Abstract
Objective:
To determine the performance of the spine sign in detecting lower chest abnormalities in the lateral view.
Methods:
This retrospective study included 200 patients who had undergone lateral view and CT scans of the chest within 1 week. Two radiologists independently read the lateral views, and a third radiologist, blinded to the aim of the study, read the scans. The spine sign was considered as positive if the progressive increase in lucency of the vertebral bodies was altered. Interreader agreement was calculated through k-statistics. Sensitivity, specificity, positive- and negative-predictive values, and accuracy were calculated compared with CT.
Results:
Agreements between readers ranged from 0.12 to 0.68. Positive spine sign could appear in two ways: absent or inversed progressive increase in lucency of the vertebral bodies. Sensitivity, specificity, positive- and negative-predictive values, and accuracy were, respectively, 60% and 70%; 64% and 84%; 91% and 97%; 19% and 29%; and 61% and 72% for each reader (p-value ranging from 0.026 to 0.196). Abnormalities most frequently associated with positive spine sign were plate-like atelectasis, ground-glass opacity, pleural effusion and consolidation.
Conclusion:
The spine sign can present as an absent or inversed progressive increase in lucency of the vertebral bodies. It has a moderate sensitivity but a good positive-predictive value, so it can be useful especially when it appears as inversed progressive increase in lucency of the vertebral bodies to detect various abnormalities usually identifiable on chest radiographs.
Advances in knowledge:
On lateral chest radiographs, the spine sign is useful to detect lower chest abnormalities and is related to various underlying abnormalities and is, per se, non-specific.
On lateral chest view obtained in normal subjects, the overall posterior opacity tends to decrease from the level of the upper thoracic spine to that of the diaphragm.1,2 The “spine sign” is any alteration in this typical pattern and is suggestive of pathology in the lower part of the chest.3 While commonly used, the diagnostic performance of this sign for detecting lower lobe abnormalities remains unknown. The aims of our study were therefore to determine its sensitivity, specificity, positive- and negative-predictive values; to determine the accuracy of the spine sign compared with CT as a method of reference; and to characterize its associated lesions.
METHODS AND MATERIALS
The ethics committee of Hôpital Erasme (Brussels, Belgium) approved our research protocol and agreed to waive the need for patient-informed consent as the study was based on existing data.
Patients
200 consecutive patients who had a lateral chest view as well as a chest CT scan between November 2008 and February 2009 were retrospectively included. The mean interval between lateral views and CT was 2 days (range, 0–7 days). There was no exclusion criterion.
Image acquisition
Chest views
Left lateral views were obtained with a digital flat panel detector radiography system (Axiom Aristos FD VB 20D; Siemens Healthcare, Forchheim, Germany) with a standard technique of 81 kVp/2.5 mAs, a focus-film distance of 180 cm, without grid.
CT examination
CT scans were obtained with commercially available multidetector row scanners equipped with 16 or 64 detector rows (Sensation 16 and Sensation 64; Siemens Healthcare). Patients were examined in the supine position with both arms raised overhead during a full-inspiration breath-hold. On the 16-detector row scanner, a frontal 52 cm scout view was first obtained at 120 kVp and 50 mA, followed by a helical scan from the apex to the base of the lungs, with a 16.00 × 0.75 mm collimation, 120 kVp and 90 effective mAs. On the 64-detector row scanner, a frontal 52 cm scout view was first obtained at 120 kVp and 35 mA, followed by a helical scan from the apex to the basis of the lungs, with a 64.0 × 0.6 mm collimation, 120 kVp and 90 effective mAs. From the raw data of each acquisition, contiguous 5-mm-thick transverse sections were obtained using B60f reconstruction algorithms at a display window width of 1600 HU and a window centre of −600 HU. CT scans were obtained with or without intravenous contrast material (IOMERON® 400; Bracco, Milan, Italy) in 28 and 172 patients, respectively. We injected 120 ml of contrast material at the rate of 4 ml s−1.
Image analysis
Information that could identify the patients was removed from all images and replaced by random numbers according to tables from Fisher and Yates.4 Lateral views and CT scans were sent to a picture archiving and communication system (Carestream Healthcare IT; Rochester, NY) and loaded on a clinical workstation with a native resolution of 1600 × 1200 (RadioForce R22; Eizo Nanao Corporation, Hakusan, Japan) equipped with a 21.3-inch viewing monitor. Lateral views were independently read by a board-certified radiologist (blinded for review) with more than 20 years' experience in reading imaging of the thorax (Reader 1) and a 5-year radiology resident (blinded for review) (Reader 2). CT scans were read by a third board-certified radiologist (blinded for review) also with more than 20 years' experience in reading imaging of the thorax (Reader 3). Readers were blinded to the interpretation performed by the radiologist who had read the examinations for clinical purposes as well as to the results obtained from any other diagnostic technique (e.g. laboratory results). Readers 1 and 2 knew the aim of the study, whereas Reader 3 was blinded to the aim of the study as well as to the interpretation of two other readers.
Lateral views
Lateral views were read independently by Readers 1 and 2 without the knowledge of the CT findings. The spine sign was recorded as negative or positive. In our clinical practice, we observed that positive spine sign could have two appearances: the density of the vertebral bodies can be constant or can increase from superior to inferior, both appearances leading to an interruption in the progressive increase in lucency of the vertebral bodies. When the spine sign was read as positive, the progressive increase in lucency of the vertebral bodies was further recorded as absent or inversed. Representative examples are given in Figures 1–3. In addition, degenerative features of the thoracic spine (spondylosis deformans and intervertebral osteochondrosis),5 tortuous aorta and elevated hemidiaphragm were recorded as present or absent. The right hemidiaphragm was considered elevated if it was more than two rib spaces higher than the left hemidiaphragm, while the left hemidiaphragm was considered elevated if it was more than one rib space higher than the right hemidiaphragm.6
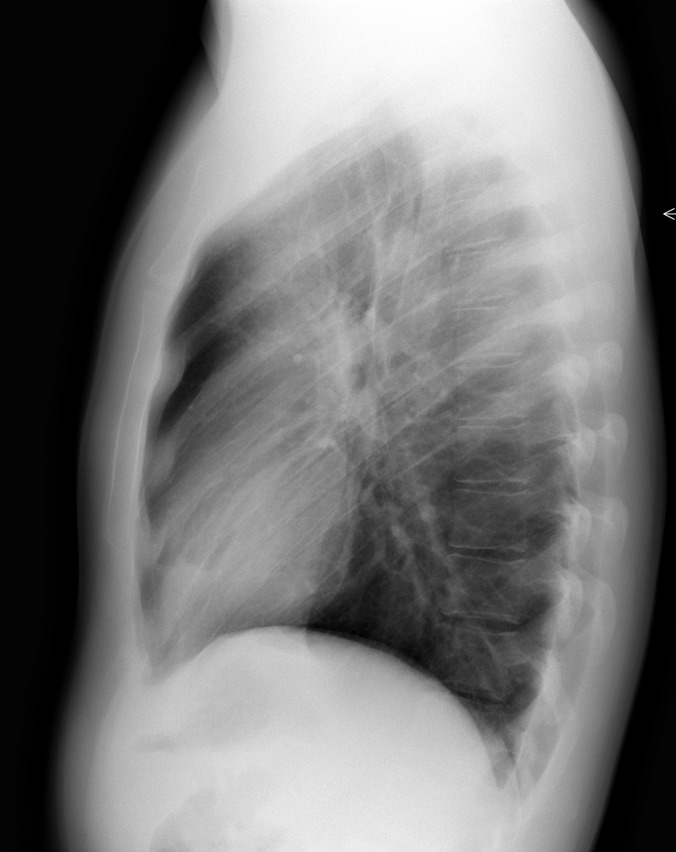
Figure 1.
Lateral chest view of a 23-year-old male showing a normal progressive increase in lucency of the vertebral bodies.
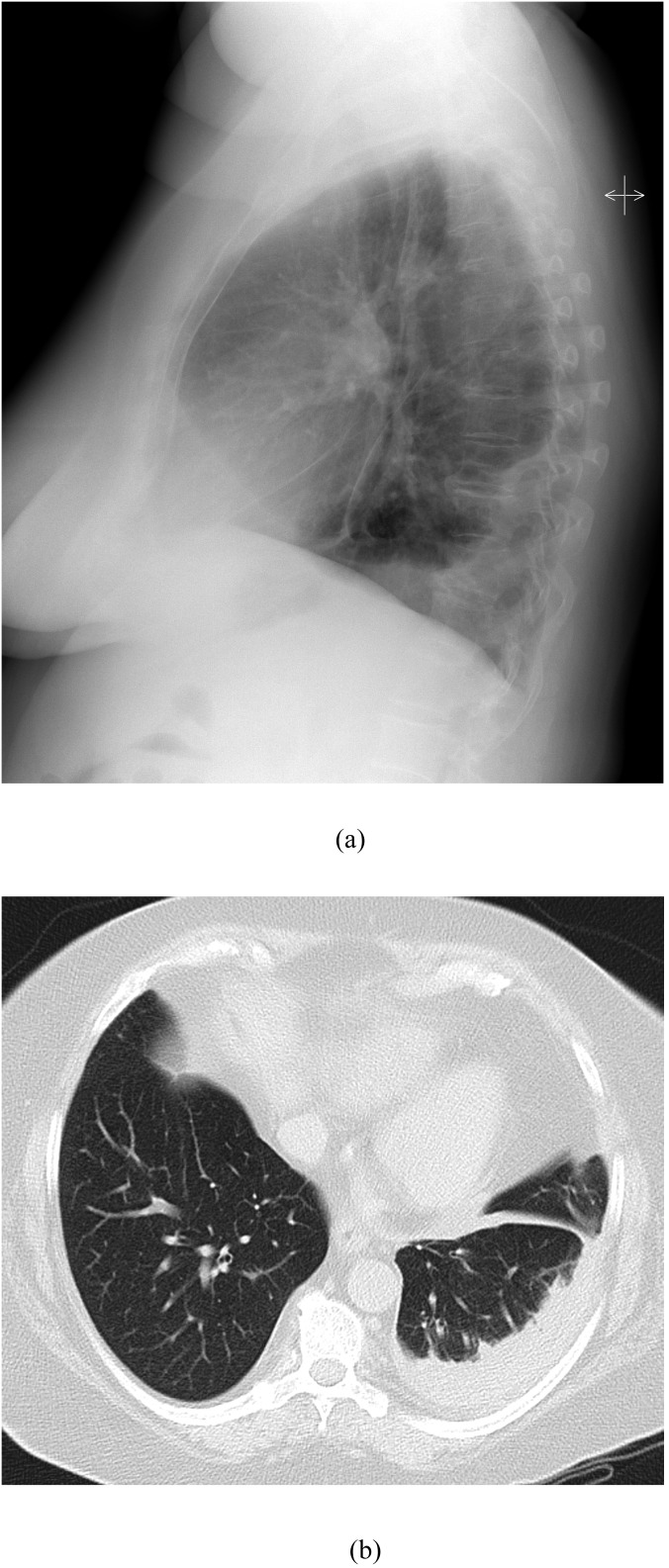
Figure 3.
Lateral chest view and CT scan of a 64-year-old female with pneumonia of the left lower lobe. (a) Lateral chest view shows the inversed progressive increase in lucency of the vertebral bodies. (b) CT scan reveals a peripheral consolidation in the left lower lobe with moderate pleural effusion.
Figure 2.
Lateral chest view and CT scan of a 60-year-old female with systemic sclerosis. (a) Lateral chest view shows the absence of the progressive increase in lucency of the vertebral bodies. (b) CT scan reveals ground-glass opacity in the lower lobes.
CT scans
Reader 3 recorded the presence of consolidation, mass, micronodules, ground-glass opacity, bronchial wall-thickening, bronchiectasis, emphysema and plate-like atelectases in the lower lobes, as defined by the glossary of terms of the Fleischner Society,7 as well as the presence of pleural effusion, pleural thickening, osteochondrosis, scoliosis and tortuous aorta.
Statistical analyses
Quantitative variables were expressed as their means ± standard deviations. Interreader agreements were investigated by calculating Cohen's κ statistics with their asymptotic standard error.8,9 The null hypothesis of no agreement between the two readers was tested, and the associated p-values were calculated. All κ values were interpreted as proposed in the literature: a κ value <0.20 indicated poor agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, good agreement; and 0.81–1.00, excellent agreement.10 Sensitivity, specificity, positive-predictive value, negative-predictive value and accuracy of the spine sign were calculated compared with CT results.
Statistical significance was set at a p-value of <0.05. The statistical software used was IBM SPSS® for Windows release 19.0 (SPSS Inc., Chicago, IL).
RESULTS
A total of 600 individual readings were performed (200 patients; 1 lateral view and 1 CT scan per patient, 2 readers for lateral views and 1 reader for CT scans). There were 80 females and 120 males (mean age, 59 years; range, 19–94 years).
Diagnostic performance
Progressive increase in lucency of the vertebral bodies was interpreted as normal, absent or inversed, respectively, by Readers 1 and 2, in 85 (42%) and 73 (37%) patients; 21 (11%) and 31 (15%) patients; and 94 (47%) and 96 (48%) patients.
The agreement between readers for normal progressive increase in lucency of the vertebral bodies (negative spine sign) was moderate (κ = 0.56). When the progressive increase in lucency of the vertebral bodies was absent (positive spine sign), the agreement between readers was poor (κ = 0.12). When the progressive increase in lucency of the vertebral bodies was inversed (positive spine sign), the agreement between readers was good (κ = 0.68).
Reader 3 interpreted the CT scans as normal in 25 patients and as abnormal in 175 patients. Compared with CT, sensitivity, specificity, positive-predictive value, negative-predictive value and accuracy of the spine sign are listed in Table 1.
Table 1.
Diagnostic performance indicators of the spine sign considered as absent or inversed progressive increase in lucency of the vertebral bodies
| Diagnostic performance indicators | Reader 1 | Reader 2 | p-value |
|---|---|---|---|
| Sensitivity | 106/175 (61%) | 123/175 (70%) | 0.072 |
| Specificity | 16/25 (64%) | 21/25 (84%) | 0.196 |
| Positive-predictive value | 106/115 (92%) | 123/127 (97%) | 0.153 |
| Negative-predictive value | 16/85 (19%) | 21/73 (29%) | 0.187 |
| Accuracy | 122/200 (61%) | 144/200 (72%) | 0.026 |
Lesions associated with spin sign
Among 175 patients with abnormal CT, 10 had a single abnormal finding (micronodules in 3 patients, ground-glass opacity in 2 patients, plate-like atelectasis in 3 patients and pleural effusion in 1 patient) and 165 patients had several abnormal CT findings. These findings consisted of consolidation in 63 patients, mass in 13 patients, micronodules in 54 patients, ground-glass opacity in 57 patients, bronchial wall thickening in 67 patients, bronchiectasis in 19 patients, plate-like atelectasis in 83 patients, pleural effusion in 76 patients and pleural thickening in 32 patients.
Among the 175 patients with abnormal CT findings, the spine sign was positive (true positive) in 106 (61%) and 123 (70%) patients, and negative (false negative) in 69 (39%) and 52 (30%) patients, respectively, by Readers 1 and 2. Frequencies of abnormalities on CT associated with false-negative and true-positive spine sign by each reader are listed in Tables 2 and 3. Among the 25 patients with normal CT, the spine sign was positive (false positive) in nine (36%) and four (16%) patients, respectively, by Readers 1 and 2. Among these patients with false-positive spine sign, degenerative features of thoracic spine, elevated hemidiaphragm and/or tortuous aorta were recorded in seven (78%) and four (100%) patients, respectively, by Reader 1 and Reader 2.
Table 2.
Frequencies of CT abnormalities in patients with false-negative spine sign
| Diagnostic performance indicators | Reader 1 | Reader 2 |
|---|---|---|
| Pleural effusion | 15 (22%) | 10 (19%) |
| Pleural thickening | 14 (20%) | 7 (13%) |
| Emphysema | 17 (25%) | 11 (21%) |
| Consolidation | 7 (10%) | 1 (2%) |
| Mass | 5 (7%) | 4 (8%) |
| Micronodule | 20 (29%) | 14 (27%) |
| Ground-glass opacity | 22 (32%) | 15 (29%) |
| Bronchiectasis | 8 (12%) | 4 (8%) |
| Bronchial thickening | 24 (35%) | 20 (38%) |
| Plate-like atelectasis | 33 (48%) | 22 (42%) |
Table 3.
Frequencies of CT abnormalities in patients with true-positive spine sign
| Diagnostic performance indicators | Reader 1 | Reader 2 |
|---|---|---|
| Pleural effusion | 61 (58%) | 66 (54%) |
| Pleural thickening | 18 (17%) | 25 (20%) |
| Emphysema | 26 (25%) | 32 (26%) |
| Consolidation | 56 (53%) | 62 (50%) |
| Mass | 8 (8%) | 9 (7%) |
| Micronodule | 34 (32%) | 40 (33%) |
| Ground-glass opacity | 35 (33%) | 42 (34%) |
| Bronchiectasis | 11 (10%) | 15 (12%) |
| Bronchial thickening | 43 (41%) | 47 (38%) |
| Plate-like atelectasis | 50 (47%) | 61 (50%) |
Frequencies of lesions detected on CT associated with each type of alteration of progressive increase in lucency of the vertebral bodies recorded by Readers 1 and 2 are listed in Tables 4 and 5.
Table 4.
Abnormalities detected on CT in patients with absent progressive increase in lucency of the vertebral bodies
| Diagnostic performance indicators | Reader 1 | Reader 2 |
|---|---|---|
| Consolidation | 4 | 10 |
| Mass | 2 | 1 |
| Micronodule | 5 | 9 |
| Ground-glass opacity | 9 | 14 |
| Bronchial wall-thickening | 5 | 10 |
| Bronchiectasis | 2 | 7 |
| Plate-like atlectasis | 6 | 15 |
| Pleural effusion | 6 | 13 |
| Pleural thickening | 3 | 6 |
Table 5.
Abnormalities detected on CT in patients with inversed progressive increase in lucency of the vertebral bodies
| Diagnostic performance indicators | Reader 1 | Reader 2 |
|---|---|---|
| Consolidation | 52 | 52 |
| Mass | 6 | 8 |
| Micronodule | 29 | 29 |
| Ground-glass opacity | 26 | 28 |
| Bronchial wall-thickening | 38 | 37 |
| Bronchiectasis | 9 | 8 |
| Plate-like atlectasis | 44 | 46 |
| Pleural effusion | 55 | 53 |
| Pleural thickening | 15 | 19 |
DISCUSSION
This study shows that (1) depending on the reader, but without statistical difference between them, the sensitivity and the specificity of the spine sign for detecting lower lobe abnormalities range, respectively, from 60% to 70% and from 64% to 84%, and its positive- and negative-predictive values range, respectively, from 91% to 97% and from 19% to 29%; (2) the spine sign is associated with various lesions among which lower lobe consolidation and pleural effusion are the most common.
Only one previous study has reported the diagnostic performance of the spine sign. Defining this sign as an abnormal opacity overlying the vertebral column and considering CT as the method of reference, McDonald et al3 reported a sensitivity of 87% and a specificity of 70%. In that study, posteroanterior (PA) and lateral views were read in consensus by non-radiologist readers with no knowledge of the CT results. These investigators considered only the reports of the CT scans as the method of reference but did not reread the scans. In that study, interreader agreement was only moderate. Our study involved radiologists as readers, and we could have expected better interreader agreements than between non-radiologist readers. We did not observe any impact of the reader on the diagnostic performance excepted for accuracy, the agreement between them was moderate when the progressive increase in lucency of the vertebral bodies was normal, and even good when inversed, but it was poor when absent. A possible cause of this observation is the high subjectivity in assessing the darkness of the vertebral bodies that is not objectively measurable.
Among the 25 patients with normal CT scans, we observed, depending on the reader, false-positive results in 4 and 9 patients. Among them, degenerative features of the thoracic spine, tortuous aorta or elevated hemidiaphragm that could explain the falsely positive sign were detected. In the study by McDonald et al, degenerative features of the thoracic spine and abnormal hemidiaphragm were also related to positive spine sign. Among the 175 patients with abnormal CT scans, we observed, depending on the reader, false-negative results in 52 and 69 patients. The falsely negative sign could be explained by the size and the attenuation of the abnormalities detected on CT: ground-glass opacity, micronodules, bronchial thickening and/or plate-like atelectasis are easily missed on lateral views. Pleural effusions were missed in 19–22% of patients. We can assume that the small pleural effusions were being missed on lateral views. An abnormality too anterior to affect the progressive increase in lucency of the vertebral bodies could be another cause of false-negative spine sign.
We attempted to explain the occurrence of the spine sign by findings detected on CT scans, but we could not demonstrate any strong association between this occurrence and a specific abnormal CT finding. This could be explained by the coexistence of several abnormalities on most of our abnormal CT scans. However, consolidation and pleural effusion are most often associated with the alteration of the progressive increase in lucency of the vertebral bodies. We indeed observed that absent or inversed progressive increases in lucency of the vertebral bodies are, respectively, most commonly associated with ground-glass opacity or consolidation and pleural effusion.
The diagnostic performance of the spine sign should be considered in the debate on the usefulness of the lateral chest view.11 The main reason for not performing the lateral view is to spare radiation dose. According to data collected by the National Radiological Protection Board in UK, the radiation doses delivered by PA and lateral chest views are, respectively, 0.02 and 0.04 mSv.12 Previous studies have addressed the value of the lateral view in specific conditions such as left lower lobe pneumonia. Ely et al13 have investigated whether the lateral view (and in particular the spine sign) offered an advantage to family physicians for the diagnosis of left lower lobe pneumonia, compared with clinical findings combined with the reading by two radiologists as Ely et al.13 These authors used receiver operating characteristic curve methodology to compare the PA and lateral views. This study shows that the lateral view does not affect the accuracy of the interpretation by board-certified family physicians in patients with left lower lobe pneumonia—the lateral view being helpful in some but misleading in others. In that study, radiologists were focused on only detecting pneumonia and were not blinded for PA view results. In contrast to this study, ours included patients with various disorders—with and without chest abnormalities—and our readers were blinded for the results of PA view as well as CT scan. CT scans were moreover read separately and independently by a third reader who was blinded to the aims of this study.
Our study has several limitations. First, we selected patients who underwent CT for various indications based on clinical and/or radiographic findings and did not include normal controls. Nevertheless, it would have been unethical to obtain a CT scan as the standard of reference in individuals who did not need any chest radiographs or CT scans. Second, most patients with community-acquired pneumonia or simple pleural effusions will not undergo a CT scan. Thus, the applicability of this study to the general population is limited. Third, owing to the small number of patients presenting each type of CT findings, we were not able to determine the value of the spine sign for predicting each CT finding. Fourth, abnormalities causing the spine sign could be decreased or modified between radiographs and CT acquisitions. Fifth, our method does not reflect the real clinical practice in which both PA and lateral views are never interpreted separately.
In conclusion, the spine sign can present as an absent or inversed progressive increase in lucency of the vertebral bodies. It has a moderate sensitivity but a good positive-predictive value, so it can be useful especially when it appears as inversed progressive increase in lucency of the vertebral bodies to detect various abnormalities usually identifiable on chest radiographs.
Contributor Information
M Medjek, Email: mmedjek@me.com.
M Hackx, Email: maxime.hackx@ulb.ac.be.
B Ghaye, Email: benoit.ghaye@uclouvain.be.
V De Maertelaer, Email: vdemaert@ulb.ac.be.
P A Gevenois, Email: pierre.alain.gevenois@erasme.ulb.ac.be.
REFERENCES
- 1.Eisenberg RL. Atlas of signs in radiology. Philadelphia, PA: Lippincott; 1984. [Google Scholar]
- 2.Collins J, Stern EJ. Chest radiology: the essentials. 2nd edn. Philadelphia, PA: Lippincott; 2007. [Google Scholar]
- 3.McDonald DR, Detsky ME, Baerlocher MO, Detsky AS. Clinical utility of abnormal opacity overlying the vertebral column on lateral chest radiography. J Hosp Med 2009; 4: E15–19. doi: 10.1002/jhm.500 [DOI] [PubMed] [Google Scholar]
- 4.Fisher RA, Yates F. Statistical Tables for Biological, Agricultural and Medical Research. 6th edn. Edinburgh and London, UK: Oliver and Boyd; 1963.
- 5.Resnick D. Degeneratives diseases of the vertebral column. Radiology 1985; 156: 3–14. doi: 10.1148/radiology.156.1.3923556 [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg RL. Gastrointestinal radiology: a pattern approach. 4th edn. Philadelphia, PA: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- 7.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology 2008; 246: 697–722. doi: 10.1148/radiol.2462070712 [DOI] [PubMed] [Google Scholar]
- 8.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas 1960; 20: 37–46. doi: 10.1177/001316446002000104 [DOI] [Google Scholar]
- 9.Armitage P, Colton T. Encyclopedia of biostatistics, 6 volume set. New York, NY: Wiley; 1998. [Google Scholar]
- 10.Dawson B, Trapp RG. Basic and clinical biostatistics. San Mateo, CA: Appleton & Lange; 1990. [Google Scholar]
- 11.Sagel SS, Evens RG, Forrest JV, Bramson RT. Efficacy of routine screening and lateral chest views in a hospital-based population. N Engl J Med 1974; 291: 1001–4. doi: 10.1056/NEJM197411072911904 [DOI] [PubMed] [Google Scholar]
- 12.Wall BF, Hart D. Revised radiation doses for typical X-ray examinations. Report on a recent review of doses to patients from medical X-ray examinations in the UK by NRPB. National Radiological Protection Board. Br J Radiol 1997; 70: 437–9. doi: 10.1259/bjr.70.833.9227222 [DOI] [PubMed] [Google Scholar]
- 13.Ely JW, Berbaum KS, Bergus GR, Thompson BH, Levy BT, Graber MA, et al. Diagnosing left lower lobe pneumonia: usefulness of the “spine sign” on lateral chest radiographs. J Fam Pract 1996; 43: 242–8. [PubMed] [Google Scholar]