Abstract
We describe a practical technique of superior turbinectomy followed by posterior ethmoidectomy as a less invasive procedure for two-surgeon technique on endoscopic endonasal transsphenoidal surgery. After identification of the superior turbinate and the sphenoid ostium, the inferior third portion of the superior turbinate was coagulated and resected. This partial superior turbinectomy procedure exposed the posterior ethmoidal sinus. Resection of the bony walls between the sphenoid and posterior ethmoid sinuses provided more lateral and superior exposure of the sphenoid sinus. This technique was performed in 56 patients with midline skull base lesions, including 49 pituitary adenomas and 7 other lesions. Meticulous manipulation of instruments was performed in all cases without surgical complications such as permanent hyposmia/anosmia or nasal bleeding. Our findings suggested that the partial superior turbinectomy followed by retrograde posterior ethmoidectomy is a simple and safe technique providing a sufficient surgical corridor for two-surgeon technique to approaching midline skull base regions, mainly involving pituitary adenomas.
Keywords: endoscopic endonasal surgery, posterior ethmoidectomy, superior turbinectomy, transsphenoidal approach
Introduction
The transsphenoidal route represents the least invasive neurosurgical approach to the sellar region. Advances in endoscopic sinus surgery (ESS) in otorhinolaryngology (ear-nose-throat; ENT) have led to the introduction of an endoscope to transsphenoidal surgery and a switch from a microscopic transseptal approach with sublabial incision to an endoscopic endonasal approach via a natural orifice, namely the nostril. The bi-nostril approach with a two-surgeon technique involving both a neurosurgeon and an ENT surgeon has played an important role in the recent development of extended endoscopic endonasal approaches to ventral skull base lesions.
The modern pituitary surgery also has come to require the meticulous manipulation of instruments under endoscopic vision to achieve an extracapsular dissection of adenomas safely. The bi-nostril two-surgeon technique can provide a wider manipulation angle and high-definition endoscopic vision, leading to fine movement of instruments. To perform this technique successfully, a creation of larger surgical space is mandatory compared to a standard single-surgeon technique.
A superior turbinectomy has been valued as a procedure not only to identify the sphenoid ostium but also to extend the sphenoidotomy more laterally in endoscopic endonasal transsphenoidal surgery (EETS); however, this procedure has not yet been described in detail by previous reports. Wherein, we applied a partial superior turbinectomy for the bi-nostril two-surgeon technique in pituitary surgery. The objectives of this study were to present the practical technique of superior turbinectomy in EETS and to discuss anatomical and availability aspects of this procedure.
Materials and Methods
After institutional review board’s approval, a retrospective case review was performed in patients who had undergone EETS for the treatment of pathologies in the sellar/parasellar region performed from January 2010 to March 2011 at the Euryclides de Jesus Zerbini Hospital, São Paulo, Brazil. We assessed the patients who had undergone the bi-nostril approach with two-surgeon technique with a more than 1-year follow-up.
Surgical Technique
An endoscopic endosnasal bi-nostril approach using the two-surgeon and four-handed technique was employed in all cases. Preoperative evaluation of the sinonasal structures is mandatory and performed by multidetector computed tomography (CT) scan (Fig. 1). Under general anesthesia, patients were placed in the supine position with head tilted to the left, without pin-fixation, and with the dorsum elevated to 30 degrees. The surgeons positioned themselves to the right side of the patient’s chest to use the right nasal cavity as a pathway for an endoscope. Nasal mucosa in the surgical corridor including the superior turbinate was decongested with cottonoids containing epinephrine diluted 1:2,000. The middle turbinate was only compressed laterally, which enabled an approach to the sphenoethmoidal recess. After identification of the superior turbinate by advancing an endoscope over the middle turbinate, the sphenoid ostium was observed medial to the superior turbinate (Fig. 2). The inferior third portion of the superior turbinate on one side was coagulated by bipolar cautery and resected. This superior turbinectomy procedure exposed the posterior ethmoidal sinus in most cases (Fig. 3). The same procedure may be performed on the other side, if necessary. The sphenoid ostium was enlarged superolaterally with a mushroom punch and Kerrison rongeur, and the bony walls between the sphenoid and posterior ethmoid sinus were identified. Partial resection of the walls provided more lateral and superior exposure of the sphenoid sinus without opening the anterior ethmoid sinus, where the optic canal, carotid prominence, and opticocarotid recess were visible (Fig. 4). The sphenoid rostrum was resected at the level of the sphenoidal floor, followed by posterior septectomy. These procedures achieved a wide sphenoidotomy which allowed surgeons to identify the whole anatomical structures in the sphenoid sinus, including the lateral walls (Fig. 5). At this stage, the ENT surgeon started guiding the endoscope through the right nostril while the neurosurgeon bi-manually manipulated the instruments through both nostrils.
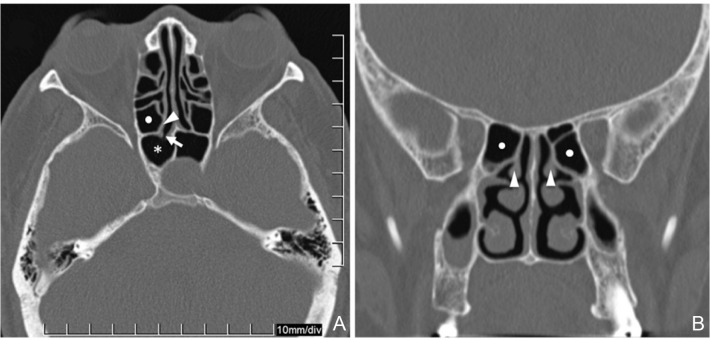
Fig. 1.
Bone window computed tomography images of patient with macroadenoma. An axial (A) and coronal (B) section clearly revealed the relationship of the landmarks of sinonasal anatomy. Arrow: ostium of the sphenoid sinus, arrowhead: superior turbinate asterisk: sphenoid sinus, white dot: posterior ethmoid cell.
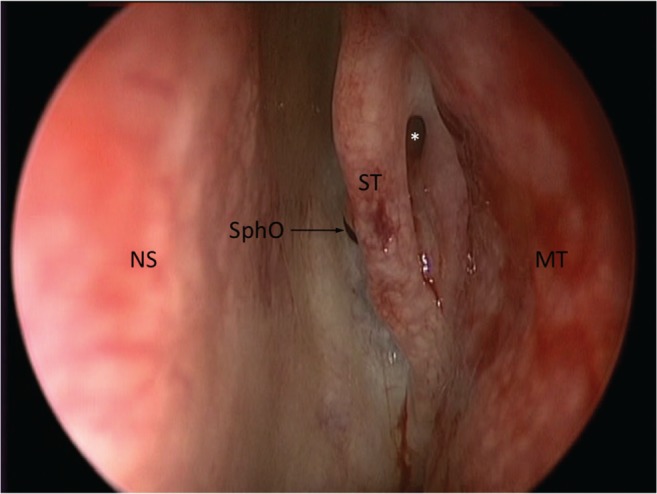
Fig. 2.
Intraoperative endoscopic view of left sphenoethmoidal recess. Sphenoid ostium (SphO) was located medial to the superior turbinate (ST). Asterisk: ostium of the posterior ethmoid sinus, MT: middle turbinate, NS: nasal septum.
Fig. 3.
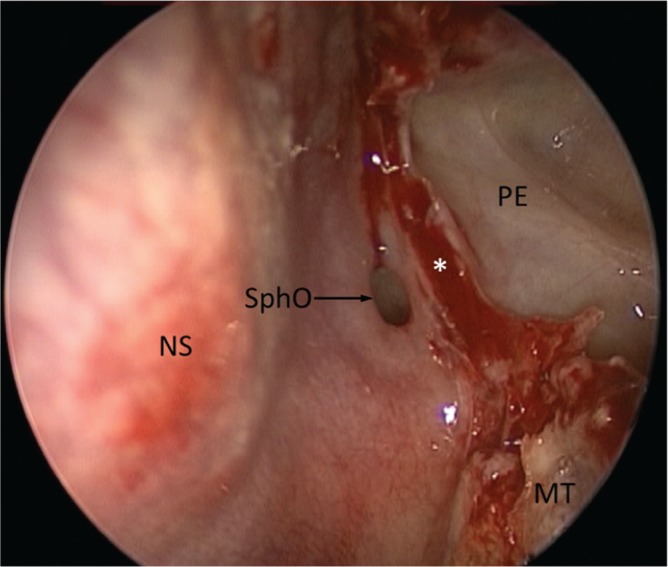
Magnified endoscopic view of left sphenoid ostium after resection of superior turbinate. The bony wall between posterior ethmoidal cell and sphenoid sinus was identified. Asterisk: stump of superior turbinate after resection, MT: middle turbinate, NS: nasal septum, SphO: ostium of the sphenoid sinus.
Fig. 4.
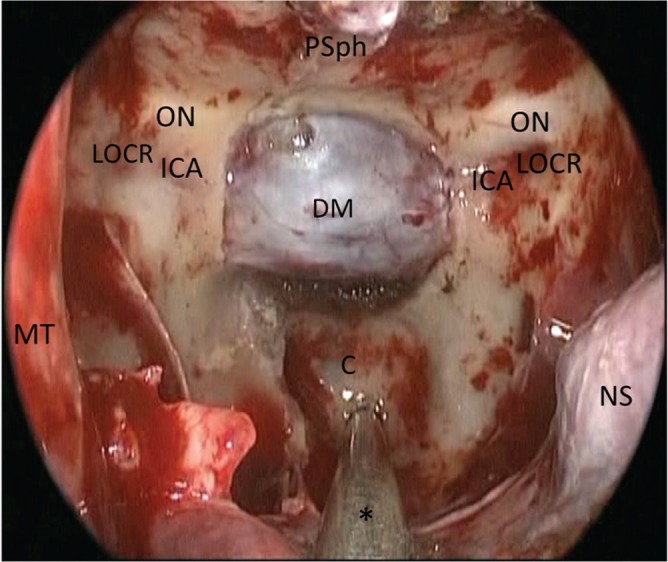
Final endoscopic view of posterior and lateral walls of the sphenoid sinus after wide sphenoidotomy. Tip of an endoscope was set in front of the right sphenoethmoidal recess. The floor of the sella turcica has been removed. The planum sphenoidale (PSph), optic canal or optic nerve (ON), carotid prominence or internal carotid artery (ICA), and lateral opticocarotid recess (LOCR) are visible bilaterally. Asterisk: suction tube, C: clivus, DM: dura mater, MT: middle turbinate, NS: nasal septum.
Fig. 5.
Postoperative three-dimensional (3D) computed tomography (CT) reconstruction bone image of sinonasal cavities in a patient who underwent partial superior turbinectomy and posterior ethmoidectomy on the right side. (A). The viewing direction was shown by a large arrow (B). The 3D image of the posterior ethmoidal area (light gray) was superimposed on that of the posterior sphenoidal wall (dark gray) in an anteroposterior direction. These images were obtained separately from multidetector CT volumetric data of region a (the posterior ethmoidal area) and region b (the posterior sphenoidal wall) (B). The areas encircled by dotted lines showed the most posterior ethmoid cells and their posterior walls were deleted deliberately on image reconstruction (A). The lateral structures in the sphenoid sinus including the opticocarotid recesses were difficult to be observed in a direction parallel with the nasal septum, and the superior turbinectomy with posterior ethmoidectomy provided a further superolateal view (small arrows) and an additional space for driving an endoscope. arrowhead: left superior turbinate, asterisk: lateral opticocarotid recess, C: clivus, CP: carotid prominence, S: sellar floor drilled away in surgery.
Results
Endoscopic endonasal surgeries with a two-surgeon technique were performed in 56 patients including 24 men and 32 women with a mean age of 47.1 years (range 14–85 years) over the period. Postoperative pathological examinations confirmed the diagnosis of pituitary adenomas in 49 patients, craniopharyngiomas in 4 patients, and chordoma, epidermoid cyst, and meningioma in 1 patient each, respectively. In all cases, the pathologies were mainly located in the midline regions. Although we had performed partial middle turbinectomy on one side (usually the right side) with superior turbinectomy in initial 3 patients with pituitary adenomas, we employed a lateralization of the middle turbinates and a partial superior turbinectomy in the last consecutive 53 patients. In these cases, an ENT surgeon was able to operate an endoscope along the space created by superior turbinectomy and bimanual meticulous manipulation of instruments was performed through both nostrils by a neurosurgeon. In 15 patients, in whom significant intraoperative cerebrospinal fluid (CSF) leak was observed, reconstruction of skull base defects with pedicled nasoseptal flap was performed. No patients presented with CSF leak after surgery. There were no complications related to the procedures of superior turbinectomy including postoperative nasal bleeding. All patients including those who had undergone reconstruction using pedicled nasoseptal flap did not complain of hyposmia or anosmia at 1-year follow-up, although no objective analysis was carried out.
Discussion
The role of superior and supreme turbinates had been overlooked even in the field of ESS, because surgeons had believed it was located superiorly outside the surgical field.1) Similarly, in standard transsphenoidal surgery via transseptal or transnasal approaches, these turbinates have received little attention and the superior turbinectomy has not yet been described in detail by previous reports, because the sphenoidotomy by enlarging the sphenoid ostia can be sufficient to approach the sella without caring about these structures. However, in the field of ESS, the role of the superior turbinate has recently been reevaluated.2)
In terms of sinonasal anatomy, the superior turbinate attaches superiorly to the skull base and posteriorly to the anterior wall of the sphenoid sinus.1,3,4) As the ostium of the sphenoid sinus is almost always located medial to the superior turbinate, it is a constant landmark to identify the sphenoid ostium.3–6) Meanwhile, the ostium of the posterior ethmoid sinus opens into the superior nasal meatus, lateral to the superior turbinate.7) Therefore, superior turbinectomy results in the opening of the antero-medial part of the posterior ethmoid sinus. Hence, the superior turbinate is also an important landmark for retrograde posterior ethmoidectomy through the superior meatus.2)
The posterior ethmoid sinus is located anteriorly, superiorly, and laterally to the sphenoid sinus, and the opening of the posterior ethmoid cells can create a sufficient space for driving an endoscope through the nostril more laterally and superiorly. Kitano and Taneda8) highlighted the possibility of submucosal posterior ethmoidectomy with resection of the superior turbinate in their extended transseptal transsphenoidal approach through sublabial incision using a microscope. In extended endoscopic endonasal surgery, a middle turbinectomy has been commonly recommended and highlighted as an additional procedure for creating a larger corridor more in previous reports.9,10) However, it is the superior turbinectomy followed by the posterior ethmoidectomy that provides not only a more superior and lateral view but also a superolateral space for positioning the tip of endoscope and for maneuvering the instruments. As outlined by Guthikonda et al.,11) the middle turbinectomy may not be necessary to approach the midline regions commonly accessed through the transsphenoidal route, although it may facilitate the exposure of the middle third of the clivus and more lateral regions such as the pterygopalatine fossa. Our experience suggests that the superior turbinectomy is an available and minimal invasive procedure to enlarge the surgical field more laterally. On the other hand, EETS may be adequately performed without superior turbinectomy if a patient has large nostrils, no deviation of the nasal septum, no hypertrophy of nasal turbinates, no anatomical variants, and a lesion located only in the midline. These conditions can be evaluated by preoperative CT scan.
Superior turbinectomy may pose several potential risks and disadvantages. First, there is a risk for hyposmia, which can occur because olfactory neuroepithelium is distributed along the superior portion of the medial surface of the superior turbinates, in addition to the cribriform plate.12) In the literature, it is controversial whether resection of the superior turbinate can cause olfactory dysfunction. In fact, there have been no reports describing the evidence of olfactory dysfunction due to partial superior turbinectomy in EETS. Eweiss et al.2) reported no olfactory change after ESS with resection of the inferior third portion of the superior turbinate. Say et al.13) described that 12% of the patients had a decrease in olfactory ability after ESS with resection of the inferior third portion of the superior turbinate, but their superior turbinate specimens did not contain olfactory marker protein-positive neuronal tissue. On the other hand, Lopes and Jankowski14) reported a rare case that developed unexplained anosmia after functional ethmoidectomy with resection of both superior turbinates, and they hypothesized that the superior turbinate may have a regulatory function in olfaction. In the present series, no patients complained of permanent olfactory dysfunction after surgery. This result suggests that partial superior turbinectomy itself might not significantly worsen olfactory function, at least at a clinically detectable level.12,15) An objective analysis of olfaction after this procedure will be an important future issue. Second, regarding risk of cerebrospinal fluid leakage, excessive resection of the superior turbinate can injure its attachment at the skull base. The lamina inserted in the skull base should be preserved. Third, the risk of injury to the optic nerve and/or internal carotid artery may occur when the Onodi cell, a posterior ethmoid cell located superolaterally to the sphenoid sinus, is present and the optic nerve and/or the internal carotid artery protrudes into this air cell.16) Fourth, the risk of hemorrhage from the main trunk of posterior ethmoidal artery may be low, as it runs in a bony canal, or the posterior ethmoidal canal, in the posterior ethmoidal roof, which may not be usually detected or manipulated during posterior ethmoidectomy. The resection of the inferior portion of the superior turbinate after bipolar coagulation without injury of the attachment can prevent the bleeding from both its main trunk and peripheral branches that supply the superior turbinate.17) The results of this study suggest the risk of these complications might be low, but surgeons should be aware of this issue and evaluate preoperative radiological examinations carefully.
Conclusion
In our experience of EETS with the two-surgeon and four-hand technique, the superior turbinate was a key anatomical landmark, and partial superior turbinectomy followed by opening of the posterior ethmoidal cell was sufficient to provide a wide surgical corridor for dissection of lesions in midline skull base, mainly involving pituitary adenomas. Although the approach has potential complications, these are rare and avoidable by careful manipulation of the sinonasal structures.
References
- 1). Orlandi RR, Lanza DC, Bolger WE, Clerico DM, Kennedy DW: The forgotten turbinate: the role of the superior turbinate in endoscopic sinus surgery. Am J Rhinol 13: 251– 259, 1999. [DOI] [PubMed] [Google Scholar]
- 2). Eweiss AZ, Ibrahim AA, Khalil HS: The safe gate to the posterior paranasal sinuses: reassessing the role of the superior turbinate. Eur Arch Otorhinolaryngol 269: 1451– 1456, 2012. [DOI] [PubMed] [Google Scholar]
- 3). Bolger WE, Keyes AS, Lanza DC: Use of the superior meatus and superior turbinate in the endoscopic approach to the sphenoid sinus. Otolaryngol Head Neck Surg 120: 308– 313, 1999. [DOI] [PubMed] [Google Scholar]
- 4). Har-El G, Swanson RM: The superior turbinectomy approach to isolated sphenoid sinus disease and to the sella turcica. Am J Rhinol 15: 149– 156, 2001. [DOI] [PubMed] [Google Scholar]
- 5). Millar DA, Orlandi RR: The sphenoid sinus natural ostium is consistently medial to the superior turbinate. Am J Rhinol 20: 180– 181, 2006. [PubMed] [Google Scholar]
- 6). Kim HU, Kim SS, Kang SS, Chung IH, Lee JG, Yoon JH: Surgical anatomy of the natural ostium of the sphenoid sinus. Laryngoscope 111: 1599– 1602, 2001. [DOI] [PubMed] [Google Scholar]
- 7). Yanagisawa E: Endoscopic view of sphenoethmoidal recess and superior meatus. Ear Nose Throat J 72: 331– 332, 1993. [PubMed] [Google Scholar]
- 8). Kitano M, Taneda M: Extended transsphenoidal approach with submucosal posterior ethmoidectomy for parasellar tumors. Technical note. J Neurosurg 94: 999– 1004, 2001. [DOI] [PubMed] [Google Scholar]
- 9). Carrau RL, Kassam AB, Snyderman CH: Pituitary surgery. Otolaryngol Clin North Am 34: 1143– 1155, ix, 2001. [DOI] [PubMed] [Google Scholar]
- 10). Cavallo LM, Messina A, Cappabianca P, Esposito F, de Divitiis E, Gardner P, Tschabitscher M: Endoscopic endonasal surgery of the midline skull base: anatomical study and clinical considerations. Neurosurg Focus 19: E2, 2005. [PubMed] [Google Scholar]
- 11). Guthikonda B, Nourbakhsh A, Notarianni C, Vannemreddy P, Nanda A: Middle turbinectomy for exposure in endoscopic endonasal transsphenoidal surgery: when is it necessary? Laryngoscope 120: 2360– 2366, 2010. [DOI] [PubMed] [Google Scholar]
- 12). Lane AP, Gomez G, Dankulich T, Wang H, Bolger WE, Rawson NE: The superior turbinate as a source of functional human olfactory receptor neurons. Laryngoscope 112: 1183– 1189, 2002. [DOI] [PubMed] [Google Scholar]
- 13). Say P, Leopold D, Cochran G, Smith L, Greiner T: Resection of the inferior superior turbinate: does it affect olfactory ability or contain olfactory neuronal tissue? Am J Rhinol 18: 157– 160, 2004. [PubMed] [Google Scholar]
- 14). Lopes G, Jankowski R: Anosmia following superior turbinate resection. Rev Laryngol Otol Rhinol (Bord) 125: 189– 191, 2004. [PubMed] [Google Scholar]
- 15). Hart CK, Theodosopoulos PV, Zimmer LA: Olfactory changes after endoscopic pituitary tumor resection. Otolaryngol Head Neck Surg 142: 95– 97, 2010. [DOI] [PubMed] [Google Scholar]
- 16). Unal B, Bademci G, Bilgili YK, Batay F, Avci E: Risky anatomic variations of sphenoid sinus for surgery. Surg Radiol Anat 28: 195– 201, 2006. [DOI] [PubMed] [Google Scholar]
- 17). Cankal F, Apaydin N, Acar HI, Elhan A, Tekdemir I, Yurdakul M, Kaya M, Esmer AF: Evaluation of the anterior and posterior ethmoidal canal by computed tomography. Clin Radiol 59: 1034– 1040, 2004. [DOI] [PubMed] [Google Scholar]