Abstract
Intraoperative angiography (IOA) is employed for the treatment of the complicated cases in neurological surgery. The IOA is usually performed with OEC portable digital subtraction angiography (DSA) unit. We are performing IOA with portable fluoroscopy unit with simple DSA function and report its usefulness on neurosurgical treatment. IOA or hybrid treatment with mobile fluoroscopy system was performed for 9 cases [cerebral arteriovenous malformation (AVM), 3; cranial dural arteriovenous fistula (AVF), 2; and spinal AVM/AVF, 4]. Thus, ex vivo analysis was performed comparing image quality of portable fluoroscopy unit and conventional DSA system. Although the resolution of portable fluoroscopy unit is not so high compared to conventional DSA system, the existence of the vascular lesions such as cerebral aneurysm, cerebral AVM, and spinal dural AVF were detected. The operation of portable fluoroscopy unit was simple and no special assistance was required. The complication related to the catheterization or IOA did not occur. IOA with portable fluoroscopy unit was useful for the identification of vascular lesion and has advantage on the cost benefit.
Keywords: intraoperative angiography, fluoroscopy, neurointervention
Introduction
Intraoperative angiography (IOA) is employed for the treatment of the complicated cases in neurological surgery.1) Recently, hybrid operating room is developed and the IOA or the combined treatment, namely, hybrid treatment is performed in limited institutes.2,3) However, it is difficult to introduce that facility to the standard institutes. The IOA is usually performed for the diagnosis of the cerebrovascular lesion using portable digital subtraction angiography (DSA) unit (OEC Diasonics Inc., Salt Lake City, Utah, USA). However, angiography has a risk of complication rate of 1–3% that can include permanent neurological deficit1) and is employed for only selected cases. Moreover, surgical treatment for the complicated lesion is not so frequent that the mobile DSA unit does not spread widely. A surgical X-ray apparatus SXT-9000 (TOSHIBA, Minato, Tokyo) is a portable fluoroscopy unit accompanied with simple DSA function (Fig. 1A). We are performing IOA with this portable fluoroscopy unit and report the usefulness on the neurosurgical treatment.
Fig. 1.
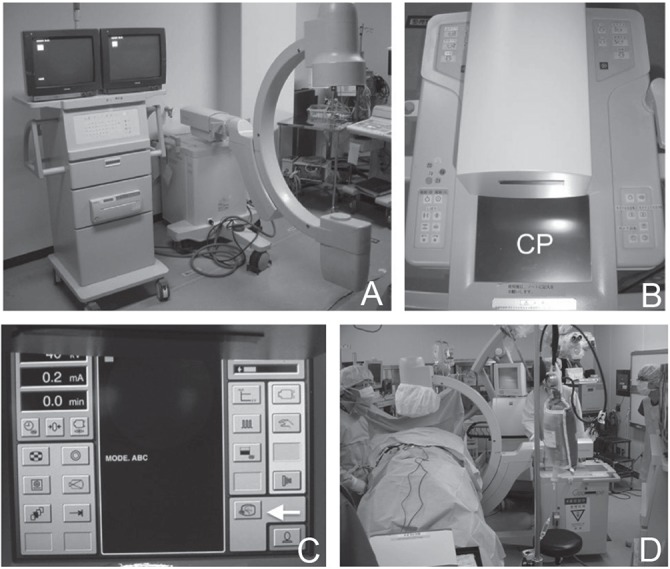
TOSHIBA mobile surgical X-ray apparatus SXT-9000. A: Overview of the system. B: Control panel (CP). C: Image of the activated monitor (arrow indicates switch for angiography mode). D: Applying intraoperative angiography in the surgical field.
Materials and Methods
I. Patient demographics
From 2005 to 2012, IOA with mobile fluoroscopy system was performed for 9 cases of vascular malformation [cerebral arteriovenous malformation (AVM), 3; cranial dural arteriovenous fistula (AVF), 2; and spinal AVM/AVF, 4]. During the same period, 35 cases of vascular malformation were treated with open surgery and 108 cases of vascular malformation were treated with neurointervention.
II. Intraoperative method
All craniotomies and laminectomies were performed by experienced neurosurgeons and IOA was performed by an endovascular team, which consisted of neurosurgeons and radiologists. After induction of general anesthesia, bilateral groin was prepared and draped in a standard sterile fashion. A 4F sheath was inserted into the femoral artery via the Seldinger technique. Patient was positioned depending on the location of the lesion and the head was fixed with Mayfield radiolucent head holder. C-arm was covered with clean drape and introduced to the surgical area. Catheter was introduced to the artery under fluoroscopy unit, and IOA was performed by the DSA mode (Fig. 1B, C). The mode was switched just one push on the control panel and proper electric current and voltage were determined automatically. Contrast medium was injected manually. The catheter was continuously irrigated with heparinized saline. Craniotomy or laminectomy was performed and IOA was repeated as necessary until the goals of the surgical procedure had been achieved (Fig. 1D). In each operation, the lesion was examined mainly pre-treatment and post-treatment. Indocyanine green fluorescence (ICG) video-angiography was additionally performed, if necessary. Catheter was withdrawn after completion of the procedure and the sheath was usually removed on the same day. The finding of the IOA was compared with preoperative and postoperative imaging studies.
III. Ex vivo analysis
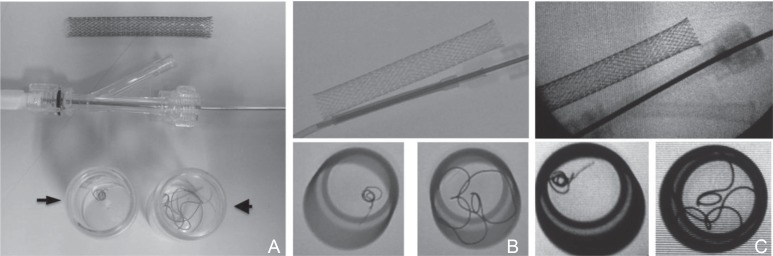
Ex vivo experiment was performed comparing fluoroscopy images of AXIOM Artis DSA system (Siemens Medical Solutions, Munich, Germany) and portable surgical X-ray apparatus SXT-9000 using carotid artery stent, 0.010 inch detachable coil, and 0.018 inch detachable coil which were placed in the glass bottle.
Results
Indication rate of IOA was 100% of the cranial dural AVF and 50% of spinal AVM/AVF, followed by cranial AVM (12%). The annual IOA rate was 1.5 times. In each operation, IOA was performed 1 to 4 times (mean 2.3). The existence of the vascular lesions such as cerebral AVM and spinal AVM/AVF including its drainer were detected with DSA with portable fluoroscopy unit. The operation of portable fluoroscopy unit was simple and no special assistance was required. Complication related to the catheterization or IOA did not occur. ICG video-angiography was additionally performed for 6 cases. The finding was consistent with IOA. Thus, postoperative imaging studies confirmed the accuracy of the IOA finding.
Approximately 1 hour was needed for the set-up of the IOA. Regarding with function of the portable fluoroscopy unit, the size of the imaging area was 6 inch or 9 inch and the resolution was 44 lp/cm. Frequency of the DSA was either 2 fps or 4 fps. Zoom in or out was not possible. Additional functions such as “overlay” or “road map” function were not available. The IOA image was stored in the hard disk and replayed. The best moment of the IOA was stopped and sent to another monitor. The data of the IOA was able to be sent to the electronic medical record system, and was attached to the patient’s file. Basic method (subtraction with a logarithmic function) of DSA with portable fluoroscopy unit is technically same with conventional DSA unit. However, the image mode of the portable fluoroscopy is fluoroscopy mode and that of portable DSA or hybrid operating room is DSA mode. Moreover, the maximum electrical current of portable fluoroscopy is 10 mA and that of conventional DSA is 1,250 mA, that value affects the resolution.
Finally, the total cost of this portable fluoroscopy unit was approximately 400,000 US dollars, which is four-tenth of portable DSA unit and one-tenth of hybrid operating system (Table 1).
Table 1.
Summary of hybrid operating room, portable digital subtraction angiography, and portable fluoroscopy
| Hybrid OR | Portable DSA | Fluoroscopy | |
|---|---|---|---|
| DSA | |||
| Resolution (bit) | 12 | 12 | 10 |
| Electrical current (mA) | 1,250 | 150 | 10 |
| Mode | DSA | DSA | Fluoroscopy |
| Image shoot frequency (fps) | 2–30 | 2–25 | 2/4 |
| Size (inch) | 12/11/10/9/6 | 9/6/4.5 | 9/6 |
| Road map | ○ | ○ | × |
| 3D image | ○ | × | × |
| Fluoroscopy | |||
| Rate (pps) | 30 | 30 | 8 |
| Resolution (lp/cm) | 26 | 46 | 44 |
| Price (US$) | 4,000,000 | 1,000,000 | 400,000 |
3D: three-dimensional, DSA: digital subtraction angiography, OR: operating room, ○: possible, ×: impossible.
Illustrative Cases
I. Case 1
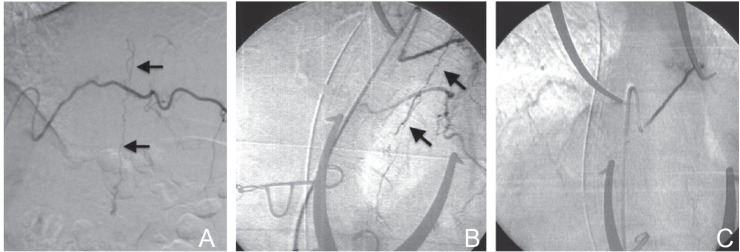
A 56-year-old man visited a nearby hospital because of right lower extremities sensory disturbance. A spinal cord edema due to the spinal dural AVF was revealed by magnetic resonance imaging (MRI) and the patient was referred to our hospital. Conventional DSA of the right T7 intercostal artery showed AVF and draining vein (Fig. 2A). The patient underwent a T7–T8 laminectomy. IOA of the right T7 intercostal artery using portable fluoroscopy unit revealed AVF and draining vein consistent with conventional DSA findings (Fig. 2B). The fistula was also identified with intra-arterial ICG angiography and was coagulated. After that, disappearance of AVF and draining vein were confirmed by IOA (Fig. 2C). Then, skin incision was closed. The postoperative course was uneventful and the spinal cord edema was improved.
Fig. 2.
Case 1 spinal dural arteriovenous fistula (AVF). A: Conventional digital subtraction angiography (DSA) shows AVF (arrow indicates draining vein). B: Intraoperative angiography (IOA) shows AVF consistent with DSA (arrow indicates draining vein). C: After occlusion of the AVF, the AVF and draining vein disappeared in the IOA.
II. Case 2
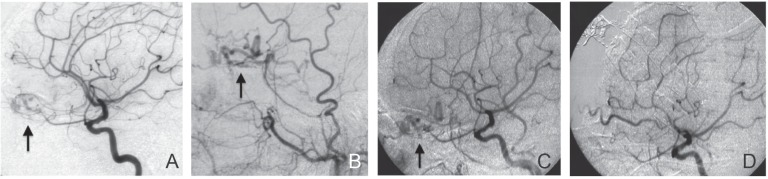
A 69-year-old man visited a nearby hospital for brain check-up. An anterior fossa dural AVF was suspected by MRI and the patient was referred to our hospital. Conventional DSA revealed left anterior fossa dural AVF fed by the branches of the ophthalmic artery and the left external carotid artery (Fig. 3A, B). The drainage was middle cerebral vein and sphenoparietal sinus. The patient underwent bifrontal craniotomy. IOA from the left common carotid artery using portable fluoroscopy unit showed anterior fossa dural AVF, consistent with conventional DSA findings (Fig. 3C). The fistula was occluded with coagulation. After confirming the disappearance of the AVF by IOA (Fig. 3D), the craniotomy was closed. The postoperative course was uneventful and MR angiography showed complete obliteration of the AVF.
Fig. 3.
Case 2 anterior fossa dural AVF. A: Conventional DSA of the left internal carotid artery shows anterior fossa dural AVF (arrow). B: Conventional DSA of the left external carotid artery shows anterior fossa dural AVF (arrow). C: IOA of the left common carotid artery shows AVF consistent with DSA (arrow). D: After occlusion of the AVF, the AVF and draining vein disappeared in IOA. AVF: arteriovenous fistula, DSA: digital subtraction angiography, IOA: intraoperative angiography.
III. Ex vivo analysis
As shown in Fig. 4, all carotid artery stents, 0.010 inch coil and 0.018 inch coil were detectable by portable fluoroscopy unit and conventional DSA system. But the quality of the image of conventional DSA system was much better. Thus, the halation was predominant in portable fluoroscopy unit.
Fig. 4.
Comparison of the resolution of the images. A: Photography of carotid artery stent, 0.010 inch coil (arrow) and 0.018 inch coil (arrowhead). B: Fluoroscopy images of conventional digital subtraction angiography system. C: Fluoroscopy images of portable surgical X-ray apparatus SXT-9000.
Discussion
Intraoperative imaging studies are developing dramatically. Intraoperative computed tomography (CT) and MRI provide updated intraoperative data that can validate stereotactic biopsy paths, correct for intraoperative brain sift, confirm the degree of resection, and provide early detection of procedure-related hematoma or infarction.4) In the field of cerebrovascular disease, DSA has been employed intraoperative imaging especially for complicated cases.5) It has been done by portable DSA unit (OEC Diasonics), mainly. Recently, the development of C-arm mounted flat-panel detectors has enhanced the quality of DSA imaging and allowed for the high resolution computed three-dimensional (3D) rotational angiography.6) Operative room equipment with DSA, which has capabilities of neurointervention, namely hybrid operating room has been developed and used in the some institute.7,8) Iihara et al. reported the advantage of hybrid operating room over the portable DSA unit because the image quality of portable DSA is insufficient for neurovascular intervention and sophisticated imaging technique, such as rotational angiography and 3D acquisition, are not usually available in the portable DSA.9) However, great investment and additional construction are needed to introduce hybrid operating room. Complicated cases which require hybrid treatment are not so frequently encountered. In fact, combined treatment in same session was performed for only 4 cases among 25 cases of AVM (16%) in an institute, which has hybrid operating room, because biplane conventional DSA was suitable for neurointervention.3) Cost-benefit of the hybrid operating room is doubtful since it is not so frequently used and the effect has been controversial.10,11)
Portable fluoroscopy unit is quite frequently used especially in the orthopedic operation. Four portable fluoroscopy units have been working in our institute and all of them are used almost every day. Some of them provide 3D image and are useful for the spinal surgery with navigation system. Portable surgical X-ray apparatus SXT-9000 was first choice among our portable fluoroscopy units because of its relatively compact size and easy to use. The most unique advantage of this fluoroscopy unit is simple DSA function. The mode was changed in just one switch and no adjustment was required for examination (Fig. 1). This is the first report on IOA with portable fluoroscopy unit. As shown in Figs. 2 and 3, the existence of cranial AVM and AVF, spinal AVM and AVF including draining vein were detected by this portable fluoroscopy unit. However, in our impression, the image quality does not stand for the neurointervention. Regarding with fluoroscopy image, we performed ex vivo experiment. As shown in Fig. 4, 0.010 inch coil was identified; however, the contrast is less than conventional DSA system. To support this weakness, we are employing ICG angiography.12) Intra-venous ICG angiography requires 10–20 minutes before dissipation of ICG fluorescence, making repeated studies somewhat tedious and time consuming.13) Intra-arterial injection of ICG from catheter shows hemodynamic status and repeated again and again since the amount of intra-arterial ICG is 1/100 of that of intra-venous ICG.12)
The limitation of this study includes retrospective nature of the data analysis. Number of cases evaluated with IOA is low, because we employed this technique for selected cases. Unfortunately, we do not have portable DSA unit and could not compare the image with portable fluoroscopy unit. However, the quality of portable DSA unit is as high as conventional DSA unit as shown in Table 1. Then, comparing with image of conventional DSA unit, we evaluated the quality of portable fluoroscopy unit indirectly.
Conclusion
IOA with portable fluoroscopy unit was useful for the identification of vascular lesion and has advantage on the cost-benefit.
References
- 1). Derdeyn CP, Moran CJ, Cross DT, Grubb RL, Dacey RG: Intraoperative digital subtraction angiography: a review of 112 consecutive examinations. AJNR Am J Neuroradiol 16: 307– 318, 1995. [PMC free article] [PubMed] [Google Scholar]
- 2). Choudhri O, Mukerji N, Steinberg GK: Combined endovascular and microsurgical management of complex cerebral aneurysms. Front Neurol 4: 108, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). Kotowski M, Sarrafzadeh A, Schatlo B, Boex C, Narata AP, Pereira VM, Bijlenga P, Schaller K: Intraoperative angiography reloaded: a new hybrid operating theater for combined endovascular and surgical treatment of cerebral arteriovenous malformations: a pilot study on 25 patients. Acta Neurochir (Wien) 155: 2071– 2078, 2013. [DOI] [PubMed] [Google Scholar]
- 4). Haydon DH, Chicoine MR, Dacey RG, Jr: The impact of high-field-strength intraoperative magnetic resonance imaging on brain tumor management. Neurosurgery 60: (Suppl 1) 92– 97, 2013. [DOI] [PubMed] [Google Scholar]
- 5). Chalouhi N, Theofanis T, Jabbour P, Dumont AS, Fernando Gonzalez L, Starke RM, Dalyai RT, Hann S, Rosenwasser R, Tjoumakaris S: Safety and efficacy of intraoperative angiography in craniotomies for cerebral aneurysms and arteriovenous malformations: a review of 1093 consecutive cases. Neurosurgery 71: 1162– 1169, 2012. [DOI] [PubMed] [Google Scholar]
- 6). Leng LZ, Rubin DG, Patsalides A, Riina HA: Fusion of intraoperative three-dimensional rotational angiography and flat-panel detector computed tomography for cerebrovascular neuronavigation. World Neurosurg 79: 504– 509, 2013. [DOI] [PubMed] [Google Scholar]
- 7). Fandino J, Taussky P, Marbacher S, Muroi C, Diepers M, Fathi AR, Remonda L: The concept of a hybrid operating room: applications in cerebrovascular surgery. Acta Neurochir Suppl 115: 113– 117, 2013. [DOI] [PubMed] [Google Scholar]
- 8). Murayama Y, Irie K, Saguchi T, Ishibashi T, Ebara M, Nagashima H, Isoshima A, Arakawa H, Takao H, Ohashi H, Joki T, Kato M, Tani S, Ikeuchi S, Abe T: Robotic digital subtraction angiography systems within the hybrid operating room. Neurosurgery 68: 1427– 1432; discussion 1433, 2011. [DOI] [PubMed] [Google Scholar]
- 9). Iihara K, Satow T, Matsushige T, Kataoka H, Nakajima N, Fukuda K, Isozaki M, Maruyama D, Nakae T, Hashimoto N: Hybrid operating room for the treatment of complex neurovascular and brachiocephalic lesions. J Stroke Cerebrovasc Dis 22: e277– e285, 2013. [DOI] [PubMed] [Google Scholar]
- 10). Yamakawa K, Kiyama S, Murayama Y, Uezono S: Incidence and neurological outcomes of aneurysm rupture during interventional neuroradiology procedures in a hybrid operating suite. J Anesth 26: 592– 594, 2012. [DOI] [PubMed] [Google Scholar]
- 11). Murayama Y, Arakawa H, Ishibashi T, Kawamura D, Ebara M, Irie K, Takao H, Ikeuchi S, Ogawa T, Kato M, Kajiwara I, Nishimura S, Abe T: Combined surgical and endovascular treatment of complex cerebrovascular diseases in the hybrid operating room. J Neurointerv Surg 5: 489– 493, 2013. [DOI] [PubMed] [Google Scholar]
- 12). Horie N, So G, Debata A, Hayashi K, Morikawa M, Suyama K, Nagata I: Intra-arterial indocyanine green angiography in the management of spinal arteriovenous fistulae: technical case reports. Spine 37: E264– E267, 2012. [DOI] [PubMed] [Google Scholar]
- 13). Woitzik J, Horn P, Vajkoczy P, Schmiedek P: Intraoperative control of extracranial-intracranial bypass patency by near-infrared indocyanine green videoangiography. J Neurosurg 102: 692– 698, 2005. [DOI] [PubMed] [Google Scholar]