Abstract
Objective:
To review the published evidence and to determine if radiological diagnostic accuracy is compromised when images are displayed on a tablet computer and thereby inform practice on using tablet computers for radiological interpretation by on-call radiologists.
Methods:
We searched the PubMed and EMBASE databases for studies on the diagnostic accuracy or diagnostic reliability of images interpreted on tablet computers. Studies were screened for inclusion based on pre-determined inclusion and exclusion criteria. Studies were assessed for quality and risk of bias using Quality Appraisal of Diagnostic Reliability Studies or the revised Quality Assessment of Diagnostic Accuracy Studies tool. Treatment of studies was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Results:
11 studies met the inclusion criteria. 10 of these studies tested the Apple iPad® (Apple, Cupertino, CA). The included studies reported high sensitivity (84–98%), specificity (74–100%) and accuracy rates (98–100%) for radiological diagnosis. There was no statistically significant difference in accuracy between a tablet computer and a digital imaging and communication in medicine-calibrated control display. There was a near complete consensus from authors on the non-inferiority of diagnostic accuracy of images displayed on a tablet computer. All of the included studies were judged to be at risk of bias.
Conclusion:
Our findings suggest that the diagnostic accuracy of radiological interpretation is not compromised by using a tablet computer. This result is only relevant to the Apple iPad and to the modalities of CT, MRI and plain radiography.
Advances in knowledge:
The iPad may be appropriate for an on-call radiologist to use for radiological interpretation.
Consumer tablet computers can be used to access and display digital radiographic images for the purpose of radiological interpretation. Because tablet computers are portable, they have a potential role in remote, emergency diagnostic radiology services. There has been limited acceptance of smartphones for radiological interpretation because of their small screen size and limited display resolution.1 Tablet computers offer similar portability to a smartphone but with high-resolution displays and a larger viewing size.2 Hence, a tablet computer may be a more suitable display device for on-call radiologists.
The luminance and contrast properties of computer displays can vary considerably causing inconsistent display of images between devices. The accepted process for achieving consistent display of medical images is by calibration of the display device to the digital imaging and communication in medicine (DICOM) greyscale display function (GSDF).3 Conformance to the GSDF has been shown to improve diagnostic accuracy.4,5 A primary display is a dedicated medical display device and is used by radiologists for primary diagnosis. Whereas, a secondary display is often a commercial-off-the-shelf computer display. Established guidelines recommend conformance to the GSDF should be better than 10% and 20% for primary and secondary displays, respectively.6 Whilst both primary and secondary liquid crystal display (LCD) devices can be calibrated to the GSDF, it is not possible to calibrate a tablet computer, which may potentially compromise accuracy.7 Despite the inability to calibrate the display, high levels of diagnostic accuracy have been reported when using tablet computers.8–10 Hence, there is contradictory information to inform practice on the use of tablet computers for radiological interpretation.
To date, there has been no attempt to synthesize the existing research evidence pertaining to diagnostic accuracy or diagnostic reliability of using tablet computers for radiological interpretation. The aim of this study was to systematically review the published literature to determine if diagnostic accuracy is compromised when images are displayed on a tablet computer, which would in turn inform practice on the appropriateness of an on-call radiologist using a tablet computer for radiological interpretation.
METHODS AND MATERIALS
Search strategy
We searched the PubMed and EMBASE databases using a combination of keywords, Medical Subject Headings (MeSH) and Emtree terms for radiology, teleradiology and tablet computers (Table 1). The MeSH and Emtree terms for tablet computers are handheld computer and microcomputer, respectively. The results were constrained to the articles published in the past 10 years. Searches were conducted in January 2015.
Table 1.
Query syntax
| Database | Syntax |
|---|---|
| PubMed | ( ( (“radiology”[MeSH Terms] OR “radiology”[All Fields]) OR (“radiography”[MeSH Terms] OR “radiography”[All Fields]) OR (“teleradiology”[MeSH Terms] OR “teleradiology”[All Fields]) ) AND ( (“computers, handheld”[MeSH Terms] OR “computers, handheld”[All Fields]) OR “handheld device”[All Fields] OR “mobile device”[All Fields] OR “tablet computer”[All Fields] OR ipad[All Fields] ) AND “last 10 years”[PDat] ) |
| Embase | ( ( (“radiology”/exp OR radiology) OR (“teleradiology”/exp OR teleradiology) ) AND (“microcomputer”/exp OR “microcomputer”) AND [2005–2015]/py ) |
Inclusion and exclusion criteria
We included studies published in peer-reviewed journals that examined either the diagnostic accuracy or the diagnostic reliability of radiological interpretation of images displayed on a tablet computer. Diagnostic reliability refers to the agreement between two or more observations of the same entity and is often reported as interrater or intrarater reliability.11 Whereas, diagnostic accuracy is the likelihood of the interpretation being correct when compared with an independent standard.12 For the purpose of this review, we defined a tablet computer as a hand-held or portable computer with a screen size of 7-inches or more. This criterion excluded studies of images displayed on smartphones, personal digital assistants and the Apple iPod® (Apple, Cupertino, CA). The modalities of diagnostic radiology, namely, plain film radiography, CT, ultrasonography, nuclear imaging or MRI were included. Dental imaging was excluded as it was not considered likely to be reported by an on-call radiologist. Studies that tested imaging that was performed on patients were included. Studies where the imaging was on phantoms or synthesized were excluded. Studies that were reported in languages other than English, conference proceedings, commentary and letters to the editor were also excluded.
Selection process
Two reviewers screened the title and abstract of studies to determine eligibility for inclusion. Screening the full text of articles was performed if the abstract did not provide sufficient information to judge eligibility. Uncertainty of inclusion was resolved by consensus discussion.
Data extraction and quality assessment
The full text of studies that met the inclusion criteria was obtained and data extracted. Data were extracted on study characteristics (year, country where the study was conducted, methodology, case metrics, reader selection and reporting instrument), outcome measures, technology (intervention display device and reference standard display device), results summary and secondary observations on the use of tablet computers for radiological diagnosis.
To evaluate the included studies for quality and risk of bias, we used two methods. The Quality Appraisal of Reliability Studies (QAREL)11 was used to assess diagnostic reliability studies, and the revised Quality Assessment of Diagnostic Accuracy Studies tool (QUADAS-2)13 was used to assess diagnostic accuracy studies. Two tools were necessary because studies of diagnostic reliability contain unique design features that are not represented on tools that assess the quality of studies investigating diagnostic accuracy.14 The QUADAS-2 tool must be tailored to each review by adding or removing signalling questions.13 Table 2 lists the signalling questions that have been added or removed during tailoring of the QUADAS-2 tool to our review.
Table 2.
Review-specific modifications to the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool
| Signalling questions | Modification to QUADAS-2 toola |
|---|---|
| Domain 1: case selection | |
| Was a consecutive or random sample of cases selected? | NC |
| Was a case–control design avoided? | NC |
| Did the study avoid inappropriate exclusions? | NC |
| Was a spectrum of disease severity included in the case selection? | + |
| Was a sample size of 50 or more cases used in the study? | + |
| Domain 2: index test | |
| Were the index test results interpreted without knowledge of the results of reference test? | NC |
| If a threshold was used, was it pre-specified | − |
| Was an entire rating scale rather than a binary scale used to record index text diagnosis? | + |
| Was the instrument used to record their diagnosis calibrated with the instrument used by the gold standard readers? | + |
| Was the study reader selection for the index test representative of a radiologist population (in terms of number of readers and range of experience)? | + |
| Was the study reader for the index test given the same referral information and previous imaging as the reference test reader? | + |
| Was the index test diagnosis not limited to a type(s) of pathology? | + |
| Was the index test read with comparable monitor luminance and ambient lighting to the reference test? | + |
| Was the case order randomized? | + |
| Were all index test outcomes reported? | + |
| Domain 3: reference test | |
| Is the reference standard likely to correctly classify the target condition? | − |
| Were the reference standard results interpreted without the knowledge of the results of the index test? | NC |
| Did all cases have a reference test? | NC |
| Was the gold standard diagnosis validated—for example, by consensus of multiple radiologists or review of clinical notes? | + |
| Domain 4: flow and timing | |
| Was there an appropriate interval between index test and reference standard? | − |
| Was there an appropriate interval between index test reading and reference test reading to address retained information? | + |
| Did all cases receive a reference standard? | NC |
| Was the same reference test used for all cases? | NC |
| Were all cases included in the analysis? | NC |
+, signalling question added; −, signalling question removed; NC, no change from default tool.
One reviewer independently performed data extraction, and quality and risk of bias assessment. A second reviewer validated the recorded information.
Analysis
For multireader, multicase (MRMC) receiver operating characteristic (ROC) studies, we calculated the 95% confidence interval (when not reported by the study's author) to aid comparability of area under the ROC curve measures. Similarly, the 95% confidence interval for sensitivity and specificity was calculated. Synthesis of results was performed narratively. Reporting of the findings of this review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
RESULTS
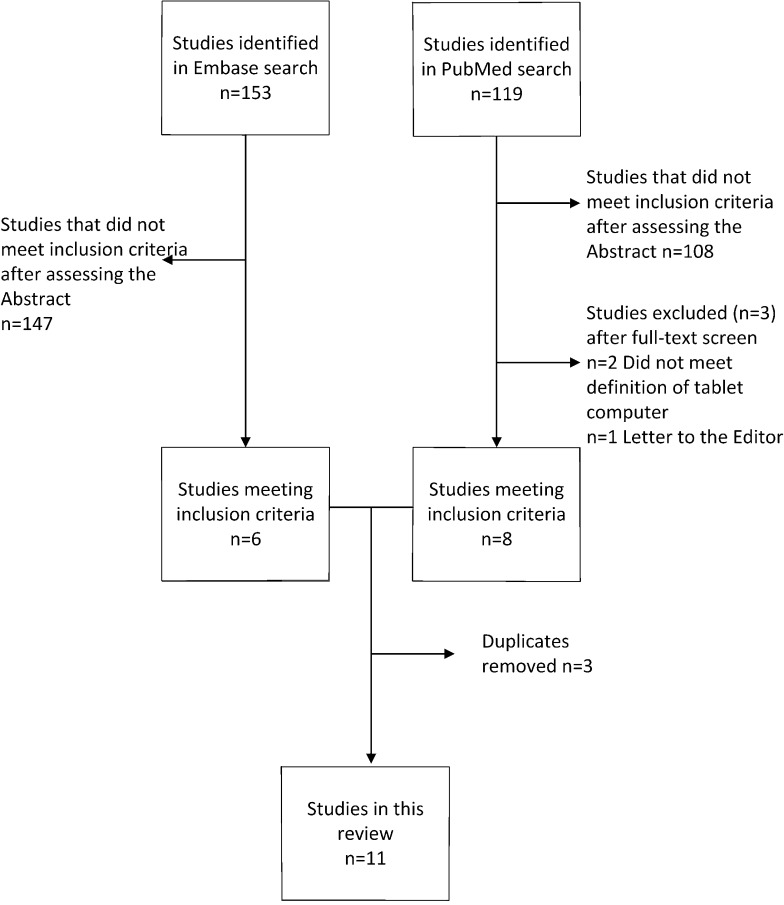
We identified 11 studies that met our inclusion criteria. The results for each stage of our search and screening processes are shown in the PRISMA flow diagram (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Study characteristics
The Apple iPad (Apple) was the intervention display in 10 studies. These studies were published between 2011 and 2013. One study evaluated an iPad with a retina display (screen matrix of 2048 × 1536 pixels).15 The resolution of the iPads in the other nine studies was 1024 × 768 pixels. The only other tablet computer tested was a Hewlett-Packard® TC1000 (Hewlett-Packard, Palo Alto, CA) tablet with a resolution of 1024 × 768 pixels.16 This study was published in 2005.
Studies originated from eight countries (United States, Ireland, Germany, Singapore, India, Taiwan, Republic of Korea and Japan). Two of the included studies evaluated large matrix plain film radiographs while the remaining studies evaluated small matrix (CT and MRI) images (Table 3). Radiologists were the readers in all but one study. Emergency department physicians were used in the remaining study (Table 4).8 Half of the studies compared the interpretation of images displayed on a tablet computer with the interpretation of images displayed on a primary picture archiving and communication system display. The remaining studies used a secondary LCD as the reference standard display (Table 5). The ambient lighting was controlled in six of the studies,9,10,15,17,19 whereas other authors intentionally used conventional lighting conditions to imitate conditions under which the tablet computer would be used.2,8 The remaining studies did not state lighting conditions.
Table 3.
Case selection summary
| Study | Examination | Pathology | Case selection rationale | Case sample size | Pathology positive (%) | Pathology negative (%) |
|---|---|---|---|---|---|---|
| Abboud et al17 | CXR | TB | Random selection of CXR from a pool of 500 TB screening cases | 240 | 40 (17%) | 200 (83%) |
| McNulty et al9 | MRI lumbar spine; MRI cervical spine | Four possible pathologies—spinal cord compression, spinal cord oedema, cauda equina syndrome, spinal cord haemorrhage | Arbitrarily selected cases from actual emergency MRI for spinal trauma. Selection designed to include pathology from emergency presentations plus normal control cases | 31 | 13 (42%) | 18 (58%) |
| Tewes et al15 | CT head; CTPA | Cerebral infarction; segmental or subsegmental PE | Arbitrarily selected cases designed to emulate typical ED cases and pathologies. Cases were actual cases performed as out-of-hours emergency imaging and included both positive and negative cases | 40 CT head; 40 CTPA | 20 (50%) CT head; 20 (50%) CTPA | 20 (50%) CT head; 20 (50%) CTPA |
| Panughpath et al10 | CT head | ICH | Random selection from an emergency radiology imaging database | 100 | 27 (27%) | 73 (73%) |
| Johnson et al18 | CTPA | Pulmonary embolism | Existing set of 50 cases of imaging for suspected PE originally compiled for QA program. The selection included both positive and negative. Positive cases ranged in subtleness of pathology from easy (main pulmonary artery) to difficult (subsegmental thrombi) | 50 | 25 (50%) | 25 (50%) |
| Yoshimura et al19 | CT head | Cerebral infraction | Arbitrarily selected cases after searching reporting database and electronic medical record for cases of suspected cerebral infarction. Selection included both positive and negative cases | 97 | 47 (48%) | 50 (52%) |
| Park et al8 | CT head | Intracranial haemorrhage | Arbitrarily selected cases from actual CT head performed in ED for trauma or headache. Cases had subtle radiological signs of ICH. Subtle meant 1st or 2nd year ED resident had missed the ICH. 10 cases were paediatric to reflect real practice of emergency radiology | 100 | 50 (50%) | 50 (50%) |
| John et al2 | CT and MRI | Common ED pathologies | Arbitrarily selected cases of common after-hours pathology that had been clinically interpreted after hours by one particular senior radiologist. The interpretation of this radiologist was used as the gold standard diagnosis | 88 (79 CT, 9 MRI) | 64 (73%) | 24 (27%) |
| McLaughlin et al1 | CT head | Various | 100 consecutive CT brain studies referred from the ED | 100 | 57 (57%) | 43 (43%) |
| Bhatia et al20 | CTBA; MR spine cervical; MR spine thoracic; MRI spine lumbar; MRI brain | Acute ischaemic event | Arbitrarily selected cases from patients that undergone ED imaging for an acute central nervous system event | 50 CTBA; 50 MRI brain; 50 MRI spine | 26 (52%) CTBA; not stated MRI brain; not stated MRI spine | 24 (48%) CTBA; not stated MRI brain; not stated MRI spine |
| Lee et al16 | AXR | Urolithiasis | Consecutive cases for patients referred for intravenous urography | 160 renal systems (80 AXR) | 28 (18%) renal stone; 24 (15%) ureteric stone | 132 (82%) kidney; 136 (85%) ureters |
AXR, abdominal radiograph; CTBA, CT brain angiography; CTPA, CT pulmonary angiogram; CXR, chest radiograph; ED, emergency department; ICH, intracranial haemorrhage; PE, pulmonary embolism; TB, tuberculosis; QA, quality assurance.
Table 4.
Reader metrics
| Study | Reference standard | Number of reference standard readers |
Index test readers and profession |
Index test reader attributes |
Index test instrument |
|---|---|---|---|---|---|
| Abboud et al17 | NA | NA | Five radiologists | Two chest fellowship, two fellowship trainees and one resident | Binary (positive/negative) |
| McNulty et al9 | Radiologist working in consensus | Two | 13 radiologists | 12 board-certified neuroradiology experts, 1 board-certified spinal and musculoskeletal expert | Six-point confidence scale |
| Tewes et al15 | NA | NA | Three radiologists | Three radiologists with 3, 4 and 6 years' experience, respectively | Five-point confidence scale |
| Panughpath et al10 | Discordant studies assessed by fellowship-trained neuroradiologist | Two | Two radiologists | Not reported | Binary (positive/negative) plus type categories, e.g. extradural, subdural, subarachnoid, intraparenchymal or intraventribular |
| Johnson et al18 | Cases reported as clinically positive were further reviewed | Three (one initial clinical radiologist plus two additional) | Two radiologists | Two fellowship trained but junior radiologists | Binary (positive/negative) |
| Yoshimura et al19 | Radiologists working in consensus plus accuracy of report confirmed by MRI and clinical records | Two | Nine radiologists | Six general radiologists and three neuroradiologists with 3–17 years' experience | Continuous confidence scale |
| Park et al8 | Neuroradiologist | One | Five emergency department physicians | Three attending and two senior residents | Five-point confidence scale |
| John et al2 | Clinical report of non-study senior radiologist | One | Three radiologists | Three attending with at least 10 years' experience each | Descriptive report. Non-study radiologist classified discrepant diagnosis as major or minor |
| McLaughlin et al1 | Clinical report of radiologist | One | Two radiologists | Two radiologists with 5 and 16 years' experience | Descriptive report. Discrepancies classified according to American College of Radiologist's RadPeer classification system |
| Bhatia et al20 | NA | NA | Five radiologists | One board-certified neuroradiologist, three fourth-year radiology residents and one second-year radiology resident | Binary (positive/negative) plus type categories, e.g. disc herniation and/or reason category, e.g. gradient echo signal abnormality |
| Lee et al16 | Results of IVU study (as opposed to plain AXR) and clinical records | One | Two radiologists | Not reported | Five-point confidence scale |
AXR, abdominal radiograph; IVU, intravenous urography; NA, not applicable.
Table 5.
Results summary
| Study | Reference standard display | Radiographic examination | Interrater reliability tablet (K) | Interrater reliability reference standard display (K) | Intrarater reliability (K) | Sensitivity tablet | Sensitivity reference standard display | Specificity tablet | Specificity reference standard display | AUC ROC tablet | AUC ROC reference standard display |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Abboud et al17 | Secondary LCD | Chest radiograph | 0.865 | 0.817 | 0.830 | NR | NR | NR | NR | NR | NR |
| Tewes et al15 | Primary display | CT head | 0.330 | 0.320 | 0.520 | NR | NR | NR | NR | NR | NR |
| Primary display | CTPA | 0.690 | 0.600 | 0.670 | NR | NR | NR | NR | NR | NR | |
| Bhatia et al20 | Secondary LCD | CT brain angiography, MRI brain and MR spine | NR | NR | >0.75 | NR | NR | NR | NR | NR | NR |
| Park et al8 | Secondary LCD—GSDF calibrated | CT head | NR | NR | 0.597 | 0.850 | 0.850 | 0.790 | 0.800 | 0.935 | 0.900 |
| McNulty et al9 | Secondary LCD—GSDF calibrated | MRI spine including lumbar and cervical | NR | NR | NR | 0.842 | 0.824 | 0.740 | 0.786 | 0.878 | 0.887 |
| Panughpath et al10 | Secondary LCD | CT head | NR | NR | NR | 0.960 | NR | 1.00 | NR | NR | NR |
| Johnson et al18 | Primary display | CTPA | NR | NR | NR | 0.980 | 1.00 | 0.980 | 0.960 | NR | NR |
| Yoshimura et al19 | Primary display—GSDF calibrated | CT head | NR | NR | NR | NR | NR | NR | NR | 0.839 | 0.875 |
| Primary display—gamma calibrated | CT head | NR | NR | NR | NR | NR | NR | NR | 0.839 | 0.884 | |
| Lee et al16 | Primary—CRT | AXR (renal calculi) | NR | NR | NR | NR | NR | NR | NR | 0.924 | 0.927 |
| Primary—CRT | AXR (ureteral calculi) | NR | NR | NR | NR | NR | NR | NR | 0.828 | 0.783 |
AUC, area under the curve; AXR, abdominal radiograph; CRT, cathode ray tube; CTPA, CT pulmonary angiogram; GSDF, greyscale display function; LCD, liquid crystal display; NR, not reported; ROC, receiver operating characteristic.
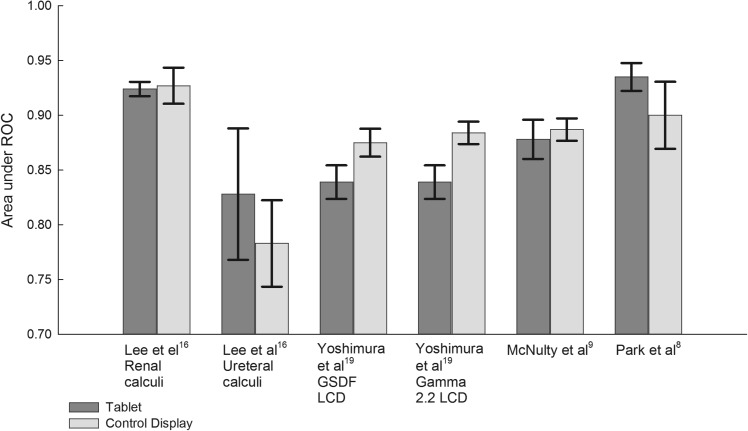
Diagnostic accuracy and diagnostic reliability
Eight of the included studies were diagnostic accuracy studies and three were diagnostic reliability studies. Different methodologies were used to test diagnostic accuracy. The diagnostic accuracy was assessed using MRMC ROC curve in four of the included studies.8,9,16,19 In these studies, the diagnosis from images displayed on a tablet computer was compared with the gold standard diagnosis (Table 4). The difference in area under the binormal ROC curve (AUROC) was used to test significance (Figure 2). No difference of statistical significance was found in five of the six studies (Table 6). Yoshimura et al19 did find the AUROC was significantly smaller for an iPad than for a gamma 2.2-calibrated LCD. The same author found no statistical difference between an iPad and DICOM GSDF-calibrated LCD. Lee et al16 found that the tablet computer performed better than the control display when assessing abdominal radiographs for ureteral calculi, whereas the control display (a GSDF-calibrated cathode ray tube monitor) was superior to the tablet for diagnosis of the renal calculi.
Figure 2.
Comparison between mean binormal area under the receiver operating characteristic (ROC) curves for tablet and control display (error bars are 95% confidence intervals). GSDF, greyscale display function; LCD, liquid crystal display.
Table 6.
Significance test summary
| Study | Significance test | Significance level | p-value | Author's conclusions |
|---|---|---|---|---|
| McNulty et al9 | DBM MRMC difference in mean AUC | 5% |
p(random readers and case) = 0.6696; p(fixed readers random case) = 0.5961; p(random readers fixed cases) = 0.6696 |
NSD diagnostic accuracy between tablet and secondary display |
| Tewes et al15 | Wilcoxon (U) rank-sum test for Likert scale evaluations; t-test (t1) for difference in mean correlation coefficient and t-test (t2) for difference in mean kappa score | 5% |
p(U) > 0.05; p(t1) > 0.05; p(t2) > 0.05 |
NSD between the tablet and primary display for both CT head and CTPA |
| Panughpath et al10 | Fisher's exact test | NR | p(F) < 1.00 | NSD between the table and secondary display for the detection of intracranial haemorrhage |
| Johnson et al18 | Difference in se, sp and ac | NR |
p(se) = 1.0; p(sp) = 1.0; p(ac) = 1.0 |
NSD in sensitivity, specificity and accuracy between a tablet and primary display |
| Yoshimura et al19 | DBM MRMC difference in mean AUC (tablet vs GSDF-calibrated primary display); DBM MRMC difference in mean AUC (tablet vs gamma-calibrated primary display; ANOVA |
5% |
p(tablet vs GSDF-calibrated primary display) > 0.05; p(tablet vs gamma-calibrated primary display) < 0.05; p(ANOVA) = 0.06 |
NSD between tablet and GSDF primary display; AUC was statistically smaller for the tablet when compared with gamma-calibrated primary display; ANOVA showed NSD between all three displays |
| Park et al8 | McNemar's test for difference in se and sp DBM MRMC difference mean AUC |
NR |
p(se) = 1.00; p(sp) = 0.885; p(AUC) = 0.183 |
NSD between iPad® and calibrated secondary liquid crystal display |
| Lee et al16 | Difference in AUC | 5% | NR | NSD between tablet and primary CRT for the detection of urolithiasis |
ac, accuracy; ANOVA, analysis of variance; AUC, area under receiver operating characteristic curve; CRT, cathode ray tube; CTPA, CT pulmonary angiogram; DBM, Dorfman-Berbaum-Metz; GSDF, greyscale display function; MRMC, multireader multicase; NR, not reported; NSD, no significant difference; se, sensitivity; sp, specificity.
iPad in the table refers to the Apple iPad (Apple, Cupertino, CA).
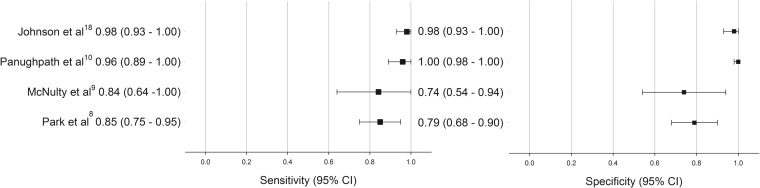
The included studies reported high sensitivity and specificity for tablet computers with values ranging from 84% to 98% and from 74% to 100%, respectively (Figure 3).8–10,18 Two of the studies that measured sensitivity and specificity also performed significance testing. No significant difference in sensitivity and specificity between a tablet computer and control display was found.8,18 Johnson et al18 reported the same accuracy rate (98%) for interpretation of CT scans for pulmonary emboli performed on an iPad and on a primary display. Panughpath et al10 reported an accuracy rate of 99.86% and 99.92% for the iPad and a secondary display, respectively, for the detection of intracranial haemorrhage on CT. In the studies performed by John et al2 and McLaughlin et al,1 the study readers produced a descriptive diagnosis that was compared with the formal clinical report. Discrepancies between the reader's diagnosis and clinical diagnosis were classified by a non-study reader. John et al2 reported 3.4% major (finding would affect immediate clinical management) discrepancy rate and a 5.6% minor (would not affect immediate clinical management) discrepancy rate when using a tablet computer. McLaughlin et al1 categorized discrepancies according to the American College of Radiologist's RadPeer classification system. There were 12 errors (3 clinically significant and 9 not clinically significant) when using the control display and 7 errors (3 clinically significant and 4 not clinically significant) when using a tablet computer. Interrater reliability was almost identical between index and reference standard for the studies by Abboud et al17 and Tewes et al15 (Table 5).
Figure 3.
Sensitivity and specificity of interpretation on tablet display [error bars are 95% confidence intervals (CIs)].
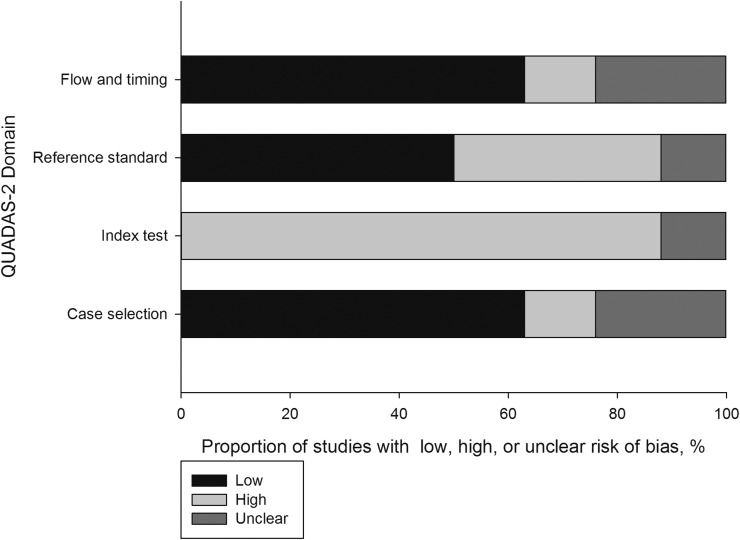
Quality and risk of bias
The eight diagnostic accuracy studies1,2,8–10,15,18,19 were assessed with the QUADAS-2 tool for quality and risk of bias. All eight studies were judged high or unclear in at least one domain. Proportions of studies for each of the risk of bias classifications are shown in Figure 4. A large proportion of these studies (88%) were judged to have a high risk of bias for the index test domain. This was owing to a number of reasons, including the index test readers not having sufficient number or range of experience to represent a radiologist population; the index test readers not having the same referral information and access to previous imaging as the reference test readers; the index test reader's diagnosis being limited to known type of pathology; and the monitor luminance and ambient lighting of the index test not being comparable to the reference test.
Figure 4.
Summary of Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) assessments for risk of bias.
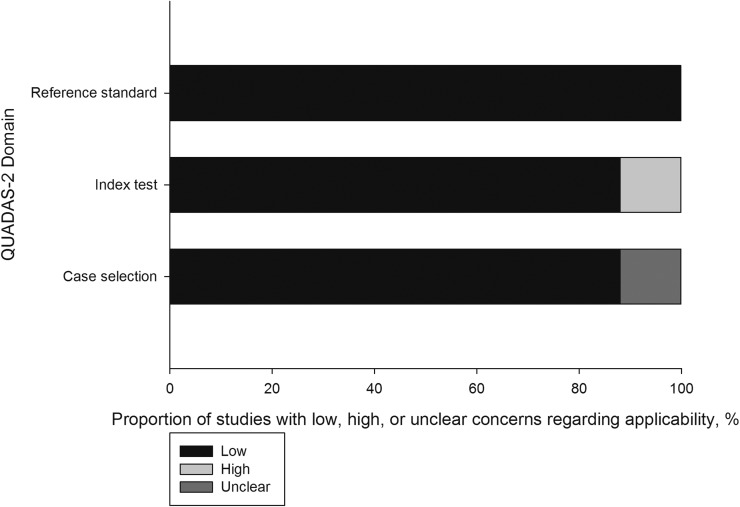
All studies in the reference standard domain and most studies (88%) in both the index test and case selection domain were judged to be applicable to the review question for all QUADAS-2 domains (Figure 5).
Figure 5.
Summary of the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) assessment for applicability.
The three diagnostic reliability studies15,17,20 were assessed using the QAREL tool. All studies had at least one item judged to indicate a poor quality in the study. The reasons for poor quality included readers not being representative of the review's population, blinding of referral and clinical information, non-randomization of reading order and the use of binary scales by study readers.
Synthesis
The results of studies included in this review could not be statistically combined. This was owing to the heterogeneity of study designs (accuracy and reliability studies), methodologies, display characteristics of intervention tablet computer and reference standard display device, profession of readers, lighting conditions and radiographic modality (large matrix and small matrix) all being evaluated.
DISCUSSION
This review revealed a near complete consensus from the study authors on the non-inferiority of diagnostic accuracy of images displayed on a tablet computer. The included studies reported high sensitivity (84–98%), specificity (74–100%) and accuracy rates (98–100%) when using a tablet computer for radiological diagnosis. There was no statistically significant difference in accuracy between tablet computers and GSDF-calibrated control displays. All of the included studies were judged to be at risk of bias. The included studies were judged to have high applicability to the review question.
The MRMC ROC method has been used in four of the included studies.8,9,16,19 All authors of MRMC ROC studies have used an entire rating scale rather than a binary scale that conforms with best practice recommendations.21 A number of studies have validated the gold standard diagnosis by using multiple readers or reviewing clinical notes (Table 4). The use of multiple readers has been shown to increase the reliability of radiological diagnosis.22 Park et al8 found the interpretation on the iPad had greater diagnostic accuracy than did a GSDF-calibrated secondary LCD. However, in this study, the luminance of the reference test LCD was set to 170 cd m−2 compared with the 400 cd m−2 on the iPad. Furthermore, the reading was performed under conventional lighting. Hence, it would be reasonable to expect inferior performance from a low luminance monitor in high ambient lighting. Yoshimura et al19 concluded that the diagnostic accuracy of images displayed on an iPad was significantly less than when displayed on a Gamma 2.2-calibrated LCD, but not significantly less than when displayed on a GSDF-calibrated monitor. DICOM GSDF is the most widely used calibration technique used in radiology today.23 There appears to be some limitation in the methods used by McLaughlin et al1 who classified discrepancies. The limitation has been caused by the index test and reference test instrument not being calibrated. This lack of calibration has resulted in inconsistency when grading discrepancies for incidental findings, e.g. mucosal thickening. This inconsistency obscures whether discrepancies are attributable to the display or a difference in radiologist's reporting style. Most authors used arbitrarily selected cases, which may not be a true representation of positive-to-negative case ratios. The use of only subtle pathology in one study may have resulted in under reporting of the accuracy rate.8 In many of the studies, the reader was blinded to clinical details of the referral and did not have access to prior imaging. In other studies, the readers were aware of a limited type of pathology in which the studies needed to be reported. Both scenarios may affect interpretative performance. The reader population was not representative of a radiologist population in a number of studies—for example, McNulty et al9 used 13 subspecialists as the study readers; whereas, only two readers were used in other studies.1,10,16,18 The use of a subspecialist may result in overreporting of diagnostic accuracy. The authors of nearly all studies have minimized bias of retained information by including a time delay between readings. To further reduce bias from the retained information, some authors have randomized the reading order (tablet vs control) and randomized the case order.17
Many authors identified the likely application of a tablet computer was for remote on-call interpretation of emergency imaging and chose cases and pathology relevant to this situation.1,2,8–10,15,18,20 Hence, the included studies were judged to have a high applicability to the review question. The exceptions were the study by Abboud et al,17 which tested the reliability of TB screening; the use of emergency department physicians as the study readers by Park et al;8 and the accuracy of diagnosing urolithiasis from the abdominal radiographs16 (which has in a large part been replaced by CT imaging24).
The studies were undertaken in eight countries indicating the international interest in the use of tablet computers for diagnostic radiology. The US Food and Drug Administration have cleared the use of the Apple iPad for primary radiological diagnosis. However, the clearance is limited to use with a Mobile MIM (MIM Software, Cleveland, OH) software application, small-matrix images and situations where there is no access to a primary diagnostic display.25 To the best of our knowledge, there is no similar approval in any other country. In the UK and Germany, regulatory guidelines prevent tablet computers being used for primary diagnosis owing to screen size.15,26
Secondary observations on the use of tablet computers were elicited in many of the studies. The various software applications were criticised by a number of authors for the difficulty in scrolling and touch movements, cumbersome user interface (especially when trying to compare previous imaging), the lack of post-processing tools and instability (especially for large studies).1,2,8 Limitations in network coverage and speed, potential effect of ambient lighting on diagnosis were also noted.8,15,20 The inability to access clinical systems for referral information and prior studies1 and the increased time to perform a read compared with primary workstation19 were other limitations of using tablet computers. The portability and fast boot time were seen as the major advantage of tablet computers.8,10,27
This review has a number of limitations. There were only a small number of heterogeneous studies, which made consolidation of results difficult. The small sample size and the large number of studies judged to be at risk of bias may reduce confidence in the findings of this review. The iPad was assessed in 10 out of 11 studies. Hence, the findings are only applicable to this device. There is currently no evidence in favour of, or against, the use of any other makes or models of tablet computer. Similarly, the findings are only applicable to modalities tested in the included studies, namely CT, MRI and plain radiography.
CONCLUSION
In conclusion, the findings of this review suggest that the diagnostic accuracy of radiological interpretation was not compromised by using a tablet computer to interpret CT, MRI or plain radiography. This conclusion is only applicable to the Apple iPad and indicates this device is suitable for an on-call radiologist to display images for interpretation. The conclusions were based on studies that were judged to be at risk of bias. There were low concerns regarding the applicability of the included studies to the review question. The use of tablet computers for a primary diagnosis may be subject to local regulatory guidelines. When considering the usage of a tablet computer for on-call radiology, the user also needs to assess the software functionality—for example, access to referral information and previous imaging; software stability and network performance. These have all been identified by the authors of included studies as potential impediments in using a tablet computer for radiological interpretation.
Contributor Information
L J Caffery, Email: l.caffery@coh.uq.edu.au.
N R Armfield, Email: N.R.Armfield@uq.edu.au.
A C Smith, Email: a.smith@uq.edu.au.
REFERENCES
- 1.Mc Laughlin P, Neill SO, Fanning N, McGarrigle AM, Connor OJ, Wyse G, et al. Emergency CT brain: preliminary interpretation with a tablet device: image quality and diagnostic performance of the Apple iPad. Emerg Radiol 2012; 19: 127–33. doi: 10.1007/s10140-011-1011-2 [DOI] [PubMed] [Google Scholar]
- 2.John S, Poh AC, Lim TC, Chan EH, Chong le R. The iPad tablet computer for mobile on-call radiology diagnosis? Auditing discrepancy in CT and MRI reporting. J Digit Imaging 2012; 25: 628–34. doi: 10.1007/s10278-012-9485-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fetterly KA, Blume HR, Flynn MJ, Samei E. Introduction to grayscale calibration and related aspects of medical imaging grade liquid crystal displays. J Digit Imaging 2008; 21: 193–207. doi: 10.1007/s10278-007-9022-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buls N, Shabana W, Verbeek P, Pevenage P, De Mey J. Influence of display quality on radiologists' performance in the detection of lung nodules on radiographs. Br J Radiol 2007; 80: 738–43. doi: 10.1259/bjr/48049509 [DOI] [PubMed] [Google Scholar]
- 5.Krupinski EA, Roehrig H. The influence of a perceptually linearized display on observer performance and visual search. Acad Radiol 2000; 7: 8–13. doi: 10.1016/s1076-6332(00)80437-7 [DOI] [PubMed] [Google Scholar]
- 6.Samei E, Badano A, Chakraborty D, Compton K, Cornelius C, Corrigan K, et al. ; AAPM TG18. Assessment of display performance for medical imaging systems: executive summary of AAPM TG18 report. Med Phys 2005; 32: 1205–25. doi: 10.1118/1.1861159 [DOI] [PubMed] [Google Scholar]
- 7.Yamazaki A, Liu P, Cheng WC, Badano A. Image quality characteristics of handheld display devices for medical imaging. PLoS One 2013; 8: e79243. doi: 10.1371/journal.pone.0079243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park JB, Choi HJ, Lee JH, Kang BS. An assessment of the iPad 2 as a CT teleradiology tool using brain CT with subtle intracranial hemorrhage under conventional illumination. J Digit Imaging 2013; 26: 683–90. doi: 10.1007/s10278-013-9580-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McNulty JP, Ryan JT, Evanoff MG, Rainford LA. Flexible image evaluation: iPad versus secondary-class monitors for review of MR spinal emergency cases, a comparative study. Acad Radiol 2012; 19: 1023–8. doi: 10.1016/j.acra.2012.02.021 [DOI] [PubMed] [Google Scholar]
- 10.Panughpath SG, Kumar S, Kalyanpur A. Utility of mobile devices in the computerized tomography evaluation of intracranial hemorrhage. Indian J Radiol Imaging 2013; 23: 4–7. doi: 10.4103/0971-3026.113610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lucas NP, Macaskill P, Irwig L, Bogduk N. The development of a quality appraisal tool for studies of diagnostic reliability (QAREL). J Clin Epidemiol 2010; 63: 854–61. doi: 10.1016/j.jclinepi.2009.10.002 [DOI] [PubMed] [Google Scholar]
- 12.Kundel HL, Polansky M. Measurement of observer agreement. Radiology 2003; 228: 303–8. doi: 10.1148/radiol.2282011860 [DOI] [PubMed] [Google Scholar]
- 13.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. ; QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011; 155: 529–36. doi: 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 14.Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003; 3: 25. doi: 10.1186/1471-2288-3-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tewes S, Rodt T, Marquardt S, Evangelidou E, Wacker FK, von Falck C. Evaluation of the use of a tablet computer with a high-resolution display for interpreting emergency CT scans. Rofo 2013; 185: 1063–9. doi: 10.1055/s-0033-1350155 [DOI] [PubMed] [Google Scholar]
- 16.Lee W-J, Lee H-T, Ching Y-T, Tsai C-H, Liu H-M, Chen S-J. Tablet PC as a PACS workstation: observer performance evaluation. Chin J Radiol 2005; 30: 277–81. [Google Scholar]
- 17.Abboud S, Weiss F, Siegel E, Jeudy J. TB or Not TB: interreader and intrareader variability in screening diagnosis on an iPad versus a traditional display. J Am Coll Radiol 2013; 10: 42–4. doi: 10.1016/j.jacr.2012.07.019 [DOI] [PubMed] [Google Scholar]
- 18.Johnson PT, Zimmerman SL, Heath D, Eng J, Horton KM, Scott WW, et al. The iPad as a mobile device for CT display and interpretation: diagnostic accuracy for identification of pulmonary embolism. Emerg Radiol 2012; 19: 323–7. doi: 10.1007/s10140-012-1037-0 [DOI] [PubMed] [Google Scholar]
- 19.Yoshimura K, Nihashi T, Ikeda M, Ando Y, Kawai H, Kawakami K, et al. Comparison of liquid crystal display monitors calibrated with gray-scale standard display function and with γ 2.2 and iPad: observer performance in detection of cerebral infarction on brain CT. AJR Am J Roentgenol 2013; 200: 1304–9. doi: 10.2214/AJR.12.9096 [DOI] [PubMed] [Google Scholar]
- 20.Bhatia A, Patel S, Pantol G, Yen-ying W, Plitnikas M, Hancock C. Intra and inter-observer reliability of mobile tablet PACS viewer system vs. standard PACS viewing stations-diagnosis of acute central nervous system events. Open J Rad 2013; 3: 91–8. doi: 10.4236/ojrad.2013.32014 [DOI] [Google Scholar]
- 21.Skaron A, Li K, Zhou XH. Statistical methods for MRMC ROC studies. Acad Radiol 2012; 19: 1499–507. doi: 10.1016/j.acra.2012.09.005 [DOI] [PubMed] [Google Scholar]
- 22.Espeland A, Vetti N, Kråkenes J. Are two readers more reliable than one? A study of upper neck ligament scoring on magnetic resonance images. BMC Med Imaging 2013; 13: 4. doi: 10.1186/1471-2342-13-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hirschorn DS, Krupinski EA, Flynn MJ. PACS displays: how to select the right display technology. J Am Coll Radiol 2014; 11: 1270–6. doi: 10.1016/j.jacr.2014.09.016 [DOI] [PubMed] [Google Scholar]
- 24.Levine JA, Neitlich J, Verga M, Dalrymple N, Smith RC. Ureteral calculi in patients with flank pain: correlation of plain radiography with unenhanced helical CT. Radiology 1997; 204: 27–31. doi: 10.1148/radiology.204.1.9205218 [DOI] [PubMed] [Google Scholar]
- 25.US Food and Drug Administration. FDA clears first diagnostic radiology application for mobile devices. 2011. [Updated 4 February 2011; cited 1 January 2015.] Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm242295.htm
- 26.Royal College of Radiologists, Board of the Faculty of Clinical Radiology. Picture archiving and communication systems (PACS) and guidelines on diagnostic display devices. [Updated 1 November 2012; cited 1 January 2015.] Available from: http://www.rcr.ac.uk/sites/default/files/docs/radiology/pdf/BFCR%2812%2916_PACS_DDD.pdf
- 27.Yoshimura K, Shimamoto K, Ikeda M, Ichikawa K, Naganawa S. A comparative contrast perception phantom image of brain CT study between high-grade and low-grade liquid crystal displays (LCDs) in electronic medical charts. Phys Med 2011; 27: 109–16. doi: 10.1016/j.ejmp.2010.06.001 [DOI] [PubMed] [Google Scholar]