Abstract
Confirming the patency of the proximal parent and distal artery is necessary in cerebral aneurysm surgery. To understand the relationship between the parent and distal arteries of the aneurysm, the blood vessels running through the subarachnoid space should be extensively dissected, which is time consuming. To examine the efficacy of a temporary clip with indocyanine green (ICG) technique, in which the parent artery is temporarily occluded using a temporary clip, an ICG videoangiography (ICGVAG) is performed to clarify the relationship between the distal artery and the proximal parent artery. Three patients with a distal aneurysm. This technique was used to confirm the connection of the parent and the distal artery in distal aneurysms. With regard to middle cerebral artery (MCA), the procedure is conducted as follows. First, the M2 within the Sylvian fissure is investigated to ensure the absence of atherosclerosis and perforators and that this vessel could undergo occlusion by temporary clipping. The subarachnoid space surrounding the distal artery of the lesion site suspected of an existent aneurysm is dissected. The image range of the ICGVAG is set sufficiently wide to accommodate the possibility that the distal artery is not the artery that was anticipated. Subsequently, after the temporary clip occlusion is completed, the ICGVAG is recorded. In the three distal aneurysms, the relationship between the aneurysm, the distal artery, and the parent artery was confirmed. This method was useful, suggesting that unnecessary dissection in the subarachnoid space might be reduced.
Keywords: cerebral aneurysm, indocianine, parent artery
Introduction
Distal cerebral aneurysms account for approximately 7.4–9.3% of all cerebral aneurysms and are reported1–10) to occur frequently in the anterior cerebral artery, middle cerebral artery (MCA) and posterior inferior cerebellar artery (PICA). Because there are few anatomical indicators for the surgical treatment of distal aneurysms, ascertaining the lesion site is more difficult2,3,5,10–14) than it is for aneurysms at the Circle of Willis. Because the simple clipping of distal aneurysms is technically challenging, parent artery occlusion and revascularization surgery7–9,15) of the distal artery is often required. Consequently, even after the aneurysm is detected, the site of anastomosis of the distal recipient arteries should be confirmed.7,8,15) In cases where aneurysm clipping is difficult, even when the aneurysm itself is detected using a navigation system,4,5,11,12) it is important to confirm the relationship between the proximal artery and the aneurysm to perform the surgical clipping safely. Germanwala et al. suggested that precise surgical localization of distal aneurysms could be difficult. Uncertainty regarding the exact location of these vascular lesions might result in larger craniotomies and unnecessary exploratory arachnoid and pial dissection. To reconstruct the artery, it is necessary7,10,12,15,16) to ascertain the vessel that is distal to the aneurysm.
The purpose of this study was to confirm the benefits of temporarily occluding the proximal artery while performing indocyanine green videoangiography (ICGVAG)16–20) to confirm the continuation of the distal/peripheral blood vessels. Since 2003, ICGVAG has become established19,20) as a noninvasive angiography technique that is performed intra-operatively,19,20) quickly, safely, and easily on intracranial blood vessels in cerebral aneurysm cases. This article describes a practical application of this technique.
Methods
During the period from March 2007 through December 2012, temporary clipping with ICGVAG was used in one case with a ruptured distal MCA aneurysm and two cases with ruptured distal PICA in which determination of the relationship between the distal and proximal artery associated with the aneurysm was necessary. A combination of temporary clipping and ICGVAG was used to clarify the relationship between the distal and proximal arteries. ICG imaging was possible in all cases and no ICG allergic reactions were observed.
I. Basic technique of temporary clip with ICG
The surgical treatments for aneurysms were performed using a Carl Zeiss surgical microscope OPMI Pentero INFRARED 800 (Carl Zeiss Co., Tokyo). Digital subtraction angiography findings were used to identify the parent artery, which was most likely upstream of the aneurysm, and to open the subarachnoid space near the parent artery. The area near the M1–M2 junction of the sylvian fissure was dissected. With regard to the distal PICA aneurysm, after an occipital midline skin incision, the PICA on the affected side within the cisterna magna was confirmed. The proximal PICA in the tonsillar segment without perforating arteries and arteriosclerotic changes was confirmed, and Sugita No. 51 temporary clips (Mizuho Corp., Tokyo) were used to occlude the vessel safely. The arachnoid membrane surrounding the artery in the section thought to contain the correct distal donor arteries was incised, and the arachnoid membrane was dissected where the blood vessel was clearly visible on the ICGVAG imaging. All the structures were placed within the ICGVAG field of vision, and the imaging was initiated after the temporary clip was applied. After performing ICGVAG (0.3 mg/kg) for 1 min, the Sugita clip was removed while continuing ICGVAG. Following the recanalization, the patency of the blood vessel with no contrast medium in its lumen was confirmed by removal of the temporary clips. The level of dye in the peripheral segment of the PICA was temporarily diminished or increased after the clip removal.
The ICGVAG was conducted in three stages. First, the area of the sulcus suspected of containing the aneurysm was dissected. In the event that revascularization was required, the ICGVAG images of the parent artery including the appropriate distal blood vessel were captured. After confirming the aneurysmal neck, the ICGVAG images were captured before applying the aneurysmal clip. Finally, the images were captured to confirm the complete clipping and patency of the distal artery.
II. Representative case 1
A 78-year-old female presented with headache and subarachnoid hemorrhage. A concurrent fourth intraventricular hemorrhage from rupture of the distal PICA was detected. Three-dimensional computed tomography (CT) angiography (Fig. 1, left) revealed a distal aneurysm (4 mm) in the cortical segment of the left PICA. The surgery involved opening the dura with a Y-shaped occipital midline skin incision. The PICA on the left side was initially confirmed in the tonsillomedullary segment.21) On the brain surface, two arteries believed to be the distal PICA were identified (Fig. 2, left). The tonsillomedullary segment of the left PICA located at the dorsal brain stem with no arteriosclerotic change and a branch toward the brainstem were temporarily occluded using a Sugita No. 51 temporary clip. The ICGVAG was then initiated. The peripheral segment of the PICA was satisfactorily dyed after an injection of ICG, and after removal of the temporary clip, the level of dye in the peripheral PICA segment temporarily diminished (Fig. 2, right). Based on this finding, the peripheral PICA segment received circulation and dye from the anterior inferior cerebellar artery collaterals. In this patient, the left PICA and the anterior inferior cerebellar artery branched from the identical left vertebral artery segment. This procedure confirmed which of the two arteries on the brain surface was the distal PICA, and by tracing this artery proximally, we confirmed the aneurysm site. Before and after the clipping (Fig. 3) of the aneurysm, the preservation of the blood flow to the distal artery was verified using ICGVAG. After the operation, the case progressed without symptomatic vasospasms, and there was no ischemic change in the cerebellum based on the postoperative diffusion-weighted imaging on day 3. The blood flow through the distal/peripheral part of the PICA was confirmed by cerebral angiography (Fig. 1, right).
Fig. 1.
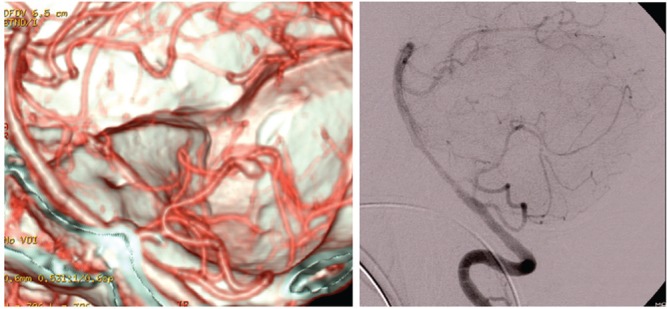
Left: Initial preoperative three-dimensional computed tomography (CT) angiography demonstrating a distal posterior inferior cerebellar artery aneurysm on the cortical segment. The posterior inferior cerebellar artery and the anterior inferior cerebellar artery were branching from almost the identical segment of the vertebral artery. Right: The post-operative lateral view of the left vertebral digital subtraction angiography showing good patency of the distal posterior inferior cerebellar artery and no residual aneurysm is seen.
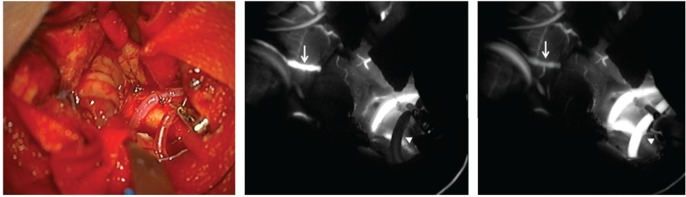
Fig. 2.
Left: The microscopic findings of the surgical field. The tonsillomedullary segment of the left posterior inferior cerebellar artery was temporary clipped. Middle: An ICGVAG image taken 16 s after the ICG infusion. The peripheral left posterior inferior cerebellar artery (white arrow) was enhanced from the collateral circulation. The proximal side of the posterior inferior cerebellar artery was not enhanced (arrowhead), because of the temporary clip. Right: An ICGVAG image taken 22 s after the ICG infusion just after the removal of the temporary clip. The enhancement of the peripheral left posterior inferior cerebellar artery (arrowhead) was diminished (white arrow) just after the removal (arrowhead) of the clip. ICGVAG: indocyanine green videoangiography.
Fig. 3.
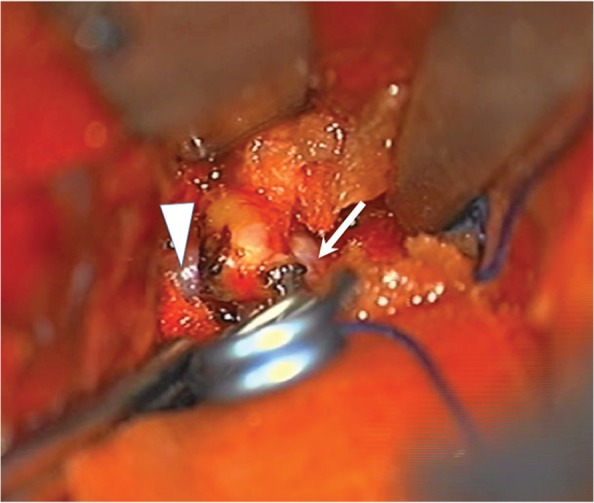
The microscopic findings of the aneurysm after clipping. The white arrow indicates the proximal artery, and the white arrowhead indicates the distal artery.
III. Representative case 2
A 52-year-old female presented with a left hemiparesis and subarachnoid hemorrhage. A concurrent intracerebral hemorrhage from rupture of the distal MCA aneurysm was detected. The M1M2 bifurcation of the MCA was initially confirmed via the pterional approach. The frontal M2 with the parent artery of the aneurysm was temporarily occluded using a Sugita No. 52 temporary clip, and ICGVAG was initiated. The frontal branch of the M4 was thinly dyed and, immediately, another branch of the M4 was thickly dyed by an injection of ICG; after removal of the temporary clip, the level of the dye in the frontal branch of the M4 temporarily increased and diminished (Fig. 4 A–C). The flow 800 analysis indicated a temporary change of intensity of the frontal branch of the M4 (Fig. 5). By tracing this artery proximally, we confirmed the sulcus, which located the aneurysm. After the clipping of the aneurysm, the preservation of the blood flow to the distal artery was verified using ICGVAG. After the operation, the case progressed without symptomatic vasospasms, and there was no ischemic CT change on day 1. The blood flow through the distal/peripheral part of the MCA was confirmed by the cerebral angiography.
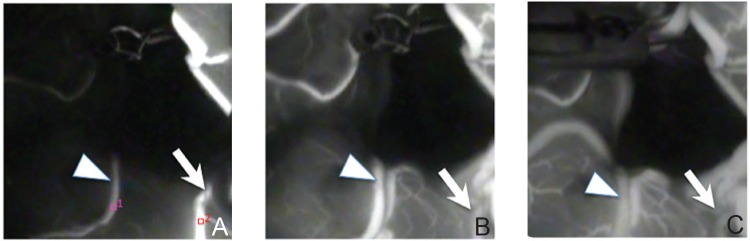
Fig. 4.
Intraoperative ICGVAG images. Image A was captured 11 s after the ICG infusion before the removal of the temporary clip. The frontal peripheral middle cerebral artery (arrowhead) has been thinly enhanced. The temporal peripheral middle cerebral artery (arrow) has been thickly enhanced. Image B was captured just before the removal of temporary clip. The frontal peripheral middle cerebral artery (arrowhead) and the temporal peripheral middle cerebral artery (arrow) have been enhanced at the same level. Image C was captured just after the removal of the temporary clip. The enhancement of the frontal peripheral middle cerebral artery (arrowhead) was diminished just after the removal of the clip. ICGVAG: indocyanine green videoangiography.
Fig. 5.
Fluorescent intensity curve with the Carl Zeiss FLOW 800 system (Carl Zeiss Co., Tokyo). The pink curve indicates the frontal peripheral middle cerebral artery and the red curve indicates the frontal peripheral middle cerebral artery. The blue circle on the pink curve indicates a temporary change of intensity just after the removal of the temporary clip.
IV. Representative case 3
An 89-year-old female presented with severe headache, nausea, and subarachnoid hemorrhage. Digital subtraction angiography (Fig. 6, upper left) revealed a distal aneurysm (5 mm) in the distal left PICA. The midline suboccipital approach and PICA on the left side was initially confirmed in the tonsillomedullary segment. On the brain surface, two arteries thought to be the distal PICA were identified. After the temporary occlusion of the left PICA located at the dorsal brain stem using a Sugita No. 51 temporary clip, the ICGVAG was initiated. The peripheral segment of the PICA was thinly dyed after an injection of ICG, and after removal of the temporary clip, the level of dye in the peripheral PICA segment temporarily increased and diminished (Fig. 6, upper right and lower left). This procedure confirmed the artery on the brain surface that was the distal PICA, and we confirmed the aneurysm site by tracing this artery proximally. Before (Fig. 6, lower right) and after the clipping of the aneurysm, the preservation of the blood flow to the distal artery was verified using ICGVAG. After the operation, there was no ischemic change in the cerebellum based on the postoperative CT on days 1 and 7.
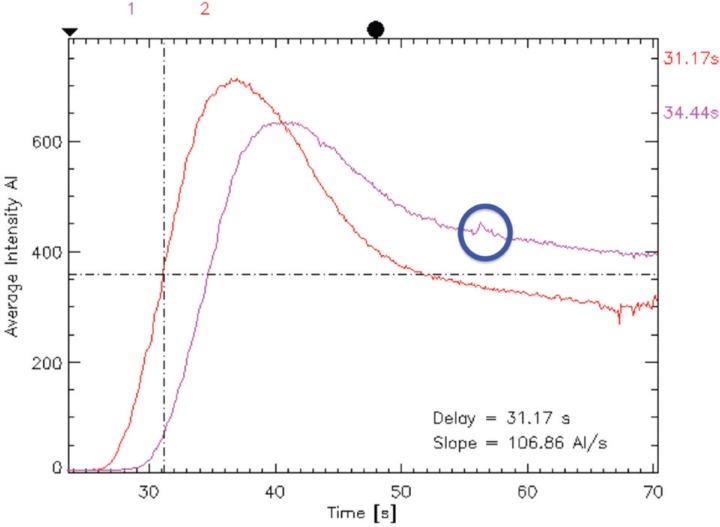
Fig. 6.
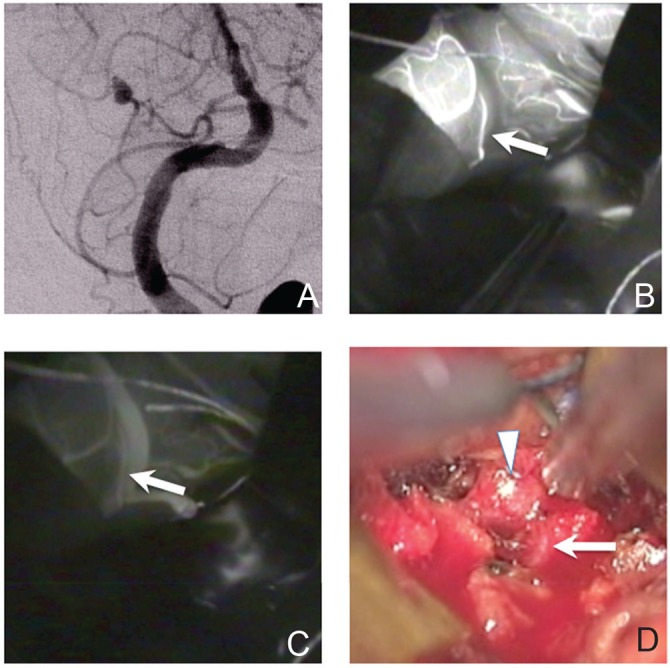
Upper left: Anterior posterior view of the initial digital subtraction angiography demonstrating a distal posterior inferior cerebellar artery aneurysm on the cortical segment. Upper right: An ICGVAG image taken 22 s after ICG infusion. The peripheral left posterior inferior cerebellar artery (white arrow) vessel has been thinly enhanced. Lower left: An ICGVAG image just after the removal of the temporary clip. The strength of the enhancement of the peripheral left PICA (white arrow) was changed. Lower right: The microscopic findings of the aneurysm before clipping. The white arrow indicates the proximal artery, and the white arrowhead indicates the aneurysm. ICGVAG: indocyanine green videoangiography, PICA: posterior inferior cerebellar artery.
Discussion
Whereas the three cases represent a very limited group, the intraoperative findings, postoperative diffusion-weighted magnetic resonance imaging, and postoperative magnetic resonance angiography revealed no complications associated with this method. With this technique, there were various types of acuity or whiteness in the ICGVAG findings of the distal artery because of the level of the collateral circulation. Because of the length from the final bifurcation to the occluded site of the occluded artery, the alterations of the acuity or whiteness of the distal artery after the removal of the temporary clipping were different among the cases. In all cases, the acuity alteration after the removal of the temporary clip was clearly visible to distinguish between the connecting artery and the non-connecting artery.
Rodríguez-Hernández et al.18) examined 140 distal aneurysm cases (61 distal anterior cerebral artery, 29 distal posterior inferior cerebellar artery, and 23 distal middle cerebral artery). Notably, 10 of the 23 distal MCA cases and 7 of the 29 distal posterior inferior cerebellar artery cases required revascularization.18) When performing revascularization, it is necessary to determine the appropriate artery suitable for vascular anastomosis peripheral to the distal aneurysm. In such instances, a temporary clip with the ICG method appears to be useful. Because there are no anatomical indices for distal aneurysms,1,4,5,7,8) detection is more difficult than for aneurysms near the Circle of Willis. Raza et al.17) demonstrated that accurate localization in neurosurgery for distal aneurysms is sometimes challenging. Inaccurate localization of these vascular lesions might result in larger craniotomies and unnecessary arachnoid and pial dissection with possible resultant permanent neurological injury. Numerous reports3,7,17) have shown the importance of stereotaxy-based studies for the localization of such vascular lesions. Small vascular lesions are frequently difficult to visualize on such imaging. Lee and Bang reported that with the assistance of neuronavigation CT, they were able to locate aneurysms accurately without corticotomy and to avoid causing further cortical injury by an approach through the sulci. With regard to neuronavigation, our method is not helpful in determining the appropriate craniotomy site. By simplifying the establishment of the relationship among the parent artery, the aneurysm, and the distal artery, cortical injury might be avoided, and this method might be useful to prevent intraoperative premature rupture.
Conclusion
In the three distal cerebral aneurysm cases in which surgery was performed, the relationship between the aneurysm, the distal artery, and the parent artery was confirmed by the temporary clip with ICG method. Our results indicate that this method might contribute to reducing the duration of surgery as well as avoiding brain damage by reducing the size of the subarachnoid space opening. We found this method to be useful and suggest that it might reduce unnecessary dissection in the subarachnoid space.
References
- 1). Dashti R, Hernesniemi J, Niemelä M, Rinne J, Lehecka M, Shen H, Lehto H, Albayrak BS, Ronkainen A, Koivisto T, Jääskeläinen JE: Microneurosurgical management of distal middle cerebral artery aneurysms. Surg Neurol 67: 553– 563, 2007. [DOI] [PubMed] [Google Scholar]
- 2). Horiuchi T, Tanaka Y, Takasawa H, Murata T, Yako T, Hongo K: Ruptured distal middle cerebral artery aneurysm. J Neurosurg 100: 384– 388, 2004. [DOI] [PubMed] [Google Scholar]
- 3). Horiuchi T, Tanaka Y, Hongo K, Nitta J, Kusano Y, Kobayashi S: Characteristics of distal posteroinferior cerebellar artery aneurysms. Neurosurgery 53: 589– 595; discussion 595–596, 2003. [DOI] [PubMed] [Google Scholar]
- 4). Joo SP, Kim TS, Choi JW, Lee JK, Kim YS, Moon KS, Kim JH, Kim SH: Characteristics and management of ruptured distal middle cerebral artery aneurysms. Acta Neurochir (Wien) 149: 661–667, 2007. [DOI] [PubMed] [Google Scholar]
- 5). Lee SH, Bang JS: Distal middle cerebral artery M4 aneurysm surgery using navigation-CT angiography. J Korean Neurosurg Soc 42: 478– 480, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Lewis SB, Chang DJ, Peace DA, Lafrentz PJ, Day AL: Distal posterior inferior cerebellar artery aneurysms: clinical features and management. J Neurosurg 97: 756– 766, 2002. [DOI] [PubMed] [Google Scholar]
- 7). Matano F, Murai Y, Tateyama K, Mizunari T, Umeoka K, Koketsu K, Kobayashi S, Teramoto A: Perioperative complications of superficial temporal artery to middle cerebral artery bypass for the treatment of complex middle cerebral artery aneurysms. Clin Neurol Neurosurg 115: 718– 724, 2013. [DOI] [PubMed] [Google Scholar]
- 8). Nussbaum ES, Madison MT, Goddard JK, Lassig JP, Nussbaum LA: Peripheral intracranial aneurysms: management challenges in 60 consecutive cases. J Neurosurg 110: 7– 13, 2009. [DOI] [PubMed] [Google Scholar]
- 9). Orakcioglu B, Schuknecht B, Otani N, Khan N, Imhof HG, Yonekawa Y: Distal posterior inferior cerebellar artery aneurysms: clinical characteristics and surgical management. Acta Neurochir (Wien) 147: 1131–1139; discussion 1139, 2005. [DOI] [PubMed] [Google Scholar]
- 10). Raza SM, Papadimitriou K, Gandhi D, Radvany M, Olivi A, Huang J: Intra-arterial intraoperative computed tomography angiography guided navigation: a new technique for localization of vascular pathology. Neurosurgery 71(2 Suppl Operative): ons240–ons252, 2012. [DOI] [PubMed] [Google Scholar]
- 11). Chibbaro S, Tacconi L: Image-guided microneurosurgical management of vascular lesions using navigated computed tomography angiography. An advanced IGS technology application. Int J Med Robot 2: 161– 167, 2006. [DOI] [PubMed] [Google Scholar]
- 12). Germanwala AV, Thai QA, Pradilla G, Tamargo RJ: Simple technique for intraoperative angiographic localization of small vascular lesions. Neurosurgery 67: 818– 822; discussion 822–823, 2010. [DOI] [PubMed] [Google Scholar]
- 13). Rodríguez-Hernández A, Zador Z, Rodríguez Mena R, Lawton MT: Distal aneurysms of intracranial arteries: application of numerical nomenclature, predilection for cerebellar arteries, and results of surgical management. World Neurosurg 80: 103– 112, 2013. [DOI] [PubMed] [Google Scholar]
- 14). Schmid-Elsaesser R, Muacevic A, Holtmannspötter M, Uhl E, Steiger HJ: Neuronavigation based on CT angiography for surgery of intracranial aneurysms: primary experience with unruptured aneurysms. Minim Invasive Neurosurg 46: 269– 277, 2003. [DOI] [PubMed] [Google Scholar]
- 15). Ishikawa T, Kamiyama H, Kobayashi N, Tanikawa R, Takizawa K, Kazumata K: Experience from “double-insurance bypass.” Surgical results and additional techniques to achieve complex aneurysm surgery in a safer manner. Surg Neurol 63: 485– 490; discussion 490, 2005. [DOI] [PubMed] [Google Scholar]
- 16). Murai Y, Adachi K, Takagi R, Koketsu K, Matano F, Teramoto A: Intraoperative Matas test using microscope-integrated intraoperative indocyanine green videoangiography with temporary unilateral occlusion of the A1 segment of the anterior cerebral artery. World Neurosurg 76: 477.e7–e477.e10, 2011. [DOI] [PubMed] [Google Scholar]
- 17). Murai Y, Adachi K, Koketsu K, Teramoto A: Indocyanine green videoangiography of optic cavernous angioma—case report. Neurol Med Chir (Tokyo) 51: 296–298, 2011. [DOI] [PubMed] [Google Scholar]
- 18). Murai Y, Adachi K, Matano F, Tateyama K, Teramoto A: Indocyanin green videoangiography study of hemangioblastomas. Can J Neurol Sci 38: 41– 47, 2011. [PubMed] [Google Scholar]
- 19). Raabe A, Nakaji P, Beck J, Kim LJ, Hsu FP, Kamerman JD, Seifert V, Spetzler RF: Prospective evaluation of surgical microscope-integrated intraoperative near-infrared indocyanine green videoangiography during aneurysm surgery. J Neurosurg 103: 982– 989, 2005. [DOI] [PubMed] [Google Scholar]
- 20). Sekhar LN, Stimac D, Bakir A, Rak R: Reconstruction options for complex middle cerebral artery aneurysms. Neurosurgery 56 (1 Suppl): 66– 74; discussion 66–74, 2005. [DOI] [PubMed] [Google Scholar]
- 21). Woitzik J, Horn P, Vajkoczy P, Schmiedek P: Intraoperative control of extracranial-intracranial bypass patency by near-infrared indocyanine green videoangiography. J Neurosurg 102: 692– 698, 2005. [DOI] [PubMed] [Google Scholar]