Abstract
Research about the influence of stigma on health outcomes in sickle cell disease is limited. We administered the recently developed Measure of Sickle Cell Stigma to 262 patients in the United States. The Measure of Sickle Cell Stigma yielded very good internal consistency and four interpretable factors. Significant associations among stigma, pain-related healthcare utilization, and perceived disease severity were observed for three of the four stigma factors (F range = 2.78–5.44). The Measure of Sickle Cell Stigma appears to be a useful tool for measuring disease-specific stigma among adults living with sickle cell disease, and further assessment of its clinical utility is warranted.
Keywords: disease severity, sickle cell, stigma, utilization
Introduction
Sickle cell disease (SCD) is a hemoglobinopathy that affects nearly 100,000 individuals in the United States (Hassell, 2010). Individuals living with SCD experience a broad range of symptoms, but the hallmark characteristic is severe, unpredictable, and episodic pain (Ballas, 1999). In the late 1970s, life expectancy estimates rarely exceeded early adulthood for SCD patients; however, advances in medical treatment have significantly reduced mortality and lengthened the life span (Kanter and Kruse-Jarres, 2013). As a result, more individuals are living with SCD beyond the fourth and fifth decades, and a growing number of researchers have begun to highlight psychological and social factors that influence adjustment and well-being among adults (Caird et al., 2011; Mann-Jiles and Morris, 2009).
Stigma is increasingly cited as a central concept in chronic illness research (Goffman, 1963; Link and Phelan, 2001; Weiss et al., 2006), and we maintain that it may also be an important consideration for adults coping with SCD. As a social process that typically results in the devaluation and discrediting of an attribute, stigma leaves an individual who possesses that attribute feeling vulnerable to negative evaluations from others (Goffman, 1963). It is well established that the process of being stigmatized has health-related consequences (Link and Phelan, 2006; Paschal et al., 2005; Sankar et al., 2006), and a voluminous literature suggests that stigma might contribute to the burden of an illness, cause delays in appropriate help seeking, and result in premature termination of treatment for health problems (Link and Phelan, 2006; Martinez et al., 2012; Weiss et al., 2006; Weiss and Ramakrishna, 2001).
It is possible that some of the physical complications associated with SCD can be a source of stigmatization and have noteworthy implications for health-related outcomes. For example, leg ulcers and jaundiced eyes are two prominently visible symptoms of SCD that may engender anxiety and shame, inhibit social activities, and negatively affect interpersonal interactions (Delaney et al., 2013; Midence and Elander, 1996). Priapism (a persistent, painful, and anomalous erection of the penis) is a complication that affects approximately 10–15 percent of men with SCD (Addis et al., 2007; Bennett and Mulhall, 2008; Bivalacqua et al., 2012). Although priapism can be successfully managed with early presentation and therapeutic intervention, embarrassment and awkwardness on the part of both patients and medical staff can impede the seeking of effective treatment. Finally, individuals living with SCD may also have comorbid complications that affect the bones, joints, or lungs. Thus, the use of assistive devices such as a walker, cane, or oxygen tank may also be a considerable source of stigma because such visual cues might amplify an individual's anticipation of being negatively evaluated by others (Bediako, 2009).
Psychosocial aspects of SCD may also constitute sources of stigma. For example, social perceptions about SCD are often filtered through a racial lens because the condition is thought to primarily affect Blacks or individuals of African descent (Tapper, 1999; Wailoo, 2001). Others have argued that a potential way in which SCD becomes stigmatized is through negative social connotations about race that are implicitly subsumed in public discourse about SCD (Bediako and Moffitt, 2011). A small sampling of other research literature yields an array of topics, ranging from reproductive decision-making (Asgharian et al., 2003; Gallo et al., 2010; Smith and Aguirre, 2012) to disclosure of disease status to others (Thomas and Taylor, 2002) that suggest socially mediated processes through which labels, expectations, and stereotypes about SCD might influence the psychological and behavioral responses of people living with the condition.
In sum, stigma's possible impact on SCD outcomes is important to the degree that feelings of shame and guilt reduce psychological well-being, inhibit social engagement, and create difficulties in social roles and interpersonal relationships (Barbarin and Christian, 1999; Ohaeri et al., 1995; Reese and Smith, 1997; Robinson, 1999). It is likely, then, that individuals living with SCD disease who perceive stigma about their condition are at increased risk for negative self-evaluations, loss of self-esteem, anxiety, and social withdrawal—all of which can have a deleterious impact on health behavior and health status (Berger et al., 2005; Goffman, 1963). Very little is known, however, about these possible associations because there is a dearth of studies that have explicitly assessed the influence of stigma on SCD-related health outcomes. Efforts to study associations between stigma and SCD outcomes have been hindered by the fact that there are no widely used, validated instruments that measure SCD-specific stigma. This inhibits what is known about actual perceptions of stigma among patients and constrains the ability of investigators to make causal connections between stigma and the high rates of psychological symptoms (namely, depression and anxiety) that have been reported in individuals living with SCD (Alao and Cooley, 2001; Asnani et al., 2010; Grant et al., 2000).
To our knowledge, only one group of researchers has published findings on the association between stigma and health-related outcomes in SCD (Jenerette et al., 2012). In a study assessing the preliminary reliability and validity of the Sickle Cell Disease Health-Related Stigma Scale among 77 adults with SCD in the United States, Jenerette et al. (2012) found significant associations between their measure of stigma and both depressive symptoms and hospitalizations for SCD pain crises. Specifically, patients who reported greater stigma had higher scores on the Beck Depression Inventory–Fast Screen, and patients with more than three SCD pain crises that resulted in hospitalizations during the past year reported greater stigma compared to those with fewer than three crises (Jenerette et al., 2012).
Our contribution toward addressing this gap in knowledge seeks to extend the findings of Jenerette et al. (2012) in two important ways. First, we note that the Sickle Cell Disease Health-Related Stigma Scale appears to focus on external stigma—an individual's awareness of devaluing attitudes that might come from the general public, healthcare providers, or family members. Our conceptualization of stigma asserts that it also includes an intrapersonal component that is expressed as internalized attitudes about one's own self-worth and capabilities—a position that reflects recent reports in the stigma literature (Drapalski et al., 2013; Taft et al., 2013; Vogel et al., 2013). Second, Jenerette and colleagues’ stigma measure emphasizes perceived or experienced stigma, where respondents reflect mostly on stigmatizing events after they have occurred. Our conceptualization of stigma acknowledges the role of anticipated stigma—that is, the expectation that one will be negatively stereotyped or discriminated against in future encounters because of his or her SCD status. Recent reports also support this view (Earnshaw et al., 2012, 2013). These added dimensions permit us to analyze stigma as a multidimensional construct (Alvidrez et al., 2010; Bresnahan and Zhuang, 2011; Sayles et al., 2008) and make our work consistent with the classic conceptualization of stigma as “the co-occurrence” of labeling, stereotyping, separation, status loss, and discrimination (Link and Phelan, 2001).
Our program of research seeks a more comprehensive understanding of SCD stigma by concurrently assessing external, internal, experienced, and anticipated domains. We recently developed the Measure of Sickle Cell Stigma (MoSCS) as an instrument that takes into account multiple contexts of disease-related stigma. Below, we briefly describe the development of the MoSCS and report our evaluation of the relations among stigma, perceived disease severity, and healthcare utilization in a sample of 262 SCD patients in the United States enrolled in a prospective cohort study.
Development of the MoSCS
The MoSCS was developed in two phases: (a) an initial phase in which the first author led a focus group of SCD patients in order to generate scale items and (b) a preliminary evaluation phase in which the developmental scale was administered to a convenience sample of adult patients.
Item generation and scale development
The initial version of the MoSCS was based on 40 items from a scale used to assess HIV stigma (Berger et al., 2001). Although there are distinct differences between the illness experiences of individuals living with HIV and those living with SCD, we felt that several of the items were also relevant to the experience of SCD. To confirm their conceptual relevance, we presented the 40 items to a focus group of nine African American adults living with SCD in Cincinnati. The group comprised four men and five women who were recruited from a community-based advocacy group for adults with SCD, and their average age was 34 years. The first author (S.M.B.), a social scientist with expertise in qualitative research, led participants in a discussion about various definitions of “stigma” and asked them to rate on a scale from 0 (not at all relevant) to 4 (very relevant) the extent to which each of the 40 items were relevant to the experiences of people living with SCD. Nine items received very low ratings (at least seven of the nine participants gave a “0” rating); thus, 31 items were retained. These 31 items were then presented to another group of 10 African American adults (six men and four women; average age = 32.2 years) who attended an out-patient SCD clinic in Cincinnati. These individuals were approached in the clinic waiting room during their regularly scheduled appointments and asked to provide feedback on the face validity of the scale. Specifically, they were asked to indicate whether the items appeared to be useful in measuring what they thought most adult SCD patients experience or think about in their daily interactions with others. Eight of the 10 participants indicated that the scale was “extremely useful” in identifying common experiences of adults with SCD, and two responded that it was “very useful.” None of the participants identified specific items that were “not very useful” or “unrelated to the experience of SCD,” nor did they generate new items when asked to think of things that the current list might have missed. The 31 items were used to construct the initial MoSCS.
Preliminary evaluation of the MoSCS
We then administered the 31-item version of the MoSCS to a convenience sample of adults who sought care for SCD at a clinic associated with an academic hospital center in Cincinnati. The 19 participants who participated in the scale development phase described above were excluded from the preliminary evaluation phase. Eligible participants were aged over 18 years, diagnosed with one of the major types of SCD hemoglobinopathy (e.g. hemoglobin SS, SC, or sickle beta thalassemia + (plus) or 0 (zero)) and enrolled in a larger study that sought to learn more about psychological and social aspects of SCD pain. Informed consent was obtained according to a protocol approved by the University of Cincinnati institutional review board. All questionnaires were self-administered in the waiting area or in a private consultation room of the clinic, and participants were given a US$10 gift card to a local grocery chain for completing the scale
A total of 86 adult patients were approached about the study, and 71 elected to participate. Complete data were collected from 70 respondents (36 women and 34 men) between the ages of 18 and 64 years (mean age = 35.3 years; standard deviation (SD) = 12.5 years). In terms of disease status, 67 percent of participants were diagnosed with homozygous sickle cell anemia (hemoglobin SS), 28% with hemoglobin SC disease, and 5% with sickle beta thalassemia. All participants were African American. In all, 49 percent of participants reported “high school” as the highest education level completed, 17 percent reported “community college,” and 26 percent reported that they had completed a 4-year college degree. With regard to employment status, 55 percent of participants were either unemployed or disabled, 18 percent were full-time students, 16 percent were employed full time, and 6 percent were employed part time. Four participants were retired; 68 percent of participants had never married, while 8 percent were married and 20 percent were divorced or separated.
The MoSCS items were presented to participants in a traditional paper-and-pencil format. Participants were instructed to respond to a series of statements that were based on the experiences of some people with SCD. Sample items are “I feel that I’m not as good as others because I have sickle cell disease”; “As a rule, telling others I have sickle cell has been a mistake”; and “I worry about being discriminated against because I have sickle cell.” Responses ranged from 1 (completely false) to 6 (completely true). Scores were summed and averaged across the total number of items to yield a global score of SCD stigma, where higher scores indicated greater levels of stigma.
A principal component analysis (PCA) was conducted on the 31 stigma items with orthogonal varimax rotation using SPSS 22.0 statistical software. The Kaiser–Meyer–Olkin (KMO) measure confirmed the sampling adequacy for the analysis, with the KMO index = .79, which is “good” by conventional standards (Field, 2009; Kaiser, 1974). Bartlett's test of sphericity, χ2 (465) = 1839.81, p < .001, indicated that correlations between items were sufficient to conduct the PCA. Seven factors had eigenvalues greater than 1; these components explained 75.86 percent of the variance. However, items were retained in the final version of the scale only if they loaded uniquely on one factor with at least one other item. Eleven items met these criteria with factor loadings after rotation ranging between .53 and .85. These 11 items loaded onto four factors that appeared to measure Social Exclusion (i.e. the extent to which individuals experience social/interpersonal rejection because of their SCD status; 3 items), Internalized Stigma (i.e. negative personal feelings or guilt about having SCD; 3 items), Disclosure Concerns (i.e. apprehension in disclosing one's SCD status to others; 3 items), and Expected Discrimination (i.e. anticipated discrimination because of one's SCD status; 2 items). Cronbach's alpha for the four factors ranged from .74 to .89. For the entire 11-item scale, Cronbach's alpha was .87, indicating very good internal consistency.
Given the iterative process that was employed to develop the MoSCS, the face validity of the scale items with approximately 90 adults living with SCD, and the reasonable psychometric properties obtained through factor analysis, we felt that it was appropriate to conduct further assessment of the 11-item instrument with a larger sample. If stigma is indeed a pertinent multidimensional construct for SCD patients, as previous findings suggest, then our findings should (a) replicate in a larger sample and (b) demonstrate a significant association between disease-specific stigma and clinically relevant outcomes. We report the main findings from this assessment below.
Methods
Adolescents and adults who received healthcare from two comprehensive SCD centers in the Baltimore/Washington metropolitan area completed the MoSCS as part of the baseline assessment for Improving Patient Outcomes through Respect and Trust (IMPORT), a longitudinal, observational study of SCD patient experiences with healthcare funded by the National Institutes of Health. Participants were eligible for the IMPORT study if they were aged over 15 years, diagnosed with one of the major types of sickle cell hemoglobinopathy, and able to speak English. Informed consent was obtained according to protocols approved by the institutional review boards at the two participating medical institutions. Participants were paid US$50 for completing an audio computer-assisted survey instrument that included the measures described below.
SCD stigma
The 11-item MoSCS was used to assess SCD-specific stigma. As noted above, higher scores indicated greater levels of stigma.
Acute care service utilization
Participants responded to a single item that asked them to indicate the number of times they went to the emergency room or infusion clinic for SCD-related pain over the past year. Rather than assess these visits separately, we created a unitary measure of utilization because we were interested in participants’ overall utilization of acute care services. At our particular site, the infusion clinic is an urgent care center specifically designed to treat acute SCD pain. It was implemented in 2008 through a collaborative relationship with emergency department staff and hospital administrators to reduce patient wait times and provide quality care specific to the needs of adults with SCD.
Hospital admissions
Participants responded to a single item that asked them to report how many hospital admissions for SCD-related pain they had over the past year.
Perceived disease severity
Participants responded to a statement that read, “Compared to other people with sickle cell disease, the severity of my disease is —.” Responses ranged on a 5-point scale from 5 (“much worse”) to 1 (“much better”). Higher scores indicated greater perceived disease severity.
Participants
A total of 279 adults were enrolled in the IMPORT study, and complete data on the variables of interest to this particular study were collected from 262 respondents (138 women and 124 men) between the ages of 15 and 70 years (mean age = 34.5 years; SD = 11.97 years). In all, 97 percent of participants were African American. Approximately 23.7 percent of participants were currently enrolled in school, and 18.7 percent were college graduates who had achieved at least a 4-year college degree (of these, about 8% had a graduate or professional degree). With regard to employment status, about one-third of participants were working full time or part time during their participation in the study, and roughly 10 percent were unemployed and looking for work. In all, 43 percent of participants reported that they were disabled and not working.
Results
PCA
We compared the psychometric properties of the MoSCS obtained from our preliminary evaluation of the scale (N = 70) with that obtained from the current study (N = 262). We performed tests identical to those reported above to assess the suitability of the 11 stigma items for factor analysis. The KMO measure confirmed the sampling adequacy for the analysis of the 11-item scale (KMO index = .83). Bartlett's test of sphericity, χ2 (55) = 1239.51, p < .001, indicated that the MoSCS items were sufficient to conduct the factor analysis. We then conducted an unrotated PCA on the 11 stigma items using Stata 9.3 statistical software (StataCorp LP, 2011) to extract the initial factors for analysis. Three factors had eigenvalues greater than 1; in combination, these components explained 67 percent of the variance. However, a fourth factor yielded an eigenvalue that approximated a value of 1.0 (actual value = .945). Inclusion of this factor increased the explained variance to 75 percent, suggesting that it was non-trivial. We then used common factor analysis (principal axis factoring) with oblique promax rotation to estimate the factor structure and loadings of the 11 items. Table 1 compares the PCA of the MoSCS between the developmental sample (n = 70) and the present sample (n = 262). As shown in the table, the 11 items loaded similarly to what we reported for the preliminary evaluation and yielded four identical factors that appeared to measure Social Exclusion (3 items), Internalized Stigma (3 items), Disclosure Concerns (3 items), and Expected Discrimination (2 items). For this sample, Cronbach's alpha for the entire 11-item scale was .86, indicating acceptable internal consistency.
Table 1.
Comparison of factor loadings of MoSCS items.a
| Social Exclusion |
Internalized Stigma |
Disclosure Concerns |
Expected Discrimination |
|||||
|---|---|---|---|---|---|---|---|---|
| A | B | A | B | A | B | A | B | |
| Cronbach's α (subscale) | .89 | .80 | .84 | .78 | .74 | .79 | .76 | .79 |
| People have physically backed away from me because I have SCD | .75 | .68 | ||||||
| As a rule, telling others that I have SCD has been a mistake | .69 | .59 | ||||||
| People seem to be afraid of me because I have SCD | .67 | .75 | ||||||
| I feel guilty because I have SCD | .85 | .77 | ||||||
| Having SCD makes me feel that I am a bad person | .81 | .69 | ||||||
| I feel I am not as good as others because I have SCD | .79 | .63 | ||||||
| In many areas of my life, no one knows that I have SCD | .76 | .74 | ||||||
| I am very careful who I tell that I have SCD | .70 | .80 | ||||||
| Telling someone I have SCD is risky | .53 | .44 | ||||||
| People lose jobs when employers learn they have SCD | .84 | .71 | ||||||
| I worry about people discriminating against me because I have SCD | .79 | .75 | ||||||
MoSCS: Measure of Sickle Cell Stigma; SCD: sickle cell disease.
Column A: developmental study (N = 70); column B: present study (N = 262).
Primary analyses
With respect to the healthcare utilization variables, roughly 15.9 percent of participants indicated that they did not utilize acute care services over the past year, while 32.9 percent reported one to two visits and 27 percent reported three to four visits. About 24.2 percent of participants reported that they had six or more acute care visits over the past year. Approximately 23.5 percent of participants indicated that they had not been admitted to the hospital over the past year, while 37.6 percent reported two or fewer admissions and 25.3 percent reported three to five admissions. Nearly 13.7 percent of participants reported that they had six or more hospital admissions over the past year. In terms of perceived disease severity, we observed that 17.8 percent of participants perceived their disease severity to be either “much worse” or “worse” than others. In contrast, about 31.4 percent perceived their severity to be “about the same,” 29.6 percent perceived their severity to be “better,” and 21.2 percent indicated that they perceived their disease severity to be “much better” compared to others with the condition.
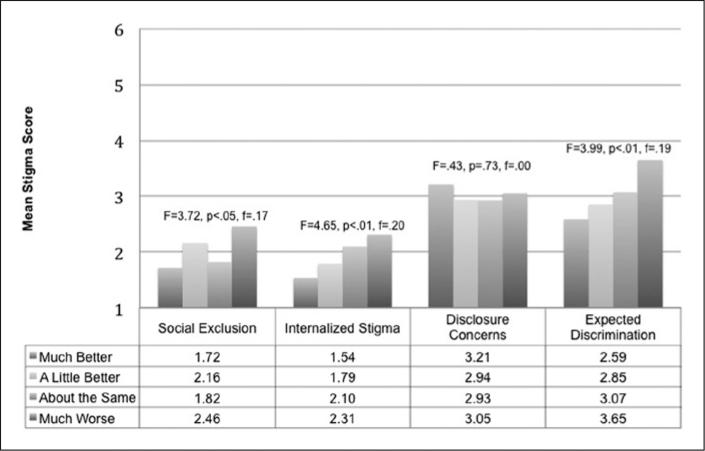
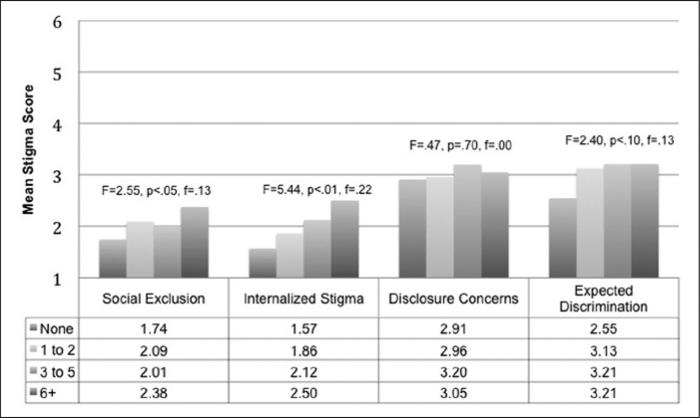
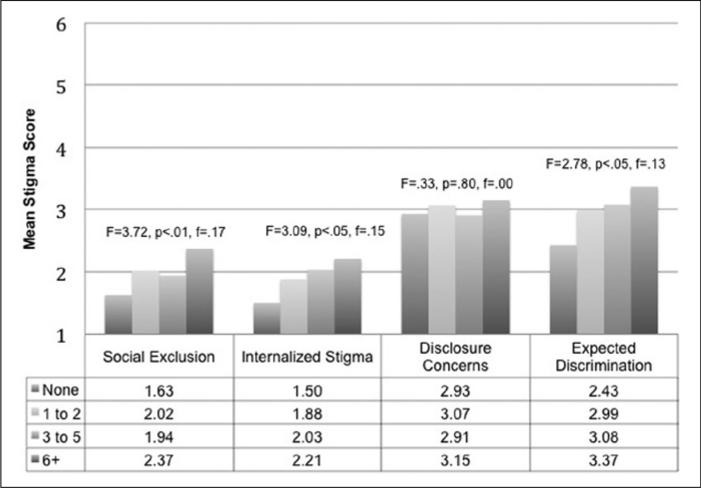
Overall, participants reported low to moderate levels of stigma, with mean values (on a scale ranging from 1 to 6) of 2.02 (SD = 1.14) for Social Exclusion, 1.94 (SD = 1.19) for Internalized Stigma, 3.02 (SD = 1.53) for Disclosure Concerns, and 3.04 (SD = 1.62) for Expected Discrimination. We conducted a series of analyses of variance to determine whether there were differences in MoSCS scores as a function of healthcare utilization and perceived disease severity. These results are summarized in Figures 1 to 3 and show that all of the MoSCS factors except Disclosure Concerns were significantly associated with perceived disease severity (Figure 1) and acute care visits for SCD pain (Figure 2). The significant F values for these analyses ranged from 2.78 to 4.65, with significance levels set at p < .05. Effect sizes were estimated using Cohen's f and are shown in each figure. Estimates ranged from .00 to .22. As shown in Figure 3, only the Social Exclusion (F(3, 258) = 2.55, p = .05, f = .13) and Internalized Stigma (F(3, 258) = 5.44, p = .001, f = .22) factors were significantly associated with hospital admissions for SCD pain. These results suggest that participants who reported higher levels of certain types of SCD stigma had more frequent contacts with the healthcare system and perceived their disease as being worse compared to others.
Figure 1.
Mean stigma scores by perceived disease severity (N = 262).
Figure 3.
Mean stigma scores by hospital admission levels (N = 262).
Figure 2.
Mean stigma scores by acute care service utilization (N = 262).
Discussion
SCD stigma is an important construct that might complicate psychosocial adjustment and interfere with health behaviors and treatment outcomes. This construct, however, is poorly understood and efforts to better understand the associations of stigma with health-related outcomes in SCD have been hampered by the lack of disease-specific instruments to assess the stigma construct. In this study, we used the recently developed MoSCS to explore the impact of stigma on SCD-related outcomes. In doing so, we have reported findings from what is perhaps the first study to concurrently examine multiple domains of stigma in a sample of adults living with SCD.
We found evidence that three of the MoSCS factors (Social Exclusion, Internalized Stigma, and Expected Discrimination) were associated with patient-reported perceptions of disease severity and acute care visits for SCD pain, while two factors (Social Exclusion and Internalized Stigma) were associated with patient-reported hospital admissions for SCD pain. Disclosure Concerns were not significantly associated with any of the outcome variables of interest in this study. Together, these findings provide evidence of the potential clinical relevance of perceived stigma in SCD research and highlight three key issues that we believe are of significant importance for researchers. First, there is a need to examine the temporal association between stigma and clinical outcomes. The design of our study does not allow us to ascertain whether stigma leads to more disease severity or increased healthcare utilization, or whether worse clinical outcomes lead to greater experience of stigma. Future research using a prospective study design (e.g. intensive longitudinal modeling or daily diaries) would permit a better understanding of the direction of the stigma-clinical outcome association. Second, there is a need to explore the experience of stigma in the context of other important psychosocial constructs (Jenerette et al., 2012). For example, depressive symptoms have often been assessed in chronic illness research and attributed to increased pain and decrements in functional limitations, healthcare utilization, and overall quality of life (Alao and Cooley, 2001; Asnani et al., 2010; Belgrave and Molock, 1991; Grant et al., 2000; Levenson et al., 2008; Schaeffer et al., 1999). We speculate that a non-trivial proportion of variance in outcomes like depressive symptoms may be related to perceived stigma. Future research should evaluate this relationship in more detail as it might help to elucidate a potential mechanism through which stigma reduction might improve psychological, social, and physiological outcomes for individuals living with SCD. Third, our results suggest that a useful way to conceptualize SCD stigma is as a multidimensional construct: stigma appears to vary in its etiology (internal vs external and actual vs perceived), and we found that the highest levels of stigma were concerned with anticipated perceptions of being discriminated against rather than internalized guilt or anxiety about one's direct experiences as a SCD patient. This appears to be consistent with recent findings reported by Earnshaw et al. (2012, 2013) suggesting that the anticipation of stigma places stressful demands upon individuals coping with a chronic illness that might exacerbate social isolation, withdrawal, and decreased social support. Future research should rigorously explore the processes of SCD stigmatization.
Finally, we note a few limitations of our study. First, despite observing robust associations between stigma and healthcare utilization that were statistically significant, we obtained small to medium effect sizes (which indicate the degree of difference between groups). It is not clear whether these differences are unique to the clinic from which our sample was drawn or due to other intervening factors. Future research should examine the association between stigma and health-related outcomes across multiple sites and with clinically diverse populations. Second, given that our focus was primarily concerned with assessing the perspectives of individuals living with SCD, an inherent assumption of our work is that stigmatizing experiences originate “inside” the individual. Because we did not assess social attitudes or public perceptions toward people living with SCD, we overestimate the degree to which SCD stigma is personally versus socially mediated. Third, even though the 11-item version of the stigma scale comprises items that clearly load on unique factors, further evaluation of the scale, including its predictive validity, is needed. Finally, because SCD is not exclusive to African Americans, it would be interesting to evaluate differences in SCD stigma among members of different ethnic groups. The degree to which issues concerning race, racism, and racial identity are related to SCD stigma is complex and not well understood (Bediako and Haywood, 2009; Bediako and Moffitt, 2011); thus, a clearer parsing of the relations among race, stigma, and adjustment to SCD might be possible with an ethnically diverse sample.
Despite these limitations, the MoSCS holds promise as a reliable, disease-specific instrument that is simple to administer in clinic or community settings. The scale may be useful for researchers who are interested in examining the global impact of stigma in SCD and those who are interested in assessing SCD stigma as an intervening variable on psychological adjustment. This study yields preliminary evidence for a multidimensional conceptualization of SCD stigma. Future work should aim to provide a more comprehensive understanding of the pathways through which SCD stigma impacts patient outcomes, and, ultimately, to develop interventions that reduce the impact of perceived stigma on the well-being of those affected by SCD.
Acknowledgements
The authors thank all members and participants of the IMPORT study for their time and generous contributions. The full list of IMPORT investigators includes the authors and the following individuals—Johns Hopkins Investigators: Tanita Woodson, Jordan Wilks, Benjamin Ajiboye, Jennifer Haythornthwaite, and Nina Shah. Howard University Investigators: Abiodun Akintilo, Margaret Fadojutimi-Akinsiku, Patricia Oneal, MD, Adriana Medina, Seyed Mehdi Nouraie, John Kwagyan, Kemi Owoyemi, and Ronke Ajala. Study data were collected and managed using REDCap (Research Electronic Data Capture) tools hosted at Johns Hopkins University. REDCap is a secure, web-based application designed to support data capture for research studies, providing (a) an intuitive interface for validated data entry, (b) audit trails for tracking data manipulation and export procedures, (c) automated export procedures for seamless data downloads to common statistical packages, and (d) procedures for importing data from external sources.
Funding
This study was funded by a grant from the National Heart, Lung, and Blood Institute (NHLBI; #1R01HL088511-01A1). Dr Bediako's effort was supported by a Career Development Award from the NHLBI (#1K07HL108742-03). Dr Lanzkron's effort was supported by a Career Development Award from the NHLBI (#1K23HL083089-01). Dr Haywood's effort was funded by a Career Development Award from the NHLBI (#1K01HL108832-01).
References
- Addis G, Spector R, Shaw E, et al. The physical, social and psychological impact of priapism on adult males with sickle cell disorder. Chronic Illness. 2007;3:145–154. doi: 10.1177/1742395307081505. DOI: 10.1177/1742395307081505. [DOI] [PubMed] [Google Scholar]
- Alao AO, Cooley E. Depression and sickle cell disease. Harvard Review of Psychiatry. 2001;9:169–177. doi: 10.1080/10673220127896. DOI: 10.1080/10673220127896. [DOI] [PubMed] [Google Scholar]
- Alvidrez J, Snowden LR, Patel SG. The relationship between stigma and other treatment concerns and subsequent treatment engagement among black mental health clients. Issues in Mental Health Nursing. 2010;31:257–264. doi: 10.3109/01612840903342266. DOI: 10.3109/01612840903342266. [DOI] [PubMed] [Google Scholar]
- Asgharian A, Anie KA, Berger M. Women with sickle cell trait: Reproductive decision-making. Journal of Reproductive and Infant Psychology. 2003;21:23–33. DOI: 10.1080/0264683021000060057. [Google Scholar]
- Asnani MR, Fraser R, Lewis NA, et al. Depression and loneliness in Jamaicans with sickle cell disease. BMC Psychiatry. 2010;10:40. doi: 10.1186/1471-244X-10-40. DOI: 10.1186/1471-244x-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballas SK. Complications of sickle cell anemia in adults: Guidelines for effective management. Cleveland Clinic Journal of Medicine. 1999;66:48–58. doi: 10.3949/ccjm.66.1.48. [DOI] [PubMed] [Google Scholar]
- Barbarin OA, Christian M. The social and cultural context of coping with sickle cell disease: I. A review of biomedical and psychosocial issues. Journal of Black Psychology. 1999;25:277–293. DOI: 10.1177/0095798499025003002. [Google Scholar]
- Bediako SM. Psychosocial aspects of sickle cell disease: A primer for African American psychologists. In: Neville HA, Tynes BM, Utsey SO, editors. Handbook of African American Psychology. SAGE; Thousand Oaks, CA: 2009. pp. 417–427. [Google Scholar]
- Bediako SM, Haywood C., Jr Sickle cell disease in a “postracial” America. Journal of the National Medical Association. 2009;101:1065–1066. doi: 10.1016/s0027-9684(15)31075-0. [DOI] [PubMed] [Google Scholar]
- Bediako SM, Moffitt KR. Race and social attitudes about sickle cell disease. Ethnicity & Health. 2011;16:423–429. doi: 10.1080/13557858.2011.552712. DOI: 10.1080/13557858.2011.552712. [DOI] [PubMed] [Google Scholar]
- Belgrave FZ, Molock SD. The role of depression in hospital admissions and emergency treatment of patients with sickle cell disease. Journal of the National Medical Association. 1991;83:777–781. [PMC free article] [PubMed] [Google Scholar]
- Bennett N, Mulhall J. Sickle cell disease status and outcomes of African-American men presenting with priapism. Journal of Sexual Medicine. 2008;5:1244–1250. doi: 10.1111/j.1743-6109.2008.00770.x. DOI: 10.1111/j.1743-6109.2008.00770.x. [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV Stigma Scale. Research in Nursing and Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Berger M, Wagner TH, Baker LC. Internet use and stigmatized illness. Social Science & Medicine. 2005;40:955–960. doi: 10.1016/j.socscimed.2005.03.025. [DOI] [PubMed] [Google Scholar]
- Bivalacqua TJ, Musicki B, Kutlu O, et al. New insights into the pathophysiology of sickle cell disease-associated priapism. Journal of Sexual Medicine. 2012;9:79–87. doi: 10.1111/j.1743-6109.2011.02288.x. DOI: 10.1111/j.1743-6109.2011.02288.x. [DOI] [PubMed] [Google Scholar]
- Bresnahan M, Zhuang J. Exploration and validation of the dimensions of stigma. Journal of Health Psychology. 2011;16:421–429. doi: 10.1177/1359105310382583. DOI: 10.1177/1359105310382583. [DOI] [PubMed] [Google Scholar]
- Caird H, Camic PM, Thomas V. The lives of adults over 30 living with sickle cell disorder. British Journal of Health Psychology. 2011;16:542–548. doi: 10.1348/135910710X529278. DOI: 10.1348/135910710X529278. [DOI] [PubMed] [Google Scholar]
- Delaney KH, Axelrod KC, Buscetta A, et al. Leg ulcers in sickle cell disease: Current practices and patterns. Hemoglobin. 2013;37:325–332. doi: 10.3109/03630269.2013.789968. DOI: 10.3109/03630269.2013.789968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drapalski AL, Lucksted A, Perrin PB, et al. A model of internalized stigma and its effects on people with mental illness. Psychiatric Services. 2013;64:264–269. doi: 10.1176/appi.ps.001322012. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Quinn DM, Park CL. Anticipated stigma and quality of life among people living with chronic illnesses. Chronic Illness. 2012;8:79–88. doi: 10.1177/1742395311429393. DOI: 10.1177/1742395311429393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Quinn DM, Kalichman SC, et al. Development and psychometric evaluation of the Chronic Illness Anticipated Stigma Scale. Journal of Behavioral Medicine. 2013;36:270–282. doi: 10.1007/s10865-012-9422-4. DOI: 10.1007/s10865-012-9422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A. Discovering Statistics Using SPSS. 3rd edn SAGE; London: 2009. [Google Scholar]
- Gallo AM, Wilkie D, Suarez M, et al. Reproductive decisions in people with sickle cell disease and sickle cell trait. Western Journal of Nursing Research. 2010;32:1073–1090. doi: 10.1177/0193945910371482. DOI: 10.1177/0193945910371482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. Prentice Hall Publishers; New York: 1963. [Google Scholar]
- Grant MM, Gil KM, Floyd MY, et al. Depression and functioning in relation to health care use in sickle cell disease. Annals of Behavioral Medicine. 2000;22:149–157. doi: 10.1007/BF02895779. DOI: 10.1007/bf02895779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassell KL. Population estimates of sickle cell disease in the US. American Journal of Preventive Medicine. 2010;38:S512–S521. doi: 10.1016/j.amepre.2009.12.022. DOI: 10.1016/j.amepre.2009.12.022. [DOI] [PubMed] [Google Scholar]
- Jenerette C, Brewer CA, Crandell J, et al. Preliminary validity and reliability of the Sickle Cell Disease Health-Related Stigma Scale. Issues in Mental Health Nursing. 2012;33:363–369. doi: 10.3109/01612840.2012.656823. DOI: 10.3109/01612840.2012.656823. [DOI] [PubMed] [Google Scholar]
- Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39:31–36. [Google Scholar]
- Kanter J, Kruse-Jarres R. Management of sickle cell disease from childhood through adulthood. Blood Reviews. 2013;27:279–287. doi: 10.1016/j.blre.2013.09.001. DOI: 10.1016/j.blre.2013.09.001. [DOI] [PubMed] [Google Scholar]
- Levenson JL, McClish DK, Dahman BA, et al. Depression and anxiety in adults with sickle cell disease: The PiSCES project. Psychosomatic Medicine. 2008;70:192–196. doi: 10.1097/PSY.0b013e31815ff5c5. DOI: 10.1097/PSY.0b013e31815ff5c5. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual Review of Sociology. 2001;27:363–385. [Google Scholar]
- Link BG, Phelan JC. Stigma and its public health implications. The Lancet. 2006;367:528–529. doi: 10.1016/S0140-6736(06)68184-1. DOI: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- Mann-Jiles V, Morris DL. Quality of life of adult patients with sickle cell disease. Journal of the American Academy of Nurse Practitioners. 2009;21:340–349. doi: 10.1111/j.1745-7599.2009.00416.x. DOI: 10.1111/j.1745-7599.2009.00416.x. [DOI] [PubMed] [Google Scholar]
- Martinez J, Harper G, Carleton RA, et al. The impact of stigma on medication adherence among HIV-positive adolescent and young adult females and the moderating effects of coping and satisfaction with health care. AIDS Patient Care and STDs. 2012;26:108–115. doi: 10.1089/apc.2011.0178. DOI: 10.1089/apc.2011.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midence K, Elander J. Adjustment and coping in adults with sickle cell disease: An assessment of research evidence. British Journal of Health Psychology. 1996;1:95–111. [Google Scholar]
- Ohaeri JU, Shokunbi WA, Akinlade KS, et al. The psychosocial problems of sickle cell disease sufferers and their methods of coping. Social Science & Medicine. 1995;40:955–960. doi: 10.1016/0277-9536(94)00154-l. DOI: 10.1016/0277-9536(94)00154-l. [DOI] [PubMed] [Google Scholar]
- Paschal AM, Ablah E, Wetta-Hall R, et al. Stigma and safe havens: A medical sociological perspective on African-American female epilepsy patients. Epilepsy & Behavior. 2005;7:106–115. doi: 10.1016/j.yebeh.2005.03.020. DOI: 10.1016/j.yebeh.2005.03.020. [DOI] [PubMed] [Google Scholar]
- Reese FL, Smith WR. Psychosocial determinants of health care utilization in sickle cell disease patients. Annals of Behavioral Medicine. 1997;19:171–178. doi: 10.1007/BF02883334. DOI: 10.1007/bf02883334. [DOI] [PubMed] [Google Scholar]
- Robinson MR. There is no shame in pain: Coping and functional ability in adolescents with sickle cell disease. Journal of Black Psychology. 1999;25:336–355. DOI: 10.1177/0095798499025003005. [Google Scholar]
- Sankar P, Cho MK, Wolpe PR, et al. What is in a cause? Exploring the relationship between genetic cause and felt stigma. Genetics in Medicine. 2006;8:33–42. doi: 10.1097/01.gim.0000195894.67756.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayles JN, Hays RD, Sarkisian CA, et al. Development and psychometric assessment of a multidimensional measure of internalized HIV stigma in a sample of HIV-positive adults. AIDS and Behavior. 2008;12:748–758. doi: 10.1007/s10461-008-9375-3. DOI: 10.1007/s10461-008-9375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaeffer JJW, Gil KM, Burchinal M, et al. Depression, disease severity, and sickle cell disease. Journal of Behavioral Medicine. 1999;22:115–126. doi: 10.1023/a:1018755831101. DOI: 10.1023/a:1018755831101. [DOI] [PubMed] [Google Scholar]
- Smith M, Aguirre RTP. Reproductive attitudes and behaviors in people with sickle cell disease or sickle cell trait: A qualitative interpretive meta-synthesis. Social Work in Health Care. 2012;51:757–779. doi: 10.1080/00981389.2012.693580. DOI: 10.1080/00981389.2012.693580. [DOI] [PubMed] [Google Scholar]
- StataCorp LP. Stata Statistical Software (Release 12) StataCorp LP.; College Station, TX: 2011. [Google Scholar]
- Taft TH, Ballou S, Keefer L. A preliminary evaluation of internalized stigma and stigma resistance in inflammatory bowel disease. Journal of Health Psychology. 2013;18:451–460. doi: 10.1177/1359105312446768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapper M. In the Blood: Sickle Cell Anemia and the Politics of Race. The University of Pennsylvania Press; Philadelphia, PA: 1999. [Google Scholar]
- Thomas VJ, Taylor LM. The psychosocial experience of people with sickle cell disease and its impact on quality of life: Qualitative findings from focus groups. British Journal of Health Psychology. 2002;7:345–363. doi: 10.1348/135910702760213724. [DOI] [PubMed] [Google Scholar]
- Vogel DL, Bitman RL, Hammer JH, et al. Is stigma internalized? The longitudinal impact of public stigma on self-stigma. Journal of Counseling Psychology. 2013;60:311–316. doi: 10.1037/a0031889. [DOI] [PubMed] [Google Scholar]
- Wailoo K. Dying in the City of the Blues: Sickle Cell Anemia and the Politics of Race and Health. The University of North Carolina Press; Chapel Hill, NC: 2001. [Google Scholar]
- Weiss MG, Ramakrishna J. Interventions: Research on reducing stigma.. Paper presented at: Stigma and Global Health: Developing a Research Agenda; Bethesda, MD.. September 5-7, 2001.2001. [Google Scholar]
- Weiss MG, Ramakrishna J, Somma D. Health-related stigma: Rethinking concepts and interventions. Psychology, Health & Medicine. 2006;11:277–287. doi: 10.1080/13548500600595053. [DOI] [PubMed] [Google Scholar]