Abstract
Aims/Introduction
The purpose of the present study was to examine glycemic control in suboptimally controlled type 2 diabetes provided by a structured education group using the Diabetes Conversation Map™ (CM™) vs usual care in a university-based hospital primary care clinic.
Materials and Methods
This was a randomized, pragmatic clinical trial. Patients with type 2 diabetes were randomly assigned to structured education or usual care groups. The primary outcome was the difference in the mean change of glycated hemoglobin (HbA1c) from baseline to 12 months. Secondary outcomes included the percentage achieving therapeutic HbA1c goal and self-behavioral changes.
Results
A total of 245 patients were randomly assigned to two groups (CM™ group n = 121; usual care group, n = 116). The absolute reduction of HbA1c was significantly greater in the CM™ group at 3 and 6 months (Δ = −0.59% and Δ = −1.13%, P < 0.01), but the difference was no longer statistically significant at 9 and 12 months (Δ = −0.43% and Δ = −0.49%), based on an intention-to-treat analysis. A per-protocol analysis showed the significant change was maintained at 12 months (Δ = −0.67%). In the intervention group, greater percentages of patients achieved their American Association of Diabetes Educators Self-Care Behaviours™ framework (AADE7) behavioral goals at 3 months, in particular being active, problem-solving, reducing risk and health coping.
Conclusions
In type 2 diabetic patients with suboptimally controlled glucose, there were greater improvements in glucose control and self-care behavioral goals in those who underwent the CM™ education program compared with outcomes achieved in patients receiving usual care.
Keywords: Structured education, Diabetes conversation map, Self-care behavior
Introduction
Type 2 diabetes is a worldwide epidemic, and its prevalence is growing, creating a global healthcare burden. According to the International Diabetes Federation, the number of people aged 20–79 years with diabetes in 2011 globally was estimated to be 366 million, and this figure is expected to rise to 552 million by 20301. According to an analysis of the 2000–2009 claims data from Taiwan National Health Insurance (NHI), there was an increase in the prevalence of type 2 diabetes of approximately 70%, from 4.31% in 2000 to 6.38% in 20082. A survey from the National Survey of Diabetes Health Promotion Institutes from 2006 to 2011 observed an improvement of overall attainments of glycated hemoglobin (HbA1c) goal across 5 years in Taiwan3. Improvements of diabetes control can be attributed to the successful introduction of the Diabetes Medical Benefits Improvement Project and the subsequent implementation of a pay-for-performance scheme in a diabetes shared care program4,5. However, the percentage of patients attaining their goal is still low. The diabetes shared care program provides patients with diabetes self-management education at every clinic visit. To effectively manage individuals with type 2 diabetes, appropriate education, lifestyle modification, medication treatment and blood glucose monitoring are all required for effective management. Education is the foundation of care for all diabetes patients who want to achieve successful health-related outcomes6.
Diabetes self-management education (DSME) can be delivered one-on-one or in a group. Group-based DSME has the added advantage of enabling patients to meet each other and discuss issues. Educational programs are complex interventions where it is often difficult to define the ‘active ingredient’ framework7. Studies have compared the effects of group-based DSME, and owing to considerable variation in the content and forms of DSME, no standardized description of the intervention can be provided7–10. There are no reviews currently published that have identified the most effective and comprehensive format for diabetes self-care education.
The American Association of Diabetes Educators Self-Care Behaviours™ framework (AADE7) consists of seven factors essential for self-management: healthy eating, physical activity, taking medications, monitoring, problem solving (related to diabetes self-care), reducing risks of acute and chronic complications, and psychosocial aspects of living with diabetes11.
The Diabetes Conversation Maps™ (CM™) are a series of educational tools; together they comprise an innovative education method that emphasizes interactive group participation to empower people with diabetes to become actively involved in managing their disease. The educational tool program is now used in many countries, and it was launched in Taiwan in 2010 in partnership with the Taiwanese Association of Diabetes Educators. However, to date, its effectiveness has not been rigorously evaluated. The primary objective of the present study was to examine glycemic control in suboptimally controlled type 2 diabetes provided by a structured education group by comparing outcomes obtained using the CM™ method vs usual care (UC) in the primary care diabetes clinic of a university-based hospital. The secondary outcome was adherence of self-care behavior after receiving the education, using the AADE7™ patient self-assessment and a goal attainment assessment.
Materials and Methods
Study Design
The present randomized, pragmatic clinical trial was carried out in type 2 diabetic patients randomly assigned to structured education or UC groups. In the structured education group we used the CM™ to provide patient education. The study was approved by the ethics committee of Chung Shan Medical University Hospital, and complies with the Helsinki Declaration. All participants provided written informed consent before enrollment.
Study Setting and Patient Population
The trial was carried out at two diabetes clinics in central Taiwan. Participants with type 2 diabetes treated with an oral antidiabetic drug with or without insulin, aged 20–70 years and with HbA1c more than 7.0% were eligible for enrolment. We excluded participants if they were pregnant, breastfeeding or intended to become pregnant, had psychotic disorders, or were participating in another research study. All Taiwan citizens are covered by national health insurance. Primary care for diabetes is provided by general practitioners (GPs) and diabetologists. Diabetes education is often provided by diabetes clinic specialists according to the standards of care of the Diabetes Shared Care System. Participants with type 2 diabetes were randomly assigned to two arms: the UC arm or intervention arm, which involves attending a structured group education program using CM™ over a 12-week period. Eligible patients were referred to diabetes education, where the participants were randomized according to sequence of visit (first participant, assigned to the CM group; second participant, assigned to the UC group and subsequently). Those who were randomized to the CM™ program were invited by our diabetes educators or physicians to participate in the education program. The allocation of the participants to the intervention or UC group is shown in Figure1.
Figure 1.
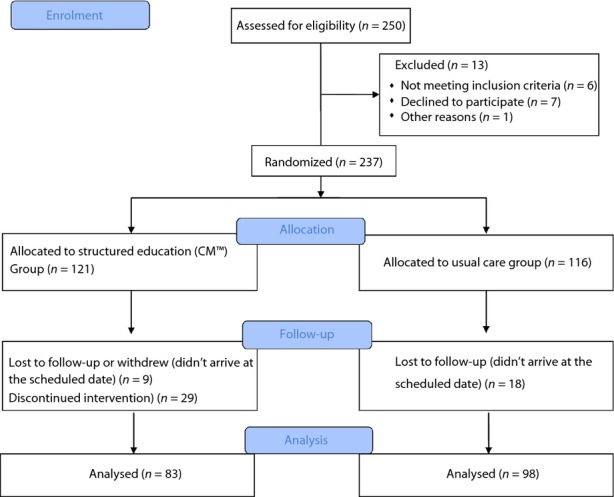
Flow diagram and allocation of participants to study groups. CM™, Diabetes Conversation Map™.
Group Diabetes Education Program Using CM™
The program was delivered in four 1–2-h sessions every week, facilitated by one certified diabetes educator in each group. The CM™ program consists of illustrated maps measuring 3 × 5 feet that are used as a resource to engage small groups of three to 10 patients with an interactive verbal and visual learning experience. Participants were allowed to share personal knowledge and experiences. In addition, competence and self-determination should be promoted, and the consequences of behaviors should be identified and discussed. The themes delivered were: (i) Starting Insulin Treatment; (ii) Understanding the Many Factors of Managing Diabetes; (iii) How Diabetes Works; (iv) Living With Diabetes; and (v) Healthy Eating and Being Active. The topics ‘Understanding the Many Factors of Managing Diabetes’ and ‘How Diabetes Works’ were given in one session.
UC Group
Participants in the UC group did not receive group education. They were all treated under the Diabetes Shared Care System, which provides standardized diabetes care. The care provided includes medical history assessment, physical examination, laboratory evaluation, management plan evaluation, as well as diabetes self-management education (such as instruction on nutrition, diet, exercise, medication, complication prevention and self-monitoring of blood glucose). UC was managed by a diabetes team including diabetologists or GPs, and certified diabetes educators (nurses and dietitians). Diabetes patient education is usually provided on an individual as-needed basis, using a preprinted case report book containing predefined scheduled visits, assessment items and treatment targets. Participants were scheduled for individual sessions every clinic visit, and the time spent on education was dependent on individual need. Occasionally, traditional group education was also provided.
Data Collection and Outcome Measurement
The primary end-point was the change in HbA1c levels from baseline to 12 months. Secondary end-points included the following: changes in fasting plasma glucose; percentage of HbA1c <7% achieved; and self-care behavior assessment.
All data regarding general medical history and diabetes history were collected by the participants’ physicians. Data for all patients entering the study were collected at baseline, the third, sixth, ninth and 12th month. Biomedical data were collected at clinic visits.
All recruited participants were required to complete a questionnaire investigating behavior attitudes. We used the initial patient self-assessment and follow-up patient self-assessment to assess self-care behavior achievements. The Perceived Diabetes Self-management Scale was used to assess behavior attitudes, lifestyle questions and illness perception. Answers were given on a five-point Likert scale, ranging from ‘strongly disagree’ to ‘strongly agree’, from ‘all of the time’ to ‘none of the time’, or from ‘extremely worried’ to ‘ not worried at all’. Questionnaire data were collected from participants at the beginning of the study and at the third month.
Statistical Analysis
Power analysis using the effect size was calculated by a difference of 0.5% in HbA1c levels. The study was designed to have a 95% power to detect this difference. This was determined using a two-sample t-test (two-sided, α = 0.05), assuming a common standard deviation of 1.5%. In the present study, 195 patients were required to achieve the specified statistical power. Allowing for a 20% dropout rate, 215 participants were therefore required in the present study.
All statistical analyses were carried out with SPSS software, version 14.0 (SPSS, Chicago, IL, USA). Primary outcome was analyzed on an intention-to-treat (ITT) basis including all randomized patients. The data analysis set included participants who were enrolled at the beginning of the study. Dropouts and missing data as a result of failure to comply with the measurement protocol were replaced with the immediately preceding values. Primary outcome was also analyzed in the per protocol (PP) population, consisting of all randomized patients who completed the study and attended at least two sessions of group education. Demographic data and efficacy variables at baseline and follow-up visits were summarized for all patients using contingency tables for qualitative variables (such as sex, education and treatment group). The comparisons of changes from baseline to follow-up visits between the two groups were repeated by χ2-test or Student's t-test. All changes between the groups were evaluated by analysis of paired t-test. All tests of intervention effects were carried out at a two-sided significance level of 0.05 unless otherwise stated.
Results
Of the 250 screened patients, 237 were eligible and were randomized to the UC group (n = 116) or CM™ (n = 121) group (Figure1). Table1 lists the baseline characteristics of all participants. The mean age was 58.99 ± 13.51 years, and mean duration of diabetes was 10.14 ± 6.94 years; 46% of the patients were women, and the percentage of patients with an education level of junior school education or higher was 46%. Overall mean HbA1c was 9.53 ± 2.05% at baseline. There were no significant differences in demographic characteristics between the two groups. The demographic characteristics between PP and ITT were not different, except for a slightly higher proportion of HbA1c >9% in the CM™ per-protocol group. The most common reason given by patients for not attending the group education was lack of time or the patient's diabetes knowledge has already improved. The attendance rate of at least two sessions of CM™ group education was 68.7%. The mean number of participants who actually attended the CM™ group sessions was eight (range 6–13).
Table 1.
Baseline characteristics
| All (n = 245) | CM™ group (ITT) (n = 121) | UC group (ITT) (n = 116) | CM™ group (PP) (n = 83) | UC group (PP) (n = 98) | |
|---|---|---|---|---|---|
| Age (years) | 58.99 ± 13.5 | 58.99 ± 11.59 | 58.98 ± 15.32 | 58.55 ± 11.58 | 59.45 ± 13.69 |
| Sex (female) | 113 (46) | 57 (46.7) | 56 (45.5) | 38 (45.7) | 46 (46.9) |
| Education level (high school and above) | 113 (46) | 62 (50.8) | 51 (41.4) | 40 (48.2) | 30 (30.6) |
| Duration of diabetes (years) | 10.14 ± 6.94 | 10.28 ± 8.43 | 9.43 ± 6.34 | 11.66 ± 7.718 | 8.70 ± 6.94 |
| Body mass index (kg/m2) | 26.68 ± 5.15 | 26.71 ± 4.49 | 26.65 ± 5.51 | 26.89 ± 5.37 | 26.95 ± 5.48 |
| FPG (mg/dL) | 198.52 ± 81.94 | 196.86 ± 78.50 | 196.87 ± 88.86 | 197.71 ± 83.80 | 200.16 ± 85.36 |
| HbA1c (%) | 9.529 ± 2.05 | 9.45 ± 1.92 | 9.70 ± 2.25 | 9.57 ± 1.96 | 9.77 ± 2.06 |
| HbA1c >9% | 132 (53.8) | 64 (52.4) | 68 (55.2) | 50 (60.1) | 53 (54.1) |
| Insulin use | 134 (54.7) | 71 (58.2) | 63 (51.2) | 65 (78.3) | 23 (76.5) |
Data are expressed as mean ± standard deviation, number and percentage in parentheses.
CM, structured education with conversation map; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; ITT, intention-to-treat; PP, per-protocol usual care; UC, routine usual care education.
Changes in HbA1c
There were significant improvements in glycemic outcomes from baseline to 3, 6 and 12 months in the CM™ group, as compared with the UC group. In the ITT population as well as in PP population, both groups showed reductions in HbA1c level (Figure2). However, over the course of the 12-month period, the CM™ group participants in the PP population had greater reductions in HbA1c than the UC group participants in the PP population. The difference between treatment groups showed a significant absolute reduction of HbA1c in the CM™ group at 3 and 6 months (Δ = −0.59% and Δ = −1.13%, P < 0.01), but the difference was no longer statistically significant at 9 and 12 months (Δ = −0.43% and Δ = −0.49%), based on an intent-to-treat analysis. However, the per-protocol analysis showed a significant change persisted at 12 months (Δ = −0.67%). The percentage of participants who achieved HbA1c below 7 and 6.5% is shown in Figure3 (42% vs 19%, CM™ and UC group, respectively, P < 0.01). For those who attended only one session (n = 39), the HbA1c reduction was 0.93 ± 0.29, compared with those who attended more than two sessions, 1.90 ± 0.22. The percentage of patients who had a change of treatment was similar in both groups (54% vs 45%, CM™ and UC group, respectively). The OAD change for SU was 71.4–50% and 73.1–49.1% for the CM and UC groups, respectively; for metformin it was 76.2–73.8%, and 63.6–68.5% for the CM and UC groups, respectively. For insulin treatment, premix insulin use was 11.2% greater in the UC group, compared with the CM group. The most common changes were adjustments of insulin doses. The change in insulin dose in the CM™ group was from 0.26 to 0.32 unit/kg/day, and in the UC group from 0.24 to 0.35 unit/kg/day (not significant between groups).
Figure 2.
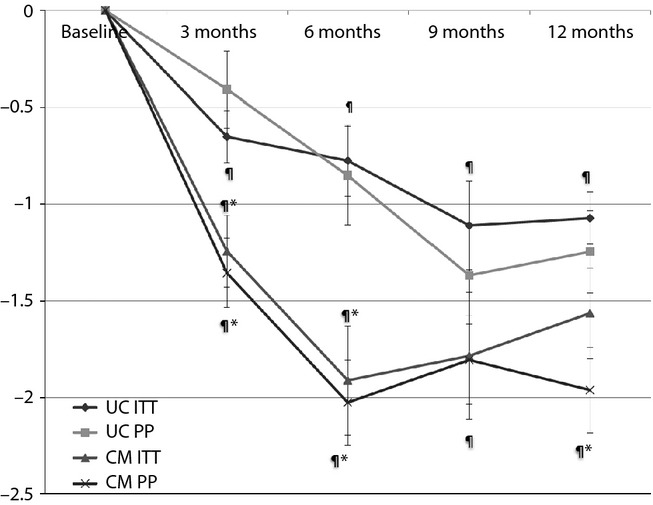
Mean change of glycated hemoglobin (HbA1c) from baseline to 3, 6, 9 and 12 months. Mean differences in change ± standard error of the mean. *P < 0.05, between groups; ¶P < 0.05 within group. CM, structured education with conversation map; ITT, intention-to-treat; PP, per-protocol UC, routine usual care education.
Figure 3.
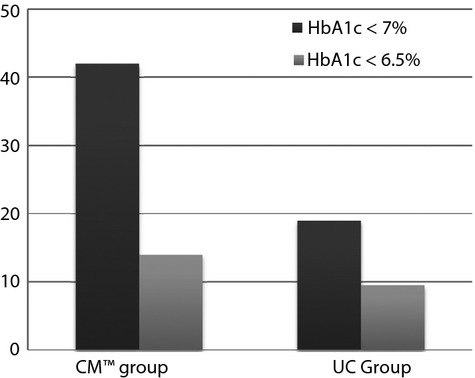
Proportion of patients achieving glycemic response with glycated hemoglobin (HbA1c) ≤7.0 and ≤6.5% at 12 months in the intention-to-treat population. *P < 0.05, between groups; ¶P < 0.05 within group. CM, structured education with conversation map; UC, routine usual care education.
Other Metabolic Parameters and Behavioral Outcomes
As shown in Table2, in the CM™ group, there was a significant change in fasting plasma glucose between the CM™ and UC group. Blood pressure and bodyweight did not show any significant changes between the two groups. Using patient self-assessment to assess self-care behavior achievements, there was a significant improvement in the CM™ group compared with the UC group. There were particular improvements in being active, problem-solving, reducing risk and health coping (Figure4). In the CM™ education group, the results of the Perceived Diabetes Self-Management Scale questionnaire showed that attitude toward diabetes care significantly improved at the third month, with higher scores in items relating to positive attitude and lower scores for items measuring negative attitude, whereas the UC group showed no significant change (Table2).
Table 2.
Changes in biomedical outcomes by follow-up times and treatment differences between participants with poorly controlled type 2 diabetes assigned to a structured group education program or to usual care
| CM™ group (ITT) Mean change (95% CI) | UC group (ITT) Mean change (95% CI) | CM™ group (PP) Mean change (95% CI) | UC group (PP) Mean change (95% CI) | |
|---|---|---|---|---|
| FPG Baseline to 12 months | −43.46¶* (−27.52 to −59.41) | −12.89 (6.86 to −32.66) | − 49.36¶* (−28.04 to −60.68) | −15.48 (5.11 to −36.07) |
| Bodyweight Baseline to 12 months | −0.98 (−2.20 to 0.22)* | −0.14 (−3.87 to 0.61) | −0.98 (−0.22 to 2.20) | −0.62 (−3.42 to 6.17) |
| Systolic blood pressure Baseline to 12 months | −27.49 (1.25 to −53.72) | −23.57 (2.69 to −49.83) | −34.47 (2.86 to −35.81) | −23.38 (6.77 to −39.9) |
| Diastolic blood pressure Baseline to 12 months | −5.03 (2.52 to −7.54) | −2.41 (4.54 to −9.36) | −4.60 (1.34 to −7.86)* | −3.91 (2.28 to −10.11) |
| Positive attitudes Baseline to 12 months | 0.67¶* (0.62 to 0.71) | −0.24 (−0.18 to −0.29) | 0.79¶* (0.75 to 0.84) | −0.43 (−0.37 to −0.48) |
| Negative attitudes Baseline to 12 months | −0.96¶* (−0.90 to −1.01) | 0.09 (0.03 to 0.14) | −1.16¶* (−1.10 to −1.21) | 0.26 (0.21 to 0.31) |
CI, confidence interval; CM, structured education with conversation map; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; ITT, intention-to-treat; PP, per-protocol usual care; PPG, postprandial plasma glucose, UC, routine usual care education.
¶P < 0.0.5 within group; *P < 0.05, between groups.
Figure 4.
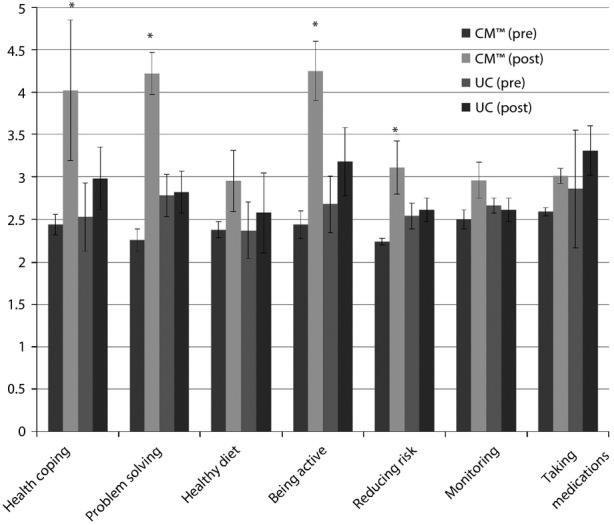
Proportions of patients achieving behavioral changes goals from baseline to 12 months using American Association of Diabetes Educators Self-Care Behaviors™ framework behavioral score survey. *P < 0.05, between groups, ¶P < 0.05 within group. CM, structured education with conversation map; UC, routine usual care education.
Discussion
The present results showed that patients with a diabetes duration of 10 years and suboptimal HbA1c under routine usual care had greater improvements in their HbA1c and self-care behavioral outcomes if they were educated with a structured education model using CM™ compared with outcomes of patients who received usual care. Outcomes that improved significantly included glycemic control, which paralleled secondary psychosocial and behavioral outcomes. The present findings were consistent with those of similar studies investigating the efficacy of structured group education compared with usual care12,13. In studies comparing group and individual education, a similar effect on HbA1c was achieved with both approaches9,14. In the aforementioned trials, there were reductions in HbA1c values of 0.6–1.49% in follow-up periods of 4 months–4 years. In addition to glycemic outcomes, improvements in psychosocial outcomes were also shown. However, there have only been a few studies CA carried out on CM™, despite its availability in many countries. The only study comparing individual and group education using CM™ and usual care was carried out at ABQ Health Partners in New Mexico and Health Partners Medical Group in Minnesota. That study showed that individual education resulted in better glucose control outcomes than group education using CM™. The study population comprised 65% Hispanic patients and HbA1c reductions of 0.27 and 0.5% were achieved in group and individual education, respectively, with baseline HbA1c levels of 8.0%. The completion rate in the patients that attended group education was lower than that of patients that received individual education15. Another study carried out in Carpi, Italy, which did not use comparators, showed improved glycemic control with HbA1c reduction of 0.5% after 3 months’ follow up in 63 participants with a mean baseline HbA1c of 8.0%16. The characteristics of the present study population were similar to those of previous studies that used the CM™. The only difference was the ethnicity of the study population, as all of our participants were East Asians (Taiwanese). The present study showed a slightly greater improvement in glycemic outcome. There are several possible explanations for this finding. First, we incorporated the AADE7 self-care behaviors assessment tool into CM™, which could reinforce the behavioral achievement goals. Second, ethnic and cultural differences might have influenced a number of factors affecting glycemic control. Third, there was a higher attendance rate in the present study, which possibly contributed to better glycemic outcome. A recent study did not show any glycemic efficacy in the group education using CM™ because of its high drop-out rate17, showing a possible correlation between attendance rate and glycemic outcome. Research evidence has shown that individual or group health-related education does not suit everyone, and alternatively structured education programs need to be available to account for the needs of a diverse population18. Traditional approaches to health behavior change delivered by a diabetes educator or physician could undermine a patient's autonomy, thereby generating resistance. However, during the period of instruction with the CM™ model, the researchers noted that the patients showed greater active participation in the instruction sessions than those who received education through the traditional model. The empowerment, discovery learning and support from others provided by the CM™ in our Asian population appeared to have a greater impact than in other populations. A study carried out in Japan showed a reduction in HbA1c of 2.0% in a 3-month intervention with 83 patients19. Furthermore, the educational effects of CM™ depend on the skills of the facilitators, as shown by the Japanese review20. The facilitators in Taiwan were also trained by expert trainers in collaboration with the Taiwan Association of Diabetes Education.
Empowerment cannot be given or taught; it is a process that people must engage in for themselves. The role of healthcare professionals is to enable patients to acquire knowledge and confidence, and to make informed choices about their actions and activities21. No published empirical study has tested the empowerment model in its entirety. Through the use of CM™, the participants in the present study were encouraged to participate actively in the learning process, and to discuss their feelings toward living with their condition and the effect it has on their day-to-day lives. Therefore, the effectiveness of the CM™ Program might be due to the extent to which patients developed the skills, knowledge, and confidence to identify and address their own problems with respect to diabetes self-management. The precise mechanism of action is likely to involve a combination of all these components and possibly other, as yet unidentified factors, such as cultural and psychosocial factors that might also play a role.
It is possible that the intervention was effective solely the result of the 4–8 h of contact time. However, even if the success of the intervention was due, in part, to the length of contact time, it would be a cost-effective and realistic strategy compared with delivering 12 h of structured education to patients on an individual basis13. It has previously been shown that when patients receive the same structured diabetes education delivered over the same time period, on either a one-to-one or group basis, the group intervention was still more effective22. We do not follow a specific treatment protocol at every visit. Changes in medication were decided by the physician. Therefore, treatment changes could also have affected the results.
The present findings suggest that a structured education using the CM™ program can probably be generalized to the majority of people with type 2 diabetes for the following reasons: (i) the present CM™ study was a randomized control trial with minimum exclusion criteria; (ii) only type 2 diabetes patients with the same healthcare access backgrounds were recruited; and (iii) the present study was delivered under normal conditions within primary care. The patient population in the present study was representative of long-term type 2 diabetics with suboptimal glycemic control worldwide. The background of routine care was the same in all patients, as they all had national health insurance coverage, and received standard care for diabetes in accordance with national guidelines. Though the patients received brief one-on-one education visits quarterly, some input was still required to achieve changes in self-care behavior. We believe that with additional input using the CM™ approach discussed herein, patients will be able to achieve adequate glycemic control.
In conclusion, the application of the CM™ education program in conjunction with the AADE7 behavioral tool was more effective in lowering HbA1c than was usual care at 3 and 6 months in all patients and at 12 months in patients who had completed at least two sessions of the CM™ program. Incorporating the CM™ education program into the usual care of patients with suboptimally controlled glucose could improve their glucose control and achieve self-care behavioral goals.
Acknowledgments
This study was supported by a grant from Chung Shan University Hospital (CSH-2013-A-011). Part of this study was presented in an oral presentation at the American Diabetes Association on 24 June 2013, in Chicago, USA.
Disclosure
The authors declare no conflict of interest.
References
- IDF Diabetes Atlas Group. Update of mortality attributable to diabetes for the IDF Diabetes Atlas: estimates for the year 2011. Diabetes Res Cin Pract. 2013;100:277–279. doi: 10.1016/j.diabres.2015.05.037. [DOI] [PubMed] [Google Scholar]
- Jiang YD, Chang CH, Tai TY, et al. Incidence and prevalence rates of diabetes mellitus in Taiwan: analysis of the 2000–2009 Nationwide Health Insurance database. J Formos Med Assoc. 2012;111:599–604. doi: 10.1016/j.jfma.2012.09.014. [DOI] [PubMed] [Google Scholar]
- Yu NC, Su HY, Chiou ST, et al. Trends of ABC control 2006–2011: a National Survey of Diabetes Health Promotion Institutes in Taiwan. Diabetes Res Clin Pract. 2013;99:112–119. doi: 10.1016/j.diabres.2012.11.018. [DOI] [PubMed] [Google Scholar]
- Jiang YD, Shiu RS, Chuang LM, et al. Is the development of a diabetes care system important for quality care? An analysis in Taiwan. J Diabetes Investig. 2011;2:79–81. doi: 10.1111/j.2040-1124.2011.00110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiou ST, Lin HD, Yu NC, et al. An initial assessment of the feasibility and effectiveness of implementing diabetes shared care system in Taiwan–some experiences from I-Lan County. Diabetes Res Clin Pract. 2001;54(Suppl 1):S67–S73. doi: 10.1016/s0168-8227(01)00311-4. [DOI] [PubMed] [Google Scholar]
- Haas L, Maryniuk M, Beck J, et al. National standards for diabetes self-management education and support. Diabetes Care. 2014;37(Suppl 1):S144–S153. doi: 10.2337/dc14-S144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinsbekk A, Rygg LO, Lisulo M, et al. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res. 2012;12:213. doi: 10.1186/1472-6963-12-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- Duke SA, Colagiuri S, Colagiuri R. Individual patient education for people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2009:CD005268. doi: 10.1002/14651858.CD005268.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loveman E, Frampton GK, Clegg AJ. The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review. Health Technol Assess. 2008;12:1–116. doi: 10.3310/hta12090. [DOI] [PubMed] [Google Scholar]
- Boren SA. AADE7TM Self-care Behaviors: systematic reviews. Diabetes Educ. 2007;33:866–871. doi: 10.1177/0145721707309662. [DOI] [PubMed] [Google Scholar]
- Trento M, Passera P, Borgo E, et al. A 5-year randomized controlled study of learning, problem solving ability, and quality of life modifications in people with type 2 diabetes managed by group care. Diabetes Care. 2004;27:670–675. doi: 10.2337/diacare.27.3.670. [DOI] [PubMed] [Google Scholar]
- Khunti K, Skinner TC, Heller S, et al. Biomedical, lifestyle and psychosocial characteristics of people newly diagnosed with Type 2 diabetes: baseline data from the DESMOND randomized controlled trial. Diabet Med. 2008;25:1454–1461. doi: 10.1111/j.1464-5491.2008.02620.x. [DOI] [PubMed] [Google Scholar]
- Deakin TA, Cade JE, Williams R, et al. Structured patient education: the diabetes X-PERT Programme makes a difference. Diabet Med. 2006;23:944–954. doi: 10.1111/j.1464-5491.2006.01906.x. [DOI] [PubMed] [Google Scholar]
- Sperl-Hillen J, Beaton S, Fernandes O, et al. Comparative effectiveness of patient education methods for type 2 diabetes: a randomized controlled trial. Arch Intern Med. 2011;171:2001–2010. doi: 10.1001/archinternmed.2011.507. [DOI] [PubMed] [Google Scholar]
- Ciardullo AV, Daghio MM, Fattori G, et al. Effectiveness of the kit Conversation Map in the therapeutic education of diabetic people attending the Diabetes Unit in Carpi, Italy. Recenti Prog Med. 2010;101:471–474. [PubMed] [Google Scholar]
- Mash RJ, Rhode H, Zwarenstein M, et al. Effectiveness of a group diabetes education programme in under-served communities in South Africa: a pragmatic cluster randomized controlled trial. Diabet Med. 2014;31:987–993. doi: 10.1111/dme.12475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalal HM, Evans PH. Achieving national service framework standards for cardiac rehabilitation and secondary prevention. BMJ. 2003;326:481–484. doi: 10.1136/bmj.326.7387.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouchi Y, Imamine R, Kusama M, et al. Evaluation of the utility of diabetes conversation MapTM in Japanese diabetic patients. J Diabetes Investig. 2012;3(Suppl 1):S240. [Google Scholar]
- Higashiyama H, Harashima S, Kitatani N, et al. The nationwide implementation program of diabetes conversation MapTM by the Japan Association of Diabetes Education and Care: a critical step to revolutionize diabetes education in Japan. J Diabetes Investig. 2012;3(Suppl 1):S64. [Google Scholar]
- Walker R. Diabetes: reflecting on empowerment. Nurs Stand. 1998;12:49–52. doi: 10.7748/ns.12.23.49.s49. [DOI] [PubMed] [Google Scholar]
- Rickheim PL, Weaver TW, Flader JL, et al. Assessment of group versus individual diabetes education: a randomized study. Diabetes Care. 2002;25:269–274. doi: 10.2337/diacare.25.2.269. [DOI] [PubMed] [Google Scholar]


