Abstract
Metabolic syndrome is highly prevalent in type 2 diabetics and is a strong risk factor for cardiovascular diseases in such patients. The aim of this study was to determine the prevalence of metabolic syndrome according to the three criteria of ATPIII, IDF and the new criteria for metabolic syndrome diagnosis in Kerman, Iran. This cross-sectional study was performed on 950 diabetic type 2 patients. Data was analyzed by independent t-test, chi-square and logistic regression using the SPSS (revision 20) software. The prevalence of metabolic syndrome in Kerman was 73.4, 64.9, and 70.4%, according to the above criteria. Fasting blood sugar, gender, triglyceride, HDL, waist circumference, and systolic blood pressure were related to the prevalence of metabolic syndrome according to the above-mentioned criteria.The prevalence of metabolic syndrome is high in type 2 diabetic patients and the above-mentioned factors exacerbate the situation.
Keywords: Metabolic syndrome, Type 2, Diabetes, Risk factors
Introduction
The burden of non-communicable disease in the developing countries is increasing and leading to high mortality rates.1 Nowadays, type 2 diabetes (T2DM) is pandemic and there are no signs of reduction in incidence rates.2
Diabetes is one of the most important risk factors for cardiovascular diseases and is the most prevalent cause of mortality in diabetic patients. At least 62% of type 2 diabetics die due to cardiovascular diseases.3
Metabolic syndrome is a common syndrome that results from obesity. The risk of cardiovascular and diabetes type 2 increases in people with metabolic syndrome.4
Metabolic syndrome is highly prevalent in type 2 diabetic patients and is a strong risk factor for cardiovascular diseases in such patients.5
Metabolic syndrome is rising worldwide and attributed to increased obesity and inactive lifestyle.6 It is estimated that 16% of people above 20 years of age globally have metabolic syndrome.7 In Iran, this syndrome is dramatically prevalent and close to 34% of people above 20 years old have metabolic syndrome, according to the adult treatment panel (ATPIII).8 Differences in genetics, diet, physical activity, age and gender in different societies can affect the prevalence of this syndrome.9
There is no globally accepted definition for the diagnosis of this syndrome and most studies use the ATPIII criteria for defining metabolic syndrome. In 2005, the International Diabetes Federation (IDF) has suggested a definition for the diagnosis of people with metabolic syndrome, which is applicable to different ethnic groups.3
In the IDF criteria, central obesity is a prerequisite6 and central obesity assessment by waist circumference for different genders and ethnic groups according to IDF is necessary.10 According to the study done by Gozashti et al., the appropriate cutoff point for the diagnosis of metabolic syndrome in men and women in Kerman has been determined.11
Currently, metabolic syndrome has become an important health problem and there is a need for investigation in this field.12 Considering the fact that diabetic patients with metabolic syndrome also have cardiovascular risk factors, the diagnosis of metabolic syndrome in such patients is very important,3,5 and leads to a better disease control and prevention of cardiovascular complications.13
The present study was performed to determine the prevalence of metabolic syndrome and its related factors in type 2 diabetic patients of Kerman, Iran.
Patients and Methods
The data used in this study was part of the coronary artery disease risk factors (KERCADR) study in Kerman.14 In KERCADR, 5,900 people were recruited from which 950 people were diagnosed with diabetes and entered into our study in 2013. The variables evaluated in this study were age, gender, job, education, BMI, total cholesterol, HDL cholesterol, LDL cholesterol, fasting blood sugar (FBS), systolic blood pressure, diastolic blood pressure, waist circumference, triglycerides, smoking, physical activity, the duration of diabetes, history of cardiovascular diseases, and the ratio of waist circumference to hip circumference. These variables were measured during the first phase of the Kerman cohort study. Data was analyzed by chi-square, t-test, and logistic regression using SPSS (revision 20) software. The prevalence of metabolic syndrome in people with diabetes was determined according to the below criteria.
The ATPIII criteria that include three or more of the following items:
Central obesity: waist circumference more than 102 centimeters in men and more than 88 cm in women
Triglycerides ≥150 mg/dl or using drugs for hyper triglyceridemia
Cholesterol HDL <40 mg/dl in men and less than 50 mgr/dl in women or under treatment for low HDL cholesterol
Hypertension systolic blood pressure more than 130 mmHg or diastolic blood pressure ≥85 mmHg or being under treatment for hypertension
FBS ≥100 mg/dl or being under treatment for diabetes or a diagnosis of type 2 diabetes.
According to the IDF 2005 criteria, central obesity (waist circumference ≥94 cm in men and 80 cm in women) and two or more of these criteria should be present:
Triglyceride ≥150 mg/dl or under treatment for hyper triglyceridemia
Cholesterol HDL <40 mg/dl in men and less than 50 mgr/dl in women or under treatment for low HDL cholesterol levels
Hypertension systolic blood pressure more than 130 mmHg or diastolic blood pressure ≥85 mmHg or being under treatment for hypertension
FBS ≥100 mg/dl or being under treatment for diabetes or a diagnosis of type 2 diabetes.
The new criteria in Kerman according to Gozashti et al. study is the presence of central obesity (waist circumference ≥86cm in men and 83 cm in women) plus two or more of these criteria:
Triglyceride ≥150 mg/dl or under treatment for hyper triglyceridemia
Cholesterol HDL <40 mg/dl in men and less than 50 mgr/dl in women or under treatment for low HDL cholesterol levels
Hypertension systolic blood pressure more than 130 mmHg or diastolic blood pressure ≥85 mmHg or being under treatment for hypertension
FBS ≥100 mg/dl or being under treatment for diabetes or a diagnosis of type 2 diabetes.
Then the frequency of metabolic syndrome was compared by the three diagnostic criteria.
Results
The present study was carried out on 950 patients with diabetes type 2 in which 392 (41.3%) were male and 558 (58.7%) were female. The mean age of the patients was 56.0±11.6 (females 55.1±11.1 and males 57.2±12.2). The prevalence of metabolic syndrome according to ATPIII was 73.4% (men 64.8% and women 79.4%). According to the IDF criteria, it was 64.9% (men 46.7% and women 77.8%) and according to the new criteria, it was 70.4% (men 69% and women 71.3%). figure 1 compares the prevalence of metabolic syndrome according to the three criteria.
Figure 1.
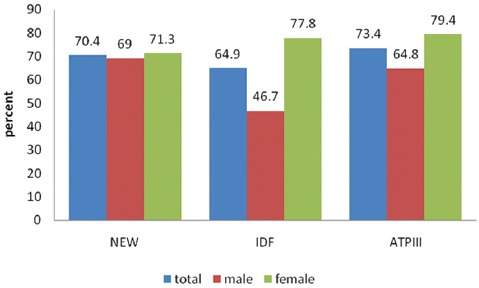
Shows the prevalence of metabolic syndrome according to the three criteria among type 2 diabetics in different age groups.
Based on the result of the three criteria, among the females low HDL, high BMI, weight, blood pressure, LDL, total cholesterol, and triglyceride were associated with increased metabolic syndrome prevalence. Age was significant according to the ATPIII and Gozashti criteria.
The compatibility score of the ATPIII and IDF according to the Kappa statistic was 0.49, for IDF and the new Kerman criteria was 0.66, and for ATPIII and the new Kerman criteria was 0.50.
Multivariate logistic regression adjusted for confounders, in people who had metabolic syndrome according to both IDF and ATPIII criteria, showed that gender, fasting blood sugar, triglycerides, HDL, waist circumference and systolic blood pressure were predictive factors for metabolic syndrome in the population. Also in people who had metabolic syndrome according to the three criteria, the same variables were able to predict the incidence of metabolic syndrome. The adjusted ORs with 95% confidence intervals are shown in table 1.
Table 1.
The adjusted OR with 95% confidence intervals for factors predicting metabolic syndrome according to both ATPIII and IDF
| Variables | P value | OR |
|---|---|---|
| Gender | 0.001 | 24.10 (12.35-47.02) |
| Waist circumference | 0.001 | 1.13 (1.10-1.17) |
| TG | 0.001 | 1.015 (1.01-1.02) |
| HDL | 0.001 | 0.87 (0.84-0.90) |
| Systolic blood pressure | 0.001 | 1.06 (1.05-1.08) |
| FBS | 0.001 | 1.01 (1.006-1.015) |
Discussion
In the present study, the prevalence of metabolic syndrome in patients with diabetes was 64% to 73%. In studies carried out in Ahvaz, the prevalence of metabolic syndrome in diabetic patients was 73.1% (ATPIII) and 64.9% (IDF),9 in Esfahan 65% (ATPIII),8 and in England 94% (both ATPIII & IDF).15 In other studies, the prevalence of metabolic syndrome was estimated to be 62.3% and 56.8% (IDF and ATPIII) in India,3 and 71.1% and 60.4% (IDF and ATPIII) in Sub-Saharan Africa.16
In the present study, according to the three criteria, the prevalence of metabolic syndrome was higher in women than men. In all other studies, the prevalence of metabolic syndrome was also higher in women than men.9,15 The reason might be less activity, more weight and higher prevalence of dyslipidemia in women.
The female gender, fasting blood sugar, triglyceride, cholesterol, HDL, waist circumference and systolic blood pressure were able to predict the prevalence of metabolic syndrome in people with diabetes. In the Ahvaz study, the female gender, physical activity, microalbuminuria, serum triglyceride and cholesterol, and in the Isfahan study, age, gender, fasting blood sugar, hypertension, BMI, serum triglyceride and serum cholesterol were the predictors of metabolic syndrome. The female gender, cholesterol, and triglyceride in all these studies were a predicting factor. The difference among other variables could be due to differences in data collection, sampling methods and using different criteria in diagnosing people with metabolic syndrome.8,9
Among the limitations of the present study is that the population was from Kerman province and the results may therefore not be generalisable to other populations.
Conclusion
The present study shows that the prevalence of metabolic syndrome in people with type 2 diabetes is very high in Kerman. People with predicting factors are in danger of developing metabolic syndrome.
Acknowledgment
This study was performed based on the data from the Kerman Healthy Heart Cohort. The authors acknowledge the Physiology Research Center of Kerman Medical University for providing data for this study. This study was funded by the deputy of Research at Kerman University of Medical Sciences.
Conflicts of Interest: None declared.
References
- 1.Katulanda P, Ranasinghe P, Jayawardana R, Sheriff R, Matthews DR. Metabolic syndrome among Sri Lankan adults: prevalence, patterns and correlates. Diabetol Metab Syndr. 2012;4:24. doi: 10.1186/1758-5996-4-24. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nolan CJ, Damm P, Prentki M. Type 2 diabetes across generations: from pathophysiology to prevention and management. Lancet. 2011;378:169–81. doi: 10.1016/S0140-6736(11)60614-4. [DOI] [PubMed] [Google Scholar]
- 3.Dhanaraj E, Bhansali A, Jaggi S, Dutta P, Jain S, Tiwari P, et al. Predictors of metabolic syndrome in Asian north Indians with newly detected type 2 diabetes. Indian J Med Res. 2009;129:506–14. [PubMed] [Google Scholar]
- 4.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–28. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 5.Basol G, Barutcuoglu B, Cakir Y, Ozmen B, Parildar Z, Kose T, et al. Diagnosing metabolic syndrome in type 2 diabetic Turkish patients: comparison of AHA/NHLBI and IDF definitions. Bratisl Lek Listy. 2011;112:253–9. [PubMed] [Google Scholar]
- 6.Motala AA, Esterhuizen T, Pirie FJ, Omar MA. The prevalence of metabolic syndrome and determination of the optimal waist circumference cutoff points in a rural South african community. Diabetes Care. 2011;34:1032–7. doi: 10.2337/dc10-1921. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rutaihwa MK. Prevalence and risk factors of metabolic syndrome among students at the University of Dar-es-salaam [dissertation] Tanzania: Muhimbili University of Health and Allied Sciences; 2011. p. 60. Available from: http://ir.muhas.ac.tz:8080/jspui/handle/123456789/40 . [Google Scholar]
- 8.Janghorbani M, Amini M. Metabolic syndrome in type 2 diabetes mellitus in isfahan, iran: prevalence and risk factors. Metab Syndr Relat Disord. 2007;5:243–54. doi: 10.1089/met.2005.0010. [DOI] [PubMed] [Google Scholar]
- 9.Rashidi H, Fardad F, Ghaderian B, Shahbazian HB, Latifi M, Karandish M, et al. Prevalence of metabolic syndrome and its predicting factors in type 2 diabetic patients in Ahvaz. Jundishapur Scientific Medical Journal. 2012;11:163–75. [Google Scholar]
- 10.Esteghamati A, Ashraf H, Rashidi A, Meysamie A. Waist circumference cut-off points for the diagnosis of metabolic syndrome in Iranian adults. Diabetes Res Clin Pract. 2008;82:104–7. doi: 10.1016/j.diabres.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 11.Gozashti MH, Najmeasadat F, Mohadeseh S, Najafipour H. Determination of most suitable cut off point of waist circumference for diagnosis of metabolic syndrome in Kerman. Diabetes Metab Syndr. 2014;8:8–12. doi: 10.1016/j.dsx.2013.10.022. [DOI] [PubMed] [Google Scholar]
- 12.Koh JH, Koh SB, Lee MY, Jung PM, Kim BH, Shin JY, et al. Optimal waist circumference cutoff values for metabolic syndrome diagnostic criteria in a Korean rural population. J Korean Med Sci. 2010;25:734–7. doi: 10.3346/jkms.2010.25.5.734. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmed N, Ahmad T, Hussain SJ, Javed M. Frequency of metabolic syndrome in patients with type-2 diabetes. J Ayub Med Coll Abbottabad. 2010;22:139–42. [PubMed] [Google Scholar]
- 14.Najafipour H, Mirzazadeh A, Haghdoost A, Shadkam M, Afshari M, Moazenzadeh M, et al. Coronary Artery Disease Risk Factors in an Urban and Peri-urban Setting, Kerman, Southeastern Iran (KERCADR Study): Methodology and Preliminary Report. Iran J Public Health. 2012;41:86–92. [ PMC Free Article] [PMC free article] [PubMed] [Google Scholar]
- 15.Song SH, Hardisty CA. Diagnosing metabolic syndrome in type 2 diabetes: does it matter? QJM. 2008;101:487–91. doi: 10.1093/qjmed/hcn034. [DOI] [PubMed] [Google Scholar]
- 16.Kengne AP, Limen SN, Sobngwi E, Djouogo CF, Nouedoui C. Metabolic syndrome in type 2 diabetes: comparative prevalence according to two sets of diagnostic criteria in sub-Saharan Africans. Diabetol Metab Syndr. 2012;4:22. doi: 10.1186/1758-5996-4-22. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]


