Abstract
Introduction/Aims
Insufficient insulin secretion or inefficient insulin response are responsible for the clinical outcome of type 2 diabetes mellitus. Administration of insulin alone is prone to cause secondary effects, resulting in an unsatisfactory outcome. Shen-Qi-Formula (SQF), a well-known Chinese medicinal formula, has been used for diabetic treatment for a long time. The present study was designed to investigate whether SQF in combination with insulin improved the clinical outcome of type 2 diabetes mellitus, and what mechanisms were possibly involved in the treatment.
Materials and Methods
A total of 219 patients were included in the study. Of these, 110 patients were treated with insulin monotherapy, and 109 with the combination therapy of SQF and insulin. Before and after 12-week treatment, the fasting blood glucose, postprandial blood glucose, β-cell function, insulin resistance and blood lipids were measured.
Results
The 12 weeks of SQF treatment in combination with insulin significantly decreased the fasting and postprandial blood glucose levels. Insulin secretion was not increased after the treatment, but β-cell function and insulin resistance were obviously improved. Furthermore, 12 weeks of treatment with SQF and insulin improved the levels of glucagon-like peptide-1, oxidative stress, blood lipids, coagulation function and bodyweight.
Conclusion
The results from our study showed that the combination therapy of SQF and insulin significantly improved the clinical outcome of type 2 diabetes mellitus compared with insulin monotherapy. The mechanism of improvement was possibly involved in the multiple pathways.
Keywords: Insulin, Shen-Qi-Formulas, Type 2 diabetes
Introduction
Diabetes mellitus is a metabolic disorder caused by insufficient insulin secretion or inefficient insulin response, which is associated with an increased blood glucose level1. Diabetes mellitus is divided into two main categories: insulin-dependent type 1 and non-insulin-dependent type 2. Approximately 90% of diabetic patients are diagnosed with type 2 diabetes2,3. Type 2 diabetes features insulin insensitivity, in which the tissues and cells do not properly respond to insulin4, and loss of pancreatic β-cell function, resulting in impairment of insulin production and secretion. The β-cell function is dominantly modulated by glucagon-like peptide-1 (GLP-1) and oxidative stress5 in reducing glucagon secretion, attenuating gastric emptying, and decreasing appetite and weight gain6. The action of GLP-1 is impaired in type 2 diabetes7–9. These cause hyperglycemia. Hyperglycemia leads to clinical complications, such as cardiovascular diseases, kidney dysfunction and neuropathy. Furthermore, abnormal lipid metabolism can result in lipid toxicity, which can further worsen diabetic complications10. Therefore, maintenance and enhancement of β-cell function are of importance for the treatment of type 2 diabetes11. However, no antidiabetic drugs are shown to be effective for the prevention of β-cell dysfunction12.
Shen-Qi-Formula (SQF), a well-known Chinese herbal formula, has been used for the treatment of diabetes for a long time in traditional Chinese medicine. SQF consists of ginseng, kudzu vine root (Huang Qi), rehmannia, Chinese yam, dogwood, radix trichosanthis, salvia and cooked rhubarb. Some of those components have been extensively studied, and their antidiabetic mechanisms have been identified. For example, ginseng as one of the main active ingredients in SQF is shown not only to have significant antihyperglycemic effect in both animal models and clinical studies13–15, but also significantly decreases insulin resistance and fasting blood glucose levels in patients with type 2 diabetes16,17. Kudzu vine root (Huang Qi), the other one of the main active ingredients in SQF, has been shown to have a strong antihyperglycemic effect18. Because the complexity of the phytochemicals and bioactivities exists in the herbs, a single antidiabetic herb could contain thousands of phytochemicals, which might have multiple benefits by targeting multiple metabolic pathways. A combination therapy of herbal and synthetic drugs in the treatment of type 2 diabetes and its complications has been documented19. In contrast, a therapy using insulin alone, although blood glucose level is relatively controlled, could bring up different secondary or undesirable effects20. Therefore, the combination of insulin with SQF might be of importance for the improvement of type 2 diabetes.
The present study was designed to examine whether the clinical outcome of type 2 diabetes was improved by the administration of SQF and insulin, and explored what possible mechanisms were involved in the combination therapy. The changes in fasting blood glucose (FBG), postprandial blood glucose (PBG) and glycosylated hemoglobin (HbA1c) as primary outcomes were examined. The alterations of insulin, lipids, GLP-1 (7–36), oxidative stress, coagulation function, blood pressure, body mass index (BMI) and bodyweight as secondary outcome results were examined in order to understand the primary outcome treated by the combination therapy, and explore the multiple pathways linked to diabetes influenced by the therapy.
Materials and Methods
Patients
Patients (aged >18 years, men and women) with type 2 diabetes presented at the Department of Endocrinology, Teaching Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan Province, China, between January 2011 and December 2013 were eligible to participate in the study. The review board of the Chengdu University of Traditional Chinese Medicine approved the study.
For inclusion in the study, all patients had to meet the criteria for type 2 diabetes defined by the World Health Organization21. Patients included in the study were those who were diagnosed as type 2 diabetes, and treated with insulin alone. Exclusion criteria included those who had systemic treatment with glucocorticoids, clinical trials of drugs within 12 weeks, liver and kidney dysfunction, pregnant or lactating women, anemia, and diabetic ketoacidosis. Individuals with those conditions or treatments would interfere with participation or completion of the protocol, which influenced the outcomes of the study. Therefore, patients who had any one of the aforementioned exclusion criteria were excluded from the study. Patient characteristics including age, sex and duration of the disease were recorded (Table1).
Table 1.
Patient characteristics and effects of Shen-Qi-Formula/insulin on the primary and secondary outcomes
| Characteristics | Ins | SQF+Ins |
|---|---|---|
| Patient (n) | 110 | 109 |
| Age (years) | 57.1 | 56.9 |
| Sex, male (%) | 50.3 | 52.8 |
| Duration of diabetes (years) | 10.9 | 10.6 |
| Baseline | At 12 weeks | Baseline | At 12 weeks | |
|---|---|---|---|---|
| Primary outcome | ||||
| FBG (mmol/L) | 8.3 ± 2.9 | 6.9 ± 1.2§ | 8.2 ± 3.0 | 6.0 ± 0.3§* |
| PBG (mmol/L) | 18 ± 4.9 | 11.7 ± 2.3 | 17.7 ± 3.6 | 8.5 ± 1.7§** |
| HbA1c (%) | 11 ± 1.2 | 8.7 ± 1.0 | 10.8 ± 1.1 | 6.5 ± 1.1§* |
| Secondary outcome | ||||
| Insulin (mmol/L) | 11.2 ± 2.4 | 22.1 ± 2.5§ | 11.1 ± 1.9 | 9.6 ± 2.5§** |
| TC (mmol/L) | 5.9 ± 1.0 | 5.6 ± 1.1 | 5.9 ± 1.1 | 5.7 ± 1.1 |
| TG (mmol/L) | 1.8 ± 1.3 | 1.8 ± 1.7 | 1.9 ± 1.3 | 1.1 ± 1.3§* |
| HDLC (mmol/L) | 0.8 ± 0.1 | 0.9 ± 0.1 | 0.8 ± 0.1 | 1.2 ± 0.1§* |
| LDLC (mmol/L) | 3.5 ± 0.3 | 3.3 ± 0.4 | 3.5 ± 0.4 | 2.2 ± 0.3§* |
| NEFA (μmol/L) | 650.1 ± 27.8 | 574.1 ± 28. 9 | 6656.8 ± 26.3 | 242.9 ± 22.2§§* |
| GLP-1 (pg/mL) | 212.3 ± 13.8 | 227.0 ± 12.2 | 2215.9 ± 12.1 | 326.2 ± 13.6§* |
| T-SOD (U/mL) | 58.8 ± 2.6 | 61.5 ± 2.8 | 559.6 ± 2.3 | 73.4 ± 2.3§* |
| MDA (nmol/L) | 15.3 ± 7.2 | 15.2 ± 7.4 | 115.5 ± 7.2 | 10.6 ± 6.6§** |
| PT (s) | 12.6 ± 0.8 | 12.7 ± 0.8 | 112.7 ± 0.8 | 13.8 ± 0.7§* |
| APTT (s) | 34.2 ± 2.7 | 34.6 ± 3.4 | 333.7 ± 3.3 | 37.0 ± 2.8§* |
| Fib (g/L) | 3.1 ± 0.5 | 3.1 ± 0.5 | 33.2 ± 0.5 | 2.8 ± 0.5§* |
| BMI (kg/m2) | 32.5 ± 2.7 | 31.7 ± 2.8 | 332.4 ± 2.8 | 30.6 ± 2.4§* |
| BW (kg) | 91.2 ± 6.2 | 92.1 ± 5.8 | 991.6 ± 5.3 | 88.3 ± 6.6§* |
| Systolic BP (mmHg) | 144.8 ± 11 | 130.1 ± 9.2 | 1144.3 ± 9.2 | 124.6 ± 4.2§* |
| Diastolic BP (mmHg) | 89.3 ± 14.2 | 88.6 ± 10.3 | 90.6 ± 12.5 | 82.1 ± 9.8§* |
APTT, activated partial thromboplastin time; BP, blood pressure; BW, bodyweight; FBG, fasting blood glucose; FIB, fibrinogen concentration; HbA1c, glycosylated hemoglobin; GLP-1, glucagon-like peptide-1; HDLC, high-density lipoprotein cholesterol ester; Ins, insulin; LDLC, low-density lipoprotein cholesterol ester; NEFA, non-esterified fatty acids; PBG, post-prandial blood glucose; PT, prothrombin time; SQF, Shen-Qi-Formula; TC, total cholesterol; TG, triglyceride. *P < 0.05, compared with the insulin alone (Ins) group; **P < 0.01, compared with the Ins group; §P < 0.05, compared within the group; §§P < 0.01, comparing within the group.
Randomization and Patient Allocation
The participants and investigators were blind to group assignment. The included patients were sequentially numbered. A computer-generated randomization list was used for treatment allocation. Randomization was carried out by a spss 21.0 version of software (SPSS, Chicago, IL, USA). The participants were randomly categorized as the insulin-alone group and SQF + insulin group (SQF+Ins).
SQF and Preparation
SQF is comprised of eight herbs with different dosages (Table2). All herbs were purchased from Tianjin Central Pharmaceutical Group Corporation Ltd, a pharmaceutical manufacturer in Tianjin, China, in a joint venture with well-known pharmaceutical enterprises, such as Glax Smith line America and Baxter America. All purchased herbs were identified by Professor Chun-Guang Xie from the Chengdu Traditional Chinese Medicinal University.
Table 2.
Components and dosage of Shen-Qi-Formula
| Components | Dosage (g) |
|---|---|
| Ginseng | 5 |
| Kudzuvine root (Huang Qi) | 30 |
| Rehmannia | 15 |
| Chinese yam | 15 |
| Dogwood | 15 |
| Radix trichosanthis | 10 |
| Salvia | 15 |
| Cooked rhubarb | 6 |
SQF was extracted by an automatic extraction machine (Shaanxi Aipu Medical Equipment Co., Ltd., Xi'an, China). Briefly, SQF was extracted twice by refluxing with boiling water (1:10 and 1:5, respectively) for 90 min, and a concentration at 29.8 g of SQF extract was obtained at a volume of 300 mL of solution. The SQF extract was then packed in a container with a volume of 100 mL.
Treatment Regimen
Participants were randomly allocated to receive either SQF plus insulin (SQF+Ins) or insulin alone (Ins). In the SQF+Ins group, 100 mL of the SQF extract was orally administered three times daily, plus insulin injection (Novo Nordisk, Beijing, China) at a dose of 3 mL (300 IU) twice daily before breakfast and dinner. In group Ins, the same dose of insulin was injected and no SQF was given.
A registered dietitian developed a plan including foods lowered in sodium and fat for those individuals. Fasting blood glucose level was tested by biweekly measurement. Insulin started at a dose of 3 mL (300 IU) twice daily, the dose was adjusted according to the tested glucose levels. Blood glucose was targeted at 5–7 mmol/L of the fasting glucose level or <7–9 mmol/L of postprandial glucose level.
A period of 12 weeks was spent to complete the study. During the period, all participants were required to not alter their regimen. This was monitored by biweekly phone call or monthly visit. A follow-up visit was carried out at 12 weeks at completion of the study.
Measurement of the Primary Outcomes
Before the start and after completion of the study, FBG, PBG and HbA1c as primary outcome measurements were tested. The administration of insulin was stopped before dinner on the day before an oral glucose tolerance test (OGTT) was carried out, and the OGTT was carried out after a 12-h overnight fast. After baseline venous blood samples were collected as fasting blood glucose, patients were required to have standard food containing100 g of carbohydrate. The postprandial glucose levels were tested 120 min after food intake.
Measurement of the Secondary Outcomes
Insulin, lipids, GLP-1 (7–36), oxidative stress, coagulation function, blood pressure, BMI and bodyweight as the secondary outcomes were tested before the start and after completion of the study.
Measurement of β-Cell Function, Insulin Resistance and Insulin Sensitivity
β-Cell function, insulin resistance and insulin sensitivity were studied by homeostatic model assessment (HOMA)22. HOMA%S is a measure of insulin sensitivity, HOMA%B is a measure of β-cell function and HOMA-IR is a measure of insulin resistance. Together, the three measures can show credible results with proper interpretation. HOMA has been shown not only to correlate closely with the euglycemic clamp method, but also to be a simple and economic measure.
Statistical Analysis
Statistical analyses were carried out using spss version 17 (SPSS). Statistical differences between groups were evaluated by one-way of analysis of variance (anova). Student's t-test was used to examine the differences between groups. A P-value <0.05 showed a significant difference.
Results
A total of 219 patients (51.5% men, range 38–74 years) were included in the study, after exclusion of 21 patients with heart, brain and psychiatric disorders; four patients on medication with glucocorticoids; six patients with liver and kidney dysfunction; and one patient with a history of diabetic ketoacidosis in the past 3 months. A total of 110 of those patients were treated with Ins and 109 with SQF+Ins (Figure1). There was no significant difference between the groups regarding their ages, sex and duration of the disease (Table1).
Figure 1.
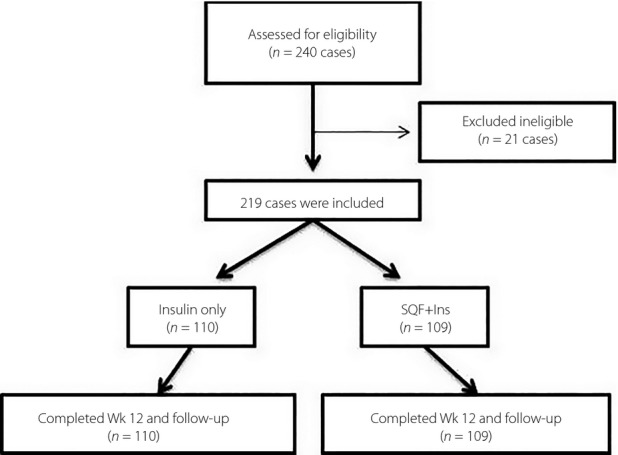
Participant flow from recruitment to completion of the study. SQF+Ins, Shen-Qi-Formula and insulin.
Effects of SQF+Ins on the Primary Outcomes
The baseline of fasting blood glucose was not different between the two groups before the start of the study. After 12-week treatment with SQF+Ins, the fasting blood glucose (P < 0.05) and postprandial blood glucose levels (P < 0.01) were significantly decreased, compared with the levels in the Ins group (P < 0.01). Similarly, the administration of SQF+Ins significantly decreased the level of HbA1c (P < 0.05), compared with that in the group treated by Ins (P < 0.05; Table1).
Effects of SQF+Ins on the Secondary Outcomes
After 12 weeks, the secondary outcomes were changed greatly in the group treated with the combination therapy of SQF+Ins (Table1).
The insulin level decreased from 11.6 mmol/L of the baseline level to 9.6 mmol/L (P < 0.05) in the SQF+Ins group, but it was increased from 11.2 mmol/L of the baseline to 22.1 mmol/L (P < 0.05) in the Ins group. The increased insulin level suggested an inappropriate utility of insulin, as the postprandial blood glucose level was not as decreased as that in the SQF+Ins group.
The cholesterol levels were not changed. The triglyceride levels were significantly decreased (P < 0.05). The decrease in triglyceride level was probably as a result of the improvement of glucose metabolism after the combination therapy. Low-density lipoprotein cholesterol ester was decreased in the SQF+Ins group (P < 0.05), the decrease was not seen in the Ins group. High-density lipoprotein cholesterol ester was increased in the two groups, but a significant increase was seen in the SQF+Ins group (P < 0.05). Similarly, the level of non-esterified fatty acids was markedly reduced after 12 weeks of the combination therapy (P < 0.001).
There was no significant difference between the two groups regarding the blood GLP-1 (7–36) levels before the start of the study. However, a significant increase was observed in the SQF+Ins group (P < 0.05). Although the GLP-1 (7–36) level was also increased in the Ins group, the increase was lower than that in the SQF+Ins group (P < 0.05), suggesting that the combination of SQF and insulin obviously stimulated GLP-1 (7–36) amide secretion.
Compared with insulin monotherapy, the combination therapy significantly increased the total superoxide dismutase (T-SOD) level (P < 0.05), but greatly decreased the melondialdehyde (MDA) level (P < 0.001). Treatment with insulin alone did not change the MDA level.
The administration of SQF in combination with insulin significantly improved the coagulation factors including prothrombin time (P < 0.05), activated partial thromboplastin time (P < 0.05) and fibrinogen (P < 0.05) activity.
In patients treated with SQF+Ins, mean bodyweight decreased from 91.6 to 88.3 kg (P < 0.05), whereas in the Ins group, bodyweight increased from 91.2 to 92.1 kg.
BMI significantly decreased after the SQF+Ins treatment (P < 0.05). In the Ins group, although BMI was decreased, the change was not statistically different.
The administration of SQF+Ins significantly lowered blood pressure (P < 0.05). Although Ins treatment also decreased blood pressure, no statistical difference was seen.
Effect of SQF+Ins on Insulin Resistance, Insulin Sensitivity and β-Cell Function
There was no significant difference between the two groups before start of the study. After 12 weeks of SQF+Ins treatment, the levels of HOMA%B and HOMA%S were significantly increased (P < 0.05). In the group using insulin monotherapy, the levels of HOMA%B were not changed. The 12 weeks of combination therapy decreased the level of HOMA%IR (P < 0.01). These results suggested that the combination therapy of SQF+Ins improved the insulin resistance and insulin sensitivity. Insulin sensitivity was decreased in the Ins group (P < 0.05; Table3).
Table 3.
Effects of Shen-Qi-Formula and insulin on insulin resistance, insulin sensitivity and β-cell function
| Variable | Ins | SQF+Ins | ||
|---|---|---|---|---|
| Baseline | After 12 weeks | Baseline | After 12 weeks | |
| HOMA%B | 76.8 ± 22.1 | 74.4 ± 27.5 | 71.3 ± 26.8 | 82.4 ± 28.2§* |
| HOMA-IR | 3.4 ± 0.2 | 4.3 ± 0.3§ | 3.4 ± 0.5 | 2.0 ± 0.31§** |
| HOMA%S | 78.2 ± 32.1 | 62.6 ± 30.2§ | 76.3 ± 20.1 | 81.2 ± 19.3§* |
HOMA%B, homeostatic model assessment of β-cell function; HOMA%S, homeostatic model assessment of insulin sensitivity; HOMA-IR: homeostatic model assessment of insulin resistance; Ins, insulin; SQF, Shen-Qi-Formula. §P < 0.05, compared within the group; *P < 0.05, compared with the insulin alone (Ins) group; **P < 0.01, compared with the Ins group.
Effect of SQF+Ins on the Consumed Amount of Insulin
During 12 weeks of the study, the daily insulin dose consumed was monitored. Administration of SQF+Ins reduced the amount of insulin consumed from an initial 600 IU/day to a final 596 IU/day. Because of better control of blood glucose in the SQF+Ins group, 10% of patients stopped using insulin injection, and used SQF only, before termination of the study. Administration of insulin alone increased the amount of insulin consumed from an initial 600 IU/day to a final 602 IU/day.
Safety and Adverse Effects of SQF+Ins
The volume of hemoglobin, and liver and kidney functions were tested in all patients before the start and throughout the study to monitor for any possible adverse reactions. SQF+Ins was well tolerated with no adverse event. There were no abnormalities in liver or kidney functions in the two groups. In the Ins group, one case developed mild fatigue, and was found to be transient hypoglycemia. The other case in the SQF+Ins group had loose bowel motions associated with fatigue due to influenza. These two patients had symptoms in the early stage of taking medicine. The symptoms were resolved in a few days (Table4).
Table 4.
Safety and adverse effects of Shen-Qi-Formula and insulin treatment
| Variable | Ins | SQF+Ins | ||
|---|---|---|---|---|
| Baseline | After 12 weeks | Baseline | After 12 weeks | |
| Laboratory data | ||||
| HGB (g/L) | 134.5 ± 14.2 | 132.1 ± 10 | 135.4 ± 11.3 | 134.2 ± 11.2 |
| ALT (IU/L) | 32.8 ± 20.2 | 29.5 ± 13.7 | 35.6 ± 21.3 | 32.4 ± 19.6 |
| AST (IU/L) | 28.6 ± 20.4 | 26.46 ± 17.1 | 29.1 ± 21.3 | 26.4 ± 1 |
| CCr (mL/min) | 86.2 ± 17.2 | 99.7 ± 13.8 | 89.4 ± 21.4 | 101.7 ± 18.7 |
| BUN (mg/dL) | 16.2 ± 2.6 | 18. 3 ± 3.2 | 17.1 ± 3.4 | 16.9 ± 2.7 |
| Clinical data | ||||
| Loose bowels | 0 | 0 | 0 | 1 |
| Fatigue | 0 | 1 | 0 | 1 |
ALT, alanine transaminase; AST, aspartate transaminase; BUN, blood urea nitrogen; CCr, creatinine clearance rate; HGB, hemoglobin; Ins, insulin; SQF, Shen-Qi-Formula.
Discussion
The present study, using Chinese antidiabetic herbal medicine in combination with insulin, showed a significant improvement on the glycemic outcome. Although insulin secretion was not significantly increased after the combination therapy, some interesting findings were observed: (i) insulin resistance (HOMA-IR), insulin sensitivity (HOMA%S) and β-cell function (HOMA%B) were greatly improved; (ii) the amount of insulin consumed decreased; and (iii) the secondary outcome results including blood lipids, T-SOD, MDA, GLP-1 secretion, coagulation function, blood pressure and bodyweight were greatly improved. These results suggested that SQF enhanced the antihyperglycemic effect of insulin possibly through multiple pathways. To our knowledge, this is the first study reporting the mechanisms of SQF and insulin treatment of type 2 diabetes in human patients.
Glycemic control in the treatment of type 2 diabetes involves insulin production, insulin secretion and insulin utilization. All currently available antidiabetic agents lack efficacy, and have undesirable adverse effects10,23. Furthermore, drugs including insulin are not only unable to prevent or rescue β-cell dysfunction, but also result in side-effects24,25. Drugs targeting one or two metabolic pathways are reported to be insufficient to treat type 2 diabetes. Drugs with the ability to target more metabolic pathways are more encouraging than those targeting a single pathway, but these drugs targeting multiple pathways are often associated with adverse effects26. Therefore, a combination of herbal medicine with other antidiabetic medicine is applied to increase insulin production, sensitization of the insulin receptor and other pathways11. Because of the complexity of the phytochemicals and bioactivities in plants, medicinal herbs have been shown to contain diverse bioactive compounds, and have multiple effects on insulin production, insulin section and insulin utilization10. A single antidiabetic herb with thousands of phytochemicals could have multiple benefits by targeting several metabolic pathways; therefore, a combination therapy of orthodox medicine and herbal medicine has shown a better effect than either medicine alone19.
In the present study, the administration of SQF in combination with insulin greatly lowered the postprandial plasma glucose level; whereas in insulin monotherapy, the postprandial plasma glucose level was still at a higher level, although insulin controlled the plasma glucose level. Postprandial hyperglycemia is a result of the body being unable to control blood glucose adequately after a loading of “sugar,” which was thought to be toxic to the β-cells and result in dysfunction of β-cells27. The tissues and cells do not respond to insulin properly, with features of insulin insensitivity4. The so-called “insulin resistance” is a decrease in responsiveness of the target tissues to normal levels of circulating insulin. Therefore, higher insulin resistance might have a higher blood insulin level, and a smaller amount of insulin response is seen in those with better insulin sensitivity. In the present study, postprandial glucose level was greatly improved in patients treated with SQF+Ins, but insulin secretion was not increased. Cut-off values for normal HOMA-IR were reported to be from 2.5 to 4.128–30. The baseline levels in the present study were 3.38 in the insulin monotherapy group and 3.39 in the combination therapy group. These levels from our study should be considered to be in the non-clinical range. However, the 12-week combination therapy of SQF+Ins significantly decreased the HOMA-IR level from 3.39 to 2.02; whereas in the insulin monotherapy group, the HOMA-IR level increased from 3.38 to 4.28. These results suggested that the combination therapy of SQF+Ins decreased insulin resistance, and increased insulin sensitivity.
Theoretically, while insulin sensitivity is improved, β-cell function (HOMA%B) is also improved. A HOMA%B value near to 100% is associated with better β-cell function31. However, in the SQF+Ins group, the level of insulin secretion did not increase, even though β-cell function (HOMA%B) and insulin sensitivity appeared to improve. Thus, a high HOMA%B might not always mean better β-cell functioning, perhaps the opposite. This was consistent with the recent study by Grant et al.31 Although it is unclear why insulin secretion decreases when insulin sensitivity increases, a possible explanation is that β-cells do not have to produce more insulin when insulin sensitivity is improved28. Decreased β-cell function as represented by HOMA%B does not seem to predict the development of diabetes31, and low insulin secretion might be adequate for an insulin-sensitive patient32.
HbA1c is a form of hemoglobin primarily used to identify blood glucose concentration. Many factors including blood lipids33, blood pressure34,35 and diabetes complications36 can affect HbA1c level. HbA1c was tested as an indicator of how blood glucose level was controlled, and monitored the influence of the combination therapy on those factors. The present findings showed that the combination therapy of SQF+Ins decreased the HbA1c level, and was associated with improvements of blood pressure, bodyweight, BMI and blood lipids.
The improvement of blood lipids could be a result of the improvement of insulin resistance by the administration of SQF+Ins, because insulin resistance is usually associated with dyslipidemia37. Targeting insulin resistance was shown to be an effective treatment of dyslipidemia38. Oxidative stress is greatly associated with the progress of type 2 diabetes and complications of the disease39,40. The T-SOD activity and MDA level are correlated with the glycemic variability and oxidative stress41. A significant increase in SOD and reduction in MDA in the combination therapy of SQF+Ins suggested that the combination therapy enhanced the ability of anti-oxidative stress, and reduced the responsiveness to oxidative stress. Hypertension and increased BMI are common in type 2 diabetes42,43, a better control of blood pressure and the reduced BMI are effective to control diabetes44. The combination therapy of SQF+Ins greatly improved the disturbance of glucose metabolism, associated with improvement of blood pressure, BMI, blood lipids and hypercoagulable state. Weight loss occurred in the combination therapy group, but did not develop in the Ins group, as insulin alone was associated with insulin insensitivity and bodyweight increase24,25. The weight loss observed in the combination therapy group might be linked with the increase in GLP-1 level and the improvement of β-cell function regulated by GLP-15.
The major effects of GLP-1 are stimulating insulin secretion, enhancing sensitivity of the tissue to insulin and enhancing β-cell proliferation, which is associated with a decrease in blood glucose and glucose toxicity45,46, GLP-1 also suppresses food intake and appetite, and helps reduce bodyweight in patients who are overweight or obese47. The present study showed that there were correlations between the glucose-lowering effect of the combination therapy and an increase in GLP-1 level. The increase in GLP-1 level was associated with the decrease in the postprandial glucose level. The combination of SQF+Ins increased GLP-1 secretion, which is associated with an improved β-cell function and enhanced insulin sensitivity.
The euglycemic clamp might provide an accurate result in assessment of insulin sensitivity, but it is costly, and not feasible in a large population; therefore, using HOMA in the study was cost-effective, with validity for clinical trials. In addition, a longer study period could provide more information regarding oxidative stress, but a significant increase in SOD and reduction in MDA were observed with SQF+Ins treatment.
In summary, the present results showed that SQF enhanced the antihyperglycemic outcome when combined with insulin. The actions and therapeutic potential of the SQF compounds were through the regulation of multiple metabolic pathways in the treatment of type 2 diabetes. Furthermore, SQF+Ins was safe and without side-effects, and provided a significant potential with polypharmacy in the clinical treatment of type 2 diabetes.
Disclosure
The authors declare no conflict of interest.
References
- Kempf K, Rathmann W, Herder C. Impaired glucose regulation and type 2 diabetes in children and adolescents. Diabetes Metab Res Rev. 2008;24:427–437. doi: 10.1002/dmrr.869. [DOI] [PubMed] [Google Scholar]
- Boyle JP, Engelgau MM, Thompson TJ, et al. Estimating prevalence of type 1 and type 2 diabetes in a population of African Americans with diabetes mellitus. Am J Epidemiol. 1999;149:55–63. doi: 10.1093/oxfordjournals.aje.a009728. [DOI] [PubMed] [Google Scholar]
- Attele AS, Zhou YP, Xie JT, et al. Antidiabetic effects of Panax ginseng berry extract and the identification of an effective component. Diabetes. 2002;6:1851–1858. doi: 10.2337/diabetes.51.6.1851. [DOI] [PubMed] [Google Scholar]
- Hui H, Tang G, Go VLW. Hypoglycemic herbs and their action mechanisms. Chin Med. 2009;4:11. doi: 10.1186/1749-8546-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang T, Han H, Yang Z. Iron, oxidative stress and gestational diabetes. Nutrients. 2014;6:3968–3980. doi: 10.3390/nu6093968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlebowicz J, Hlebowicz A, Lindstedt S, et al. Effects of 1 and 3 g cinnamon on gastric emptying, satiety, and postprandial blood glucose, insulin, glucose-dependent insulinotropic polypeptide, glucagon-like peptide 1, and ghrelin concentrations in healthy subjects. Am J Clin Nutr. 2009;3:815–821. doi: 10.3945/ajcn.2008.26807. [DOI] [PubMed] [Google Scholar]
- Nauck M, Stockmann F, Ebert R, et al. Reduced incretin effect in Type 2 (non-insulin-dependent) diabetes. Diabetologia. 1986;1:46–52. doi: 10.1007/BF02427280. [DOI] [PubMed] [Google Scholar]
- N'aslund E, Backman L, Holst JJ, et al. Importance of small bowel peptides for the improved glucose metabolism 20 years after jejunoileal bypass for obesity. Obes Surg. 1998;3:253–260. doi: 10.1381/096089298765554449. [DOI] [PubMed] [Google Scholar]
- Muscelli E, Mari A, Casolaro A, et al. Separate impact of obesity and glucose tolerance on the incretin effect in normal subjects and type 2 diabetic patients. Diabetes. 2008;5:1340–1348. doi: 10.2337/db07-1315. [DOI] [PubMed] [Google Scholar]
- Chang LT, Lin Y, Bartolome AP, et al. Herbal therapies for type 2 diabetes mellitus: chemistry, biology, and potential application of selected plants and compounds cicero. Evid Based Complement Alternat Med. 2013;2013:33. doi: 10.1155/2013/378657. . Article ID 378657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahy JL, Hirsch IB, Peterson KA, et al. Targeting β-cell function early in the course of therapy for type 2 diabetes mellitus. J Clin Endocrinol Metab. 2010;9:4206–4216. doi: 10.1210/jc.2010-0668. [DOI] [PubMed] [Google Scholar]
- Yu YL, Lu SS, Yu S, et al. Huang-Lian-Jie-Du-Decoction modulates glucagon-like peptide-1 secretion in diabetic rats. J Ethnopharmacol. 2009;124:444–449. doi: 10.1016/j.jep.2009.05.027. [DOI] [PubMed] [Google Scholar]
- Vuksan V, Sievenpiper JL, Xu Z, et al. Konjac-mannan and American ginseng: emerging alternative therapies for type 2 diabetes mellitus. J Am Coll Nutr. 2001;5:370S–380S. doi: 10.1080/07315724.2001.10719170. [DOI] [PubMed] [Google Scholar]
- Sotaniemi EA, Haapakoski E, Rautio A. Ginseng therapy in non-insulin-dependent diabetic patients. Diabetes Care. 1995;10:1373–1375. doi: 10.2337/diacare.18.10.1373. [DOI] [PubMed] [Google Scholar]
- Vuksan V, Sievenpiper JL, Koo VYY, et al. American ginseng (Panax quinquefolius L) reduces postprandial glycemia in nondiabetic subjects and subjects with type 2 diabetes mellitus. Arch Intern Med. 2000;7:1009–1013. doi: 10.1001/archinte.160.7.1009. [DOI] [PubMed] [Google Scholar]
- Ma SW, Benzie IFF, Chu TTW, et al. Effect of Panax ginseng supplementation on biomarkers of glucose tolerance, antioxidant status and oxidative stress in type 2 diabetic subjects: results of a placebo-controlled human intervention trial. Diabetes Obes Metab. 2008;11:1125–1127. doi: 10.1111/j.1463-1326.2008.00858.x. [DOI] [PubMed] [Google Scholar]
- Vuksan V, Sung MK, Sievenpiper JL, et al. Korean red ginseng (Panax ginseng) improves glucose and insulin regulation in well-controlled, type 2 diabetes: results of a randomized, double-blind, placebo-controlled study of efficacy and safety. Nutr Metab Cardiovasc Dis. 2008;1:46–56. doi: 10.1016/j.numecd.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Xie W, Zhao Y, Zhang Y. Traditional Chinese medicines in treatment of patients with type 2 diabetes mellitus. Evid Based Complement Alternat Med. 2011;2011:13. doi: 10.1155/2011/726723. . Article ID 726723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur R, Afzal M, Kazmi I, et al. Polypharmacy (herbal and synthetic drug combination): a novel approach in the treatment of type-2 diabetes and its complications in rats. J Nat Med. 2012;3:662–671. doi: 10.1007/s11418-012-0720-5. [DOI] [PubMed] [Google Scholar]
- Leiter LA, Lewanczuk RZ. Of the renin-angiotensin system and reactive oxygen species type 2 diabetes and angiotensin inhibition. Am J Hypertens. 2005;18:121–128. doi: 10.1016/j.amjhyper.2004.07.001. [DOI] [PubMed] [Google Scholar]
- World Health Organization: Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia. (Accessed October 15, 2014, at http://www.who.int/diabetes/publications/Definition%20and%20diagnosis%20of%20diabetes_new.pdf )
- Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21:2191–2192. doi: 10.2337/diacare.21.12.2191. [DOI] [PubMed] [Google Scholar]
- Krentz AJ, Bailey CJ. Oral antidiabetic agents: current role in type 2 diabetes mellitus. Drugs. 2005;3:385–411. doi: 10.2165/00003495-200565030-00005. [DOI] [PubMed] [Google Scholar]
- Modi P. Diabetes beyond insulin: review of new drugs for treatment of diabetes mellitus. Curr Drug Discov Technol. 2007;4:39–47. doi: 10.2174/157016307781115476. [DOI] [PubMed] [Google Scholar]
- Neustadt J, Pieczenik SR. Medication-induced mitochondrial damage and disease. Mol Nutr Food Res. 2008;52:780–788. doi: 10.1002/mnfr.200700075. [DOI] [PubMed] [Google Scholar]
- Zhang BB, Moller DE. New approaches in the treatment of type 2 diabetes. Curr Opin Chem Biol. 2000;4:461–467. doi: 10.1016/s1367-5931(00)00103-4. [DOI] [PubMed] [Google Scholar]
- Robertson RP, Harmon J, Tran PO, et al. Glucose toxicity in β-cells: type 2 diabetes, good radicals gone Bad, and the glutathione connection. Diabetes. 2003;52:581–587. doi: 10.2337/diabetes.52.3.581. [DOI] [PubMed] [Google Scholar]
- Wallace TMLJC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- Ramachandran B, Kandaswamy M, Narayanan V, et al. Insulin mimetic effects of macrocyclic binuclear oxovanadium complexes on streptozotocin-induced experimental diabetes in rats. Diabetes Obes Metab. 2003;5:455–461. doi: 10.1046/j.1463-1326.2003.00302.x. [DOI] [PubMed] [Google Scholar]
- Snehalatha C, Mary S, Selvam S, et al. Changes in insulin secretion and insulin sensitivity in relation to the glycemic outcomes in subjects with impaired glucose tolerance in the Indian diabetes prevention programme-1 (IDPP-1) Diabetes Care. 2009;32:1796–1801. doi: 10.2337/dc09-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant SJ, Chang DHT, Liu J, et al. Chinese herbal medicine for impaired glucose tolerance: a randomized placebo controlled trial. BMC Complement Altern Med. 2013;13:104. doi: 10.1186/1472-6882-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haffner SM, Kennedy E, Gonzalez C, et al. A prospective analysis of the HOMA model. The Mexico city diabetes study. Diabetes Care. 1996;19:1138–1141. doi: 10.2337/diacare.19.10.1138. [DOI] [PubMed] [Google Scholar]
- Khan HA, Sobki SH, Khan SA. Association between glycaemic control and serum lipids profile in type 2 diabetic patients: HbA1c predicts dyslipidaemia. Clin Exp Med. 2007;7:24–29. doi: 10.1007/s10238-007-0121-3. [DOI] [PubMed] [Google Scholar]
- Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–419. doi: 10.1136/bmj.321.7258.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilgin R, Donma O, Sagliker Y. Glucose, glycated hemoglobin and fructosamine levels in essential hypertension. Biochem Mol Biol Int. 1993;31:1129–1133. [PubMed] [Google Scholar]
- Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Festa AMD, Hanley AJGP, Tracy RPP, et al. Inflammation in the prediabetic state is related to increased insulin resistance rather than decreased insulin secretion. Circulation. 2003;108:1822–1830. doi: 10.1161/01.CIR.0000091339.70120.53. [DOI] [PubMed] [Google Scholar]
- Pavo I, Jermendy G, Varkonyi TT, et al. Effect of pioglitazone compared with metformin on glycemic control and indicators of insulin sensitivity in recently diagnosed patients with type 2 diabetes. J Clin Endocrinol Metab. 2003;88:1637–1645. doi: 10.1210/jc.2002-021786. [DOI] [PubMed] [Google Scholar]
- Signorini AM, Fondelli C, Renzoni E, et al. Antioxidant effects of gliclazide, glibenclamide and metformin in Patients with type 2 diabetes mellitus. J Curr Ther Res. 2002;63:411. [Google Scholar]
- Ceriello A, Motz E. Is oxidative stress the pathogenic mechanism underlying insulin resistance, diabetes, and cardiovascular disease? The common soil hypothesis revisited. Arterioscler Thromb Vasc Biol. 2004;24:816–823. doi: 10.1161/01.ATV.0000122852.22604.78. [DOI] [PubMed] [Google Scholar]
- Garg MK, Dutta MK, Mahalle N. Study of beta-cell function (by HOMA model) in metabolic syndrome. Indian J Endocrinol Metab. 2011;15(Suppl1):S44–S49. doi: 10.4103/2230-8210.83059. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creager MA, Lüscher TF, Beckman JA. Diabetes and vascular disease pathophysiology, clinical consequences, and medical therapy: part I. Circulation. 2003;108:1527–1532. doi: 10.1161/01.CIR.0000091257.27563.32. [DOI] [PubMed] [Google Scholar]
- Yardley JE, MacMillan F, Hay J, et al. The blood pressure response to exercise in youth with impaired glucose tolerance and type 2 diabetes. Pediatr Exerc Sci. 2014;10:120–127. doi: 10.1123/pes.2014-0062. [DOI] [PubMed] [Google Scholar]
- Kumagai S, Kai Y, Hanada H, et al. Relationships of the systolic blood pressure response during exercise with insulin resistance, obesity, and endurance fitness in men with type 2 diabetes mellitus. Metabolism. 2002;51:1247–1252. doi: 10.1053/meta.2002.35180. [DOI] [PubMed] [Google Scholar]
- McIntosh CHS, Pederson RA. Degradation of glucose-dependent Insulinotropicpoly peptide and truncated glucagon-like peptide 1 in vitro and in vitro by dipeptidylpeptidase IV. Endocrinology. 1995;136:3585–3596. doi: 10.1210/endo.136.8.7628397. [DOI] [PubMed] [Google Scholar]
- Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696–1705. doi: 10.1016/S0140-6736(06)69705-5. [DOI] [PubMed] [Google Scholar]
- Vilsbøll T, Christensen M, Junker AE, et al. Effects of glucagon-like peptide-1 receptor agonists on weight loss: systematic review and meta-analyses of randomised controlled trials. BMJ. 2012;344:d7771. doi: 10.1136/bmj.d7771. [DOI] [PMC free article] [PubMed] [Google Scholar]


