Abstract
Rationale: Although numerous studies have documented that family members in intensive care units struggle with end-of-life decisions for incapacitated patients, there is little information about whether prior advance care planning lessens the burden of decision making.
Objectives: We sought to measure decisional conflict in surrogates of critically ill patients and to examine whether prior advance care planning is associated with less decisional conflict.
Methods: We performed a secondary data analysis of a multicenter, prospective cohort study done at five U.S. academic medical centers that included 471 surrogates of 257 patients with acute respiratory distress syndrome. The main outcome was surrogates’ burden of decision making as measured using the Decisional Conflict Scale. Surrogates completed a questionnaire item addressing whether they had had any prior advance care planning conversations with their loved ones. We used multilevel linear regression modeling to measure the association between decisional conflict and advance care planning.
Measurements and Main Results: Moderate or high levels of decisional conflict (Decisional Conflict Scale score ≥25) were present in 48% of surrogates. After adjusting for potential confounders, surrogates who had engaged in prior advance care planning conversations had significantly lower levels of decisional conflict than those who had not (mean score 3.3 points lower on the Decisional Conflict Scale; 95% confidence interval, −6.4 to −0.2; P = 0.03).
Conclusions: Nearly half of surrogates for critically ill patients have moderate or high levels of decisional conflict. Prior advance care planning was associated with less decisional conflict. These results suggest that the scope of the benefit of advance care planning may extend beyond respecting patients’ wishes to also ameliorating the burden on patients’ loved ones who act as surrogates.
Keywords: cohort study, communication, critical illness, decision making, respiratory distress syndrome
Surrogate decision makers often struggle when making decisions for critically ill patients (1–3). Guilt and other strong emotions may lead to making treatment decisions that are not aligned with the patient’s preferences (4–7) and may contribute to surrogates’ poor psychological outcomes (8). Decisional conflict measurement is a way to evaluate this burden. Decisional conflict has been described as wavering between choices, delaying decisions, and feeling emotionally distressed regarding the decision (9). Individuals with higher decisional conflict are up to five times more likely than others to subsequently express decisional regret (10). Decisional regret has been associated with lower quality of life in patients with cancer who have made treatment decisions regarding malignancy (11, 12).
Although numerous qualitative studies have suggested that surrogates struggle with decisions (2, 13–15), it is unclear whether advance care planning conversations between patients and surrogates ease the burden of decision making. This gap is important because, although the conventional view is that advance care planning is intended to ensure that patients’ values and preferences inform decision making, the benefits of advance care planning theoretically could extend to surrogate decision makers. Two small qualitative studies have shown that surrogates’ perceived burden of decision making decreases if the surrogate is aware of the patient’s preferences (16, 17).
We conducted this analysis to measure decisional conflict in surrogates facing actual end-of-life decisions and to determine whether advance care planning is associated with less decisional conflict.
Methods
Design
We performed a secondary analysis of a prospective, multicenter cohort study of surrogate decision makers for critically ill patients conducted between November 2010 and October 2012 in the medical-surgical, trauma, cardiac, and neurologic intensive care units (ICUs) of five U.S. academic medical centers, located in California, Pennsylvania, Washington, North Carolina, and Massachusetts, respectively (18). Our analysis was conducted at the University of Pittsburgh.
Participants
A total of 275 patients with acute respiratory distress syndrome (ARDS) and 546 surrogate decision makers were enrolled in this study. Only 251 patients and 471 surrogate decision makers had the opportunity to complete both questionnaires needed for this analysis.
Patients were eligible if they lacked decision-making capacity and had respiratory failure requiring mechanical ventilation owing to ARDS as defined by a paO2/fio2 ratio less than 300 and bilateral infiltrates not due to left atrial hypertension that were visualized by chest radiography. Eligible patients had a 50% or higher risk of hospital mortality or long-term and severe functional impairment as estimated by an Acute Physiology and Chronic Health Evaluation (APACHE) II score of at least 25 or by the attending physician’s estimate for patients with neurologic diagnoses. Patients who were awaiting organ transplantation, were facing imminent death, or had no surrogate available were ineligible.
We enrolled family members who self-identified as being involved in surrogate decision making for the patient. If multiple individuals identified themselves as surrogates for a patient, we then enrolled all surrogates who were willing to participate in the study and complete the questionnaire. Therefore, each patient could have more than one surrogate enrolled. To be considered, surrogates needed to be at least 18 years old and speak and read English well enough not to require an interpreter.
The study coordinator at each site obtained a daily list of all patients with ARDS identified through existing ARDS network screening mechanisms. The research coordinator then assessed whether the patient met the enrollment criteria for the study. If so, the study investigator sought permission from the attending physician to approach the surrogate decision maker regarding study participation. This study was approved by the University of Pittsburgh Institutional Review Board. All surrogates provided written consent for all study procedures.
Predictor Variable
Patient and surrogate demographic variables were obtained via baseline questionnaires administered on ICU Day 3 before a scheduled family conference that is part of routine clinical care. Whether surrogates had participated in prior advance care planning was assessed before the family conference on ICU Day 3 by asking the following yes-no question: “Have you ever discussed with your loved one the treatments he/she would want (or would not want) if he/she were too sick to speak for him/herself”? We selected this question because, although there is controversy about exactly the best way to implement advance care planning, there is general agreement that an important element is conversation about treatment options between patients and their surrogates.
Outcome Variables
The primary outcome measure was the surrogate’s score on the Decisional Conflict Scale (DCS) (19) regarding the decision whether to continue the patient’s life support. The DCS was administered to surrogates by a research nurse immediately after a family meeting that occurred on ICU Day 3 in which goals of care were addressed. The validity of the DCS is supported by test–retest correlations, Cronbach α coefficients exceeding 0.78, and an ability to discriminate between groups that make and delay decisions, with an effect size ranging from 0.4 to 0.8 (19). The DCS score ranges from 0 to 100, with scores lower than 25 often categorized as low decisional conflict, scores of 25–37.5 rated as moderate, and scores above 37.5 considered as high (20). High decisional conflict has been shown to be associated with decision delay and feeling unsure about continuing the course of treatment (20). Individuals with higher decisional conflict have more decisional regret (10), which has been associated with lower quality-of-life scores (11, 12).
As another outcome measure, we asked surrogates to rate the following question on a 10-point Likert scale on ICU Day 3 before the family meeting: “How well do you think you understand the treatments your loved one would want in his/her current medical situation”? A surrogate’s rating on this question is another important outcome of advance care planning.
Statistical Analysis
We used multilevel linear regression modeling to assess for an association between the presence or absence of a prior advance care planning conversation and surrogates’ decisional conflict. Multilevel modeling was used to account for the hierarchical nature of the data, in which there can be multiple surrogates per patient, and to take into account the correlation between family members who tend to share certain traits.
To assess for confounding variables that may affect the relationship between decisional conflict and advance care planning, we used the change-in-estimate approach (21, 22). This method of model selection is advocated by some methodologists because it has been shown to afford potential gains in precision (23). In this approach, we fit multilevel bivariate linear models, each with advance care planning as the primary predictor and a potential confounding variable as the covariate. We considered a variable as a confounder if it changed the effect size of the relationship between the main predictor (prior advance care planning) on the outcome measure (decisional conflict) by at least 10% when that variable was added to the model.
We tested the following variables as potential confounders in this manner: patients’ and surrogates’ age, sex, and ethnicity; surrogates’ relationship to the patient and their religious affiliation, religiosity, health literacy, and education level; and patients’ APACHE II scores and whether they were admitted from home. Table E1 in the online supplement contains the results of this testing. The variables that changed the effect size by at least 10% were included in the final multivariate model. These variables were whether the surrogate was a first-degree relative of the patient and if the patient was of a minority race and/or ethnicity.
To triangulate the main finding, we used the same approach to create another multilevel linear regression model with prior advance care planning as the predictor and surrogates’ self-ratings of how well they knew which treatments the patient would want as the outcome. We also compared surrogates’ self-ratings of how well they knew which treatments the patient would want, based on those who completed advance care planning and those who did not. We compared these scores using medians and interquartile ranges (IQRs), as well as a Wilcoxon rank-sum test because of the skewed nature of the data.
We also performed multivariate multilevel logistic regression for surrogates’ characteristics associated with completion of advance care planning. We performed this additional analysis to identify surrogate decision makers at high risk for high levels of decisional conflict.
All analyses were performed using STATA version 13 software (StataCorp, College Station, TX), and two-sided statistical significance was defined as a P value of 0.05 or less.
Results
Characteristics of Study Participants
Table 1 shows the demographic characteristics of the patients and surrogates who participated in the study. Among 405 eligible patients, 275 of them had surrogates who agreed to participate, for a patient enrollment rate of 68%. Of 546 surrogates in the original cohort, 471 completed the questionnaires and were available for analysis. Among 471 DCS questionnaires, 25 were incomplete, which is a missing rate of 5.3%. Because there is no validated way to handle missing responses in the DCS, we excluded unfinished surveys. The sample was diverse in terms of sex, religious affiliation, and level of education. Patients were admitted mostly from home, an outside hospital, or another acute care facility. At the time of enrollment, the patients had a mean APACHE II score of 32 ± 5. A majority of surrogates were the patient’s spouse or child and had a least some college education and adequate health literacy. About half of surrogates had prior experience in medical decision making.
Table 1.
Characteristics of study participants
| Surrogates | Patients | |||
|---|---|---|---|---|
| N = 471 |
N = 257 |
|||
| Characteristics | n | (%) | n | (%) |
| Age, yr, mean (SD) | 49.45 | (14.2) | 58.44 | (16.5) |
| Male | 187 | (34.67) | 139 | (54.1) |
| Race | ||||
| White | 364 | (80.2) | 207 | (81.8) |
| Black | 52 | (11.5) | 30 | (11.9) |
| Asian | 18 | (4.0) | 12 | (4.7) |
| Multiethnic | 18 | (4.0) | 3 | (1.2) |
| Native American | 2 | (0.4) | 1 | (0.4) |
| Pacific Islander/Samoan/Hawaiian | 0 | (0.0) | 0 | (0.0) |
| Hispanic | 42 | (9.0) | 21 | (9.6) |
| Importance of religion/spiritual beliefs | ||||
| Very important | 223 | (47.6) | ||
| Fairly important | 139 | (29.6) | ||
| Not too important | 70 | (14.9) | ||
| Not at all important | 37 | (7.89) | ||
| Education | ||||
| High school or less | 162 | (34.5) | ||
| Undergraduate degree/some college | 223 | (47.5) | ||
| Graduate degree | 85 | (18.1) | ||
| Relationship to the patient | ||||
| Spouse | 107 | (22.8) | ||
| Child | 167 | (35.5) | ||
| Sibling | 65 | (13.8) | ||
| Parent | 57 | (12.1) | ||
| Other relationship | 74 | (15.7) | ||
| Prior advance care planning discussion | 267 | (57.1) | ||
| Self-rated understanding about which treatments patient would want, 10-point Likert scale, mean (SD) | 7.8 | (2.6) | ||
| Prior decision-making experience | 227 | (48.6) | ||
| Total Decisional Conflict Scale (DCS) score, mean (SD) | 21.5 | (15.0) | ||
| Acute Physiology and Chronic Health Evaluation II score on enrollment, mean (SD) | 31.52 | (5.3) | ||
| Limited code status at enrollment | 27 | (10.5) | ||
| Admission source | ||||
| Home | 136 | (52.9) | ||
| Acute care facility | 104 | (40.5) | ||
| Other type of medical facility | 17 | (6.6) | ||
Surrogates’ Advance Care Planning Completion Rates and Levels of Decisional Conflict
Ninety-nine percent of surrogates (468 of 471) responded to the question about prior advance care planning. Fifty-seven percent (267 of 468) reported that they had had a prior advance care planning conversation with their loved one.
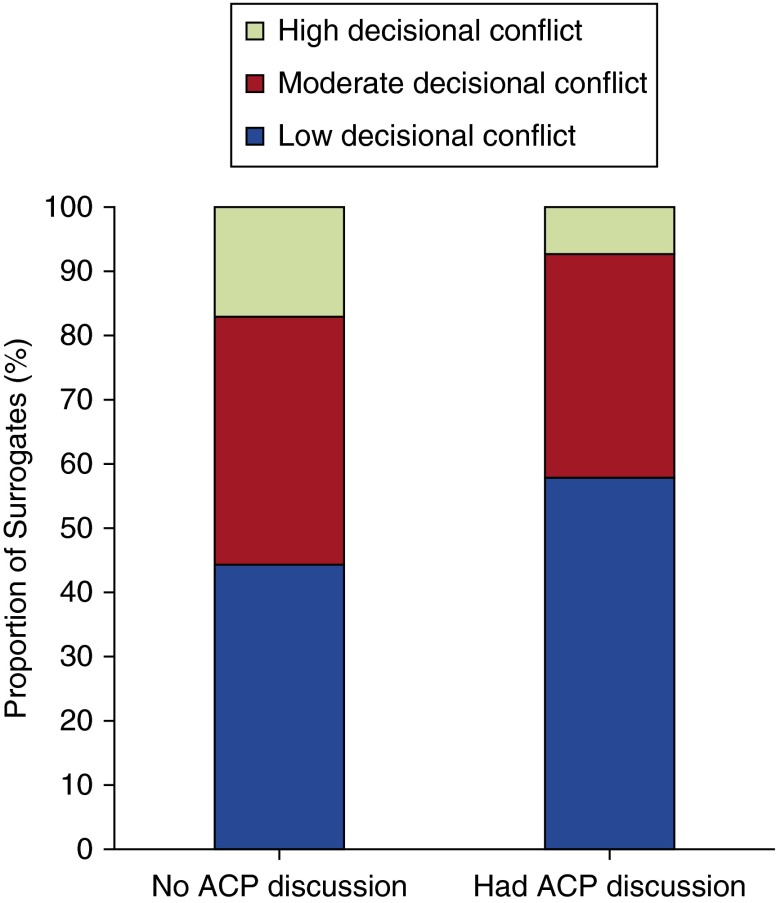
Ninety-five percent of surrogates (446 of 471) completed all 16 questions required to compute the total DCS. Surrogates’ mean decisional conflict score was 21.5 ± 15.0. Surrogates who completed advance care planning had a mean DCS score of 19.5 ± 14.0, and surrogates who had not completed advance care planning had a mean DCS score of 24.3 ± 16.1 (P = 0.001). Fifty-two percent of surrogates had low decisional conflict about continuing life support (DCS score <25), 37% had moderate decisional conflict (DCS score 25–37.5), and 11% had high decisional conflict (DCS score >37.5). Figure 1 shows the distribution of DCS scores by those who had completed prior advance care planning and those who had not.
Figure 1.
Distribution of decisional conflict by completion of advance care planning (ACP).
Predictors of Change in Decisional Conflict
Table 2 shows the multivariate model we used to analyze the relationship between the presence of a prior advance care planning conversation and decisional conflict, controlling for surrogates’ relationship to the patient and patients’ minority status. These confounders were chosen because they are the variables that changed the effect size by at least 10% as described above in the Statistical Analysis section. In this model, there was a statistically significant association between the presence of a prior advance care planning conversation and lower decisional conflict. After adjusting for the surrogates’ relationship to the patient and the patient’s minority status, surrogates who had engaged in prior advance care planning conversations with the patient scored a mean of 3.3 points lower on the DCS (95% confidence interval [CI], −6.4 to −0.2; P = 0.04).
Table 2.
Multilevel linear model estimates for total Decisional Conflict Scale
| Estimated Effect on Total Decisional Conflict Scale (95% CI) | P Value | |
|---|---|---|
| No adjustment | ||
| Advance care planning discussion | −5.35 (−8.19 to −2.50) | <0.001 |
| Adjusted for relationship and race | ||
| Advance care planning discussion | −3.31 (−6.39 to −0.23) | 0.04 |
| First-degree relative | −4.30 (−8.25 to −0.34) | 0.03 |
| Patient race (minority) | 1.10 (−2.59 to 4.80) | 0.56 |
Definition of abbreviations: CI = confidence interval.
In addition, surrogates who were first-degree relatives of the patient—spouse, child, sibling, or parent—scored a mean of 4.3 points lower on the DCS (95% CI, −8.2 to −0.3; P = 0.03).
Table E2 shows the results of the additional analysis with surrogates’ self-rating of how well they knew which treatments the patient would want as the outcome and the presence or absence of prior advance care planning as the predictor. This result is similar to the main analysis in that, after adjusting for confounders, surrogates who had completed prior advance care planning gave a higher rating to this question by an average of 2.1 points (95% CI, 1.6–2.6; P < 0.001).
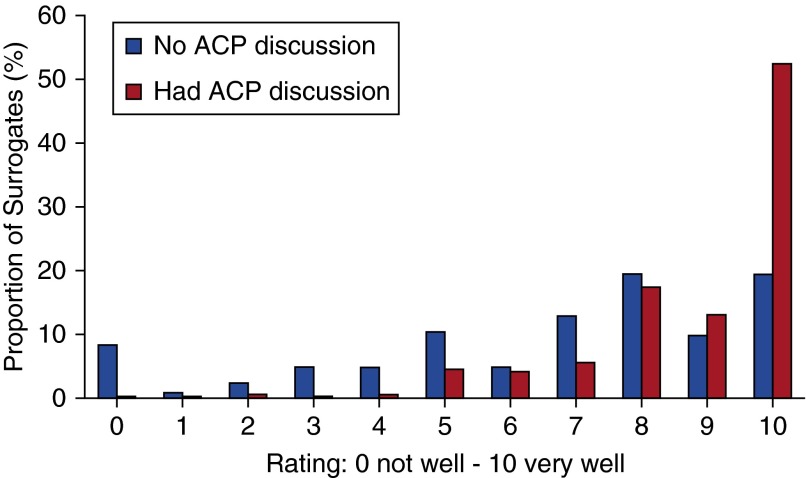
Figure 2 shows the distribution of surrogates’ self-rated understanding of which treatments the patient would want, comparing those who had completed advance care planning with those who had not. Surrogates who had completed prior advance care planning had significantly higher self-ratings regarding knowledge of patient treatment preferences (median, 10; IQR, 8–10) than did surrogates who had not completed advance care planning (median, 7; IQR, 5–9) (P < 0.001).
Figure 2.
Distribution of surrogates’ self-rated understanding of which treatments their loved one would want by completion of advance care planning (ACP).
Table E3 shows the results of the additional analysis of surrogates’ characteristics that were associated with completion of advance care planning. This analysis shows that surrogates significantly more likely to complete advance care planning were female (odds ratio [OR], 2.4; 95% CI, 4.3–24.0; P < 0.001) and spouses of the patient (OR, 2.42; 95% CI, 1.4–4.2; P = 0.002).
Discussion
We found that that nearly half of surrogates for critically ill patients had moderate or high levels of decisional conflict regarding forgoing life-sustaining treatment and that prior advance care planning was associated with lower decisional conflict.
This study provides new information about how advance care planning benefits surrogates for critically ill patients. Our main finding is consistent with data from a randomized controlled trial in which researchers found that advance care planning with patients during a hospitalization resulted in improved psychological outcomes for their surrogates (24). This contrasts with a study in which investigators found that advance care planning increased decisional conflict among surrogates for hospitalized patients with advanced dementia (25). However, that was a secondary finding in a small, exploratory trial, and, most important, the discussions involved only surrogates. Our data suggest that surrogates were significantly more likely to know the patient’s treatment preferences after advance care planning was completed with the patient, a finding that is consistent with prior work showing that surrogates have a lower burden of decision making when they are aware of the patient’s preferences (16, 17, 26). Without such information, however, the goals-of-care discussions may cause the surrogate stress (17).
This study also provides new information about the prevalence of decisional conflict in surrogates for critically ill patients. Our findings are consistent with a secondary data analysis of surrogate decision makers for patients with chronic critical illness that showed increased decisional burden in surrogates as measured by the single item of role stress (26). Decisional conflict both reflects how well individuals feel supported in the decision-making process and correlates with other long-term outcomes of clinical importance. For example, evidence suggests that surrogates with higher decisional conflict who later question their treatment decisions have worse psychological outcomes (2). In addition, those who resolve their decisional conflict have significantly less anxiety at follow-up than nonresolvers (27).
Our study has several limitations. First, because we asked surrogates if they had engaged in any prior advance care planning conversations (i.e., some vs. none), we were not able to evaluate the association between decisional conflict and the amount of advance care planning. Second, we measured decisional conflict at one point in time. It is unclear how decisional conflict scores change over the arc of an ICU admission or which scores are most predictive of adverse surrogate outcomes. Finally, although this is one of the largest cohorts of surrogate decision makers in the ICU, our study did not have adequate power for us to conduct subgroup analyses regarding age, religion, or racial group. Latinos, blacks, and whites have different attitudes toward life-sustaining treatments (28), and these differences may affect the conflict experienced during in-the-moment decision making.
In conclusion, we found that prior advance care planning is associated with lower surrogate decisional conflict regarding forgoing life-sustaining treatment. This suggests that the benefit of advance care planning may extend beyond respecting patients’ wishes to also ameliorating the burden on surrogate decision makers.
Footnotes
Supported by National Heart, Lung, and Blood Institute Grants 5R01 HL094553-02 and 2T32 HL007563-26.
Author Contributions: J.C. contributed to data analysis, data interpretation, and drafting and critical revision of the manuscript; P.B. contributed to data analysis, data interpretation, and critical revision of the manuscript; R.M.A. contributed to data interpretation and critical revision of the manuscript; and D.B.W. contributed to study conception and design, data interpretation, and critical revision of the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Breen CM, Abernethy AP, Abbott KH, Tulsky JA. Conflict associated with decisions to limit life-sustaining treatment in intensive care units. J Gen Intern Med. 2001;16:283–289. doi: 10.1046/j.1525-1497.2001.00419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154:336–346. doi: 10.7326/0003-4819-154-5-201103010-00008. [DOI] [PubMed] [Google Scholar]
- 3.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med. 2006;166:493–497. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 4.Danis M, Mutran E, Garrett JM, Stearns SC, Slifkin RT, Hanson L, Williams JF, Churchill LR. A prospective study of the impact of patient preferences on life-sustaining treatment and hospital cost. Crit Care Med. 1996;24:1811–1817. doi: 10.1097/00003246-199611000-00009. [DOI] [PubMed] [Google Scholar]
- 5.The Writing Group for the SUPPORT Investigators. A controlled trial to improve care for seriously ill hospitalized patients: the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) JAMA. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 6.Cosgriff JA, Pisani M, Bradley EH, O’Leary JR, Fried TR. The association between treatment preferences and trajectories of care at the end-of-life. J Gen Intern Med. 2007;22:1566–1571. doi: 10.1007/s11606-007-0362-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnato AE, Herndon MB, Anthony DL, Gallagher PM, Skinner JS, Bynum JP, Fisher ES. Are regional variations in end-of-life care intensity explained by patient preferences? A study of the US Medicare population. Med Care. 2007;45:386–393. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kross EK, Engelberg RA, Gries CJ, Nielsen EL, Zatzick D, Curtis JR. ICU care associated with symptoms of depression and posttraumatic stress disorder among family members of patients who die in the ICU. Chest. 2011;139:795–801. doi: 10.1378/chest.10-0652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Connor AM, Jacobsen MJ, Stacey D. An evidence-based approach to managing women’s decisional conflict. J Obstet Gynecol Neonatal Nurs. 2002;31:570–581. doi: 10.1111/j.1552-6909.2002.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 10.Sun Q.Predicting downstream effects of high decisional conflict: meta-analyses of the Decisional Conflict Scale [master’s thesis.]. Ottawa, ON, Canada: University of Ottawa; 2005[accessed 2015 Aug 21]. Available from: https://www.ruor.uottawa.ca/bitstream/10393/27050/1/MR11422.PDF [Google Scholar]
- 11.Davison BJ, So AI, Goldenberg SL. Quality of life, sexual function and decisional regret at 1 year after surgical treatment for localized prostate cancer. BJU Int. 2007;100:780–785. doi: 10.1111/j.1464-410X.2007.07043.x. [DOI] [PubMed] [Google Scholar]
- 12.Diefenbach MA, Mohamed NE. Regret of treatment decision and its association with disease-specific quality of life following prostate cancer treatment. Cancer Invest. 2007;25:449–457. doi: 10.1080/07357900701359460. [DOI] [PubMed] [Google Scholar]
- 13.Pochard F, Darmon M, Fassier T, Bollaert PE, Cheval C, Coloigner M, Merouani A, Moulront S, Pigne E, Pingat J, et al. French FAMIREA study group. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death: a prospective multicenter study. J Crit Care. 2005;20:90–96. doi: 10.1016/j.jcrc.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Tilden VP, Tolle SW, Drach LL, Perrin NA. Out-of-hospital death: advance care planning, decedent symptoms, and caregiver burden. J Am Geriatr Soc. 2004;52:532–539. doi: 10.1111/j.1532-5415.2004.52158.x. [DOI] [PubMed] [Google Scholar]
- 15.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, et al. FAMIREA Study Group. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171:987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 16.Braun UK, Beyth RJ, Ford ME, McCullough LB. Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. J Gen Intern Med. 2008;23:267–274. doi: 10.1007/s11606-007-0487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vig EK, Starks H, Taylor JS, Hopley EK, Fryer-Edwards K. Surviving surrogate decision-making: what helps and hampers the experience of making medical decisions for others. J Gen Intern Med. 2007;22:1274–1279. doi: 10.1007/s11606-007-0252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiarchiaro J, Buddadhumaruk P, Arnold RM, White DB. Quality of communication in the ICU and surrogate’s understanding of prognosis. Crit Care Med. 2015;43:542–548. doi: 10.1097/CCM.0000000000000719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 20.O’Connor A.User manual: Decisional Conflict Scale. Ottawa, ON, Canada: Ottawa Hospital; 1993 [accessed 2015 Aug 21]. Available from: https://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Decisional_Conflict.pdf
- 21.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129:125–137. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- 22.Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79:340–349. doi: 10.2105/ajph.79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weng HY, Hsueh YH, Messam LLM, Hertz-Picciotto I. Methods of covariate selection: directed acyclic graphs and the change-in-estimate procedure. Am J Epidemiol. 2009;169:1182–1190. doi: 10.1093/aje/kwp035. [DOI] [PubMed] [Google Scholar]
- 24.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345. doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sampson EL, Jones L, Thuné-Boyle ICV, Kukkastenvehmas R, King M, Leurent B, Tookman A, Blanchard MR. Palliative assessment and advance care planning in severe dementia: an exploratory randomized controlled trial of a complex intervention. Palliat Med. 2011;25:197–209. doi: 10.1177/0269216310391691. [DOI] [PubMed] [Google Scholar]
- 26.Hickman RL, Jr, Pinto MD. Advance directives lessen the decisional burden of surrogate decision-making for the chronically critically ill. J Clin Nurs. 2014;23:756–765. doi: 10.1111/jocn.12427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenberg LS, Webster MC. Resolving decisional conflict by Gestalt two-chair dialogue: relating process to outcome. J Couns Psychol. 1982;29:468–477. [Google Scholar]
- 28.Allen RS, Allen JY, Hilgeman MM, DeCoster J. End-of-life decision-making, decisional conflict, and enhanced information: race effects. J Am Geriatr Soc. 2008;56:1904–1909. doi: 10.1111/j.1532-5415.2008.01929.x. [DOI] [PubMed] [Google Scholar]