Abstract
Objectives:
Recently, studies have performed three-dimensional analyses of upper airways in children. However, there was a lack of airway delineation according to anatomical boundaries and/or easily mobile soft-tissue landmarks were used. The aim of the present study was to define new upper airway margins in children on CBCT according to anatomical bony landmarks and to validate the method.
Methods:
25 scans were randomly selected from a larger database containing CBCT scans of children prior to orthodontic treatment (14 girls and 11 boys; mean age, 10.9 ± 2.5 years). Scans were evaluated by two observers. Specific head positioning and virtual orientation protocols were adopted and greyscale thresholding was established for each patient. Volume and minimum cross-sectional area of the oropharynx were calculated. Intra- and interobserver reliability were assessed by reassessment of the CBCTs 2 weeks later.
Results:
The new airway margins were defined superiorly by a line passing through the palatal plane (anterior nasal spine to posterior nasal spine) extending to the posterior wall of the pharynx, inferiorly by a line passing from the anterosuperior edge of C4 to menton, anteriorly by a line passing from the soft palate to menton, posteriorly and laterally by the respective pharyngeal walls. Method error for airway volume and minimal cross-sectional area was ≤2.00%, and intra- and interobserver reliability ranged from 0.99 to 1.00.
Conclusions:
The proposed protocol utilizes easily identifiable bony landmarks to delineate the upper airway on cone beam scans of children and was found to be reliable and reproducible.
Keywords: upper airway, children, cone beam computed tomography, validation
Introduction
Increased interest in upper airway dimensions and morphology over the past few decades can be attributed to the appreciation that upper airway configuration is associated with sleep-disordered breathing (SDB) as well as its general relationship to craniofacial morphology.1,2 The upper airway volume and minimal cross-sectional area are significantly smaller in children with SDB and tend to be narrower laterally than in children without sleep disorders.3–6 Early diagnosis of SDB, or potential associations of SDB, is essential to encourage normal facial development.7,8 Reduced pharyngeal dimensions established early in life could potentially pre-dispose to later development of SDB or even obstructive sleep apnoea,9 as soft-tissue changes related to ageing, obesity or genetic background further reduce oropharyngeal patency.10
Previously, most studies that assessed the upper airway were based on lateral cephalometry as it was part of standard records for orthodontic treatment planning. Although a wealth of information was obtained, lateral cephalograms are of limited use for detailed airway analysis. They provide two-dimensional information (height and depth) of a three-dimensional structure, therefore restricting accurate assessment of the complexity and size of these structures. The axial plane, which is not visualized on a lateral cephalogram, is also a physiologically relevant plane because it is perpendicular to airflow.11,12 Previous studies that relied on two-dimensional cephalometry to assess upper airway dimensions were limited to drawing major conclusions from the narrowest anteroposterior sections in the airway. Measuring the narrowest constriction in a two-dimensional image may not adequately represent the spatial relationship of the associated structures in all three dimensions.13
CBCT has become an unprecedented diagnostic method to analyse the airway in all three planes.1 CBCT is capable of defining the boundaries between soft tissue and empty spaces (air) accurately.14 Furthermore, CBCT provides excellent hard-tissue detail (bone and teeth), and anatomical landmarks are easily identified without superimposition or distortion.15 Magnification is negligible with isotropic resolution and a 1 : 1 ratio in all three planes.16 Its advantages over medical CT include reduced radiation dose to the patient, lower cost and the ability to scan the patient in an upright position, which is recommended for baseline assessment of upper airway morphology and dimensions.1 However, medical CT demonstrates better soft-tissue contrast and detail than does CBCT.17
Recently, studies have performed three-dimensional analyses of upper airways in healthy children or included healthy children as a control18–27 (Table 1). However, there was a lack of airway delineation according to anatomical boundaries in children,18–20,24–27 and/or easily mobile soft-tissue landmarks were used.21,22 Furthermore, anterior or posterior anatomical margins were generally not described (Table 1). CBCT is a low-contrast imaging medium, which can only adequately differentiate between considerably different radiographic densities, such as air and soft tissue, and soft tissue and the bone. However, soft-tissue contrast is poor.14,17,28–30 Anatomically, the airway is surrounded by soft tissue of varying thickness. Radiographically, the lateral and posterior pharyngeal walls are easily identifiable. By contrast, anteriorly, superiorly and inferiorly, differentiation of the pharyngeal airway is much more complicated owing to the close association of very mobile soft tissue. However, hard-tissue points are easily identifiable and can be used to develop margins that approximate the soft-tissue boundaries.
Table 1.
Previous CBCT studies on anatomical landmarks that included oropharyngeal assessment in healthy children
| Study | Anatomical landmarks |
|||
|---|---|---|---|---|
| Superior | Inferior | Anterior | Posterior | |
| El and Palomo18–20 | Palatal plane (ANS–PNS) and extending to posterior wall of the pharynx | Plane parallel to palatal plane that passes from the most antero-inferior point of the second cervical vertebrae | – | – |
| Alves et al21,22 | Edge of the hard palate to the posterior of the pharynx (parallel to Frankfurt plane) | Tip of the epiglottis on a plane parallel to Frankfurt plane | – | – |
| Schendel et al23 | PNS | Anterosuperior edge of C4, which is generally consistent with the position of the epiglottis | – | – |
| Chiang et al24 | Palatal plane | Lowermost border of C4 | ||
| Claudino et al26 | Palatal plane extended to the posterior pharyngeal wall | Plane parallel to the palatal lane that intersected the lower and the most anterior point of the C4 | – | – |
| Diwakar et al25 | Line joining the ANS–PNS and extending to the posterior pharyngeal wall | Line parallel to the ANS–PNS plane, passing through the antero-inferior border of the second cervical vertebrae | – | – |
| Celikoglu et al27 | A plane perpendicular to the sagittal plane that includes the PNS and the lower medial border of the first cervical vertebrae | Plane tangent to the most caudal medial projection of the third cervical vertebra perpendicular to the sagittal plane | A vertical plane through the point (the intersection of the vertical plane from sella to nasion–basion plane) to the sagittal plane at the lowest border of the vomer | Posterior wall of the pharynx |
ANS, anterior nasal spine; C4, the fourth cervical vertebrae; PNS, posterior nasal spine.
Studies in adults have demonstrated that the use of CBCT in evaluation of the upper airway was accurate and reliable.1,29,31 However, reliability assessments of various upper airway margins in young children have not yet been performed. Differences in upper airway assessment exist between adults and children, as anatomically structures vary with growth and development.32–34 A standardized, consistent, reproducible method has not yet been proposed for three-dimensional airway analysis in children.
Therefore, the aims of the present study were (1) to define new upper airway margins in children assessed on CBCT and (2) to validate the new upper airway margins.
Methods and materials
25 CBCT scans of healthy children, 14 girls and 11 boys, aged 8–16 years (mean age, 10.9 ± 2.5 years) obtained prior to the commencement of orthodontic treatment were assessed for this study. The scans were randomly selected from a database consisting of all patients who attended one private practice in Victoria, Australia, for orthodontic treatment between January 2011 and July 2014. Inclusion criteria were healthy children between 8 and 16 years prior to the commencement of orthodontic treatment who had complete imaging of the cranial base, maxilla, mandible, the first four cervical vertebrae (C1–C4) and the associated airway. The exclusion criteria were previous orthodontic treatment and/or orthognathic surgery; previous adeno-tonsillectomy; known syndromal conditions; presence of pathology detectable along the upper airway; history of obstructive sleep apnoea; movement artefacts and swallowing during scan acquisition. The experimental protocol used in the present study was approved by the James Cook University Human Research Ethics Committee (H5115) as part of a larger research thesis.
Scan protocol
All patients were imaged in the same i-CAT® Next Generation Cone Beam CT machine (Imaging Sciences International, Hatfield, PA) by the same operator, as part of their dental and orthodontic assessment prior to treatment. All the images were taken in a standardized sitting position: patients were restrained using a headrest and velcro head strap; the chin rest was not used to allow for the patient's head to be positioned so that Frankfurt horizontal was parallel to the floor. Patients were instructed to close into centric occlusion, relax their tongue and lips, and to breathe gently and not swallow or move during the acquisition. A standardized protocol was used: 120 kV; 5 mA; 0.3 mm of voxel resolution, 8.9 s scan time, 13 cm (height) × 16 cm (diameter) scan volume. All CBCTs were reviewed by a dento-maxillofacial radiologist (RD) to ensure no significant pathology was identified and that all inclusion criteria were met.
Airway assessment
The digital imaging and communications in medicine data were processed using Dolphin Imaging software v. 11.5 (Dolphin Imaging and Management Solutions, Chatsworth, CA). After training and calibration by the supervisor (LS), all digital imaging and communications in medicine data were evaluated separately by the principal investigator (SA) and another observer (YA) to determine the interobserver reliability. In addition, each patient was reassessed separately by each investigator 2 weeks later to determine the intraobserver reliability and the method error. Therefore, the 25 scans were measured twice by each investigator. The airway was assessed according to the following protocol.
First the scan was reorientated in three planes:
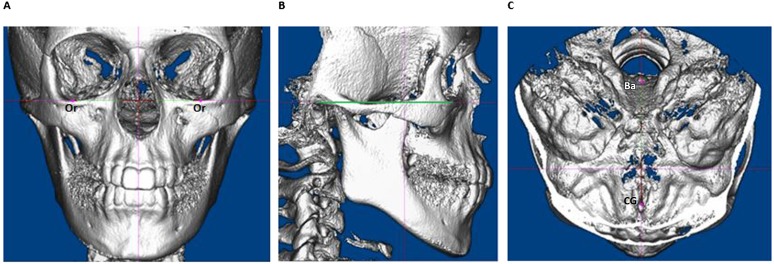
• coronal view—so that the most inferior point on the infraorbital margin (orbitale) of both sides lies on the same horizontal plane (Figure 1a)
• sagittal plane—so that the Frankfort plane (line joining the most superior point on the external auditory meatus to the infraorbital margin) is horizontal (Figure 1b)
• axial plane—with the patient facing down (endocranial view), so that a line through the crista galli and the midpoint on the anterior margin of foramen magnum (basion) is vertical. With the patient facing up (exocranial view), it was ensured that no transverse rotation of the mandible or the zygomatic arches were present (Figure 1c).
Figure 1.
Orientation of the CBCT scan. (a) Coronal plane; (b) sagittal plane, Frankfort plane is indicated by the green line; (c) axial plane. Ba, basion; CG, crista galli; Or, orbitale. For colour images please see online.
Definitions of the new upper airway margins were then proposed according to anatomical margins of the upper airway in children35–37 and previous CBCT studies of children18–27 (Table 1). The margins were outlined on the mid-sagittal plane. The mid-sagittal plane was identified as the sagittal slice that included the anterior nasal spine and incisive canal and confirmed visually using the three-dimensional volume rendered image. To ensure the anterior boundary was completely in soft issue, the mid-sagittal soft-palate tip point was identified and confirmed on either side (left and right) on the sagittal slices where the incisive canal initially reached its minimal width.
The process of airway segmentation was systemized as follows:
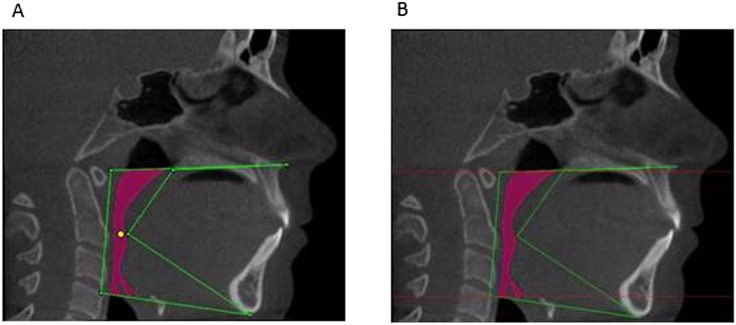
• The “seed point” was defined as a virtual marker for the region of interest demarcation and was placed centrally in the airway region immediately posterior to the soft-palate tip (Figure 2a) to facilitate automated segmentation of the airway based on greyscale values.
• The most appropriate threshold value for each patient was then determined. After the sagittal view was maximized as much as possible while ensuring visualization of all previously determined margins, the software-determined threshold value was manually adjusted for each data set (operator-adjusted threshold) until the airway volume (pink area, Figure 2) adequately depicted the airway–soft-tissue interface. Other views were then checked to ensure that an adequate threshold was used and that there was no incorrect extension of airway segmentation into the soft tissues.
Figure 2.
Upper airway assessment. (a) Margins for delineation of the upper airway. Green lines indicate the margins used to delineate the airway according to Table 2. The yellow point represents the seed point. (b) Margins for minimal cross-sectional area. The red lines indicate the upper and lower limits used to measure the minimal cross-sectional area. For colour images please see online.
The airway volume (mm3) was then automatically calculated by the software within the defined margins.
For calculation of minimum cross-sectional area, the upper and lower limits (red lines, Figure 2b) were then set within the previously defined margins that included both anterior and posterior margins of the airway. This was to ensure that the entire area was calculated and not a partial section created by the difference in airway boundary for volume calculation and the plane of area calculation. Within the defined margins, the software automatically calculated the minimum cross-sectional area (mm2).
Statistical analyses
The systematic error between the two sets of data was assessed by paired t-test. The method errors were calculated according to Dahlberg's formula38 and the Houston39 reliability coefficient. Intraclass correlation coefficient (ICC) according to Donner and Koval40 was calculated to assess intraobserver reliability as well as interobserver agreement between the measurements of airway volume and minimal cross-sectional area. The results from the tests were considered to be significant at p-values <0.05. All statistical analyses were performed using SPSS® Statistical Package for Social Sciences, v. 20.00 (SPSS Inc., Chicago, IL).
Results
The following new airway margins were defined (Table 2, Figure 2):
• superior: the line passing from the palatal plane (anterior nasal spine to posterior nasal spine) extending to the posterior wall of the pharynx
• inferior: line passing from the anterosuperior edge of the fourth cervical vertebra (C4) to menton
• anterior: line passing from the soft palate to menton
• posterior: posterior wall of the pharynx
• lateral: respective pharyngeal walls.
Table 2.
Anatomical and technical limits of the upper airway
| Limit | Anatomical | Technical |
|---|---|---|
| Superior | Hard and soft palate | The line passing from the palatal plane (ANS to PNS) extending to the posterior wall of the pharynx |
| Inferior | Vallecula (plane of the hyoid bone; base of the epiglottis) | Line passing from the anterosuperior edge of C4 to menton |
| Anterior | Circumvallate papillae and the oropharyngeal isthmus | Line passing from the soft palate to menton |
| Posterior | Respective pharyngeal walls | Posterior wall of the pharynx |
| Laterally | Respective pharyngeal walls | Respective pharyngeal walls |
ANS, anterior nasal spine; C4, the fourth cervical vertebrae; PNS, posterior nasal spine.
No systematic error was found between the two sets of data, and the method errors for airway volume and the minimal cross-section area were <2.00% (Table 3).
Table 3.
Method error, intra- and interobserver reliability for proposed protocol
| Reliability test | Airway volume (mm3) |
Minimal cross-sectional area (mm2) |
||
|---|---|---|---|---|
| Observer 1 | Observer 2 | Observer 1 | Observer 2 | |
| Systematic error | Non | Non | Non | Non |
| Method error | 197.54 (1.90%) | 116.50 (1.10%) | 0.59 (0.46%) | 1.15 (0.89%) |
| Houston reliability coefficient | 0.99 | 1.00 | 1.00 | 1.00 |
| Intra-class correlation | 1.00 | 1.00 | 1.00 | 1.00 |
| 1.00 | 1.00 | |||
The Houston reliability coefficient and ICC for both intra- and interobserver reliability was 0.99–1.00 for the airway volume and the minimal cross-section area (Table 3).
The airway volume ranged from 5217.7 to 23,519.3 mm3 (mean, 10,398.5 ± 5372.0 mm3), and the minimal cross-sectional area ranged from 39.5 to 348.5 mm2 (mean, 129.3 ± 83.6 mm2).
Discussion
The oropharynx extends from the hard and soft palate superiorly to the vallecula inferiorly (plane of the hyoid bone; base of epiglottis).35 It is bordered anteriorly by the circumvallate papillae and the oropharyngeal isthmus and posteriorly by a muscular wall made up of the superior, middle and inferior constrictor muscles that lie in front of the cervical spine. The lateral pharyngeal walls are complicated and consist of numerous muscles (the pharyngeal constrictors, hypoglossus, styloglossus, stlylopharyngeus, palatoglossus, stylohyoid, palatopharyngeus), pharyngeal mucosa and lymphoid tissue.35–37 Radiographic assessment of the oropharynx should therefore be based on these structures to adequately encompass the entire area of interest as has been performed in the newly proposed protocol of this study.
Furthermore, airway dimensions are influenced by dynamic variables such as respiration state of the patient,1,3 head posture1,41,42 and mobility of the soft tissues.1,3 Patient positioning for the scan is very important. The patient can either be scanned in a vertical seated or upright position or in a supine position, depending on the CBCT apparatus. Data gathered from patients sitting or standing cannot be adequately compared with those obtained with the individual in the supine position owing to the gravitational effects on oropharyngeal structures.13 The upper airway and associated soft tissues morphologically change as a result of gravity and posture.41–43 Because the upright position is closer to the natural head posture and is recommended for baseline assessment of upper airway morphology and dimensions,1 the scans in the present study were obtained from patients scanned in a vertical seated position.
Radiographically, the lateral and posterior airway margins are easily identifiable as CBCT scans demonstrate adequate contrast between the soft tissue (muscle) and pharyngeal air space to allow for differentiation.14 Therefore, in the present study, these anatomical structures were used to delineate the corresponding margins. This is in agreement with a previous study where the posterior wall of the pharynx was used to delineate the posterior airway margin.27
Anteriorly, superiorly and inferiorly, identification of the pharyngeal airway margins is much more complicated owing to the close association with mobile soft tissues.30,36,37 However, hard-tissue points that can be used to develop margins that approximated the soft-tissue boundaries are easily identifiable (Table 2). Furthermore, the hyoid bone and soft tissue of the airway can easily move depending on the respiration state of the patient, which can be an issue with children, especially with longer scan acquisition times, sometimes resulting in movement artefact.44,45 In the present study, the superior margin was defined according to a plane through the anterior nasal spine and the posterior nasal spine. This is in agreement with previous studies.18–20,24–26
As patients are in centric occlusion during scan acquisition, a plane from the anterosuperior point of C4 to the most inferior point of the mandibular symphysis (menton) was used in this study to demarcate the inferior margin. The plane represents the anatomical inferior boundary of the oropharyngeal airway23 as well as being approximately parallel to the palatal plane.
In the present study, the soft palate was used to demarcate the anterior limit of the airway. A soft-tissue landmark had to be used for this margin because no hard-tissue landmarks could be identified to delineate the airway according to anatomical limits. In a previous study that validated delineation of the airway in adults,46 the anterior limit was the frontal plane perpendicular to Frankfurt horizontal passing through the posterior nasal spine. However, by that method, parts of the oral cavity were included in some measurements. The landmarks used in the present study have been shown to pass through the structures that anatomically border the oropharynx in children.35
To our knowledge, the reproducibility of upper airway margins in children has not previously been reported in the literature. However, a few studies have assessed the reliability of different protocols to delineate the upper airway in adults.46–48 Very high reproducibility was found in all three studies in relation to airway volume assessment, with intra- and interexaminer ICC values of 0.99 reported in all studies, even with examiners of different backgrounds.48 This is in agreement with the present study were the ICC value was 1.00. However, there was greater variation in the reliability of minimal oropharyngeal cross-sectional area measurements in previous adult studies. Intraexaminer ICC values ranged from 0.78 to 0.99, and interexaminer values ranged from 0.83 to 0.98.46–48 In the present study, very high intra- and interobserver reliability for calculation of the minimal cross-sectional area was observed with ICC values of 1.00.
Previously, only a few studies had calculated the method error of the upper airway margins in adults in various ways.46,48 Guijarro-Martínez and Swennen46 calculated relative errors ranging from 13.45% to 15.92% for minimal oropharyngeal cross-sectional area measurements and ranging from 1.03% to 1.53% for oropharyngeal volume measurements, depending on the observer. Mattos et al48 determined measurement errors by the ratio of the absolute mean difference to the mean measurement value. This ranged from 2.7% to 6.4% for intra- and interobserver measurements of minimal cross-sectional area and volume. In the present study, no systematic error was found, and the method errors were ≤2.00% according to Dahlberg's formula,38 which is considered a standard calculation for the method error of cephalometric measurements.
The results of the study indicate that the newly proposed protocol for three-dimensional airway analysis in children is accurate, reliable and reproducible. The findings may be owing to the use of easily identifiable hard-tissue landmarks and the limited use of soft-tissue landmarks.
Conclusion
A new method for upper airway delineation on cone beam scans of children for the assessment of upper airway morphology has been proposed and was found to be reliable and reproducible. This has the potential to standardize upper airway analysis in children and permit comparisons among future studies.
Acknowledgments
Acknowledgments
We would like to acknowledge the assistance of Professor Eliyathamby A Selvanathan from the Griffith University (Brisbane, QLD) for his statistical assistance.
Contributor Information
S Anandarajah, Email: seerone.anandarajah@gmail.com.
Y Abdalla, Email: yousef.abdalla@jcu.edu.au.
R Dudhia, Email: rdudhia.dmfr@gmail.com.
L Sonnesen, Email: alson@sund.ku.dk.
References
- 1.Guijarro-Martínez R, Swennen GR. Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg 2011; 40: 1227–37. doi: 10.1016/j.ijom.2011.06.017 [DOI] [PubMed] [Google Scholar]
- 2.Flores-Mir C, Korayem M, Heo G, Witmans M, Major MP, Major PW. Craniofacial morphological characteristics in children with obstructive sleep apnea syndrome: a systematic review and meta-analysis. J Am Dent Assoc 2013; 144: 269–77. doi: 10.14219/jada.archive.2013.0113 [DOI] [PubMed] [Google Scholar]
- 3.Schwab RJ, Gefter WB, Hoffman EA, Gupta KB, Pack AI. Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am Rev Respir Dis 1993; 148: 1385–400. doi: 10.1164/ajrccm/148.5.1385 [DOI] [PubMed] [Google Scholar]
- 4.Schwab RJ, Gupta KB, Gefter WB, Metzger LJ, Hoffman EA, Pack AI. Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med 1995; 152: 1673–89. doi: 10.1164/ajrccm.152.5.7582313 [DOI] [PubMed] [Google Scholar]
- 5.Isono S, Shimada A, Utsugi M, Konno A, Nishino T. Comparison of static mechanical properties of the passive pharynx between normal children and children with sleep-disordered breathing. Am J Respir Crit Care Med 1998; 157: 1204–12. doi: 10.1164/ajrccm.157.4.9702042 [DOI] [PubMed] [Google Scholar]
- 6.Fregosi RF, Quan SF, Kaemingk KL, Morgan WJ, Goodwin JL, Cabrera R, et al. Sleep-disordered breathing, pharyngeal size and soft tissue anatomy in children. J Appl Physiol (1985) 2003; 95: 2030–8. doi: 10.1152/japplphysiol.00293.2003 [DOI] [PubMed] [Google Scholar]
- 7.Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2009; 135: 468–79. doi: 10.1016/j.ajodo.2007.04.043 [DOI] [PubMed] [Google Scholar]
- 8.Peltomäki T. The effect of mode of breathing on craniofacial growth–revisited. Eur J Orthod 2007; 29: 426–9. [DOI] [PubMed] [Google Scholar]
- 9.Papaioannou G, Kambas I, Tsaoussoglou M, Panaghiotopoulou-Gartagani P, Chrousos G, Kaditis AG. Age-dependent changes in the size of adenotonsillar tissue in childhood: implications for sleep-disordered breathing. J Pediatr 2013; 162: 269–74. doi: 10.1016/j.jpeds.2012.07.041 [DOI] [PubMed] [Google Scholar]
- 10.Martin SE, Mathur R, Marshall I, Douglas NJ. The effect of age, sex, obesity and posture on upper airway size. Eur Respir J 1997; 10: 2087–90. doi: 10.1183/09031936.97.10092087 [DOI] [PubMed] [Google Scholar]
- 11.Abramson ZR, Susarla S, Tagoni JR, Kaban L. Three-dimensional computed tomographic analysis of airway anatomy. J Oral Maxillofac Surg 2010; 68: 363–71. doi: 10.1016/j.joms.2009.09.086 [DOI] [PubMed] [Google Scholar]
- 12.Isono S, Morrison DL, Launois SH, Feroah TR, Whitelaw WA, Remmers JE. Static mechanics of the velopharynx of patients with obstructive sleep apnea. J Appl Physiol (1985) 1993; 75: 148–54. [DOI] [PubMed] [Google Scholar]
- 13.Sutthiprapaporn P, Tanimoto K, Ohtsuka M, Nagasaki T, Iida Y, Katsumata A. Positional changes of oropharyngeal structures due to gravity in the upright and supine positions. Dentomaxillofac Radiol 2008; 37: 130–5. doi: 10.1259/dmfr/31005700 [DOI] [PubMed] [Google Scholar]
- 14.Yamashina A, Tanimoto K, Sutthiprapaporn P, Hayakawa Y. The reliability of computed tomography (CT) values and dimensional measurements of the oropharyngeal region using cone beam CT: comparison with multidetector CT. Dentomaxillofac Radiol 2008; 37: 245–51. doi: 10.1259/dmfr/45926904 [DOI] [PubMed] [Google Scholar]
- 15.Mah JK, Yi L, Huang RC, Choo H. Advanced applications of cone beam computed tomography in orthodontics. Semin Orthod 2011; 17: 57–71. doi: 10.1053/j.sodo.2010.08.011 [DOI] [Google Scholar]
- 16.Lagravère MO, Gordon JM, Flores-Mir C, Carey J, Heo G, Major PW. Cranial base foramen location accuracy and reliability in cone-beam computerized tomography. Am J Orthod Dentofacial Orthop 2011; 139: e203–10. doi: 10.1016/j.ajodo.2009.06.027 [DOI] [PubMed] [Google Scholar]
- 17.Miracle AC, Mukherji SK. Conebeam CT of the head and neck, part 2: clinical applications. AJNR Am J Neuroradiol 2009; 30: 1285–92. doi: 10.3174/ajnr.A1654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El H, Palomo JM. Airway volume for different dentofacial skeletal patterns. Am J Orthod Dentofacial Orthop 2011; 139: e511–21. doi: 10.1016/j.ajodo.2011.02.015 [DOI] [PubMed] [Google Scholar]
- 19.El H, Palomo JM. An airway study of different maxillary and mandibular sagittal positions. Eur J Orthod 2013; 35: 262–70. doi: 10.1093/ejo/cjr114 [DOI] [PubMed] [Google Scholar]
- 20.El H, Palomo JM. Three-dimensional evaluation of upper airway following rapid maxillary expansion: a CBCT study. Angle Orthod 2014; 84: 265–73. doi: 10.2319/012313-71.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alves M, Jr, Baratieri C, Nojima LI, Nojima MC, Ruellas AC. Three-dimensional assessment of pharyngeal airway in nasal- and mouth-breathing children. Int J Pediatr Otorhinolaryngol 2011; 75: 1195–9. doi: 10.1016/j.ijporl.2011.06.019 [DOI] [PubMed] [Google Scholar]
- 22.Alves M, Jr, Franzotti ES, Baratieri C, Nunes LK, Nojima LI, Ruellas AC. Evaluation of pharyngeal airway space amongst different skeletal patterns. Int J Oral Maxillofac Surg 2012; 41: 814–19. doi: 10.1016/j.ijom.2012.01.015 [DOI] [PubMed] [Google Scholar]
- 23.Schendel SA, Jacobson R, Khalessi S. Airway growth and development: a computerized 3-dimensional analysis. J Oral Maxillofac Surg 2012; 70: 2174–83. doi: 10.1016/j.joms.2011.10.013 [DOI] [PubMed] [Google Scholar]
- 24.Chiang CC, Jeffres MN, Miller A, Hatcher DC. Three-dimensional airway evaluation in 387 subjects from one university orthodontic clinic using cone beam computed tomography. Angle Orthod 2012; 82: 985–92. doi: 10.2319/122811-801.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diwakar R, Sidhu MS, Jain S, Grover S, Prabhakar M. Three-dimensional evaluation of pharyngeal airway in complete unilateral cleft individuals and normally growing individuals using cone beam computed tomography. Cleft Palate Craniofac J July 2014. Epub ahead of print. doi: 10.1597/13-292 [DOI] [PubMed] [Google Scholar]
- 26.Claudino LV, Mattos CT, Ruellas AC, Sant' Anna EF. Pharyngeal airway characterization in adolescents related to facial skeletal pattern: a preliminary study. Am J Orthod Dentofacial Orthop 2013; 143: 799–809. doi: 10.1016/j.ajodo.2013.01.015 [DOI] [PubMed] [Google Scholar]
- 27.Celikoglu M, Ucar FI, Sekerci AE, Buyuk SK, Ersoz M, Sisman Y. Assessment of pharyngeal airway volume in adolescent patients affected by bilateral cleft lip and palate using cone beam computed tomography. Angle Orthod 2014; 84: 995–1001. doi: 10.2319/121913-930.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Angelopoulos C. Cone beam tomographic imaging anatomy of the maxillofacial region. Dent Clin North Am 2008; 52: 731–52. doi: 10.1016/j.cden.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 29.Lenza MG, Lenza MM, Dalstra M, Melsen B, Cattaneo PM. An analysis of different approaches to the assessment of upper airway morphology: a CBCT study. Orthod Craniofac Res 2010; 13: 96–105. doi: 10.1111/j.1601-6343.2010.01482.x [DOI] [PubMed] [Google Scholar]
- 30.De Vos W, Casselman J, Swennen GR. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. Int J Oral Maxillofac Surg 2009; 38: 609–25. doi: 10.1016/j.ijom.2009.02.028 [DOI] [PubMed] [Google Scholar]
- 31.Ghoneima A, Kula K. Accuracy and reliability of cone-beam computed tomography for airway volume analysis. Eur J Orthod 2013; 35: 256–61. doi: 10.1093/ejo/cjr099 [DOI] [PubMed] [Google Scholar]
- 32.Tourné LP. Growth of the pharynx and its physiologic implications. Am J Orthod Dentofacial Orthop 1991; 99: 129–39. doi: 10.1016/0889-5406(91)70115-d [DOI] [PubMed] [Google Scholar]
- 33.King EW. A roentgenographic study of pharyngeal growth. Angle Orthod 1952; 22: 23–37. [Google Scholar]
- 34.Bench RW. Growth of the cervical vertebrae as related to tongue, face, and denture behavior. Am J Orthod 1963; 49: 183–214. doi: 10.1016/0002-9416(63)90050-2 [DOI] [Google Scholar]
- 35.Wadhawan N, Kharbanda OP. An airway study of different maxillary and mandibular sagittal positions. Eur J Orthod 2013; 35: 271. doi: 10.1093/ejo/cjs008 [DOI] [PubMed] [Google Scholar]
- 36.Standring S. Gray's anatomy: the anatomical basis of clinical practice. 40th edn. Edinburgh, UK: Elsevier; 2008. [Google Scholar]
- 37.Norton NS, Netter FH. Netter's head and neck anatomy for dentistry. Philadelphia, PA: Elsevier; 2007. [Google Scholar]
- 38.Dahlberg G. Statistical methods for medical and biological students. New York, NY: Interscience Publications, 1940. [Google Scholar]
- 39.Houston WJ. The analysis of errors in orthodontic measurements. Am J Orthod 1983; 83: 382–90. doi: 10.1016/0002-9416(83)90322-6 [DOI] [PubMed] [Google Scholar]
- 40.Donner A, Koval JJ. The estimation of intraclass correlation in the analysis of family data. Biometrics 1980; 36: 19–25. doi: 10.2307/2530491 [DOI] [PubMed] [Google Scholar]
- 41.Muto T, Takeda S, Kanazawa M, Yamazaki A, Fujiwara Y, Mizoguchi I. The effect of head posture on the pharyngeal airway space (PAS). Int J Oral Maxillofac Surg 2002; 31: 579–83. doi: 10.1054/ijom.2002.0279 [DOI] [PubMed] [Google Scholar]
- 42.Muto T, Yamazaki A, Takeda S, Kawakami J, Tsuji Y, Shibata T, et al. Relationship between the pharyngeal airway space and craniofacial morphology, taking into account head posture. Int J Oral Maxillofac Surg 2006; 35: 132–6. doi: 10.1016/j.ijom.2005.04.022 [DOI] [PubMed] [Google Scholar]
- 43.Hellsing E. Changes in the pharyngeal airway in relation to extension of the head. Eur J Orthod 1989; 11: 359–65. [DOI] [PubMed] [Google Scholar]
- 44.Hanzelka T, Dusek J, Ocasek F, Kucera J, Sedy J, Benes J, et al. Movement of the patient and the cone beam computed tomography scanner: objectives and possible solutions. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116: 769–73. doi: 10.1016/j.oooo.2013.08.010 [DOI] [PubMed] [Google Scholar]
- 45.Hamidaddin A, Sarkis T, Lee R, Nummikoski P. A breath away from high resolution: patient movement during cone-beam computed tomography exposure. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: e49. doi: 10.1016/j.tripleo.2006.09.032 [DOI] [Google Scholar]
- 46.Guijarro-Martínez R, Swennen GR. Three-dimensional cone beam computed tomography definition of the anatomical subregions of the upper airway: a validation study. Int J Oral Maxillofac Surg 2013; 42: 1140–9. doi: 10.1016/j.ijom.2013.03.007 [DOI] [PubMed] [Google Scholar]
- 47.Souza KR, Oltramari-Navarro PV, Navarro Rde L, Conti AC, Almeida MR. Reliability of a method to conduct upper airway analysis in cone-beam computed tomography. Braz Oral Res 2013; 27: 48–54. [DOI] [PubMed] [Google Scholar]
- 48.Mattos CT, Cruz CV, da Matta TC, Pereira Lde A, Solon-de-Mello Pde A, Ruellas AC, et al. Reliability of upper airway linear, area, and volumetric measurements in cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2014; 145: 188–97. doi: 10.1016/j.ajodo.2013.10.013 [DOI] [PubMed] [Google Scholar]