Abstract
Rationale: State-specific case numbers and costs are critical for quantifying the burden of pulmonary nontuberculous mycobacterial disease in the United States.
Objectives: To estimate and project national and state annual cases of nontuberculous mycobacterial disease and associated direct medical costs.
Methods: Available direct cost estimates of nontuberculous mycobacterial disease medical encounters were applied to nontuberculous mycobacterial disease prevalence estimates derived from Medicare beneficiary data (2003–2007). Prevalence was adjusted for International Classification of Diseases, 9th Revision, undercoding and the inclusion of persons younger than 65 years of age. U.S. Census Bureau data identified 2010 and 2014 population counts and 2012 primary insurance-type distribution. Medical costs were reported in constant 2014 dollars. Projected 2014 estimates were adjusted for population growth and assumed a previously published 8% annual growth rate of nontuberculous mycobacterial disease prevalence.
Measurements and Main Results: In 2010, we estimated 86,244 national cases, totaling to $815 million, of which 87% were inpatient related ($709 million) and 13% were outpatient related ($106 million). Annual state estimates varied from 48 to 12,544 cases ($503,000–$111 million), with a median of 1,208 cases ($11.5 million). Oceanic coastline states and Gulf States comprised 70% of nontuberculous mycobacterial disease cases but 60% of the U.S. population. Medical encounters among individuals aged 65 years and older ($562 million) were twofold higher than those younger than 65 years of age ($253 million). Of all costs incurred, medications comprised 76% of nontuberculous mycobacterial disease expenditures. Projected 2014 estimates resulted in 181,037 national annual cases ($1.7 billion).
Conclusions: For a relatively rare disease, the financial cost of nontuberculous mycobacterial disease is substantial, particularly among older adults. Better data on disease dynamics and more recent prevalence estimates will generate more robust estimates.
Keywords: cost analysis, epidemiology, nontuberculous mycobacteria, pulmonary
The prevalence of pulmonary nontuberculous mycobacterial disease (NTM) is increasing in the United States (1, 2), with notable variation by geographic region (1). Both host and climatic factors are associated with disease (1, 3–6). Host factors related to increased disease susceptibility include preexisting disease (e.g., bronchiectasis, rheumatoid arthritis, chronic obstructive pulmonary disease), age, race and/or ethnicity, and sex (1, 7). Although a relatively rare disease, NTM is an important cause of morbidity among older adults, particularly women (1). Because NTM is not a reportable condition, other approaches have been used to estimate disease burden, including analysis of large datasets using International Classification of Diseases, 9th Revision (ICD-9), codes (1, 8) and laboratory-based studies (2, 9). However, these measures have their own limitations and may over- or underestimate disease burden (1, 2, 9). The chronic and slowly progressive nature of the disease, with required treatment of at least 12–18 months, leads to costly prescription medications and recurring hospital visits as a result of relapse or reinfection (10–14).
National direct cost estimates of NTM encounters based on health care claims and hospital discharge databases have been published, including costs of hospitalization and outpatient visits as well as prescription medications (2004–2007) (15). However, state-specific estimates of the total NTM disease burden, including case numbers and costs, are currently lacking. Our objectives are to estimate national and state-specific numbers of NTM cases with associated health care costs and to project case estimates and costs through 2014. These estimates will highlight the absolute burden of NTM and facilitate local clinical and public health planning. Preliminary results of this study were previously reported in the form of an abstract (16).
Methods
To generate annual estimates of national and state-specific NTM case numbers and associated costs, we conducted a literature search through the National Library of Medicine (PubMed) database to identify published national prevalence and cost estimates for NTM in the United States. We identified two articles with relevant U.S. cost estimates, including annual inpatient and outpatient visit costs and prescription medication expenditures (15, 17). For prevalence estimates, we relied on the estimates generated from our previous national NTM studies using Medicare and national survey data (1, 18).
NTM Case Estimates
For generating annual case numbers for persons aged 65 years and older, we relied on state-specific NTM prevalence data generated from a 5% sample of Medicare Part B beneficiaries based on ICD-9 coding. The 2003–2007 average annual prevalence was applied to 2010 census data to obtain conservative 2010 case estimates (1). For case estimates among persons younger than 65 years of age, we used the age distribution of cases from a previously published survey of NTM treatment (18) and applied this proportion to the estimated cases among persons aged 65 years and older to obtain the case numbers for persons younger than 65 years of age. Specifically, we estimated that 31% of all NTM patients are younger than 65 years old (18). For example, if we found that a state had 500 annual NTM cases of patients 65 years of age and older, that state was estimated to have 225 cases of patients younger than 65 years old. In addition, because it is estimated that only 27% of microbiologically confirmed cases are coded with the ICD-9 code for pulmonary NTM (031.0), meaning that 73% of these cases are missed when relying on ICD-9 coding alone, we further adjusted our Medicare prevalence estimates to account for this. Specifically, our final estimates were generated by increasing existing prevalence estimates by 73% (2). For example, if ICD-9 coding identified 100 cases of NTM, we estimated 370 cases of NTM to truly exist. The national annual case estimates were derived by summing state estimates. The District of Columbia is omitted from this analysis owing to insufficient data.
NTM Cost Estimates
Cost estimates obtained from published articles included the annual cost per medical encounter of NTM, including prescription medication costs and the annual cost of prescription medications per patient. Medical care consumer price index data from the Bureau of Labor Statistics were used to adjust nominal published and estimated costs to reflect constant 2014 U.S. dollars (19). Collier and colleagues provided data on the number of medical encounters (defined as one episode of admission) and payment costs, including prescription medications, dependent on type of NTM-related medical encounter (hospitalizations vs. outpatient visits) and insurance provider (private, Medicaid, or Medicare) (15). Using these data, we estimated the proportion of inpatient versus outpatient encounters for each insurance provider. Uninsured and alternative insurance provider (i.e., TRICARE) costs were excluded from our cost estimates owing to insufficient data. U.S. Census Bureau data from 2012 identified the distribution of primary health insurance types among state residents, and the annual national and state-specific NTM costs were calculated by weighting the generated case counts by insurance type and applying the proportional cost of hospitalizations and outpatient visits (15). These cost estimates therefore reflect only one NTM medical encounter per person per year and do not include additional costs incurred for recurrence of infection or multiple inpatient or outpatient medical encounters per person in a given year. Data from an additional single-site natural history cohort provided median monthly and annual costs of prescription medications per patient, which were used to estimate the proportion of prescription medication costs in this analysis (17).
Sensitivity Analysis for Case and Cost Estimates
Our estimates relied on two key assumptions: (1) 73% of cases are missed when relying on ICD-9 coding, and (2) 31% of all NTM patients are younger than 65 years old. Therefore, we conducted a sensitivity analysis by varying these factors to determine their impact on our overall national estimates. For ICD-9 undercoding, we calculated a national case and cost estimate using a 50% and 25% undercoding adjustment. Similarly, we calculated the national case and cost estimates should the patients younger than 65 years of age actually represent 25% and 35% of all NTM cases. Additional case and cost discrepancies occur as a result of the increasing prevalence of NTM and likelihood of an individual to have more than one medical encounter in a given year. We also applied an 8.2% annual growth rate of NTM prevalence, as identified in our previous study, to our 2005 estimated population prevalence (midpoint of 2003–2007 average annual prevalence adjusted for undercoding of 73% of cases and assuming 31% of all patients are younger than 65 years old) and used 2014 U.S. Census Bureau population data to calculate projected case and cost estimates through 2014 (1). Additionally, in consideration of the chronic nature of NTM, we provided national case and cost estimates that accounted for one to three additional outpatient visits for each medical encounter in a given year.
Results
National Estimates
Assuming no increase in annual NTM prevalence from 2005 to 2010, a total of 86,244 NTM cases were estimated in the United States for 2010 with an associated annual cost of $815 million, resulting in an average cost per medical encounter of $9,451. The annual cost of inpatient encounters was $709 million (87% of all costs) and was $106 million (13% of all costs) for outpatient encounters. The annual cost of prescription medication alone was estimated at $617 million, or 76% of all associated costs across all encounter settings. Of all NTM costs, $562 million was attributable to adults 65 years of age and older, twofold higher than the $253 million cost among adults younger than 65 years old.
State-specific and Regional Estimates
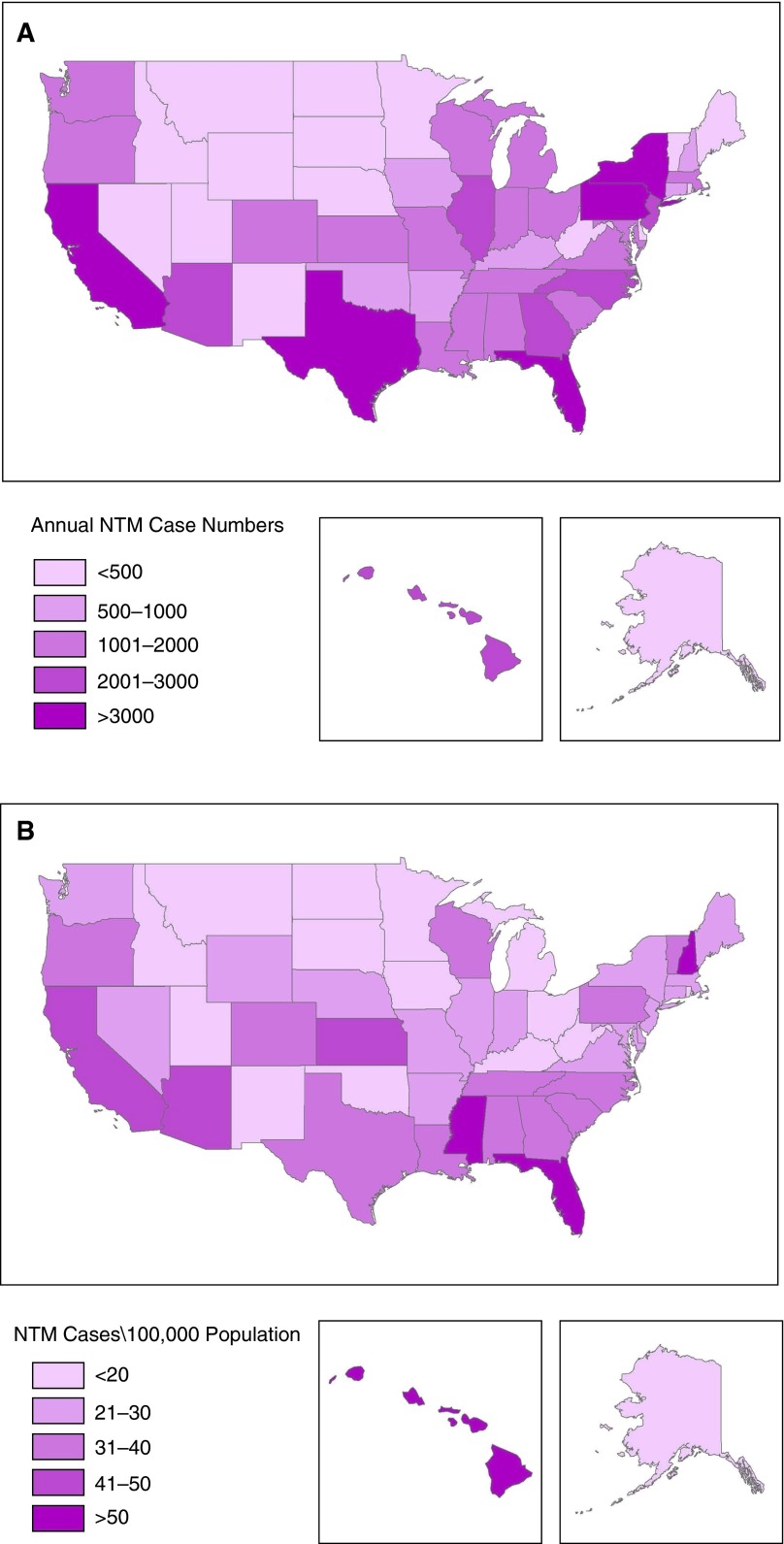
Overall, the median number of cases estimated for 2010 was 1,208 per state, ranging from 48 cases in North Dakota to 12,544 cases in California (Table 1). Similarly, the annual costs per state varied greatly, from $513,000 to $111 million per year. In general, case numbers were higher in coastal and southeastern states than in landlocked states (Figure 1). California, Florida, Texas, New York, and Pennsylvania had the highest number of cases (range, 3,969–12,544 cases), which, when combined, encompassed 44% of the annual costs in the United States. In contrast, the states with the lowest number of cases per year were North Dakota, South Dakota, Montana, Alaska, and Wyoming (range, 48–105 cases per year). The estimated annual number of cases in Hawaii was 2,131, the 10th highest state case count, despite its having the 10th smallest population size of the 50 states.
Table 1.
State-specific annual cases and cost of pulmonary nontuberculous mycobacterial disease in the United States (2010)
| State | Total 2010 Cases* | Rank of State Population (Largest to Smallest) | Cases per 100,000 Population | Annual Cost† |
|---|---|---|---|---|
| California | 12,544 | 1 | 44.5 | $110,690,528 |
| Florida | 11,580 | 4 | 53.6 | $98,527,193 |
| Texas | 6,792 | 2 | 39.4 | $54,983,825 |
| New York | 5,055 | 3 | 29.1 | $48,600,779 |
| Pennsylvania | 3,969 | 6 | 30.5 | $41,312,486 |
| North Carolina | 2,890 | 10 | 35.3 | $26,071,179 |
| Arizona | 2,859 | 16 | 48.9 | $24,664,441 |
| Illinois | 2,643 | 5 | 24.8 | $26,361,795 |
| Georgia | 2,365 | 9 | 34.5 | $20,847,084 |
| Hawaii | 2,131 | 40 | 164.6 | $21,800,504 |
| New Jersey | 2,055 | 11 | 26.1 | $20,973,701 |
| Wisconsin | 1,947 | 20 | 37.8 | $20,330,793 |
| Tennessee | 1,858 | 17 | 32.8 | $17,165,448 |
| Virginia | 1,731 | 12 | 26.7 | $17,502,520 |
| South Carolina | 1,672 | 24 | 39.9 | $16,121,152 |
| Missouri | 1,623 | 18 | 29.2 | $16,252,708 |
| Louisiana | 1,423 | 25 | 38.5 | $12,712,661 |
| Alabama | 1,411 | 23 | 32.3 | $13,450,119 |
| Ohio | 1,405 | 7 | 13.1 | $14,040,923 |
| Colorado | 1,335 | 22 | 36.6 | $13,209,552 |
| Washington | 1,332 | 13 | 24.3 | $12,697,994 |
| Indiana | 1,329 | 15 | 23.8 | $13,153,847 |
| Mississippi | 1,312 | 31 | 52.0 | $11,542,996 |
| Michigan | 1,247 | 8 | 13.8 | $13,192,603 |
| Massachusetts | 1,236 | 14 | 20.6 | $13,332,548 |
| Oregon | 1,181 | 27 | 33.4 | $11,388,940 |
| Maryland | 1,043 | 19 | 22.2 | $10,849,856 |
| Kansas | 1,039 | 33 | 41.6 | $10,447,033 |
| Connecticut | 850 | 29 | 25.3 | $9,102,625 |
| Arkansas | 772 | 32 | 27.7 | $6,486,736 |
| Oklahoma | 635 | 28 | 18.9 | $5,664,779 |
| New Hampshire | 625 | 42 | 52.9 | $6,595,683 |
| Iowa | 599 | 30 | 20.0 | $6,270,923 |
| Kentucky | 594 | 26 | 15.5 | $5,414,209 |
| Nevada | 447 | 35 | 20.8 | $3,854,280 |
| Minnesota | 421 | 21 | 9.3 | $4,613,055 |
| Maine | 382 | 41 | 27.3 | $3,806,463 |
| Nebraska | 336 | 38 | 20.6 | $3,495,265 |
| Utah | 237 | 34 | 14.3 | $2,355,140 |
| Idaho | 221 | 39 | 17.1 | $2,127,479 |
| Delaware | 217 | 45 | 25.3 | $2,133,709 |
| Vermont | 204 | 49 | 33.7 | $2,110,627 |
| New Mexico | 147 | 36 | 8.1 | $1,220,242 |
| Rhode Island | 119 | 43 | 11.8 | $1,186,009 |
| West Virginia | 116 | 37 | 5.9 | $1,105,662 |
| Wyoming | 105 | 50 | 22.6 | $1,053,977 |
| Alaska | 60 | 47 | 16.4 | $519,845 |
| Montana | 53 | 44 | 5.4 | $502,927 |
| South Dakota | 50 | 46 | 6.5 | $506,019 |
| North Dakota | 48 | 48 | 7.4 | $512,820 |
| U.S. total | 86,244 | n.a. | 27.9 | $815,098,690 |
Estimates represent entire population, reflect a 73% International Classification of Diseases, 9th Revision, undercoding adjustment, and assume 31% of nontuberculous mycobacterial disease cases of patients aged <65 yr in 2010. The District of Columbia is omitted from analysis owing to insufficient data.
Costs are presented in constant 2014 dollars.
Figure 1.
(A) Case number estimates of pulmonary nontuberculous mycobacterial disease (NTM) in the United States across all age groups, adjusted for International Classification of Diseases, 9th Revision (ICD-9), undercoding, 2010. (B) Prevalence (cases/100,000 population) estimates of pulmonary NTM in the United States across all age groups, adjusted for ICD-9 undercoding, 2010.
Sensitivity Analysis
Assuming 31% of patients are younger than 65 years old and using undercoding adjustments of 25% and 50% applied to the national case estimates resulted in totals of 30,933 ($292 million) and 46,399 ($439 million) cases in 2010, respectively (Table 2). Assuming that 27% of cases were coded according to ICD-9 for pulmonary NTM and that individuals younger than 65 years old comprised 25% and 35% of all NTM cases, the number of cases and costs were estimated at 79,344 cases ($750 million) and 91,551 cases ($865 million) per year, respectively (Table 2). In addition, we previously estimated an annual increase in NTM prevalence of 8.2% (1). On the basis of this figure, we projected national case numbers of NTM to be 181,037 in 2014, with an associated annual cost of $1.7 billion. Further, accounting for the likelihood that an individual with NTM will have more than one outpatient visit in a given year, national case and cost estimates of multiple outpatient visits are provided. One additional outpatient visit for each medical encounter (inpatient or outpatient visits) increases annual cost to $937 million (172,487 annual medical encounters), and three additional outpatient visits results in $1.2 billion (344,974 annual medical encounters) in a given year (Table 3).
Table 2.
Sensitivity of national pulmonary nontuberculous mycobacterial disease cases* and cost† estimates to ICD-9 undercoding and proportion of patients aged <65 years
| Proportion of Cases Coded for Pulmonary Nontuberculous Mycobacterial Disease per ICD-9 (031.0) | |||
|---|---|---|---|
| Proportion of patients aged <65 yr | 27% | 50% | 75% |
| 25% | 79,344 ($749,890,795) | 42,687 ($403,441,248) | 28,458 ($268,960,832) |
| 31% | 86,244 ($815,098,690) | 46,399 ($438,523,095) | 30,933 ($292,348,730) |
| 35% | 91,551 ($865,258,610) | 49,254 ($465,509,132) | 32,836 ($310,339,421) |
Definition of abbreviations: ICD-9 = International Classification of Diseases, 9th Revision.
Case numbers reflect year 2010 estimates.
Costs are presented in constant 2014 dollars.
Table 3.
Sensitivity of national pulmonary nontuberculous mycobacterial disease case and cost estimates to the number of annual outpatient visits per person
| National Nontuberculous Mycobacterial Disease Estimates | National Nontuberculous Mycobacterial Disease Estimates Assuming 1 Additional Outpatient Visit per Year | National Nontuberculous Mycobacterial Disease Estimates Assuming 2 Additional Outpatient Visits per Year | National Nontuberculous Mycobacterial Disease Estimates Assuming 3 Additional Outpatient Visits per Year | |
|---|---|---|---|---|
| Annual medical encounters* | 86,244 | 172,487 | 258,731 | 344,974 |
| Annual cost† | $815,098,690 | $937,491,959 | $1,059,885,228 | $1,182,278,496 |
Medical encounters reflect a 73% International Classification of Diseases, 9th Revision, undercoding adjustment and assume 31% of nontuberculous mycobacterial disease patients were aged <65 yr in 2010.
Costs are presented in constant 2014 dollars.
Discussion
This study provides the first-ever state-specific NTM case and cost estimates for the entire United States, based on a nationally representative sample and including adjustment for ICD-9 undercoding. Although NTM is a relatively rare disease, the associated financial burden in the United States is substantial, particularly in the older adult population. Our 2010 national annual case and cost estimates, at 86,244 NTM cases and a total cost of $815 million, surpass those described in previous studies (15). Nearly 80% of this financial burden is attributed to high prescription medication costs, which are due in part to the generally chronic nature of this disease and associated with intensive recommended antibiotic treatment regimens of at least three antibiotics for a minimum of 12–18 months (20). Further, given that inpatient and outpatient cost estimates were based on one medical encounter per year per patient, the actual financial burden of NTM is likely far greater (Table 3), again owing to the chronic, complicated nature of this disease for a high proportion of patients.
We identified two previous studies in which authors reported cost estimates. In a retrospective analysis (2004–2005) of antibiotic use among 27 patients with NTM enrolled in a single-site, natural history cohort, researchers found median monthly medication costs of $596 (range, $4–$2,573; $7,157 annually) per patient (17). Additional direct costs of NTM were excluded (i.e., administration of intravenous antibiotics, outpatient visits, nursing care). These costs were greater than those found in a Canadian retrospective chart review (2003–2008) of patients with NTM that found median monthly medication costs of approximately $314, encompassing approximately 70% of the NTM treatment costs (21). Our own estimates resulted in prescription medications, independent of additional expenses, costing $617 million, approximately 76% of NTM direct costs. A second national analysis accounted for direct costs in addition to prescription medication costs derived from health care claims and hospital discharge databases, and the researchers found a mean cost per hospitalization of $32,000 and annual hospitalization costs of $241 million (7,659 hospitalizations per year) (15). We believe our findings provide a more accurate assessment of NTM disease burden in the United States by accounting for ICD-9 undercoding, all direct costs, and a geographically representative sample encompassing all ages.
We found the highest case numbers in the states with the highest prevalence, as these also happen to be the states with some of the largest population sizes (1, 2, 8). These states also happen to be located in southeastern and coastal regions of the United States, areas with climatic conditions associated with increased NTM risk (Figure 1) (4, 5). States with oceanic coastlines, including the Gulf States, encompass approximately 60% of the U.S. population and 70% of annual NTM cases, whereas landlocked and Great Lakes states comprise 46% of the population but only 36% of the annual cases. Gulf States had the greatest variations between percentage of U.S. population (18%) and percentage of U.S. NTM cases (26%), followed by southeastern states (25% of population vs. 32% of NTM cases).
In addition to case and cost estimates, we provide state-specific prevalence rates representative of the entire population (Table 1). Certain states, such as Hawaii, Mississippi, Florida, and Arizona, had a high number of NTM cases relative to state population size, likely reflecting a combination of host and environmental risk factors in these regions. Regional differences may also be due in part to differences in NTM species distributions. In a previous analysis of spatial clustering among patients with cystic fibrosis, investigators found that the proportion of patients with positive NTM cultures due to Mycobacterium abscessus versus Mycobacterium avium complex varied geographically, with 80–100% of isolates identified as M. abscessus in Hawaii, Louisiana, and Oregon (22). Median annual treatment costs of M. abscessus infections ($14,626) are reported to be over twofold higher than M. avium complex infections ($6,443) (17, 21). Therefore, reported costs in certain regions and states with greater burdens of M. abscessus infections may be even higher than reported here, especially relative to areas with NTM due predominantly to M. avium complex.
Our estimated direct cost per medical encounter for NTM ($9,451) is comparable to other prevalent chronic and infectious diseases in the United States. Ballarino and colleagues believe NTM medication costs may be comparable to the costs of other chronic diseases of infectious origins, such as multidrug-resistant tuberculosis (reported average direct costs per patient of $5,113) (17, 23). Some chronic conditions may be comparable as well. For example, mean simple inpatient admissions (no intubation or intensive care unit stay) for chronic obstructive pulmonary disease were estimated to cost $8,659 per patient (mean costs vary from $774 for emergency department visits to $53,694 for intensive care admissions) (24). Still, it is important to note that the cost per medical care encounter for NTM likely varies greatly at the patient level, depending on the NTM species and comorbid conditions present.
We projected national NTM cases to increase to an estimated 181,037 cases in 2014, with an associated cost of $1.7 billion. These projections represent the increasing burden of NTM in the United States. However, systematic, ongoing disease monitoring of NTM would provide more robust epidemiologic data on national disease prevalence, allowing an opportunity to fully assess trends, specifically by species of mycobacteria, host factors, and geography, in addition to the financial impact of NTM in the United States.
Although our NTM case estimates are based on the most reliable population-level data currently available, our cost estimates likely underestimate the true financial burden of NTM, owing to several limitations. The lack of standardized nationwide data on NTM patient and treatment practices limited our ability to precisely estimate the annual mean number of inpatient and outpatient medical encounters experienced by a typical patient with NTM by infecting species and other cofactors, particularly among uninsured patients. The annual cost estimates reported here reflect just one encounter per case per year, as this is what was available in the literature. However, because of the characteristic chronic course of NTM disease, we expect that many patients have more than one medical encounter per year, especially outpatient visits. Even a second medical encounter within a given year dramatically increases our total cost estimates (Table 3).
Updated estimates on the average number of hospitalization days and outpatient visits per patient per year are needed to more accurately characterize the burden of NTM costs. Further characterization of cases and costs by disease severity, NTM species, comorbidities, and adherence to diagnosis and treatment guidelines, as well as improved age distribution estimates and population-based prevalence trends by age group, would improve the reliability of these estimates. Additionally, indirect costs (e.g., work loss, disability, poor quality of life), although not included in this analysis, greatly contribute to the total financial burden, whereas direct costs are representative of the treatment portion (25). Direct costs of medical encounters vary greatly, depending on provider specialty, testing conducted, insurance provider, and cost variations by state. Health care providers may alter the cost-to-charge ratio (hospital service cost vs. amount billed) by insurance providers (e.g., health plan, government programs) in an effort to accommodate for predetermined low Medicare and Medicaid payment rates (26). This process, known as “cost shifting,” although difficult to account for, impacts cost analysis (26). Finally, better adherence to American Thoracic Society diagnostic treatment guidelines by clinicians, which is currently poor even among specialists (18), could serve to reduce costs of NTM by limiting unnecessary procedures, visits, and treatment with incorrect and even harmful antibiotic regimens resulting in greater medical care needs of affected patients.
Our analyses provide the first state-specific estimates of NTM cases and associated costs in the United States. These estimates serve to better assess the economic burden and impact of NTM on public health. Because of the increasing prevalence of NTM, the chronic nature of the disease, and the lack of standardized national monitoring, additional research is needed to better characterize the clinical and epidemiologic features of this disease, including distribution of species as well as rates of survival, relapse, and/or reinfection.
Footnotes
Supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Author Contributions: All authors met all four criteria for authorship suggested by the International Committee of Medical Journal Editors. Study concept and design: S.E.S., J.A., and D.R.P.; acquisition of data: S.E.S., J.A., M.K.A., and D.R.P.; analysis and interpretation of data: S.E.S., J.A., M.K.A., and D.R.P.; drafting of the manuscript: S.E.S., J.A., and D.R.P.; critical revision of the manuscript for important intellectual content: S.E.S., J.A., M.K.A., and D.R.P.; statistical analysis: S.E.S., J.A., M.K.A., and D.R.P.; and study supervision: J.A. and D.R.P.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Adjemian J, Olivier KN, Seitz AE, Holland SM, Prevots DR. Prevalence of nontuberculous mycobacterial lung disease in U.S. Medicare beneficiaries. Am J Respir Crit Care Med. 2012;185:881–886. doi: 10.1164/rccm.201111-2016OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prevots DR, Shaw PA, Strickland D, Jackson LA, Raebel MA, Blosky MA, Montes de Oca R, Shea YR, Seitz AE, Holland SM, et al. Nontuberculous mycobacterial lung disease prevalence at four integrated health care delivery systems. Am J Respir Crit Care Med. 2010;182:970–976. doi: 10.1164/rccm.201002-0310OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dirac MA, Horan KL, Doody DR, Meschke JS, Park DR, Jackson LA, Weiss NS, Winthrop KL, Cangelosi GA. Environment or host? A case-control study of risk factors for Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2012;186:684–691. doi: 10.1164/rccm.201205-0825OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adjemian J, Olivier KN, Seitz AE, Falkinham JO, III, Holland SM, Prevots DR. Spatial clusters of nontuberculous mycobacterial lung disease in the United States. Am J Respir Crit Care Med. 2012;186:553–558. doi: 10.1164/rccm.201205-0913OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prevots DR, Adjemian J, Fernandez AG, Knowles MR, Olivier KN. Environmental risks for nontuberculous mycobacteria: individual exposures and climatic factors in the cystic fibrosis population. Ann Am Thorac Soc. 2014;11:1032–1038. doi: 10.1513/AnnalsATS.201404-184OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Falkinham JO. Impact of human activities on the ecology of nontuberculous mycobacteria. Future Microbiol. 2010;5:951–960. doi: 10.2217/fmb.10.53. [DOI] [PubMed] [Google Scholar]
- 7.Marras TK, Daley CL. Epidemiology of human pulmonary infection with nontuberculous mycobacteria. Clin Chest Med. 2002;23:553–567. doi: 10.1016/s0272-5231(02)00019-9. [DOI] [PubMed] [Google Scholar]
- 8.Billinger ME, Olivier KN, Viboud C, de Oca RM, Steiner C, Holland SM, Prevots DR. Nontuberculous mycobacteria-associated lung disease in hospitalized persons, United States, 1998-2005. Emerg Infect Dis. 2009;15:1562–1569. doi: 10.3201/eid1510.090196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winthrop KL, Baxter R, Liu L, McFarland B, Austin D, Varley C, Radcliffe L, Suhler E, Choi D, Herrinton LJ. The reliability of diagnostic coding and laboratory data to identify tuberculosis and nontuberculous mycobacterial disease among rheumatoid arthritis patients using anti-tumor necrosis factor therapy. Pharmacoepidemiol Drug Saf. 2011;20:229–235. doi: 10.1002/pds.2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kendall BA, Winthrop KL. Update on the epidemiology of pulmonary nontuberculous mycobacterial infections. Semin Respir Crit Care Med. 2013;34:87–94. doi: 10.1055/s-0033-1333567. [DOI] [PubMed] [Google Scholar]
- 11.Iseman MD, Marras TK. The importance of nontuberculous mycobacterial lung disease. Am J Respir Crit Care Med. 2008;178:999–1000. doi: 10.1164/rccm.200808-1258ED. [DOI] [PubMed] [Google Scholar]
- 12.Johnson MM, Odell JA. Nontuberculous mycobacterial pulmonary infections. J Thorac Dis. 2014;6:210–220. doi: 10.3978/j.issn.2072-1439.2013.12.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Field SK, Fisher D, Cowie RL. Mycobacterium avium complex pulmonary disease in patients without HIV infection. Chest. 2004;126:566–581. doi: 10.1378/chest.126.2.566. [DOI] [PubMed] [Google Scholar]
- 14.Jarand J, Levin A, Zhang L, Huitt G, Mitchell JD, Daley CL. Clinical and microbiologic outcomes in patients receiving treatment for Mycobacterium abscessus pulmonary disease. Clin Infect Dis. 2011;52:565–571. doi: 10.1093/cid/ciq237. [DOI] [PubMed] [Google Scholar]
- 15.Collier SA, Stockman LJ, Hicks LA, Garrison LE, Zhou FJ, Beach MJ. Direct healthcare costs of selected diseases primarily or partially transmitted by water. Epidemiol Infect. 2012;140:2003–2013. doi: 10.1017/S0950268811002858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Strollo SE, Adjemian J, Prevots DR. The burden of pulmonary nontuberculous mycobacterial disease in the United States: state-specific case estimates and associated cost [abstract] Am J Respir Crit Care Med. 2015;191(Abstract issue):A5260. [Google Scholar]
- 17.Ballarino GJ, Olivier KN, Claypool RJ, Holland SM, Prevots DR. Pulmonary nontuberculous mycobacterial infections: antibiotic treatment and associated costs. Respir Med. 2009;103:1448–1455. doi: 10.1016/j.rmed.2009.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adjemian J, Prevots DR, Gallagher J, Heap K, Gupta R, Griffith D. Lack of adherence to evidence-based treatment guidelines for nontuberculous mycobacterial lung disease. Ann Am Thorac Soc. 2014;11:9–16. doi: 10.1513/AnnalsATS.201304-085OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.S. Department of Labor Bureau of Labor Statistics (BLS)Chained consumer price index for all urban consumers (C-CPI-U), 2002–2014, Medical Care [Internet data tool]. Washington, DC: BLS; [accessed 2015 Aug 17]. Available from: http://data.bls.gov/cgi-bin/surveymost?su [Google Scholar]
- 20.Griffith DE, Winthrop KL. Mycobacterium avium complex lung disease therapy. Am J Respir Crit Care Med. 2012;186:477–479. doi: 10.1164/rccm.201207-1321ED. [DOI] [PubMed] [Google Scholar]
- 21.Leber A, Marras TK. The cost of medical management of pulmonary nontuberculous mycobacterial disease in Ontario, Canada. Eur Respir J. 2011;37:1158–1165. doi: 10.1183/09031936.00055010. [DOI] [PubMed] [Google Scholar]
- 22.Adjemian J, Olivier KN, Prevots DR. Nontuberculous mycobacteria among patients with cystic fibrosis in the United States: screening practices and environmental risk. Am J Respir Crit Care Med. 2014;190:581–586. doi: 10.1164/rccm.201405-0884OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tupasi TE, Gupta R, Quelapio MI, Orillaza RB, Mira NR, Mangubat NV, Belen V, Arnisto N, Macalintal L, Arabit M, et al. Feasibility and cost-effectiveness of treating multidrug-resistant tuberculosis: a cohort study in the Philippines. PLoS Med. 2006;3:e352. doi: 10.1371/journal.pmed.0030352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dalal AA, Shah M, D’Souza AO, Rane P. Costs of COPD exacerbations in the emergency department and inpatient setting. Respir Med. 2011;105:454–460. doi: 10.1016/j.rmed.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Boccuzzi SJ.Indirect health care costs Weintraub WS.editor. Cardiovascular health care economics. Totowa, NJ: Humana Press; 200363–79 [Google Scholar]
- 26.Frakt AB. How much do hospitals cost shift? A review of the evidence. Milbank Q. 2011;89:90–130. doi: 10.1111/j.1468-0009.2011.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]