Abstract
Objectives. We sought to describe changes in young adults’ routine care and usual sources of care (USCs), according to provider specialty, after implementation of extended dependent coverage under the Affordable Care Act (ACA) in 2010.
Methods. We used Medical Expenditure Panel Survey data from 2006 to 2012 to examine young adults’ receipt of routine care in the preceding year, identification of a USC, and USC provider specialties (pediatrics, family medicine, internal medicine, and obstetrics and gynecology).
Results. The percentage of young adults who sought routine care increased from 42.4% in 2006 to 49.5% in 2012 (P < .001). The percentage identifying a USC remained stable at approximately 60%. Among young adults with a USC, there was a trend between 2006 and 2012 toward increasing percentages with pediatric (7.6% vs 9.1%) and family medicine (75.9% vs 80.9%) providers and declining percentages with internal medicine (11.5% vs 7.6%) and obstetrics and gynecology (5.0% vs 2.5%) providers.
Conclusions. Efforts under the ACA to increase health insurance coverage had favorable effects on young adults’ use of routine care. Monitoring routine care use and USC choices in this group can inform primary care workforce needs and graduate medical education priorities across specialties.
Decreasing the number of uninsured Americans is a central goal of the Affordable Care Act (ACA; Pub L No. 111-148). Historically, young adults have been less likely than adolescents and older adults to have insurance coverage.1–3 In addition to low coverage rates, previous research suggests that emergency department use is higher among young adults than adolescents and that use of primary care services is lower.2,4,5 This decreased access to and use of health care occurs during a period of risky behavior that results in high preventable mortality and morbidity rates among young adults.6–8
The ACA offers several mechanisms for increasing health insurance coverage among young adults. One of the earliest expansions under the ACA occurred on September 23, 2010, when all insurance plans offering dependent coverage were required to extend this coverage to young adults until they were 26 years old.1 The requirement does not depend on an individual’s living situation or student, marriage, or tax-dependent status. Previously, most employer-based health insurance plans terminated young people’s dependent coverage at the age of 19 years or upon their graduation from college.9 The extended dependent coverage provision has resulted in more than 3 million young adults gaining health insurance coverage.10
One anticipated impact of expanded insurance coverage for young adults was increased access to primary care services.11–15 Studies involving data from 2011, immediately after implementation of extended dependent coverage, demonstrated increases in young adults’ receipt of routine and preventive care16 and declines in the numbers of young adults forgoing care and experiencing delays in care as a result of high costs.12 However, other researchers found no significant changes in young adults’ use of routine health care services in 2011 and 2012, and no significant increases in the proportion of young adults with a usual source of care (USC).12,15,17
Recent health insurance marketplaces and 2013 state-based Medicaid expansions have further increased rates of insurance coverage among young adults and are expected to subsequently affect their use of health care.18–20 Because young adults may see providers from multiple specialties, including pediatrics, family medicine, internal medicine, and obstetrics and gynecology, monitoring not only whether their use of routine care changes but also what types of providers they identify as their USC can inform efforts to determine how to best meet this population’s health care needs. In this study, we sought to add to the existing literature by using nationally representative data from 2006 to 2012 to describe changes in young adults’ use of routine care and their USC choices.
METHODS
We used data from the 2006 to 2012 versions of the Medical Expenditure Panel Survey (MEPS) to assess trends in use of routine care and USCs among young adults before and after implementation of the ACA dependent coverage provision.
Data Source
The MEPS is an ongoing large-scale annual household panel survey sponsored by the Agency for Healthcare Research and Quality that provides data from a nationally representative sample of the US civilian noninstitutionalized population.21 The survey includes data on household health service use and expenditures, insurance coverage, sources of payment, access to care, and health care quality. Data are collected in 5 rounds of interviews from panels of approximately 15 000 households over 2 years.
The preventive care section of the survey’s household component, which includes questions on routine care use, is incorporated into rounds 3 and 5, whereas the access to care section, with questions pertaining to USC, is included in rounds 2 and 4. Typically, one person per household provides information for all household members. In our analysis, we pooled data for the calendar years 2006 (the second year of panel 10 and the first year of panel 11) through 2012 (the second year of panel 16 and the first year of panel 17). We included young adults aged 19 to 25 years in our study.
Outcome Variables
Study outcomes were receipt of a routine check-up in the preceding 12 months, identification of a USC, and USC provider specialty. MEPS participants were asked “About how long has it been since (the young adult) had a routine check-up by a doctor or other health professional?” Young adults were said to have a USC if they usually went to a clinic, health center, or other place if they were sick or needed medical advice about their health. If a young adult was reported to have a USC, the type and specialty of the provider were documented: pediatric, family or general medicine (hereafter FM), internal medicine (IM), or obstetrics and gynecology (OB/GYN; only in the case of women). Although an additional “other” category (inclusive of physicians in other specialties or advanced practice nurses) was included, we omitted it from subanalyses focusing on provider specialties because fewer than 5% of responses fell in this category.
Covariates
Covariates were drawn from the MEPS household component. Health insurance coverage was defined as follows: private insurance coverage indicated that a person had private coverage any time during the year; public insurance indicated only public insurance coverage during the year; and uninsured indicated lack of insurance for the entire year. Age was defined as the respondent’s age at the end of each calendar year. Respondents were stratified into younger (19–22 years) and older (23–25 years) groups.
Race/ethnicity was coded as non-Hispanic White (including the fewer than 5% of respondents who reported other or multiple races), non-Hispanic Black, Hispanic, or non-Hispanic Asian. Family income was reported as a percentage of the federal poverty level: less than 125% (low), 125% to 400% (medium), or above 400% (high).21 Employment was coded as any or no employment in the preceding year. Student status was assessed for participants up to the age of 23 years; responses were collapsed, with a yes response indicating that the participant was a full- or part-time student. Finally, a binary marital status indicator was created in which a yes response indicated that the respondent was married at the end of the calendar year in question.
Statistical Analysis
We used pooled data from 2006 to 2012 to summarize study outcomes according to young adults’ sociodemographic characteristics, and outcomes were compared via χ2 test. Logistic regression models adjusting for age as a continuous variable were used to compare the percentages of young adults in different groups with a routine visit in the preceding year, a USC, and insurance coverage from 2006 to 2012. We calculated yearly rates by including indicator variables for each calendar year. We considered 2010 a transition period because extended dependent coverage was implemented in September of that year. Unadjusted logistic regression was used to compare the period after the implementation of the ACA (2011–2012) with the preimplementation period (2006–2009). We conducted tests for trends by including a grouped linear calendar year term.
When examining young adults’ USCs by provider specialty over time, we collapsed years into 3 periods (2006–2007, 2008–2009, and 2011–2012) because of small cell sizes. Cells with fewer than 100 observations generated estimates that must be interpreted with caution as a result of data instability. These data are presented as descriptive trends.
Among young adults who indicated that they had a USC, a logistic regression model was used to estimate the likelihood, by provider specialty, that they had made routine visits in given 2-year time periods. USC, the primary predictor, was nested according to gender into 7 categories (e.g., female respondent with pediatric USC). The model included an interaction term for the nested provider categories and time period (2006–2007, 2008–2009, 2011–2012). Other covariates (age, race/ethnicity, family income, region of residence, marital and employment status) were selected according to whether P < .2 in univariable models. We used coefficients standardized on the other covariates in the model to estimate marginal probabilities of receipt of usual care by provider specialty and gender.
As a means of accounting for the complex stratified multistage design, sampling weights and design-based variance estimators were used to produce nationally representative estimates; all proportions presented here are weighted. Our analyses focused on the subpopulation of young adults in the MEPS sample so that variances could be appropriately estimated.22 The significance level was set at P < .05. The svy suite of commands in Stata version 13.1 (StataCorp LP, College Station, TX) was used in conducting all analyses.
RESULTS
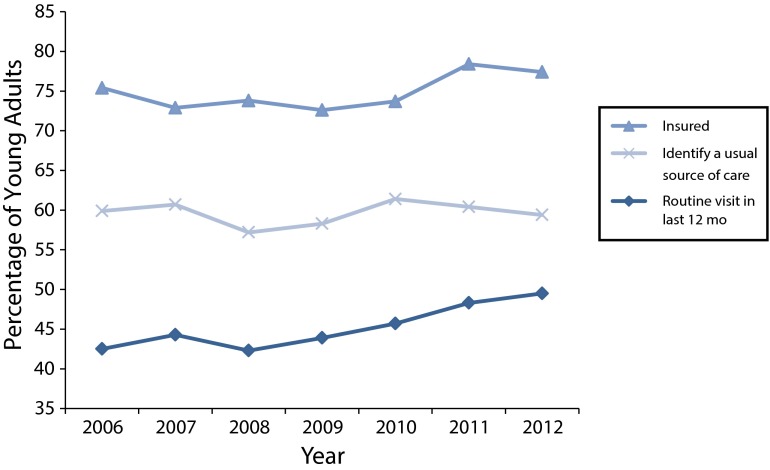
In the pooled 2006 to 2012 MEPS data, the initial unweighted samples of young adults aged 19 to 25 years accounted for 23 396 person-years. The majority of young adults in the sample were privately insured, non-Hispanic White, unmarried, and employed (Table 1). Over the pooled 2006 to 2012 period, 61.3% and 13.6% of young adults were privately and publicly insured, respectively (Table 1). The percentage of young adults with insurance coverage (either private or public) increased from 75.5% in 2006 to 78.4% in 2011 and 77.4% in 2012 (P < .001 for comparison of 2011–2012 with 2006–2009; P = .009 for test of trend; Figure 1).
TABLE 1—
Percentages of Young Adults Who Reported a Routine Health Care Visit in the Preceding Year and a Usual Source of Care, by Demographic Characteristics: Medical Expenditure Panel Survey, United States, 2006–2012
| Total, % | Routine Visit in Past Year, % or Pa | Identified a Usual Source of Care, % or Pa | |
| Total | 45.3 | 59.6 | |
| Insurance status | < .001 | < .001 | |
| Any private | 61.3 | 49.2 | 68.8 |
| Public only | 13.6 | 56.5 | 63.9 |
| Uninsured | 25.1 | 26.4 | 35.6 |
| Age group, y | < .001 | ||
| 19–22 | 56.3 | 45.7 | 63.3 |
| 23–25 | 43.7 | 44.8 | 54.9 |
| Gender | < .001 | < .001 | |
| Male | 50.9 | 34.4 | 52.7 |
| Female | 49.2 | 56.3 | 66.8 |
| Race/ethnicity | < .001 | < .001 | |
| Non-Hispanic White | 54.3 | 45.0 | 65.7 |
| Non-Hispanic Black | 20.2 | 52.8 | 58.2 |
| Hispanic | 19.6 | 38.0 | 45.8 |
| Non-Hispanic Asian | 6.0 | 46.1 | 53.4 |
| Region of residence | < .001 | < .001 | |
| Northeast | 18.4 | 59.0 | 71.7 |
| Midwest | 21.1 | 44.5 | 64.4 |
| South | 37.1 | 43.3 | 53.1 |
| West | 23.4 | 38.3 | 56.4 |
| Family income category | < .001 | < .001 | |
| Low (< 125% FPL) | 24.3 | 44.3 | 52.2 |
| Middle (125%–400% FPL) | 46.9 | 43.1 | 56.4 |
| High (> 400% FPL) | 28.8 | 49.8 | 71.2 |
| Student statusb | < .001 | < .001 | |
| Student | 52.5 | 51.2 | 70.4 |
| Nonstudent | 47.5 | 39.4 | 53.2 |
| Marital status | <.05 | ||
| Married | 13.6 | 46.6 | 56.3 |
| Not married | 86.4 | 45.1 | 60.2 |
| Employment status | < .001 | <.05 | |
| Employed | 71.2 | 43.5 | 58.9 |
| Not employed | 28.9 | 49.6 | 61.6 |
Note. FPL = federal poverty level. All percentages are weighted to account for the complex stratified multistage design of the survey. The sample size was n = 23 396 person-years.
Significant within-category differences according to the χ2 test.
Limited to respondents younger than 23 years.
FIGURE 1—
Percentage of young adults who reported having insurance (either private or public), identified a usual source of care, and reported having made a routine health care visit: Medical Expenditure Panel Survey, United States, 2006–2012.
Note. All models adjusted for age. All percentages are weighted to account for the survey’s complex stratified multistage design.
Receipt of Routine Care
The percentage of young adults with routine visits increased from 42.4% in 2006 to 48.3% in 2011 and 49.5% in 2012 (P < .001 for test of trend and for comparison of 2011–2012 with 2006–2009; Figure 1). Young adults who had had a routine visit in the preceding 12 months were more likely than those who had not to be publicly insured, female, and non-Hispanic Black; to live in the Northeast and have a high income; and to be a student or unemployed (all Ps < .001; Table 1).
Identification of a Usual Source of Care
There was no significant change from 2006 to 2012 in the proportion of young adults who identified a USC (Figure 1). Overall, approximately 59% of young adults identified a USC over the study period (Table 1). Young adults with a USC were more likely to have had a routine visit (71.8%) than those without a USC (32.1%; P < .001) and more likely to be privately (68.7%) or publicly (63.3%) insured as opposed to uninsured (35.2%; P < .001). They were also more likely to be in the younger age group (19–22 vs 23–25 years); to be female, non-Hispanic White, a student, unmarried, and unemployed; to live in the Northeast or Midwest; and to have a high income (Table 1). Among participants with a USC, 96.9% reported using their USC for preventive care.
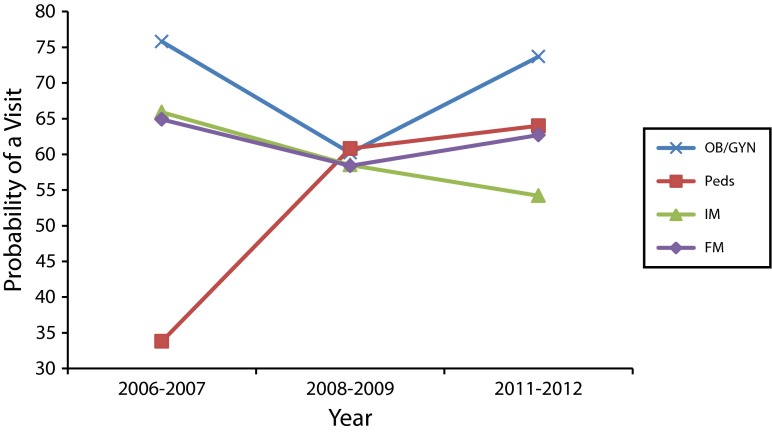
Provider Specialty
We noted a trend over time between 2006 and 2012 according to which an increasing percentage of young adults with a USC reported pediatricians (7.6% in 2006–2007 vs 9.1% in 2011–2012) and FM providers (75.9% vs 80.9%) as their USC. Conversely, there was a trend toward declining percentages of young adults reporting IM (11.5% to 7.6%) and OB/GYN (5.0% to 2.5%) providers as their USC (Table 2).
TABLE 2—
Changes in Usual Source of Care (USC) Provider Specialties: Medical Expenditure Panel Survey, United States, 2006–2012
| USC Provider Specialty | 2006–2007, % (No.) | 2008–2009, % (No.) | 2011–2012, % (No.) |
| Pediatrics | 7.6 (91) | 7.6 (119) | 9.1 (117) |
| Family medicine | 75.9 (810) | 80.1 (949) | 80.9 (922) |
| Internal medicine | 11.5 (117) | 8.8 (111) | 7.6 (96) |
| Obstetrics and gynecology | 5.0 (59) | 3.5 (60) | 2.5 (42) |
Note. All percentages are weighted to account for the complex stratified multistage design of the survey. Cells including data from fewer than 100 respondents must be interpreted with caution.
The overall trends indicating increased numbers of routine visits by young adults were influenced by increases in young adult women’s routine visits to pediatricians, for which the standardized probability increased from 0.34 in 2006–2007 to 0.64 in 2011–2012 (Figure 2). Trends in numbers of routine visits among young adult men across all specialties remained stable over the study period.
FIGURE 2—
Probability of young adult women having routine health care visits in the preceding 12 months, by usual source of care provider specialty: Medical Expenditure Panel Survey, United States, 2006–2012.
Note. FM = family medicine; IM = internal medicine; OB/GYN = obstetrics and gynecology; Peds = pediatrics. The following covariates were included in the model: study year, age, race/ethnicity, family income, region of residence, marital status, and employment status.
DISCUSSION
Our findings reveal changes in patterns of primary health care use among young adults aged 19 to 25 years after the first efforts under the ACA in September 2010 to increase health insurance enrollment in this population via dependent coverage expansion. We demonstrated encouraging increases in young adults’ insurance coverage and use of routine care services. Although the overall proportion of young adults identifying a USC did not change over the study period, we identified trends suggesting changes in their choices of providers. Our results offer an important context for ongoing monitoring strategies given young adults’ increased opportunities to obtain insurance independent of parental coverage through the 2013 ACA health insurance marketplaces and state-based Medicaid expansions.9,18 Our findings highlight opportunities for the ACA to improve young adults’ health care and provide guidance on issues that warrant further attention.
Young adults were more likely to have had insurance coverage and to have undergone routine check-ups after the 2010 ACA expansion of dependent insurance coverage to the age of 26 years, showing that it is feasible to increase access to and use of health care services in this sometimes hard-to-reach group. Nonetheless, in 2012, 50% of young adults reported not having had a routine check-up in the preceding year, representing a missed opportunity for them to receive evidence-based preventive services including vaccinations and screening for obesity, sexually transmitted infections, depression, and tobacco and alcohol use.23 These recommended services allow for prevention, early identification, and management of behaviors and risk factors that have major influences on young adults’ health as well as overall population health.
In addition, young adults with chronic illnesses or risk markers for early-onset adult diseases identified in youth (e.g., hypertension) may not be receiving routine monitoring and management services. In the future, there is a need to ensure that young adults with insurance coverage use appropriate routine health care services and to more clearly define high-quality care and comprehensive preventive health care goals for this population.23,24
Opportunities for improved primary care access are linked to USCs because people with a USC are more likely to use appropriate care services and to have continuity of care, especially when they also have insurance coverage.2,25–31 In our study, as expected, young adults with a USC were much more likely than those without a USC to have had a routine visit and to be insured. However, the percentage of young adults without a USC, a sizable 40%, did not change after the 2010 ACA initiatives. Educating newly insured young adults on how to identify a primary care provider could even further enhance their access to care.32 Alternatively, although the benefits of USCs have been well documented, an access-focused health care model or metric that relies on a USC may not be ideal for young adults given that they are in a transitional phase of life, with frequent residential, educational, and employment changes.33 These transitions can result in churning between health insurance and health care providers and affect young adults’ ability to obtain a USC and continuity of care.34
We noted trends in the distribution of providers among the young adults in our study with a USC. An increasing majority of young adults saw FM providers, suggesting that, at a population level, quality of care for young adults will be driven by FM services. Although not explored in our study, it is possible that pediatric and IM providers are disproportionately seeing young adults with complex or chronic medical needs and thus need to be skilled in providing high-quality care to these patients. Several factors may be involved in the other shifts we observed in types of young adult care providers. The extension of dependent insurance coverage may result in continued capitation or assignment of young adults to their childhood pediatrician, or limited access to general internists may be pushing young adults toward FM and pediatric providers. The decrease in the number of young women with OB/GYN providers may be attributable to the revised cervical cancer screening recommendations instituted in the early 2000s, which for many delayed the need for pelvic examinations.35
Monitoring how young adults seek routine care and select providers can inform future primary care workforce needs. This is especially relevant as further gains in insurance coverage and health care use among young adults and millions of other Americans, through the ACA’s health insurance marketplaces and state-based Medicaid expansions, increase the projected shortage of primary care physicians.9,18,19,36 An adequate provider network skilled in delivering primary care services to young adults will be needed to meet the anticipated growth in demand in this group.37
Providers who see young adult patients should be aware of the unique needs of this age group and the opportunities inherent in delivering services to these patients. There are normal developmental variations among these emerging young adults with respect to perceptions of risk, experimentation, and patterns of behaviors that affect health, autonomy, and living, employment, and educational scenarios.33 Young adults, including those with chronic illnesses, disabilities, and identified risks for early-onset adult diseases, are acquiring skills to independently manage their health and interact with complex health care systems.33,38
Because young adults seek primary care from providers in multiple specialties, our findings have implications for revising graduate medical education curricula across these disciplines. There are specialty-specific strengths and weaknesses in training related to the health issues faced by young adults, including development, recommended preventive services, reproductive health, and quality of care. For example, the mandatory rotation requirements designed to improve adolescent medicine training in pediatric residencies over the past 2 decades have promoted high-quality pediatric care for more children through late adolescence and early young adulthood.39 Multidisciplinary collaboration among the specialties caring for young adults could lead to improvements in the health care services offered to this group.40
Limitations
Although our study involved a nationally representative sample and data gathered before and after implementation of a new national health policy, it is subject to limitations. For example, the timing of the policy’s implementation is complicated by the phase-in period for extended dependent coverage; 37 states encouraged expansion and many major insurance companies responded to calls for early implementation of extended dependent coverage before September 2010.41,42 Because of this phase-in period and the limitations of our study design, some of our findings, such as the increase in the number of young adults seeking routine care and the shifts in USC provider types, may have been attributable to secular trends in addition to or instead of the ACA. Regardless, our study’s implications with respect to anticipating workforce development and graduate medical education needs are the same.
Also, MEPS data are self-reported or reported by a household representative, and they are thus subject to recall error. Although MEPS does not determine the amount or proportion of a person’s care that is provided by his or her USC, the vast majority of our participants reported using their USC for preventive care as well as for new health problems. Finally, because 40% of young adults in our study did not identify a USC, some of our analyses focusing on provider specialties may have produced unstable estimates as a result of small cell sizes, even when multiple years of data were pooled. However, we believed that it was important to examine the distribution of USC provider specialties around the implementation of the ACA given the potential implications with respect to provider training and workforce issues.
Conclusions
The ACA has provided young adults with new opportunities to obtain insurance coverage, which influences their access to and use of health care services and has implications for providers across multiple specialties. Although our study focused on changes occurring after implementation of extended dependent coverage in 2010, we anticipate that the health insurance marketplaces and state-based Medicaid expansions implemented in 2013 will further affect young adults’ use of health care.9,18 Monitoring changes in young adults’ primary care, including their use of routine care and choice of usual providers, can inform future primary care workforce needs and priorities for graduate medical education curricula across specialties, with the goal of optimizing care services for this population.
Acknowledgments
This study was supported in part by the Robert Wood Johnson Foundation Clinical Scholars Program at the University of Pennsylvania.
An earlier version of the study was presented at the national meeting of the Pediatric Academic Societies; May 3–6; Vancouver, British Columbia, Canada.
Human Participant Protection
No protocol approval was needed for this study because no human participants were involved.
References
- 1.Collins SR, Nicholson JL. Rite of passage: young adults and the Affordable Care Act of 2010. Issue Brief (Commonw Fund) 2010;87:1–24. [PubMed] [Google Scholar]
- 2.Callahan ST, Cooper WO. Uninsurance and health care access among young adults in the United States. Pediatrics. 2005;116(1):88–95. doi: 10.1542/peds.2004-1449. [DOI] [PubMed] [Google Scholar]
- 3.Cohen RA, Bloom B. Access to and utilization of medical care for young adults ages 20–29 years: United States, 2008. Available at: http://www.cdc.gov/nchs/data/databriefs/db29.PDF. Accessed June 4, 2015. [PubMed]
- 4.Chua KP, Schuster MA, McWilliams JM. Differences in health care access and utilization between adolescents and young adults with asthma. Pediatrics. 2013;131(5):892–901. doi: 10.1542/peds.2012-2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fortuna RJ, Robbins BW, Mani N, Halterman JS. Dependence on emergency care among young adults in the United States. J Gen Intern Med. 2010;25(7):663–669. doi: 10.1007/s11606-010-1313-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mulye TP, Park MJ, Nelson CD, Adams SH, Irwin CE, Jr, Brindis CD. Trends in adolescent and young adult health in the United States. J Adolesc Health. 2009;45(1):8–24. doi: 10.1016/j.jadohealth.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 7.McCracken M, Jiles R, Blanck HM. Health behaviors of the young adult U.S. population: Behavioral Risk Factor Surveillance System, 2003. Prev Chronic Dis. 2007;4(2):A25. [PMC free article] [PubMed] [Google Scholar]
- 8.Park MJ, Scott JT, Adams SH, Brindis CD, Irwin CE., Jr Adolescent and young adult health in the United States in the past decade: little improvement and young adults remain worse off than adolescents. J Adolesc Health. 2014;55(1):3–16. doi: 10.1016/j.jadohealth.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 9.Goldman TR. Young adults and the Affordable Care Act. Available at: http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=105. Accessed June 4, 2015.
- 10.Sommers BD. Number of Young Adults Gaining Insurance Due to the Affordable Care Act Now Tops 3 Million. Washington, DC: US Department of Health and Human Services; 2012. [Google Scholar]
- 11.Kirzinger WK, Cohen RA, Gindi RM. Trends in insurance coverage and source of private coverage among young adults aged 19–25: United States, 2008–2012. Available at: http://www.cdc.gov/nchs/data/databriefs/db137.htm. Accessed June 4, 2015. [PubMed]
- 12.Sommers BD, Buchmueller T, Decker SL, Carey C, Kronick R. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Aff (Millwood) 2013;32(1):165–174. doi: 10.1377/hlthaff.2012.0552. [DOI] [PubMed] [Google Scholar]
- 13.Antwi YA, Moriya AS, Simon K. Effects of Federal Policy to Insure Young Adults: Evidence From the 2010 Affordable Care Act Dependent Coverage Mandate. Cambridge, MA: National Bureau of Economic Research; 2012. [Google Scholar]
- 14.Collins SR, Rasmussen PW, Garber T, Doty MM. Covering young adults under the Affordable Care Act: the importance of outreach and Medicaid expansion: findings from the Commonwealth Fund Health Insurance Tracking Survey of Young Adults, 2013. Issue Brief (Commonw Fund) 2013;21:1–15. [PubMed] [Google Scholar]
- 15.Chua KP, Sommers BD. Changes in health and medical spending among young adults under health reform. JAMA. 2014;311(23):2437–2439. doi: 10.1001/jama.2014.2202. [DOI] [PubMed] [Google Scholar]
- 16.Lau JS, Adams SH, Park MJ, Boscardin WJ, Irwin CE., Jr Improvement in preventive care of young adults after the Affordable Care Act: the Affordable Care Act is helping. JAMA Pediatr. 2014;168(12):1101–1106. doi: 10.1001/jamapediatrics.2014.1691. [DOI] [PubMed] [Google Scholar]
- 17.Kotagal M, Carle AC, Kessler LG, Flum DR. Limited impact on health and access to care for 19- to 25-year-olds following the Patient Protection and Affordable Care Act. JAMA Pediatr. 2014;168(11):1023–1029. doi: 10.1001/jamapediatrics.2014.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Office of the Assistant Secretary for Planning and Evaluation. Health Insurance Marketplace: Summary Enrollment Report for the Initial Annual Open Enrollment Period. Washington, DC: US Department of Health and Human Services; 2014. [Google Scholar]
- 19.Dubay L, Kenney GM, Buettgens M, Wengle E, Dev J. Measuring Medicaid and CHIP Enrollment Progress Under the Affordable Care Act: An Update. Washington, DC: Urban Institute; 2014. [Google Scholar]
- 20.McMorrow S, Kenney GM, Long SK, Anderson N. Uninsurance among young adults continues to decline, particularly in Medicaid expansion states. Health Aff (Millwood) 2015;34(4):616–620. doi: 10.1377/hlthaff.2015.0044. [DOI] [PubMed] [Google Scholar]
- 21.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. Available at: http://meps.ahrq.gov/mepsweb/. Accessed June 4, 2015.
- 22.Agency for Healthcare Research and Quality. Computing standard errors for MEPS estimates. Available at: http://meps.ahrq.gov/mepsweb/survey_comp/standard_errors.jsp. Accessed June 4, 2015.
- 23.Ozer EM, Urquhart JT, Brindis CD, Park MJ, Irwin CE., Jr Young adult preventive health care guidelines: there but can’t be found. Arch Pediatr Adolesc Med. 2012;166(3):240–247. doi: 10.1001/archpediatrics.2011.794. [DOI] [PubMed] [Google Scholar]
- 24.Cogan JA., Jr The Affordable Care Act’s preventive services mandate: breaking down the barriers to nationwide access to preventive services. J Law Med Ethics. 2011;39(3):355–365. doi: 10.1111/j.1748-720X.2011.00605.x. [DOI] [PubMed] [Google Scholar]
- 25.Sox CM, Swartz K, Burstin HR, Brennan TA. Insurance or a regular physician: which is the most powerful predictor of health care? Am J Public Health. 1998;88(3):364–370. doi: 10.2105/ajph.88.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93(5):786–791. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeVoe JE, Tillotson CJ, Lesko SE, Wallace LS, Angier H. The case for synergy between a usual source of care and health insurance coverage. J Gen Intern Med. 2011;26(9):1059–1066. doi: 10.1007/s11606-011-1666-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lau JS, Adams SH, Irwin CE, Jr, Ozer EM. Receipt of preventive health services in young adults. J Adolesc Health. 2013;52(1):42–49. doi: 10.1016/j.jadohealth.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ettner SL. The relationship between continuity of care and the health behaviors of patients: does having a usual physician make a difference? Med Care. 1999;37(6):547–555. doi: 10.1097/00005650-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Walls CA, Rhodes KV, Kennedy JJ. The emergency department as usual source of medical care: estimates from the 1998 National Health Interview Survey. Acad Emerg Med. 2002;9(11):1140–1145. doi: 10.1111/j.1553-2712.2002.tb01568.x. [DOI] [PubMed] [Google Scholar]
- 31.Franks P, Clancy CM, Nutting PA. Gatekeeping revisited—protecting patients from overtreatment. N Engl J Med. 1992;327(6):424–429. doi: 10.1056/NEJM199208063270613. [DOI] [PubMed] [Google Scholar]
- 32.Health Insurance Marketplace. From coverage to care: a roadmap to better care and a healthier you. Available at: https://marketplace.cms.gov/outreach-and-education/downloads/c2c-roadmap.pdf. Accessed June 4, 2015.
- 33.Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 34.Sommers BD, Graves JA, Swartz K, Rosenbaum S. Medicaid and marketplace eligibility changes will occur often in all states; policy options can ease impact. Health Aff (Millwood) 2014;33(4):700–707. doi: 10.1377/hlthaff.2013.1023. [DOI] [PubMed] [Google Scholar]
- 35.Henderson JT, Saraiya M, Martinez G, Harper CC, Sawaya GF. Changes to cervical cancer prevention guidelines: effects on screening among U.S. women ages 15–29. Prev Med. 2013;56(1):25–29. doi: 10.1016/j.ypmed.2012.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schwartz MD. Health care reform and the primary care workforce bottleneck. J Gen Intern Med. 2012;27(4):469–472. doi: 10.1007/s11606-011-1921-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gindi RM, Kirzinger WK, Cohen RA. Health insurance coverage and adverse experiences with physician availability: United States, 2012. Available at: http://www.cdc.gov/nchs/data/databriefs/db138.htm. Accessed June 4, 2015. [PubMed]
- 38.Tanner JL, Arnett JJ. Approaching young adult health and medicine from a developmental perspective. Adolesc Med State Art Rev. 2013;24(3):485–506. [PubMed] [Google Scholar]
- 39.Fox HB, McManus MA, Klein JD et al. Adolescent medicine training in pediatric residency programs. Pediatrics. 2010;125(1):165–172. doi: 10.1542/peds.2008-3740. [DOI] [PubMed] [Google Scholar]
- 40.Institute of Medicine. Improving the Health, Safety, and Well-Being of Young Adults: Workshop Summary. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 41.Center for Consumer Information and Insurance Oversight. Young adults and the Affordable Care Act: protecting young adults and eliminating burdens on families and businesses. Available at: https://www.dol.gov/ebsa/newsroom/fsdependentcoverage.html. Accessed June 4, 2015.
- 42.O’Hara B, Brault MW. The disparate impact of the ACA-dependent expansion across population subgroups. Health Serv Res. 2013;48(5):1581–1592. doi: 10.1111/1475-6773.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]