Abstract
Twenty years have passed since distraction osteogenesis was introduced into the field of craniomaxillofacial surgery, with distraction osteogenesis gradually consolidating its position for midface advancement in syndromic craniosynostosis. On the other hand, no consensus has been reached regarding its adaptation to calvarial bone. We reported that distraction osteogenesis was useful in posterior cranial vault expansion, and subsequently, similar reports have been successively observed worldwide. In posterior cranial vault distraction, intracranial capacity could be greatly expanded due to its simultaneous expansion with the scalp, with little risk of relapse because new bone is regenerated in the distraction gap. The possibility was suggested that the standard of first carrying out fronto-orbital advancement (FOA) for brachycephaly observed in syndromic craniosynostosis will greatly change posterior cranial vault distraction.
Keywords: craniosynostosis, distraction osteogenesis, posterior cranial vault distraction
Introduction
There are two major objectives of surgery for craniosynostosis. The first objective is to expand the cranial vault volume and prevent or reduce the raised intracranial pressure (ICP), while the second objective is to make an aesthetically prominent skull shape. In cases of syndromic craniosynostosis, sufficient cranial vault expansion becomes necessary due to severe stenosis of the cranial vault. Conventionally, it was regarded that carrying out fronto-orbital advancement (FOA) for cranial vault expansion was the standard and it has been recommended to carry out this treatment within 1 year following birth.1) However, in cases with posterior skull stenosis, it is not possible to achieve sufficient skull expansion through FOA alone. We were the first to report that in cases of craniosynostosis with posterior flattening, using the technique of distraction osteogenesis was very effective when carrying out posterior cranial vault expansion.2–5) In recent years, it has been reported from several influential craniofacial centers overseas that they routinely perform posterior cranial surgery as the initial intervention in such cases, with the efficacy thereof now clarified, thereby greatly changing the regime of treatment for syndromic craniosynostosis.6–9) We hereby provide an explanation on the updated experiences of posterior cranial vault distraction that the authors are conducting, in addition to reporting on recent trends regarding posterior cranial vault distraction.
Materials and Methods
A total of 13 patients, 6 males and 7 females aged between 3 months and 7 years averaged 1 year and 9 months old, were included in this series. Of the 13 patients, there were 3 with Crouzon syndrome, 1 with Pfeiffer syndrome, 1 with Apert syndrome, 1 with Saethre-Chotzen syndrome, 2 with multiple suture synostosis, 1 with unilateral coronal synostosis, 1 with unilateral lambdoid synostosis, 1 with pancraniosynostosis, 1 with frontonasal dysplasia, and 1 with cranial cleft. Outcomes were assessed by clinical examination and comparison of pre- and post-clinical photographs, three dimensional computed tomography (3D-CT) and magnetic resonance imaging (MRI) images. The follow-up period ranged from 3 months to 14 years.
Surgical Technique
The surgery was performed with the patient in a prone position. The scalp was elevated above the periosteum, while at the caudal side from the superior nuchal line the scalp was elevated under the muscle to reach the foramen magnum. In case of chronic tonsillar herniation, foramen magnum decompression was performed by shaving the upper half of the lip of the foramen magnum with a surgical burr. A biparietal craniectomy was performed at the widest portion of the calvarium and a transverse bioccipital craniectomy was made below the superior nuchal line. Osteotomized parietal and occipital bones were not detached from underlying dura. Barrel stave osteotomies were also performed on the inferior occipital segment and bone segments were greenstick fractured posteriorly to expand the suboccipital region. Occipital bone was fixed to these bone segments with absorbable plates bilaterally. It would improve contour of suboccipital region and obviate a bump between the osteotomized segment and cranial base. Care was taken to avoid injury to the sagittal and transverse sinuses. Finally two or three distractors (Keisei Medical Industrial Co., Tokyo) were applied to the osteotomized sites. Distraction was initiated on the 5th day postoperatively (Figs. 1, 2). The rate of distraction was 1 mm per day (rhythm: twice a day). The length of distraction ranged from 25 mm to 35 mm. From 8 weeks to 10 weeks after the completion of distraction, the patients returned for surgery to remove the distraction devices. In 5 out of 13 cases, FOA or fronto-orbital remodeling were performed at the time of removal of distraction devices.
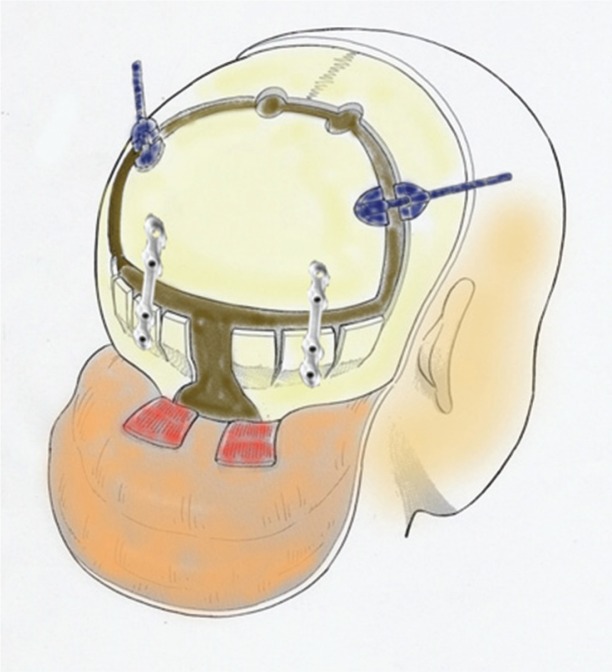
Fig. 1.
Schematic illustration of posterior cranial vault distraction with barrel stave osteotomy. A biparietal is performed and a transverse occipital osteotomy is made about 2 cm below Inion. Barrel stave osteotomy is also performed to expand subtentrial region. In the case with chronic tonsillar herniation, foramen magnum decompression is made. Finally, distractors are applied. (From CP Neurosurg 23: 1025–1031–2013,5) with permission.)
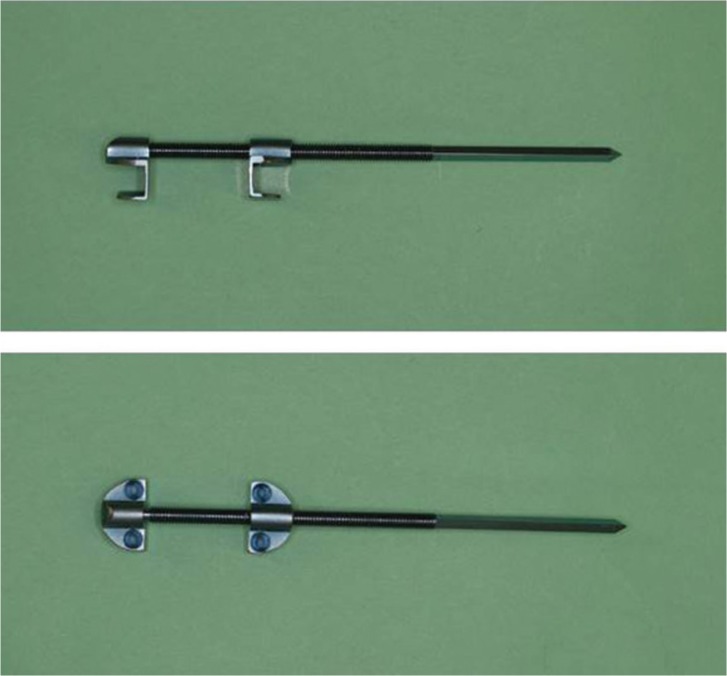
Fig. 2.
Distraction device with U-shaped plate used in this clinical series (Keisei Medical Industrial Co. Ltd., Tokyo).
Results
The patient in 1 case of Crouzon syndrome died from postoperative respiratory dysfunction with no causal relationship to the surgery. Sufficient posterior cranial expansion was carried out in the remaining 12 cases. The expanded distance was 23 mm to 35 mm. Regenerated bone was observed in the distraction gap upon 3D-CT. Subarachnoid spaces were expanded and stricture of the occipital lobe and the cerebellum was improved upon MRI, and it was revealed that the shapes of corpus callosum had greatly changed. In 2 cases of Pfeiffer syndrome and multiple suture synostosis, MRI demonstrated Chiari malformation preoperatively. In both cases, ascent of the cerebellar tonsil was noticed on MRI after expansion of occipital bone. Cerebrospinal fluid leak was observed in 1 case, for which dural repair was carried out in the operating room. The distraction device became dislodged in 1 case and so was re-fixated. Minor infection of the insertion site of the extender was observed in 6 cases, among which incisional drainage was required in 1 case; however, treatment was carried out by irrigating the affected area in the remaining 5 cases.
Cases
I. Case 1
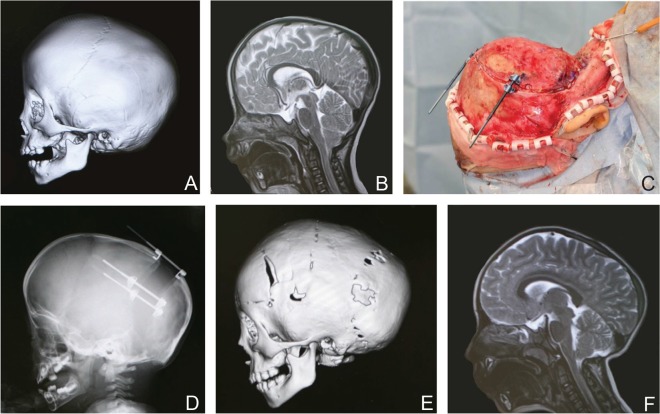
A male child with multiple suture synostosis. 3D-CT revealed that sagittal and bilateral lambdoid sutures were fused prematurely. In terms of appearance, his forehead was recessing. At 1 year and 10 months of age, he underwent posterior cranial vault distraction. Thirty millileter distraction was performed and then, the axis of distractors was cut at the point where it came out from scalp. After 2 months of consolidation period, distraction devices were removed and frontal remodeling was performed. The posterior cranium expanded, leading to good skull shape being acquired. Postoperative MRI revealed a reduction of Chiari malformation (Fig. 3).
Fig. 3.
A 1 year and 10 months old male child with multiple suture synostosis. A: Preoperative 3D-CT. Sagittal and bilateral lambdoid sutures were fused. B: Preoperative MRI image. Chiari malformation was noted. C: Intraoperative view. D: Skull X-P just after 32 mm distraction. E: 3D-CT at 1 year and 3 months after frontal remodeling. F: MRI image at 1 year and 3 months after frontal remodeling. Reduction of Chiari malformation was demonstrated. 3D-CT: three dimensional computed tomography, MRI: magnetic resonance imaging.
II. Case 2
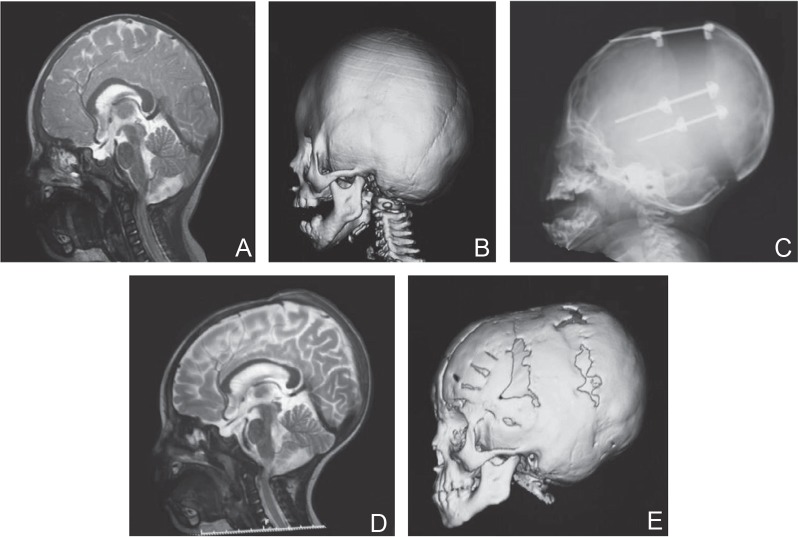
A male child with Saethre-Chotzen syndrome with bicoronal synostosis underwent posterior distraction at 1 year 3 months of age. After 4 days of waiting period, distraction was performed at a rate of 0.5 mm twice a day for 30 days. Followed by consolidation period for 2 months, the patient came back to the operative theater for the secondary surgery for removal of distractors and fronto-orbital remodeling. Postoperative course was uneventful. Large skull was obtained and posterior stenosis was released by observation of MRI image. Good aesthetic contour in forehead region was reconstructed (Fig. 4).
Fig. 4.
A 1 year and 3 months old boy with Saetre-Chotzen syndrome. A: Preoperative MRI. Significant stenosis of posterior in cerebellum and medulla oblongata region was seen. B: Preoperative 3D-CT image. C: Plain X-P after completion of 30 mm distraction. D: MRI image after distraction. Posterior stenosis was released and subarachnoid space was expanded. Note the change of the shape of corpus callosum. E: 3D-CT image at 1 year after fronto-orbital remodeling. 3D-CT: three dimensional computed tomography, MRI: magnetic resonance imaging.
Discussion
I. Distraction osteogenesis for the treatment of craniosynostosis
Since the report on mandibular lengthening by gradual distraction osteogenesis by McCarthy et al. in 1992,10) distraction osteogenesis of the facial bone has come to be widely used. Particularly in syndromic craniosynostosis such as Crouzon syndrome, Apert syndrome, Pfeiffer syndrome, etc., distraction osteogenesis is used for advancement of the midface, and has become widely diffused.11–13) Recently, there have been reports mentioning that monoblock osteotomy, which has been conventionally regarded as being of high risk, may be safely carried out by the distraction technique.14) The first use of bone lengthening of the skull was its use with FOA for brachycephaly by Hirabayashi et al.15) and subsequently, there have been reports on its use in nonsyndromic craniosynostosis such as plagiocephaly, scaphocephaly, brachydephaly, etc. in Japan, leading the world.11,16–20) However, many of these reports were on a small number of cases, with an evaluation of whether or not bone lengthening is useful for the skull not established as of yet.
Distraction osteogenesis offers the advantages of no need for bone grafting, no residual extradural dead space, the ability to maintain vascularity to the osteotomized bone through the attached dura, providing simultaneous scalp expansion, and the postoperative feasibility to actively reshape the skull. On the other hand, there is a disadvantage in that remodeling of the frontal skull cannot be performed. In particular, for cases involving regression of the lateral supraorbital region, modification is difficult.
II. Posterior cranial vault expansion
Occipital vault expansion should be considered for the patients of craniosynostosis with Chiari malformation, increased ICP, or syndromic cases with posterior flattening.21) At the same time, performing foramen magnum decompression enables suboccipital decompression, which can be a more effective surgical treatment. Particularly in syndromic cases with posterior flattening some cases were observed with stenosis of the outflow tract, inhibition of the venous reflux, etc. due to posterior stenosis, and it was believed that these may be improved by posterior cranial vault expansion. For typical cases of posterior vault expansion, after removing the supratentorial occipital bone, the torcular and transverse sinus are separated from the bone while epidural dissection is performed for the posterior fossa, and when the posterior edge of the foramen magnum is reached, the circumferential bones are dissected to the extent possible. The removed bones are treated via remodeling, if necessary, and replaced. However, in cases with high ICP, the occipital bone may be insufficiently formed and may show a honeycomb appearance. In such cases, it is extremely difficult to remove the occipital bone from the dura mater and this may cause tearing of the dura and massive bleeding. Therefore, it is difficult to remove the occipital bone and only a circumferential craniectomy may be performed in such a case. The occipital bone undergoing a craniectomy is fixed by a plate at the position where the occipital bone is expanded to the extent possible; however the expansion of the occipital bone was limited by scalp closure. Moreover, in cases with thin bones, it is difficult to perform plate fixation, and therefore, it is often the case that only craniectomy may be conducted. In cases with high ICP, a craniectomy alone causes expansion of the brain, which allows skull expansion to be achieved. However, there is a possibility that the occipital expansion may be insufficient when there is only natural expansion accompanied by expansion of the brain parenchyma. In addition, when the patient lies down in a supine position after the surgery, relapse may occur easily due to compression of the occipital bone. Furthermore, for patients with a ventriculoperitoneal (VP) shunt, it is difficult to achieve brain expansion after the surgery and there is high potential for the occurrence of relapse. From the above, although the necessity of posterior cranial expansion was evident, the acquired results were unfavorable despite complicated and high-risk surgery; therefore, it never became prevalent.
III. Posterior cranial vault distraction
We carried out posterior cranial vault distraction for unilateral lambdoid synostosis in 2004 that distraction osteogenesis was useful for posterior cranial vault expansion, reporting that good result was acquired.2) Subsequently, we have reported that posterior cranial vault distraction is also useful for multiple suture synostosis3) and syndromic craniosynostosis.4) Subsequently, several institutes have reported on posterior cranial vault distraction osteogenesis.6–9) With distraction osteogenesis, there is no need to elevate the bone from the dura by osteotomy alone; therefore, there is low risk for massive bleeding and by means of using distraction osteogenesis along with an extension tool following bone lengthening, the position of the osteotomized bone is retained during bone lengthening, rendering relapse uncommon even when children are placed in a supine position following surgery. Moreover, because neonatal bone is shaped in the distraction gap in the long term, relapse is uncommon. Another advantage of distraction osteogenesis is that scalp expansion may be carried out simultaneously, allowing great expansion exceeding 30 mm. Our method involves simultaneously carrying out barrel stave osteotomy. The subtentrial region may also be expanded by barrel stave osteotomies. Moreover, one section each on the left and right of the bone segments of barrel stave osteotomy and occipital bone were fixed with an absorbable plate, thereby allowing formation of a smooth posterior cranium. The distraction device used in this study does not employ a plate for fixation on the bone and only involves the insertion of a U-shaped plate into the osteotomized region. White et al. used a distractor with even footplates which requires screws to fix and carried out posterior calvarial vault distraction, with complications experienced involving loosening of the footplate in 3 among 6 cases.6) The skull bone of craniosynostosis patients is thin, so it is believed that using the same distractor having the U-shaped plate as we used is advisable.
Recently, spring-assisted cranioplasty in which springs have been applied to separate the calvarium across open lambdoid sutures have been reported.22) However, in spring-assisted cranioplasty, there are times when the expansion cannot be controlled and end with an insufficient result; therefore, it is believed that distraction osteogenesis using a distraction device is more effective.
IV. FOA vs. posterior cranial vault distraction
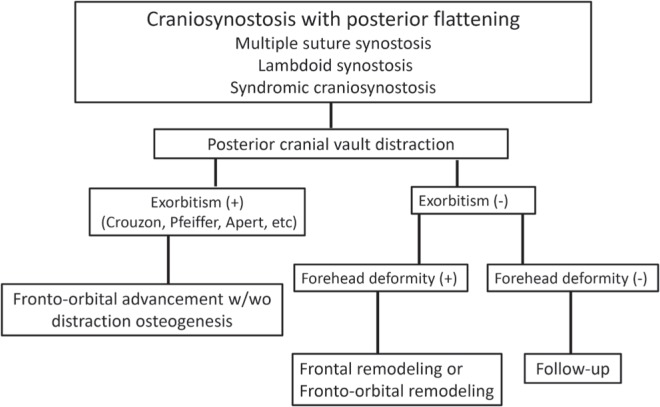
Conventionally, the standard was to carry out FOA as the treatment against syndromic craniosynostosis at age 1 or younger. However, in reality, there were cases in which the cranium could not be expanded as desired and regression was also observed even when FOA was carried out, and as a result, we frequently experienced deformation of the turricephalia of the cranium extending upwards (turribrachycephaly) along with the course. Such unfavorable results are believed to be caused due to the fact that sufficient intracranial capacity cannot be carried out using FOA alone. Moreover, improvement in exorbitism was observed due to FOA in cases observed with exorbitism, which was cosmetically significant; however, regarding cases without exorbitism, excessive FOA carried out in an attempt to increase the cranial volume resulted in a strange facial appearance with a protruding forehead. In cases of craniosynostosis with posterior flattening, it is believed to be important to first expand the posterior cranium and acquire sufficient expansion of the intracranial capacity. If the intracranial capacity may be sufficiently expanded at the posterior cranium, there is no need to forcibly expand the anterior cranium, thereby allowing formation of an anterior cranium with a specific shape. Choi et al. measured the scale of expansion of the intracranial capacity in the anterior cranium and posterior cranium in cranium expansion by computer simulation, and indicated that the effect of intracranial capacity expansion is greater by 35% when the posterior cranium is extended compared to the anterior cranium.23) We took a brain MRI of the posterior cranial vault distraction before and after surgery to observe the changes, and confirmed expansion of the corpus callosum in addition to the occipital lobe and cerebellum, along with normalization of the brain shape.5) Such changes are never observed in FOA. Moreover, there are reports mentioning that the shape of the anterior cranium naturally improved by expanding the posterior cranium in treatment for syndromic craniosynostosis (improvement of the anterior appearance of even the anterior vault which is untouched).8) In this manner, in recent years, a succession of reports have been released worldwide on replication studies of posterior cranial vault distraction osteogenesis and evaluating this, with the conventional standard of first carrying out FOA for brachycephalic skull changed and the paradigm potentially greatly shifting to “initially expand the posterior cranial vault.” Our procedures include carrying out posterior cranial vault distraction osteogenesis as the initial procedure for craniosynostosis with posterior flattening such as multiple suture synostosis, bicoronal synostosis, and syndromic craniosynostosis. For the case with a raised ICP, surgery should be carried out early in less than 1 year old. Even in the case with thin occipital bone which has a radiographic honeycomb appearance observed sometimes in turribrachycephaly, syndromic craniosynostosis and clover-leaf skull, it is possible to perform the expansion of the skull using this method. However, since the strength of the bone is weak, it is necessary to consider increasing the number of distraction devices or slowing extension rate down. If the patient is observed with exorbitism, FOA is continually carried out by distraction osteogenesis. If exorbitism is not observed, the case is followed-up; alternatively, frontal remodeling or fronto-orbital remodeling may be carried out for improving the forehead shape (Fig. 5).
Fig. 5.
Algorism for the treatment of craniosynostosis with posterior flattening.
Acknowledgments
This work was supported in part by a research grant from the Ministry of Health, Labor, and Welfare, Japan.
References
- 1). Persing JA, Jane JA: Neurosurgical treatment of craniosynostosis, in Cohen MM, Jr, Maclean RE. (eds): Craniosynostosis: Diagnosis, Evaluation, and Management. New York, Oxford University Press, 2000, pp 209–211 [Google Scholar]
- 2). Komuro Y, Yanai A, Hayashi A, Miyajima M, Nakanishi H, Arai H: Treatment of unilateral lambdoid synostosis with cranial distraction. J Craniofac Surg 15: 609– 613, 2004. [DOI] [PubMed] [Google Scholar]
- 3). Komuro Y, Hashizume K, Koizumi T, Miyajima M, Nakanishi H, Arai H: Cranial expansion with distraction osteogenesis for multiple-suture synostosis in school-aged children. J Craniofac Surg 20: 457– 460, 2009. [DOI] [PubMed] [Google Scholar]
- 4). Komuro Y, Shimizu A, Ueda A, Miyajima M, Nakanishi H, Arai H: Whole cranial vault expansion by continual occipital and fronto-orbital distraction in syndromic craniosynostosis. J Craniofac Surg 22: 269– 272, 2011. [DOI] [PubMed] [Google Scholar]
- 5). Komuro Y, Shimoji K, Miyajima M, Arai H: Distraction osteogenesis in the treatment of craniosynostosis. CP Neurosurg 23: 1025– 1031, 2013. (Japanese) [Google Scholar]
- 6). White N, Evans M, Dover MS, Noons P, Solanki G, Nishikawa H: Posterior calvarial vault expansion using distraction osteogenesis. Childs Nerv Syst 25: 231– 236, 2009. [DOI] [PubMed] [Google Scholar]
- 7). Steinbacher DM, Skirpan J, Puchała J, Bartlett SP: Expansion of the posterior cranial vault using distraction osteogenesis. Plast Reconstr Surg 127: 792– 801, 2011. [DOI] [PubMed] [Google Scholar]
- 8). Goldstein JA, Paliga JT, Wink JD, Low DW, Bartlett SP, Taylor JA: A craniometric analysis of posterior cranial vault distraction osteogenesis. Plast Reconstr Surg 131: 1367– 1375, 2013. [DOI] [PubMed] [Google Scholar]
- 9). Nowinski D, Di Rocco F, Renier D, SainteRose C, Leikola J, Arnaud E: Posterior cranial vault expansion in the treatment of craniosynostosis. Comparison of current techniques. Childs Nerv Syst 28: 1537– 1544, 2012. [DOI] [PubMed] [Google Scholar]
- 10). McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH: Lengthening the human mandible by gradual distraction. Plast Reconstr Surg 89: 1– 8; discussion 9–10, 1992. [PubMed] [Google Scholar]
- 11). Akizuki T, Komuro Y, Ohmori K: Distraction osteogenesis for craniosynostosis. Neurosurg Focus 9: 1– 7, 2000. [DOI] [PubMed] [Google Scholar]
- 12). Cohen SR, Rutrick RE, Burstein FD: Distraction osteogenesis of the human craniofacial skeleton: initial experience with new distraction system. J Craniofac Surg 6: 368– 374, 1995. [DOI] [PubMed] [Google Scholar]
- 13). Polley JW, Figueroa AA: Management of severe maxillary deficiency in childhood and adolescence through distraction osteogenesis with an external, adjustable, rigid distraction device. J Craniofac Surg 8: 181– 185; discussion 186, 1997. [DOI] [PubMed] [Google Scholar]
- 14). Bradley JP, Gabbay JS, Taub PJ, Heller JB, O’Hara CM, Benhaim P, Kawamoto HK: Monobloc advancement by distraction osteogenesis decreases morbidity and relapse. Plast Reconstr Surg 118: 1585– 1597, 2006. [DOI] [PubMed] [Google Scholar]
- 15). Hirabayashi S, Sugawara Y, Sakurai A, Harii K, Park S: Frontoorbital advancement by gradual distraction. Technical note. J Neurosurg 89: 1058– 1061, 1998. [DOI] [PubMed] [Google Scholar]
- 16). Imai K, Komune H, Toda C, Nomachi T, Enoki E, Sakamoto H, Kitano S, Hatoko M, Fujimoto T: Cranial remodeling to treat craniosynostosis by gradual distraction using a new device. J Neurosurg 96: 654– 659, 2002. [DOI] [PubMed] [Google Scholar]
- 17). Komuro Y, Yanai A, Hayashi A, Nakanishi H, Miyajima M, Arai H: Cranial reshaping employing distraction and contraction in the treatment of sagittal synostosis. Br J Plast Surg 58: 196– 201, 2005. [DOI] [PubMed] [Google Scholar]
- 18). Sugawara Y, Hirabayashi S, Sakurai A, Harii K: Gradual cranial vault expansion for the treatment of craniofacial synostosis: a preliminary report. Ann Plast Surg 40: 554– 565, 1998. [DOI] [PubMed] [Google Scholar]
- 19). Sugawara Y, Uda H, Sarukawa S, Sunaga A: Multidirectional cranial distraction osteogenesis for the treatment of craniosynostosis. Plast Reconstr Surg 126: 1691– 1698, 2010. [DOI] [PubMed] [Google Scholar]
- 20). Kobayashi S, Honda T, Saitoh A, Kashiwa K: Unilateral coronal synostosis treated by internal forehead distraction. J Craniofac Surg 10: 467– 471; discussion 472, 1999. [DOI] [PubMed] [Google Scholar]
- 21). Persing JA, Delashaw JB, Jane JA, Edgerton MT: Lambdoid synostosis: surgical considerations. Plast Reconstr Surg 81: 852– 860, 1988. [DOI] [PubMed] [Google Scholar]
- 22). Lauritzen CG, Davis C, Ivarsson A, Sanger C, Hewitt TD: The evolving role of springs in craniofacial surgery: the first 100 clinical cases. Plast Reconstr Surg 121: 545– 554, 2008. [DOI] [PubMed] [Google Scholar]
- 23). Choi M, Flores RL, Havlik RJ: Volumetric analysis of anterior versus posterior cranial vault expansion in patients with syndromic craniosynostosis. J Craniofac Surg 23: 455– 458, 2012. [DOI] [PubMed] [Google Scholar]