Abstract
Objectives:
This epidemiological study aimed to analyse economical and societal consequences in Denmark if CBCT is used routinely as a diagnostic method before removal of the mandibular third molar. Furthermore, the aim was to calculate the excess cancer incidence from this practice.
Methods:
17 representative dental clinics in the regions of Denmark were visited by two observers, who registered the total number of patients in each clinic, the number of removed mandibular third molars from patients' files together with the age and gender of these patients. The data were collected from 2008 to 2014. The total number of removed mandibular third molars in Denmark each year was derived from the collected data and information on patients' contacts with dentists from Statistics Denmark as a sum of contributions from each region. The contribution of a region was obtained as the number of removed mandibular third molars in the selected clinics in the region times the ratio of the number of patients in the selected clinics in the region to the total number of patients with contact to a general practitioner in the region in 2011. Existing knowledge on the costs for panoramic and CBCT imaging was used to calculate total costs. The cancer incidence was calculated from lifetime attributable risk curves based on linear risk assumptions.
Results:
The selected clinics included 109,686 patients, and 1369 mandibular third molars had been surgically removed. Using data from Statistics Denmark gave an estimated annual number of removed mandibular third molars of 36,882 at a total cost of €6,633,400. The additional cancer incidence was estimated to be approximately 0.46 per year.
Conclusions:
The data should be used in a cost-effectiveness analysis of the clinical efficacy of CBCT imaging before removal of mandibular third molars.
Keywords: mandibular third molar, CBCT scanning, panoramic imaging, costs, cancer incidence
Introduction
Implementation of new medical technology should be based on patient benefits and societal advantages.1 Ideally, a Health Technology Assessment (HTA) should be performed before introducing new medical technology.2 It is a complex task to develop a HTA, and very often, there is neither will nor time or resources for this kind of analysis. However, the assessment of new equipment or procedures is not sufficient without considering economic parameters. Limited resources and an ever-increasing introduction of new or pseudo-new technology underline the necessity of prioritizing based on achieved benefits in relation to costs. Performing a health economic analysis on the other hand requires data describing the interventions or procedures and the consequences for the patients. Furthermore, there must be reliable information concerning the incidence and/or prevalence of the studied interventions.
The most common surgical procedure in dentistry is probably the removal of the mandibular third molar.3 In Denmark (DK), no data have been available about the annual number of surgical removals of the third molar. The Danish Public Health Statistics does not differentiate between different types and sites of surgical interventions in dentistry. International studies reporting quantitative data about surgical removals of third molars are rare. A Norwegian study from 1995 used data from questionnaires to estimate the number of surgical removals,4 but the validity of these data may be questionable owing to the study design. National differences and changing indications and guidelines are furthermore likely to complicate the use of these data in an assessment of the number of surgical interventions performed in DK. A recent study focusing on England, Wales and Scotland pertained to determine the trend in the number of surgically removed mandibular third molars over time, but data describing the absolute numbers of removals in these populations are lacking.5
Owing to the risk of nerve injuries following third molar removal, new diagnostic methods and surgical procedures have been introduced in recent years. CBCT scanning and coronectomy are examples of diagnostic and treatment strategies, which have been suggested to reduce complications and decrease morbidity following removal of the mandibular third molar. CBCT has been shown to require around four times the resources compared with panoramic imaging, which until now has been the state-of-the-art for pre-operative assessment and treatment planning.6 Furthermore, CBCT does not seem to change surgical treatment planning substantially,7 and a recent study reported that no differences were seen in operation time or common morbidity among patients treated on the basis of CBCT or panoramic examination.6 It is currently unclear if pre-operative diagnostic use of CBCT will reduce the number of neurosensoric disturbances. However, it is evident that the use of CBCT is associated with an increase in radiation exposure to the population.8,9 Possible benefits from performing a CBCT examination pre-operatively must be compared with the public health consequences of the imaging technique being routinely and extensively implemented.
The aims of this study were to:
(1) estimate the annual incidence of removed mandibular third molars in DK
(2) calculate the annual costs of using CBCT as a routine diagnostic method before removal of a mandibular third molar
(3) estimate the annual increase in cancer incidence assuming that CBCT is accepted as the standard pre-operative diagnostic method.
Methods and materials
Field study
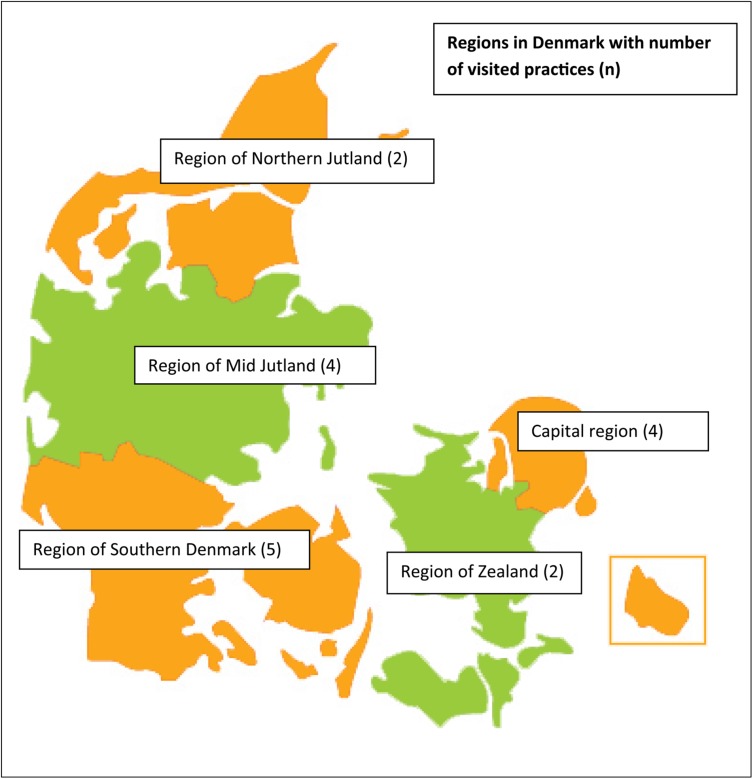
In DK, almost all patients older than 18 years who visit a dentist are treated in private practice. Patients younger than 18 years are primarily treated in the community healthcare system. However, no national data are available on the number of surgically removed mandibular third molars. Therefore, a field study was planned to collect samples from general dental practices (GP) in the five administrative regions of DK. Only patients treated in private practices were included in the study since extremely few patients have their third molars removed before the age of 18 years. For patients of age 18 years or older, regional data about visits to and treatments by private dentists are available from Statistics Denmark (Figure 1). Unfortunately, the information does not distinguish between different surgical procedures. Therefore, the study was designed as an observational study visiting two to five GPs in each region.
Figure 1.
Five regions in Denmark and number of visited practices in brackets.
The inclusion criteria for the participating practices were: (1) patients with indications for removal of the mandibular third molar should be treated within the practice and not referred to specialists, clinics or universities, (2) the practices should in the years of interest have implemented one of the two dental software systems “DentalSuite®” (Vallensbæk, DK) or “AlDente®” (Horning, DK). These two software systems are holding an overwhelming part of the market share of dental administration software in DK. Both systems facilitate the possibility of extracting data about number of patients and number and type of treatments. Exclusion criteria for the participating practices were: (1) status as specialist practice based on referrals from other dentists and (2) GPs where surgical removal of the mandibular third molar is referred to specialists. The GPs were randomly chosen from lists provided by the software companies. For practical reasons, only practices with more than five workstation licenses were included. Information about the study was sent to 19 selected GPs. One practice declined participation, and one practice did not answer.
2 observers visited together 17 GPs (Figure 1) between October 2011 and June 2014 collecting data concerning number of patients, number of third molar removals and pre-operative radiological methods. The data were organized in Epidata v. 3.1 (EpiData Association, Odense, DK). Data on the number of patients in each region in each of the years 2009–12 were obtained from Statistics Denmark.10 Because of the very constant numbers of patients in the population in the years studied, as well as the stable number of patients and surgical removals in the samples, it was decided to simplify the calculations by simulating that all data were sampled in 2011. This means that the accumulated data sample was compared with data from Statistics Denmark in 2011.
Cost study
Based on the epidemiological data from the field study, it was possible to derive the overall costs from using CBCT as a routine procedure before surgical removal of the mandibular third molar. In a previous randomized controlled trial, the absolute and relative costs for panoramic imaging and CBCT were calculated using microeconomically collected data combined with health economic standards and national statistical information.6 Data were collected in the Danish population in a comparable period of time. The randomized controlled trial cost study concluded that the costs for a CBCT image in DK would vary between €70 and €180 depending on initial capital costs and number of performed images per year. The same study showed a range in the costs for a panoramic image between €25 and €50 determined by the same variables. In the present study, different scenarios were used to simulate possible economic outcomes if CBCT was considered as the standard pre-operative imaging method before surgical removal of the mandibular third molar. Furthermore, sensitivity to a change in assumptions was analysed. These assumptions included number of images, initial equipment costs and depreciation.6
Dose–response study
Increased radiation exposure to the population will most probably lead to an increase in the cancer incidence. The linearity principle can be expressed in a lifetime attributable risk curve (Figure 2). This curve provides an estimate of the increased cancer incidence on the population level given the age distribution and the exposure values. Unfortunately, it is difficult to access unique dose information concerning CBCT since there are significant differences between CBCT units and imaging modes.12–14 In this study, different dose settings were simulated to provide an estimate of the possible variation in the cancer incidence increase between a minimum and maximum limit. The formula for the calculation was: AC = CR × NR 10−6 × ED 10−4, where AC is the annual number of additional cancers, CR is the curve reading of the age-related lifetime risk, NR is the number of removals (= number of CBCT examinations) and ED is the estimated mean dose of the CBCT examination.
Figure 2.
Lifetime attributable risk curves for the relation between exposure and age in a population. Adapted from Hall and Brenner11 with permission from the British Institute of Radiology.
Data treatment
For each clinic, the number of surgically removed mandibular third molars during the years 2009–12 was extracted using the software available in the clinics. The total number, T, of removed mandibular third molars was estimated as:
where Vr is the estimated number of removed third molars in region r; Pr is the number of adult patients in region r; pr is the number of adult patients in region r in the sample; and vr is the number of removed third molars in region r in the sample.
For each region, the number of removed mandibular third molars was considered following a Poisson distribution, and the standard error of the estimate T [SE(T)] was therefore computed as:
Results
Field study
Accumulating the number of patients registered in all visited GPs simulating a period of 1 year provided a total sample of 95,789. The total number of removed mandibular third molars in this sample was 1369. This includes 40 coronectomies, corresponding to 2.9% of the removed third molars in the sample. 25 (62.5%) of the coronectomies were performed in the capital region, equalizing 5.1% of the surgically removed third molars in this region. The capital region holds 29.3% of the adult population with dental contacts in 2011.
The total number of adult patients with contact to a GP in 2011 was 2,545,670. This number varied <1% in a period of 3 years (2009–12). Applying the summation formula described above provided a total number of 36,882 removed mandibular third molars annually in DK. The overall incidence of annually removed third molars in the total Danish population was thus calculated to 663 per 100,000. Table 1 summarizes basic demographic information, distributions, calculations and standard deviations of the field study.
Table 1.
Demographic data for the included general dental practices (GPs) in the five regions of Denmark
| Regions | Capital region | Region of Zealand | Region of Northern Jutland | Region of Mid Jutland | Region of Southern Denmark | Total Denmark |
|---|---|---|---|---|---|---|
| Number of practices | 4 | 2 | 2 | 4 | 5 | 17 |
| Number of patients accumulated | 32,259 | 9334 | 12,593 | 23,684 | 17,919 | 95,789 |
| Age mean, years (standard deviation) | 32.5 (12.5) | 36.7 (13.8) | 35.1 (12.2) | 30.8 (12.9) | 33.1 (12.1) | 33.1 (12.9) |
| Number of removed mandibular third molars | 491 | 191 | 158 | 345 | 184 | 1369 |
| Number of patients with contact to GP in 2011 | 747,947 | 379,090 | 274,386 | 592,898 | 551,349 | 2,545,670 |
| Annual number of removed mandibular third molars (standard error) | 11,384 (513) | 7757 (561) | 3443 (273) | 8637 (464) | 5661 (417) | 36,882 (1021) |
| Population in 2011 | 1,702,388 | 819,071 | 579,787 | 1,262,115 | 819,071 | 5,564,219 |
| Annual incidence per 100,000 inhabitants | 669 | 947 | 593 | 684 | 471 | 663 |
| Ratio of removals vs ratio population in regions | 1.05 | 1.41 | 0.92 | 1.00 | 0.71 | – |
Cost study
Implementing CBCT as the routine pre-operative diagnostic and treatment-planning method would mean that €6,638,400 additional costs would be spent. Costs were also calculated in a sensitivity setting, presuming CBCT imaging in 100%, 50%, 25% and 12.5% of the third molar removal cases. Table 2 shows the sensitivity of the costs including settings if panoramic imaging were the method of choice. Setting A includes high initial equipment costs and 5 years' depreciation, whereas Setting B includes low initial costs and 10 years' depreciation.
Table 2.
Costs in euros for CBCT and panoramic imaging
| Number of images | 36,880 | 18,440 | 9220 | 4610 |
|---|---|---|---|---|
| Costs CBCT, Setting A | 6,638,400 | 3,319,200 | 1,659,600 | 829,800 |
| Costs panoramic, Setting A | 1,844,000 | 922,000 | 461,000 | 230,500 |
| Costs CBCT + panoramic, Setting A | 8,482,400 | 4,241,200 | 2,120,600 | 1,060,300 |
| Costs CBCT, Setting B | 2,581,600 | 1,290,800 | 645,400 | 322,700 |
| Costs panoramic, Setting B | 922,000 | 461,000 | 230,500 | 115,250 |
| Costs CBCT + panoramic, Setting B | 3,503,600 | 1,751,800 | 875,900 | 437,950 |
Dose–response study
As the radiation dose differs tremendously between CBCT units depending on type, individual machine, field of view (FOV), protocol and voxel resolution, it is impossible to determine a precise single patient dose.12–14 Therefore, different dose settings are used to describe the consequences of routine CBCT for the increase in annual cancer incidence. The lifetime attributable risk curve in Figure 2 expresses dose in Gray, and in the present calculation, this unit was used synonymously with Sievert. At the mean level of 125 µSv, an increase in annual cancer incidence of 0.46 was calculated, assuming that CBCT examination would be routinely used pre-operatively. Table 3 visualizes the consequences for the cancer incidence of different dose settings. Furthermore, variation in number of images was part of this sensitivity analysis. Depending of the assumptions, the annual cancer incidence in the Danish population would increase with a figure between 0.09 and 0.74.
Table 3.
Increased cancer incidence depending on dose assumptions
| Number of images | 36,880 | 18,440 |
|---|---|---|
| Dose 125 µSv | 0.46 | 0.23 |
| Dose 50 µSv | 0.18 | 0.09 |
| Dose 200 µSv | 0.74 | 0.37 |
Discussion
Guidelines for the use of CBCT imaging before removal of the mandibular third molar are provided by the SEDENTEXCT project.15 According to these guidelines, the availability of high evidence studies is limited, and the recommendations are categorized as “C” on an evidence grade scale from A to D,16 meaning that future research eventually may change the knowledge basis of the recommendations. Currently, the guidelines do not recommend CBCT imaging before third molar surgery as a routine diagnostic and treatment planning method. Fryback and Thornbury1 suggested a six-step hierarchical model for evaluating diagnostic imaging methods. The three upper levels in this model describe treatment decisions, patient outcome and societal consequences. Studies reaching these levels should be the foundation for evidence-based decisions; however, the literature supporting the SEDENTEXCT guidelines does not include any Level 4, 5 or 6 studies. A recently published review emphasizes this lack of relevant evidence.17 Therefore, the actual GRADE categorization could be challenged claiming that the evidence level is “D” rather than “C”. This means that there is little reliable knowledge concerning the consequences of pre-operative use of CBCT in the management of mandibular third molars, for neither the patients nor society. The SEDENTEXCT guidelines concerning this topic are developed without figures for number of mandibular third molar removals, costs for CBCT examination, patient morbidity, changes in number of neurosensoric disturbances to the alveolar inferior nerve, cost effectiveness or cost utility. The decision for using CBCT before surgical removal of third molars in dental clinics will therefore also be based most probably on local opinions and beliefs, legal considerations or other arbitrary reasons. There may be a tendency to perform diagnostic imaging, which exceeds existing and accepted indications,18 and this tendency could be intensified when the recommendations are based on low evidence levels. The impressive marketing of existing and upcoming advanced technical equipment could disturb the clinical user's intellectual interface to basic scientific principles, especially when solid knowledge is absent. In a very strict interpretation of the Fryback and Thornbury categories, cost-effectiveness should be analysed to reach Level 6; however, the present study represents elements of the “societal efficacy” level since societal consequences could also be costs, equity measurements, cost utility, ethical components etc. The first part introduced an estimate of the actual number of surgically removed mandibular third molars in the studied regions of DK. Without this information, any attempt to assess societal implications will fail. We cannot estimate economic consequences of the use of new technology without knowing the amount of interventions, and we cannot estimate additional cancer incidence without quantitative figures for the use of the relatively high-level radiation procedure, which CBCT imaging constitutes. The limitations of the first part of the study include problems with the internal and external validity. Although the random error of the results may be interpreted as minimal, there could be some systematic errors affecting the internal validity. The sample of visited GPs was not entirely randomly collected. Owing to the need of excluding practices without internal surgical activity as well as specific surgical referral practices, there is a potential risk of under- or overestimating the number of surgical removals. Practicality also determined inclusion criteria, which could induce systematic errors. The included practices all had an advanced technological level, including digital imaging and digital file systems. Furthermore, a majority of the practices in the sample had a certain size, based on a minimal number of digital file licenses, indicating that these GPs were larger than the average practice. There could be differences in the indications, the clinical thinking and the treatment decisions linked to different GP sizes and the different technological levels of dental practices. It is difficult to estimate the consequences of a possible selection bias in the study. The Health Authorities in DK do not provide guidelines for removal of third molars, and it is uncertain if international guidelines19,20 or recommendations from the national universities are known and implemented in private dental practice.
Our knowledge on treatment decisions in GPs is limited. One cohort study from 2014 concluded that general dentists most often recommend removal of third molars to avoid future problems rather than based on symptoms and pathology.21 According to these assumptions, the decision outcome for when to remove a mandibular third molar may be quite similar in different general practices. This means that the quantitative variation in this study may also be limited despite possible selection bias. On the other hand, from Table 1 it seems there is an overestimate of third molar removals in the region of Zeeland. This region is, such as the region of North Jutland and the region of Southern DK, a rural area. From the figures in Table 1, it can be concluded that there is, in general, a lower removal rate in the rural areas. The two practices visited in the region of Zeeland were situated in the largest towns of the region, and this fact could reflect and explain a possible overestimate in this region. Some general parameters related to inclusion and exclusion criteria in the study could be connected to an underestimation of the total removals. Patients under the age of 18 years were not a part of this study and although the removal rate among these patients probably is low, it could add to the total sum of removals. Patients referred to surgical practices, clinics or hospitals from outside the network of general practices were not included in the study and would also increase the total number of removals. In this study, a removal was only registered if the intervention was classified as a surgical procedure. Owing to this classification, removals classified as simple or complex extractions were not included. These criteria are entirely based on the subjective opinion of the surgeons.
The external validity implies the generalization of the study results to other populations. Because of the lack of international data, it is difficult to validate the results. A Norwegian survey4 estimated the annual incidence of removed mandibular third molars in Norway in 1995 to almost 50,000. A British study reported a drop in the number of removals up to the millennium.5 The change was interpreted to be induced by new indications from the National Institute for Health and Care Excellence and Scottish Intercollegiate Guidelines Network guidelines.19,20 The data from Norway4 are therefore probably quite congruent with the data from the present study, although the Norwegian data are based on a study design with limited external validity. The two studies support each other in estimating the quantity of annually removed mandibular third molars in Scandinavia. However, the studies are typical “first world studies” conducted in one of the wealthiest and most technologically developed areas in the world. The results should therefore, of course, be interpreted with caution on a global scale. Comparing the study data from DK with other countries or regions will probably only be meaningful in areas with a comparable socioeconomic structure. Technology dissemination and healthcare distribution should also possess similar features. Although the absolute figures and numbers in the first part of this study do not involve global validity, the basic considerations of the relationship between technology, benefits and costs remain important.
The costs for imaging were in this study viewed from a basic health economic point of view, meaning that the use of basic resources for the society is measured. Absolute costs are of course often relevant, but in most cases, the costs have to be compared with an outcome measuring prevention, curing or minimizing a certain disease or treatment complication. Six million euros is a high sum if no effects of the procedure can be registered but may be a small investment if severe morbidity can be avoided for many patients. If the relation between benefits and costs shall be analysed, simple epidemiological data must be collected. Without this information, neither a cost-effectiveness nor a cost-utility analysis can be performed. Economic considerations, of course, cannot stand alone in the assessment of a given procedure. Ethical, social, environmental and equity aspects have to be taken into account, but without an economical overview, no essential decisions should be made. There is, however, more to the cost subject than the health economic societal point of view. Costs can at least be viewed from two other positions: from the view of the provider of the health service and from the patient's view. Most of the dental health professionals in DK and comparable countries are operating in a private market setting or in a combination of a public and a private economic sphere. The underlying ideology behind this way of organizing the oral health services is probably the concept of market economy, which through “the invisible hand” should lead to a higher quality and efficiency in prevention and treatment of oral diseases. Whether this concept is anchored in scientific facts is not the subject of this study, but it seems that incitements for implementing new technology will tend to follow market rules and not entirely scientific or ethical standards.17 There could be a discrepancy between the financial interests of the health provider and the society's demand for evidence-based practice. From the patient's point of view, the total price for surgical removal of a mandibular third molar in DK most probably will double if CBCT imaging becomes the routine.6,22 The consequences for the treatment accept by the mostly young patients are not predictable. Some patients would maybe avoid proper treatment owing to the increase in costs. For the patients, this could have a severe impact on their oral and general health. This development also could deepen problems concerning equity in the society and contradict public health strategies.
CBCT-induced radiation doses vary depending on FOV, resolution, imaging mode and type of unit. Variations between 3.9 and 674.0 µSv have been reported for FOVs of a height between 5.1 and 10.0 cm.12,14 According to this fact, the cancer incidence could theoretically be much higher or lower than the reported values in this study. Furthermore, the study is based on the assumption that no re-examinations are required. Owing to these uncertainties, the true values probably would remain unknown if CBCT imaging turned into the routine pre-operative radiographic method. But because there, without any doubt, will be an increase in the cancer incidence in the study simulation, different sensitivity settings should be performed to compare these values with possible patient benefits. These settings of course are arbitrary not knowing the national distribution of CBCT scanners and the FOV used.
Conclusions
(1) The annual incidence of surgically removed mandibular third molars in DK can be estimated to 663 out of 100,000 or 36,880 in the Danish adult population.
(2) The annual costs if CBCT were routinely introduced before removal of a mandibular third molar would be €6,638,400 in DK.
(3) The annual increase in cancer incidence in DK would be approximately 0.46 if CBCT is accepted as the standard pre-operative diagnostic method.
Acknowledgments
Acknowledgments
The authors wish to thank the private dental practitioners who opened their offices for the study.
References
- 1.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11: 88–94. doi: 10.1177/0272989X9101100203 [DOI] [PubMed] [Google Scholar]
- 2.Petersen LB, Christensen JH, Olsen KR, Wenzel A. Health Technology Assessment (HTA) in dentistry. [In Danish.] Dan Dent J 2012; 116: 726–34. [Google Scholar]
- 3.Fuster Torres MA, Gargallo Albiol J, Berini Aytés L, Gay Escoda C. Evaluation of the indication for surgical extraction of third molars according to the oral surgeon and the primary care dentist. Experience in the Master of Oral Surgery and Implantology at Barcelona University Dental School. Med Oral Pathol Oral Cir Buccal 2008; 13: E499–504. [PubMed] [Google Scholar]
- 4.Berge TI. Third molars in Norwegian general practice. Acta Odontol Scand 1992; 50: 17–24. doi: 10.3109/00016359209012741 [DOI] [PubMed] [Google Scholar]
- 5.McArdle W, Renton T. The effects of NICE guidelines on the management of third molar teeth. Br Dent J 2012; 213: E8. doi: 10.1038/sj.bdj.2012.780 [DOI] [PubMed] [Google Scholar]
- 6.Petersen LB, Olsen KR, Christensen J, Wenzel A. Image and surgery-related costs comparing cone beam CT and panoramic imaging before removal of impacted mandibular third molars. Dentomaxillofac Radiol 2014; 43: 20140001. doi: 10.1259/dmfr.20140001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matzen LH, Christensen J, Hintze H, Schou S, Wenzel A. Influence of cone beam CT on treatment plan before surgical intervention of mandibular third molars and impact of radiographic factors on deciding on coronectomy vs surgical removal. Dentomaxillofac Radiol 2013; 42: 98870341. doi: 10.1259/dmfr/98870341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ludlow JB, Timothy R, Walker C, Hunter R, Benavides E, Samuelson DB, et al. Effective dose of dental CBCT—a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol 2015; 44: 20140197. doi: 10.1259/dmfr.20140197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suomalainen A, Kiljunen T, Käser Y, Peltola J, Kortesniemi M. Dosimetry and image quality of four dental cone beam computed tomography scanners compared with multislice computed tomography scanners. Dentomaxillofac Radiol 2009; 38: 367–78. doi: 10.1259/dmfr/15779208 [DOI] [PubMed] [Google Scholar]
- 10.StatBank Denmark; Copenhagen, Denmark. Available from: http://www.statbank.dk
- 11.Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology. Br J Radiol 2008; 81: 362–78. doi: 10.1259/bjr/01948454 [DOI] [PubMed] [Google Scholar]
- 12.Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 2012; 81: 267–71. doi: 10.1016/j.ejrad.2010.11.028 [DOI] [PubMed] [Google Scholar]
- 13.Wenzel A. Radiographic display of carious lesions and cavitation in approximal surfaces: advantages and drawbacks of conventional and advanced modalities. Acta Odontol Scand 2014; 72: 251–64. doi: 10.3109/00016357.2014.888757 [DOI] [PubMed] [Google Scholar]
- 14.Al-Okshi A, Lindh C, Salé H, Gunnarsson M, Rohlin M. Effective dose of cone beam CT (CBCT) of the facial skeleton: a systematic review. Br J Radiol 2015; 88: 20140658. doi: 10.1259/bjr.20140658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.SEDENTEXCT. Guidelines on CBCT for dental and maxillofacial radiology. Available from: http://www.sedentexct.eu
- 16.GRADE Guidelines. Available from: http://www.gradeworkinggroup.org
- 17.Matzen LH, Wenzel A. Efficacy of CBCT for assessment of impacted mandibular third molars: a review—based on a hierarchical model of evidence. Dentomaxillofac Radiol 2014; 43: 20140189. doi: 10.1259/dmfr.20140189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Council of Radiation Protection and Measurements (US). Report no. 160-ionizing radiation exposure of the population of the United States 2009. Bethesda, MD: National Council of Radiation Protection and Measurement.
- 19.NICE Guidelines; London, UK. Available from: https://www.nice.org.uk
- 20.Scottish Intercollegiate Guidelines Network (SIGN); Edinburgh, UK. Available from: http://www.sign.ac.uk/
- 21.Cunha-Cruz J, Rothen M, Spiekerman C, Drangsholt M, McClellan L, Huang GJ. Recommendations for third molar removal: a practice-based cohort study. Am J Public Health 2014; 104: 735–43. doi: 10.2105/AJPH.2013.301652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matzen LH, Petersen LB, Vaeth M, Wenzel A. Radiographic examination before surgical intervention of mandibular third molars among randomly selected general dental clinics. EADMFR 2014 (Abstr OP7B). [DOI] [PMC free article] [PubMed]