychiatrists.
Footnotes
Conflict of interest statement
Dr. Dr. Reissner, Professor Hebebrand, and Dr. Kollmann are the editors of the therapy manual evaluated in this study. The manual is published by Kohlhammer Verlag.
The remaining authors declare that no conflict of interest exists.
References
- 1.Steiner M, Wagner E. Dropoutstrategie. Grundlagen zur Prävention und Reintegration von Dropouts in Ausbildung und Beschläftigung. Wien. Institut für höhere Studien. 2007 [Google Scholar]
- 2.Flakierska N, Lindstrom M, Gillberg C. School refusal: A 15-20-year follow-up study of 35 Swedish urban children. Compr Psychiatry. 1997;38:17–22. doi: 10.1192/bjp.152.6.834. [DOI] [PubMed] [Google Scholar]
- 3.Farrington D. Later life outcomes of truants in the Cambridge study. In: Berg I, Nursen J, editors. Unwillingly to school. London: Gaskell; 1996. pp. 96–116. [Google Scholar]
- 4.Jans T, Warnke A. Schulverweigerung. Monatsschr Kinderheilkd. 2004;152:13002–13012. [Google Scholar]
- 5.Wagner M, Dunkake I, Weiß B. Schulverweigerung. Empirische Analysen zum abweichenden Verhalten von Schülern. Kölner Zeitschrift für Soziologie und Sozialpsychiatrie. 2004;56:457–489. [Google Scholar]
- 6.Knollmann M, Knoll S, Reissner V, Metzelaars J, Hebebrand J. School avoidance from the point of view of child and adolescent psychiatry: symptomatology, development, course, and treatment. Dtsch Arztebl Int. 2010;107:43–49. doi: 10.3238/arztebl.2010.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Egger HL, Costello EJ, Angold A. School refusal and psychiatric disorders: a community study. J Am Acad Child Adolesc Psychiatry. 2003;42:797–807. doi: 10.1097/01.CHI.0000046865.56865.79. [DOI] [PubMed] [Google Scholar]
- 8.Lehmkuhl U, Lehmkuhl G. Schulverweigerung - ein heterogenes Störungsbild. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2004;47:890–895. doi: 10.1007/s00103-004-0899-z. [DOI] [PubMed] [Google Scholar]
- 9.Walter D, Hautmann C, Rizk S, et al. Short term effects of inpatient cognitive behavioral treatment of adolescents with anxious-depressed school absenteeism: an observational study. Eur Child Adolesc Psychiatry. 2010;19:835–844. doi: 10.1007/s00787-010-0133-5. [DOI] [PubMed] [Google Scholar]
- 10.Heyne D, Sauter FM, Van Widenfelt BM, Vermeiren R, Westenberg PM. School refusal and anxiety in adolescence: non-randomized trial of a developmentally sensitive cognitive behavioral therapy. J Anxiety Disord. 2011;25:870–878. doi: 10.1016/j.janxdis.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Maric M, Heyne DA, MacKinnon DP, van Widenfelt BM, Westenberg PM. Cognitive mediation of cognitive-behavioural therapy outcomes for anxiety-based school refusal. Behav Cogn Psychother. 2013;41:549–564. doi: 10.1017/S1352465812000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bandura A. Exercise of personal agency through the self-efficacy mechanism. In: Schwarzer R, editor. Self-Efficacy Thought Control of Action. Washington: DC Hemisphere; 1992. [Google Scholar]
- 13.King NJ, Tonge BJ, Heyne D, et al. Cognitive-behvioral treatment of school-refusing children: A controlled evaluation. J Am Acad Child Adolesc Psychiatry. 1998;37:395–403. doi: 10.1097/00004583-199804000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Am Acad Child Adolesc Psychiatry. 1998;37:404–411. doi: 10.1097/00004583-199804000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Heyne D, King NJ, Tonge BJ, et al. Evaluation of child therapy and caregiver training in the treatment of school refusal. J Am Acad Child Adolesc Psychiatry. 2002;41:687–695. doi: 10.1097/00004583-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Pahlke F, König IR, Ziegler A. Randomization In Treatment Arms (RITA): Ein Randomisierungsprogramm für klinische Studien. Informatik, Biometrie und Epidemiologie in Medizin und Biologie. 2004;35:1–22. [Google Scholar]
- 17.Reissner V, Hebebrand J, Knollmann M, editors. Multimodale Interventionen für psychisch belastete Schulvermeider - das Essener Manual. Stuttgart: Kohlhammer; 2015. Beratung und Therapie bei schulvermeidendem Verhalten. in press. [Google Scholar]
- 18.Joormann J, Unnewehr S. Göttingen: Hogrefe; 2002. Behandlung der Sozialen Phobie bei Kindern und Jugendlichen. [Google Scholar]
- 19.Döpfner M, Schürmann S, Frölich J. THOP. Weinheim: Beltz-PVU; 2002. Therapieprogramm für Kinder mit hyperkinetischem und oppositionellem Problemverhalten. [PubMed] [Google Scholar]
- 20.Achenbach TM. Burlington: University of Vermont Department of Psychiatry; 1991. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. [Google Scholar]
- 21.Greenhill LL, Pine D, March J, Birmaher B, Riddle M. Assessment issues in treatment research of pediatric anxiety disorders: what is working, what is not working, what is missing, and what needs improvement. Psychopharmacol Bull. 1998;34:155–164. [PubMed] [Google Scholar]
- 22.Derogatis LR, Rickels K, Rock AF. The SCL-90 and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry. 1976;128:280–289. doi: 10.1192/bjp.128.3.280. [DOI] [PubMed] [Google Scholar]
- 23.Lambert MJ, Hill CE. Assessing psychotherapy outcomes and processes. In: Bergin AE, Garfield SL, editors. Handbook of psychotherapy and behavior change. Oxford, UK: John Wiley & Sons; 1994. pp. 72–113. [Google Scholar]
- 24.Spitzer C, Hammer S, Lowe B, et al. The short version of the Brief Symptom Inventory (BSI-18): preliminary psychometric properties of the German translation. Fortschr Neurol Psychiatr. 2011;79:517–523. doi: 10.1055/s-0031-1281602. [DOI] [PubMed] [Google Scholar]
- 25.Jerusalem M, Schwarzer R. Selbstwirksamkeit. In: Schwarzer R, editor. Skalen zur Befindlichkeit und Persönlichkeit Forschungsbericht 5. Berlin: Institut für Psychologie, Pädagogische Psychologie, Freie Universität Berlin; 1986. [Google Scholar]
- 26.Schwarzer R, Scholz U. Cross-cultural assessment of coping resources: the general perceived self-efficacy scale. http://userpage.fu-berlin.de/gesund/publicat/world_data.htm. (last accessed on 1 October 2003). [Google Scholar]
- 27.Ravens-Sieberer U. Der Kindl-R Fragebogen zur Erfassung der gesundheitsbezogenen Lebensqualität bei Kindern und Jugendlichen - Revidierte Form. In: Schumacher J, Brähler E, editors. Diagnostische Verfahren zu Lebensqualität und Wohlbefinden. Göttingen: Hogrefe; 2003. pp. 184–148. [Google Scholar]
- 28.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 29.Verbeke G, Molenberghs G. New York: Springer; 2000. Linear Mixed Models for longitudinal data. [Google Scholar]
- 30.Little RJA, Rubin DB. New York: John Wiley & Sons; 1987. Statistical analysis with missing data. [Google Scholar]
- 31.Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomized Trials. Ann Intern Med. 2010;152:1–7. doi: 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 32.Lyon A, Cotler S. Toward reduced bias and increased utility in the assessment of school refusal behavior: The case for diverse samples and evaluations of context. Psychol Sch. 2007;33:551–565. [Google Scholar]
- 33.Kearney CA, Silverman WK. A preliminary analysis of a functional model of assessment and treatment for school refusal behavior. Behav Modif. 1990;14:340–366. doi: 10.1177/01454455900143007. [DOI] [PubMed] [Google Scholar]
- 34.Pina AA, Zerr AA, Gonzales NA, Ortiz CD. Psychosocial interventions for school refusal behavior in children and adolescents. Child Dev Perspect. 2009;3:11–20. doi: 10.1111/j.1750-8606.2008.00070.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schneider S, Unnewehr S, Margraf J. Berlin: Springer; 2009. Diagnostisches Interview bei psychischen Störungen im Kindes- und Jugendalter. [Google Scholar]
- 36.Winkler J, Stolzenberg H. Der Sozialschichtindex im Bundesgesundheitssurvey. Gesundheitswesen. 1999;61:178–183. [PubMed] [Google Scholar]