Abstract
Cervical laminoplasty was developed as an alternative to cervical laminectomy for treatment of cervical myelopathy, in which hinges are created to lift the lamina. Various techniques of laminoplasty have since been developed after two prototype techniques: Hirabayashi’s open-door laminoplasty and Kurokawa’s spinous process splitting (double-door) laminoplasty. Several in vitro studies report superior biomechanical stability of the cervical spine after laminoplasty compared with laminectomy. In clinical situation, randomized control studies are scarce and superiority of one procedure over another is not uniformly shown. Lack of hard evidence supporting the purported advantages of laminoplasty over laminectomy, that is, reduced rate of postoperative instability and kyphosis development, while preserving range of motion (ROM), has been a weak selling point. Currently, laminoplasty is performed by majority of spine surgeons in Japan, but is rarely performed in the United States and Europe. Recent development in laminoplasty is preservation of muscle attachment, which enabled dynamic stabilization of the cervical spine by neck extensor muscles. After treatment with new laminoplasty techniques with active postoperative neck ROM exercises, postoperative instability, kyphosis, axial neck pain, and loss of ROM seems minimal. Well-designed clinical trials to show the effectiveness and long-term outcome of this surgical procedure are warranted.
Keywords: cervical spine, spinal cord, myelopathy, radiculopathy, laminectomy
Definition
The term “laminoplasty” denotes several operative procedures in which vertebral lamina is reconstructed after opening the spinal canal. The word “laminoplasty” most commonly means creating hinge(s) on which the lamina is lifted but not removed.1–4) This review will focus on this type of laminoplasty, and will not discuss about “reconstructive laminoplasty,” which involves en bloc removal of the lamina with subsequent reattachment used mainly for pediatric intradural procedures,5,6) which others consider that it should be termed “laminotomy.”7,8)
History
Cervical laminoplasty was devised to avoid problems associated with laminectomy such as postoperative segmental instability, kyphosis, perineural adhesions, and late neurological deterioration.3) The first laminoplasty technique was the modification of Kirita’s technique for laminectomy, in which the laminae were thinned and then partially removed in the midline using an air drill. The lateral edges of the laminae close to the pedicles were further thinned until the laminae could be bent and lifted up. It was considered important to lift multiple laminae expeditiously so that multiple segments of the cord could be simultaneously decompressed. The laminae were then removed with scissors.9) Based on this technique, Oyama et al. developed z-plasty method of laminoplasty.1) After thinning the laminae, z-shaped cuts were made in each laminae, which were lifted and then fixed with sutures to reconstruct the expanded spinal canal (Fig. 1). They reported that all the 15 cases were neurologically improved after the operation.
Fig. 1.
Schematic drawing showing the posterior aspect of the cervical spine and z-laminoplasty. a: Laminae of C2 to C7 are exposed after subperiosteal dissection. b: The laminae are thinned with drill and z-shaped cuts are made in each laminae. c: The split laminae are lifted from the spinal canal and fixed with sutures, reconstructing the expanded spinal canal.
Tsuji reported a variation of en bloc laminectomy in which laminae were cut bilaterally along the imaginary line separating laminar arches and articular processes and made completely free from their bony attachments. The lamiae were reflected as a flap and then permitted to float on the cord without fixing sutures or bone grafting.2) Based on this technique, Hirabayashi et al. reported expansive open-door laminoplasty.3) In this procedure, bony gutters are drilled bilaterally at the border of laminae corresponding to the medial portion of the pedicles. The lamina border on one side is excised, and then the laminae are pushed laterally towards the other side as if to open a door, so that the spinal canal is enlarged. The yellow ligaments and deep muscles around the facets of the hinge side are supported by sutures to prevent the laminar door from being closed (Fig. 2). Kurokawa et al. developed spinous process splitting laminoplasty,4) in which the spinous processes and laminae are split in the midline and hinges are made bilaterally along the lateral borders of the laminae, which are lifted bilaterally. This is also called double-door laminoplasty,10) French-window,11) or French-door laminoplasty12) (Fig. 3).
Fig. 2.
Schematic drawing depicting the procedure for Hirabayshi’s open-door laminoplasty. a: Bony gutters are drilled bilaterally at the lateral borders of laminae, on one side completely removing the bone and on the other side thinned inner cortex is preserved as a hinge. b: The laminae are lifted on the hinges to expand the spinal canal.
Fig. 3.
Schematic drawing showing Kurokawa’s double-door laminoplasty. a: Spinous processes and underlying laminae are drilled, making a midline cut. The lateral borders of laminae are drilled leaving thin inner cortex to make hinge gutters. b: The laminae are lifted on the hinges bilaterally.
There are many reports of “new method” of laminoplasty in the literature, but the basic technique to expand the spinal canal falls into either Hirabayashi’s open-door technique with a hinge on one side or Kurokawa’s double-door technique with hinges on both sides. Many modifications were also developed to keep the expanded lamina from being closed, for example by using sutures,3,11) autologous bone grafts,4,13) hydroxyapatite or other ceramic materials,14,15) titanium miniplates16) or spacers,17) allograft and titanium plates,18) and hydroxyapatite and screws.19)
It had been noted that detachment of posterior cervical muscles, especially the semispinalis cervicis muscle on the C2 spinous process, was associated with the development of postoperative kyphosis20) and axial neck pain.21–23) Detachment of semispinalis cervicis from the C2 spinous process followed by reattachment was advocated by some authors,24,25) but it was later found that the results of preservation of the attachment was superior to repairing.20,22,26) Preservation of muscle attachments on C7 spinous processes was also noted to be important to prevent axial neck pain.27,28) Awareness of importance of functional cervical muscles prompted development of various techniques to preserve muscle attachment on the spinous processes. In one of such techniques, the spinous processes and the laminae were exposed by subperiosteal dissection on one side, and then the spinous processes were cut off from the laminae and retracted to the contralateral side to expose the lamina bilaterally. It was possible to preserve attachment of the semispinalis muscles on the spinous processes on one side.29–33) A prospective randomized study found this technique to result in significantly decreased axial pain compared with open-door laminoplasty in which muscle attachments were completely dissected.34)
Up to this development, reconstruction was limited to that of the bony structures, and muscles responsible for maintenance of static and dynamic motor functions basically were not preserved.
A meta-analysis study has found that there was no significant difference in clinical improvement between open-door and double-door laminoplasty techniques.35) Multiple systematic reviews of literature showed that clinical improvement of cervical myelopathy and/or radiculopathy after cervical laminoplasty was essentially the same as those after laminectomy with or without fusion or anterior cervical discectomy or corpectomy with fusion.36–40) But the purported advantage of laminoplasty, that is, reduced instability and preventing kyphosis as well as preserving range of motion (ROM), could not be verified due to lack of high-quality evidence.
In 2002, Shiraishi reported a technique for exposure of cervical spine laminae that preserved the attachments of semispinalis cervicis and multifidus muscles on the cervical spinous processes and limiting the damage to the attachments of interspinous and rotator muscles41) (Fig. 4). He showed that it was possible to perform interlaminar decompression, intervertebral foraminotomy, hemilaminectomy, and double-door laminoplasty. Kim et al. developed myoarchitectonic spinolaminoplasty, in which the spinous processes are cut in the midline and then cut off from the laminae without severing the muscular attachments and then the laminae are exposed, without damaging the attachments of the semispinalis cervicis, multifidus, interspinalis, and rotator muscles42) (Fig. 5). Development of the technique perfected reconstruction and preservation of the entire musculoskeletal elements in the posterior neck. It became possible to expand the spinal canal effectively while preserving the attachments of semispinalis cervicis, multifidus, semispinalis capitis, and reconstructing the stress-bearing midline fascia of the splenius cervicis and trapezius. They showed that after myoarchitectonic spinolaminoplasty, neurosurgical cervical spine scale score improved from 10.7 to 13.4 with an improvement rate of 87.3%. Deep extensor muscles did not become atrophic, postoperative loss of lordosis was less than 1°, the ROM of C2–C7 angle 1 year after surgery was 67.7% of preoperative value, and the incidence of axial neck pain was 2.36%. This development seems to overcome the weakness of posterior decompression procedures in preventing postoperative instability and preserving ROM, which was previously pointed out in systematic review.36) Further clinical study comparing the results of laminoplasty with that of laminectomy or anterior decompression is warranted.
Fig. 4.
Schematic drawing showing Shiraishi’s techniques for posterior exposure of the cervical spine while preserving semispinalis muscle attachments. a: A midline gap between the interspinalis muscles is opened with retractors to expose the interlaminar space. b: By severing the attachments of the interspinalis muscles, the cephalad aspect of the spinous process and parts of lamina and rotator muscles can be exposed.
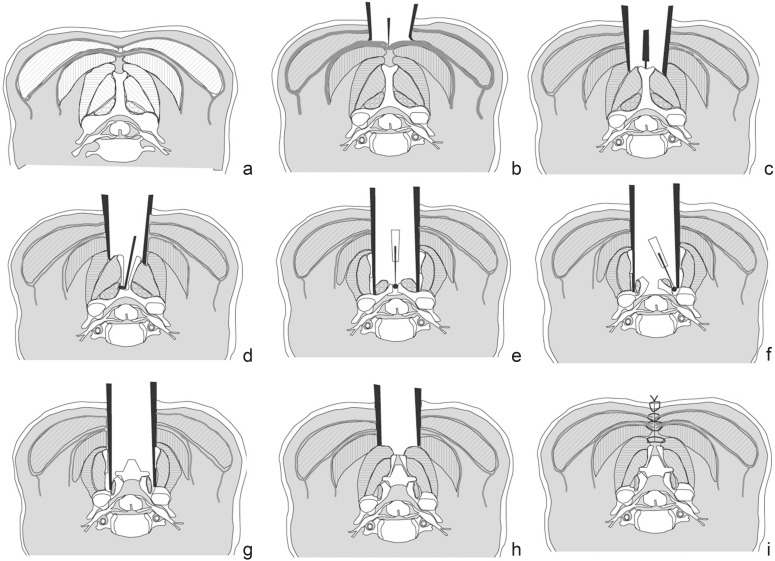
Fig. 5.
Schematic drawing depicting Kim’s myoarchitectonic spinolaminoplasty, in which attachments of all posterior muscles are preserved while expanding the spinal canal. Cross section of the cervical spine and layers of nuchal muscles: the trapezius in the 1st layer, the splenius in the 2nd layer, and the semispinalis capitis in the 3rd layer of the nuchal ligament. a: Semispinalis cervicis and multifidus are attached to the sides of the spinous process. b: The fascia in the midline of the trapezius is sharply cut. c: The midline fascia of the splenius is sharply divided and the tip of the spinous process is proved. d: The spinous process is split in the midline with a sagittal saw, and through this opening the spinous process is cut off from the lamina. e: The spinous process is retracted laterally with the semispinalis cervicis attachment intact. The lamina is drilled in the midline. f: Hinge gutters are made at the border between the lamina and the lateral mass, preserving the attachment of the multifidus. g: The laminal flaps are elevated on the hinges and are inter-bridged using a hydroxyapatite implant. h: The split halves of the spinous process with the attached semispinalis cervicis is attached to the hydroxyapatite implant. i: The Three layers of the nuchal ligament is firmly reconstructed in the midline.
Indication for Laminoplasty
Laminoplasty is most effective in decompressing the spinal cord when lordosis of the cervical spine is maintained as with any methods of dorsal approach decompression.43) It is, therefore, indicated in patients with cervical spinal canal stenosis under 12 mm of the anterior-posterior diameter of the spinal canal, continuous type of ossification of posterior longitudinal ligaments (OPLL), and multiple spondylotic lesions over three or four intervertebral spaces, in lordotic cervical spine.3,44) However, laminoplasty improves myelopathy even in the presence of kyphosis45) and is indicated for patients with cervical kyphosis if more than three levels needs to be decompressed, because anterior decompression and fusion spanning over three levels is associated with higher incidence of complications related to graft and fixation.46–49) Clinical improvement after laminoplasty may be unsatisfactory if the focal kyphosis angle is larger than 13°43) or if the thickness of ossification of posterior longitudinal ligament exceeds the line that connects the midpoints of the spinal canal at C2 and C7 (K-line).50) In such cases, anterior decompression with fusion may be performed at the most compressed segment after laminoplasty.3,51)
Postoperative Outcome
In most published studies, clinical status of cervical myelopathy is assessed using Nurick grade,52) Japanese Orthopedic Association (JOA) scale,53) or Neurosurgical Cervical Spine Scale (NCSS)54) (Table 1). The recovery rate (%) is calculated as 100 × [(JOA scale score at follow-up – JOA scale score before surgery) ÷ (17 – JOA scale score before surgery)]. In the earliest report by Hirabayashi, of 40 patients undergoing open-door laminoplasty, most of the patients had good results, with a recovery rate of 66% in JOA scale score. Others reported similar results on neurological recovery after various techniques of laminoplasty, the improvement being stable for more than 10 years in most patients.10,55–58) In neurosurgical literatures, NCSS is often employed to describe the status because of its simplicity and clarity.42,54)
Table 1.
Various scales used for neurological assessment of patients with cervical myelopathy
|
MMT: manual muscle testing.
ROM
In early reports, patients were kept in bed for 1 week to 3 months after laminoplasty and then allowed to ambulate with a cervical brace for 3–6 months.3,4,59) The follow-up studies in the early case series reported decrease in the ROM to 53% at 1 year after surgery and to 35% at average of 7 years after surgery.60–62) The decrease was especially prominent among patients with OPLL, decreasing from 36° to 8° at a mean follow-up of 153 months.10) One study revealed that the decrease in ROM was correlated significantly with the decrease in cervical lordosis.59) In modern practice, patients are allowed to sit up and walk on the first postoperative day while wearing a Philadelphia collar for 2 weeks30,63) or no orthosis at all.42) In a large series of 520 patients who were instructed to perform cervical ROM exercises starting on the after the laminoplasty operation, the ROM decreased from 40.1° to 33.5° (87.9%) at an average follow-up period of 33.3 months.63) In a series of patients undergoing myoarchitectonic spinolaminoplasty, the ROM was 67.7% of preoperative value 1 year after operation.42) There is no controlled study that shows the effect of different postoperative cervical immobilization programs on the long-term results of cervical ROM, but it seems that shorter bed rest and cervical orthosis and early neck ROM exercises results in less restriction of ROM in the long term.
Kyphosis Development
Early report of series of patients undergoing cervical laminoplasty with up to 2 years follow-up reported that no patients developed kyphosis.3,13,46,64) However, others found kyphosis development in 28% of patients 5 years after laminoplasty, the incidence being similar to laminectomy.11) In a series of patients who were instructed to perform ROM exercises after surgery, kyphosis developed in 33 (7.2%) out of 457 patients whose cervical spine was lordotic before surgery, at average follow-up period of 33.3 months. In the same series, 31 (49.2%) of 63 patients whose cervical spine was kyphotic before surgery showed lordosis after surgery.63) In patients who underwent myoarchitectonic spinolaminoplasty, the loss of lordosis in the C2–C7 angle was 0.71° at 1 year after surgery.42)
Holmes et al. showed in a cadaver study that the volume of spinal canal space was correlated with C2–C7 angle and the volume capacity decreased with increasing extension angle, and it was greatest at full flexion.65) Cervical kyphosis may be a result of body’s protective reaction to increase the spinal canal volume when the spinal cord is under compression. By expanding the spinal canal inherent lordosis may be restored, if the posterior musculature is functionally preserved.
The mechanical force that maintains cervical lordosis is exerted by extensor muscles, especially the semispinalis cervicis and capitis.66) Repairing of semispinalis cervicis attachment on C2 spinous process by sutures resulted in dehiscence of the muscle attachment and loss of lordosis in 18% of patients after laminoplasty.20) It is important to preserve the ability of the muscles to apply force to the cervical vertebra in physiological orientation to maintain lordosis. It is not surprising to find that the method in which all the posterior muscle attachment is preserved (myoarchitectonic spinolaminoplasty) resulted in the least loss of lordosis.42)
Biomechanical Studies
In vitro biomechanical studies using cadavers revealed that range of movement in response to physiologic load became larger after laminectomy with 25% facetectomy 67) or without foraminotomy,68,69) but was not significantly different from intact spine after open-door laminoplasty. Double-door laminoplasty also results in more stable cervical spine than laminectomy.70) However, load to failure was significantly smaller in spines after laminoplasty than intact spine.71) Importance of nuchal ligament in resisting flexion moment was noted by other investigator.72) The importance of extensor muscles of the cervical spine was also noted, especially those attached to the occiput and spinous processes of C2 and C7.66)
Animal studies showed that kyphotic deformity developed after laminectomy in goats73) and rabbits,74) but not after laminoplasty.
Clinical comparative studies reveal contradictory results, some showing no difference between laminectomy and laminoplasty,11,64,75) some showing comparable neurological outcome with more complications in laminoplasty than laminectomy,38,39) and others showing better improvement with laminoplasty than laminectomy.76,77) The reason for lack of consistent difference between laminectomy and laminoplasty may be that laminoplasty procedures in these studies did not preserve or reconstruct muscle attachments. Reconstructing laminar arches without muscle insertion would not be so different from removing laminar arches in terms of forces exerted onto the cervical vertebrae.
Issues for Future Studies
Surgical techniques for treatment of cervical myelopathy caused by spondylosis or OPLL include anterior cervical discectomy with fusion, anterior cervical corpectomy with fusion, laminectomy, laminectomy with fusion, and laminoplasty.78) Cervical laminoplasty is by far the most commonly performed surgery for compressive cervical myelopathy in Japan,58,79) but it is not performed by majority of spine surgeons in the United States and Europe.80–82)
The theoretical advantage of laminoplasty is that it can preserve stability of the cervical spine preventing postoperative kyphosis which can be seen after laminoplasty, and at the same time, it can preserve motion preventing adjacent segment diseases observed as late sequelae after anterior or posterior fusion surgery. For laminoplasty to be an ideal option to classic laminectomy and anterior decompression and fusion, it must prove to be better than laminectomy in preventing instability and kyphosis, and better than anterior fusion in preserving cervical ROM. Early laminoplasty technique did not preserve dynamic stabilizing effect of extensor muscles and failed to show the stability of the cervical spine superior to laminectomy. Postoperative care in early clinical series required long periods of bed rest and cervical orthosis immobilization and resulted in loss of ROM similar to anterior fusion. Critical literature review found laminoplasty to be as unstable as laminectomy and at the same time as immobilizing as fusion surgery.36) Laminoplasty as practiced today, with myoarchitectonic techniques and early postoperative mobilization, may be able to show better stability than laminectomy and better preserved ROM than anterior fusion.
The literature lacks randomized control study comparing laminectomy and laminoplasty, laminectomy with fusion and laminoplasty, or anterior corpectomy with fusion and laminoplasty. There is one randomized control study comparing laminectomy with fusion and laminoplasty and showed similar neurological improvement and preservation of ROM to be better in laminoplasty, but the number of patients were small, with seven patients undergoing laminectomy with fusion and nine patients undergoing laminoplasty.81) Many studies are conducted as comparison between different methods of laminoplasty34,42,83) or lack a control group.58) The modern methods of laminoplasty are better than early laminoplasty practices in preserving motion and stability. Its advantages should be scientifically shown in well-coordinated randomized control trial comparing with other surgical techniques that can stand the test of the world.
References
- 1). Oyama M, Hattori S, Moriwaki N, Nitta S: [A new method of cervical laminectomy]. Chuubu Nippon Seikeigeka Gakkai Zasshi 16: 792– 794, 1973. (Japanese) [Google Scholar]
- 2). Tsuji H: Laminoplasty for patients with compressive myelopathy due to so-called spinal canal stenosis in cervical and thoracic regions. Spine 7: 28– 34, 1982 [DOI] [PubMed] [Google Scholar]
- 3). Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y: Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine 8: 693– 699, 1983 [DOI] [PubMed] [Google Scholar]
- 4). Kurokawa T, Tsuyama N, Tanaka H, Kobayashi M, Machida H, Nakamura K, Iizuka T, Hoshino Y: [Enlargement of spinal canal by the sagittal splitting of spinous processes]. Bessatsu Seikeigeka 2: 234– 240, 1982. (Japanese) [Google Scholar]
- 5). Cobb MA, Boop FA: Replacement laminoplasty in selective dorsal rhizotomy: possible protection against the development of musculoskeletal pain. Pediatr Neurosurg 21: 237– 242, 1994 [DOI] [PubMed] [Google Scholar]
- 6). McGirt MJ, Garcés-Ambrossi GL, Parker SL, Sciubba DM, Bydon A, Wolinksy JP, Gokaslan ZL, Jallo G, Witham TF: Short-term progressive spinal deformity following laminoplasty versus laminectomy for resection of intradural spinal tumors: analysis of 238 patients. Neurosurgery 66: 1005– 1012, 2010 [DOI] [PubMed] [Google Scholar]
- 7). Raimondi AJ, Gutierrez FA, Di Rocco C: Laminotomy and total reconstruction of the posterior spinal arch for spinal canal surgery in childhood. J Neurosurg 45: 555– 560, 1976 [DOI] [PubMed] [Google Scholar]
- 8). Yucesoy K, Sonntag VK: Terminology confusion in spinal surgery: laminotomy, laminoplasty, laminectomy. J Neurosurg 92: 371, 2000 [DOI] [PubMed] [Google Scholar]
- 9). Kirita Y, Miyazaki K, Hayashi T, Nosaka K, Shima M, Yamamura H, Tamaki S: [Ossification of posterior longitudinal ligament of the cervical spine]. Rinsho Seikeigeka 10: 1077– 1085, 1975. (Japanese) [Google Scholar]
- 10). Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, Kitagawa T, Nakamura K: Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine 26: 479– 487, 2001 [DOI] [PubMed] [Google Scholar]
- 11). Hukuda S, Ogata M, Mochizuki T, Shichikawa K: Laminectomy versus laminoplasty for cervical myelopathy: brief report. J Bone Joint Surg Br 70: 325– 326, 1988 [DOI] [PubMed] [Google Scholar]
- 12). Nakama S, Nitanai K, Oohashi Y, Endo T, Hoshino Y: Cervical muscle strength after laminoplasty. J Orthop Sci 8: 36– 40, 2003 [DOI] [PubMed] [Google Scholar]
- 13). Itoh T, Tsuji H: Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. Spine 10: 729– 736, 1985 [DOI] [PubMed] [Google Scholar]
- 14). Hase H, Watanabe T, Hirasawa Y, Hashimoto H, Miyamoto T, Chatani K, Kageyama N, Mikami Y: Bilateral open laminoplasty using ceramic laminas for cervical myelopathy. Spine 16: 1269– 1276, 1991 [DOI] [PubMed] [Google Scholar]
- 15). Tomita K, Kawahara N, Toribatake Y, Heller JG: Expansive midline T-saw laminoplasty (modified spinous process-splitting) for the management of cervical myelopathy. Spine 23: 32– 37, 1998 [DOI] [PubMed] [Google Scholar]
- 16). O’Brien MF, Peterson D, Casey AT, Crockard HA: A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization. A computerized morphometric analysis. Spine 21: 474– 483; discussion 484, 1996 [DOI] [PubMed] [Google Scholar]
- 17). Tani S, Suetsua F, Mizuno J, Uchikado H, Nagashima H, Akiyama M, Isoshima A, Ohashi H, Hirano Y, Abe T: New titanium spacer for cervical laminoplasty: initial clinical experience. Technical note. Neurol Med Chir 50: 1132– 1136, 2010 [DOI] [PubMed] [Google Scholar]
- 18). Shaffrey CI, Wiggins GC, Piccirilli CB, Young JN, Lovell LR: Modified open-door laminoplasty for treatment of neurological deficits in younger patients with congenital spinal stenosis: analysis of clinical and radiographic data. J Neurosurg 90( 2 Suppl): 170– 177, 1999 [DOI] [PubMed] [Google Scholar]
- 19). Takayasu M, Takagi T, Nishizawa T, Osuka K, Nakajima T, Yoshida J: Bilateral open-door cervical expansive laminoplasty with hydroxyapatite spacers and titanium screws. J Neurosurg 96: 22– 28, 2002 [DOI] [PubMed] [Google Scholar]
- 20). Iizuka H, Shimizu T, Tateno K, Toda N, Edakuni H, Shimada H, Takagishi K: Extensor musculature of the cervical spine after laminoplasty: morphologic evaluation by coronal view of the magnetic resonance image. Spine 26: 2220– 2226, 2001 [DOI] [PubMed] [Google Scholar]
- 21). Sasai K, Saito T, Akagi S, Kato I, Ogawa R: Cervical curvature after laminoplasty for spondylotic myelopathy—involvement of yellow ligament, semispinalis cervicis muscle, and nuchal ligament. J Spinal Disord 13: 26– 30, 2000 [DOI] [PubMed] [Google Scholar]
- 22). Takeuchi K, Yokoyama T, Aburakawa S, Saito A, Numasawa T, Iwasaki T, Itabashi T, Okada A, Ito J, Ueyama K, Toh S: Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3–C7 laminoplasty: a modified laminoplasty preserving the semispinalis cervicis inserted into axis. Spine 30: 2544– 2549, 2005 [DOI] [PubMed] [Google Scholar]
- 23). Kato M, Nakamura H, Konishi S, Dohzono S, Toyoda H, Fukushima W, Kondo K, Matsuda H: Effect of preserving paraspinal muscles on postoperative axial pain in the selective cervical laminoplasty. Spine 33: E455– E459, 2008 [DOI] [PubMed] [Google Scholar]
- 24). Matsuzaki H, Hoshino M, Kiuchi T, Toriyama S: Dome-like expansive laminoplasty for the second cervical vertebra. Spine 14: 1198– 1203, 1989 [DOI] [PubMed] [Google Scholar]
- 25). Takeuchi K, Yokoyama T, Aburakawa S, Itabashi T, Toh S: Anatomic study of the semispinalis cervicis for reattachment during laminoplasty. Clin Orthop Relat Res 126– 131, 2005. [DOI] [PubMed] [Google Scholar]
- 26). Iizuka H, Nakajima T, Iizuka Y, Sorimachi Y, Ara T, Nishinome M, Takagishi K: Cervical malalignment after laminoplasty: relationship to deep extensor musculature of the cervical spine and neurological outcome. J Neurosurg Spine 7: 610– 614, 2007 [DOI] [PubMed] [Google Scholar]
- 27). Hosono N, Sakaura H, Mukai Y, Yoshikawa H: The source of axial pain after cervical laminoplasty-C7 is more crucial than deep extensor muscles. Spine 32: 2985– 2988, 2007 [DOI] [PubMed] [Google Scholar]
- 28). Takeuchi T, Shono Y: Importance of preserving the C7 spinous process and attached nuchal ligament in French-door laminoplasty to reduce postoperative axial symptoms. Eur Spine J 16: 1417– 1422, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29). Roselli R, Pompucci A, Formica F, Restuccia D, Di Lazzaro V, Valeriani M, Scerrati M: Open-door laminoplasty for cervical stenotic myelopathy: surgical technique and neurophysiological monitoring. J Neurosurg 92: 38– 43, 2000 [DOI] [PubMed] [Google Scholar]
- 30). Tani S, Isoshima A, Nagashima Y, Tomohiko Numoto R, Abe T: Laminoplasty with preservation of posterior cervical elements: surgical technique. Neurosurgery 50: 97– 101; discussion 101–102, 2002 [DOI] [PubMed] [Google Scholar]
- 31). Yoshida M, Tamaki T, Kawakami M, Nakatani N, Ando M, Yamada H, Hayashi N: Does reconstruction of posterior ligamentous complex with extensor musculature decrease axial symptoms after cervical laminoplasty? Spine 27: 1414– 1418, 2002. [DOI] [PubMed] [Google Scholar]
- 32). Hosono N, Sakaura H, Mukai Y, Ishii T, Yoshikawa H: En bloc laminoplasty without dissection of paraspinal muscles. J Neurosurg Spine 3: 29– 33, 2005 [DOI] [PubMed] [Google Scholar]
- 33). Liu J, Ebraheim NA, Sanford CG, Patil V, Haman SP, Ren L, Yang H: Preservation of the spinous process-ligament-muscle complex to prevent kyphotic deformity following laminoplasty. Spine J 7: 159– 164, 2007 [DOI] [PubMed] [Google Scholar]
- 34). Okada M, Minamide A, Endo T, Yoshida M, Kawakami M, Ando M, Hashizume H, Nakagawa Y, Maio K: A prospective randomized study of clinical outcomes in patients with cervical compressive myelopathy treated with open-door or French-door laminoplasty. Spine 34: 1119– 1126, 2009 [DOI] [PubMed] [Google Scholar]
- 35). Heller JG, Raich AL, Dettori JR, Riew KD: Comparative effectiveness of different types of cervical laminoplasty. Evid Based Spine Care J 4: 105– 115, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36). Ratliff JK, Cooper PR: Cervical laminoplasty: a critical review. J Neurosurg 98: 230– 238, 2003 [DOI] [PubMed] [Google Scholar]
- 37). Matz PG, Anderson PA, Groff MW, Heary RF, Holly LT, Kaiser MG, Mummaneni PV, Ryken TC, Choudhri TF, Vresilovic EJ, Resnick DK, Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and Congress of Neurological Surgeons : Cervical laminoplasty for the treatment of cervical degenerative myelopathy. J Neurosurg Spine 11: 157– 169, 2009 [DOI] [PubMed] [Google Scholar]
- 38). Nurboja B, Kachramanoglou C, Choi D: Cervical laminectomy vs laminoplasty: is there a difference in outcome and postoperative pain? Neurosurgery 70: 965– 970; discussion 970, 2012 [DOI] [PubMed] [Google Scholar]
- 39). Bartels RH, van Tulder MW, Moojen WA, Arts MP, Peul WC: Laminoplasty and laminectomy for cervical sponydylotic myelopathy: a systematic review. Eur Spine J 2013. [Epub ahead of print] [DOI] [PubMed]
- 40). Yoon ST, Hashimoto RE, Raich A, Shaffrey CI, Rhee JM, Riew KD: Outcomes after laminoplasty compared with laminectomy and fusion in patients with cervical myelopathy: a systematic review. Spine 38: S183– S194, 2013 [DOI] [PubMed] [Google Scholar]
- 41). Shiraishi T: A new technique for exposure of the cervical spine laminae. Technical note. J Neurosurg 96: 122– 126, 2002 [DOI] [PubMed] [Google Scholar]
- 42). Kim P, Murata H, Kurokawa R, Takaishi Y, Asakuno K, Kawamoto T: Myoarchitectonic spinolaminoplasty: efficacy in reconstituting the cervical musculature and preserving biomechanical function. J Neurosurg Spine 7: 293– 304, 2007 [DOI] [PubMed] [Google Scholar]
- 43). Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M: Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine 28: 1258– 1262, 2003 [DOI] [PubMed] [Google Scholar]
- 44). Naderi S, Benzel EC, Baldwin NG: Cervical spondylotic myelopathy: surgical decision making. Neurosurg Focus 1: e1, 1996 [DOI] [PubMed] [Google Scholar]
- 45). Kim SW, Hai DM, Sundaram S, Kim YC, Park MS, Paik SH, Kwak YH, Kim TH: Is cervical lordosis relevant in laminoplasty? Spine J 13: 914– 921, 2013. [DOI] [PubMed] [Google Scholar]
- 46). Herkowitz HN: Cervical laminaplasty: its role in the treatment of cervical radiculopathy. J Spinal Disord 1: 179– 188, 1988 [PubMed] [Google Scholar]
- 47). Yonenobu K, Hosono N, Iwasaki M, Asano M, Ono K: Laminoplasty versus subtotal corpectomy. A comparative study of results in multisegmental cervical spondylotic myelopathy. Spine 17: 1281– 1284, 1992 [PubMed] [Google Scholar]
- 48). Edwards CC, Heller JG, Murakami H: Corpectomy versus laminoplasty for multilevel cervical myelopathy: an independent matched-cohort analysis. Spine 27: 1168– 1175, 2002 [DOI] [PubMed] [Google Scholar]
- 49). Cunningham MR, Hershman S, Bendo J: Systematic review of cohort studies comparing surgical treatments for cervical spondylotic myelopathy. Spine 35: 537– 543, 2010 [DOI] [PubMed] [Google Scholar]
- 50). Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda M, Okawa A, Takahashi K, Konishi H: A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine 33: E990– E993, 2008 [DOI] [PubMed] [Google Scholar]
- 51). Kawaguchi Y, Nakano M, Yasuda T, Seki S, Hori T, Kimura T: Anterior decompressive surgery after cervical laminoplasty in patients with ossification of the posterior longitudinal ligament. Spine J 14: 955– 963, 2014 [DOI] [PubMed] [Google Scholar]
- 52). Nurick S: The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain 95: 87– 100, 1972 [DOI] [PubMed] [Google Scholar]
- 53). Japanese Orthopedic Association Scoring system for cervical myelopathy. Nippon Seikeigeka Gakkai Zasshi 68: 490– 503, 1994. [Google Scholar]
- 54). Kadoya S: Grading and scoring system for neurological function in degenerative cervical spine disease—Neurosurgical Cervical Spine Scale. Neurol Med Chir (Tokyo) 32: 40– 41, 1992 [DOI] [PubMed] [Google Scholar]
- 55). Satomi K, Ogawa J, Ishii Y, Hirabayashi K: Short-term complications and long-term results of expansive open-door laminoplasty for cervical stenotic myelopathy. Spine J 1: 26– 30, 2001 [DOI] [PubMed] [Google Scholar]
- 56). Chiba K, Ogawa Y, Ishii K, Takaishi H, Nakamura M, Maruiwa H, Matsumoto M, Toyama Y: Long-term results of expansive open-door laminoplasty for cervical myelopathy—average 14-year follow-up study. Spine 31: 2998– 3005, 2006 [DOI] [PubMed] [Google Scholar]
- 57). Kimura A, Seichi A, Inoue H, Hoshino Y: Long-term results of double-door laminoplasty using hydroxyapatite spacers in patients with compressive cervical myelopathy. Eur Spine J 20: 1560– 1566, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58). Machino M, Yukawa Y, Hida T, Ito K, Nakashima H, Kanbara S, Morita D, Kato F: Modified double-door laminoplasty in managing multilevel cervical spondylotic myelopathy: surgical outcome in 520 patients and technique description. J Spinal Disord Tech 26: 135– 140, 2013 [DOI] [PubMed] [Google Scholar]
- 59). Maeda T, Arizono T, Saito T, Iwamoto Y: Cervical alignment, range of motion, and instability after cervical laminoplasty. Clin Orthop Relat Res 132– 138, 2002. [DOI] [PubMed] [Google Scholar]
- 60). Hirabayashi K, Satomi K: Operative procedure and results of expansive open-door laminoplasty. Spine 13: 870– 876, 1988 [DOI] [PubMed] [Google Scholar]
- 61). Satomi K, Nishu Y, Kohno T, Hirabayashi K: Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine 19: 507– 510, 1994 [DOI] [PubMed] [Google Scholar]
- 62). Hyun SJ, Rhim SC, Roh SW, Kang SH, Riew KD: The time course of range of motion loss after cervical laminoplasty: a prospective study with minimum two-year follow-up. Spine 34: 1134– 1139, 2009 [DOI] [PubMed] [Google Scholar]
- 63). Machino M, Yukawa Y, Hida T, Ito K, Nakashima H, Kanbara S, Morita D, Kato F: Cervical alignment and range of motion after laminoplasty: radiographical data from more than 500 cases with cervical spondylotic myelopathy and a review of the literature. Spine 37: E1243– E1250, 2012 [DOI] [PubMed] [Google Scholar]
- 64). Nakano N, Nakano T, Nakano K: Comparison of the results of laminectomy and open-door laminoplasty for cervical spondylotic myeloradiculopathy and ossification of the posterior longitudinal ligament. Spine 13: 792– 794, 1988 [DOI] [PubMed] [Google Scholar]
- 65). Holmes A, Han ZH, Dang GT, Chen ZQ, Wang ZG, Fang J: Changes in cervical canal spinal volume during in vitro flexion-extension. Spine 21: 1313– 1319, 1996 [DOI] [PubMed] [Google Scholar]
- 66). Nolan JP, Sherk HH: Biomechanical evaluation of the extensor musculature of the cervical spine. Spine 13: 9– 11, 1988 [DOI] [PubMed] [Google Scholar]
- 67). Nowinski GP, Visarius H, Nolte LP, Herkowitz HN: A biomechanical comparison of cervical laminaplasty and cervical laminectomy with progressive facetectomy. Spine 18: 1995– 2004, 1993 [DOI] [PubMed] [Google Scholar]
- 68). Subramaniam V, Chamberlain RH, Theodore N, Baek S, Safavi-Abbasi S, Senoğlu M, Sonntag VK, Crawford NR: Biomechanical effects of laminoplasty versus laminectomy: stenosis and stability. Spine 34: E573– E578, 2009 [DOI] [PubMed] [Google Scholar]
- 69). Kode S, Gandhi AA, Fredericks DC, Grosland NM, Smucker JD: Effect of multilevel open-door laminoplasty and laminectomy on flexibility of the cervical spine: an experimental investigation. Spine 37: E1165– E1170, 2012 [DOI] [PubMed] [Google Scholar]
- 70). Kubo S, Goel VK, Yang SJ, Tajima N: The biomechanical effects of multilevel posterior foraminotomy and foraminotomy with double-door laminoplasty. J Spinal Disord Tech 15: 477– 485, 2002 [DOI] [PubMed] [Google Scholar]
- 71). Tadepalli SC, Gandhi AA, Fredericks DC, Grosland NM, Smucker J: Cervical laminoplasty construct stability: an experimental and finite element investigation. Iowa Orthop J 31: 207– 214, 2011 [PMC free article] [PubMed] [Google Scholar]
- 72). Takeshita K, Peterson ET, Bylski-Austrow D, Crawford AH, Nakamura K: The nuchal ligament restrains cervical spine flexion. Spine 29: E388– E393, 2004 [DOI] [PubMed] [Google Scholar]
- 73). Baisden J, Voo LM, Cusick JF, Pintar FA, Yoganandan N: Evaluation of cervical laminectomy and laminoplasty. A longitudinal study in the goat model. Spine (Phila Pa 1976) 24: 1283– 1288; discussion 1288–12899, 1999. [DOI] [PubMed] [Google Scholar]
- 74). Fields MJ, Hoshijima K, Feng AH, Richardson WJ, Myers BS: A biomechanical, radiologic, and clinical comparison of outcome after multilevel cervical laminectomy or laminoplasty in the rabbit. Spine 25: 2925– 2931, 2000 [DOI] [PubMed] [Google Scholar]
- 75). Lao L, Zhong G, Li X, Qian L, Liu Z: Laminoplasty versus laminectomy for multi-level cervical spondylotic myelopathy: a systematic review of the literature. J Orthop Surg Res 8: 45, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76). Kaminsky SB, Clark CR, Traynelis VC: Operative treatment of cervical spondylotic myelopathy and radiculopathy. A comparison of laminectomy and laminoplasty at five year average follow-up. Iowa Orthop J 24: 95– 105, 2004 [PMC free article] [PubMed] [Google Scholar]
- 77). Hardman J, Graf O, Kouloumberis PE, Gao WH, Chan M, Roitberg BZ: Clinical and functional outcomes of laminoplasty and laminectomy. Neurol Res 32: 416– 420, 2010 [DOI] [PubMed] [Google Scholar]
- 78). Mummaneni PV, Kaiser MG, Matz PG, Anderson PA, Groff MW, Heary RF, Holly LT, Ryken TC, Choudhri TF, Vresilovic EJ, Resnick DK, Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and Congress of Neurological Surgeons : Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine 11: 130– 141, 2009 [DOI] [PubMed] [Google Scholar]
- 79). Hirabayashi K, Toyama Y, Chiba K: Expansive laminoplasty for myelopathy in ossification of the longitudinal ligament. Clin Orthop Relat Res 35– 48, 1999. [DOI] [PubMed] [Google Scholar]
- 80). Halvorsen CM, Lied B, Harr ME, Rønning P, Sundseth J, Kolstad F, Helseth E: Surgical mortality and complications leading to reoperation in 318 consecutive posterior decompressions for cervical spondylotic myelopathy. Acta Neurol Scand 123: 358– 365, 2011 [DOI] [PubMed] [Google Scholar]
- 81). Manzano GR, Casella G, Wang MY, Vanni S, Levi AD: A prospective, randomized trial comparing expansile cervical laminoplasty and cervical laminectomy and fusion for multilevel cervical myelopathy. Neurosurgery 70: 264– 277, 2012 [DOI] [PubMed] [Google Scholar]
- 82). Bydon M, Macki M, Kaloostian P, Sciubba DM, Wolinsky JP, Gokaslan ZL, Belzberg AJ, Bydon A, Witham TF: Incidence and prognostic factors of c5 palsy: a clinical study of 1001 cases and review of the literature. Neurosurgery 74: 595– 604; discussion 604–605, 2014 [DOI] [PubMed] [Google Scholar]
- 83). Hosono N, Sakaura H, Mukai Y, Fujii R, Yoshikawa H: C3–6 laminoplasty takes over C3–7 laminoplasty with significantly lower incidence of axial neck pain. Eur Spine J 15: 1375– 1379, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]