Abstract
Objectives. We examined factors associated with frequent hospitalizations and emergency department (ED) visits among Medicaid members who were homeless.
Methods. We included 6494 Massachusetts Medicaid members who received services from a health care for the homeless program in 2010. We used negative binomial regression to examine variables associated with frequent utilization.
Results. Approximately one third of the study population had at least 1 hospitalization and two thirds had 1 or more ED visits. More than 70% of hospitalizations and ED visits were incurred by only 12% and 21% of these members, respectively. Homeless individuals with co-occurring mental illness and substance use disorders were at greatest risk for frequent hospitalizations and ED visits (e.g., incidence rate ratios [IRRs] = 2.9–13.8 for hospitalizations). Individuals living on the streets also had significantly higher utilization (IRR = 1.5).
Conclusions. Despite having insurance coverage, homeless Medicaid members experienced frequent hospitalizations and ED visits. States could consider provisions under the Patient Protection and Affordable Care Act (e.g., Medicaid expansion and Health Homes) jointly with housing programs to meet the needs of homeless individuals, which may improve the quality and cost effectiveness of care.
Homeless individuals experience very high rates of behavioral health disorders, chronic and acute physical conditions, and injuries related to assaults and accidents.1–4 However, they face multiple competing demands in their daily life, such as food and shelter, and therefore sometimes cannot prioritize medical care.5 In addition, many of them are uninsured or do not have a usual source of care, which often leads them to rely on emergency departments (EDs) as a source of routine medical care. Furthermore, when unmanaged symptoms trigger urgent events or injuries occur, homeless individuals may seek care in EDs, and they may be hospitalized.
Consequently, homeless individuals experience frequent hospitalizations and ED visits.3,4,6–9 Studies have reported that a quarter to one third of homeless people are hospitalized during a year, which is 4 times higher than the US average.3,4 Also, one third to two thirds of homeless people have at least 1 ED visit, which is much higher than the national average of one fifth of the general population.3,4,6,10 Furthermore, hospitalizations and ED visits account for approximately half of medical expenditures for insured homeless individuals.4
Having a clear understanding of risk factors for frequent hospitalizations and ED visits among homeless individuals is crucial as many states expand Medicaid coverage under the Patient Protection and Affordable Care Act.11 Individuals struggling with homelessness are more likely to be eligible to enroll because of their low income and lack of insurance. Medicaid programs could face significant challenges in managing homeless individuals’ complex needs and high health care utilization. Insurance coverage enables homeless people to access primary care, which might be expected to lower nonurgent visits to EDs or hospitalizations for preventable conditions. However, recent studies based on claims data have shown that insured homeless people in the United States and Canada still experience very high rates of hospitalization and ED visits.4,7–9 In addition, survey-based studies have indicated that homeless people with insurance are more likely to be hospitalized than those without insurance, although the evidence regarding ED visits is mixed.3,6,12
Studies of health care utilization among homeless people in the United States have not provided comprehensive information about what happens when they are insured, in particular, what factors are associated with frequent hospitalizations and ED visits.3,6,12,13 Also, studies that rely on self-reported data or survey data are subject to recall bias, and those using records from a single clinic have less complete data than insurance claims. Although a Canadian study of insured homeless people has shown that several enabling and need factors (e.g., perceived unmet mental health needs, individual’s health being controlled by powerful others, and health status) are associated with hospitalizations and ED visits, these data are neither routinely collected nor readily available in existing databases.8,9 Also, these results might not be fully applicable to homeless people in the United States because of differences in health care delivery and financing between the 2 countries.
We analyzed Massachusetts Medicaid claims data for a large sample of homeless individuals with Medicaid coverage to enhance our understanding of factors associated with frequent hospitalizations and ED visits in the United States. Early Medicaid expansion in Massachusetts, beginning in the 1990s, provided health insurance coverage for a large number of individuals experiencing homelessness. A health insurance mandate implemented in 2006 further reduced the number of uninsured homeless people. Therefore, Massachusetts serves as a unique environment to better understand reasons for hospitalizations and ED visits and factors associated with frequent utilization for insured homeless people. These findings can be useful to states in developing care management strategies or other specialized interventions for this vulnerable population.
METHODS
We merged data from the Boston Health Care for the Homeless Program (BHCHP) and Medicaid administrative data in calendar year (CY) 2010. Approximately 40% of homeless people in Massachusetts received care from BHCHP and 80% of BHCHP patients had Medicaid coverage.14 BHCHP is the major health care for the homeless program in the city of Boston and serves the majority of homeless people accounted for in the city’s annual homeless census. The population served by BHCHP includes individual adults, families, and unaccompanied youths. In addition, BHCHP continues to be the health care provider for some homeless people who are placed in housing programs. Details of the BHCHP have been reported elsewhere.15
Medicaid administrative data include member eligibility and enrollment information for population characteristics and comprehensive medical claims for health care utilization and expenditures. Claims data provide diagnostic information for both behavioral health services and general medical care across a broad range of health care settings. We derived race/ethnicity and housing status from BHCHP data, which provided more comprehensive information on these measures than did Medicaid administrative data.
Study Population
The BHCHP database included 6846 potential Medicaid recipients. We linked Medicaid identification numbers obtained from BHCHP records with Medicaid enrollment data to confirm Medicaid status. We also used the provider number in the Medicaid claims data to verify that these individuals received services from BHCHP.
We excluded individuals who could not be identified in Medicaid administrative data and those individuals enrolled in specific Medicaid managed care programs for older adults. The former group accounted for the majority of the exclusion, and we did not have access to health care utilization records for the latter group. The final study population included 6494 Massachusetts Medicaid members who received care from the BHCHP in CY2010.
Dependent and Independent Variables
We examined variables associated with 2 outcomes: the number of hospitalizations and the number of ED visits. In addition to the high annual average number of these events experienced by BHCHP patients, a subgroup of them had 3 or more hospitalizations or ED visits in a year.4 Thus, instead of using a dichotomous variable to indicate whether an event occurred or to classify people as low or high users, we studied the number of events to better understand how variables were associated with hospitalizations and ED visits.
According to the behavioral model of health services utilization for vulnerable populations,16 we grouped variables associated with hospitalizations and ED visits into 3 groups: predisposing, enabling, and need factors. Predisposing factors included demographic characteristics (age, gender, race/ethnicity), enabling factors included health insurance characteristics (Medicare coverage, number of Medicaid enrollment days), and need factors included characteristics that affect need for health care (disability, housing status, mental illness, substance use disorders, and general medical conditions). In the descriptive analysis, we also reported disease burden using DxCG score.17 DxCG score was set to 1.0 for the general Medicaid population in its original development sample. Individuals with a higher than average disease burden will have DxCG scores greater than 1.0, and vice versa.
The regression analysis focused on the association between need factors and frequent hospitalizations or ED visits after adjusting for predisposing and enabling factors. Housing status was an individual’s last known place of residence in CY2010 derived from records maintained by BHCHP. Patients were classified into street, shelter, transitional housing or residential treatment program, doubled up or motel, and housed with or without support services.
Using the Clinical Classification Software developed by the Agency for Healthcare Research and Quality (Rockville, MD), we grouped diagnoses reported in Medicaid claims and encounter data into clinically meaningful disease groups. We identified members with mental illness, substance use disorders, and selected physical conditions. Mental illness included schizophrenia and other psychosis, bipolar disorders, depression, anxiety, and other mental illness. Substance use disorders (SUDs) included alcohol abuse or dependence and drug abuse or dependence. Selected physical conditions were hepatitis C, HIV, liver cirrhosis, asthma or chronic obstructive pulmonary disease, hypertension, congestive heart failure, ischemic heart disease, and diabetes. Because the final modeling already included these clinically meaningful disease groups, we did not include the overall disease burden represented by the DxCG score.
Statistical Analysis
We examined population characteristics and disease profiles by level of health care utilization (zero, moderate, and high number of events). We used the χ2 test for categorical variables and analysis of variance for continuous variables to examine differences between these utilization groups.
Because the number of hospitalizations and ED visits were count data with greater variability (i.e., overdispersion), we used negative binomial regression to examine variables associated with these 2 outcomes. All analyses were performed with SAS statistical software, version 9.2 (SAS Institute, Cary, NC).
RESULTS
A total of 6494 BHCHP patients with Medicaid coverage in CY2010 were included in the analysis. Almost three quarters of BHCHP patients were male (71%), and the average age was 45.5 years (Table 1). More than two thirds of patients were nonhoused (70%), one fifth were housed with or without support services (21%), and 9% were unknown. Mental illness (68%) and SUDs (60%) were highly prevalent, and 48% of homeless individuals had co-occurring mental illness and SUD. The 3 leading physical conditions were hypertension (37%), asthma or chronic obstructive pulmonary disease (26%), and hepatitis C (23%). More details on population characteristics have been reported elsewhere.4
TABLE 1—
Population Characteristics for Boston Health Care for the Homeless Program Patients With Medicaid by Number of Hospitalizations and ED Visits: Boston, MA, 2010
| No. of Hospitalizations |
No. of ED Visits |
|||||||
| Characteristics | Total (n = 6494), Mean ±SD or No. (%) | 0 (n = 4287), Mean ±SD or No. (%) | 1–2 (n = 1436), Mean ±SD or No. (%) | ≥ 3 (n = 771), Mean ±SD or No. (%) | 0 (n = 1990), Mean ±SD or No. (%) | 1–2 (n = 1932), Mean ±SD or No. (%) | 3–5 (n = 1168), Mean ±SD or No. (%) | ≥ 6 (n = 1404), Mean ±SD or No. (%) |
| Age,a,b y | 45.5 ±13.3 | 45.4 ±13.5 | 45.5 ±13.1 | 46.8 ±12.1 | 47.8 ±13.4 | 45.1 ±14.2 | 44.3 ±12.5 | 43.8 ±11.7 |
| Genderb,c | ||||||||
| Male | 4587 (71) | 3058 (71) | 956 (67) | 573 (74) | 1472 (74) | 1329 (69) | 801 (69) | 985 (70) |
| Female | 1907 (29) | 1229 (29) | 480 (33) | 198 (26) | 428 (26) | 603 (31) | 367 (31) | 419 (30) |
| Race/ethnicityb | ||||||||
| Non-Latino White | 2868 (44) | 1692 (39) | 709 (49) | 467 (61) | 786 (40) | 756 (39) | 530 (45) | 796 (57) |
| Non-Latino African American | 2058 (32) | 1487 (35) | 397 (28) | 174 (23) | 683 (34) | 660 (34) | 369 (32) | 346 (25) |
| Latino | 986 (15) | 702 (16) | 210 (15) | 74 (10) | 333 (17) | 314 (16) | 169 (14) | 170 (12) |
| Other | 214 (3) | 155 (4) | 43 (3) | 16 (2) | 77 (4) | 73 (4) | 35 (3) | 29 (2) |
| Unknown | 368 (6) | 251 (6) | 77 (5) | 40 (5) | 111 (6) | 129 (7) | 65 (6) | 63 (4) |
| Insurance and disability | ||||||||
| Medicareb,d | 1761 (27) | 1006 (23) | 440 (31) | 315 (41) | 579 (29) | 532 (28) | 294 (25) | 356 (25) |
| Medicaid enrollment daysa,c | 340.8 ±61.7 | 335.9 ±68.9 | 347.4 ±49.6 | 356.0 ±33.3 | 326.7 ±79.9 | 340.4 ±61.3 | 349.1 ±46.7 | 354.6 ±35.9 |
| Disabilityb,c | 3734 (58) | 2191 (51) | 951 (66) | 592 (77) | 1044 (52) | 1085 (56) | 682 (58) | 923 (66) |
| Housing statusb,c | ||||||||
| Housed | 1391 (21) | 953 (22) | 306 (21) | 132 (17) | 527 (26) | 453 (23) | 214 (18) | 197 (14) |
| Doubled up or motel | 696 (11) | 486 (11) | 146 (10) | 64 (8) | 248 (12) | 217 (11) | 100 (9) | 131 (9) |
| Transitional housing or residential treatment | 1105 (17) | 700 (16) | 257 (18) | 148 (19) | 250 (13) | 303 (16) | 271 (23) | 281 (20) |
| Shelter | 2448 (38) | 1602 (37) | 545 (38) | 301 (39) | 681 (34) | 732 (38) | 446 (38) | 589 (42) |
| Street | 253 (4) | 135 (3) | 60 (4) | 58 (8) | 53 (3) | 54 (3) | 39 (3) | 107 (8) |
| Unknown | 601 (9) | 411 (10) | 122 (9) | 68 (9) | 231 (12) | 173 (9) | 98 (8) | 99 (7) |
| Behavioral health disorders | ||||||||
| Any mental illnessb,c | 4384 (68) | 2469 (58) | 1186 (83) | 729 (95) | 944 (47) | 1274 (66) | 921 (79) | 1245 (89) |
| Any SUDsb,c | 3890 (60) | 2017 (48) | 1104 (77) | 714 (93) | 701 (35) | 1078 (56) | 860 (74) | 1251 (89) |
| Co-occurring mental illness and SUDsb,c | 3135 (48) | 1489 (35) | 961 (67) | 685 (89) | 463 (23) | 818 (42) | 722 (62) | 1132 (81) |
| Selected physical conditions: anyb,c | 4215 (65) | 2395 (56) | 1119 (78) | 701 (91) | 1061 (53) | 1201 (62) | 810 (69) | 1143 (81) |
| Disease burden: DxCG scoreb,c | 3.8 ±3.8 | 2.2 ±1.8 | 5.3 ±3.1 | 9.9 ±5.3 | 1.9 ±2.2 | 3.2 ±3.2 | 4.5 ±4.0 | 6.6 ±4.4 |
| Service utilization | ||||||||
| Ambulatory care office visitsb,c | 10.0 ±11.0 | 8.6 ±9.8 | 12.0 ±11.4 | 14.3 ±14.0 | 7.1 ±8.4 | 9.6 ±9.4 | 11.8 ±13.1 | 13.3 ±12.8 |
| Hospitalizationsb,c | 1.0 ±2.4 | 0 | 1.3 ±0.5 | 6.0 ±4.0 | 0.2 ±0.7 | 0.5 ±1.1 | 1.0 ±1.8 | 2.8 ±4.0 |
| ED visitsb,c | 4.0 ±7.3 | 2.1 ±3.7 | 5.1 ±6.8 | 12.7 ±14.0 | 0 | 1.4 ±0.5 | 3.8 ±0.8 | 13.6 ±11.1 |
Note. ED = emergency department; SUD = substance use disorders. Selected physical conditions include hepatitis C, HIV, liver cirrhosis, asthma or chronic obstructive pulmonary disease, hypertension, congestive heart failure, ischemic heart disease, and diabetes.
P < .05 for hospitalizations.
P < .01 for ED visits.
P < .01 for hospitalizations.
P < .05 for ED visits.
BHCHP patients with frequent hospitalizations or ED visits had significantly different population characteristics than those with lower utilization (Table 1). These frequent utilizers were more likely to be non-Latino White, be dually eligible for Medicare and Medicaid, live on the streets, and have much higher disease burden. Furthermore, frequent hospital and ED utilizers had 13 to 14 ambulatory care office visits annually, much higher than the 7 to 9 visits for those without hospitalization or ED visit.
One third of BHCHP patients had 1 or more hospitalizations and approximately two thirds had at least 1 ED visit during 2010 (Table 1 and Figure 1). Frequent users accounted for a disproportionate share of these services (Figure 1). Although 12% of BHCHP patients had 3 or more hospitalizations, they accounted for 71% of all hospitalizations. Similarly, BHCHP patients with 6 or more ED visits (21%) accounted for 73% of all ED visits.
FIGURE 1—
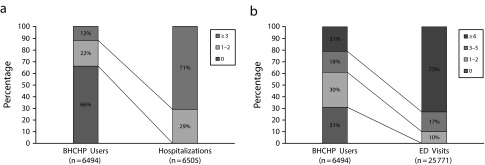
Distribution of Boston Health Care for the Homeless Program (BHCHP) patients and (a) hospitalizations and (b) emergency department (ED) visits: Boston, MA, 2010.
Principal diagnoses for hospitalizations and ED visits were classified into clinically meaningful disease groups (Table 2). Half of hospitalizations were for behavioral health disorders (n = 3044), and bipolar disorder was the most common principal reason for behavioral health hospitalization (30%) followed by alcohol-related disorders (22%), drug-related disorders (16%), schizophrenia (11%), and major depression (10%). For general medical conditions (n = 3461), the leading disease groups were those for circulatory system (15%), injury and poisoning (14%), respiratory system (13%), and digestive system (13%). Approximately one third of ED visits were attributable to behavioral health disorders (n = 7531), with alcohol-related disorders being the most common reason (52%), followed by drug-related disorders (18%). Among ED visits for general medical conditions (n = 18 240), the leading diagnosis was injury and poisoning (20%).
TABLE 2—
Leading Disease Groups for Hospitalizations and ED Visits Among Boston Health Care for the Homeless Program Patients With Medicaid: Boston, MA, 2010
| Disease Group | Hospitalization, No. (%) or % | ED Visit, No. (%) or % |
| Alla | ||
| Behavioral health disorders | 3 044 (47) | 7 531 (29) |
| General medical | 3 461 (53) | 18 240 (71) |
| Behavioral health disordersb | ||
| Bipolar disorders | 30 | 4 |
| Alcohol-related disorders | 22 | 52 |
| Drug-related disorders | 16 | 18 |
| Schizophrenia and other psychotic disorders | 11 | 4 |
| Major depression | 10 | 2 |
| Other depression | 4 | 11 |
| Anxiety disorders | 2 | 5 |
| Other | 5 | 5 |
| General medical conditionsc | ||
| Circulatory system | 15 | 7 |
| Injury and poisoning | 14 | 20 |
| Respiratory system | 13 | 10 |
| Digestive system | 13 | 6 |
| Skin and subcutaneous tissue | 8 | 6 |
| Endocrine, nutritional, and metabolic diseases | 7 | 3 |
| Musculoskeletal system and connective tissue | 5 | 12 |
| Nervous system and sense organs | 4 | 10 |
| Symptoms, signs, ill-defined conditions | 4 | 12 |
| Infectious and parasitic diseases | 4 | 2 |
| Genitourinary system | 4 | 4 |
| Otherd | 8 | 8 |
Note. ED = emergency department.
n = 6505 for hospitalization; n = 25 771 for ED visit.
n = 3044 for hospitalization; n = 7531 for ED visit.
n = 3461 for hospitalization; n = 18 240 for ED visit.
Includes neoplasms, pregnancy complications, childbirth, puerperium, blood and blood-forming organ diseases, residual codes, all E codes, and unclassified diagnoses.
Table 3 shows the incident rate ratios (IRRs) and 95% confidence intervals from the negative binomial models for hospitalizations and ED visits, respectively, after adjusting for demographic and health insurance characteristics. The IRRs represent the ratio of the count of events (e.g., hospitalization) for the variable of interest (e.g., people with co-occurring schizophrenia and SUD) to its reference group (e.g., people with no mental illness and no SUD). The multivariate analyses showed that homeless individuals with co-occurring mental illness and SUDs were at the greatest risk of frequent hospitalizations and ED visits (e.g., IRRs = 2.9–13.8 for all-cause hospitalizations) followed by those with schizophrenia or SUD alone (IRRs = 3.6 and 2.4 for hospitalizations and IRRs = 2.3 and 3.0 for ED visits, respectively). With a more moderate impact, most selected physical conditions were also associated with increased hospitalizations (IRRs = 1.4–2.3) and ED visits (IRRs = 1.1–1.5). In addition, unhoused individuals had significantly higher utilization than those who had been housed with or without support services (e.g., IRRs = 1.5 and 2.1 for hospitalizations and ED visits, respectively, among those living on the streets).
TABLE 3—
Incident Rate Ratios for Variables Associated With the Number of Hospitalizations and Emergency Department Visits Among Boston Health Care for the Homeless Program Patients With Medicaid: Boston, MA, 2010
| Variables | Hospitalizations, IRR (95% CI) | ED Visits, IRR (95% CI) |
|
Housing status | ||
| Housed (Ref) | 1.0 | 1.0 |
| Doubled up or motel | 1.3 (1.1, 1.6) | 1.2 (1.1, 1.3) |
| Transitional housing or residential treatment | 1.2 (1.1, 1.4) | 1.0 (0.9, 1.2) |
| Shelter | 1.4 (1.2, 1.6) | 1.5 (1.4, 1.6) |
| Street | 1.5 (1.2, 1.9) | 2.1 (1.8, 2.4) |
| Unknown | 1.1 (0.9, 1.3) | 1.1 (1.0, 1.3) |
| Behavioral health disorders | ||
| No behavioral health disorder (Ref) | 1.0 | 1.0 |
| Schizophrenia with SUD | 13.8 (11.4, 16.6) | 7.8 (6.9, 8.8) |
| Schizophrenia only | 3.6 (2.8, 4.6) | 2.3 (1.9, 2.7) |
| Bipolar with SUD | 6.1 (5.0, 7.4) | 4.4 (3.9, 5.0) |
| Bipolar only | 1.0 (0.7, 1.5) | 2.0 (1.7, 2.5) |
| Depression with SUD | 4.4 (3.6, 5.4) | 3.9 (3.5, 4.4) |
| Depression only | 1.8 (1.4, 2.3) | 1.8 (1.6, 2.1) |
| Anxiety with SUD | 2.9 (2.1, 3.9) | 3.7 (3.1, 4.4) |
| Anxiety only | 1.3 (0.7, 2.1) | 2.2 (1.7, 2.8) |
| Other mental illness with SUD | 3.6 (2.5, 5.3) | 4.4 (3.5, 5.7) |
| Other mental illness only | 1.6 (1.1, 2.4) | 1.0 (0.8, 1.3) |
| SUD only | 2.4 (1.9, 2.8) | 3.0 (2.6, 3.4) |
| Physical conditions | ||
| Hepatitis C | 1.5 (1.3, 1.6) | 1.2 (1.1, 1.2) |
| HIV | 1.0 (0.8, 1.2) | 0.9 (0.8, 1.0) |
| Cirrhosis | 1.9 (1.6, 2.3) | 1.5 (1.3, 1.8) |
| Asthma/COPD | 1.5 (1.4, 1.6) | 1.5 (1.4, 1.6) |
| Hypertension | 1.8 (1.6, 2.0) | 1.3 (1.2, 1.4) |
| Congestive heart failure | 2.3 (1.9, 2.8) | 1.2 (1.0, 1.4) |
| Ischemic heart disease | 1.9 (1.6, 2.1) | 1.1 (1.0, 1.2) |
| Diabetes | 1.4 (1.2, 1.5) | 1.2 (1.1, 1.3) |
| Demographics | ||
| Age | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) |
| Female | 1.0 (1.0, 1.1) | 1.0 (1.0, 1.1) |
| Race/ethnicity | ||
| Non-Latino White (Ref) | 1.0 | 1.0 |
| Non-Latino African American | 0.7 (0.7, 0.8) | 1.0 (0.9, 1.0) |
| Latino | 0.7 (0.6, 0.8) | 0.8 (0.7, 0.9) |
| Others | 0.8 (0.6, 1.1) | 0.9 (0.7, 1.0) |
| Unknown | 0.9 (0.7, 1.1) | 0.9 (0.8, 1.0) |
| Health insurance and disability | ||
| Medicare and Medicaid | 1.4 (1.2, 1.5) | 0.9 (0.8, 0.9) |
| Medicaid enrollment days | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) |
| Disability | 1.2 (1.1, 1.3) | 1.0 (1.0, 1.1) |
Note. CI = confidence interval; COPD = chronic obstructive pulmonary disease; ED = emergency department; IRR = incidence rate ratio; SUD = substance use disorder.
DISCUSSION
Our findings show very high rates of hospitalizations and ED visits for Medicaid members experiencing homelessness, even though Medicaid coverage improves access to care and affords members a wide range of services in the outpatient setting. Notably, a small group of frequent users accounted for the majority of hospitalizations and ED visits. Also, contrary to conventional belief, these frequent users had a significantly higher number of ambulatory care office visits than those with less frequent hospitalizations and ED visits. This finding is similar to those of other studies showing that frequent ED users also have high rates of other ambulatory care visits.18–20 Furthermore, the significant association between frequent utilization and mental illness, SUDs, and unstable housing suggests that combining housing with improved behavioral health treatment and support could be helpful to meet complex medical and social needs for homeless individuals. By analyzing complete claims data, this study highlights areas in which states can develop enhanced care coordination strategies and housing programs for homeless individuals.
Mental illness and SUDs, particularly when they co-occur, place homeless individuals at substantially increased risk for frequent hospitalizations and ED visits. Individuals with mental illness, SUDs, or both experience greater medical comorbidities, poorer quality of care, lower adherence to treatment regimens, and higher health care expenditures than those without these conditions.21–25 Although Medicaid coverage improves access to general medical care, homeless individuals might face challenges in locating their behavioral health services and coordinating with general medical care if additional assistance is lacking. The shortage of behavioral health specialists and facilities and the lack of trusted relationships with providers also pose challenges in service coordination. Furthermore, traditionally compartmentalized physical and behavioral health services remain the general approach in ongoing payment and delivery system reforms, such as accountable care organizations.26 One current opportunity to leverage would be the Health Homes option in the Affordable Care Act. This option provides states a higher federal match rate (90%) during the first 2 years to develop programs to enhance care coordination and integrate physical and behavioral health services for Medicaid members with multiple chronic conditions.
Many homeless individuals are likely to be eligible for Health Homes because of their multiple and co-occurring physical and behavioral health conditions. States can develop innovative care delivery models with the support of designated providers, such as health care for the homeless programs, who have a long-standing and established relationship with homeless individuals. These designated providers are likely to be homeless individuals’ principal point of contact with the health care delivery system, and they are well equipped to coordinate services for mental illness and substance use disorders among homeless people. In other areas, Health Homes may need to add specialized services to those offered by local mental health providers or community health centers.
The significantly high number of ambulatory care visits among people with frequent hospitalizations and ED visits indicates that this group has complex care needs. A previous analysis indicated that most ambulatory care visits (90%) were for general medical conditions, and only 10% were attributable to behavioral health disorders.4 Although not reported here, these ambulatory care visits were evenly split between BHCHP and other providers. It is likely that frequent users received care from multiple providers, which could pose significant challenges in maintaining the care continuum and engagement. Medical subspecialty visits are also expected in this population with great disease burden. However, we do not have complete information to verify the specialties of other providers. Further study is warranted to examine the association between these health care services and to identify opportunities and strategies for care improvement.
We also found that in this group of individuals, unstable housing is a significant contributor to frequent hospitalizations and ED visits. A lack of housing makes health care delivery more complex. Leading diagnoses for general medical hospitalizations indicated poor care of injuries and problems in managing chronic conditions. Simple regimens such as diet, exercise, and insulin use for a diabetic patient may become insurmountable challenges on the street. Violence and injuries are also a constant risk, with many individuals arriving in the ED with a diagnosis of injuries or pain. Conventional medical intervention models alone are unlikely to reduce frequent hospitalizations and ED visits for homeless people. Studies have shown that stable housing with adequate support helps reduce substance use, acute care services, and health care expenditures.27–30 More specifically, targeted investments in care coordination and housing together may be needed to improve the quality and cost effectiveness of care for homeless people. However, many current programs are limited to grant-funded initiatives or not scalable in their current health care system. This effort would require interagency support to couple medical services with housing resources, but it would be well worth the effort. Our analysis suggests that moving a person from the streets to stable housing could reduce ED visits by half and hospitalizations by one quarter or more.
Limitations
Using comprehensive information from linked Medicaid administrative data and health care for the homeless program data, we have identified several areas for states to develop effective strategies to help manage the complex care needs of insured homeless people. Nevertheless, several limitations warrant consideration in interpreting our findings. First, data used in this analysis show results before recent state initiatives taken by BHCHP, such as implementation of a patient-centered medical home model and recent Massachusetts primary care payment reform. The utilization pattern might be changing with a more patient-centered approach. Second, this is a cross-sectional study with 1 year of data. We are not able to compare results during the pre-Medicaid expansion era. Also, the housing status used in the study was the last known place of residence in CY2010. When data are available, time-varying housing status could be considered to reflect the dynamic housing status throughout the year and improve the modeling. Third, our study was located in a region with a higher than average number of hospital beds and health care providers per capita, which have been shown to contribute to higher utilization.31
Conclusions
Homeless individuals, particularly those with co-occurring mental illness and substance use disorders and those without stable housing, experienced heavy inpatient and ED use. States could consider provisions under the Affordable Care Act (e.g., Medicaid expansion and Health Homes) jointly with increased housing resources to meet the needs of homeless individuals, which may improve the quality and cost effectiveness of care. These efforts can target individuals with increased risk of high utilization and better engage them in preventive care to help manage health conditions and reduce inappropriate utilization. Expanded health care coverage without concomitant improvements in housing accessibility could increase health care utilization but have relatively little impact on the health and well-being of individuals experiencing homelessness.
Acknowledgments
Findings from the initial analysis for this article were presented at the 141st Conference of the American Public Health Association; November 2–6, 2013; Boston, MA.
Note. This article is solely the responsibility of the authors and does not necessarily reflect the opinions or policies of MassHealth or of the Commonwealth of Massachusetts Executive Office of Health and Human Services.
Human Participant Protection
The institutional review boards at the University of Massachusetts Medical School and Harvard School of Public Health reviewed and approved this study.
References
- 1.Padgett DK, Struening EL. Victimization and traumatic injuries among the homeless: associations with alcohol, drug, and mental problems. Am J Orthopsychiatry. 1992;62(4):525–534. doi: 10.1037/h0079369. [DOI] [PubMed] [Google Scholar]
- 2.Padgett DK, Struening EL, Andrews H, Pittman J. Predictors of emergency room use by homeless adults in New York City: the influence of predisposing, enabling and need factors. Soc Sci Med. 1995;41(4):547–556. doi: 10.1016/0277-9536(94)00364-y. [DOI] [PubMed] [Google Scholar]
- 3.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 4.Bharel M, Lin W-C, Zhang J, O’Connell E, Taube R, Clark RE. Health care utilization patterns of homeless individuals in Boston: preparing for Medicaid expansion under the Affordable Care Act. Am J Public Health. 2013;103(suppl 2):S311–S317. doi: 10.2105/AJPH.2013.301421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–220. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778–784. doi: 10.2105/ajph.92.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hwang SW, Chambers C, Chiu S et al. A comprehensive assessment of health care utilization among homeless adults under a system of universal health insurance. Am J Public Health. 2013;103(suppl 2):S294–S301. doi: 10.2105/AJPH.2013.301369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chambers C, Chiu S, Katic M et al. High utilizers of emergency health services in a population-based cohort of homeless adults. Am J Public Health. 2013;103(suppl 2):S302–S310. doi: 10.2105/AJPH.2013.301397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chambers C, Katic M, Chiu S et al. Predictors of medical or surgical and psychiatric hospitalizations among a population-based cohort of homeless adults. Am J Public Health. 2013;103(suppl 2):S380–S388. doi: 10.2105/AJPH.2013.301646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Center for Health Statistics. Health, United States, 2013: With Special Feature on Prescription Drugs. Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- 11. Patient Protection and Affordable Care Act, Pub L No. 111–148, 42 U.S.C. §§ 18001-18121 (2010)
- 12.Ku BS, Scott KC, Kertesz SG, Pitts SR. Factors associated with use of urban emergency departments by the US homeless population. Public Health Rep. 2010;125(3):398–405. doi: 10.1177/003335491012500308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han B, Wells BL, Taylor AM. Use of the Health Care for the Homeless Program services and other health care services by homeless adults. J Health Care Poor Underserved. 2003;14(1):87–99. [PubMed] [Google Scholar]
- 14.Office of Community Planning and Development. The 2010 Annual Homeless Assessment Report to Congress. Washington, DC: US Department of Housing and Urban Development, Office of Community Planning and Development; 2012. [Google Scholar]
- 15.O’Connell JJ, Oppenheimer SC, Judge CM et al. The Boston Health Care for the Homeless Program: a public health framework. Am J Public Health. 2010;100(8):1400–1408. doi: 10.2105/AJPH.2009.173609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 17.Pope GC, Kautter J, Ellis RP et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004;25(4):119–141. [PMC free article] [PubMed] [Google Scholar]
- 18.Peppe EM, Mays JW, Chang HC, Becker E, DiJulio B. Characteristics of Frequent Emergency Department Users. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2007. [Google Scholar]
- 19.Zuckerman S, Shen Y-C. Characteristics of occasional and frequent emergency department users. Med Care. 2004;42(2):176–182. doi: 10.1097/01.mlr.0000108747.51198.41. [DOI] [PubMed] [Google Scholar]
- 20.Blank FSJ, Li H, Henneman PL et al. A descriptive study of heavy emergency department users at an academic emergency department reveals heavy ED users have better access to care than average users. J Emerg Nurs. 2005;31(2):139–144. doi: 10.1016/j.jen.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 21.Lin WC, Zhang J, Leung GY, Clark RE. Chronic physical conditions in older adults with mental illness and/or substance use disorders. J Am Geriatr Soc. 2011;59(10):1913–1921. doi: 10.1111/j.1532-5415.2011.03588.x. [DOI] [PubMed] [Google Scholar]
- 22.Clark RE, Weir S, Ouellette RA, Zhang J, Baxter JD. Beyond health plans: behavioral health disorders and quality of diabetes and asthma care for Medicaid beneficiaries. Med Care. 2009;47(5):545–552. doi: 10.1097/MLR.0b013e318190db45. [DOI] [PubMed] [Google Scholar]
- 23.Clark RE, Samnaliev M, McGovern MP. Impact of substance disorders on medical expenditures for Medicaid beneficiaries with behavioral health disorders. Psychiatr Serv. 2009;60(1):35–42. doi: 10.1176/ps.2009.60.1.35. [DOI] [PubMed] [Google Scholar]
- 24.Druss BG, Rosenheck RA, Desai MM, Perlin JB. Quality of preventive medical care for patients with mental disorders. Med Care. 2002;40(2):129–136. doi: 10.1097/00005650-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Bartels SJ, Clark RE, Peacock WJ, Dums AR, Pratt SI. Medicare and Medicaid costs for schizophrenia patients by age cohort compared with costs for depression, dementia, and medically ill patients. Am J Geriatr Psychiatry. 2003;11(6):648–657. doi: 10.1176/appi.ajgp.11.6.648. [DOI] [PubMed] [Google Scholar]
- 26.Lewis VA, Colla CH, Tierney K, Van Citters AD, Fisher ES, Meara E. Few ACOs pursue innovative models that integrate care for mental illness and substance abuse with primary care. Health Aff (Millwood) 2014;33(10):1808–1816. doi: 10.1377/hlthaff.2014.0353. [DOI] [PubMed] [Google Scholar]
- 27.Martinez TE, Burt MR. Impact of permanent supportive housing on the use of acute care health services by homeless adults. Psychiatr Serv. 2006;57(7):992–999. doi: 10.1176/ps.2006.57.7.992. [DOI] [PubMed] [Google Scholar]
- 28.Larimer ME, Malone DK, Garner MD et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- 29.Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771–1778. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 30.Poulin SR, Maguire M, Metraux S, Culhane DP. Service use and costs for persons experiencing chronic homelessness in Philadelphia: a population-based study. Psychiatr Serv. 2010;61(11):1093–1098. doi: 10.1176/ps.2010.61.11.1093. [DOI] [PubMed] [Google Scholar]
- 31.Wennberg JE, Freeman JL, Culp WJ. Are hospital services rationed in New Haven or over-utilised in Boston? Lancet. 1987;329(8543):1185–1189. doi: 10.1016/s0140-6736(87)92152-0. [DOI] [PubMed] [Google Scholar]


